Disaster Mythology and Fact: Hurricane Katrina and Social Attachment (original) (raw)
SYNOPSIS
Misconceptions about disasters and their social and health consequences remain prevalent despite considerable research evidence to the contrary. Eight such myths and their factual counterparts were reviewed in a classic report on the public health impact of disasters by Claude de Ville de Goyet entitled, The Role of WHO in Disaster Management: Relief, Rehabilitation, and Reconstruction (Geneva, World Health Organization, 1991), and two additional myths and facts were added by Pan American Health Organization.
In this article, we reconsider these myths and facts in relation to Hurricane Katrina, with particular emphasis on psychosocial needs and behaviors, based on data gleaned from scientific sources as well as printed and electronic media reports. The review suggests that preparedness plans for disasters involving forced mass evacuation and resettlement should place a high priority on keeping families together—and even entire neighborhoods, where possible—so as to preserve the familiar and thereby minimize the adverse effects of separation and major dislocation on mental and physical health.
Misconceptions about disasters and their social and health consequences abound, despite considerable research evidence to the contrary. Eight such myths and their factual counterparts were reviewed in a classic report on the public health impact of disasters by de Ville de Goyet1 and two additional myths were added by the Pan American Health Organization (PAHO) and subsequently listed by Noji.2 This article reconsiders these myths and facts in relation to the known impact of Hurricane Katrina, with particular emphasis on psychosocial needs and behaviors.
Katrina was the deadliest hurricane since 1900—when a hurricane hit Galveston, Texas—and it was the costliest natural disaster on record in the United States.3 The hurricane made landfall near Buras, Louisiana, on August 29, 2005, as a strong Category 3 hurricane. The 125-mile-per-hour winds and storm surge virtually obliterated entire coastal communities in its wake. More than 1,300 people died as a direct result of the storm and subsequent floods, 700,000 were displaced, and about 273,000 people were evacuated to shelters.4
Hurricane Katrina was a highly complex event in terms of its overall impact, due to the interaction of natural forces and the engineering failure of man-made storm and flood protection structures, notably in New Orleans. High winds and flooding destroyed homes, businesses, and health infrastructure across a 90,000-square-mile area of Louisiana, Alabama, Mississippi, and the Florida Panhandle.3 Storm-induced breaks in the levee system surrounding New Orleans caused rapid and deep flooding in more than 80% of the city.
The disaster was compounded 26 days later when Hurricane Rita made landfall near the Texas-Louisiana border, forcing the cessation of hurricane response activities in New Orleans and the evacuation of coastal regions of western Louisiana and Texas. The economic and health consequences of Hurricanes Katrina and Rita extended beyond the Gulf region and continue to affect states and communities adversely throughout the country.5 The aggregate monetary costs of Katrina in Orleans Parish alone are estimated at 40to40 to 40to50 billion, including direct property losses, continuing economic losses, and emergency assistance.6 The data for this article were gleaned from scientific sources as well as printed and electronic media reports on Hurricane Katrina and its sequelae.
THE “MYTHS”
The 10 myths and facts on disasters are as follows:
- Myth #1: Foreign medical volunteers with any kind of clinical background are needed. Fact: The local population almost always provides for its own immediate health needs. Only medical personnel with skills that are not available in the affected country may be needed.
- Myth #2: Any kind of international assistance is needed immediately. Fact: A hasty response, not based on an impartial evaluation, contributes to the chaos. Most needs are met by the victims themselves and their government and local agencies, not by foreign aid workers.
- Myth #3: Epidemics and plagues are inevitable after every disaster. Fact: Epidemics seldom occur after a disaster, and dead bodies do not lead to catastrophic outbreaks of infectious diseases. Improving sanitary conditions and educating the public on hygienic measures are the best means of preventing disease.
- Myth #4: Disasters bring out the worst in people (e.g., looting, rioting). Fact: While there are isolated cases of antisocial behavior, which tend to be highlighted by the media, most people respond positively and generously.
- Myth #5: The affected population is too shocked and helpless to take responsibility for its own survival. Fact: Many people find new strength and resiliency during an emergency.
- Myth #6: Disasters are random killers. Fact: Disasters strike the most vulnerable groups hardest, i.e., minorities and the poor, especially women, children, and the elderly.
- Myth #7: Locating disaster victims in temporary settlements is the best solution to the housing problem. Fact: This is the least desirable option. The preferred strategy is to purchase construction materials and rebuild.
- Myth #8: Food aid is always required for the victims of natural disasters. Fact: Massive food aid is not usually required; natural disasters only rarely cause loss of crops.
- Myth #9: Clothing is always needed by disaster victims. Fact: Clothing is almost never needed; it is usually culturally inappropriate, and although it is accepted by disaster victims it is almost never worn.
- Myth #10: Things return to normal within a few weeks. Fact: Disasters have enduring effects and major economic consequences. International interest tends to wane just as needs and shortages become more pressing.
The present review supports the generalizations overall, but sets the behavioral observations in a context of the social attachment model of psychosocial needs and behaviors.7,8 The central premises of the model are that the overriding tendency in disasters is to seek the proximity of loved ones, familiar possessions, and places (i.e., affiliation rather than “fight or flight”); these tendencies lead to altruism, camaraderie, and social solidarity at the community level rather than social breakdown, passivity, or escape; and separation from loved ones and familiars is a greater stressor than physical danger.
DISASTER MYTHS AND FACTS IN LIGHT OF HURRICANE KATRINA
Myth #1: Are foreign medical volunteers needed?
