Assessment of neurocognitive impairment after off-pump and on-pump techniques for coronary artery bypass graft surgery: prospective randomised controlled trial (original) (raw)
Abstract
Objective
To assess neurocognitive impairment after the off-pump and on-pump techniques for coronary artery bypass graft surgery in patients with triple vessel disease.
Design
Randomised controlled trial.
Setting
University Hospital of Wales, Cardiff.
Participants
60 patients undergoing coronary artery bypass graft surgery for triple vessel disease prospectively randomised to the off-pump or on-pump technique.
Main outcome measures
Change in scores in nine standard neuropsychometric tests administered preoperatively and at 1 and 10 weeks postoperatively.
Results
The on-pump group showed a significantly greater deterioration in scores for two and three tests at 1 week and 10 weeks postoperatively, respectively, than the off-pump group. The on-pump group also showed a significantly higher incidence of major deterioration in one of the tests both 1 week and 10 weeks postoperatively. The incidence of neurocognitive impairment at 1 week postoperatively was 27% (8 out of 30) in the off-pump group and 63% (19 out of 30) in the on-pump group (P=0.004); and at 10 weeks postoperatively was 10% (3 out of 30) in the off-pump group and 40% (12 out of 30) in the on-pump group (P=0.017).
Conclusion
Off-pump coronary artery bypass graft surgery results in less neurocognitive impairment than the on-pump technique.
What is already known on this topic
Neurocognitive impairment after coronary artery bypass graft surgery occurs in a major proportion of patients
Cardiopulmonary bypass has been implicated, but the evidence is inconclusive
What this study adds
Off-pump coronary artery bypass graft surgery results in less neurocognitive impairment than the on-pump technique
Introduction
Coronary artery bypass graft surgery is one of the most commonly performed procedures. Advances in surgical techniques, anaesthetic management, and postoperative care resulted in a steady decline in mortality from the procedure during the 1980s and '90s, despite a gradual increase in the risk profile of patients.1 Neurological injury is an important complication after coronary artery bypass graft surgery. It comprises two types.2 Type 1 injury includes stroke, transient ischaemic attack, and coma (incidence 3 to 6%). Type 2 injury is more subtle and includes impairment of cognitive function. These are defects associated with attention, concentration, short term memory, fine motor function, and speed of mental and motor responses. The incidence of neurocognitive impairment after cardiac surgery varies from 20% to 80%.3–6 These defects are not always transient, and longitudinal assessment studies have shown a major impairment at 5 years7,8; impairment immediately after surgery has been shown to correlate with long term impairment.8 Recent work has focused on the role of cardiopulmonary bypass in neurocognitive impairment, but the literature is inconclusive.6,9–11 In recent years coronary artery bypass graft surgery without using cardiopulmonary bypass (off-pump technique) has been shown to be a reliable and reproducible technique, and both short and medium term results have been favourable.12,13
Patients with single and double vessel disease are increasingly being managed by percutaneous coronary interventions. Most patients undergoing coronary artery bypass graft surgery have triple vessel disease. We aimed to assess the impact of the on-pump and off-pump techniques on neurocognitive impairment in patients undergoing coronary artery bypass graft surgery for triple vessel disease.
