Number and location of venous valves within the popliteal and femoral veins – a review of the literature (original) (raw)
Abstract
Although deep venous insufficiency is common and important, the anatomy of deep vein valves is poorly understood. The aim of this study was to investigate the location, number and consistency of venous valves in the femoral and popliteal veins in normal subjects. A detailed literature search of PubMed was performed. Abstracts and selected full text articles were scrutinised and relevant studies published between 1949 and 2010 reporting anatomical details of deep vein valves were included. From 7470 articles identified by the initial search strategy, nine studies with a total of 476 legs were included in this review. All studies were cadaveric and subjects ranged from stillborn fetuses to 103 years of age. Studies suggested that femoral veins contain between one and six valves, and popliteal veins contain between zero and four valves. Deep vein valves were consistently located in the common femoral vein (within 5 cm of the inguinal ligament), the femoral vein (within 3 cm of the deep femoral vein tributary) and in the popliteal vein near the adductor hiatus. Valves are consistently located at specific locations in the deep veins of the leg, although there is often significant variability between subjects. Further anatomical and functional studies using new imaging modalities available should target these areas to identify whether certain valves play a more important role in venous disease. This may guide us in the development of new treatment options for patients with deep venous disease.
Keywords: chronic venous disease, femoral vein, popliteal vein, vein valve, venous insufficiency
Introduction
Venous disease affects up to a third of the United Kingdom adult population and is estimated to cost the National Health Service 2% of the annual budget (Van den Oever et al. 1998). The usual cause is a failure of the valves in the superficial or deep veins of the legs either due to primary valve failure or secondary to deep venous thrombosis. A number of treatments are available for superficial venous reflux, including traditional surgery and minimally invasive endovenous modalities. However, significant deep vein disease, usually due to valve failure, may be a feature in up to a quarter of patients (Hanrahan et al. 1991). The deep veins of the lower limb accompany all major arteries and their branches. Blood flows back to the heart in the deep veins and is maintained by unidirectional (Lurie et al. 2002), usually bicuspid (Powell & Lynn, 1951; Basmajian, 1952), valves which close as the valve leaflets move towards the centre of the vein (Lurie et al. 2003). Although the discovery of venous valves is generally attributed to Fabricus ab Aquapendente in 1579, earlier anatomists including Charles Estienne (1539), Giovanni Battista Canano (1551) demonstrated valves but were ridiculed as their work could not be repeated (Scultetus et al. 2001).
Treatment options for patients with deep venous disease are limited to conservative measures, compression hosiery, which is often poorly tolerated by patients (Raju & Neglén, 2009) or major deep venous surgery, often with limited success (Perrin, 2004). Advances in the treatment of deep veins are needed to benefit this large cohort of people. The number, location and consistency of deep vein valves in normal subjects are poorly understood. An understanding of these details is essential to inform and guide the development of novel interventions and treatments for patients with deep venous disease.
The aim of this review article was to investigate the location, number and consistency of venous valves in the femoral and popliteal veins in normal subjects.
Materials and methods
The review was conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (http://www.prisma-statement.org). Relevant papers were identified through systematic searches of PubMed (1966 to October 2010). The search terms ‘femoral vein valve’, ‘popliteal vein valve’, ‘femoral vein’, ‘venous valves’ and ‘venous valve AND lower limb’ were used. Human limits were applied and article titles and abstracts were screened for inclusion. A manual reference list search was also carried out for further appropriate studies to be considered for inclusion, ensuring relevant papers published before 1966 were included. Relevant full text articles were scrutinised and all anatomical studies reporting details of deep vein valves were included. Articles concerning deep vein thrombosis, the treatment of deep venous disease, deep venous valve surgery or replacement, superficial vein anatomy and cardiac valves were excluded.
Results
Although the initial search strategy yielded 7472 results, following exclusion of non-relevant publications, a total of nine articles were included (Fig. 1). All selected studies involved cadaveric dissections with numbers of legs ranging from two to 184. In this review, the junction of the femoral vein (FV) and deep femoral vein (DFV) was chosen as the reference point for valve positions as it is easily identified on colour duplex ultrasound imaging. This is in contrast to the inguinal ligament and is unlikely to have been surgically altered or removed, unlike superficial venous reference points, which may have been stripped or ablated. Other venous reference points described included the saphenofemoral junction (SFJ) and saphenopopliteal junction (SPJ). The distances and locations obtained from the publications were adjusted, as they were all based on different reference points. These adjustments were calculated using the average values: from the mouth of deep femoral vein to the inguinal ligament is 9 cm and from the mouth of the long saphenous tributary to the inguinal ligament is 5 cm (Basmajian, 1952). Tables 1 and 2 summarise the studies included and present the number and location of valves within the femoral and popliteal veins, respectively.