As noted by de Goyet,1 immediate lifesaving needs are almost always met by the local population rather than by outside medical volunteers. Only medical personnel with skills that are unavailable in the affected area may be needed. The U.S. government response to Hurricane Katrina in Louisiana was actually delayed, partly due to initial reports that New Orleans had escaped the brunt of the storm, and perhaps also due to political and bureaucratic wrangling over state and local vs. federal jurisdiction. However, short-term health and medical needs were largely met following the hurricane. In fact, in locations where overall coordination and infrastructure were lacking, attempts to provide direct care distracted attention from more urgent tasks of meeting security and other immediate needs. Many clinicians and health-care organizations self-deployed to Louisiana following Hurricane Katrina, but their arrival occasionally compounded the disorganization of health services. Physicians wrote prescriptions for hypertension and diabetes, but there were no pharmacies open or even available to fill them. Lacking an assigned role, and in the absence of communication facilities and electrical power, many volunteers were unable to meet the actual needs of victims.9
Emergency workers from Canada, however, were the first to arrive at the Hurricane operations center in St. Bernard Parish, a New Orleans suburb of 70,000 people, on August 31, 2005. The team of 45 was warmly welcomed by the parish president, rescued 119 people from flooded homes, treated about 150 patients, saved many evacuees, and resupplied a local medical clinic before returning to Canada on September 6, 2005.10 Only subsequently was a disaster response mobilized throughout the country, and it included volunteers from, among others, the National Institute of Environmental Health Sciences, the National Institutes of Health (NIH), the Environmental Protection Agency (EPA), the Occupational Safety and Health Administration, the Centers for Disease Control and Prevention (CDC), the Department of Defense, the Food and Drug Administration, the U.S. Department of Agriculture (USDA), the Department of Homeland Security, the American Red Cross (ARC), and the Federal Emergency Management Agency (FEMA), in addition to volunteers from medical facilities and groups.11 This would tend to support de Goyet's generalization that foreign medical workers are not usually needed in natural disasters in countries where resources are adequate. But those with poor resources would clearly benefit from intervention by structured disaster response teams.
Myth #2: Is international assistance needed?
Because Hurricane Katrina destroyed businesses as well as the medical and public health infrastructure along a broad swath of the U.S. Gulf Coast, including New Orleans, assistance from federal agencies was essential. Massive aid was provided by ARC, FEMA, and other governmental and private agencies. CDC, for instance, deployed approximately 500 professionals for recovery operations. However, the severity of wind damage and flooding was shown by a survey of evacuees in Houston. Forty percent reported spending at least a day on a street or overpass waiting to be rescued, and 34% were trapped in homes. Of those trapped in their own homes, half of them waited three or more days to be rescued. Of those rescued, equal percentages (43%) were saved either by official agencies (Coast Guard, National Guard, and military) or by friends or neighbors.12
Within 14 days after the hurricane, ARC and the Mississippi Department of Health had established case definitions of illnesses and set up a toll-free number for shelter staff to report illnesses.13 Just two days after the hurricane, work began at the field headquarters of ARC in Baton Rouge, Louisiana. The medical team deployed from ARC headquarters in Washington, DC, performed critical-needs assessments and helped define the public health response to the hurricane. Within four days, multidisciplinary and interagency ARC teams had assessed more than 200 shelters housing nearly 30,000 people and provided care to about 50,000 displaced people. These teams rapidly identified immediate and longer-term needs and developed a coordinated response plan.9 U.S. President George W. Bush did not request foreign aid officially, but offers of aid from the United Nations and approximately 90 member countries were received by the U.S. government.14
In New Orleans, health services were provided by Ochsner Clinic, located at the more elevated, southwestern end of the city, as well as by other local medical institutions (including Touro Infirmary in the uptown area and East Jefferson General Hospital in the suburb of Metairie) that had escaped major flooding.15 However, local and federal assistance was hampered by a dearth of resources and infrastructure in New Orleans. For example, more than 9,000 hospital beds in New Orleans were unusable because of flooding;8 shelters had difficulty obtaining medications;16 and many health-care workers were themselves displaced by the hurricane. Makeshift clinics in the larger shelters had limited supplies but provided medical support.17 On the other hand, the medical infrastructure of Gulfport, Mississippi, an area severely affected by the hurricane, was relatively intact. Patients were seen effectively in clinics, and hospitals were open with sufficient bed capacity in at least six different communities of the Gulfport region, not necessitating assistance from the NIH medical mission team.18
These observations on Hurricane Katrina, though far from representative, support de Goyet's thesis that disaster-related needs are met by national and local governmental agencies. However, were it not for the massive resources available for mobilization within the U.S., almost any other country dealing with a hurricane on the scale of Hurricane Katrina would have required assistance.
Myth #3: Do epidemics and plagues follow disasters?
Intuitively, epidemic diseases, illnesses, and injuries might be expected following major disasters. However, as noted by de Goyet, epidemics seldom occur after disasters, and unless deaths are caused by one of a small number of infectious diseases such as smallpox, typhus, or plague, exposure to dead bodies does not cause disease.2,19 Rumors to the contrary can lead to mass burials, inhibiting the identification of bodies and interfering with religiously and culturally appropriate burial practices.19
The keys to disease prevention are excellent sanitary conditions, swift and competent response management, and public education. Cholera and typhoid seldom pose a major health threat after disasters unless they are already endemic.19 Although there is no (or very limited) endemic potential for epidemics of cholera or measles in the U.S.,20 outbreaks of vector-borne disease and cholera have occurred after hurricanes and flooding in developing countries.21,22
West Nile virus (WNV), St. Louis encephalitis, and dengue have ties to the Mississippi delta,23 and vast areas of stagnant and tainted floodwaters following Hurricane Katrina caused concern about vector-borne diseases. But there were no reported outbreaks of these illnesses in Mississippi.24 There were, however, reports by CDC of other infectious illnesses, including gastroenteritis (Norovirus), bacterial infection (sometimes lethal) of open wounds (Vibrio vulnificus, V. parahaemolyticus, V. cholerae, leptospirosis infections, skin abscesses and methicillin-resistant Staphylococcus aureus infections, WNV, and varicella). There were also reports of scabies/lice infestation and carbon monoxide poisoning, which were attributed mainly to lack of potable (or any) water; crowded, unsanitary conditions; and limited knowledge of health risks among shelter occupants.
Extensive damage to the infrastructure of the Louisiana Department of Health and Hospitals (LDHH) resulted in limited opportunities for disease surveillance, although resources in Louisiana were rapidly mobilized to restore essential public health services. CDC, the LDHH, functioning hospitals, disaster medical assistance teams, and military aid stations established an active surveillance system, beginning September 9, 2005, to report post-hurricane injuries and illnesses, initiate interventions, and deliver prevention messages to residents and relief workers.20
Myth #4: Do disasters trigger social breakdown?
