Transgender Stigma and Health: A Critical Review of Stigma Determinants, Mechanisms, and Interventions (original) (raw)
. Author manuscript; available in PMC: 2016 Dec 1.
Abstract
Rationale
Transgender people in the United States experience widespread prejudice, discrimination, violence, and other forms of stigma.
Objective
This critical review aims to integrate the literature on stigma towards transgender people in the US.
Results
This review demonstrates that transgender stigma limits opportunities and access to resources in a number of critical domains (e.g., employment, healthcare), persistently affecting the physical and mental health of transgender people. The applied social ecological model employed here elucidates that transgender stigma operates at multiple levels (i.e., individual, interpersonal, structural) to impact health. Stigma prevention and coping interventions hold promise for reducing stigma and its adverse health-related effects in transgender populations.
Conclusion
Additional research is needed to document the causal relationship between stigma and adverse health as well as the mediators and moderators of stigma in US transgender populations. Multi-level interventions to prevent stigma towards transgender people are warranted.
Keywords: Transgender, Stigma, Health, Inequities, Interventions
Transgender is as an umbrella term used to define individuals whose gender identity or expression differs from the culturally-bound gender associated with one’s assigned birth sex (i.e., male or female) (Davidson, 2007; Valentine, 2007). While there is considerable variability in who falls under the transgender umbrella, it is estimated that 0.03–0.05% of the population are transgender (Conron et al., 2012; Gates, 2011; Reisner et al., 2014a). Transgender individuals define their gender identity (e.g., man, woman, transgender man, transgender woman, genderqueer, bigender, butch queen, femme queen) and express their gender in a variety of ways, which may vary according to racial/ethnic background, socio-economic status, and place of residence (Valentine, 2007). Some transgender individuals choose to socially transition (e.g., change their name, pronoun, gender expression) and/or medically transition (e.g., cross-sex hormones, surgery) to align their gender expression with their gender identity, while others choose to have a gender expression or identity outside of the traditional gender binary (e.g. gender nonconforming people) (Davidson, 2007). In the US, transgender individuals are considered deviant for having a gender identity or expression that is discordant with the gender typically associated with their assigned birth sex and experience widespread stigma as a result (Bockting et al., 2013; Grant, 2011; Lombardi et al., 2002).
Stigma is the social process of labeling, stereotyping, and rejecting human difference as a form of social control (Link & Phelan, 2001; Phelan et al., 2008). Given that stigma is a complex and dynamic process, the measurement of stigma is inherently thwarted by challenges including concerns regarding the level (e.g., interpersonal, structural) and perspective (e.g., objective versus subjective experiences) at which to operationalize stigma and measure its severity and frequency (e.g., hate crimes versus everyday discrimination) (Meyer, 2003a). Here we draw on sociological and public health theory (socio-ecological model; Baral et al., 2013; Link & Phelan, 2006), operationalizing stigma according to the levels and means through which it is experienced—structural, interpersonal, and individual (Figure 1). Structural stigma refers to the societal norms and institutional policies that constrain access to resources, while interpersonal stigma refers to direct or enacted forms of stigma such verbal harassment, physical violence, and sexual assault due to one’s gender identity or expression. At the individual level, stigma includes the feelings people hold about themselves or the beliefs they perceive others to hold about them that may shape future behavior such as the anticipation and avoidance of discrimination. Structural, interpersonal, and individual forms of stigma are highly prevalent among transgender people and have been linked to adverse health outcomes including depression, anxiety, suicidality, substance abuse, and HIV (Clements-Nolle et al., 2006; Grant, 2011; Nemoto et al., 2011; Reisner et al., 2014b; Sevelius, 2013).
Figure 1.
