A Systematic Review and Meta-Analysis of Pregnancy Outcomes in Patients with Systemic Lupus Erythematosus and Lupus Nephritis (original) (raw)
Abstract
Background and objectives: Studies of the impact of systemic lupus erythematosus (SLE) and its pregnancy complications have yielded conflicting results. Major limitations of these studies relate to their small numbers of patients and retrospective designs. The aim of this study was to perform a systematic literature review of pregnancy outcomes in women with SLE and a meta-analysis of the association of lupus nephritis with adverse pregnancy outcomes.
Design, setting, participants, & measurements: We searched electronic databases from 1980 to 2009 and reviewed papers with validity criteria. Random-effects analytical methods were used to evaluate pregnancy complications rates.
Results: Thirty-seven studies with 1842 patients and 2751 pregnancies were included. Maternal complications included lupus flare (25.6%), hypertension (16.3%), nephritis (16.1%), pre-eclampsia (7.6%), and eclampsia (0.8%). The induced abortion rate was 5.9%, and when excluded, fetal complications included spontaneous abortion (16.0%), stillbirth (3.6%), neonatal deaths (2.5%), and intrauterine growth retardation (12.7%). The unsuccessful pregnancy rate was 23.4%, and the premature birth rate was 39.4%. Meta-regression analysis showed statistically significant positive associations between premature birth rate and active nephritis and increased hypertension rates in subjects with active nephritis or a history of nephritis. History of nephritis was also associated with pre-eclampsia. Anti-phospholipid antibodies were associated with hypertension, premature birth, and an increased rate of induced abortion.
Conclusions: In patients with SLE, both lupus nephritis and anti-phospholipid antibodies increase the risks for maternal hypertension and premature births. The presented evidence further supports timing of pregnancy relative to SLE activity and multispecialty care of these patients.
Systemic lupus erythematosus (SLE) is a multisystem autoimmune connective tissue disorder that primarily affects women of childbearing age. Normal fertility and sterility rates have been reported, and as such, pregnancy is a frequent occurrence in these patients (1).
Two major issues exist regarding the risks and management of pregnancy in women with SLE and renal disease. First, pregnancy may increase SLE activity and the short- and long-term adverse effects on renal function, potentially leading to accelerated progression to end-stage renal disease. Second, these pregnancies are at high risk for maternal and fetal complications, including spontaneous abortion and premature delivery, intrauterine growth retardation (IUGR), and superimposed pre-eclampsia. However, multiple studies directed at elucidating the impact of SLE on pregnancy outcomes have yielded conflicting results.
Although early studies suggested an association between SLE and poor pregnancy prognosis (2,3), more recent data have shown improved outcomes, (4,5), including recently quoted live birth rates in at least 85% of pregnancies. Published data have identified several risk factors for poor pregnancy outcomes, including hypertension (6), anti-phospholipid syndrome, and SLE renal involvement (7–9).
The impact of lupus nephritis on fetal and maternal prognoses is not fully understood and has been a subject of controversy. Stable renal disease throughout pregnancy has been observed in some SLE patients, even in those with lupus nephritis and diffuse glomerular lesions (10,11). In contrast, the rate of pregnancy loss in patients with active nephritis was reported to be as high as 60% (12). However, the studies supporting this association are retrospective in character, with relatively small numbers of patients. In this study, we perform a systematic review and meta-analysis by combining information from relevant studies to (1) examine the association of maternal and fetal complications and SLE and (2) study the effects of the activity of lupus nephritis, including the World Health Organization biopsy classification, and the presence of anti-phospholipid antibodies (APAs) on pregnancy outcomes.
Materials and Methods
Study Selection
We conducted an electronic literature search from 1966 to April 2009 in Medline, PubMed, Embase, Lilacs, Science Citation Index, and the Cochrane Controlled Trials Register. We used a protocol that included the Cochrane Collaboration's search strategy for randomized controlled trials and the following terms: SLE, pregnancy outcome, lupus nephritis.
Studies were included if they addressed the outcome of SLE pregnancies and fulfilled the predefined requirements. Study quality was assessed using the study validation score (Table 1), developed by the investigators. Variables included are defined in Table 1. All variables were scored equally, with a value of four or greater used to classify papers for inclusion.
Table 1.
Study validation criteria
| SLE defined using 1982 American College of Rheumatology criteria |
|---|
| Histology using World Health Organization classification |
| Defined hypertension in pregnancy |
| Defined pregnancy outcomes |
| Follow up for at least 1 month |
| At least 80% patients had follow up |
| SLE disease activity index used |
We contacted the authors of these papers to retrieve additional data not published in their analyses. Language was not an exclusion criterion, and translators were used when required. Data were extracted into a preformed Microsoft Excel database using predefined variables to obtain data about pregnancies and maternal and fetal outcomes. Study selection, data extraction, and assigning of a quality score were performed independently by two investigators, with discrepancies resolved by consensus.
Statistical Analyses
The primary fetal outcome was unsuccessful pregnancy, which included spontaneous abortion, stillbirth, or neonatal death. Secondary fetal endpoints included the individual outcomes for unsuccessful pregnancy and IUGR. For all fetal complications, induced abortions were excluded from further analysis. Maternal complications included maternal death, stroke, hypertension, pre-eclampsia or eclampsia, nephritis, and SLE flares.
Pooled event rate estimates and 95% confidence intervals (CIs) were computed using a fixed-effects approach, which reflects only the specific studies included in the analysis. Each complication was tested for study heterogeneity, with those detected as such further analyzed using the random-effects technique. Unlike the fixed-effects approach, the random-effects extends valid inferences to larger populations.
Random-effects meta-regression based on nonlinear mixed modeling was used to investigate the effect of nephritis on each of the maternal and fetal complications that showed heterogeneity across studies. P values for testing for heterogeneity or associations were computed based on the difference in log-likelihood statistics from two nested models compared with a χ2 distribution. All tests are two-tailed, with P < 0.05 considered statistically significant.