It is commonly assumed that the social contract is tenuous at best and that major natural disasters and other crises trigger mass disruption, disorder, and social breakdown. While there were well-documented instances of brutal hijacking, rioting, and looting in New Orleans after the deep flooding caused by the hurricane, there were many more reports of altruism, cooperativeness, and camaraderie among the affected population.8,25,26 The overall cooperative, prosocial, and altruistic individual and community response following Hurricane Katrina was similarly observed after the Asian tsunami of December 2004, and the July 7, 2005, terrorist bombings in London,27 and may have been reflected in the transient 40% to 60% drop in the homicide rate in New York City after September 11, 2001.28 In support of de Goyet's thesis, it is well documented that natural and man-made disasters are followed by increases in altruistic behavior and social solidarity.29–32
Following Hurricane Katrina, many residents of Baton Rouge, for example, invited someone to stay in their home; hotels housed displaced families, extended families, and pets; and nearly every large shelter created a clinic run by local doctors and nurses.9 At New Orleans' Charity Hospital (the Medical Center of Louisiana), people of different races, old and young, patients and providers, both rich and poor, held hands and prayed for rescue. Notwithstanding the chaos and confusion, the medical staff remained calm and communicated coherently, dispensing care and comfort. A flashlight-illuminated talent show was held in which everyone was invited to participate, including patients with masks donned to prevent the spread of tuberculosis.25
Myth #5: Are those affected unable to take responsibility for their own survival?
Against the common misconception that disaster victims are too shocked and helpless to take responsibility for their own welfare and survival, many find new strength and resiliency during emergencies. Thousands of local volunteers spontaneously united to sift through the rubble in search of victims after the 1985 Mexico City earthquake. Most rescue work, including providing first-aid and transportation, is done by disaster victims themselves, as witnessed after the Asian tsunami in 2004, the 9/11 attacks in New York and Washington, DC, and the 2005 bombing attacks in London.
Similarly, following Hurricane Katrina, despite the loss of infrastructure and power outages at some shelters, the affected population engaged in active coping behavior.17 The medical staff of Charity Hospital maintained a disciplined schedule while electrical power was lost and food and many medications were lacking.25 Desperately ill patients also took responsibility for their own care.15 On the other hand, most residents of New Orleans who remained in the city were stranded by the floodwater and depended on emergency workers for rescue.
Myth #6: Do disasters kill at random?
A common misconception is that disasters tend to strike human populations at random. On the contrary, de Goyet notes that disasters typically strike more vulnerable groups the hardest, such as those on low or fixed incomes, and especially women, children, elderly, and disabled people who tend to reside in more exposed locations and have fewer resources.6,33,34 Marginalized populations generally suffer disproportionately after environmental disasters.
Hurricane Katrina was a special case because of its enormity and severity, and its impact was felt by entire communities across the Gulf states of Louisiana, Mississippi, and Alabama. However, in New Orleans, where major flooding occurred due to the levees' failure, the destroyed neighborhoods were mainly in low-lying areas that were once marsh and swampland, and housed predominantly African American residents (76%), 29% of the population having incomes below the poverty line.35 In one notable incident, while patients and staff at a private hospital were rescued by helicopter, those at adjacent Charity Hospital could not be rescued due to practical and technical reasons.25,36 Residents of affluent neighborhoods tended to evacuate in their own vehicles in response to the call for mandatory evacuation, whereas poorer citizens either lacked a means of transportation or were unwilling to leave, and many took shelter in the Louisiana Superdome or New Orleans Morial Convention Center. Others sought refuge in hospitals, nursing homes, upstairs in their own homes, or on elevated highways.6
The 2000 U.S. Census revealed that 27% of New Orleans households (about 120,000 people) were without privately owned transportation. In a survey conducted in Houston shelters soon after the hurricane (September 10–12, 2005), more than a third of respondents reported that lack of a car or other means of transportation was their main reason for not evacuating.12 About 75% (1 million) of residents in the greater New Orleans area evacuated, but the remaining 25% were unable or unwilling to leave.6
Myth #7: Should disaster victims be housed in temporary settlements?
It has been said that locating disaster victims in temporary settlements is the best solution to the housing problem. To the contrary, this is the least desirable option according to de Goyet, who suggested that construction materials be purchased and homes rebuilt in the affected areas. In the case of Hurricane Katrina, however, the widespread destruction of residential neighborhoods and of shopping areas and infrastructure made immediate reconstruction impracticable, and temporary housing had to be found for the estimated 400,000 homeless evacuees from New Orleans and the coastal regions of Mississippi and Alabama. As noted, about 25% of the population remained in the area, requiring rescue and local aid in the aftermath. Tendencies to remain in disaster areas and to refuse or delay evacuation have been noted in other disasters.37–39
By February 18, 2006, FEMA had provided 42,460 travel trailers and mobile homes to residents in Louisiana alone,40 in part to encourage workers to return to their jobs and save businesses that would otherwise fail. However, many trailers were never delivered or were delivered very late or in an unusable/unsafe condition. A survey conducted on 366 displaced people to assess basic needs and health among residents of trailer parks in Louisiana and Mississippi found that shelter, transportation, security, and lack of finance were the most pressing problems since displacement; 16% reported not having enough drinking water, and only 13% of those living in areas under boil orders could comply.41 More than 50% reported an ill adult or child in the previous two months, and parents reported that problems getting children to school were increased threefold post-displacement. Intimate partner violence rates also rose threefold above U.S. baseline rates and 50% of respondents met criteria for major depression, similar to the number of depressive disorders among prehurricane residents of the New Orleans metropolitan area.42 Suicide rates after displacement were more than 14 times higher than baseline rates, while suicide attempt rates were more than 78 times above baseline.41
Myth #8: Is there a need for food aid?
It is commonly thought that food aid is always required following natural disasters. According to PAHO (Personal communication, Claude de Ville de Goyet, World Health Organization [WHO], February 2008), this is not the case, as natural disasters only rarely cause loss of crops. However, crop failure is not the only situation in which food aid may be needed on a large scale in a disaster. In regard to Hurricane Katrina, many who failed to evacuate prior to the hurricane endured several days without food, if not water.43 Ice, food, and water all had to be brought in by truck. Even in relatively unaffected areas shops and stores were closed; hence, large numbers of people had to rely on outside assistance. Distressing images were shown on television of stranded victims lacking basic necessities and exposed to human waste, toxins, and physical violence.13 Communication breakdowns contributed to the difficulties faced by relief workers in obtaining needed supplies and services for the shelters. Most shelters on the Mississippi coast received adequate supplies of food and water, but there were concerns about the safety of drinking and showering water, wastewater disposal, and reliance on portable toilets for water in some shelters.17
The magnitude and urgency of the need for food and potable water after the hurricane were unprecedented. The manual of the U.S. Office of Foreign Disaster Assistance (OFDA) calculates water needs based on a minimum daily requirement of 15 to 20 liters per person. ARC recommends a gallon (4.5 liters) of potable water per person per day, and a seven-day supply. Although needs may be greater in hot weather, the amount needed for 20,000 people (the number housed in the New Orleans Convention Center), based on a 15-liter requirement, translates into 300,000 liters, or about 79,000 gallons of water per day. These facts point to the importance of ensuring that required amounts of food, water (especially potable), and other essential supplies are deliverable at large and secure venues designated as staging areas, to prevent a man-made disaster from following a natural one.19
By September 17, 2005, in Orleans Parish alone, winds and flooding had resulted in structural damage to approximately 3,800 wholesale and retail food establishments. Loss of power and floodwater in affected areas also resulted in food spoilage and contamination. Supplies of drinking water were sufficient for only about 30 days post-hurricane, and city water provided to the New Orleans' East Bank, housing about 90% of the population, was not potable. The main water treatment facility on Carrollton Avenue had low water pressure throughout the distribution system.