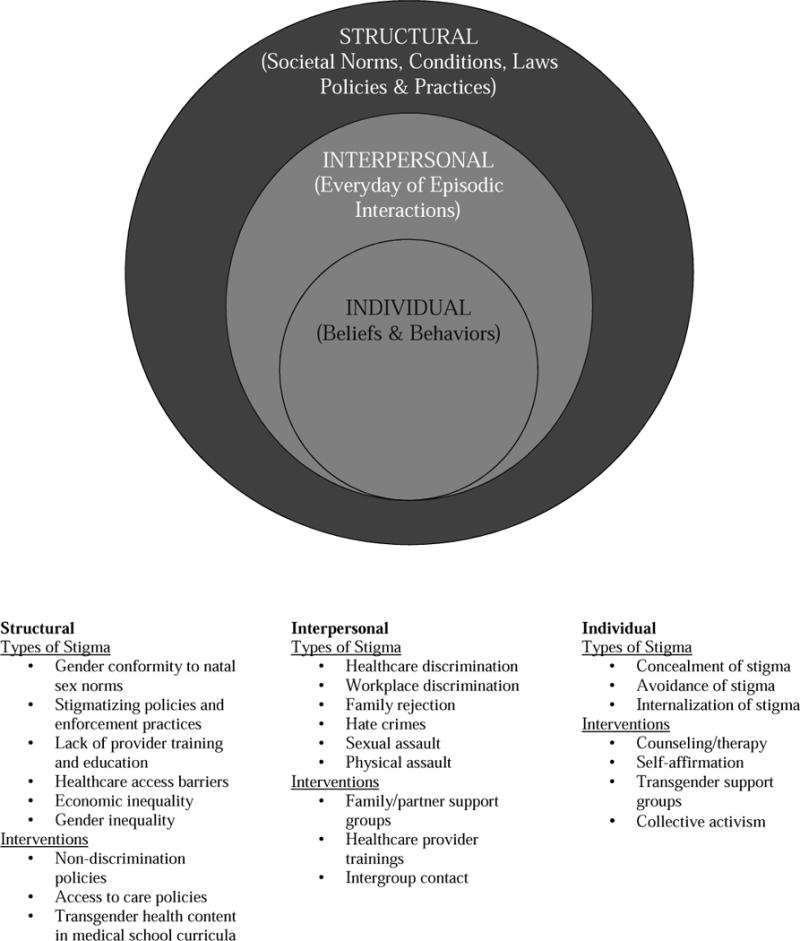
Modified Social-Ecological Model of Transgender Stigma & Stigma Interventions
Stigma is a fundamental cause of adverse health in transgender populations as it works directly to induce stress (a key driver of morbidity and mortality) and indirectly by restricting access to health protective resources (e.g. knowledge, money, power) (Hatzenbuehler et al., 2013; Link & Phelan, 1995). Transgender stigma works through multiple risk factors to impact multiple health outcomes. Indeed, interpersonal and structural stigma are associated with inequities in employment, healthcare, and housing for transgender people compared to cisgender (non-transgender) people—fundamental resources that when restricted are associated with poor health in transgender communities (e.g., depression, suicidality, conditions requiring emergency care) (Clements-Nolle et al., 2006; Nemoto et al., 2011; Reisner et al., 2015b). Consistent with fundamental cause theory, transgender stigma occurs across place and time, such that even when one form of stigma is eliminated (e.g., healthcare providers become knowledgeable about transgender care), other forms of stigma (e.g., insurance policies impede access to gender affirming care) will continue to ensure adverse health outcomes for transgender individuals.
While emerging evidence suggests that stigma makes transgender persons vulnerable to stress and subsequent mental and physical health problems (Bockting et al., 2013; Gamarel et al., 2014; Operario et al., 2014; Reisner et al., 2015b; Xavier et al., 2013), to our knowledge, synthesized findings on the health consequences of transgender stigma and interventions to reduce stigma towards transgender people remain absent from the literature. This article aims to fill the gap in the literature by reviewing transgender stigma at the multiple levels it operates to influence the health of transgender people. This review then summarizes interventions targeting transgender stigma at multiple levels and concludes by outlining a research agenda to understand and reduce stigma toward this marginalized segment of the US population.
Stigma at Multiple Levels
Stigma has the ability to affect transgender health at multiple levels. Using an applied ecological model, this section reviews transgender stigma at the structural, interpersonal, and individual levels.