Fig. 1.
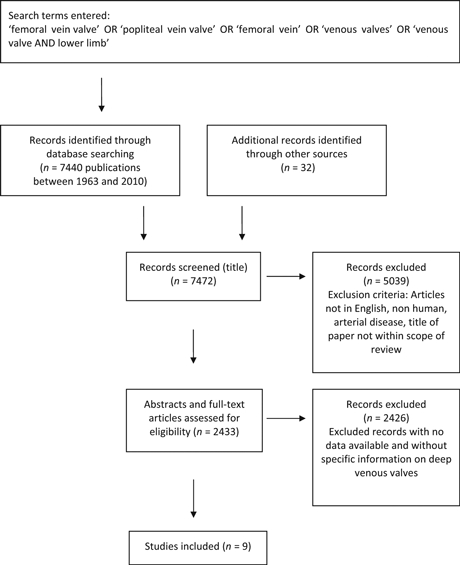
Summary of search strategy.
Table 1.
Summary of number and location of valves within the femoral veins
| Reference | No. of subjects (limbs) | Age of subjects | Sex of subjects | No. of valves in femoral vein | Location of valves in femoral vein (distance from deep femoral vein) |
|---|---|---|---|---|---|
| Genovese (c2002) | 1 (2) | Not known | Not known | 3–4 | – |
| Muhlberger et al. (2008) | 32 (63) | 56.5–103.25 | 17 male | 1–6 | 0–2 valves proximal 0–9 cm |
| 15 female | 1–3 valves distal 1.9–11.2 cm | ||||
| Powell & Lynn (1951) | 27 (54) | Still born fetus – 84 | 14 male | 2–6 | 1–2 valves proximal 44 limbs, last at inguinal ligament 9 cm |
| 13 female | 50 limbs valve ‘just below’ 1–3 cm distal, then every 2.5–16 cm | ||||
| Banjo (1987) | 92 (184) (study in black Africans) | All adults | 73 male | Not stated: All had a least 1 valve | 169 limbs ≥1 valve proximal at 5–9 cm |
| 19 female | 13 limbs ≥ 1 valve proximal at 0–5 cm | ||||
| 184 limbs ≥ 1 valve distal at 0–3 cm | |||||
| Basmajian (1952) | 38 (76) | 31–94 | 38 male | 0–6 | 51 limbs 1 valve 5–9 cm proximal |
| 2 limbs 1 valve 0–5 cm proximal | |||||
| 68 limbs 1 valve 1–3 cm distal | |||||
| Kwayke (1971) | 25 (50) | 60–85 | 20 male | 2–6 | Most constant sites: 5–9 cm proximal and 1–3 cm distal. |
| 5 female | 6 cm distal often 2nd valve (exact figures not given) | ||||
| Eger & Wagner (1949) | 100 (200) | 91 adults, 4 children, 5 infants | Not stated | Not stated | 138 limbs ≥ 1 valve at 4–9 cm proximal |
| 62 limbs no valves at 4–9 cm proximal |
Table 2.
Summary of number and location of valves within the popliteal veins
| Reference | No. of subjects (limbs) | Age of subjects | Sex of subjects | No. of valves in popliteal vein | Location of valves in popliteal vein (distance adductor hiatus) |
|---|---|---|---|---|---|
| Genovese (c2002) | 1 (2) | Not known | Not known | 1–2 | – |
| Santilli et al. (2000) | 39 (47) | Not known | 13 male | 1.8 ± 0.5 | 1st valve: 7.0 ± 5.0 cm |
| 26 female | Last valve: 14.1 ± 3.0 cm | ||||
| Powell & Lynn (1951) | 27 (54) | Still born fetus – 84 | 14 male | 1 in upper 1/3 (rest not visualised) | Just distal to adductor hiatus (1–3 cm) |
| 13 female | |||||
| Kwayke (1971) | 25 (50) | 60–85 | 20 male | 0–4, average 1–2 | Most constant sites: above junction anterior and posterior tibial veins and near adductor ring |
| 5 female |
Femoral vein valves
In a study reported in 2008, Muhlberger et al. used the saphenofemoral junction as a reference point and investigated 63 limbs (32 patients). Some 83% of legs had at least one valve proximal to the junction of the DFV and FV and distal to the inguinal ligament within the common femoral vein. Distally, 76–100% of legs had a valve distal to the junction between DFV and FV. A further cadaveric study of 54 legs from Powell & Lynn (1951) reported that a valve in the common femoral vein (CFV) was present in nearly three quarters of patients. The CFV valve was located consistently at the level of the inguinal ligament. The FV contained one to four valves in all cases, with at least two valves seen in over 90% of cases. The most common site for a valve was just distal to the junction of the DFV and FV (93% of cases).