The USDA delivered food and nutrition assistance to states directly affected by Hurricane Katrina as well as host states. By September 22, 2005, 428,000 displaced households had applied for more than $151 million in food stamp benefits in Louisiana and Texas alone. For more than three weeks, massive food aid was provided for nearly 637,000 households by FEMA.
Pre-disaster emergency planning should include assigning responsibility to local people for maintaining critical infrastructure. For example, during Hurricane Floyd—which struck North Carolina on September 16, 1999—engineers made it possible for the Pitt County Memorial Hospital to use the Rehab Unit swimming pool as a watertight reservoir to pressurize the water system for providing potable water and flushable toilets throughout the hospital.44
Myth #9: Is clothing needed by disaster victims?
Clothes are one of the major items donated after disasters, and clothing, along with other basic necessities, is routinely provided to disaster victims by emergency relief organizations. Yet, according to PAHO (Personal Communication, Claude de Ville de Goyet, WHO, February 2008), donated clothing is almost never needed, and although it may be accepted by disaster victims, it is almost never worn.
In the case of Hurricane Katrina, the rapid and devastating flooding of New Orleans created by breaks in three levee systems led to massive losses of homes, possessions, and employment. As a result, clothing, bedding, and footwear were needed on an unprecedented scale, not only in early phases of the disaster but also as temperatures cooled and fall turned into winter. Relief agencies and many neighborhood and charity organizations collected donated clothing for evacuees, and school systems provided uniforms for children (Personal communication, Karen Quay, Director of Evacuee Resettlement, Lutheran Episcopal Services, Jackson, Mississippi, May 2006). A survey of Hurricane Katrina evacuees in Colorado by CDC in September 2005 found that 45% of households (_n_=105) needed clothing, and that it was one of the most common long-term needs of evacuees.45
Myth #10: Does life return to normal in a few weeks?
Contrary to popular misconception, disasters can have profoundly adverse effects and major economic consequences that can take months or years to overcome. A return to normalcy seldom occurs quickly.1 International (as well as national or domestic) interest also tends to wane just as needs and shortages become more pressing. Developing countries and even relatively impoverished and economically precarious areas in generally prosperous countries can deplete most of their financial and material resources in the immediate post-impact phase of major natural disasters, so relief programs have their greatest impact when international interest declines and local needs and shortages become acute.
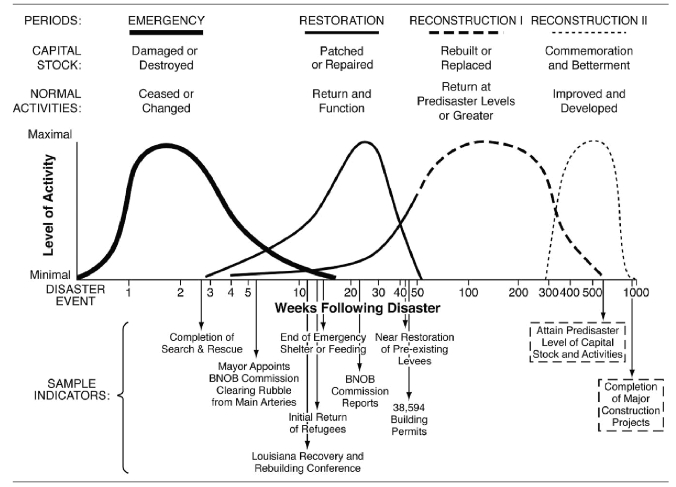
In the 300-year history of New Orleans, the city has had 27 major river- or hurricane-induced disasters at a rate of one about every 11 years.46 After each event, the city rebuilt and often expanded. Figure 1 shows a plot of the reconstruction experience for one year after Hurricane Katrina and projects future reconstruction activity by using the four periods of historical experience.6
Figure 1.
The sequence and timing of reconstruction after Hurricane Katrina in New Orleansa
aActual experience (solid line) and sample indicators for the first year are shown along a logarithmic timeline of weeks after the disaster. The long-term projections (dashed lines) are based on an emergency period of six weeks, a restoration period of 45 weeks, and an expected tenfold increase in the duration of reconstruction compared with previous disaster experience. (Kates RW, Colten CE, Laska S, Leatherman SP. Reconstruction of New Orleans after Hurricane Katrina: a research perspective. Proc Natl Acad Sci USA 2006;103:14653-60.)
BNOB = Bring New Orleans Back
The adverse effects of Hurricane Katrina on the physical environment as well as business and residential infrastructure continue to be felt, and the consequences for both physical and mental health are still being documented. In some areas, relief agencies are still struggling to build sustainable procurement and distribution systems to address long-term needs.
A major health issue for displaced populations has been the reduced ability to manage preexisting or worsening chronic illness, including mental illness, which can be compounded by diminished community resources. A study of 18,000 evacuees relocated to San Antonio after Hurricane Katrina reported a substantial demand for drugs used to treat chronic conditions. Health-care encounters from September 2–21, 2005, were monitored using a patient syndromic surveillance system based on major complaints that were classified as either acute or chronic, and medication-dispensing records were collected from federal disaster relief agencies and local pharmacies. Of more than 4,000 health-care encounters, 15% were for chronic medical conditions. Of all medications dispensed, 68% were for chronic conditions, of which 39% were for cardiovascular disease.47 Exacerbation of chronic medical conditions thus contributes importantly to the public health burden of disasters.