Methods
Patient selection
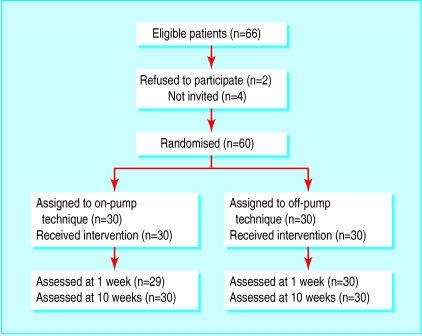
We enrolled 60 patients undergoing urgent or elective coronary artery bypass graft surgery for triple vessel disease between May and October 2001. All patients gave written informed consent. We excluded patients with a greater than 50% carotid artery stenosis, recent myocardial infarction (within one month), previous transient ischaemic attack or cerebrovascular attack, previous psychiatric illness, renal failure, or those who needed emergency operation, reoperation, or combined valvular surgery. We screened 76 patients; 10 had one or more of the exclusion criteria leaving 66 eligible for randomisation (figure). Two patients refused to take part and four were not invited because they were last minute additions to the operating list and therefore precluded performance of the neuropsychometric tests. We randomised the patients into two groups using sequentially numbered, sealed, opaque envelopes containing computer generated random allocations. We randomised 30 patients to receive conventional on-pump coronary artery bypass graft surgery (group A) and 30 to receive the off-pump technique (group B). The operations were performed by one surgeon (VZ) at the University Hospital of Wales, Cardiff. We obtained ethical approval for our study from the Bro Taf local research ethics committee.
The anaesthetic technique was standardised and all patients received the same medication. The surgical technique was standardised, the left internal mammary artery being attached to the left anterior descending artery, and vein grafts to the other coronary arteries as appropriate in all patients. In both groups the top end anastomoses were constructed with the help of a side biting clamp. The only difference between the two groups was the use of cardiopulmonary bypass. Cardiotomy suction was not used in the on-pump group. In both groups the cell saver was used.
Neuropsychometric assessment
We carried out nine neuropsychometric tests to assess the patients both preoperatively and at 1 week and 10 weeks postoperatively. A qualified examiner (CC), blinded to treatment allocation, carried out the tests in a standardised fashion, in the same order. The battery of tests included the core tests according to the recommendations of the statement of consensus on assessment of neurobehavioural outcomes after cardiac surgery.14 The tests comprised the Rey auditory verbal learning test, part A and part B of the trail making test, the digit symbol substitution test, the digit span forward and the digit span backward test, the grooved pegboard test using the dominant hand and the non-dominant hand, and the controlled oral word association test. We estimated the premorbid full scale IQ by using the national adult reading test.15
Statistical analysis
We expressed continuous data as means (standard deviations) and compared them by using the independent sample t test or Mann-Whitney U test as appropriate. We compared proportions with χ2 tests with continuity correction or Fisher's exact test as appropriate.
The primary outcome variable was the change in scores at 10 weeks from preoperative levels, assessed by repeated measures analysis of variance with post hoc comparison and Bonferroni correction. We considered a patient to have major deterioration in a particular test if the score deteriorated by 1 SD of the baseline score of all patients.16 We considered a patient to have neurocognitive impairment if there was a major deterioration in two or more tests.16 We used the χ2 test to compare the proportion of patients with neurocognitive deterioration in the two groups.
Our sample size was based on data obtained from a previous non-randomised study performed in our department (unpublished data). The standardised difference was 1. To achieve a power of 87% we needed 40 patients (20 per group), with an α error set at 0.05 (two sided). Overall, we recruited 60 patients (30 in each group) to allow for loss to follow up and conversions to the other technique during surgery.
We performed all analyses with the SPSS10 software package. We present 95% confidence intervals for the main results. We considered a P value of <0.05 as significant.
Results
Table 1 shows the patient characteristics in both groups. Both groups were similar for age, sex, angina class, left ventricle function, and extent of coronary artery disease, and they had a similar number of grafts (table 2). Neither group had any deaths, major neurological complications, or perioperative myocardial infarctions (based on electrocardiographic evidence only). Intubation time and length of hospital stay were shorter in the off-pump group than in the on-pump group but did not reach significance. Significantly fewer patients in the off-pump group required blood transfusion. Both groups had similar baseline scores for the neuropsychometric tests and full scale IQ (table 3).
Table 1.
