A Review of Articular Cartilage Pathology and the Use of Glucosamine Sulfate (original) (raw)
. 2001 Oct-Dec;36(4):413–419.
Abstract
Objective:
To refresh the athletic trainer's knowledge of articular cartilage biomechanics, physiology, and structure and explore the role of glucosamine sulfate in treating articular cartilage pathologic conditions, including supplementation methods and clinical outcomes.
Data Sources:
We searched MEDLINE from 1989 through 2000 and SPORT Discus from 1975 through 2000 using the following key words: glucosamine sulfate, articular cartilage, osteoarthritis, and proteoglycans.
Data Synthesis:
Articular cartilage functions as a wear-resistant, smooth, nearly frictionless, load-bearing surface. Glucosamine sulfate can be thought of as a building block that helps restore the proteoglycan-rich extracellular matrix and thus balance articular cartilage catabolism and anabolism. Beneficial clinical effects of glucosamine sulfate in the osteoarthritic population have been documented. However, the use of glucosamine sulfate for athletic articular cartilage injuries is unproved.
Conclusions/Recommendations:
Clinical studies indicate that glucosamine sulfate has been shown to be a safe and relatively effective treatment for osteoarthritis. However, no evidence to date supports or refutes a carryover effect to the athletic population and the injuries that occur in sport.
Keywords: osteoarthritis, proteoglycans, outcomes, treatment, supplements
Glucosamine sulfate is being extensively marketed as a treatment for osteoarthritis. Glucosamine is an endogenous aminomonosaccharide synthesized from glucose.1–3 It is used in the biosynthesis of proteoglycans and glycosaminoglycans (GAGs) as a proposed substrate for the synthesis of these important cartilage components and perhaps a direct stimulator of their synthesis.1–3 Glucosamine can be thought of as a building block that helps restore the proteoglycan-rich matrix and thus balance cartilage catabolism and anabolism.1–3 Glucosamine is also proposed to protect damaged cartilage from metabolic impairment.4,5
Osteoarthritis is a gradual disease characterized by a continual wearing of the articular cartilage, resulting in changes in the underlying subchondral bone.5 Management of osteoarthritis currently includes weight reduction, physical therapy, occupational therapy, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs).4 NSAIDs have been shown to have both positive and negative effects on cartilage metabolism, but neither NSAIDs nor acetaminophen has been shown to reverse the degenerative process of osteoarthritis.4
The anatomic, physiologic, and biomechanical properties of articular cartilage should be considered in treating articular cartilage pathologic conditions. Understanding these articular cartilage properties allows the athletic trainer to better appreciate how glucosamine sulfate may affect articular cartilage. The purpose of our review was to explore the relationship between articular cartilage pathology and glucosamine sulfate.
THE ROLE OF HUMAN ARTICULAR CARTILAGE
Articular cartilage functions to distribute the load, minimize peak stresses on subchondral bone, and provide a friction-reducing, weight-bearing surface. Articular cartilage can be deformed and regain its original shape, because it is remarkably elastic. In comparison with other soft tissues, articular cartilage has a low level of metabolic activity and lacks blood vessels, lymphatic vessels, and nerves. Essentially, articular cartilage functions and stands alone. The simple homogeneous appearance of cartilage hides its highly ordered complex structure. This structure apparently remains unchanged unless affected by disease or injury.6
COMPOSITION AND STRUCTURE OF ARTICULAR CARTILAGE
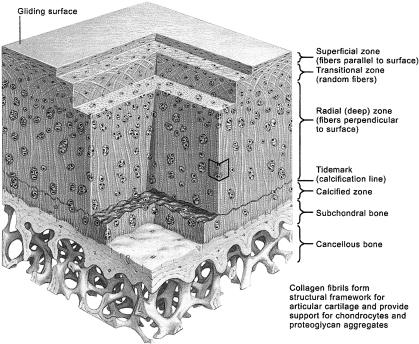
Articular cartilage is typically depicted in 4 zones (Figure). Each zone has its own distinct matrix region. The superficial zone includes the gliding surface of the joint. This layer of cell-free matrix contains fine fibrils with few polysaccharides and adjoins a layer of elongated chondrocytes organized parallel to the articular surface. The cells in this zone are almost inactive but contain endoplasmic reticulum, Golgi membranes, and mitochondria. The next layer is the transitional zone, which includes active chondrocytes containing endoplasmic reticulum, Golgi membranes, mitochondria, glycogen, and intracytoplasmic filaments. The collagen fibrils of this zone are larger than those of the superficial zone. In this layer, collagen fiber orientation transitions from parallel to columnar. The deep zone contains chondrocytes that are similar to those of the transitional zone but are organized in a columnar pattern perpendicular to the joint surface. These cells hold large amounts of intermediate filaments and glycogen granules. Furthermore, the largest collagen fibrils of articular cartilage and the highest content of proteoglycans are also contained here. As the number of proteoglycans increases, the amount of water decreases from the superficial to the deep zone. The deepest zone of calcified cartilage divides the softer cartilage from subchondral bone. The cells from the deep zone bore directly into the calcified cartilage. These chondrocytes contain little cytoplasm and almost no endoplasmic reticulum but connect the articular cartilage to the underlying bone.6
The 4 zones of articular cartilage. Copyright 1995. Reprinted with permission from Havas MediMedia, illustrated by Drs. John A. Craig and Carlos Machado. Clin Symp. 1995;47(2). All rights reserved.
