Personality and Depressive Symptoms: Individual-Participant Meta-Analysis of 10 Cohort Studies (original) (raw)
. Author manuscript; available in PMC: 2016 Jul 1.
Published in final edited form as: Depress Anxiety. 2015 May 26;32(7):461–470. doi: 10.1002/da.22376
Abstract
Background
Personality is suggested to be a major risk factor for depression but large-scale individual-participant meta-analyses on this topic are lacking.
Method
Data from 10 prospective community cohort studies with a total of 117 899 participants (mean age 49.0 years; 54.7% women) were pooled for individual-participant meta-analysis to determine the association between personality traits of the Five Factor Model and risk of depressive symptoms.
Results
In cross-sectional analysis, low extraversion (pooled standardized regression coefficient (B)=-0.08; 95 % confidence interval=-0.11, -0.04), high neuroticism (B=0.39; 0.32, 0.45), and low conscientiousness (B=-0.09; -0.10, -0.06) were associated with depressive symptoms. Similar associations were observed in longitudinal analyses adjusted for baseline depressive symptoms (n=56,735; mean follow-up of 5.0 years): low extraversion (B=-0.03; -0.05, -0.01), high neuroticism (B=0.12; 0.10, 0.13), and low conscientiousness (B=-0.04; -0.06, -0.02) were associated with an increased risk of depressive symptoms at follow-up. In turn, depressive symptoms were associated with personality change in extraversion (B=-0.07; 95 % CI=-0.12, -0.02), neuroticism (B=0.23; 0.09, 0.36), agreeableness (B=-0.09; -0.15, -0.04), conscientiousness (B=-0.14; -0.21, -0.07), and openness to experience (B=-0.04; -0.08, 0.00).
Conclusions
Personality traits are prospectively associated with the development of depressive symptoms. Depressive symptoms, in turn, are associated with changes in personality that may be temporary or persistent.
Keywords: Depressive disorders, psychiatric epidemiology, depression risk, personality, publication bias, neuroticism, prospective studies
Depression is a highly prevalent and often long-term mental disorder reducing quality of life and causing increased health care costs, loss of productive working days and disability 1. Although the aetiology of depression is multifactorial, personality is among the important characteristics that have been hypothesized to predict depression. In addition, personality dysfunction has been associated with poor outcome of depression, increased risk of suicide, and extensive use of treatment 2, 3. Different personality traits have been associated with depressive disorders, e.g., major depressive disorder (MDD), and depressive symptoms 4-6, and at least six theoretical models (i.e., common cause, spectrum, vulnerability, precursor, pathoplasty, and scar) have been proposed to explain these associations 7-11. However, it has been argued that research in this field may be biased in favour of publishing positive results 12, 13. Thus, published evidence may have overestimated the strength of the personality-depression association. In addition, only few studies have taken into account reverse causation, that is, that depressive symptoms might also predict change in personality.
The largest meta-analytic review of published data to date included up to 14 563 patients and 60 576 controls and reported that individuals suffering from depressive disorders, i.e., MDD, unipolar depression, and dysthymic disorder, had higher levels of neuroticism and lower levels of both extraversion and conscientiousness when compared to healthy controls 5. A longitudinal association between high neuroticism and depressive symptoms or depression was observed in another recent meta-analysis that examined the relationship between neuroticism and depressive symptoms in prospective studies 6. However, other personality dimensions were not included in meta-analyses of prospective studies. In addition, the degree and direction of potential publication bias in the literature-based meta-analyses has not been examined 12, 14, 15. It has also been shown that depressive symptoms might predict change in personality 16. Recently, in a sample of 1739 Finnish men and women reciprocal relationship between negative emotionality, i.e., neuroticism, and depressive symptoms was found over 15 years of follow-up 17. However, it is not known whether these results can be generalized to other populations.
To address these limitations, we pooled unpublished data from 10 prospective cohort studies with 117 899 participants for an individual-participants meta-analysis to investigate the possible two-way relationship between personality traits of the Five-factor model of personality with depressive symptoms. The Five-factor model of personality includes five personality traits (extraversion, neuroticism, agreeableness, conscientiousness and openness to experience) and is currently the most widely used theory of personality 18. Based on previous findings 5,6, we hypothesized that low extraversion, high neuroticism and low conscientiousness may be associated with increased depressive symptoms. We also expected that the association between high neuroticism and depressive symptoms would be stronger than the associations between low extraversion and low conscientiousness with depressive symptoms. As age, gender, education, ethnicity, and marital status have also been linked to depressive symptoms 19, 20, we tested whether these factors might moderate the association between personality and depressive symptoms.
Materials and Methods
Data for the current study was selected by searching the data collections of the Inter-University Consortium for Political and Social Research (ICPSR; http://www.icpsr.umich.edu/icpsrweb/ICPSR/) and the Economic and Social Data Service (http://ukdataservice.ac.uk/) to identify eligible large-scale cohort studies that have repeated measurements of personality and depressive symptoms. Studies that included information on participant's personality assessed with at least the brief 15-item questionnaire or with more comprehensive questionnaires based on the Five Factor Model and depressive symptoms were eligible for the analysis.
Following cohorts studies were included in the present meta-analysis: the National Longitudinal Study of Adolescent Health (Add Health), the British Household Panel Survey (BHPS), the German Socio-Economic Panel Study (GSOEP), the Household, Income and Labour Dynamics in Australia (HILDA) Survey, the Health and Retirement Study (HRS), the Midlife in the United States (MIDUS), the National Child Development Study (NCDS), the Understanding Society (US), the Wisconsin Longitudinal Study graduate (WLSG) sample, and the Wisconsin Longitudinal Study sibling (WLSS) sample. All these studies are well-characterized longitudinal cohort studies with large sample sizes. Add Health and US did not have follow-up data on depressive symptoms after the assessment of personality, and thus these cohorts were included only in the cross-sectional analyses. The relevant local ethics committees approved all the included cohort studies. Full details of the cohorts and used measures can be found in the Online Supplementary Appendix.