Level 1: Stigma at the Structural-Level
Structural stigma refers to the societal norms, environmental conditions, and institutional laws and practices that limit the resources, opportunities, and wellbeing of stigmatized people (Hatzenbuehler et al., 2010). Central to structural stigma is power, which is used by the stigmatizing majority to exclude and marginalize those who are different. Across modern Euro-American history, cultural schemas have created and reinforced a binary gender system (i.e., male and female) derived from biological sex characteristics (e.g., chromosomes and genitalia) (West & Zimmerman, 1987). Under this binary system, having a gender identity or expression that aligns with one’s sex characteristics is seen as normative, while transgender people are seen as the “other” (Link & Phelan, 2014; Schilt & Westbrook, 2009). It is the very process of labeling transgender people as non-normative (e.g., through community beliefs, medical/psychiatric diagnoses) that legitimatizes social norms and bestows the cisgender majority (“gender normals”) with power and privilege (Link & Phelan, 2014; Schilt & Westbrook, 2009). Structural stigma in this context may therefore operate as a form symbolic violence in which structures, such as communities, institutions, or governments perpetrate violence through the laws, policies, and community mores that restrict and forcibly reshape transgender individuals in ways that ultimately serve to maintain the power and privilege of the cisgender minority (Valentine, 2007).
The medicalization of gender nonconformity represents one form of structural stigma that both shapes and reinforces societal perceptions of transgender people as deviant. The movement to medicalize gender nonconformity first began in the early 1900’s in an effort to legitimate gender nonconformity as biologically innate, rather than a choice (Bockting, 2014). The movement eventually led to the development of surgical and hormonal treatments to assist transgender individuals in altering their bodies to align with their gender identities. While medical gender affirmation (e.g., sex change) procedures were opposed by most of the mainstream medical community well into the 1960’s (Green, 1969; Worden & Marsh, 1955), mounting data demonstrating the apparent success of medical interventions (i.e., patient satisfaction, improved quality of life), paired with the failure of psychoanalytic interventions to alter a person’s gender identity, eventually led more medical and mental health providers to support these surgeries in the later half of the 20th century (Meyerowitz & Meyerowitz, 2009). Although shifting attitudes provided potential surgical access for transgender people seeking to masculinize or feminize their body, the movement towards medicalized gender conformity maintained the rigid binary construction of gender, making gender conforming transgender people invisible, and further stigmatizing those who do not conform to socially sanctioned expressions of gender (Bockting, 2014; Conrad & Schneider, 2010; Meyerowitz & Meyerowitz, 2009; Namaste, 2000). Moreover, possessing a gender identity or expression incongruent with one’s assigned birth sex was viewed as sexually deviant or disordered and listed as such in the Diagnostic and Statistical Manual of Mental Disorders from 1968 to 2013 (APA, 1968, 2013).
Today, having a nonconforming gender identity or expression is no longer viewed as medically disordered. This notion is reflected in the change from gender identity disorder to gender dysphoria in the DSM, whereby gender dysphoria describes the distress associated with sex/gender incongruence, rather than the experience of gender variation itself (APA, 2013). Medical treatment for those experiencing distress is aimed as eliminating the state of dysphoria, rather than helping patients to conform to a binary gender expression (Coleman et al., 2012). Similar changes have also been made in the International Classification of Diseases; however, some activists argue that any formal diagnosis related to the “symptoms” of gender nonconformity serve to perpetuate stigma for transgender individuals (Drescher, 2014). Still, formal diagnoses are required for healthcare reimbursement and to access many gender affirmation procedures and thus persist (Drescher, 2014).
Structural stigma can also affect transgender health through policies and practices that restrict access to healthcare. Many transgender people lack insurance, which may be due in part to higher prevalence of unemployment among transgender people relative to the general population – a likely product of employment discrimination (Conron et al., 2012; Grant, 2011). Lack of insurance coverage restricts access to care. Although even when transgender people are insured, barriers to accessing gender affirming care often persist, as many private insurers may attempt to exclude coverage for gender affirming medical interventions claiming these procedures are, “pre-existing,” “cosmetic,” or “medically unnecessary” (Khan, 2013).