A chondrocyte cell membrane adheres directly to the pericellular matrix, which contains proteoglycans, noncollagenous proteins, and glycoproteins. A layer of territorial matrix encompasses the pericellular matrix. This matrix surrounds individual cells or pairs or clusters of chondrocytes. The interterritorial matrix forms the majority of articular cartilage and accounts for its mechanical characteristics.6
Chondrocytes provide 10% or less of the total volume of cartilage; consequently, the functional properties of cartilage, including stiffness, durability, and distribution of load, rely on the extracellular matrix. Overall, tissue fluid contributes 60% to 80% of the wet weight of cartilage and contains water with dissolved gases, small proteins, and metabolites. The structural macromolecules contribute 20% to 40% of the wet weight7 and include collagens, proteoglycans, and glycoproteins. The chondrocytes and matrix depend on each other. The material properties of articular cartilage depend on its extracellular matrix, but the existence and maintenance of the matrix depend on the chondrocytes.6
BIOMECHANICAL PROPERTIES OF ARTICULAR CARTILAGE
Articular cartilage functions as a wear-resistant, smooth, nearly frictionless, load-bearing surface. The composition and physicochemical properties of articular cartilage, the fundamental organization of the collagen network, and the molecular organization of collagen and proteoglycans all have profound effects on the intrinsic mechanical properties of the extracellular matrix and the fluid transport and diffusional properties of the cartilage. These characteristics provide articular cartilage with its normal function, lubrication, wear, and load-bearing features.8
When an external load is placed on the cartilage surface, immediate deformation is produced primarily by a change in the proteoglycan molecular domain. This external load can also make the interstitial fluid pressure in the porous solid matrix exceed the osmotic swelling pressure; therefore, the interstitial fluid begins to flow and exudation occurs. After exudation occurs and the load is removed, GAGs function hydrophilically, pulling the fluid back into the cartilage, similar to the action of a sponge soaking up water, in preparation for the next load. With a decrease in the interstitial fluid, the proteoglycan concentration within the solid matrix increases, which in turn increases the osmotic swelling pressure, charge-charge repulsive force, and bulk compressive stress until they are balanced with the applied external load. In this manner, the physicochemical characteristics of the proteoglycan gel trapped within the collagen meshwork enable cartilage to resist compression. This mechanism supplements the role played by collagen fibers, which are strong in tension but can easily fold under compression.8
Articular cartilage demonstrates a viscoelastic response when placed under loads and deformation.7–10 It creeps under a constant applied load and stress relaxes under a constant applied deformation.7–10 This viscoelastic response of articular cartilage relies on 2 essentially different physical mechanisms: (1) the intrinsic viscoelastic properties of the macromolecules that form the organic solid matrix9 and (2) the frictional drag from the flow of the interstitial fluid through the permeable solid matrix.7–9 Each mechanism promotes the overall viscoelastic response of cartilage under tension, compression, and shear.8 Additionally, the rate at which a load is applied to articular cartilage affects its viscoelastic response. Under a slow, sustained force, articular cartilage is able to respond accordingly and accommodate this load. However, under a concentrated force, articular cartilage is unable to react to the load, and therefore, the tissue is vulnerable to injury.
Alterations associated with injuries, osteoarthritis, and other degenerative processes vary normal structure-function relationships that exist within the articular cartilage. Particular compositional, molecular, and structural changes detected in degenerated tissues include decreased proteoglycan and increased water content,11 collagen fibril network disorganization, and proteoglycan separation. These changes may alter the intrinsic mechanical properties of articular cartilage and produce swelling.8 The organizational structure of collagen and proteoglycans in conjunction with water normally determines the mechanical properties of articular cartilage. This structural relationship among collagen, proteoglycans, and water does not exist for healing articular cartilage or osteoarthritic cartilage.12
ARTICULAR CARTILAGE DAMAGE AND REPAIR
Acute injuries to articular cartilage can be categorized into 2 broad groups: (1) the loss of matrix macromolecules without mechanical damage to the chondrocytes or the collagen fibril meshwork (ie, prolonged joint immobilization) and (2) mechanical disruption of the chondrocytes and the extracellular matrix (ie, impact-load injury). Progressive loss of matrix macromolecules leads to mechanical disruption of the articular cartilage surface, and mechanical disruption may result in factors that stimulate matrix degeneration. Thus, the 2 groups may overlap.12