Measurement of personality
The Five-Factor Model personality traits were assessed with standardized questionnaire instruments as follows: 20-item International Personality Item Pool measure was used in Add Health 21; 15-item version of the Big Five Inventory (BFI) was used in BHPS, GSOEP, and US 22, 23; 36-item inventory based on the Saucier's and Goldberg's Big Five Markers Scale was used in HILDA 24; 25-item questionnaire was used in HRS and MIDUS 25; 50-item International Personality Item Pool questionnaire in NCDS 26; and 29-item version of the BFI was used in WLSG and WLSS 22, 23. These instruments measure the following five higher-order personality traits that sum up individual variation in personality dispositions: extraversion (e.g., sociability and sensitivity to positive emotions), neuroticism (e.g., low emotional stability and proneness to anxiety), agreeableness (e.g., cooperativeness and trust toward other people), conscientiousness (e.g., self-control and allegiance to social norms), and openness to experience (e.g., curiosity and open-mindedness).
Measurement of depressive symptoms
Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CES-D) 27 in AddHealth, HRS, WLSG, and WLSS; General Health Questionnaire (GHQ) 28 in BHPS and US; Mental Component Summary Scale (MCS) 29 in GSOEP; Mental Health Inventory (MHI), a subscale from the SF-36 general health survey, in HILDA; the World Mental Health Organization's Composite International Diagnostic Interview Short Form (CIDI-SF) 30 in MIDUS; and Malaise Inventory in NCDS 31.
Statistical analysis
Cross-sectional associations between the personality traits and depressive symptoms in the total sample and within different subgroups were examined using linear regression analysis and partial correlation adjusting for sex, age at baseline, and ethnicity/nationality (0 = majority, i.e. in most cohort non-Hispanic Caucasians; 1 = other). Personality scores and depressive symptoms were standardized (standard deviation (SD) = 1). Longitudinal associations between the personality traits and depressive symptoms were analysed in two separate ways. First, the association between the personality traits at baseline and depressive symptoms at follow-up was examined adjusting for depressive symptoms at baseline plus sex, age at baseline, ethnicity/nationality and the length of follow-up period in months. Second, to examine reverse causality, i.e., the hypothesis that depressive symptoms predict change in personality, the association between baseline depressive symptoms and personality at follow-up was examined adjusting the models for baseline personality trait, sex, age at baseline, ethnicity/nationality and the length of follow-up in months. To facilitate interpretation of effect sizes in the personality change analysis, personality traits were first transformed into T-scores (Mean=50, standard deviation=10) before analysis using means and standard deviations at Time 1 as the metric against which to standardize scores at both Time 1 and Time 2.
In the main analyses, two-step individual participant meta-analysis was used 32. All models were first fitted separately within each cohort, and the results from the individual cohorts were then pooled by using random-effects meta-analysis. Standard errors in cohorts based on household sampling were calculated by using a robust estimator method to take into account the non-independence of individuals from the same households. Heterogeneity in the effect sizes was examined using the I2 estimates. To examine potential sources of heterogeneity 33, additional sensitivity analyses were carried out using one-step individual participant meta-analysis where data were first pooled and models then fitted taking into account the clustering of observations within each study. Meta-analysis was performed with the metan package of Stata, version 13.1, software (StataCorp LP, College Station, Texas).
Results
The sample characteristics are shown in Table 1. A total of 117 899 participants (age range 15-104; mean age 49.0 years; 54.7% women) were included in the meta-analysis.