Transgender people who do not have access to insurance for transgender-specific care are forced to pay out of pocket for gender affirmation procedures, which may be cost prohibitive (Khan, 2013). Unable to pay for medically necessary care, some transgender people resort to the use of street hormones acquired through friends or online (Grossman & D’augelli, 2006; Sanchez et al., 2009). Street hormones can pose health risks if taken in excess of recommended doses or if hormone syringes are contaminated with HIV or other diseases. Street hormones can also pose health risks if the hormones contain a dangerous substance, which is common as street hormones are unregulated (Coleman et al., 2012; Nemoto et al., 1999; Williamson, 2010).
Due to social systems that favor masculinity over femininity (Schilt, 2010), transgender women often experience greater discrimination in employment and subsequent economic stressors relative to transgender men (Grant, 2011; Movement Advancement Project, 2013). Faced with societal pressures to conform to feminine ideals of beauty and unable to pay for surgery, some transgender women, often women of color, resort to “pumping” or using liquid silicone to enlarge their hips, breasts, butt and/or lips (Garofalo et al., 2006; Herbst et al., 2008; Sevelius, 2013; Wallace, 2010; Williamson, 2010). Pumping can pose adverse consequences as loose silicone can shift, causing permanent disfigurement, pulmonary embolism, pneumonia, renal failure, and even death (CDC, 2008; Gaber, 2004; Williamson, 2010). Lack of access to medically necessary care has also been shown to lead to depression, suicidal ideation, non-suicidal self-injury, and suicide for individuals of diverse transgender experience (Huft, 2008; Spicer, 2010).
Institutional practices that lead to inadequate access to essential resources such as healthcare represent another form of structural stigma. Indeed, lack of trained healthcare providers can limit access to care (Khan, 2013). Lack of trained providers is driven in part by the failure of most medical schools and healthcare institutions to train their students and staff in transgender care (Makadon, 2008; Obedin-Maliver et al., 2011; Solursh et al., 2003). In fact, a 2011 study of deans of medical education in North America found that the median number of hours dedicated to LGBT-related curricular content was five (Obedin-Maliver et al., 2011). Insufficient education in medical school translates into lack of knowledge on the job, as medical providers report lack of sufficient training and exposure to transgender patients, impacting their ability to provide medically competent and sensitive care to transgender patients (Lurie, 2005; Poteat et al., 2013). The limited availability of trained providers forces some transgender people to travel long distances to receive care, pay out of pocket for a trained provider not covered under one’s insurance, or postpone care altogether – an outcome of structural stigma with direct health implications (see interpersonal stigma section below) (Cruz, 2014; Dewey, 2008).
Policies that favor one group over another represent another form of structural stigma which produce and reflect community beliefs that stigmatized groups (e.g., transgender people) are unworthy of equal protections under the law (Westbrook & Schilt, 2013). For example, as recently as 2000, state-level anti-discrimination policies excluded transgender individuals as a protected class (National Gay and Lesbian Task Force, 2008); as a result, transgender people could be victimized without legal recourse. In 2012 Massachusetts passed a non-discrimination law providing protections for transgender people in employment, education, and housing; however, the policy failed to include public accommodation protections despite activists efforts to include them. Exclusion of public accommodation protections means that, as of 2015, transgender people in Massachusetts can legally be refused access to public bathrooms, denied healthcare, and removed from public transportation among other spaces - discrimination experiences associated with increased risk of adverse physical symptoms (such as headache, upset stomach, tensing of muscles, or pounding heart) and emotional symptoms (feeling emotionally upset, sad, or frustrated) (Reisner et al., 2015b). While the original bill had included public accommodations, the protections were removed due to stigma-driven concerns from conservative groups that individuals who were not actually transgender would gain access to women’s bathrooms, posing a threat to women and children (Massachusetts Family Institute, 2011; MassResistance, 2008; Westbrook & Schilt, 2013). As of 2015, efforts to pass a state-wide public accommodations bill remain stalled in the Massachusetts legislature and other states where supporting the unsubstantiated claims of some members of the cisgender minority is of greater importance than providing transgender people with access to essential resources such as bathrooms and other public spaces (Westbrook & Schilt, 2013).
Level 2: Interpersonal Stigma
Societal norms and beliefs often translate into enacted stigma at the interpersonal level, which can produce negative consequences for transgender people. Indeed, individuals may hold the same community-level biases around gender nonconformity, which may be explicit (known to the individual and within their control) or implicit (automatically activated, often subconscious biases for which people have limited control) (Major et al., 2013). However, in order for a person to enact their biases towards a transgender person, they must first be aware that the individual is transgender.