Cartilage exposure to an injurious agent can stimulate degeneration of proteoglycans or suppress proteoglycan synthesis. These insults may also have effects on the matrix and the chondrocytes, but the loss of matrix proteoglycans is the most obvious initial change. Immediate cessation of the process responsible for the loss of matrix proteoglycans allows the chondrocytes to restore the lost matrix components, perhaps allowing the articular cartilage to regain its normal composition and function. However, if this process continues, damage sustained by the articular cartilage may become irreversible.12
Blunt trauma, penetrating injuries, frictional injuries, and concentrations of weight-bearing forces destroy chondrocytes and disrupt the extracellular matrix. Physiologic levels of impact loading do not seem to cause articular cartilage damage. Blunt trauma to articular cartilage occurs often, even in the absence of fractures, and may be the cause of significant long-term joint dysfunction. The severity of acute, blunt trauma can be categorized as greater than normal loading but less than that necessary to fracture bone or cartilage or sufficient to fracture bone and cartilage. The effect of a penetrating injury depends on whether the defect is confined to the substance of the articular cartilage or extends into the subchondral bone.12
The response of articular cartilage to an injury is determined by numerous factors: the type of injury, the extent and severity of the injury, the state of the cartilage and the joint at the time of the injury, the age of the individual, and the structure, composition, function, and durability of the repair tissue. For repaired tissue to fulfill the demands of a joint surface, it must return normal, pain-free motion to the joint for an extended period and prohibit further degeneration of the joint. An abundance of methods for promoting cartilage repair have been researched. These include cartilage shaving,13–16 abrasion of subchondral bone,17–20 change in the loading of the injured articular surface,21 passive motion,22–24 resurfacing with periosteum or perichondrium,25–32 digestion or extraction of matrix proteoglycans, laser stimulation of chondrocytes,33 implantation of immature chondrocytes,34 implantation of gels,34–36 pulsed electromagnetic fields,37,38 and chondrogenesis-stimulating factors.12,39,40 Conservative measures for treating articular cartilage injury include the use of NSAIDs and chondroprotective supplements, such as glucosamine sulfate.
NATURAL PRODUCTION AND ABSORPTION OF GLUCOSAMINE SULFATE
Glucosamine is a building block for articular cartilage's extracellular matrix. Specifically, it is used to produce GAGs and proteoglycans.4,5,41–44 Glucosamine is synthesized by chondrocytes from glucose to produce GAGs,43 and the production of GAGs stimulates proteoglycan production.44 The lack of proteoglycans can lead to degeneration of articular cartilage.16 Glucosamine is present in meat, fish, poultry,45 and almost all human tissue and has a special positive attraction for cartilaginous tissue.
Glucosamine sulfate was rapidly absorbed into the bloodstream regardless of the route of administration.46 Approximately 90% of orally administered glucosamine sulfate was absorbed through the digestive tract.1 However, only 26% of this oral dose of glucosamine was available for processing by the body's tissues.47 Glucosamine concentrates in the liver, where it is combined with plasma proteins, reduced into smaller molecules, or used for other biologic processes.1,4 The highest concentrations are found in liver, kidney, and articular cartilage.4,43,46 Glucosamine is used in GAG synthesis.4
ACTION OF GLUCOSAMINE SULFATE
Glucosamine sulfate is the salt of D-glucosamine with sulfuric acid. In solution, glucosamine sulfate separates into the D-glucosamine ion and the sulfate ion.48,49 Glucosamine ions are used to synthesize GAGs, which are combined with proteins to form proteoglycans, critical components of articular cartilage ground substance. Researchers48 believe that the glucosamine ion is the active element, but some evidence indicates that a benefit of the glucosamine sulfate is related to sulfur residues, because sulfur is an essential nutrient for the stabilization of the connective tissue matrix. Glucosamine sulfate stimulates the uptake of sulfate ions,50 which can be used as an indicator of GAG synthesis by the chondrocytes.50–55 Sulfate is also an important component of proteoglycans.50–52 Glucosamine sulfate, which provides both glucosamine and sulfate ions, facilitates GAG production and synthesis of proteoglycans as a whole.49 Glucosamine also hinders hyaluronidase, the tissue-damaging enzyme, and helps to rebuild the damaged articular cartilage. In addition, glucosamine sulfate improves the lubricant properties of synovial fluid.46
THE ROLE OF GLUCOSAMINE SULFATE
Glucosamine sulfate is proposed to be a safe and effective treatment of osteoarthritis.56 Glucosamine supposedly plays a part in the repair and maintenance of joint cartilage, stimulating cartilage cells to produce GAGs and proteoglycans.57 Investigators have compared glucosamine sulfate with placebos41,49,50,58–62 and with common NSAIDs (ie, ibuprofen).42,63–66 Glucosamine sulfate has been described as a slow-acting drug in osteoarthritis by the International League Against Rheumatism.44,49,63 However, the Arthritis Foundation does not recognize glucosamine sulfate as a treatment for osteoarthritis or any other form of arthritis.3,5 The National Collegiate Athletic Association has classified glucosamine sulfate as a nonpermissible supplement for institutions to provide to their athletes.67