In 1971, Kwayke reported results from 50 legs and stated that a mean of four valves were present in the femoral vein, ranging from two to six. In keeping with other studies, a valve was consistently seen just distal to the DFV opening, although a constant valve was also reported just proximal to the SFJ. This may correspond to the valve just below or at the inguinal ligament, consistently reported in other papers. Of note, the proximal part of the femoral vein was more likely to contain valves than was the distal part, unlike the popliteal vein, where valves were more frequently sited distally. A further study measured valves from the inguinal ligament and reported that 76% of the 76 legs studied had a valve in the 5 cm distal to the inguinal ligament. A valve immediately distal to the DFV/FV junction was present in nearly 90% of legs and although one limb had no valves throughout the femoral vein, the median number identified was three, with a maximum of six.
In a study of 92 black African subjects, Banjo et al. (1987) divided veins into seven segments and investigated the presence of valves. A valve was present in the CFV in 93% of legs. In keeping with other reports, all patients in this study had a valve in the 3 cm distal to the DFV junction of the FV.
Eger & Wagner (1949) by dissection of 200 limbs (100 cadavers) found that 69% of the 200 limbs studied had valves present within the common femoral vein proximal to the saphenofemoral junction, that is within 9 cm proximal to the junction of the FV and DFV. There was complete absence of valves within this region in 31%. There are significant limitations to this study, however, as only the region above the saphenofemoral junction was studied, excluding the 4 cm immediately proximal to the FV and DFV junction. The exact locations of these valves are also not discussed.
Popliteal vein valves
Defining the popliteal vein (PV) as between the adductor hiatus and confluence of anterior and posterior tibial veins, a number of studies, including Powell & Lynn (1951) and Kwayke (1971) have consistently reported the presence of a valve just distal to the adductor hiatus (Table 1). A second valve was commonly seen in the very distal segment of the PV, just proximal to anterior and posterior tibial veins (Kwayke, 1971; Santilli et al. 2000).
Discussion
This study has demonstrated that in the studies included, venous valves are consistently located in specific sites in the common femoral, femoral and popliteal veins of the leg. This is summarised in Fig. 2. Valves in the CFV, near the inguinal ligament, in the FV just distal to the DFV tributary and in the PV near the adductor hiatus were the most consistently reported sites. These findings have implications for researchers, as further clinical studies of deep vein valve function should specifically target these anatomical locations. Also, this information is also of value to those developing new surgical and minimally invasive treatments for patients with deep vein valve failure.
Fig. 2.
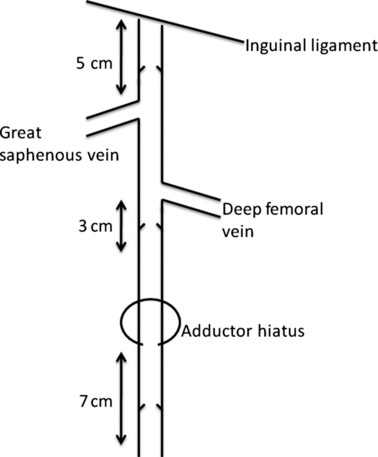
The most constant locations of valves within the femoral and popliteal veins.