Table 1.
Descriptive characteristics of the participants by cohort study.
| Add Health | BHPS | GSOEP | HILDA | HRS | MIDUS | NCDS | US | WLSg | WLSs | |
|---|---|---|---|---|---|---|---|---|---|---|
| N of participants | ||||||||||
| Cross-sectional analysis | 5,025 | 13,626 | 18,303 | 11,046 | 13,614 | 6,259 | 8,608 | 30,877 | 6,612 | 3,929 |
| Longitudinal analysis | - | 10,585 | 12,679 | 8,462 | 12,195 | 4,634 | - | - | 5,214 | 2,966 |
| Age | 29.0 (1.8) | 45.4 (18.3) | 47.3 (17.3) | 43.8 (17.9) | 67.2 (10.4) | 46.8 (12.9) | 47.2 (17.9) | 50.3 (0.5) | 54.1 (0.5) | 53.1 (7.3) |
| Sex | ||||||||||
| Men | 45.9 (2,309) | 45.4 (6,282) | 47.9 (9,790) | 46.7 (5,182) | 40.8 (5,669) | 47.5 (2,971) | 48.1 (4,141) | 43.8 (13,532) | 46.2 (3,083) | 46.5 (1,847) |
| Women | 54.1 (2,717) | 54.6 (7,541) | 52.1 (10,644) | 53.3 (5,909) | 59.2 (8,231) | 52.5 (3,288) | 51.9 (4,467) | 56.2 (17,386) | 53.8 (3,591) | 53.5 (2,122) |
| Education | ||||||||||
| Primary | 33.6 (1,687) | 27.8 (3,788) | 16.1 (2,787) | 34.6 (3,825) | 18.2 (2,481) | 8.7 (545) | 18.1 (1,557) | 42.6 (13,009) | 72.1 (4,769) | 5.2 (204) |
| Secondary | 53.5 (2,686) | 57.7 (7,861) | 61.3 (10,636) | 44.3 (4,894) | 55.3 (7,524) | 59.3 (3,704) | 61.7 (5,308) | 20.2 (6,177) | 27.9 (1,843) | 64.2 (2,521) |
| Tertiary | 13.0 (652) | 14.5 (1,972) | 22.6 (3,927) | 21.1 (2,327) | 26.4 (3,594) | 32.0 (1,997) | 20.3 (1,743) | 37.2 (11,357) | - | 30.6 (1,204) |
| Nationality / ethnicity | ||||||||||
| Majority | 71.8 (3,609) | 85.5 (11,644) | 93.1 (17,045) | 79.2 (8,751) | 78.1 (10,631) | 88.9 (5,567) | 98.0 (8,437) | 83.1 (25,674) | 100.0 (6,612) | 100.0 (3,929) |
| Minority | 28.2 (1,416) | 14.5 (1,982) | 6.9 (1,258) | 20.8 (2,295) | 21.9 (2,983) | 11.1 (692) | 2.0 (171) | 16.9 (5,203) | - | - |
| Marital status | ||||||||||
| Married/cohabiting | 41.6 (2,092) | 52.0 (7,081) | 60.1 (11,009) | 59.3 (6,551) | 63.7 (8,675) | 67.7 (4,234) | 70.0 (6,028) | 63.3 (19,531) | 83.3 (5,504) | 80.9 (3,151) |
| Single | 58.4 (2,933) | 48.0 (6,540) | 39.9 (7,294) | 40.7 (4,495) | 36.3 (4,936) | 32.3 (2,022) | 30.0 (2,580) | 36.7 (11,345) | 16.7 (1,107) | 19.1 (744) |
| Follow-up time (months) | - | 36.1 (1.3) | 48.1 (1.6) | 48.0 (1.3) | 35.6 (15.9) | 107.5 (6.3) | - | - | 134.0 (4.2) | 135.9 (6.7) |
| Baseline depressive symptoms | 2.6 (2.5) | 11.3 (5.5) | 11.4 (3.6) | 25.8 (16.8) | 1.4 (1.9) | 0.7 (1.9) | 3.4 (4.5) | 11.1 (5.5) | 17.3 (6.0) | 17.4 (6.3) |
| Follow-up depressive symptoms | - | 11.5 (5.6) | 11.5 (3.5) | 24.8 (16.7) | 1.4 (1.9) | 0.6 (1.7) | - | - | 16.5 (5.6) | 16.8 (5.9) |
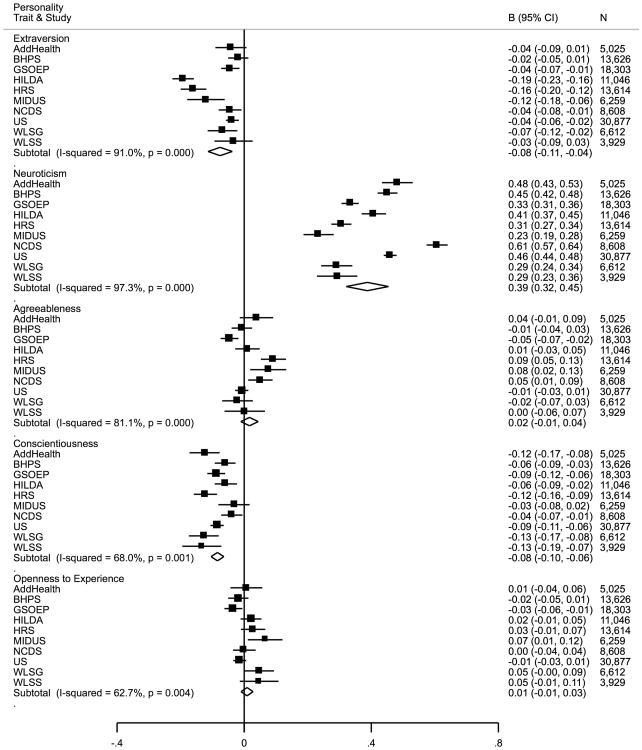
Cross-sectional associations between personality traits and depressive symptoms are presented in Figure 1. Low extraversion (pooled B=-0.08; 95 % CI=-0.11, -0.04) and high neuroticism (pooled B=0.39; 95 % CI=0.32, 0.45) were associated with depressive symptoms. In addition, low conscientiousness was associated with depressive symptoms (pooled B=-0.08; 95 % CI=-0.10, -0.06). However, there was heterogeneity across studies (extraversion and depressive symptoms: I2=91 %, p<.001; neuroticism and depressive symptoms: I2=97 %, p<.001; conscientiousness and depressive symptoms: I2=68 %, p<.01). Subgroup analyses according to sex, age, education, marital status, and ethnicity/nationality are reported in eTable 1. Low openness to experience was associated with depressive symptoms among individuals from ethnical or national minorities (pooled B=-0.03; 95 % CI=-0.06, 0.00), but not among individual from ethnic or national majorities (pooled B=0.01; 95 % CI=-0.02, 0.03). There were no other significant differences in associations between any of the sub-groups (p > .05). Additional sensitivity analyses with multilevel regression showed that the covariates (i.e., age, sex, race/ethnicity, marital status, and education) reduced the observed heterogeneity only marginally, that is, by 5.0% in extraversion and 3.4% in neuroticism (eTable 2).
Figure 1.