SUPPLEMENTATION METHODS
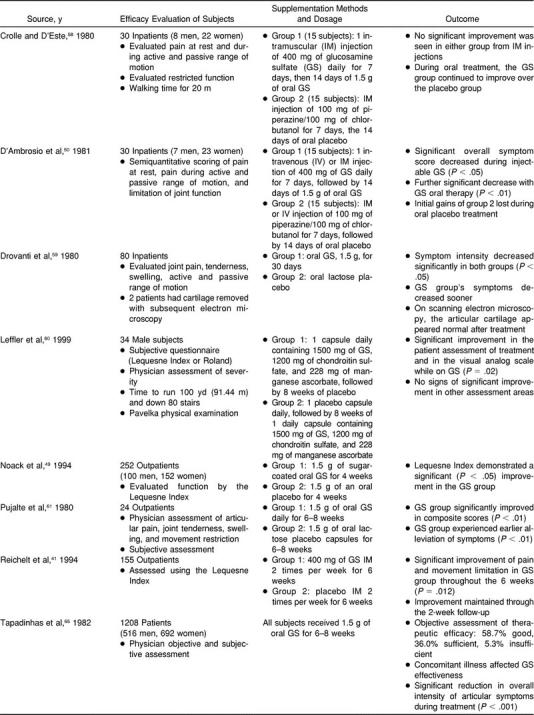
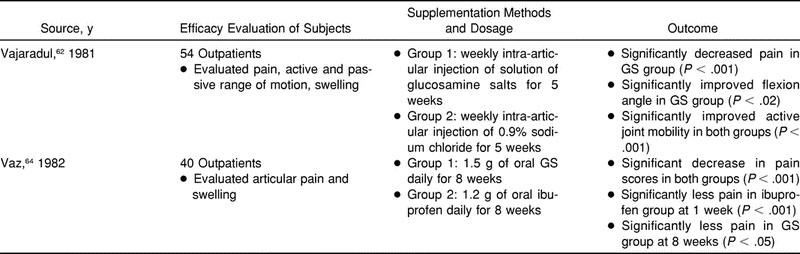
Various methods have been used to provide glucosamine supplementation to subjects (Table). These methods included oral supplements,42,46,50,58–61,63–66 intravenous injections,50 intramuscular injections,50,58 and intra-articular injections.46,62 However, oral supplementation has been deemed the most effective because of the mode of delivery and is the most commonly used method.51 The current recommended dosage is 1500 mg of glucosamine sulfate daily. This typical 1500-mg dosage is generally divided into 3 doses (500 mg each) per day.
Summary of Glucosamine Sulfate (GS) Clinical Trials
A concern with oral supplementation of glucosamine sulfate is that it does not require Food and Drug Administration approval. “The Dietary Supplement Health and Education Act of 1994 provides for the use of various types of statements on the label of dietary supplements, although claims may not be made about the use of a dietary supplement to diagnose, prevent, mitigate, treat, or cure a specific disease (unless approved under the new drug provisions of the Federal Food, Drug, and Cosmetic Act).”68 For any “dietary supplement,” the consumer should investigate the quality of the product before supplementation.5,56
TOLERANCE
All studies reported low incidence of adverse effects with glucosamine supplementation. The few adverse effects that were reported, all mild to moderate in intensity, included abdominal pain,42,65 epigastric pain or tenderness,49,64 heartburn,64 vomiting,41 diarrhea,49 nausea,41,49,64 drowsiness,42 headache,49 and itching.41,49 Increased insulin resistance has been reported after intravenous glucosamine doses in laboratory animals69 and after a 12-week course of oral glucosamine supplementation in humans.70 Insulin resistance decreases the ability of insulin receptors to transmit glucose into tissue's cells. Certainly, further investigation into this phenomenon is necessary; patients with diabetes may need to be followed closely during glucosamine treatment.
CLINICAL OUTCOMES
Bassleer et al44 showed a stimulatory effect of glucosamine sulfate on the biosynthetic activity of human chondrocytes. Their findings agree with other reports that glucosamine exerts a protective action in animal models of experimental osteoarthritis.71 Glucosamine counteracts the damage induced on chondrocytes by dexamethasone49,72 and some NSAIDs,49,55,73 and its effect in patients with osteoarthritis compares favorably with that of NSAIDs.44,49,54,55,64,74,75 Glucosamine sulfate also displays a definite, although mild, anti-inflammatory activity in in vivo models of inflammation and arthritis.49,63 Glucosamine did not show any inhibiting activities of prostaglandin biosynthesis; therefore, the mild anti-inflammatory activities described are most likely achieved through this prostaglandin-independent mechanism.49,63 This may also explain its low toxicity and better therapeutic index when compared with NSAIDs.49,63
In one study,64 NSAIDs reduced pain within 2 weeks; however, this action tended to fade away as treatment continued. Researchers concluded that treatment with glucosamine sulfate was slower to become effective, but it was consistent and progressive throughout the trial period and overall produced significantly better results than the NSAID. Additionally, the effects from treatment with glucosamine sulfate lasted longer, even after treatment was discontinued.49
Authors of recent reviews4,76 noted that the studies conducted thus far have indicated improved pain and mobility. However, Barclay et al4 reported that most of the studies have shown significant flaws in design or data analysis. Although glucosamine sulfate does not appear to have negative short-term side effects, long-term effects are unknown.4,5 Rovati51 explained that long-term studies are difficult to perform, whereas the short-term studies often have several methodologic problems. The most common problems associated with clinical trials of disease-modifying drugs in osteoarthritis can be summarized into the following categories: (1) number of patients, (2) experimental design, (3) diagnosis, (4) disease status, and (5) evaluation criteria and end points.51
One unique report has been published by Drovanti et al.59 Like many other studies, these researchers administered 1500 mg of glucosamine sulfate or an identical placebo daily. Articular pain, joint tenderness and swelling, and restriction of active or passive motion, as well as other diagnostic tests, were assessed, with promising results. However, these authors, unlike any others, also used electron microscopy scanning to evaluate the integrity of the articular cartilage surface of 5 subjects. They examined 1 healthy subject with no articular cartilage damage, 2 subjects from the placebo treatment group, and 2 subjects from the glucosamine sulfate treatment group. Glucosamine sulfate supplementation appeared to help rebuild the articular cartilage of the 2 subjects who underwent that treatment.