Goffman (1963) described those with visible stigmas as the discredited, as their stigmatized condition is readily apparent and therefore more susceptible to mistreatment. Conversely, the discreditable are those whose stigma is invisible, but who would experience stigma should their stigma become known. To that end, transgender people with low visual conformity (other people can tell they are transgender) experience more discrimination and worse health outcomes than those with high visual conformity (Grant, 2011; Reisner et al., 2015b). Transgender individuals who are unable to access gender affirmation procedures (e.g., due to cost, familial rejection, or health concerns), those who have socially transitioned, but never plan to medically transition, and individuals for whom medical interventions are less effective in producing gender conformity (e.g., those transitioning post-puberty, transgender women on estrogen relative to transgender men on testosterone) may therefore be particularly at risk of experiencing enacted forms of stigma as their nonconforming appearance is visible to others (Bockting et al., 2013; Grant, 2011; Reisner et al., 2015b).
Transgender individuals whose gender/sex incongruence becomes known to others are at risk for enacted forms of stigma such as physical and sexual assault (Grant et al., 2011; see Stotzer, 2009 for a review). Indeed, a review of violence against US transgender people found that prevalence of lifetime physical assault due to gender identity ranged from 33–53% (Stotzer, 2009). It is theorized that gender nonconformity causes perpetrators of violence to become anxious and angry, ultimately enacting violence against transgender people as a means of rejecting and diminishing that which they fear (Westbrook & Schilt, 2013). Gender, race and class also shape violence against transgender people. According to the US National Coalition of Anti-Violence Programs, of the 18 anti-LGBT or HIV-related homicides in 2013, 72% of victims were transgender women, and 67% were transgender women of color (Ahmed & Jindasurat, 2014). Sexual assault is also highly prevalent (13–86%) among transgender individuals independent of gender (Stotzer, 2009), though specific subgroups, including sex workers and transgender women of color, may be particularly vulnerable (Ahmed & Jindasurat, 2014; Stotzer, 2009) due to interlocking systems of oppression (e.g., racism, sexism) (Crenshaw, 1991; Grollman, 2014). Physical and sexual assault is most frequently perpetrated by cisgender males (Stotzer, 2009) and used to exert power over devalued individuals (Schilt, 2009). In the case of sexualized interactions between cisgender men and transgender women, it has been argued that cisgender men feel threatened when they learn a woman is transgender, and react violently in an effort to prove their heterosexuality and reclaim their masculinity and power (Schilt, 2009). Studies also show high levels of reported violence among young and low-income transgender people (Stotzer, 2009), suggesting that violence on the basis of transgender identity or expression often affects the most marginalized transgender subpopulations.
Violence against transgender people is often perpetuated by someone known to the victim, including family members (Stotzer, 2009). Indeed, rejection by one’s family of origin is common among transgender people and may be enacted through physical assault as well as through less overt means such as lack of support around gender expression or barring access to medical gender affirmation procedures (Factor & Rothblum, 2008; Grossman & D’augelli, 2006; Wren, 2002). Familial rejection can occur at any age, although it may be particularly distressful for transgender youth who not only rely on their parents for emotional support (Garofalo et al., 2006), but may become homeless as a result familial rejection (Grant, 2011; Grossman & D’augelli, 2006; Sullivan et al., 2001). For both transgender youth and adults, lack of support is associated with isolation, low self-esteem, depression, and other negative health outcomes (Grossman & D’augelli, 2006; Koken et al., 2009; Nemoto et al., 2011; Simons et al., 2013). Lack of support may also lead some transgender individuals to transition later in life (Fabbre, 2014; Gagné & Tewksbury, 1998). Transitioning later in life may confer economic benefits (particularly for transgender women who are able to earn more as men), while avoiding discrimination in workplace settings (Schilt & Wiswall, 2008). However, delaying one’s transition and concealing one’s transgender identity may cause psychological distress in adolescents and adults (Bryant & Schilt, 2008; Gagné & Tewksbury, 1998). Moreover, delaying transition until adulthood can present transition barriers for those who wish to visually conform to a stereotypically masculine or feminine gender expression as one’s secondary sex characteristics are already formed and therefore may be difficult to reverse or minimize later (Cohen-Kettenis & van Goozen, 2002).