Results
Study Selection and Demographics
Our literature search yielded 133 studies, of which 74 were deemed unsuitable by title alone. The remaining 59 were independently assessed, and 37 fulfilled study entry criteria (Figure 1). Twenty-nine studies were case series, five studies were case-control studies, and three were cohort studies. Twelve studies were prospective, and 25 studies were retrospective. The 37 studies (3–7,9,11,13–42) included a total of 1842 patients and 2751 pregnancies (Table 2).
Figure 1.
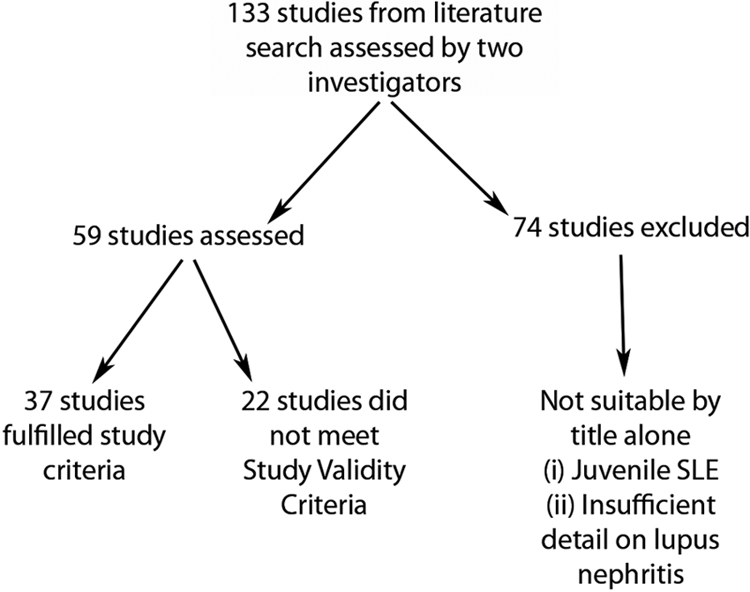
Flow diagram of studies assessed and used in this meta-analysis.
Table 2.
Characteristics of the studies included in the analyses
| No. | Author | Year | No. Patients | No. of Pregnancies | APA Positive | History of Nephritis | Active Nephritis | Flare During Pregnancy |
|---|---|---|---|---|---|---|---|---|
| 1 | Daskalakis et al. (6) | 1998 | 11 | 12 | 6 | 12 | 7 | 4 |
| 2 | Mintz et al. (13) | 1986 | 75 | 102 | n/a | 58 | 9 | 55 |
| 3 | Sittiwangkul et al. (14) | 1999 | 42 | 48 | n/a | 24 | 13 | 16 |
| 4 | Oviasu et al. (15) | 1991 | 25 | 53 | 8 | 53 | 6 | 1 |
| 5 | Le Houng et al. (16) | 1997 | 38 | 62 | 28 | 17 | 1 | 17 |
| 6 | Rahman et al. (9) | 1998 | 73 | 141 | 17 | n/a | 23 | 72 |
| 7 | Georgiou et al. (17) | 2000 | 47 | 59 | 10 | n/a | 6 | 14 |
| 8 | Imbasciati et al. (11) | 1984 | 19 | 26 | n/a | 18 | 18 | 21 |
| 9 | Le Thi Houng et al. (3) | 1994 | 84 | 103 | 15 | 28 | 8 | 34 |
| 10 | Packham et al. (18) | 1992 | 41 | 64 | 21 | 46 | 34 | 16 |
| 11 | Wong et al. (19) | 1991 | 22 | 29 | 6 | 17 | 11 | 13 |
| 12 | Ruiz-Irastorza et al. (41) | 1996 | 68 | 78 | 33 | 0 | 12 | 63 |
| 13 | Julkunen et al. (20) | 1993 | 112 | 242 | 56 | 22 | n/a | n/a |
| 14 | Nossent and Swaak (21) | 1990 | 37 | 63 | 17 | 5 | 2 | 21 |
| 15 | Houng et al. (7) | 2001 | 22 | 32 | 17 | 32 | 4 | 5 |
| 16 | Wagner et al. (22) | 2009 | 58 | 90 | n/a | 43 | 23 | 2 |
| 17 | Tandon et al. (23) | 2004 | 53 | 78 | 0 | 78 | 65 | 33 |
| 18 | Wong et al. (4) | 2006 | 17 | 24 | 0 | n/a | 12 | 5 |
| 19 | Whitelaw et al. (24) | 2008 | 31 | 47 | 6 | 13 | 2 | 13 |
| 20 | Soubassi et al. (25) | 2004 | 22 | 24 | 12 | 24 | 12 | 20 |
| 21 | Surita et al. (26) | 2007 | 67 | 76 | 24 | 47 | 29 | 58 |
| 22 | Molad et al. (27) | 2005 | 20 | 29 | 11 | 2 | n/a | 6 |
| 23 | Phadungkiatwattana et al. (28) | 2007 | 68 | 122 | 0 | 0 | 8 | 20 |
| 24 | Imbasciati et al. (29) | 2008 | 81 | 113 | 27 | 113 | 34 | 34 |
| 25 | Clowse et al. (30) | 2005 | 203 | 267 | 124 | 52 | 42 | 32 |
| 26 | Cortes-Hernandez et al. (31) | 2002 | 60 | 103 | 17 | 20 | 8 | 39 |
| 27 | Cavallasca et al. (32) | 2008 | 61 | 72 | 20 | 20 | 12 | 14 |
| 28 | Chandran et al. (33) | 2005 | 31 | 52 | 17 | 17 | 0 | 3 |
| 29 | Clark et al. (34) | 2003 | 88 | 88 | 16 | 22 | 2 | 0 |
| 30 | Moroni et al. (35) | 2002 | 48 | 70 | 16 | 51 | 25 | 13 |
| 31 | Carmona et al. (36) | 2005 | 35 | 42 | 11 | 42 | 13 | 8 |
| 32 | Wang et al. (37) | 2006 | 66 | 66 | n/a | 26 | 26 | 15 |
| 33 | Zhang et al. (38) | 2007 | 26 | 34 | n/a | 34 | n/a | 8 |
| 34 | Julkunen et al. (40) | 1993 | 16 | 26 | 8 | 26 | n/a | 2 |
| 35 | Lima et al. (42) | 1995 | 90 | 108 | 44 | 14 | 14 | 74 |
| 36 | Derksen et al. (5) | 1994 | 25 | 35 | 16 | 14 | 9 | 6 |
| 37 | Carmona et al. (39) | 1999 | 46 | 60 | 16 | 10 | 2 | 15 |
| Totals (n) | 1842 | 2751 | 619 | 1000 | 492 | 747 |
Study heterogeneity was noted, with variable definitions of a history of nephritis, active nephritis and flare used in the included papers (Table 3). The 1982 American College of Rheumatology criteria for the diagnosis of systemic lupus erythematosus (43) were the most commonly used criteria, but others were also used (Table 3). Those patients who had a renal biopsy were classified according to the World Health Organization 1995 Classification System. The definitions of SLE activity varied; a few used the systemic lupus erythematosus disease activity index (SLEDAI) (Table 3).