Cross-sectional associations between Five-Factor Model personality traits and depressive symptoms. Values are regression coefficients (and 95% confidence intervals) per 1 standard deviation increment in personality trait. Personality traits are adjusted for each other in addition to sex, age and race/ethnicity. Add Health, National Longitudinal Study of Adolescent Health; BHPS, British Household Panel Survey; GSOEP, German Socio-Economic Panel Study; HILDA, Household, Income and Labour Dynamics in Australia; HRS, Health and Retirement Study; MIDUS, Midlife in the United States; NCDS, National Child Development Study; US, Understanding Society; WLSG, Wisconsin Longitudinal Study Graduate Sample; WLSS, Wisconsin Longitudinal Study Sibling Sample.
Mean follow-up period across cohort studies with two depression measurement points was 5.0 years (n=56,735). The test-retest partial correlation (adjusted for age, sex, and race) of depressive symptoms was 0.41, and the equivalent test-retest correlation of personality traits was as follows: extraversion: r=0.69; neuroticism: r=0.61; agreeableness: r=0.57; conscientiousness: r=0.59; and openness to experience: r=0.66.
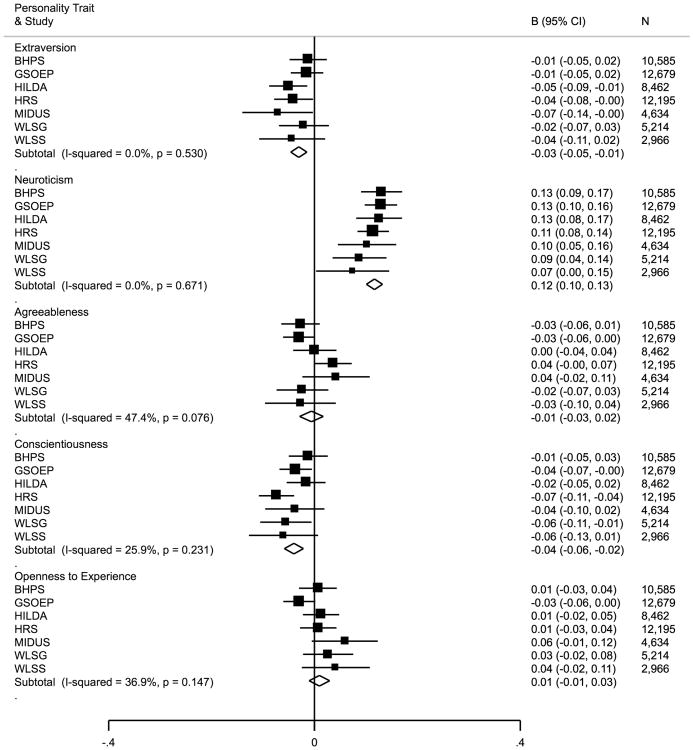
Longitudinal associations between personality at baseline and depressive symptoms at follow-up, adjusted for depressive symptoms at baseline, are shown in Figure 2. Again, low extraversion was associated with increased depressive symptoms (pooled B=-0.03; 95 % CI=-0.05, -0.01) and high neuroticism was positively associated with depressive symptoms (pooled B=0.12; 95 % CI=0.10, 0.13). In addition, low conscientiousness was associated with increased depressive symptoms (pooled B=-0.04; 95 % CI=-0.06, -0.02). There was no significant heterogeneity in study-specific estimates in the longitudinal analysis.
Figure 2.
Longitudinal associations between Five-Factor Model personality traits and depressive symptoms adjusted for baseline depressive symptoms. Values are regression coefficients (and 95% confidence intervals) per 1 standard deviation increment in personality trait. Personality traits are also adjusted for each other in addition to sex, age and race/ethnicity. Add Health, National Longitudinal Study of Adolescent Health; BHPS, British Household Panel Survey; GSOEP, German Socio-Economic Panel Study; HILDA, Household, Income and Labour Dynamics in Australia; HRS, Health and Retirement Study; MIDUS, Midlife in the United States; WLSG, Wisconsin Longitudinal Study Graduate Sample; WLSS, Wisconsin Longitudinal Study Sibling Sample.
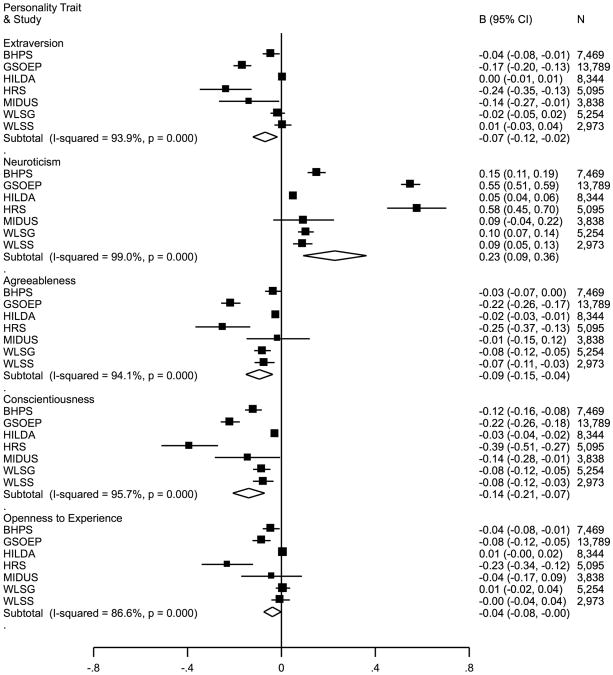
Test of reverse causality, that is, baseline depressive symptoms predicting change in personality traits are shown in Figure 3. Depressive symptoms were associated with lower subsequent extraversion (pooled B=-0.07; 95 % CI=-0.12, -0.02), higher neuroticism (pooled B=0.23; 95 % CI=0.09, 0.36), and lower scores of agreeableness (pooled B=-0.09; 95 % CI=-0.15, -0.04), conscientiousness (pooled B=-0.14; 95 % CI=-0.21, -0.07), and openness to experience (pooled B=-0.04; 95 % CI=-0.08, 0.00). However, there was considerable heterogeneity in these associations across studies (extraversion: I2=94%, p<0.001; neuroticism: I2=99%, p<0.001; agreeableness: I2=94%, p<0.001; conscientiousness: I2=96%, p<0.001; openness to experience: I2=87%, p<0.001).