Mistreatment in everyday settings such as healthcare is another form of interpersonal stigma commonly experienced by transgender people. A national study of over 6,000 transgender adults found that 28% had experienced harassment in medical settings, 19% were refused care, and 2% experienced violence in their doctor’s office (Grant, 2011). The prevalence of discrimination was even higher among people of color as 17% of White respondents reported healthcare discrimination compared to 36% of Native Americans, 27% of multi-racial individuals, 22% of Hispanics and 19% of Black respondents (Grant, 2011). In some cases, provider discrimination may be explicit and grounded in stigma-related beliefs (Dewey, 2008; Lurie, 2005; Poteat et al., 2013; Snelgrove et al., 2012). In other cases, provider mistreatment, such as the use of outdated or incorrect language (e.g., wrong pronoun), may be the result of structural factors such as lack of training or implicit biases unknown to the provider (Major et al., 2013). To that end, qualitative research shows that insufficient provider training creates uneasiness and discomfort for both patients and providers, and even hostile treatment for transgender patients (Lurie, 2005; Poteat et al., 2013). Stigma in healthcare settings has individual behavioral implications, including the anticipation and avoidance of stigma in future healthcare interactions (see below) (Grant, 2011; Poteat et al., 2013; Reisner et al., 2015b; Schilder et al., 2001).
Level 3: Individual Stigma
Stigma at the interpersonal level can shape stigmatized individuals’ cognitive, affective, and behavioral processes. Thus, at the individual level, stigmatized individuals’ psychological processes are affected by stigma, which powerfully shapes their basic orientation to themselves, others, and their environmental circumstances. These processes include anxious expectations of rejection and stigma avoidance, stigma concealment, and reduced self-efficacy to cope with stigma-related stressors.
Experiencing stigma at the interpersonal level can affect how transgender people evaluate and approach future situations. Anxiously expecting discrimination can lead to avoidance of interpersonal situations, which can take a toll on one’s mental and physical health (Reisner et al., 2015a; Reisner et al., 2015b). For example, many transgender people report experiencing mistreatment in healthcare settings, which is associated with postponing necessary care and the development of conditions requiring emergency care (Cruz, 2014; Dewey, 2008; Grant, 2011; Reisner et al., 2015b; Xavier et al., 2013). Transgender individuals’ avoidance of healthcare due to mistreatment supports the stigma-based rejection sensitivity model proposed by Mendoza-Denton et al., (2002), in which stigmatized individuals nervously anticipate (hypervigilance), routinely observe (perceived stigma), and anxiously react to rejection with important health costs (e.g., the onset of otherwise preventable health conditions).
Transgender individuals who are visually conforming may choose not to disclose their transgender identity as a form of stigma management (Cruz, 2014; Dewey, 2008; Goffman, 1963; Mizock & Mueser, 2014). To that end, visually conforming transgender individuals are said to have “passing privilege” as their stigma is hidden and they are able to avoid mistreatment (Sevelius, 2013; Xavier, 1999). While the ability to pass may help transgender individuals avoid stigma, concealing a core aspect of one’s self can impart profound stress on individuals who question when their stigma will be discovered and whether they should disclose their stigma to others (Smart & Wegner, 1999). Concealing one’s transgender status can also limit the extent to which stealth individuals (those who do not disclose their transgender history to anyone) are able to access support from the transgender community or medical and mental health interventions. Additionally, concealment by those who have not transitioned can restrict access to transition-related care for those who desire it, as well as prevent those who have transitioned from receiving appropriate preventative care for anatomy they may still possess (e.g., pap tests for transgender men, prostate exams for transgender women) (Alegria, 2011; Samuel & Zaritsky, 2008).
