Scalpel versus electrosurgery: Comparison of gingival perfusion status using ultrasound Doppler flowmetry (original) (raw)
Abstract
The main prerequisites of any surgical procedure are achievement of good visibility and access to the site with minimal bleeding and rapid and painless healing. With the advancement of technology the armamentarium for oral surgical procedures has also widened. The use of alternate methods to the traditional scalpel such as electrosurgery, laser, and chemicals has been widely experimented with. This article aims to report the gingival perfusion pre-operatively and post-operatively, comparing the use of scalpel and electrosurgery in different anatomic sites in patient. Since wound healing is influenced by its revascularization rate, which follows the pattern of new connective tissue formation, the perfusion status of the gingiva has been studied using ultrasound spectral Doppler. The results of our study show that there was 30% more blood flow by 7th day, 19% more blood flow by 15th day and 11% more blood flow by 30th day in sites where the scalpel was used compared with sites where electrosurgery technique was used.
KEY WORDS: Electrosurgery, gingival vasularity, scalpel technique, ultrasound Doppler, wound healing
The main objectives of any minor oral surgical procedures are an improvement of prognosis of teeth and improvement of esthetics. While surgical entry relies mainly on scalpel, it can be approached by other means also that includes electrodes, lasers or chemicals. In all cases, however certain technical goals are essential, including control of hemorrhage, visibility, absence of harmful effects to the surgical site and adjacent tissues, post-operative comfort and rapid healing.
Successful wound healing following oral surgery is strongly influenced by the revascularization rate as well as by the preservation and reconstruction of the microvasculature of the tissues. Repair of connective tissue also depends on the development of a new vascular system, which can supply blood and nutrients to the wound area. The nutritional demands of the wound are greater than those of the non-wounded connective tissue and they are the greatest at the time when the local circulation is least capable of complying with the demand. Furthermore, an improved healing process would also imply less post-operative complications and improved post-operative comfort for the patients.[1]
Several methods have been documented for measuring the gingival blood flow (GBF) including vital microscopy of the gingival margin,[2] implantation of microspheres into the internal carotid artery,[3] infused radioisotopes and radio labeled microspheres[4] and high speed cinematography,[5] most of which are invasive and not suitable for clinical application on patients. The laser Doppler flowmetry,[6] is a non-invasive and real time method for perfusion measurements, but it has several significant shortcomings. Only a localized small area of gingival tissue beneath the area of placement of the laser probe can be studied at a time. Furthermore, comparison of blood flow changes between different sites in the same patient and between different patients is not possible.[1]
To overcome the above mentioned shortcomings, we have measured the perfusion status of the gingiva by using ultrasound Doppler based on the use of soft-tissue ultrasonography (USG) and spectral Doppler studies in patients with soft-tissue,[7,8] vascular,[9] and osseous lesions,[10] in oral and maxillofacial regions.
A case of delayed apical migration of the gingiva (excessive gingival display due to delayed migration of the gingival margin apical to the cementoenamel junction during tooth eruption),[11] with hyperpigmentation is reported. Gingivoplasty and depigmentation was carried out using both scalpel and electrosurgery at different anatomic sites. Their perfusion status was compared with soft-tissue USG and spectral Doppler study.
Case Report
A 22-year-old female patient reported, with a chief complaint of small teeth and black gums. On examination, gingiva appeared hyperpigmented (blackish purple in color) and the marginal gingiva was enlarged thick and fibrotic [Figure 1]. Complete medical history and blood investigation was carried out to rule out any systemic condition. A diagnosis of delayed apical migration of the gingiva with hyperpigmentation was made. Treatment plan included gingivoplasty and depigmentation under local anesthesia. The surgical procedure was explained to patient and informed consent was obtained.
Figure 1.

Pre-operative view
The procedure was planned to be performed using a scalpel in lower anterior and electrosurgery (surgical techniques performed using controlled, high frequency electrical currents i.e., 1.5-7.5 million cycles/s) in upper anterior to determine the healing pattern with these two different techniques. Gingival vascularity was determined using soft-tissue USG with spectral Doppler study.
Ultrasound doppler methodology
USG studies were performed using a high definition USG unit with 2D, 3D and color Doppler facilities [Figure 2]. For gingival study, intracavitary convex transducer with 9-5 MHz capacity was used since this probe facilitated adequate and satisfactory intra-oral accessibility. For the study of anterior segment gingiva, a cheek retractor was used and a water filled glove finger was placed over the gingiva. The transducer was applied over the water filled glove finger in a coronal plane with interspersed ultrasonic gel for proper contact. The water filled glove finger served as a water path for the sound waves and provided better clarity and detail. USG settings were adjusted for 4.5 cm depth, which would be adequate for covering the depth of the water path and the gingiva.