Chronic illness in disaster survivors can also be exacerbated by adverse weather conditions, lack of food or water, and physical or emotional trauma. Those with mental illness or disabilities, low incomes, and lack of regular access to health care are most at risk.48,49 A recent survey of the 70,000 families still living in temporary housing found high levels of mental distress: rates of depression and anxiety have doubled since 2006; 68% of female caregivers and 44% of children suffer from depression, anxiety, and sleep disorders; and badly affected neighborhoods remain deserted, adding to feelings of loss and helplessness.50
For many Katrina survivors, uncertainty and disrupted health services had enduring effects that were compounded by environmental contamination due to toxic floodwater, as well as localized threats such as fire ants, rats, and water moccasins.13 An important post-hurricane priority has been to monitor the consequences of dumping contaminated mud and floodwater into areas surrounding the city of New Orleans. Initial tests by the EPA and the Louisiana Department of Environmental Quality ruled out high fecal bacteria counts and exposure to chemicals as potential causes of serious health effects.51
Long-term support and follow-up will be needed for those psychologically traumatized by the storm and related stresses, ranging from separation from family members, pets, and possessions to perceptions (justified or imagined) of hostility or indifference on the part of officialdom or strangers in other areas to which people were summarily evacuated.
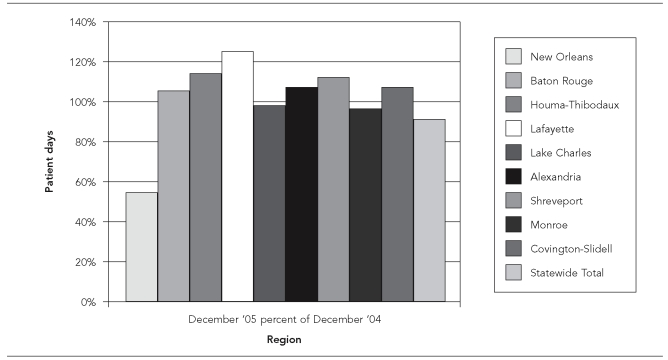
In the continuing aftermath of the disaster, competing proposals for rebuilding the health-care infrastructure, often backed by conflicting interest groups, resulted in cumbersome decision-making and slow implementation. By May 2006, the population of metropolitan New Orleans was about 24% smaller than before the hurricane, but only 15 of the 22 area hospitals were open and less than half of the usual 4,400 beds were in use. New Orleans had 3.03 hospital beds per 1,000 population before the hurricane compared with a mean of 3.26 beds per 1,000 in the U.S. as a whole. By May 2006, there were only 1.99 beds per 1,000 population and in-patient days were increased significantly (Figure 2). Total hospital capacity was also reduced and fewer health-care providers were available. The Medical Center of New Orleans (formerly Charity Hospital) remains closed, forcing indigent patients to travel 75 miles to the nearest safety-net hospital in Baton Rouge; and there was confusion about which hospitals were open and what services were provided.52
Figure 2.
General acute patient days (December 2005 as a percentage of 2004)
Reprinted with permission from Louisiana Hospital Association. (Utilization trends, March 17, 2006 [cited 2006 Mar 18]. Available from: URL: http://www.lhaonline.org/associations/3880/files/Utilization%20Trends.pdf)
The restoration of this vital center of commerce, intermodal transportation, and culture is slowly proceeding, but questions remain about how to rebuild damaged areas of the city and its levees and wetlands, and the extent to which further catastrophic flooding can be prevented or managed.6,53
DISCUSSION
This review of the public health impact of Hurricane Katrina tends to support de Goyet's generalizations about disasters,1 except for Myths #8 and 9, regarding the need for food aid and clothing, respectively. In fact, food aid was provided by FEMA to about 637,000 households for more than three weeks. Clothing was also needed on a massive scale due to the loss of, or evacuees' protracted separation from homes, possessions, and employment related to the hurricane. Indeed, the destructive power and extent of the damage caused by Hurricane Katrina was unprecedented in the U.S.
Regarding the issue of psychosocial responses to disaster, it was believed and hyped in the media that massive trauma led to the abandonment of social mores and relationships and even to violence, as people attempted to escape or to satisfy their own individual needs (Myth #4). To the contrary, studies of behavior in disaster show that the great majority of those directly affected tend to remain calm and behave in an orderly and considerate fashion.54,55 However, what has been lacking to date is a conceptual framework for understanding behavior in disaster.
Although de Goyet presented his generalizations without an overall conceptual framework, his observations related to psychosocial needs and behaviors can be usefully framed in the context of the Social Attachment Model of collective responses to threat and disaster.7,8 The central tenets of the model are that individuals develop attachments to other people (significant others), as well as pets, objects, and places; moreover, once these attachments are formed, individuals strive to maintain them by seeking proximity to the objects of attachment, particularly under conditions of threat or danger. Hence, the overriding tendency expected in disasters would be to seek the familiar and, in particular, the proximity of attachment objects rather than flight or passivity. Thus, increases in altruism, camaraderie, and social solidarity would tend to occur at the community level rather than social breakdown and individualism. Being in proximity to attachment figures also influences the perception of danger and reduces fear, so that in situations where individuals are physically close to their attachment figures and objects, as in community disasters, even severe environmental threats normally induce affiliation rather than flight. Indeed, separation from loved ones and familiars is generally a greater stressor than physical danger itself.
Against the view that disasters cause overwhelming self-interest and social breakdown, manifested in aggression, looting, or rioting (Myth #4), a large body of evidence indicates that the dominant response in community disasters is indeed to seek telephone and physical contact with loved ones and possessions as well as other familiar people and places (affiliative behavior). Contrary to the view that affected populations respond with shock, helplessness, and overall passivity (Myth #5), the tendency toward social affiliation also leads to a multicultural dedication to the common good, expressed in altruism, camaraderie, and social solidarity among victims, enabling many to find new strength and resiliency during the emergency and to respond positively and generously.7,56 With an increasing sense of shared plight, a desire to help predominates. The greater the danger sensed by people in their familiar environment, the more likely they are to strengthen their attachments with family, friends, and neighbors, and to develop new attachments with people sharing the same environment, overriding traditional differences and barriers among people such as race, age, and socioeconomic status. The Social Identity Model of crowd behavior57 also postulates that altruism and self-sacrifice occur when a common identity emerges among people in the same predicament, even when great risk is involved.27
These tendencies were all in evidence during Hurricane Katrina and its aftermath, yet sporadic rioting and acts of violence also erupted after the hurricane at the New Orleans Superdome and other areas in the city business district.16,25,58 These acts may have reflected separation from—or the loss of—family members and friends, devastation of homes, and disruption of community and social networks, caused by the unexpectedly sudden and intense flooding of many parts of the city.