Table 3.
Biopsy rates, disease activity rates upon study entry, and definitions used in the studies included for analysis
| No. | Author | Percent Biopsy Proven on Study Entry | Diagnostic Criteria | Disease Activity | Flare | Hypertension Definition |
|---|---|---|---|---|---|---|
| 1 | Daskalakis et al. (6) | 100% (11/11) | 1 | 1 | n/a | BP >140/90 mmHg |
| 2 | Mintz et al. (13) | 73% (55/75) | 1, 2 | 1 | 1 | n/a |
| 3 | Sittiwangkul et al. (14) | n/a | 1 | 2 | 1, 2 | SBP >140 mmHg and/or DBP >90 mmHg |
| 4 | Oviasu et al. (15) | 100% (25/25) | 3 | n/a | n/a | n/a |
| 5 | Le Houng et al. (16) | 29% (11/38) | 1 | n/a | 1 | DBP >90 mmHg |
| 6 | Rahman et al. (9) | n/a | 1 | 3 | 1 | SBP >140 mmHg and/or DBP >90 mmHg |
| 7 | Georgiou et al. (17) | n/a | 1 | 1 | 1 | n/a |
| 8 | Imbasciati et al. (11) | 100% (19/19) | 3 | n/a | n/a | n/a |
| 9 | Le Thi Houng et al. (3) | n/a | 1 | 1 | n/a | DBP ≥90 mmHg |
| 10 | Packham et al. (18) | 100% (41/41) | 3 | n/a | n/a | DBP ≥95 mmHg or drug therapy |
| 11 | Wong et al. (19) | 77% (17/22) | 1 | 4 | 1 | SBP ≥130 mmHg and/or DBP ≥90 mmHg |
| 12 | Ruiz-Irastorza et al. (41) | n/a | 1 | 5 | 3 | n/a |
| 13 | Julkunen et al. (20) | 12% (13/112) | 1 | n/a | n/a | n/a |
| 14 | Nossent and Swaak (21) | 13% (95/37) | 1 | 1, 6 | n/a | >140/85 mmHg |
| 15 | Houng et al. (7) | 100% (22/22) | 4 | n/a | n/a | DBP >90 mmHg |
| 16 | Wagner et al. (22) | 33% (19/58) | 4 | 1 | 1 | BP >140/90 mmHg |
| 17 | Tandon et al. (23) | 36% (19/53 | 1 | 1, 7, 8 | 1 | n/a |
| 18 | Wong et al. (4) | n/a | 1 | 1 | 1 | n/a |
| 19 | Whitelaw et al. (24) | 29% (9/31) | 4 | 3 | 1 | BP >140/90 |
| 20 | Soubassi et al. (25) | 100% (22/22) | 5 | 1 | n/a | n/a |
| 21 | Surita et al. (26) | n/a | 1 | 3 | 1 | n/a |
| 22 | Molad et al. (27) | n/a | 1 | 3 | 1 | BP 140/90 mmHg |
| 23 | Phadungkiatwattana et al. (28) | n/a | 1 | n/a | 1 | SBP >140 mmHg and/or DBP >90 mmHg |
| 24 | Imbasciati et al. (29) | 100% (81/81) | 4 | 1 | 1 | SBP >140 mmHg and/or DBP >90 mmHg or drug therapy |
| 25 | Clowse et al. (30) | n/a | 1 | 9 | 1 | n/a |
| 26 | Cortes-Hernandez et al. (31) | 20% (12/60) | 1 | 3 | 1 | SBP >140 mmHg and/or DBP >90 mmHg |
| 27 | Cavallasca et al. (32) | n/a | 1 | 1 | 1 | BP ≥140/90 mmHg |
| 28 | Chandran et al. (33) | 29% (9/31) | 1 | 1, 3 | 1, 4 | SBP >140 mmHg and/or DBP >90 mmHg |
| 29 | Clark et al. (34) | n/a | 1 | 3 | n/a | n/a |
| 30 | Moroni et al. (35) | 94% (45/48) | 4 | 1 | 1 | SBP >140 mmHg and/or DBP >90 mmHg |
| 31 | Carmona et al. (36) | 100% (35/35) | 1 | 6 | 1 | BP >140/90 mmHg |
| 32 | Wang et al. (37) | n/a | 4 | 3, 7 | n/a | n/a |
| 33 | Zhang et al. (38) | 46% (12/26) | 1 | 3 | n/a | n/a |
| 34 | Julkunen et al. (40) | 100% (16/16) | 3 | 1 | 1 | n/a |
| 35 | Lima et al. (42) | n/a | 1 | 1 | 1 | n/a |
| 36 | Derksen et al. (5) | 40% (14/25) | 1 | 3 | 1 | BP >140/90 mmHg |
| 37 | Carmona et al. (39) | n/a | 1 | 6 | n/a | n/a |
Of the 37 papers included, varying terminology was used to identify women with a history of lupus nephritis, but inactive renal disease at conception, including “quiescent lupus nephritis.” For the purposes of this study, we defined having a history of nephritis as those patients with clinical, laboratory, and/or histologic evidence of lupus nephritis at the time of conception. Active nephritis was defined as the presence of proteinuria >500 mg in 24 hours and/or having an active urine sediment, with or without an elevation in serum creatinine, at the time of conception; having a lupus nephritis flare during pregnancy; and having a new diagnosis of lupus nephritis during pregnancy. APAs were considered positive if any of the following were present: anti-cardiolipin antibodies, and/or lupus anticoagulant, and/or anti-phospholipid syndrome (positive APA and clinical manifestations, including arterial and/or venous thromboses). Flares were defined as having a flare of SLE and/or lupus nephritis during pregnancy and up to, on average, 6 months postpartum, attributable to pregnancy.