Figure 2.

High definition ultrasonography unit with 2D, 3D and color doppler facilities
In Doppler settings, sound waves pass through blood vessels and get scattered (reflected) by moving red blood cells. Color Doppler settings delineate the color coded blood vessels as rounded or oval dots or linear or cylindrical structures. The number of color coded structures will indicate the number of blood vessels in the region under study. Thus, color Doppler gives information about the amount of vascularity in the region of interest. For spectral Doppler studies, pulse wave Doppler cursor is focused over the blood vessels, which are depicted as color coded blood vessels and the update key is pressed. This enables delineation of flow pattern in the gingival graphically. Recording the flow pattern in the form of a graph (spectral Doppler) allows measurement of velocity of flow both in peak systolic velocity (PSV) and end diastolic velocity phases. These values are displayed on the monitor once the tracing over the graph is marked by auto or manual mode. This helps to measure the velocity of flow.
By the placement of the transducer in a sagittal plane over both upper (13-23 region) and lower (33-43 region) segments, study of the gingiva in both arches is possible in the same field.
Pre-operative
Pre-operatively the spectral Doppler study was performed in both upper [Figure 3] and lower anterior gingival segment [Figure 4]. The PSV was determined.
Figure 3.
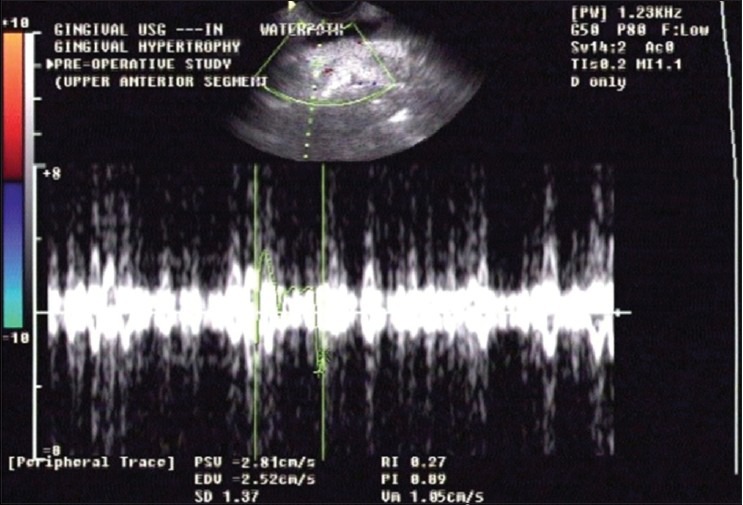
Pre-operative spectral Doppler of upper anterior segment
Figure 4.
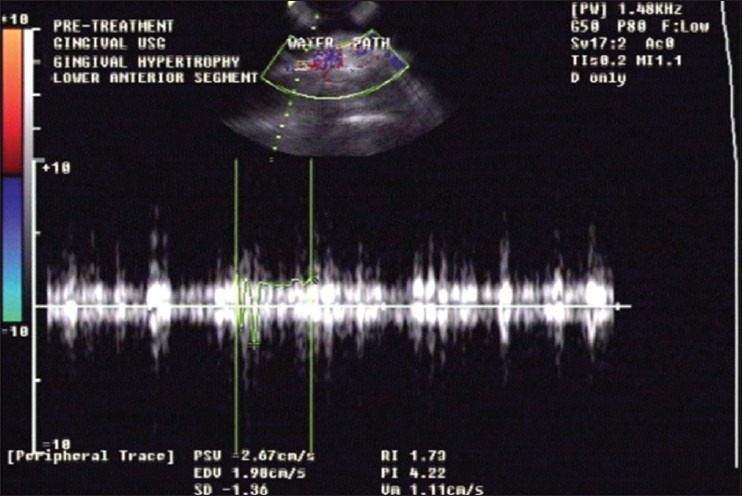
Pre-operative spectral Doppler of lower anterior segment
Surgical procedure
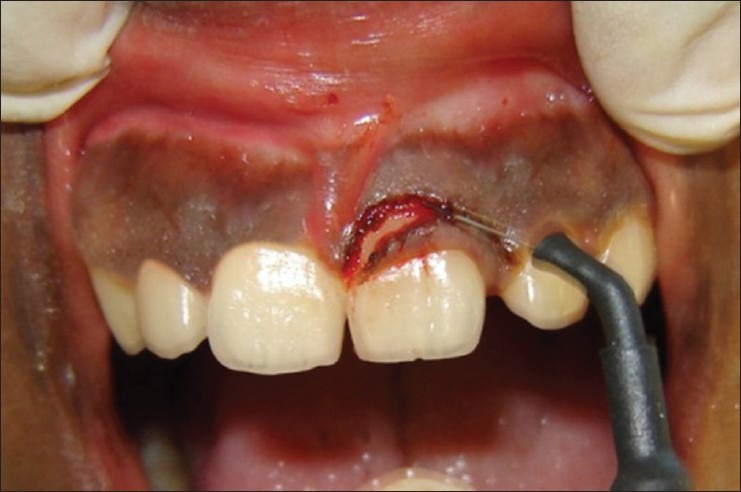
After administration of local anesthesia, gingivoplasty and depigmentation (the entire pigmented epithelium along with a thin layer of connective tissue was removed) was performed using No. 15 blade (scalpel) in lower anterior segment [Figures 5 and 6]. Hemostasis was obtained using sterile gauze and applying direct pressure on the surgical wound.