Human beings under threat of death are not invariably motivated by a simple drive for physical safety. As noted, rather than fight or flight, the typical response to danger is to seek the proximity of familiar people and places, even if this involves remaining in or approaching danger. Official organizations often have difficulty in getting people to evacuate before disasters, partly because family ties and other attachments (home, possessions, and their safeguarding) keep individual members in the danger zone. While residents tend to remain in the disaster area, those who flee often lack attachments to the area. However, when residents are forced to evacuate, they strive strongly to do so as a group or in family units, thereby maintaining contact and proximity with familiars.
On the other hand, forcible separation and arbitrary evacuation of separated people to unknown destinations during the chaos following a major disaster would be expected to give rise to hostility and mistrust of intervening authority, as well as “officialdom” at all levels of government, from local to federal, even though the purpose of the intervention was to save lives. Evacuees also tend to orient themselves in the direction of relatives whose homes are outside the danger area, while those forced to go to official evacuation sites form clusters that partially duplicate their old neighborhoods. Affiliative behavior and interactions with family or community members often continue at a high level of intensity and frequency for years after disasters.7,8
Physical danger as a whole is generally far less disturbing or stressful than separation from familiar people and surroundings. During the London bombing raids in World War II, children showed few signs of distress, even if exposed to scenes of death and violence, if they were with a parent or with schoolmates and teachers; it was only if they were separated from parents or other attachment figures under these conditions that serious psychological disturbances occurred.59 More frequent symptoms of disturbance also occur among people who are forced to move because of damage to their homes than among those able to remain in their homes;60 likewise, non-returning evacuees experience significantly greater anxiety, injuries, and other problems than evacuees who are able to remain in the disaster area.61,62 Separation from or the loss of familiar people and surroundings also has profoundly adverse effects on mental and physical health; conversely, individuals of many species tend to remain calm and unafraid in danger situations if they are in the presence of attachment figures and objects.63 Maintaining social attachments is thus essential for preserving mental and physical health and overall well-being. Indeed, the literature on disaster suggests that the greater the loss of the familiar social and physical environment, the greater is the adverse impact on mental health and social adjustment.6,64
Following Hurricane Katrina, only about 50,000 people went to shelters. Consistent with the social attachment model,7 most of the nearly one million displaced people went to the homes of family and friends or stayed together in hotels.65 Evacuees in temporary housing reportedly moved 3.5 times on average after the storm,64 adding to the burden of stress and readjustment. A psychological needs assessment of Hurricane Katrina evacuees in Houston shelters (_n_=124) from September 4 to 12, 2005, showed that moderate and severe symptoms of post-traumatic stress disorder were shown by 39% and 24% of evacuees, respectively.66 The suddenness and extent of post-hurricane flooding in New Orleans meant that many individuals and families were separated during the hurricane, and in the aftermath it was difficult for families to be reunited. Evacuees who had to rely on emergency transport out of the city were taken to totally unfamiliar locations, and some family members were taken to different locations.
The public health importance of individual and family registration systems and of communication between authorities and evacuees was shown by the fact that 10 days after the hurricane, more than 50% of the known dialysis patients in New Orleans could not be located. A tracking program was launched by the Centers for Medicare and Medicaid Services to remedy this situation.15 Large gathering places such as the Superdome and the New Orleans Convention Center were designated as initial staging points for registration and first aid and for contacting missing relatives and friends. However, these venues were suitable only for the briefest occupancy.19
CONCLUSION
There is a major practical implication of the social attachment model regarding official policy for disaster preparedness and response: that is, a high priority should be given to keeping family members and pets united (and even entire neighborhoods where possible) during evacuation and resettlement, so as to preserve social attachments and thereby minimize the adverse effects of separation on mental and physical health. To that end, training programs could usefully be developed for first responders and volunteer aid organizations. Such programs would provide information on the importance of social attachments in understanding how people respond to community disasters, and would offer strategies and guidelines for respecting and helping to maintain social attachments in the affected population in the event of major disasters. In fact, many states have developed State Animal Response Teams to deal with issues of providing temporary housing for pets with or near their owners, recognizing the vital importance of pets to their owners, and the fact that many owners will refuse to evacuate without them.
Footnotes
This research was supported in part by grant #5P20-MD00534-02 from the National Institutes of Health/National Center on Minority Health and Health Disparities (Marinelle Payton, MD, PhD, MS, MPH, Principal Investigator, Center of Excellence in Minority Health, School of Allied Health Sciences, College of Public Service, Jackson State University, Jackson, Mississippi).