Figure 3.
Associations between depressive symptoms and personality change between baseline and follow-up. Analyses are adjusted for sex, age, race, and follow-up time. Values are regression coefficients (and 95% confidence intervals) indicating linear change in personality traits T-score. Add Health, National Longitudinal Study of Adolescent Health; BHPS, British Household Panel Survey; GSOEP, German Socio-Economic Panel Study; HILDA, Household, Income and Labour Dynamics in Australia; HRS, Health and Retirement Study; MIDUS, Midlife in the United States; WLSG, Wisconsin Longitudinal Study Graduate Sample; WLSS, Wisconsin Longitudinal Study Sibling Sample.
Discussion
This study examined the association between personality traits and depressive symptoms using individual-participant-meta-analysis of unpublished open-access data. Over 115 000 participants were included in the cross-sectional analysis and over 55 000 participants in the longitudinal analysis. Low extraversion, high neuroticism, and low conscientiousness were associated with depressive symptoms in both cross-sectional and longitudinal analysis. There was no evidence of heterogeneity in study-specific estimates of the longitudinal associations. However, we found some evidence that the association between personality and depressive symptoms might be bi-directional. The analysis of reverse causation showed that depressive symptoms predicted higher neuroticism and lower extraversion, agreeableness and conscientiousness at baseline although there was significant heterogeneity in study-specific estimates of these associations.
This is the largest meta-analysis of multiple personality traits and depressive symptoms to date 5, and the first based on a prospective study design. These results are in line with previous findings, which have shown that low extraversion, high neuroticism and low conscientiousness are associated with depression 4, 5. However, the effect sizes in the current study were considerable lower in both cross-sectional and longitudinal analyses than in the earlier literature-based meta-analyses. In the literature-based meta-analysis of Kotov and co-workers 3, the correlations with major depressive disorder were 0.47 for neuroticism, -0.25 for extraversion, and -0.36 for conscientiousness. In the current study, the corresponding partial correlations (adjusted for age, sex, race and other personality traits) were 0.37, -0.07, and -0.09. Thus, the present associations of neuroticism, extraversion, and conscientiousness were 21%, 72%, and 75% smaller compared to the literature meta-analysis. A corresponding discrepancy was found in the longitudinal analysis where the effect size between neuroticism and depressive symptoms was two thirds lower when compared to cross-sectional analysis, whereas the previous literature-based meta-analysis reported that the effect size was about half lower in the longitudinal versus the cross-sectional analyses 6. The reasons for these differences are not known, however, it is possible that publication bias may have contributed to the higher effect estimates in previous meta-analyses based on published data. In addition, methodological differences may be a contributing factor for the relatively high attenuation in the associations of extraversion and conscientiousness with depressive symptoms because the current study analyses were adjusted for neuroticism while this adjustment was missing in previous meta-analyses.
We found evidence of reverse causation because depressive symptoms predicted change in all personality traits. The largest effect was found in increase of neuroticism, which was equal to the effect size of a previous study showing effects sizes of single chronic diseases associated with changes in neuroticism 34, and moderate or small effects in decrease of extraversion, agreeableness and conscientiousness. There are relatively few prior studies that have examined the association between depressive symptoms and personality change using large prospective samples. Although there are some findings showing that depression is associated with personality change 16, 17, 35, supporting the hypothesis that depression causes ‘a scar’ in personality, other studies have failed to support this 36, 37. However, it has been argued that the possible scarring effect of depression should be examined using continuous depressive symptoms scores rather than depression diagnosis to capture the interplay between depression and personality, especially neuroticism 38. Although, based on our results, it might be an overestimation to say that depressive symptoms cause persistent scars in personality, our findings clearly indicate that there is a bidirectional relationship between depressive symptoms and neuroticism. However, considerably heterogeneity across studies indicates that there are some other factors that play a role also in this reciprocal relationship.
There are at least six alternative and partially overlapping theoretical models (i.e., common cause, spectrum, vulnerability, precursor, pathoplasty, and scar/complication) that have been proposed to explain the personality-depression association, and all these models have been supported to some degree 7-11. The common cause model posits that common determinants, for example genetic factors, explain the association between personality and depression; the finding that neuroticism and depressive symptoms share a large genetic background is consistent with this possibility 39. The spectrum model postulates that high neuroticism and depressive symptoms are different manifestations of the same underlying processes. This model implies that depression is defined by symptoms as well as personality style and is discussed in particularly in relation to atypical depression 40. According to the vulnerability model, personality represents a risk or contributing factor for the depression onset (e.g., high neuroticism either causes depression or enhances the impact of other depression risk factors such as stressful live events 41, 42). In the pathoplasty model, personality does not directly cause depression, but once depression has developed, personality influences the severity of pattern of symptoms 43, 44. Finally, whereas the scar model suggests that depression causes persistent personality change, the complication model suggests that this change is likely to be only temporary 45.
Although the aim of the current study was not to compare these models, the results suggest that certain explanations may be more plausible than others. The findings that neuroticism was cross-sectionally and prospectively associated with depressive symptoms and that neuroticism was slightly more stable than depressive symptoms, are consistent with both the common cause and vulnerability models. In addition, the association between depressive symptoms and future personality change supports both the scar and complication models. These findings are partially in agreement with previous studies suggesting that common cause, spectrum, and vulnerability models best explain the association between neuroticism and depression 6. Future studies should examine in more detail these issues and in particularly whether the changes observed in personality dispositions are temporary or persistent.