Figure 5.

Scalpel being used in lower anterior segment
Figure 6.

Immediate post-operative view of lower anterior segment
In relation to upper anterior segment, the procedure was performed using the electrosurgery. Using a loop electrode, the entire pigmented epithelium along with a thin layer of connective tissue was removed by a planning motion from the mucogingival junction to the marginal gingiva [Figures 7 and 8]. The region was irrigated with saline frequently to dissipate the heat generated by the electrode. Care was taken that the electrode did not touch the bone. Compared with the surgical technique carried out by using a scalpel, the electrosurgery procedure produced less bleeding, which offered better visibility. Patient was placed on analgesics and 0.2% chlorhexidine digluconate mouth rinse twice daily for 2 weeks.
Figure 7.
Loop electrode being used in upper anterior segment
Figure 8.

Immediate post-operative view of lower anterior segment (below)
Post-operative follow-up
Patient was recalled on 7th, 15th and 30th day following surgery. Both clinical examination [Figure 9a-d] and spectral Doppler studies [Figure 10a-f] were performed in upper and lower anterior region to compare the perfusion state.
Figure 9a.

7th day post-operative view of lower anterior segment
Figure 9d.

30th day post-operative view of upper anterior segment
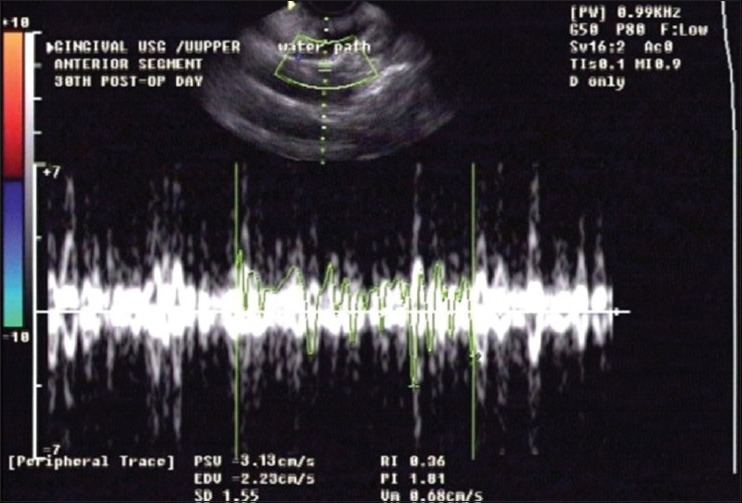
Figure 10a.
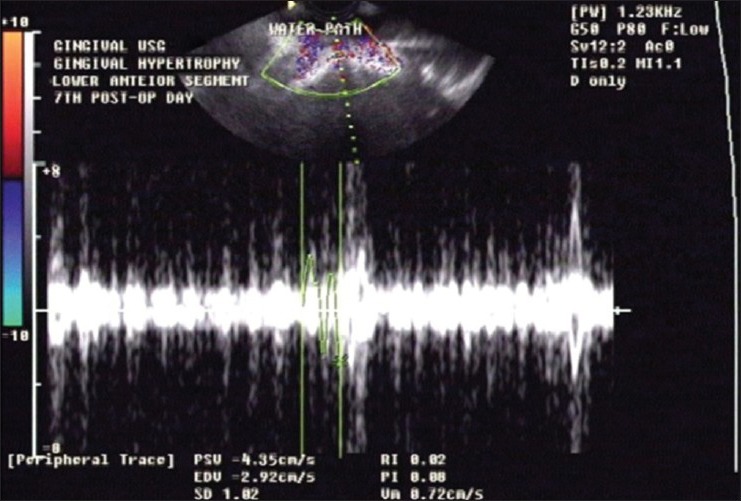
7th day post-operative spectral Doppler of lower anterior segment
Figure 10f.