Significantly, not all participants in every study had biopsy-proven lupus nephritis, although all had a confirmed diagnosis of SLE upon entry into their respective studies. Some papers included exclusively those patients with biopsy-proven lupus nephritis (n = 9); others had a varying number of patients with biopsy-proven lupus nephritis (Table 3). The proportion of patients with histories of lupus nephritis varied, as did the number of patients with active lupus nephritis upon study entry (Table 3). Very few biopsies were performed to confirm the diagnosis of lupus nephritis during pregnancy. The majority of papers included patients with both active and inactive SLE at the time of conception; only three papers assessed inactive disease only (6,16,25) and one paper looked at stable disease (15).
Analysis
Among 37 studies selected and reviewed, 34 studies had data for active nephritis at the time of conception, whereas 33 reported data on history of nephritis. The fixed-effect and random-effect rates estimated for active nephritis were 19.0 and 16.1% of pregnancies, respectively. The interstudy rates of nephritis were highly variable, as were the overall rate estimates from the fixed-effect (40.5%) and random-effect (60.9%) approaches. Thirty-two studies included data on APAs, with a positive APA rate of 26.2 (fixed-effect) and 23.6% (random-effect) of pregnancies.
Fixed-effects and random-effects rates were estimated for both fetal events (Table 4) and maternal events (Table 5). In addition, a test for study heterogeneity was performed for each complication. For the sake of brevity, and because heterogeneity was detected for most complications, only the random-effects estimates are discussed.
Table 4.
Analysis of fetal events
| Event | Denominator | Fixed-Effects Analysis | Random-Effects Analysis | ||
|---|---|---|---|---|---|
| Test for Heterogeneity | Estimated Rate (95% CI) | Estimated Rate (95% CI) | SD Estimatea | ||
| Induced abortions | Number of pregnancies | <0.001 | 7.2% (6.0%, 8.4%) | 5.9% (3.2%, 8.6%) | 5.6% |
| Spontaneous abortions | Number of pregnancies without induced abortions | <0.001 | 16.6% (14.7%, 18.5%) | 16.0% (12.1%, 19.9%) | 7.6% |
| Stillbirths | Number of pregnancies without induced abortions | 0.001 | 4.0% (2.9%, 5.1%) | 3.6% (2.0%, 5.2%) | 2.2% |
| Neonatal deaths | Number of pregnancies without induced abortions | 0.050 | 2.8% (1.9%, 3.8%) | 2.5% (1.2%, 3.8%) | 1.5% |
| Unsuccessful pregnancies | Number of pregnancies without induced abortions | 0.025 | 23.0% (20.3%, 25.6%) | 23.4% (19.5%, 27.3%) | 4.7% |
| Intra Uterine Growth Retardation (IUGR) | Number of pregnancies without induced abortions | <0.001 | 14.3% (12.4%, 16.2%) | 12.7% (8.8%, 16.7%) | 6.8% |
| Premature Birth Rate | Number of live births | <0.001 | 37.1% (34.8%, 39.4%) | 39.4% (32.4%, 46.4%) | 17.6% |
Table 5.
Maternal events analysis
| Event | Denominator | Fixed-Effects Analysis | Random-Effects Analysis | ||
|---|---|---|---|---|---|
| Test for Heterogeneity | Estimated Rate (95% CI) | Estimated Rate (95% CI) | SD Estimatea | ||
| Maternal deathb | No. of Pregnancies | <0.001 | 2.1% (1.3%, 3.0%) | 1.0% (0.0%, 2.0%) | 1.3% |
| Strokeb | No. of Pregnancies | 1.00 | 0.8% (0.0%, 1.5%) | — | — |
| Hypertension | No. of Pregnancies | <0.001 | 15.3% (13.3%, 17.3%) | 16.3% (10.3%, 22.3%) | 11.2% |
| Pre-eclampsia | No. of Pregnancies | <0.001 | 9.1% (7.4%, 10.8%) | 7.6% (3.6%, 11.6%) | 7.6% |
| Eclampsia | No. of Pregnancies | 0.184 | 0.8% (0.0%, 1.6%) | — | — |
| Active nephritis | No. of Pregnancies | <0.001 | 19.0% (17.4%, 20.6%) | 16.1% (9.0%, 23.2%) | 18.9% |
| Flares | No. of Pregnancies | <0.001 | 29.2% (27.3%, 31.0%) | 25.6% (17.4%, 33.8%) | 22.8% |
The induced abortion rate across all studies was 5.9% (95% CI, 3.2 to 8.6%). When these pregnancies were excluded, the most common fetal complications included spontaneous abortion (16.0%), IUGR (12.7%), stillbirth (3.6%), and neonatal deaths (2.5%). In all, 23.4% (95% CI, 19.5 to 27.3%) of pregnancies, without induced abortion, were unsuccessful. Among all live births, the premature birth rate was considerably high at 39.4% (95% CI, 32.4 to 46.4%).
The most frequent maternal complications included lupus flare (25.6%), hypertension (16.3%), nephritis (16.1%), and pre-eclampsia (7.6%). Severe complications, including eclampsia, stroke, and maternal death, were observed in ∼1% of subjects. Maternal deaths occurred because of opportunistic infections, sepsis, flares of lupus nephritis, and renal impairment (3,7,11,17,22,30,33,35). Of these deaths, three of the reported cases described the renal histologic subclass, and all had proliferative disease (7,17,22). Hemodialysis was rarely reported and included two patients who required hemodialysis during their pregnancies (32) and one patient who progressed to end-stage renal disease and continued dialysis therapy (35).