Studies comparing glucosamine sulfate to placebos have demonstrated significant reduction in knee pain,49,58,60–62 improved range of motion,41,50,58,60–62 decreased swelling,59,61 improved function,58,60,62 and improved patient or physician (or both) qualitative assessment.60,61 Glucosamine sulfate and NSAIDs both significantly decreased knee pain,42,63,64 decreased swelling,42 and improved patients' subjective assessments,64 but glucosamine tended to elicit greater improvements in function.42 In investigations without a control group,46,65,66 glucosamine sulfate significantly decreased pain and range-of-motion limitation and increased function. No published studies have shown that supplementation of glucosamine sulfate is an effective prophylactic measure against osteoarthritis.
CONCLUSION
Glucosamine assists the body in providing the components necessary to synthesize proteoglycans, which are required for articular cartilage synthesis. It appears to slow the process of articular degeneration and facilitate the recovery of normal joint mobility. In osteoarthritis, changes occur in the articular cartilage (due to mechanical insult) and in its metabolism. Glucosamine sulfate appears to have a positive effect on the metabolism of articular cartilage. However, whether sports injuries result in the same articular cartilage changes found in osteoarthritis is unclear. Mechanical insults associated with sports are common, but no clinical trials on this population are currently available. Further research needs to be completed on the use of glucosamine sulfate in patients without osteoarthritis.
REFERENCES
- 1.Glucosamine sulfate. Altern Med Rev. 1999;4:193–195. [PubMed] [Google Scholar]
- 2.Adams ME. Hype about glucosamine. Lancet. 1999;354:353–354. doi: 10.1016/S0140-6736(99)90040-5. [DOI] [PubMed] [Google Scholar]
- 3.Cerrato PL. Can these compounds curb arthritis? RN. 1998;61(4):57–58. [PubMed] [Google Scholar]
- 4.Barclay TS, Tsourounis C, McCart GM. Glucosamine. Ann Pharmacother. 1998;32:574–579. doi: 10.1345/aph.17235. [DOI] [PubMed] [Google Scholar]
- 5.da Camara CC, Dowless GV. Glucosamine sulfate for osteoarthritis. Ann Pharmacother. 1998;32:580–587. doi: 10.1345/aph.17214. [DOI] [PubMed] [Google Scholar]
- 6.Buckwalter J, Hunziker E, Rosenberg L, Coutts R, Adams M, Eyre D. Articular cartilage: composition and structure. In: Woo SLY, Buckwalter JA, editors. Injury and Repair of the Musculoskeletal Soft Tissues. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1988. pp. 405–425. [Google Scholar]
- 7.Mow VC, Kuei SC, Lai WM, Armstrong CJ. Biphasic creep and stress relaxation of articular cartilage in compression? Theory and experiments. J Biomech Eng. 1980;102:73–84. doi: 10.1115/1.3138202. [DOI] [PubMed] [Google Scholar]
- 8.Mow V, Rosenwasser M. Articular cartilage: biomechanics. In: Woo SLY, Buckwalter JA, editors. Injury and Repair of the Musculoskeletal Soft Tissues. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1988. pp. 427–463. [Google Scholar]
- 9.Mow VC, Holmes MH, Lai WM. Fluid transport and mechanical properties of articular cartilage: a review. J Biomech. 1984;17:377–394. doi: 10.1016/0021-9290(84)90031-9. [DOI] [PubMed] [Google Scholar]
- 10.Woo SLY, Simon BR, Kuei SC, Akeson WH. Quasi-linear viscoelastic properties of normal articular cartilage. J Biomech Eng. 1980;102:85–90. doi: 10.1115/1.3138220. [DOI] [PubMed] [Google Scholar]
- 11.Bollet AJ, Nance JL. Biochemical findings in normal and osteoarthritic articular cartilage, II: chondroitin sulfate concentration and chain length, water, and ash content. J Clin Invest. 1966;45:1170–1177. doi: 10.1172/JCI105423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buckwalter J, Rosenberg L, Coutts R, Hunziker E, Hari Reddi A, Mow V. Articular cartilage: injury and repair. In: Woo SLY, Buckwalter JA, editors. Injury and Repair of the Musculoskeletal Soft Tissues. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1988. pp. 465–482. [Google Scholar]
- 13.Johnson LL. Diagnostic and Surgical Arthroscopy. St Louis, MO: CV Mosby; 1980. [Google Scholar]
- 14.O'Donoghue DH. Treatment of chondral damage to the patella. Am J Sports Med. 1981;9:1–10. doi: 10.1177/036354658100900101. [DOI] [PubMed] [Google Scholar]