Preoperative clinical data. Values are numbers of patients unless stated otherwise
| Variable | On-pump (n=30) | Off-pump (n=30) |
|---|---|---|
| Mean (SD) age (years) | 61.6 (10) | 63.5 (9.1) |
| Male | 27 | 25 |
| Angina class: | ||
| Grade 1 | 0 | 0 |
| Grade 2 | 8 | 5 |
| Grade 3 | 19 | 22 |
| Grade 4 | 3 | 3 |
| Three vessel disease | 30 | 30 |
| Left main stem lesion (>50%) | 2 | 4 |
| Left ventricular function (ejection fraction): | ||
| Good (>50%) | 23 | 23 |
| Fair (30-50%) | 5 | 6 |
| Poor (<30%) | 2 | 1 |
Table 2.
Operative details and postoperative details. Values are numbers of patients unless stated otherwise
| Variable | On-pump (n=30) | Off-pump (n=30) | P value |
|---|---|---|---|
| Mean (SD) No of grafts; range | 2.93 (0.45); 2-4 | 2.93 (0.37); 2-4 | 1 |
| No of grafts: | |||
| 2 grafts | 4 | 2 | |
| 3 grafts | 24 | 26 | |
| 4 grafts | 2 | 1 | |
| Mean (SD) cross clamp time (min); range | 29.9 (8.9); 20-62 | ||
| Mean (SD) cardiopulmonary bypass time (min); range | 54.7 (14.8); 36-104 | ||
| Low cardiac output: | 0.34 | ||
| Ionotropes | 7 | 4 | |
| Intra-aortic balloon pump | 0 | 0 | |
| Postoperative atrial fibrillation | 10 | 4 | 0.18 |
| Transfused patients | 23 | 10 | 0.01 |
| Mean (SD) ventilation (h) | 10.7 (7.8) | 7.9 (9.4) | 0.23 |
| Mean (SD) discharge (days) | 9 (5.5) | 7.6 (2.7) | 0.23 |
Table 3.
Mean (SD) preoperative scores for all tests, and full scale IQ and mean differences for all tests*
| Test | Mean (SD) preoperative scores | Mean difference 7 days postoperatively | Mean difference 10 weeks postoperatively | |||||
|---|---|---|---|---|---|---|---|---|
| Off-pump (n=30) | On-pump (n=30) | Off-pump (n=30) | On-pump (n=29) | P value | Off-pump (n=30) | On-pump (n=30) | P value | |
| Rey auditory verbal learning test | 36 (8.83) | 35.2 (8.99) | −1.20 (4.1) | −2.58 (10.0) | 0.98 | 2.60 (9.2) | 1.33 (8.0) | 0.99 |
| Part A of trail making test | 43.57 (15.41) | 40.37 (14.22) | −6.20 (17.8) | −13.55 (15.5) | 0.20 | 3.00 (8.6) | 1.63 (13.0) | 0.99 |
| Part B of trail making test | 98.30 (36.09) | 94.93 (34.99) | −17.96 (53.1) | −33.41 (34.4) | 0.38 | −0.26 (19.9) | −27.24 (31.0) | <0.002 |
| Grooved pegboard test using dominant hand | 99.93 (48.52) | 91.20 (38.05) | −5.33 (32.5) | −13.44 (37.2) | 0.76 | 4.20 (14.1) | −20.70 (22.9) | <0.002 |
| Grooved pegboard test using non-dominant hand | 109.37 (37.99) | 106.57 (42.45) | −4.53 (26.0) | −32.27 (35.2) | 0.002 | 3.63 (15.2) | 0.80 (36.2) | 0.99 |
| Digit symbol substitution test | 42.47 (10.23) | 42.80 (18.19) | −1.50 (8.1) | −7.34 (9.6) | 0.028 | 2.83 (6.7) | −4.06 (8.1) | 0.002 |
| Digit span forward test | 9.00 (2.48) | 8.97 (2.37) | −0.26 (1.9) | −0.75 (2.5) | 0.78 | 0.36 (1.4) | −0.16 (2.0) | 0.54 |
| Digit span backward test | 6.43 (2.27) | 6.57 (2.47) | −0.02 (1.8) | −1.14 (2.9) | 0.14 | 0.67 (1.3) | 0.97 (0.9) | 0.84 |
| Controlled oral word association test | 40.97 (10.49) | 40.93 (16.01) | 0.23 (7.8) | −0.79 (16.8) | 0.99 | 2.23 (7.9) | 1.66 (10.4) | 0.99 |
| Full scale IQ | 114.9 (8.81) | 114.16 (8.24) |
Change in scores
One patient in the on-pump group was not tested 1 week postoperatively because of tiredness and loss of motivation. All patients were tested 10 weeks postoperatively. At 1 week postoperatively the on-pump group showed a significantly greater deterioration in scores in the grooved pegboard test using the non-dominant hand and the digit symbol substitution test than the off-pump group. At 10 weeks postoperatively the on-pump group showed a significantly greater deterioration in part B of the trail making test, the grooved pegboard test using the dominant hand, and the digit symbol substitution test (table 3).