Random-effects meta-regression was performed to assess the effects of nephritis on maternal and fetal complications. Active nephritis was significantly associated with maternal hypertension (P < 0.001) and premature birth (P = 0.020), whereas a history of nephritis was associated with hypertension (P < 0.001) and pre-eclampsia (P = 0.017) (Table 6). After controlling for hypertension, the association between active nephritis and premature birth was still statistically significant (P = 0.016).
Table 6.
Summary of meta-regression of nephritis and adverse pregnancy outcomes
| _Y_-Variable | Meta-Regression (X) | |||
|---|---|---|---|---|
| Active Nephritis | History of Nephritis | |||
| Estimate (95% CI) | P | Estimate (95% CI) | P | |
| Induced abortion rate | 0.0508 (−0.0863, 0.1878) | 0.412 | 0.0480 (−0.0426, 0.1385) | 0.269 |
| Spontaneous abortions | 0.0604 (−0.1352, 0.2560) | 0.507 | 0.0324 (−0.0772, 0.1420) | 0.540 |
| Stillbirths | 0.0193 (−0.0510, 0.0896) | 0.544 | −0.0183 (−0.0754, 0.0387) | 0.506 |
| Neonatal death rate | 0.0496 (−0.0296, 0.1289) | 0.163 | 0.0312 (−0.0091, 0.0715) | 0.136 |
| Unsuccessful pregnancy | 0.0502 (−0.1706, 0.2709) | 0.622 | 0.0041 (−0.1200, 0.1282) | 0.943 |
| IUGR rate | −0.0855 (−0.3115, 0.1405) | 0.457 | −0.087 (−0.1450, 0.1277) | 0.892 |
| Premature birth rate | 0.4261 (0.0627, 0.7896) | 0.020 | 0.1717 (−0.0462, 0.3896) | 0.111 |
| Hypertension rate | 0.5379 (0.2647, 0.8112) | <0.001 | 0.2931 (0.1763, 0.4009) | <0.001 |
| Preeclampsia | 0.1055 (−0.1237, 0.3348) | 0.328 | 0.1352 (0.0176, 0.2528) | 0.017 |
| Eclampsia | 0.0174 (−0.0423, 0.0772) | 0.252 | 0.0174 (−0.0423, 0.0772) | 0.252 |
Additional analyses were performed to assess for an association between APAs and pregnancy outcomes. Similar to active nephritis, the presence of positive APAs was associated with hypertension (P = 0.029) and premature birth (P = 0.004). The presence of APAs correlated with an increased rate of induced abortion (P = 0.016). Importantly, there was not a statistically significant association between having APAs and the rate of active nephritis (P = 0.82).
Subgroup analyses were performed using only those studies with a 100% rate of biopsy-proven lupus nephritis on study entry (n = 9). These showed statistically significant associations between active nephritis and hypertension (P = 0.010) and between having a history of nephritis and hypertension (P = 0.002) and pre-eclampsia (P = 0.040). In addition, the presence of APAs was positively associated with premature birth rate (P < 0.001) in biopsy-proven patients. Associations approaching statistical significance were noted for premature birth rate with both active nephritis (P = 0.079) and history of nephritis (P = 0.073) and for positive APAs with both hypertension (P = 0.068) and unsuccessful pregnancy (P = 0.089).
We also analyzed pregnancy outcomes by histologic subtype in a subset of papers that correlated renal histology with maternal and/or fetal outcomes (11,13,15,16,19,22,29,31,36). Because of limited data, we grouped histologic subclasses into proliferative (classes III and IV), and nonproliferative (classes II and V) lesions. There was not a statistically significant association between histologic subclass and rate of unsuccessful pregnancy (P = 0.39) or rate of any maternal complication (P = 0.58).
Discussion
Our meta-analysis of 37 selected papers investigating the associations among pregnancy and SLE shows high rates of SLE flare, hypertension, nephritis, and pre-eclampsia. Fetal complications included spontaneous abortion, stillbirth, neonatal death, and IUGR. Overall, one quarter of pregnancies were unsuccessful, whereas among all live births, the premature birth rate was 39.4%. Active lupus nephritis seemed to increase the risk for adverse pregnancy outcomes, particularly premature birth and hypertension. Our findings provide further support for the current recommendations calling for avoidance of pregnancy until all manifestations of nephritis are quiescent. History of nephritis was associated with higher rates of pre-eclampsia, thus emphasizing the need for a multispecialty approach in the care of these patients with respect to close monitoring and early recognition of clinical signs of pre-eclampsia. Because positive APAs were associated with higher rates of hypertension, premature birth, and induced abortion, early screening for anti-cardiolipin antibodies and a lupus anti-coagulant may identify those at risk.
Studies of the associations of SLE and lupus nephritis with pregnancy outcomes showed significant variation with respect to study design, definitions, statistical methods, bias and outcomes. Early studies reported poor clinical outcomes, but a number of recent papers have shown that outcomes are better than previously thought. These differences may reflect the changing clinical environment and the emergence of new therapeutic options. In addition, discrepancies in reported pregnancy events may reflect the heterogeneity of the studies with respect to the patient populations studied, the activity of lupus nephritis, World Health Organization classification, and the presence of APAs. By performing a meta-analysis, we have more power to detect existing associations than the individual studies alone, especially given the low prevalence of these pregnancy outcomes. Furthermore, the random-effects approach to this meta-analysis allowed us to assess these rates in the larger population while appropriately accounting for all of the different types of study populations and designs used. Our results indicate that active lupus nephritis is a significant risk factor for both premature birth and hypertension, which may further contribute to maternal and fetal morbidity and mortality.