This review was limited by the small number and heterogeneity in reporting of studies. This is in part due to the selection bias of the papers included, papers not included on PubMed or cited by other papers have been omitted. However, by using fixed anatomical reference points such as the inguinal ligament and DFV tributary, these findings can be amalgamated with some confidence, although this will have caused some inaccuracy, as the distances used to adjust the distances used were average values. Moreover, many of the reports were of cadaveric studies in patients without venous disease or in which the presence or absence of venous disease was not discussed. Clearly, the application of these data to a patient population with deep venous disease is suboptimal. In individual papers there are also limitations; for example, Muhlberger et al. (2008) studied femoral veins that had previously been dissected by medical students, which may have introduced some error. Further anatomical and functional studies of the importance of deep venous function are needed as this is a relatively neglected clinical area. Further studies should also aim to investigate whether some venous valves are more important than others. Such investigations could offer important clues to indicate where treatment advances for this important patient group would be best directed.
Authors' contributions
HMM: Concept, literature search, data collection, data interpretation, manuscript preparation. MSG: Literature search, data interpretation, manuscript preparation. AHD: Concept, manuscript preparation, guarantor.
References
- Banjo AO. Comparative study of the distribution of venous valves in the lower extremities of black Africans and caucasians: pathogenetic correlates of prevalence of primary varicose veins in the two races. Anat Rec. 1987;217:407–412. doi: 10.1002/ar.1092170413. [DOI] [PubMed] [Google Scholar]
- Basmajian JV. The distribution of valves in the femoral, external iliac, and common iliac veins and their relationship to varicose veins. Surg Gynecol Obstet. 1952;95:537–542. [PubMed] [Google Scholar]
- Eger AS, Wagner FB. Etiology of varicose veins. Postgrad Med. 1949;6:234–238. doi: 10.1080/00325481.1949.11945609. [DOI] [PubMed] [Google Scholar]
- Genovese G. Venous anatomy of the lower limb. Società Italiana di Flebologia. c2002. Available at: http://www.societaitalianaflebologia.it/banner/g.genovese%20anatomia.pdf.
- Hanrahan LM, Araki CT, Rodriguez AA, et al. Distribution of valvular incompetence in patients with venous stasis ulceration. J Vasc Surg. 1991;13:805–811. discussion 811–812. [PubMed] [Google Scholar]
- Kwayke LB. Frequency and distribution of the valves in the large deep and superficial veins of the lower limb in the aged. Acta Morphol Neerl Scand. 1971;9:41–46. [PubMed] [Google Scholar]
- Lurie F, Kistner RL, Eklof B. The mechanism of venous valve closure in normal physiologic conditions. J Vasc Surg. 2002;35:713–717. doi: 10.1067/mva.2002.121123. [DOI] [PubMed] [Google Scholar]
- Lurie F, Kistner RL, Eklof B, et al. Mechanism of venous valve closure and the role of the valve in circulation: a new concept. J Vasc Surg. 2003;38:955–961. doi: 10.1016/s0741-5214(03)00711-0. [DOI] [PubMed] [Google Scholar]
- Muhlberger D, Morandini L, Brenner E. An anatomical study of femoral vein valves near the saphenofemoral junction. J Vasc Surg. 2008;48:994–999. doi: 10.1016/j.jvs.2008.04.045. [DOI] [PubMed] [Google Scholar]
- Perrin M. Surgery for deep venous reflux in the lower limb. J Mal Vasc. 2004;29:73–87. doi: 10.1016/s0398-0499(04)96718-2. [DOI] [PubMed] [Google Scholar]
- Powell T, Lynn RB. The valves of the external iliac, femoral, and upper third of the popliteal veins. Surg Gynecol Obstet. 1951;92:453–455. [PubMed] [Google Scholar]
- Raju S, Neglén P. Clinical practice. Chronic venous insufficiency and varicose veins. N Engl J Med. 2009;360:2319–2327. doi: 10.1056/NEJMcp0802444. [DOI] [PubMed] [Google Scholar]
- Santilli SM, Lee ES, Wernsing SE, et al. Superficial femoral popliteal vein: an anatomic study. J Vasc Surg. 2000;31:450–455. [PubMed] [Google Scholar]
- Scultetus AH, Villavicencio L, Rich NM. Facts and fiction surrounding the discovery of venous valves. J Vasc Surg. 2001;33:435–441. doi: 10.1067/mva.2001.109772. [DOI] [PubMed] [Google Scholar]
- Van den Oever R, Hepp B, Debbaut B, et al. Socio-economic impact of chronic venous insufficiency. An underestimated public health problem. Int Angiol. 1998;17:161–167. [PubMed] [Google Scholar]