Patients with 1 SD or more deterioration in individual tests
One week postoperatively two patients (7%) in the off-pump group and 14 patients (48%) in the on-pump group showed a deterioration of 1 SD or more in the grooved pegboard test using the non-dominant hand (P=0.001; table 4). Ten weeks postoperatively no patient in the off-pump group and six patients (20%) in the on-pump group showed a deterioration of 1 SD or more in the grooved pegboard test using the dominant hand (P=0.03). In the other tests the difference in the proportion of patients in each group did not reach significance.
Table 4.
Percentage of patients in each group who had deterioration ⩾1 standard deviation in individual tests at 1 week and 10 weeks postoperatively
| Test | 1 week postoperatively | 10 weeks postoperatively | ||||||
|---|---|---|---|---|---|---|---|---|
| Off-pump (n=30) | On-pump (n=29) | Difference | Off-pump (n=30) | On-pump (n=30) | Difference | |||
| % | 95% CI | % | 95% CI | |||||
| Rey auditory verbal learning test | 13.3 | 34.5 | 21.2 | (−0.7 to 41.0) | 10.0 | 23.3 | 13.3 | (−6.1 to 32.1) |
| Part A of trail making test | 26.7 | 44.8 | 18.2 | (−6.0 to 39.8) | 6.7 | 16.7 | 10.0 | (−7.4 to 27.6) |
| Part B of trail making test | 23.3 | 44.8 | 21.5 | (−2.6 to 42.6) | 10.0 | 30.0 | 20.0 | (−0.5 to 39.0) |
| Grooved pegboard test using dominant hand | 13.3 | 31.0 | 17.7 | (−3.7 to 37.6) | 0 | 20.0 | 20.0 | (4.5 to 37.3)* |
| Grooved pegboard test using non-dominant hand | 6.7 | 48.3 | 41.6 | (19.3 to 59.6)* | 3.3 | 16.7 | 13.3 | (−2.9 to 30.5) |
| Digit symbol substitution test | 6.7 | 24.1 | 17.5 | (−1.4 to 36.1) | 3.3 | 13.3 | 10.0 | (−5.6 to 26.6) |
| Digit span forward test | 10.0 | 27.6 | 17.6 | (−2.7 to 36.9) | 0 | 10.0 | 10.0 | (−3.1 to 25.6) |
| Digit span backward test | 6.7 | 20.7 | 14.0 | (−4.2 to 32.4) | 0 | 0 | 0 | (−11.4 to 11.4) |
| Controlled oral word association test | 6.7 | 27.6 | 20.9 | (1.4 to 39.7)* | 3.3 | 10.0 | 6.7 | (−8.2 to 22.5) |
Patients with neurocognitive impairment
Patients were considered to have neurocognitive impairment if they showed a deterioration of 1 SD or more in two or more tests. One week postoperatively eight patients (27%) in the off-pump group and 19 (66%) in the on-pump group (P=0.004) had neurocognitive impairment. Ten weeks postoperatively three patients (10%) in the off-pump group and 12 (40%) in the on-pump group (P=0.017) had neurocognitive impairment.