The internalization of stigma can also impact an individual’s ability to cope with external stressors, erode self-efficacy for enacting health-promoting behaviors, and eventually diminish an individual’s ability to remain resilient in the face of negative events (Hendricks & Testa, 2012; Meyer, 2003b; Mizock & Mueser, 2014). In fact, high levels of internalized transgender stigma is associated with increased probability of lifetime suicide attempts (Perez-Brumer et al., 2015). Additionally, internalized stigma in transgender people may reduce self-care and help-seeking behaviors for mental health problems resulting in a failure to access mental health services when needed (Hellman & Klein, 2004; Ziguras et al., 2003).
Direct Health Effects of Stigma
The negative health impact of multiple forms of stigma are summarized in the gender minority stress theory (Hendricks & Testa, 2012). Derived from minority stress theories applied to other stigmatized statuses (e.g., SES, Dohrenwend, 2000; race, Williams, 2001; sexual minority status, Meyer, 2003b), gender minority stress theory proposes that added stressors related to the stigma attached to one’s discordant gender identity/expression adversely affect health and accounts for health differences between transgender and cisgender individuals on a population level. In this model, structural forms of stigma establish stressful environments for stigmatized populations, which then generate the cognitive, affective, and behavioral stress processes with health consequences reviewed here.
Experimental studies among diverse populations show that stressors have immediate effects on the body including diastolic blood pressure reactivity, increased cortisol output, and elevated cardiometabolic risk (Guyll et al., 2001; Hatzenbuehler et al., 2014b; Townsend et al., 2011). Chronic activation of the body’s stress response system can compromise health over time, a phenomenon termed allostatic load (McEwen & Stellar, (1993). For many, chronic stress is associated with adverse health outcomes, such as hypertension, diabetes, and even death (Anderson, 1989; Hatzenbuehler et al., 2014a; Taylor et al., 2006). Persistent stress has also been linked to anxiety, depression, suicidality, and substance use to cope (Clements-Nolle et al., 2006; Hatzenbuehler et al., 2008; Reisner et al., 2014b). While a dearth of research has explored the long-term physical health effects of stigma-related stress in transgender people, studies among other stigmatized groups reveal that stigma can affect health over the life-course, as middle age Black women in one study, were found to be 7.5 years biologically older than their white peers (Geronimus et al., 2010). Given that transgender people experience stigma in numerous contexts throughout their lives, it is likely that these experiences take a similarly additive toll on their health, yet this remains understudied. Further, adults with multiple disadvantaged statuses are more likely to experience poor physical and mental health than those with a single stigmatized identity (Grollman, 2014). Thus, transgender individuals with multiple disadvantaged statuses (e.g., low income, transgender women of color) may be at particularly increased risk of poor health due the chronic stress associated with experiencing discrimination through multiple pathways.
Interventions to Reduce Stigma and Its Negative Health Impact
To prevent the onset of adverse health outcomes in diverse transgender populations, interventionists need to reduce the factors that cause stress and intervene directly to help transgender people mitigate stress responses. Stigma interventions have been developed to change attitudes and improve coping at the individual-level, reduce the perpetration of stigma at the interpersonal-level, and change the norms, policies, and systems that perpetuate stigma at the structural-level. This section reviews interventions relevant to transgender populations at each level, and across multiple levels, providing potential intervention strategies for future development and testing.
Individual and Interpersonal Stigma Interventions
Clinicians have long recognized the need to intervene to reduce the effects of stigma in transgender people. A primary focus of counseling for transgender individuals involves reducing the shame around one’s transgender identity and helping individuals to cope with the effects of stigma (Coleman et al., 2012; Johnson & Yarhouse, 2013). While the success of these therapeutic strategies have largely been reported through qualitative reports (Bockting et al., 2006; Byne et al., 2012), more recently researchers have attempted to measure the effects of individual-level coping interventions that target the psychological, emotional, and behavioral responses to stigma. A 2014 study of lesbian, gay, bisexual, transgender, and queer or questioning college students and allies (LGBTQA) aimed to build collective self-esteem and reduce the effects of stigma by having participants listen to a presentation on positive LGBTQA identities and write narratives related to their own positive identity experiences (Riggle et al., 2014). Post-intervention, participants showed an increase in positive LGBTQA identity, collective self-esteem, and individual self-esteem; however, these results were not maintained one month later. More intensive interventions (e.g., more sessions, multiple components) aimed at building identity-related self-esteem have been conducted in non-transgender sexual minority populations with more sustained positive results (Pachankis & Goldfried, 2010; Pachankis et al., 2015). While individual-level coping interventions tend to be feasible to implement, they are limited in their ability to reach all stigmatized individuals in need of support. Thus, efforts that reach a larger audience of stigmatized people may yield more sustainable and far-reaching results.