- 15.Schmid A, Schmid F. Results after cartilage shaving studied by electron microscopy. Am J Sports Med. 1987;15:386–387. [Google Scholar]
- 16.Mitchell N, Shepard N. Effect of patella shaving in the rabbit. J Orthop Res. 1987;5:388–392. doi: 10.1002/jor.1100050311. [DOI] [PubMed] [Google Scholar]
- 17.Haggart GE. The surgical treatment of degenerative arthritis of the knee joint. J Bone Joint Surg. 1940;22:717–729. [Google Scholar]
- 18.Insall J. The Pridie debridement operation for osteoarthritis. Clin Orthop. 1974;101:61–67. [PubMed] [Google Scholar]
- 19.Magnuson PB. Joint debridement: surgical treatment of degenerative arthritis. Surg Gynecol Obstet. 1941;73:1–9. [PubMed] [Google Scholar]
- 20.Mitchell N, Shepard N. The resurfacing of adult rabbit articular cartilage by multiple perforations through the subchondral bone. J Bone Joint Surg Am. 1976;58:230–233. [PubMed] [Google Scholar]
- 21.Radin EL, Burr DB. Hypothesis: joints can heal. Semin Arthritis Rheum. 1984;13:293–302. doi: 10.1016/0049-0172(84)90031-3. [DOI] [PubMed] [Google Scholar]
- 22.DePalma AF, McKeever CD, Subin DK. Process of repair of articular cartilage demonstrated by histology and autoradiography with tritiated thymidine. Clin Orthop. 1966;48:229–242. [PubMed] [Google Scholar]
- 23.Salter RB, Minster RR, Bell R, et al. Continuous passive motion and the repair of full-thickness articular cartilage defects: a one-year follow-up. Trans Orthop Res Soc. 1982;7:167. [Google Scholar]
- 24.Salter RB, Simmonds DF, Malcolm BW, Rumble EJ, MacMichael D, Clements ND. The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage: an experimental study in the rabbit. J Bone Joint Surg Am. 1980;62:1232–1251. [PubMed] [Google Scholar]
- 25.Rubak JM. Reconstruction of articular cartilage defects with free periosteal grafts: an experimental study. Acta Orthop Scand. 1982;53:175–180. doi: 10.3109/17453678208992197. [DOI] [PubMed] [Google Scholar]
- 26.Engkvist O, Johansson SH. Perichondrial arthroplasty: a clinical study in twenty-six patients. Scand J Plast Reconstr Surg. 1980;14:71–87. doi: 10.3109/02844318009105737. [DOI] [PubMed] [Google Scholar]
- 27.Pastacaldi P, Engkvist O. Perichondrial wrist arthroplasty in rheumatoid patients. Hand. 1979;11:184–190. doi: 10.1016/s0072-968x(79)80032-7. [DOI] [PubMed] [Google Scholar]
- 28.Kleiner JB, Coutts RD, Woo SLY, et al. The short term evaluation of different treatment modalities upon full thickness articular cartilage defects: a study of rib perichondrial chondrogenesis. Trans Orthop Res Soc. 1986;11:282. [Google Scholar]
- 29.Kwan MK, Woo SLY, Amiel D, et al. Neocartilage generated from rib perichondrium: a long-term multidisciplinary evaluation. Trans Orthop Res Soc. 1987;12:277. [Google Scholar]
- 30.O'Driscoll SW, Keeley FW, Salter R. The chondrogenic potential of free autogenous periosteal grafts for biological resurfacing of major full-thickness defects in joint surfaces under the influence of continuous passive motion: an experimental study in the rabbit. J Bone Joint Surg Am. 1986;68:1017–1035. [PubMed] [Google Scholar]
- 31.O'Driscoll SW, Salter RB. The induction of neochondrogenesis in free intra-articular periosteal autografts under the influence of continuous passive motion: an experimental investigation in the rabbit. J Bone Joint Surg Am. 1984;66:1248–1257. [PubMed] [Google Scholar]
- 32.Zarnett R, Delaney JP, O'Driscoll SW, Salter RB. Cellular origin and evolution of neochondrogenesis in major full-thickness defects of a joint surface treated by free autogenous periosteal grafts and subjected to continuous passive motion in rabbits. Clin Orthop. 1987;222:267–274. [PubMed] [Google Scholar]
- 33.Schultz RJ, Krishnamurthy S, Thelmo W, Rodriguez JE, Harvey G. Effects of varying intensities of laser energy on articular cartilage: a preliminary study. Lasers Surg Med. 1985;5:577–588. doi: 10.1002/lsm.1900050606. [DOI] [PubMed] [Google Scholar]
- 34.Itay S, Abramovici A, Nevo Z. Use of cultured embryonal chick epiphyseal chondrocytes as grafts for defects in chick articular cartilage. Clin Orthop. 1987;220:284–303. [PubMed] [Google Scholar]