Discussion
The incidence of neurocognitive impairment after coronary artery bypass graft surgery varies noticeably between studies.3–5,16 This is because of variations in the tests used, the time points of assessment, the definition of impairment, and the statistical methods used for comparing groups.16
We found significantly less neurocognitive impairment 1 week and 10 weeks after off-pump coronary artery bypass graft surgery for patients with triple vessel disease. Previous studies have shown equivocal results. One prospective randomised study found increased concentrations of S100 protein, a marker of neurological injury, in the on-pump group, but no difference in neurocognitive impairment.11 The definition of neurocognitive impairment was, however, unclear. More than 60% of patients recruited in that study had single or double vessel disease. Another study found a higher concentration of serum S100 protein, a higher number of high intensive transient signals picked up by transcranial Doppler, and an increased incidence of neurocognitive impairment in the on-pump than off-pump group.9 This was a randomised study including 40 patients. The neuropsychological assessment was limited to the preoperative period and 1 week postoperatively, and the tests used did not conform to the consensus statement.14 In one randomised controlled trial, neurocognitive outcome was assessed in 281 patients, using 10 neuropsychometric tests.6 Improved cognitive outcomes were found in the off-pump group at 3 months, but the effects were limited and became negligible at 12 months. A significant proportion of the patients in this study had single and double vessel disease (76%); only 24% had triple vessel disease. Anaesthetic management differed between the groups: 99% of patients in the on-pump group received total intravenous anaesthesia including high dose opioids, and 54% of patients in the off-pump group received thoracic epidural anaesthesia.
Strengths of study
Overall, we included 91% of eligible patients in our trial. The operations were performed by a single surgeon (VZ). We standardised anaesthetic and surgical factors that might lead to cerebral injury. Both groups underwent the same surgical procedure, including the use of the same conduits and the same technique for proximal grafting. We included only patients with triple vessel disease. Previous studies have included a significant proportion of patients with single or double vessel disease.6,9–11 No cross over occurred. None of the patients in the off-pump group required conversion to on-pump surgery. Follow up was 100% at 10 weeks. Our prospective randomised trial produced two similar groups (table 1). We are thus confident that cardiopulmonary bypass was the only major difference between our study groups.
Limitations of study
One limitation of our study is that a single surgeon operating in a single hospital, with standardisation of the anaesthetic and surgical techniques allows reproducibility of findings, but generalisability is affected. Our findings need to be tested in a multicentric study with different surgeons and hospitals. Aortic atherosclerosis is an important factor in neurological and neurocognitive outcomes. We did not use epiaortic scanning or transoesophageal echocardiography to detect aortic atherosclerosis. Our patients were assessed only at 1 week and 10 weeks postoperatively. Although outcomes at 10 weeks may reflect more important longer term outcomes, they may not necessarily reflect any permanent sequelae. The incidence of neurocognitive outcome decreased from 1 to 10 weeks; future studies need to incorporate longer term follow up.
Cardiopulmonary bypass has been implicated in the pathogenesis of neurocognitive impairment. Various mechanisms are responsible, including hypoperfusion during cardiopulmonary bypass, venous hypertension due to manipulation of the heart during surgery, emboli originating from the cardiopulmonary bypass circuit and the ascending aorta, and systemic inflammatory response syndrome leading to cerebral swelling and an increase in the permeability of the blood-brain barrier.17–22
Neuropsychometric testing and the measurement of serum levels of biochemical markers (S100β and neurone specific enolase) are two ways of measuring neurological injury. Neuropsychometric tests assess specific domains of the brain, whereas the serum markers assess global injury. Two studies showed an association between neurocognitive impairment and S100β and neurone specific enolase levels.14,15 Others have found no such association.11,23 Administering a comprehensive battery of neuropsychometric tests is time consuming. Development of a serum marker or a computerised objective test that could be administered in less time and that correlated well with the severity of neuropsychometric impairment would improve the work of future researchers. At present, comprehensive neuropsychometric tests need to be administered to assess neurocognitive impairment.