REFERENCES
- de Ville de Goyet C. Geneva: World Health Organization; 1991. [cited 2008 Jan 8]. The role of WHO in disaster management: relief, rehabilitation, and reconstruction. Also available from: URL: http://www.crid.or.cr/digitalizacion/pdf/eng/doc10525/doc10525.htm. [Google Scholar]
- 2.Noji EK. The public health consequences of disasters. New York: Oxford University Press; 1997. pp. 17–8. [Google Scholar]
- 3.Knabb RD, Rhome JR, Brown DP. Tropical cyclone report: Hurricane Katrina 23–30 August 2005. Miami: U.S. Department of Commerce, National Oceanic and Atmospheric Administration, National Weather Service, National Hurricane Center; 2005. [Google Scholar]
- 4.Department of Homeland Security (US). Committee on Homeland Security and Governmental Affairs. U.S. Senate. Statement of Richard L. Skinner; 2003 Apr 21; Hope, Arkansas. [cited 2008 May 8]. Available from: URL: http://www.dhs.gov/xoig/assets/katov rsght/OIGtm_RLS_Katrina_042106.pdf. [Google Scholar]
- 5.Public health response to Hurricanes Katrina and Rita—Louisiana, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(2):29–30. [PubMed] [Google Scholar]
- 6.Kates RW, Colten CE, Laska S, Leatherman SP. Reconstruction of New Orleans after Hurricane Katrina: a research perspective. Proc Natl Acad Sci USA. 2006;103:14653–60. doi: 10.1073/pnas.0605726103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mawson AR. Understanding mass panic and other collective responses to threat and disaster. Psychiatry. 2005;68:95–113. doi: 10.1521/psyc.2005.68.2.95. [DOI] [PubMed] [Google Scholar]
- 8.Mawson AR. Brookfield (VT): Ashgate Publishers; 2007. Mass panic and social attachment: the dynamics of human behavior. [Google Scholar]
- 9.Cranmer HH. Hurricane Katrina. Volunteer work-logistics first. N Engl J Med. 2005;353:1541–4. doi: 10.1056/NEJMp058234. [DOI] [PubMed] [Google Scholar]
- 10.Eggertson L. Katrina scars tens of thousands psychologically. CMAJ. 2005;173:857. doi: 10.1503/cmaj.051177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Twombly R. NIEHS responds to Katrina. Environ Health Perspect. 2006;114:A28–9. doi: 10.1289/ehp.114-a28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brodie M, Weltzien E, Altman D, Blenon RJ, Benson JM. Experiences of Hurricane Katrina evacuees in Houston shelters: implications for future planning. Am J Public Health. 2006;96:1402–8. doi: 10.2105/AJPH.2005.084475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenough PG, Kirsch TD. Hurricane Katrina. Public health response—assessing needs. N Engl J Med. 2005;353:1544–6. doi: 10.1056/NEJMp058238. [DOI] [PubMed] [Google Scholar]
- 14.Godlee F. The kindness of strangers. BMJ. 2005;331:7516. [Google Scholar]
- 15.Cohen AJ. Hurricane Katrina. Lethal levels. N Engl J Med. 2005;353:1549. doi: 10.1056/NEJMp058250. [DOI] [PubMed] [Google Scholar]
- 16.Frohlich ED. Hurricane Katrina. Aftershocks. N Engl J Med. 2005;353:1545. doi: 10.1056/NEJMp058231. [DOI] [PubMed] [Google Scholar]
- 17.Johns Hopkins Bloomberg School of Public Health, Public Health News Center. Kellogg Schwab: assessing the aftermath of Hurricane Katrina. 2005. Sep 12, [cited 2005 Dec 2]. Available from: URL: http://www.jhsph.edu/katrina/schwab_aftermath.html.
- 18.Schwartz DA. The NIEHS responds to Hurricane Katrina. Environ Health Perspect. 2005;113:A722. doi: 10.1289/ehp.113-a722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nieburg P, Waldman RJ, Krumm DM. Hurricane Katrina. Evacuated populations—lessons from foreign refugee crises. N Engl J Med. 2005;353:1547–9. doi: 10.1056/NEJMp058237. [DOI] [PubMed] [Google Scholar]
- 20.Surveillance for illness and injury after Hurricane Katrina—New Orleans, Louisiana, September 8–25, 2005. MMWR Morb Mortal Wkly Rep. 2005;54(40):1018–21. [PubMed] [Google Scholar]
- 21.Saenz R, Bissell RA, Paniagua F. Post-disaster malaria in Costa Rica. Prehosp Disaster Med. 1995;10:154–60. doi: 10.1017/s1049023x00041935. [DOI] [PubMed] [Google Scholar]
- 22.Sur D, Dutta P, Nair GB, Bhattacharya SK. Severe cholera outbreak following floods in a northern district of West Bengal. Indian J Med Res. 2000;112:178–82. [PubMed] [Google Scholar]
- 23.Ehrenkranz NJ, Ventura AK, Cuadrado RR, Pond WL, Porter JE. Pandemic dengue in Caribbean countries and the southern United States—past, present and potential problems. N Engl J Med. 1971;285:1460–9. doi: 10.1056/NEJM197112232852606. [DOI] [PubMed] [Google Scholar]
- 24.Singer E. Research losses surface in Hurricane Katrina's aftermath. Nat Med. 2005;11:1015. doi: 10.1038/nm1005-1015a. [DOI] [PubMed] [Google Scholar]
- 25.Berggren R. Hurricane Katrina. Unexpected necessities—inside Charity Hospital. N Engl J Med. 2005;353:1550–3. doi: 10.1056/NEJMp058239. [DOI] [PubMed] [Google Scholar]
- 26.Henderson GS. Hurricane Katrina. Triaging tragedy. N Engl J Med. 2005;353:1551. doi: 10.1056/NEJMp058252. [DOI] [PubMed] [Google Scholar]
- 27.Cocking C, Drury J, Reicher S. The psychology of crowd behaviour in emergency evacuations: results from two interview studies and implications for the Fire & Rescue Services. Irish J Psychol. Special Edition: Psychology and the Fire & Rescue Services 2008. In press. [Google Scholar]
- 28.Hampson R. Dropping murder rates surprises NYC; “Something terrific is going on,” and overall, crime is down. USA Today 2002 Mar 25:A.03/NEWS [Google Scholar]
- 29.Kinston W, Rosser R. Disaster: effects on mental and physical state. J Psychosom Res. 1974;18:437–56. doi: 10.1016/0022-3999(74)90035-x. [DOI] [PubMed] [Google Scholar]
- 30.Quarantelli EL, Dynes RR. Response to social crisis and disaster. Annu Rev Sociol. 1977;3:23–49. [Google Scholar]
- 31.Johnson NR. Panic and the breakdown of social disorder: popular myth, social theory, empirical evidence. Sociol Focus. 1987;20:171–83. [Google Scholar]
- 32.Glass TA, Schoch-Spana M. Bioterrorism and the people: how to vaccinate a city against panic. Clin Infect Dis. 2002;34:217–23. doi: 10.1086/338711. [DOI] [PubMed] [Google Scholar]
- 33.Bern C, Sniezek J, Mathbor GM, Siddiqi MS, Ronsmans C, Chowdhury AM, et al. Risk factors for mortality in the Bangladesh cyclone of 1991. Bull World Health Org. 1993;71:73–8. [PMC free article] [PubMed] [Google Scholar]
- 34.Brouwer R, Akter S, Brander L, Haque E. Socioeconomic vulnerability and adaptation to environmental risk: a case study of climate change and flooding in Bangladesh. Risk Anal. 2007;27:313–26. doi: 10.1111/j.1539-6924.2007.00884.x. [DOI] [PubMed] [Google Scholar]
- 35.Ferdinand KC. The Hurricane Katrina disaster: focus on the hypertensive patient. J Clin Hypertens (Greenwich) 2005;7:679–80. doi: 10.1111/j.1524-6175.2005.05250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katrina, climate change and the poor. CMAJ. 2005;173:837–839. doi: 10.1503/cmaj.051215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Auf der Heide E. Common misconceptions about disasters: panic, the “disaster syndrome” and looting. In: O'Leary MR, editor. The first 72 hours: a community approach to disaster preparedness. Lincoln (NE): iUniverse Publishing; 2004. pp. 340–80. [Google Scholar]
- 38.Bates FL. The social and psychological consequences of a natural disaster: a longitudinal study of Hurricane Audrey. Washington: National Academy of Sciences, National Research Council; 1963. [Google Scholar]
- 39.Gladwin H, Peacock WG. Warning and evacuation: a night for hard houses. In: Peacock WG, Morrow BH, Gladwin H, editors. Hurricane Andrew: ethnicity, gender and the sociology of disasters. London: Routledge; 1997. pp. 52–74. [Google Scholar]
- 40.Federal Emergency Management Agency (US) Louisiana weekly housing update. [cited 2006 Feb 18]. Available from: URL: http://www.fema.gov/news/newsrelease.fema?id=23748.