- 35.Speer DP, Chvapil M, Volz RG, Holmes MD. Enhancement of healing in osteochondral defects by collagen sponge implants. Clin Orthop. 1979;144:326–335. [PubMed] [Google Scholar]
- 36.Hart JAL. The use of carbon fibre implants for articular cartilage defects. Paper presented at: 47th Annual Meeting of the Australian Orthopedic Association; 1987; Melbourne, Australia. [Google Scholar]
- 37.Aaron RK, Ciomber DM, Jolly G. Modulation of chondrogenesis and chondrocyte differentiation by pulsed electromagnetic fields. Trans Orthop Res Soc. 1987;12:272. [Google Scholar]
- 38.Aaron RK, Plaas AAK. Stimulation of proteoglycan synthesis in articular chondrocyte cultures by a pulsed electromagnetic field. Trans Orthop Res Soc. 1987;12:273. [Google Scholar]
- 39.Dunn AR, Sampsell R. Regrowth of articular cartilage by direct hormonal induction with growth hormone following full-thickness surgical debridement. Paper presented at: 53rd Annual Meeting of the American Academy of Orthopaedic Surgeons; February 25, 1986; New Orleans, LA. [Google Scholar]
- 40.Syftestad G, Caplan A. A 31,000 dalton bone matrix protein stimulates chondrogenesis in chick limb and bud cell cultures. Trans Orthop Res Soc. 1986;11:278. [Google Scholar]
- 41.Reichelt A, Forster KK, Fischer M, Rovati LC, Setnikar K. Efficacy and safety of intramuscular glucosamine sulfate in osteoarthritis of the knee: a randomised, placebo-controlled, double-blind study. Arzneimettelforschung. 1994;44:75–80. [PubMed] [Google Scholar]
- 42.Qiu GX, Gao SN, Giacovelli G, Rovati L, Setnikar J. Efficacy and safety of glucosamine sulfate versus ibuprofen in patients with knee osteoarthritis. Arzneimettelforschung. 1998;48:469–474. [PubMed] [Google Scholar]
- 43.Glucosamine and chondroitin for osteoarthritis: relief without side effects. Sports Med Alert. 1999 Mar;:22–23. [Google Scholar]
- 44.Bassleer C, Rovati L, Franchimont P. Stimulation of proteoglycan production by glucosamine sulfate in chondrocytes isolated from human osteoarthritic articular cartilage in vitro. Osteoarthritis Cartilage. 1998;6:427–434. doi: 10.1053/joca.1998.0146. [DOI] [PubMed] [Google Scholar]
- 45.Runkel DR, Cupp MJ. Glucosamine sulfate use in osteoarthritis. Am J Health Syst Pharm. 1999;56:267–269. doi: 10.1093/ajhp/56.3.267. [DOI] [PubMed] [Google Scholar]
- 46.Vajranetra P. Clinical trial of glucosamine compounds for osteoarthritis of knee joints. J Med Assoc Thai. 1984;67:409–418. [PubMed] [Google Scholar]
- 47.Setnikar I, Palumbo R, Canali S, Zanolo G. Pharmacokinetics of glucosamine in man. Arzneimettelforschung. 1993;43:1109–1113. [PubMed] [Google Scholar]
- 48.Schiedermayer D. Glucosamine sulfate for the treatment of osteoarthritis. Altern Med Alert. 1998;1:121–124. [Google Scholar]
- 49.Noack W, Fischer M, Forster KK, Rovati LC, Setnikar I. Glucosamine sulfate in osteoarthritis of the knee. Osteoarthritis Cartilage. 1994;2:51–59. doi: 10.1016/s1063-4584(05)80006-8. [DOI] [PubMed] [Google Scholar]
- 50.D'Ambrosio ED, Casa B, Bompani R, Scali G, Scali M. Glucosamine sulphate: a controlled clinical investigation in arthrosis. Pharmatherapeutica. 1981;2:504–508. [PubMed] [Google Scholar]
- 51.Rovati LC. Clinical research in osteoarthritis: design and results of short-term and long-term trials with disease-modifying drugs. Int J Tissue React. 1992;14:243–251. [PubMed] [Google Scholar]
- 52.Roden L. Effect of hexosamines on the synthesis of chondroitin sulfuric acid in vitro. Arkh Kemi. 1956;10:345–352. [Google Scholar]
- 53.Karzel K, Domenjoz R. Effects of hexosamine derivatives and uronic acid derivatives on glycosaminoglycan metabolism of fibroblast cultures. Pharmacology. 1971;5:337–345. doi: 10.1159/000136209. [DOI] [PubMed] [Google Scholar]
- 54.Vidal y Plana RR, Bizzarri D, Rovati AL. Articular cartilage pharmacology, I: in vitro studies on glucosamine and non steroidal antiinflammatory drugs. Pharmacol Res Comm. 1978;10:557–569. doi: 10.1016/s0031-6989(78)80054-x. [DOI] [PubMed] [Google Scholar]
- 55.Vidal y Plana RR, Karzel K. Glucosamine: its role in the articular cartilage metabolism: studies on rat and human articular cartilage. Fortschr Med. 1980;98:801–806. [PubMed] [Google Scholar]
- 56.Glucosamine for osteoarthritis. Med Lett. 1997;39:91–92. [PubMed] [Google Scholar]