30th day post-operative spectral Doppler of upper anterior segment
Figure 9b.

30th day post-operative view of lower anterior segment
Figure 9c.

7th day post-operative view of upper anterior segment
Figure 10b.
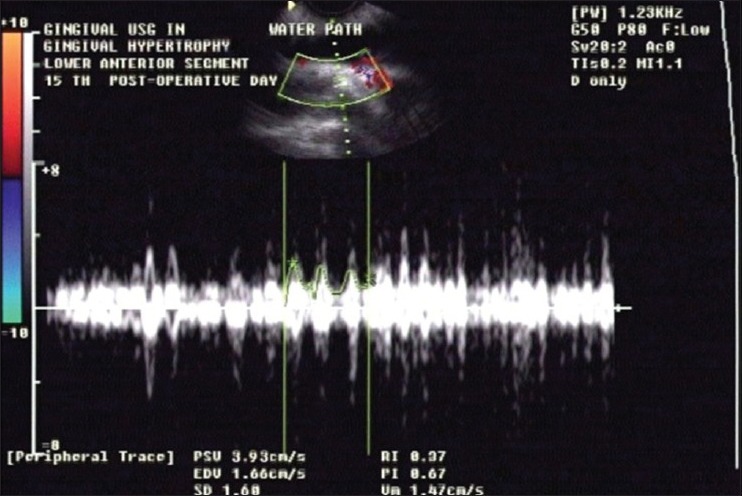
15th day post-operative spectral Doppler of lower anterior segment
Figure 10c.
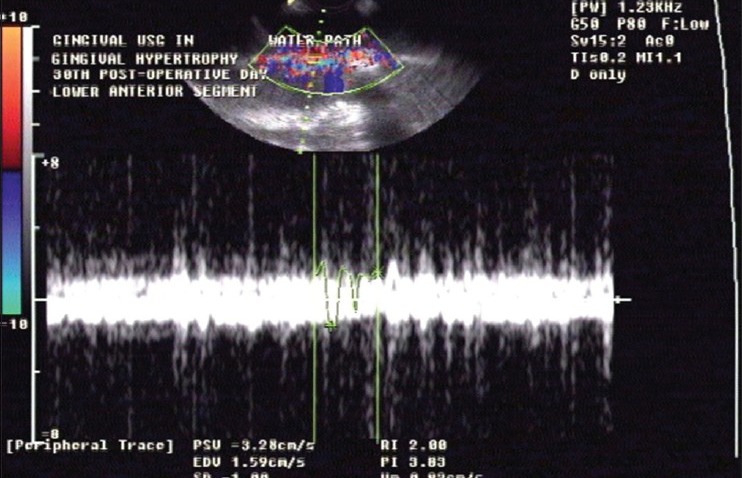
30th day post-operative spectral Doppler of lower anterior segment
Figure 10d.

7th day post-operative spectral Doppler of upper anterior segment
Figure 10e.
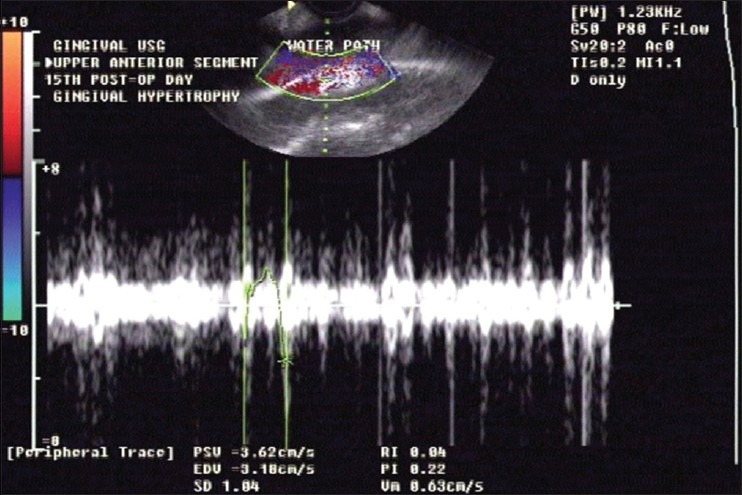
15th day post-operative spectral Doppler of upper anterior segment
Results
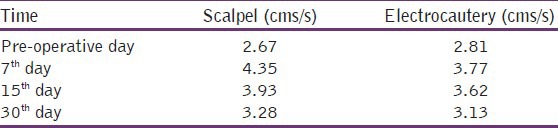
From the above table, it is shown that there was about 30% more blood flow by 7th day, 19% more blood flow by 15th day and 11% more blood flow by 30th day with scalpel technique when compared to that with the electrosurgery technique.