- 41.Larrance R, Anastario M, Lawry L. Health status among internally displaced persons in Louisiana and Mississippi travel trailer parks. Ann Emerg Med. 2007;49:590–601. doi: 10.1016/j.annemergmed.2006.12.004. 601.e1-12. [DOI] [PubMed] [Google Scholar]
- 42.Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64:1427–34. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Charatan F. US government declares emergency after Hurricane Katrina. BMJ. 2005;331:531. doi: 10.1136/bmj.331.7516.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Public Health Grand Rounds. Learning from Katrina: tough lessons in preparedness and emergency response. [cited 2006 Feb 29]. Available from: URL: http://www.publichealthgrandrounds.unc.edu/katrina306/index.htm.
- 45.Illness surveillance and rapid needs assessment among hurricane Katrina evacuees: Colorado, September 1–23, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(9):244–7. [PubMed] [Google Scholar]
- 46.U.S. Army Corps of Engineers, New Orleans District. History of hurricane occurrences along coastal Louisiana. New Orleans: U.S. Army Corps of Engineers; 1972. [Google Scholar]
- 47.Jhung MA, Shehab N, Rohr-Allegrini C, Pollock DA, Sanchez R, Guerra F, et al. Chronic disease and disasters: medical demands of Hurricane Katrina evacuees. Am J Prev Med. 2007;33:207–10. doi: 10.1016/j.amepre.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 48.Noji EK. The public health consequences of disasters. Prehosp Disaster Med. 2000;15:147–57. [PubMed] [Google Scholar]
- 49.Mokdad AH, George GA, Posner SF, Reed E, Simoes EJ, Engelgau MM. When chronic conditions become acute: prevention and control of chronic diseases and adverse health outcomes during natural disasters. Prev Chronic Dis. 2005;2 Spec no: A04. [PMC free article] [PubMed] [Google Scholar]
- 50.Harrison E. Suffering a slow recovery: failed rebuilding after Katrina sets off a mental health crisis. Sci Am. 2007;297(22):25. [PubMed] [Google Scholar]
- 51.Bohannon J. After Katrina. Katrina leaves behind a pile of scientific questions. Science. 2005;309:1981. doi: 10.1126/science.309.5743.1981. [DOI] [PubMed] [Google Scholar]
- 52.Berggren R, Curiel TJ. After the storm—health care infrastructure in post-Katrina New Orleans. N Engl J Med. 2006;354:1549–52. doi: 10.1056/NEJMp068039. [DOI] [PubMed] [Google Scholar]
- 53.Bohannon J, Enserink M. Hurricane Katrina. Scientists weigh options for rebuilding New Orleans. Science. 2005;309:1808–9. doi: 10.1126/science.309.5742.1808. [DOI] [PubMed] [Google Scholar]
- 54.Quarantelli EL, Dynes RR. When disaster strikes (it isn't much like what you've heard and read about) Psychology Today. 1972;5:66–70. [Google Scholar]
- 55.Tierney K. Disaster beliefs and institutional interests: recycling disaster myths in the aftermath of 9-11. In: Clarke L, editor. Terrorism and disaster: new threats, new ideas. Research in social problems and public policy, vol 11. Burlington (MA): Elsevier Science; 2003. pp. 33–51. [Google Scholar]
- 56.Schoch-Spana M. Educating, informing and mobilizing the public. In: Levy BS, Sidel VW, editors. Terrorism and public health: a balanced approach to strengthening systems and protecting people. New York: Oxford University Press; 2003. pp. 118–35. [Google Scholar]
- 57.Reicher SD, Hopkins N. Self and nation: categorization, contestation and mobilisation. London: Sage Publications; 2001. [Google Scholar]
- 58.Henderson GS. Hurricane Katrina. Finding supplies. N Engl J Med. 2005;353:1542. doi: 10.1056/NEJMp058230. [DOI] [PubMed] [Google Scholar]
- 59.Freud A, Burlingham DT. War and children. New York: Medical War Books; 1943. [Google Scholar]
- 60.Moore HE. Tornadoes over Texas: a study of Waco and San Angelo in disaster. Austin (Texas): University of Texas Press; 1958. [Google Scholar]
- 61.Milne G. Cyclone Tracy: I. Some consequences of the evacuation of adult victims. Aust Psychologist. 1977;12:39–54. [Google Scholar]
- 62.Milne G. Cyclone Tracy: II. Some consequences of the evacuation for adult victims. Aust Psychologist. 1977;12:55–62. [Google Scholar]
- 63.DeVries AC, Glasper ER, Detillion CE. Social modulation of stress responses. Physiol Behav. 2003;79:399–407. doi: 10.1016/s0031-9384(03)00152-5. [DOI] [PubMed] [Google Scholar]
- 64.Katrina lessons. The New York Times 2006 Apr 21.
- 65.Rathbun KC, Cranmer H. Hurricane Katrina and disaster medical care. N Engl J Med. 2006;354:772–3. doi: 10.1056/NEJMc052957. [DOI] [PubMed] [Google Scholar]
- 66.Coker AL, Hanks JS, Eggleston KS, Risser J, Tee PG, Chronister KJ, et al. Social and mental health needs assessment of Katrina evacuees. Disaster Manag Response. 2006;4:88–94. doi: 10.1016/j.dmr.2006.06.001. [DOI] [PubMed] [Google Scholar]