- 57.Considering the alternatives. Harvard Health Lett. 1999;24:7. [PubMed] [Google Scholar]
- 58.Crolle G, D'Este E. Glucosamine sulphate for the management of arthrosis: a controlled clinical investigation. Curr Med Res Opin. 1980;7:104–109. doi: 10.1185/03007998009112035. [DOI] [PubMed] [Google Scholar]
- 59.Drovanti A, Bignamini AA, Rovati AL. Therapeutic activity of oral glucosamine sulfate in osteoarthrosis: a placebo-controlled double-blind investigation. Clin Ther. 1980;3:260–272. [PubMed] [Google Scholar]
- 60.Leffler CT, Philippi AF, Leffler SG, Mosure JC, Kim PD. Glucosamine, chondroitin, and manganese ascorbate for degenerative joint disease of the knee or low back: a randomized, double-blind, placebo-controlled pilot study. Mil Med. 1999;164:85–91. [PubMed] [Google Scholar]
- 61.Pujalte JM, Llavore EP, Ylescupidez FR. Double-blind clinical evaluation of oral glucosamine sulphate in the basic treatment of osteoarthritis. Curr Med Res Opin. 1980;7:110–114. doi: 10.1185/03007998009112036. [DOI] [PubMed] [Google Scholar]
- 62.Vajaradul Y. Double-blind clinical evaluation of intra-articular glucosamine in outpatients with gonarthrosis. Clin Ther. 1981;3:336–343. [PubMed] [Google Scholar]
- 63.Muller-Fabbender H, Bach GL, Haase W, Rovati LC, Setnikar I. Glucosamine sulfate compared to ibuprofen in osteoarthritis of the knee. Osteoarthritis Cartilage. 1994;2:61–69. doi: 10.1016/s1063-4584(05)80007-x. [DOI] [PubMed] [Google Scholar]
- 64.Vaz AL. Double-blind clinical evaluation of the relative efficacy of ibuprofen and glucosamine sulphate in the management of osteoarthritis of the knee in out-patients. Curr Med Res Opin. 1982;8:145–149. doi: 10.1185/03007998209112375. [DOI] [PubMed] [Google Scholar]
- 65.Tapadinhas MJ, Rivera IC, Bignamini AA. Oral glucosamine sulphate in the management of arthrosis: report on a multi-centre open investigation in Portugal. Pharmatherapeutica. 1982;3:157–168. [PubMed] [Google Scholar]
- 66.Shankland WE., II The effects of glucosamine and chondroitin sulfate on osteoarthritis of the TMJ: a preliminary report of 50 patients. Cranio. 1998;16:230–235. doi: 10.1080/08869634.1998.11746062. [DOI] [PubMed] [Google Scholar]
- 67.Smith BW. New guidance available for supplement use. Available at: http://www.ncaa.org/news/20000717/comment.html. Accessed July 17, 2000.
- 68.United States Congress. Dietary Supplement Health and Education Act of 1994. Pub L 103–417. Available at: http://vm.cfsan.fda.gov/~dms/dietsupp.html. Accessed January 4, 2001.
- 69.McClain DA, Crook ED. Hexosamines and insulin resistance. Diabetes. 1996;45:1003–1009. doi: 10.2337/diab.45.8.1003. [DOI] [PubMed] [Google Scholar]
- 70.Almada AL, Harvey PW, Platt KJ. Effect of chronic oral glucosamine sulfate upon fasting insulin resistance index (FIRI) in nondiabetic individuals. Paper presented at: Annual Meeting of Professional Research Scientists; April 15–18, 2000; San Diego, CA. [Google Scholar]
- 71.Eichler J, Noh E. Therapy of deforming arthrosis through the action upon cartilaginous metabolism. Orthop Praxis. 1970;9:225–229. [Google Scholar]
- 72.Raiss R. Influence of glucosamine sulfate on experimentally impaired articular cartilage: test of ultrastructural changes in chondrocytes using morphometry. Fortschr Med. 1985;103:658–662. [PubMed] [Google Scholar]
- 73.Setnikar I, Giachetti C, Zanologo G. Absorption, distribution and excretion of radioactivity after a single intravenous or oral administration of [14C] glucosamine to the rat. Pharmatherapeutica. 1984;3:538–550. [PubMed] [Google Scholar]
- 74.Rovati LC, Giacovelli G, Annfield M, Dreiser RL, Avouac B. A large, randomised, placebo-controlled, double-blind study of glucosamine sulfate vs. piroxicam and versus their association on the kinetics of the symptomatic effect in knee osteoarthritis. Osteoarthritis Cartilage. 1994;2(suppl 1):56. [Google Scholar]
- 75.Giacovelli G, Rovati LC. Clinical efficacy of glucosamine sulfate in osteoarthritis of the spine. Rev Esp Rheumatol. 1993;20(suppl 1):325. [Google Scholar]
- 76.McAlindon TE, LaValley MP, Gulin JP, Felson DT. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283:1469–1475. doi: 10.1001/jama.283.11.1469. [DOI] [PubMed] [Google Scholar]