The presence of either APA or anti-phospholipid syndrome is frequently associated with SLE. When present, a high titer of anti-cardiolipin antibodies has been shown to be predictive of the clinical outcome of anti-phospholipid syndrome in SLE patients (43). A Greek study has shown that up to 50% of SLE patients may be anti-cardiolipin antibody positive (44). Similarly, the presence of a lupus anti-coagulant is also associated with adverse fetal outcomes, with an overall live birth rate of 73% and a prematurity rate of 37%, despite the use of a number of treatment modalities (45). To date, few papers have examined the associations among lupus nephritis, APAs, and pregnancy outcomes in a systematic manner. Our univariate regression analysis showed positive associations between APAs and hypertension in pregnancy, premature birth, and induced abortion. Conceivably, an increased risk for hypertension in these patients may lead to a higher risk for pre-eclampsia, a well-recognized pregnancy complication among patients with anti-phospholipid syndrome (46).
The main weakness of our paper is that of all meta-analyses: it is limited by the quality of the studies included. Because the studies were mainly observational in nature, the statistical combination of data might have been subject to selection and reporting biases (47). By establishing a strict methodology and a predefined review process, including a validity scale, we eliminated bias from our analysis where possible. Our review process was also designed to ensure that studies included were of appropriate quality because we excluded papers with insufficient methodological details, as well as those with apparent deficiencies in trial design. This is in keeping with internationally accepted approaches to meta-analysis (48). Furthermore, by using a random-effects approach for all parameters that showed study heterogeneity, we appropriately accounted for the study design variability in our analyses. We included papers of all languages by using translators when needed.
Our analysis showed positive associations between hypertension and both active nephritis and a history of nephritis in those patients with biopsy-proven lupus nephritis. We further stratified pregnancy outcomes by the World Health Organization lupus nephritis classification, which showed no differences in either fetal or maternal outcomes. However, a limited amount of data were available for this analysis, with only seven and five studies reporting sufficient data on fetal and maternal outcomes, respectively. In addition, the renal histologic pattern might not have influenced the pregnancy outcomes because of the fact that most of these biopsies were performed years before the pregnancies that were analyzed. Finally, data that were provided by the studies included in the meta-analysis were not sufficient to analyze the impact of the level of kidney function and the degree of proteinuria at the start of pregnancy on kidney function and pregnancy outcomes. These important clinical questions should be addressed by future prospective studies.
Conclusions
Our meta-analysis of 2751 pregnancies in patients with SLE showed lupus nephritis to be associated with premature birth and hypertension during pregnancy. In addition, positive APAs were associated with an increased risk for hypertension in these patients. Of note, hypertensive pregnancy disorders are increasingly recognized as risk factors for future cardiovascular disease, which is a leading cause of morbidity and mortality in SLE patients (49). Therefore, optimal timing of pregnancy in SLE patients with lupus nephritis may both decrease hypertensive pregnancy events and have a long-term impact on cardiovascular events later in life.
Our data further support the importance of pre-pregnancy counseling of women with SLE and lupus nephritis with respect to optimal timing of pregnancy relative to disease activity. It also emphasizes the importance of screening for APAs in these patients. Because much of the evidence is derived from studies focused on different outcomes, heterogeneous study designs, and defined endpoints, our study highlights the need for prospective studies with well-defined SLE activity and pregnancy outcomes.
Disclosures
None.
Acknowledgments
This study was supported in part by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K08HD051714). These data were presented at the Annual Meeting of the American Society of Nephrology; October 27 through November 1, 2009; San Diego, CA.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Cox JB: Disseminated lupus erythematosus in pregnancy. Obstet Gynecol 26: 511–514, 1965 [PubMed] [Google Scholar]
- 2.Bear R: Pregnancy and lupus nephritis. A detailed report of six cases with a review of the literature. Obstet Gynecol 47: 715–718, 1976 [PubMed] [Google Scholar]
- 3.Le Thi Huong D, Wechsler B, Piette JC, Bletry O, Godeau P: Pregnancy and its outcome in systemic lupus erythematosus. Q J Med 87: 721–729, 1994 [DOI] [PubMed] [Google Scholar]
- 4.Wong CH, Chen TL, Lee CS, Lin CJ, Chen CP: Outcome of pregnancy in patients with systemic lupus erythematosus. Taiwan J Obstet Gynecol 45: 120–123, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Derksen RH, Bruinse HW, de Groot PG, Kater L: Pregnancy in systemic lupus erythematosus: A prospective study. Lupus 3: 149–155, 1994 [DOI] [PubMed] [Google Scholar]
- 6.Daskalakis GJ, Kontessis PS, Papageorgiou IS, Paraskevopoulos AP, Digenis GE, Karaiskakis PT, Antsaklis AK, Zerefos NS: Lupus nephritis and pregnancy. Hypertens Pregnancy 17: 23–30, 1998 [Google Scholar]
