Adult orthostatic proteinuria (original) (raw)
Introduction
Orthostatic proteinuria is characterized by elevated levels of urinary protein excretion while in the upright or lordotic position and normal excretion when in the supine or recumbent position, such as that during bed rest. This type of proteinuria is the most frequent cause of isolated proteinuria in children and adolescents. In adolescents, the prevalence of orthostatic proteinuria is reported to be between 2 and 5% [1]. However, it is an uncommon disorder in individuals over 30 years of age [2]. As it is a benign condition requiring no further evaluation or specific therapy, the differential diagnosis of orthostatic proteinuria is crucial in clinical practice to avoid unnecessary interventions such as a kidney biopsy.
Case report
A 25-year-old woman was referred to our hospital because of recurrent proteinuria. When she was 13 years old, proteinuria was noted for the first time, and she was followed by her local outpatient clinic until the age of 22, as her proteinuria disappeared then. However, it reappeared when she was 25 years old, and thus, she was referred to our hospital. She had a past medical history of tonsillitis without gross hematuria. She was not on any medication and had no family history of proteinuria. Her height was 160 cm, body weight was 44 kg and body mass index (BMI) was 17.2 kg/m2. Clinical examination and renal ultrasound in the recumbent position were unremarkable. Her serum albumin level was 46 g/L, and her urinary protein level was 0.82 g/day, consisting mainly of albumin without hematuria or other abnormal findings in the urinary sediment, indicating the absence of active proliferative glomerular nephritis. To examine the cause of proteinuria, she was admitted to our hospital.
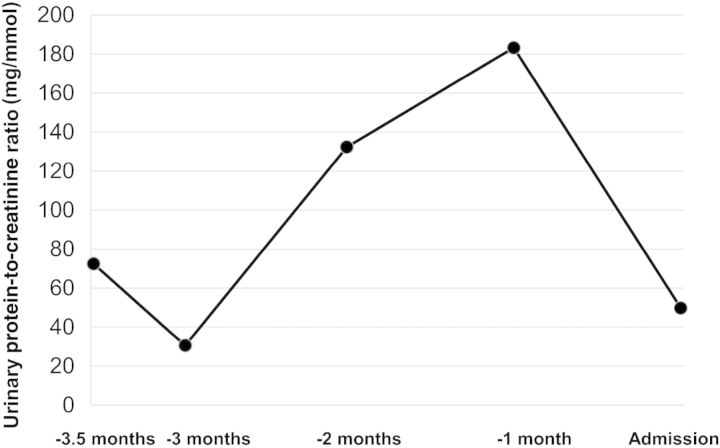
Initially, we planned to perform percutaneous needle biopsy of the kidney; however, her urinary protein-to-creatinine ratio fluctuated highly [30.5–183.3 mg/mmol (270–1620 mg/g)], and we thus considered the possibility of orthostatic proteinuria (Figure 1). To make a definite diagnosis of orthostatic proteinuria, the next morning, we collected a urine sample with the patient lying in the recumbent position after an extended period of rest and another sample immediately after assuming the lordotic position for 5 min. The ratio of urinary protein-to-urinary creatinine increased from 18.1 mg/mmol (160 mg/g) in the recumbent position to 575.8 mg/mmol (5090 mg/g) in the lordotic position, which is regarded as nephrotic-range proteinuria. On further assessment, we found completely bland urinary sediments and an absence of serum markers, such as autoantibodies, as well as hypocomplementemia. Based on the clinical course, laboratory data and the results of the urine samples collected in the recumbent and lordotic positions, we diagnosed orthostatic proteinuria. The patient was uneventfully discharged the next day and is currently being followed twice a year. At the latest visit, her urine protein-to-urinary creatinine ratio obtained in the recumbent position was <17.0 mg/mmol (150 mg/g), and her renal function was maintained.
Fig. 1.
Changes in urinary protein levels during the clinical course. The urinary protein levels (ratio of urinary protein-to-creatinine) fluctuated from 30.5 to 183.3 mg/mmol (270–1620 mg/g).
Discussion
Orthostatic proteinuria is characterized by elevated levels of urinary protein excretion while in the upright position and normal protein excretion when in the supine or recumbent position and is generally regarded as a benign condition [2, 3]. Therefore, we need to differentiate other glomerular diseases from orthostatic proteinuria to avoid unnecessary invasive interventions such as kidney biopsy. Furthermore, since orthostatic proteinuria might reflect an incipient glomerular disease, regular follow-up of the patients is required.
In the patient described here, completely bland urinary sediment and absence of serum markers, such as the presence of autoantibodies or hypocomplementemia, excluded a diagnosis of active proliferative glomerular disease. In addition, the large fluctuation of proteinuria from almost normal to the nephrotic range suggested a diagnosis of orthostatic proteinuria. By comparing the urinary protein excretion in both recumbent and lordotic positions, which are likely to be overlooked in our daily clinical practice, we were able to make the final and definitive diagnosis.
The mechanisms responsible for orthostatic proteinuria are currently not well understood. In addition to the normal variant, subtle glomerular abnormality and exaggerated hemodynamic response in the upright position as previously described, left renal vein entrapment has recently been shown to be related to orthostatic proteinuria [1, 4]. Milani et al. [5] showed that patients with lower BMI were more likely to show persistent orthostatic proteinuria than those with higher BMI, and they also pointed out that the space between the aorta and the superior mesenteric artery varies according to BMI. Our patient's renal ultrasound examination in the supine position was unremarkable; however, if her low BMI and elevated proteinuria after retaining a lordotic posture is considered, left renal vein entrapment in the upright position is a possibility.
Conclusion
When evaluating proteinuria with bland sediment, especially in young patients, urine samples collected in both recumbent and lordotic positions should be assessed to rule out orthostatic proteinuria and to avoid unnecessary evaluations and interventions.
Conflict of interest statement
None declared.
Acknowledgements
We thank Sayaka Shimizu, Minako Igarashi-Shimazaki and Masahito Miyamoto from our department for helping in patient care and management and Kenjiro Kimura for providing valuable clinical advice for this case.
References
- 1.Mazzoni MB, Kottanatu L, Simonetti GD, et al. Renal vein obstruction and orthostatic proteinuria: a review. Nephrol Dial Transplant. 2011;26:562–565. doi: 10.1093/ndt/gfq444. [DOI] [PubMed] [Google Scholar]
- 2.Springberg PD, Garrett LE, Jr, Thompson AL, Jr, et al. Fixed and reproducible orthostatic proteinuria: results of a 20-year follow-up study. Ann Intern Med. 1982;97:516–519. doi: 10.7326/0003-4819-97-4-516. [DOI] [PubMed] [Google Scholar]
- 3.Rytand DA, Spreiter S. Prognosis in postural (orthostatic) proteinuria: forty to fifty-year follow-up of six patients after diagnosis by Thomas Addis. N Engl J Med. 1981;305:618–621. doi: 10.1056/NEJM198109103051105. [DOI] [PubMed] [Google Scholar]
- 4.Shintaku N, Takahashi Y, Akaishi K, et al. Entrapment of left renal vein in children with orthostatic proteinuria. Pediatr Nephrol. 1990;4:324–327. doi: 10.1007/BF00862509. [DOI] [PubMed] [Google Scholar]
- 5.Milani G, Bianchetti MG, Bozzani S, et al. Body mass index modulates postural proteinuria. Int Urol Nephrol. 2010;42:513–515. doi: 10.1007/s11255-009-9550-0. [DOI] [PubMed] [Google Scholar]