Some evidence suggests that personality predicts recurrent depressive episodes 46, 47. Although we were able to demonstrate an association between depression and a change in personality dispositions, we did not have data to determine those related to the first depressive episode or recurrent depression and whether the association with personality would differ between the two. Thus, the possibility that the role of personality is bigger in recurrent depression than in single depressive episodes should be further examined in future studies with more than two waves of personality and depressive symptoms measures.
Considerable heterogeneity was observed in the associations between personality and depressive symptoms, and this heterogeneity was not explained by the covariates available. Future studies should examine biological and socio-cultural factors, which were unmeasured or measured imprecisely in the present study, to identify the source of heterogeneity across the studies. The etiology of depression is multifactorial, including genetic, epigenetic, biological, behavioral and environmental factors, so personality should be considered only as one of the factors contributing to depression risk. Also, personality may be differently related to different subtypes of depression, such as atypical or melancholic depression, which could not be examined in the present study.
It has been consistently found that prevalence of depressive symptoms is higher among women than men 48, 49, and there is some evidence that neuroticism might be stronger predictor of depression in women than men 50. However, our results did not find any differences between women and men in the association of neuroticism and depressive symptoms.
Although neuroticism has been hypothesized to be an important predictor of physical diseases 51, recent studies with larger sample sizes have shown that low conscientiousness may be the only personality trait that is consistently associated with chronic diseases and risk factors such as obesity 52, diabetes 53, and coronary heart disease and stroke 54, and all-cause mortality 55. Whether depression is a mediating factor between neuroticism and physical disease should be investigated in future studies.
The clinical utility of the five-factor model has been challenged by some studies 56, but other studies suggest that the five-factor model has prognostic value and is useful in defining normal and abnormal personality functioning 57. For example, interventions for alcohol and drug misuse may be more effective when targeted at individuals with certain personality dispositions, at least in adolescents 58. Thus, information on personality may contribute to optimal allocation of prevention and treatment resources. In future studies, it would be worth considering also targeting individuals who are in high-risk depression group due to their personality. This could be especially important because it has been estimated that the costs of neuroticism are larger than the costs of common mental disorders 59. It would also be important to start planning interventions that focus more on the roots of neuroticism rather than the outcomes of it.
Study limitations
This study has some limitations. First, due to nature of the included studies, i.e., large epidemiological community studies, personality was measured with relatively short questionnaires, which reduces the reliability of the used personality measures. However, it has been demonstrated that short questionnaires work adequately well 60, and thus their use can be justified. In addition, depressive symptoms were measured with a number of different instruments from which some are specific measures of depressive symptoms such as CES-D, whereas others such as GHQ are general measures of mental health. This can naturally create measurement error and thus bias in the study results. However, the study results were rather consistent, which inclines that measurement error was not a significant source of bias. Study participants were mostly adults with mean age of 49 years, which indicates that current results might not be generalizable to younger participants. For example, the levels of both depressive symptoms and neuroticism have been to shown to vary across life-span 61, 62, which creates the possibility that the relationship between personality and depressive symptoms might differ across life course. This is something that further studies should investigate in detail.
Conclusion
In conclusion, results from the current individual-participant study with 117 899 participants demonstrate that personality traits extraversion, neuroticism, and conscientiousness are associated with depressive symptoms. In turn, depressive symptoms are associated with future personality change that could be a temporary or persistent. Further research is needed to determine whether personality should be taken into account when designing future preventions and interventions targeting to reduce the burden of depression.
Supplementary Material
1
Acknowledgments
M.K. is supported by the UK Medical Research Council (K013351), the Economic and Social Research Council, and the National Institutes of Health, US (R01HL036310, R01AG034454). M.E. is supported by the Academy of Finland (265977). M.V. is supported by Academy of Finland (258598, 265174). L.P. is supported by the Juho Vainio Foundation.
Footnotes
Declarations of interest: None.
Contributor Information
Christian Hakulinen, Institute of Behavioural Sciences, University of Helsinki, Finland.
Marko Elovainio, Institute of Behavioural Sciences, University of Helsinki, Finland; National Institute for Health and Welfare, Helsinki, Finland.
Laura Pulkki-Råback, Helsinki Collegium for Advanced Studies, University of Helsinki, Finland; Institute of Behavioural Sciences, University of Helsinki, Finland.
Marianna Virtanen, Finnish Institute of Occupational Health, Finland.
Mika Kivimäki, Department of Epidemiology and Public Health, University College London, UK; Department of Public Health, Faculty of Medicine, University of Helsinki, Finland.
Markus Jokela, Institute of Behavioural Sciences, University of Helsinki, Finland.