- 7.Huong DL, Wechsler B, Vauthier-Brouzes D, Beaufils H, Lefebvre G, Piette JC: Pregnancy in past or present lupus nephritis: A study of 32 pregnancies from a single centre. Ann Rheum Dis 60: 599–604, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johns KR, Morand EF, Littlejohn GO: Pregnancy outcome in systemic lupus erythematosus (SLE): A review of 54 cases. Aust N Z J Med 28: 18–22, 1998 [DOI] [PubMed] [Google Scholar]
- 9.Rahman P, Gladman DD, Urowitz MB: Clinical predictors of fetal outcome in systemic lupus erythematosus. J Rheumatol 25: 1526–1530, 1998 [PubMed] [Google Scholar]
- 10.Strauch BS, Hayslett JP: Kidney disease and pregnancy. BMJ 4: 578–582, 1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Imbasciati E, Surian M, Bottino S, Cosci P, Colussi G, Ambroso GC, Massa E, Minetti L, Pardi G, Ponticelli C: Lupus nephropathy and pregnancy. A study of 26 pregnancies in patients with systemic lupus erythematosus and nephritis. Nephron 36: 46–51, 1984 [DOI] [PubMed] [Google Scholar]
- 12.Petri M: Systemic lupus erythematosus and pregnancy. Rheum Dis Clin North Am 20: 87–118, 1994 [PMC free article] [PubMed] [Google Scholar]
- 13.Mintz G, Niz J, Gutierrez G, Garcia-Alonso A, Karchmer S: Prospective study of pregnancy in systemic lupus erythematosus. Results of a multidisciplinary approach. J Rheumatol 13: 732–739, 1986 [PubMed] [Google Scholar]
- 14.Sittiwangkul S, Louthrenoo W, Vithayasai P, Sukitawut W: Pregnancy outcome in Thai patients with systemic lupus erythematosus. Asian Pac J Allergy Immunol 17: 77–83, 1999 [PubMed] [Google Scholar]
- 15.Oviasu E, Hicks J, Cameron JS: The outcome of pregnancy in women with lupus nephritis. Lupus 1: 19–25, 1991 [DOI] [PubMed] [Google Scholar]
- 16.Le Huong D, Wechsler B, Vauthier-Brouzes D, Seebacher J, Lefebvre G, Bletry O, Darbois Y, Godeau P, Piette JC: Outcome of planned pregnancies in systemic lupus erythematosus: A prospective study on 62 pregnancies. Br J Rheumatol 36: 772–777, 1997 [DOI] [PubMed] [Google Scholar]
- 17.Georgiou PE, Politi EN, Katsimbri P, Sakka V, Drosos AA: Outcome of lupus pregnancy: A controlled study. Rheumatology (Oxf) 39: 1014–1019, 2000 [DOI] [PubMed] [Google Scholar]
- 18.Packham DK, Lam SS, Nicholls K, Fairley KF, Kincaid-Smith PS: Lupus nephritis and pregnancy. Q J Med 83: 315–324, 1992 [PubMed] [Google Scholar]
- 19.Wong KL, Chan FY, Lee CP: Outcome of pregnancy in patients with systemic lupus erythematosus. A prospective study. Arch Intern Med 151: 269–273, 1991 [PubMed] [Google Scholar]
- 20.Julkunen H, Jouhikainen T, Kaaja R, Leirisalo-Repo M, Stephansson E, Palosuo T, Teramo K, Friman C: Fetal outcome in lupus pregnancy: A retrospective case-control study of 242 pregnancies in 112 patients. Lupus 2: 125–131, 1993 [DOI] [PubMed] [Google Scholar]
- 21.Nossent HC, Swaak TJ: Systemic lupus erythematosus. VI. Analysis of the interrelationship with pregnancy. J Rheumatol 17: 771–776, 1990 [PubMed] [Google Scholar]
- 22.Wagner SJ, Craici I, Reed D, Norby S, Bailey K, Wiste HJ, Wood CM, Moder KG, Liang KP, Liang KV, Rose C, Rozkos T, Sitina M, Grande JP, Garovic VD: Maternal and foetal outcomes in pregnant patients with active lupus nephritis. Lupus 18: 342–347, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tandon A, Ibanez D, Gladman DD, Urowitz MB: The effect of pregnancy on lupus nephritis. Arthritis Rheum 50: 3941–3946, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Whitelaw DA, Hall D, Kotze T: Pregnancy in systemic lupus erythematosus: A retrospective study from a developing community. Clin Rheumatol 27: 577–580, 2008 [DOI] [PubMed] [Google Scholar]
- 25.Soubassi L, Haidopoulos D, Sindos M, Pilalis A, Chaniotis D, Diakomanolis E, Antsaklis A, Zerefos N: Pregnancy outcome in women with pre-existing lupus nephritis. J Obstet Gynaecol 24: 630–634, 2004 [DOI] [PubMed] [Google Scholar]
- 26.Surita FG, Parpinelli MA, Yonehara E, Krupa F, Cecatti JG: Systemic lupus erythematosus and pregnancy: Clinical evolution, maternal and perinatal outcomes and placental findings. Sao Paulo Med J 125: 91–95, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Molad Y, Borkowski T, Monselise A, Ben-Harous A, Sulkes J, Hod M, Feldberg D, Bar J: Maternal and fetal outcome of lupus pregnancy: A prospective study of 29 pregnancies. Lupus 14: 145–151, 2005 [DOI] [PubMed] [Google Scholar]
- 28.Phadungkiatwattana P, Sirivatanapa P, Tongsong T: Outcomes of pregnancies complicated by systemic lupus erythematosus (SLE). J Med Assoc Thai 90: 1981–1985, 2007 [PubMed] [Google Scholar]
- 29.Imbasciati E, Tincani A, Gregorini G, Doria A, Moroni G, Cabiddu G, Marcelli D: Pregnancy in women with pre-existing lupus nephritis: Predictors of fetal and maternal outcome. Nephrol Dial Transplant 24: 519–525, 2009 [DOI] [PubMed] [Google Scholar]
- 30.Clowse ME, Magder LS, Witter F, Petri M: The impact of increased lupus activity on obstetric outcomes. Arthritis Rheum 52: 514–521, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Cortes-Hernandez J, Ordi-Ros J, Paredes F, Casellas M, Castillo F, Vilardell-Tarres M: Clinical predictors of fetal and maternal outcome in systemic lupus erythematosus: A prospective study of 103 pregnancies. Rheumatology (Oxf) 41: 643–650, 2002 [DOI] [PubMed] [Google Scholar]
- 32.Cavallasca JA, Laborde HA, Ruda-Vega H, Nasswetter GG: Maternal and fetal outcomes of 72 pregnancies in Argentine patients with systemic lupus erythematosus (SLE). Clin Rheumatol 27: 41–46, 2008 [DOI] [PubMed] [Google Scholar]