Table 1.
Data analysis of peak systolic velocity values
Discussion
Wound healing is influenced by revascularization rate, preservation and reconstruction of microvasculature. Revascularization of the wound area generally tends to follow the pattern of new connective tissue formation. The initial response after gingivoplasty and depigmentation is the formation of protective surface clot; the underlying tissues become acutely inflamed, with some necrosis. The clot is then replaced by granulation tissue. Capillaries derived from blood vessels of the periodontal ligament migrate into the granulation tissue and within 2 weeks, they connect with gingival vessels.[12] Vascularity increases initially, then begins to decrease gradually as healing takes place and returns to normal in about 2-3 weeks.[13] After 5-14 days surface epithelialization is generally complete, but complete epithelial repair takes about 1 month.[14]
In the present case report, soft-tissue USG with spectral Doppler facility was used to record the changes in GBF following gingivoplasty and depigmentation carried out by two different techniques i.e., scalpel and electrosurgery.
We have performed USG with 9-5 MHz capacity convex intracavitory transducer with color Doppler facility to determine the gingival vascularity. Color Doppler studies depict vascular areas by color coding. The flow pattern by spectral Doppler clearly indicates the velocity of venous blood flow to the region.
Doppler results in this case show comparatively decreased blood flow with electrosurgery especially by the 7th day, which could be a reason for delayed wound healing. Our results are in agreement with Almas and Sadig,[15] who reported that healing was faster with a scalpel than other techniques. The only disadvantage of the scalpel technique was unpleasant bleeding during and after the operation. Furthermore in a comparative study of electrosurgical and scalpel wounds carried out by Nixon et al., it was observed that healing of electrosurgical wounds were delayed.[16] If only the preceding reports are taken into account, then electrosurgery has no place in dentistry. There are as many reports[17,18,19] that have shown that there is no difference in the clinical healing of electrosurgery and scalpel wounds. The inconsistency of reports on healing of electrosurgical wounds may be attributed to the lack of standardization of factors such as power setting, cutting stroke, surface condition of the tissue, thickness and shape of the active electrodes and depth of incision.[20]
The advantages of scalpel technique include less amount of damage to adjacent tissue and comparatively faster wound healing. However, it is time consuming and allows more bleeding at the operative site. On the other end of the balance, the advantages of using electrosurgical procedures include.[20]
- Clean tissue separation, with little or no bleeding
- Clear view of the surgical site
- Planning of soft-tissue is possible
- Access to, difficult-to-reach areas is increased
- Chair time and operator fatigue are reduced
- The technique is pressure less and precise.
However, this technique has certain disadvantages,[20] such as:
- The initial cost of the equipment is far greater than the scalpel
- Odor of burning tissue is present if high volume suction is not used
- Although electrosurgical units are compatible with most modern pacemakers, it cannot be used on patients with older pacemakers that are not shielded against external interference
- It cannot be used near inflammable gases.
Conclusion
Before planning a surgery, the merits and demerits of both the techniques should be evaluated and a decision on which technique to follow should be taken, keeping both the surgeon's convenience and patient's comfort in view. Our results in this case have shown the use of a scalpel to be more advantageous over the use of electrosurgey as far as wound healing is concerned. The use of ultrasound Doppler flowmetry as a simple, non-invasive technique enabling direct and continuous observation of on-going changes and alterations in the blood flow has also been depicted.