References
- 1.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2013;380:2163–96. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newton-Howes G, Tyrer P, Johnson T, et al. Influence of Personality on the Outcome of Treatment in Depression: Systematic Review and Meta-Analysis. J Personal Disord. 2014;4:577–93. doi: 10.1521/pedi_2013_27_070. [DOI] [PubMed] [Google Scholar]
- 3.Leichsenring F, Leibing E, Kruse J, et al. Borderline personality disorder. The Lancet. 2011;377:74–84. doi: 10.1016/S0140-6736(10)61422-5. [DOI] [PubMed] [Google Scholar]
- 4.Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. J Abnorm Psychol. 1994;103:103–16. [PubMed] [Google Scholar]
- 5.Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychol Bull. 2010;136:768. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- 6.Ormel J, Jeronimus BF, Kotov R, et al. Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clin Psychol Rev. 2013;33:686–97. doi: 10.1016/j.cpr.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watson D, Clark LA. Depression and the melancholic temperament. European Journal of Personality. 1995;9:351–66. [Google Scholar]
- 8.Clark LA. Temperament as a Unifying Basis for Personality and Psychopathology. J Abnorm Psychol. 2005;114:505–21. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- 9.Krueger RF, Tackett JL. Personality and psychopathology: Working toward the bigger picture. J Personal Disord. 2003;17:109–28. doi: 10.1521/pedi.17.2.109.23986. [DOI] [PubMed] [Google Scholar]
- 10.Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Annu Rev Clin Psychol. 2011;7:269–95. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enns MW, Cox BJ. Personality dimensions and depression: review and commentary. Canadian Journal of Psychiatry. 1997;42:274–84. doi: 10.1177/070674379704200305. [DOI] [PubMed] [Google Scholar]
- 12.Fanelli D. “Positive” results increase down the hierarchy of the sciences. PloS one. 2010;5:e10068. doi: 10.1371/journal.pone.0010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferguson CJ, Heene M. A vast graveyard of undead theories publication bias and psychological science's aversion to the null. Perspectives on Psychological Science. 2012;7:555–61. doi: 10.1177/1745691612459059. [DOI] [PubMed] [Google Scholar]
- 14.Ioannidis JP. Why most published research findings are false. PLoS medicine. 2005;2:e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munafo MR, Flint J. How reliable are scientific studies? Br J Psychiatry. 2010;197:257–8. doi: 10.1192/bjp.bp.109.069849. [DOI] [PubMed] [Google Scholar]
- 16.Kendler KS, Neale MC, Kessler RC, et al. A longitudinal twin study of personality and major depression in women. Arch Gen Psychiatry. 1993;50:853–62. doi: 10.1001/archpsyc.1993.01820230023002. [DOI] [PubMed] [Google Scholar]
- 17.Elovainio M, Jokela M, Rosenström T, et al. Temperament and depressive symptoms: What is the direction of the association? J Affect Disord. 2015;170:203–12. doi: 10.1016/j.jad.2014.08.040. [DOI] [PubMed] [Google Scholar]
- 18.Digman JM. Personality structure: Emergence of the five-factor model. Annu Rev Psychol. 1990;41:417–40. [Google Scholar]
- 19.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–38. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riolo SA, Nguyen TA, Greden JF, King CA. Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. Am J Public Health. 2005;95:998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnellan MB, Oswald FL, Baird BM, Lucas RE. The mini-IPIP scales: tiny-yet-effective measures of the Big Five factors of personality. Psychol Assess. 2006;18:192–203. doi: 10.1037/1040-3590.18.2.192. [DOI] [PubMed] [Google Scholar]
- 22.John OP, Donahue EM, Kentle RL. The “Big Five” inventory – version 4a and 5a. 1991 [Google Scholar]
- 23.John OP, Naumann LP, Soto CJ. Paradigm shift to the integrative big-five trait taxonomy: History, measurement, and conceptual issues. In: John OP, Robins RW, Pervin LA, editors. Handbook of Personality: Theory and Research. Guilford Press; 2008. pp. 114–158. [Google Scholar]
- 24.Saucier G. Mini-markers: A brief version of Goldberg's unipolar Big-Five markers. J Pers Assess. 1994;63:506–16. doi: 10.1207/s15327752jpa6303_8. [DOI] [PubMed] [Google Scholar]
- 25.Lachman ME, Weaver SL. The Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. Waltham, MA: Brandeis University; 1997. [Google Scholar]
- 26.Goldberg LR. A broad-bandwidth, public domain, personality inventory measuring the lower-level facets of several five-factor models. Personality psychology in Europe. 1999;7:7–28. [Google Scholar]
- 27.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1:385–401. [Google Scholar]
- 28.Goldberg DP. The detection of psychiatric illness by questionnaire: A technique for the identification and assessment of non-psychotic psychiatric illness. 1972 [Google Scholar]
- 29.Ware JE, Kosinski M. SF-36 physical & mental health summary scales: a manual for users of version 1. Quality Metric Inc; 2001. [Google Scholar]
- 30.Kessler RC, Andrews G, Mroczek D, et al. The World Health Organization Composite International Diagnostic Interview Short–Form (CIDI–SF) International journal of methods in psychiatric research. 1998;7:171–85. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodgers B, Pickles A, Power C, et al. Validity of the Malaise Inventory in general population samples. Soc Psychiatry Psychiatr Epidemiol. 1999;34:333–41. doi: 10.1007/s001270050153. [DOI] [PubMed] [Google Scholar]
- 32.Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ British Medical Journal. 2010:521–5. doi: 10.1136/bmj.c221. [DOI] [PubMed] [Google Scholar]
- 33.Teramukai S, Matsuyama Y, Mizuno S, Sakamoto J. Individual patient-level and study-level meta-analysis for investigating modifiers of treatment effect. Jpn J Clin Oncol. 2004;34:717–21. doi: 10.1093/jjco/hyh138. [DOI] [PubMed] [Google Scholar]