- 33.Chandran V, Aggarwal A, Misra R: Active disease during pregnancy is associated with poor foetal outcome in Indian patients with systemic lupus erythematosus. Rheumatol Int 26: 152–156, 2005 [DOI] [PubMed] [Google Scholar]
- 34.Clark CA, Spitzer KA, Nadler JN, Laskin CA: Preterm deliveries in women with systemic lupus erythematosus. J Rheumatol 30: 2127–2132, 2003 [PubMed] [Google Scholar]
- 35.Moroni G, Quaglini S, Banfi G, Caloni M, Finazzi S, Ambroso G, Como G, Ponticelli C: Pregnancy in lupus nephritis. Am J Kidney Dis 40: 713–720, 2002 [DOI] [PubMed] [Google Scholar]
- 36.Carmona F, Font J, Moga I, Lazaro I, Cervera R, Pac V, Balasch K: Class III-IV proliferative lupus nephritis and pregnancy: a study of 42 cases. Am J Reprod Immunol 53: 182–188, 2005 [DOI] [PubMed] [Google Scholar]
- 37.Wang YH, Wu XX, Tan JP, Zhang JP: Influential factors of systemic lupus erythematosus activity during pregnancy and its relationship with pregnancy outcome [in Chinese]. Chin J Obstet Gynecol 41: 601–604, 2006 [PubMed] [Google Scholar]
- 38.Zhang L, Abe K, Hashimoto H, Takasaki Y: Pregnancy and fetal outcomes in patients with lupus nephritis [in Japanese]. Jpn J Clin Immunol 30: 185–192, 2007 [DOI] [PubMed] [Google Scholar]
- 39.Carmona F, Font J, Cervera R, Munoz F, Cararach V, Balasch J: Obstetrical outcome of pregnancy in patients with systemic lupus erythematosus. A study of 60 cases. Eur J Obstet Gynecol Reprod Biol 83: 137–142, 1999 [DOI] [PubMed] [Google Scholar]
- 40.Julkunen H, Kaaja R, Palosuo T, Gronhagen-Riska C, Teramo K: Pregnancy in lupus nephropathy. Acta Obstet Gynecol Scand 72: 258–263, 1993 [DOI] [PubMed] [Google Scholar]
- 41.Ruiz-Irastorza GLF, Alves J, Khamashta MA, Simpson J, Hughes GRV, Buchanan NMM: Increased rate of lupus flare during pregnancy and the puerperium: A prospective study of 78 pregnancies. Br J Rheum 35: 133–138, 1996 [DOI] [PubMed] [Google Scholar]
- 42.Lima FNM, Khamashta MA, Kerslake S, Hughes GRV: Obstetric outcome in systemic lupus erythematosus. Semin Arthrit Rheum 25: 184–192, 1995 [DOI] [PubMed] [Google Scholar]
- 43.Lynch A, Marlar R, Murphy J, Davila G, Santos M, Rutledge J, Emlen W: Antiphospholipid antibodies in predicting adverse pregnancy outcome. A prospective study. Ann Intern Med 120: 470–475, 1994 [DOI] [PubMed] [Google Scholar]
- 44.Mavragani CP, Dafni UG, Tzioufas AG, Moutsopoulos HM: Pregnancy outcome and anti-Ro/SSA in autoimmune diseases: A retrospective cohort study. Br J Rheumatol 37: 740–745, 1998 [DOI] [PubMed] [Google Scholar]
- 45.Branch DW, Silver RM, Blackwell JL, Reading JC, Scott JR: Outcome of treated pregnancies in women with antiphospholipid syndrome: An update of the Utah experience. Obstet Gynecol 80: 614–620, 1992 [PubMed] [Google Scholar]
- 46.Saha SP, N B, Ganguli RP, Sil S, Patra KK, Sengupta M, Barui G, Goswami BK: Prevalence and significance of antiphospholipid antibodies in selected at-risk obstetrics cases: A comparative prospective study. Obstet Gynecol 29: 614–618, 2009 [DOI] [PubMed] [Google Scholar]
- 47.Egger M, Schneider M, Davey Smith G: Spurious precision? Meta-analysis of observational studies. BMJ 316: 140–144, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Juni P, Altman DG, Egger M: Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 323: 42–46, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Agarwal S, Elliott JR, Manzi S: Atherosclerosis risk factors in systemic lupus erythematosus. Curr Rheumatol Rep 11: 241–247, 2009 [DOI] [PubMed] [Google Scholar]
- 50.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ: The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25: 1271–1277, 1982 [DOI] [PubMed] [Google Scholar]
- 51.Cohen AS: Preliminary criteria for the classification of systemic lupus erythematosus. Bull Rheum Dis 21: 643–648, 1971 [Google Scholar]
- 52.Hochberg MC: Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40: 1725, 1997 [DOI] [PubMed] [Google Scholar]
- 53.Ruiz-Irastorza G, Khamashta M, Hughes GR: Does SLE flare during pregnancy? Scand J Rheumatol Suppl 107: 76–79, 1998 [DOI] [PubMed] [Google Scholar]
- 54.Guzman J, Cardiel MH, Arce-Salinas A, Sanchez-Guerrero J, Alarcon-Segovia D: Measurement of disease activity in systemic lupus erythematosus. Prospective validation of 3 clinical indices. J Rheumatol 19: 1551–1558, 1992 [PubMed] [Google Scholar]
- 55.Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH: Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35: 630–640, 1992 [DOI] [PubMed] [Google Scholar]
- 56.Lockshin MD, Reinitz E, Druzin ML, Murrman M, Estes D: Lupus pregnancy. Case-control prospective study demonstrating absence of lupus exacerbation during or after pregnancy. Am J Med 77: 893–898, 1984 [DOI] [PubMed] [Google Scholar]
- 57.Petri M, Genovese M, Engle E, Hochberg M: Definition, incidence and clinical description of flare in systemic lupus erythematosus: A prospective cohort study. Arthritis Rheum 34: 937–944, 1991 [DOI] [PubMed] [Google Scholar]
- 58.Urowitz MB, Gladman DD, Tozman EC, Goldsmith CH: The lupus activity criteria count (LACC). J Rheumatol 11: 783–787, 1984 [PubMed] [Google Scholar]
- 59.Gladman DD, Ibanez D, Urowitz MB: Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29: 288–291, 2002 [PubMed] [Google Scholar]
- 60.Ibanez D, Urowitz MB, Gladman DD: Summarizing disease features over time: I. Adjusted mean SLEDAI derivation and application to an index of disease activity in lupus. J Rheumatol 30: 1977–1982, 2003 [PubMed] [Google Scholar]
- 61.Petri M, Howard D, Repke J: Frequency of lupus flare in pregnancy. The Hopkins Lupus Pregnancy Center experience. Arthritis Rheum 34: 1538–1545, 1991 [DOI] [PubMed] [Google Scholar]