Further longitudinal studies on larger samples are required to confirm the merits of scalpel over the use of electrocautery in minor oral surgical procedures.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Donos N, D’Aiuto F, Retzepi M, Tonetti M. Evaluation of gingival blood flow by the use of laser Doppler flowmetry following periodontal surgery. A pilot study. J Periodontal Res. 2005;40:129–37. doi: 10.1111/j.1600-0765.2005.00777.x. [DOI] [PubMed] [Google Scholar]
- 2.Staple PH, Copley AL. Observations on the microcirculation in the gingiva of hamsters and other laboratory animals. Circ Res. 1959;7:243–9. doi: 10.1161/01.res.7.2.243. [DOI] [PubMed] [Google Scholar]
- 3.Vandersall DC, Zander HA. Experimental obstruction of the periodontal blood circulation. Helv Odontol Acta. 1967;11:74–9. [PubMed] [Google Scholar]
- 4.Hock J, Nuki K, Schlenker R, Hawks A. Clearance rates of xenon-113 in non-inflamed and inflamed gingiva of dogs. Arch Oral Biol. 1980;25:445–9. doi: 10.1016/0003-9969(80)90050-3. [DOI] [PubMed] [Google Scholar]
- 5.Hock J, Nuki K. Erythrocyte velocity in vascular networks of young noninflamed dog gingiva. J Dent Res. 1976;55:1058–60. doi: 10.1177/00220345760550060801. [DOI] [PubMed] [Google Scholar]
- 6.Stern MD. In vivo evaluation of microcirculation by coherent light scattering. Nature. 1975;254:56–8. doi: 10.1038/254056a0. [DOI] [PubMed] [Google Scholar]
- 7.Rajaram PC, Naidu ME, Rao SP, Sindhuvenugopal M: Mode echomyography: A new technique for the functional assessment of striated muscles. Indian J Radiol Imaging. 2002;12:537–41. [Google Scholar]
- 8.Rekha M, Ananthanarayanan P, Manikandan R, Rajaram PC. M: Mode echomyography of tongue function during swallowing of saliva in cleft palate patients before and after surgery. J Maxillofac Oral Surg. 2005;4:27–9. [Google Scholar]
- 9.Rathan JJ, Vardhan BG, Muthu MS, Venkatachalapathy, Saraswathy K, Sivakumar N. Oral lymphangioma: A case report. J Indian Soc Pedod Prev Dent. 2005;23:185–9. doi: 10.4103/0970-4388.19007. [DOI] [PubMed] [Google Scholar]
- 10.Vardhan BG, Saraswathy K, Koteeswaran D. Primary hyperparathyroidism presenting as multiple giant cell lesions. Quintessence Int. 2007;38:e342–7. [PubMed] [Google Scholar]
- 11.Michael Mc Guire. Periodontal plastic surgery. Dent Clin North Am. 1998;42:416–8. [PubMed] [Google Scholar]
- 12.Watanabe Y, Suzuki S. An experimental study in capillary vascularization in the periodontal tissue following gingivectomy or flap operation. J Dent Res. 1963;42:758. [Google Scholar]
- 13.Goldman HM, Cohen WD. Periodontal therapy. 1980:689–93. [Google Scholar]
- 14.Stanton G, Levy M, Stahl SS. Collagen restoration in healing human gingiva. J Dent Res. 1969;48:27–31. doi: 10.1177/00220345690480011901. [DOI] [PubMed] [Google Scholar]
- 15.Almas K, Sadig W. Surgical treatment of melanin-pigmented gingiva; an esthetic approach. Indian J Dent Res. 2002;13:70–3. [PubMed] [Google Scholar]
- 16.Nixon KC, Adkins KF, Keys DW. Histological evaluation of effects produced in alveolar bone following gingival incision with an electrosurgical scalpel. J Periodontol. 1975;46:40–4. doi: 10.1902/jop.1975.46.1.40. [DOI] [PubMed] [Google Scholar]
- 17.Aremband D, Wade AB. A comparative wound healing study following gingivectomy by electrosurgery and knives. J Periodontal Res. 1973;8:42–50. doi: 10.1111/j.1600-0765.1973.tb00741.x. [DOI] [PubMed] [Google Scholar]
- 18.Schneider AR, Zaka AE. Gingival wound healing following experimental electrosurgery: An electron microscopic investigation. J Periodontol. 1974;45:685–94. doi: 10.1902/jop.1974.45.9.685. [DOI] [PubMed] [Google Scholar]
- 19.Rathofer SA, Gardner FM, Vermilyea SG. A comparison of healing and pain following excision of inflammatory papillary hyperplasia with electrosurgery and blade-loop knives in human patients. Oral Surg Oral Med Oral Pathol. 1985;59:130–5. doi: 10.1016/0030-4220(85)90003-9. [DOI] [PubMed] [Google Scholar]
- 20.Gnanasekhar JD, al-Duwairi YS. Electrosurgery in dentistry. Quintessence Int. 1998;29:649–54. [PubMed] [Google Scholar]