- 34.Jokela M, Hakulinen C, Singh-Manoux A, Kivimäki M. Personality change associated with chronic diseases: pooled analysis of four prospective cohort studies. Psychol Med. 2014:1–12. doi: 10.1017/S0033291714000257. [DOI] [PubMed] [Google Scholar]
- 35.Rosenström T, Jylhä P, Pulkki-Råback L, et al. Long-term personality changes and predictive adaptive responses after depressive episodes. Evolution and Human Behavior. 2015 [Google Scholar]
- 36.Shea MT, Leon AC, Mueller TI, et al. Does major depression result in lasting personality change? Am J Psychiatry. 1996 doi: 10.1176/ajp.153.11.1404. [DOI] [PubMed] [Google Scholar]
- 37.Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode: a 3-wave population-based study. Arch Gen Psychiatry. 2004;61:990–6. doi: 10.1001/archpsyc.61.10.990. [DOI] [PubMed] [Google Scholar]
- 38.Wichers M, Geschwind N, van Os J, Peeters F. Scars in depression: is a conceptual shift necessary to solve the puzzle? Psychol Med. 2010;40:359. doi: 10.1017/s0033291709990420. [DOI] [PubMed] [Google Scholar]
- 39.Kendler KS, Gatz M, Gardner CO, Pedersen NL. Personality and major depression: a Swedish longitudinal, population-based twin study. Arch Gen Psychiatry. 2006;63:1113–20. doi: 10.1001/archpsyc.63.10.1113. [DOI] [PubMed] [Google Scholar]
- 40.Parker GB, Crawford J. A spectrum model for depressive conditions: extrapolation of the atypical depression prototype. J Affect Disord. 2007;103:155–63. doi: 10.1016/j.jad.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 41.Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry. 2004;161:631–6. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- 42.Vinkers CH, Joëls M, Milaneschi Y, et al. Stress exposure across the life span cumulatively increases depression risk and is moderated by neuroticism. Depress Anxiety. 2014;31:737–45. doi: 10.1002/da.22262. [DOI] [PubMed] [Google Scholar]
- 43.Morris BH, Bylsma LM, Rottenberg J. Does emotion predict the course of major depressive disorder? A review of prospective studies. British Journal of Clinical Psychology. 2009;48:255–73. doi: 10.1348/014466508X396549. [DOI] [PubMed] [Google Scholar]
- 44.Wilson S, DiRago A, Iacono W. Prospective inter-relationships between late adolescent personality and major depressive disorder in early adulthood. Psychol Med. 2014;44:567–77. doi: 10.1017/S0033291713001104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karsten J, Penninx BW, Riese H, et al. The state effect of depressive and anxiety disorders on big five personality traits. J Psychiatr Res. 2012;46:644–50. doi: 10.1016/j.jpsychires.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 46.Durbin CE, Hicks BM. Personality and psychopathology: A stagnant field in need of development. European Journal of Personality. 2014;28:362–86. doi: 10.1002/per.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rosenström T, Jylhä P, Robert Cloninger C, et al. Temperament and character traits predict future burden of depression. J Affect Disord. 2014;158:139–47. doi: 10.1016/j.jad.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 48.Weissman MM, Bland RC, Canino GJ, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–9. [PubMed] [Google Scholar]
- 49.Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC medicine. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kendler KS, Gardner CO. Sex Differences in the Pathways to Major Depression: A Study of Opposite-Sex Twin Pairs. Am J Psychiatry. 2014 doi: 10.1176/appi.ajp.2013.13101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lahey BB. Public health significance of neuroticism. Am Psychol. 2009;64:241. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jokela M, Hintsanen M, Hakulinen C, et al. Association of personality with the development and persistence of obesity: a meta–analysis based on individual–participant data. Obesity Reviews. 2013;14:315–23. doi: 10.1111/obr.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jokela M, Elovainio M, Nyberg ST, et al. Personality and Risk of Diabetes in Adults: Pooled Analysis of 5 Cohort Studies. Health Psychology. 2014;33:1618–21. doi: 10.1037/hea0000003. [DOI] [PubMed] [Google Scholar]
- 54.Jokela M, Pulkki-Råback L, Elovainio M, Kivimäki M. Personality traits as risk factors for stroke and coronary heart disease mortality: pooled analysis of three cohort studies. J Behav Med. 2013:1–9. doi: 10.1007/s10865-013-9548-z. [DOI] [PubMed] [Google Scholar]
- 55.Jokela M, Batty GD, Nyberg ST, et al. Personality and All-Cause Mortality: Individual-Participant Meta-Analysis of 3,947 Deaths in 76,150 Adults. American Journal of Epidemiology. 2013;178:667–75. doi: 10.1093/aje/kwt170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rottman BM, Ahn W, Sanislow CA, Kim NS. Can clinicians recognize DSM-IV personality disorders from five-factor model descriptions of patient cases? The American Journal of Psychiatry. 2009;166:427–33. doi: 10.1176/appi.ajp.2008.08070972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Widiger TA, Costa PT. Integrating normal and abnormal personality structure: the five–factor model. J Pers. 2012;80:1471–506. doi: 10.1111/j.1467-6494.2012.00776.x. [DOI] [PubMed] [Google Scholar]
- 58.Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills interventions and survival as a non–drug user over a 2-year period during adolescence. Arch Gen Psychiatry. 2010;67:85–93. doi: 10.1001/archgenpsychiatry.2009.173. [DOI] [PubMed] [Google Scholar]
- 59.Cuijpers P, Smit F, Penninx BW, et al. Economic costs of neuroticism: a population-based study. Arch Gen Psychiatry. 2010;67:1086–93. doi: 10.1001/archgenpsychiatry.2010.130. [DOI] [PubMed] [Google Scholar]
- 60.Gosling SD, Rentfrow PJ, Swann WB., Jr A very brief measure of the Big-Five personality domains. Journal of Research in personality. 2003;37:504–28. [Google Scholar]
- 61.Sutin AR, Terracciano A, Milaneschi Y, et al. The trajectory of depressive symptoms across the adult life span. JAMA psychiatry. 2013;70:803–11. doi: 10.1001/jamapsychiatry.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychol Bull. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1