We found one notable difference between our patient population and those in other studies. The average IQ of our patients was 115, higher (107 and 108) than in other studies.10,20 It is possible that the slightly higher incidence of neurocognitive impairment in our patients could be related to a higher premorbid IQ. One study found a higher composite neurocognitive score at baseline to be a significant predictor of change in the composite cognitive index.7
Figure.
Flow of participants through trial
Acknowledgments
We thank Gwen Phillips (Department of Neuropsychology, University Hospital of Wales) for advice on the neuropsychometric tests.
Editorial by Taggart
Footnotes
Funding: The Welsh Office for Research and Development provided £22 000 ($34 206; €34,854) towards the study. It had no role in the conduct of the study, interpretation of the results, or the decision to send the study for publication.
Competing interests: None declared.
References
- Keogh BE, Kinsman R on behalf of the Society of Cardiothoracic Surgeons of Great Britain and Ireland. National adult cardiac surgical database report 1999-2000; 133.
- 2.Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, et al. Adverse cerebral outcomes after coronary bypass surgery. N Engl J Med. 1996;335:1857–1863. doi: 10.1056/NEJM199612193352501. [DOI] [PubMed] [Google Scholar]
- 3.Vingerhoets G, Van Nooten G, Vermassen F, De Soete G, Jannes C. Short-term and long-term neuropsychological consequences of cardiac surgery with extra-corporeal circulation. Eur J Cardiothorac Surg. 1997;11:424–431. doi: 10.1016/s1010-7940(96)01031-7. [DOI] [PubMed] [Google Scholar]
- 4.Shaw PJ, Bates D, Cartlidge NEF, French JM, Heaviside D, Julian DG, et al. An analysis of factors predicting neurological injury in patients undergoing coronary bypass operations. Q J Med. 1989;72:633–646. [PubMed] [Google Scholar]
- 5.McKhann GM, Goldsborough MA, Borowicz Jr LM, Selnes OA, Mellits D, Enger C, et al. Cognitive outcome after coronary artery bypass: a one-year prospective study. Ann Thorac Surg. 1997;63:510–515. doi: 10.1016/s0003-4975(96)01057-0. [DOI] [PubMed] [Google Scholar]
- 6.Van Dijk D, Jansen EWL, Hijman R, Nierich AP, Diephuis JC, Moons KG, et al. Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery: a randomised trial. JAMA. 2002;287:1405–1412. doi: 10.1001/jama.287.11.1405. [DOI] [PubMed] [Google Scholar]
- 7.Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, et al. Longitudinal assessment of neurocognitive function after coronary artery bypass surgery. N Engl J Med. 2001;344(6):395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 8.Sontaniemi KA, Mononen MA, Hokkanen TE. Long-term cerebral outcome after open-heart surgery: a five year neuropsychological follow-up study. Stroke. 1986;17:410–416. doi: 10.1161/01.str.17.3.410. [DOI] [PubMed] [Google Scholar]
- 9.Diegeler A, Hirsch R, Schneider F, Schilling LO, Falk V, Rauch T, et al. Neuromonitoring and neurocognitive outcome in off-pump versus conventional coronary bypass operation. Ann Thorac Surg. 2000;69:1162–1166. doi: 10.1016/s0003-4975(99)01574-x. [DOI] [PubMed] [Google Scholar]
- 10.Taggart DP, Browne SM, Halligan PW, Wade DT. Is cardiopulmonary bypass still the cause of cognitive dysfunction after cardiac operations? J Thorac Cardiovasc Surg. 1999;118:414–421. doi: 10.1016/S0022-5223(99)70177-7. [DOI] [PubMed] [Google Scholar]
- 11.Lloyd CT, Ascione R, Underwood MJ, Gardner F, Black A, Angelini GD. Serum S-100 protein release and neuropsychologic outcome during coronary revascularization on the beating heart: a prospective randomized study. J Thorac Cardiovasc Surg. 2000;119:148–154. doi: 10.1016/s0022-5223(00)70230-3. [DOI] [PubMed] [Google Scholar]
- 12.Angelini GD, Taylor FC, Reeves BC, Ascione R. Early and midterm outcome after off-pump and on-pump surgery in beating heart against cardioplegic arrest studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet. 2002;359:1194–1199. doi: 10.1016/S0140-6736(02)08216-8. [DOI] [PubMed] [Google Scholar]
- 13.Zamvar V, Khan NU, Madhavan A, Kulatilake N, Butchart EG. Clinical outcomes in coronary artery bypass graft surgery: comparison of off-pump and on-pump techniques. Heart Surgery Forum. 2002;5(2):109–113. [PubMed] [Google Scholar]
- 14.Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59:1289–1295. doi: 10.1016/0003-4975(95)00106-u. [DOI] [PubMed] [Google Scholar]
- 15.Nelson HE. Test manual. Windsor: NFER-Nelson; 1978. National adult reading test (NART) [Google Scholar]
- 16.Mahanna EP, Blumenthal JA, White WD, Croughwell ND, Clancy CP, Smith LR, et al. Defining neuropsychological dysfunction after coronary artery bypass grafting. Ann Thorac Surg. 1996;61:1342–1347. doi: 10.1016/0003-4975(95)01095-5. [DOI] [PubMed] [Google Scholar]
- 17.Taylor KM. Cardiac surgery and the brain. In: Smith P, Taylor KM, editors. Cardiac surgery and the brain. London: Edward Arnold; 1993. pp. 1–14. [Google Scholar]
- 18.Blauth CI, Arnold JV, Schulenberg WE, McCartney AC, Taylor KM. Cerebral microembolism during cardiopulmonary bypass. Retinal microvascular studies in vivo with fluorescein angiography. J Thorac Cardiovasc Surg. 1988;95:668–676. [PubMed] [Google Scholar]
- 19.Pugsley W, Klinger L, Paschalis C, Treasure T, Harrison M, Newman S. The inpact of microemboli during cardiopulmonary bypass on neuropsychological functioning. Stroke. 1994;25:1393–1399. doi: 10.1161/01.str.25.7.1393. [DOI] [PubMed] [Google Scholar]
- 20.Borger MA, Peniston CM, Weisel RD, Vasiliou M, Green REA, Feindel CM. Neuropsychologic impairment after coronary bypass surgery: effects of gaseous microemboli during perfusionist interventions. J Thorac Cardiovasc Surg. 2001;121:743–749. doi: 10.1067/mtc.2001.112526. [DOI] [PubMed] [Google Scholar]
- 21.Harris DNF, Bailey SM, Smith PLC, Taylor KM, Oatridge A, Bydder GM. Brain swelling in first hour after coronary artery bypass surgery. Lancet. 1993;342:586–587. doi: 10.1016/0140-6736(93)91412-f. [DOI] [PubMed] [Google Scholar]
- 22.Gillinov AM, Davis EA, Curtis WE, Schleien CL, Koehler RC, Gardner TJ, et al. Cardiopulmonary bypass and blood brain barrier: an experimental study. J Thorac Cardiovasc Surg. 1991;104:1110–1115. [PubMed] [Google Scholar]
- 23.Westaby S, Saatvedt K, White S, Katsumata T, van Oeveren W, Bhatnagar N, et al. Is there a relationship between S-100β protein and neuropsychologic dysfunction after cardiopulmonary bypass? J Thorac Cardiovasc Surg. 2000;119:132–137. doi: 10.1016/s0022-5223(00)70228-5. [DOI] [PubMed] [Google Scholar]