While clinical interventions can be useful in addressing individual challenges, interventions that help transgender individuals to connect and share strategies for resilience can be effective in managing stigma (Schrock et al., 2004). In fact, awareness and engagement with other transgender people significantly influences risk and resilience during early gender identity development as both prior awareness and engagement with other transgender people are related to less fearfulness, less suicidality, and more comfort (Testa et al., 2014). Recognizing the utility of community support, groups have been developed to provide transgender people with the opportunity to connect with one another and manage the effects of stigma (Bradford et al., 2013; Schrock et al., 2004). In evaluating the effects of a transgender support groups, Schrock et al., (2004) found that participants were able to “find relief from shame, fear, powerlessness, alienation, and inauthenticity” (p. 76). Moreover, transgender social support and community involvement have been shown to protectively moderate the association between stigma and psychological distress (Bockting et al., 2013) and physical health outcomes (i.e. HIV/STI infection) (Nuttbrock et al., 2015). One limitation of social support interventions, however, is that they teach individuals to behaviorally manage the effects of stigma without addressing the structural forces that create and perpetuate stigma (Schrock et al., 2004). Thus, individual interventions that foster social change may be more effective and sustainable.
Collective activism serves as a means to combat the effects of stigma. Activism around a shared cause can create a sense of unity and collective identity and help individuals to feel empowered against stigma (Ashmore et al., 2004; Testa et al., 2014). Activism generally requires an individual to be out about their transgender identity. Through their visibility, out activists reject societal efforts to keep transgender people down and concealed (Bornstein & Bergman, 2010), while also avoiding the psychiatric distress associated with concealing a stigmatized aspect of one’s self (Schrock et al., 2004). Activism may be particularly empowering for transgender people as it simultaneously yields personal fulfillment and fights systems of oppression (Mizock & Mueser, 2014; Schrock et al., 2004).
Interventions to reduce transgender stigma and its effects need not be limited to transgender people, but also individuals who hold the power to constrain the opportunities and resources of transgender people, such as family members, peers, and providers. Interventions aimed at family members can have positive effects, including fostering understanding and acceptance of transgender loved ones as well as recognizing one is not alone (Broad, 2011; Menvielle & Hill, 2010; Menvielle & Tuerk, 2002). A central component of many family support groups is education about transgender experiences which allows non-transgender participants to develop a humanizing perspective of their transgender family member and no longer see them as the “other” (MacNish & Gold-Peifer, 2014; Menvielle & Hill, 2010). Support groups can also aid family members in coping with the loss of their transgender family member as they knew them, as well as combating the stigma that families also face due to having a transgender loved one (MacNish & Gold-Peifer, 2014; Menvielle & Tuerk, 2002). Such interventions can also help to create allies who can educate the broader community about transgender issues in order to reduce structural and interpersonal stigma (Broad, 2011; Broad et al., 2008).
Many providers lack training in transgender care and are in need of interventions to prevent enacted stigma in healthcare settings (Lurie, 2005; Poteat et al., 2013; Snelgrove et al., 2012). Educational efforts to increase transgender cultural competency (e.g., “Transgender 101” trainings) are often successful in improving healthcare provider awareness and understanding of transgender patients by exposing them to the healthcare barriers that transgender people encounter and improving their skills in caring for transgender patients (Hanssmann et al., 2008). Empirical interventions to improve providers’ transgender medical knowledge have also demonstrated success, as a lecture covering the durability of gender identity and hormonal treatment regimens significantly increased physician-residents’ knowledge and willingness to provide hormonal therapy for transgender patients (Thomas & Safer, 2015). An intervention to reduce providers’ implicit racial biases was also successful (Burgess et al., 2007) and could be adapted to reduce providers’ implicit transgender bias in healthcare settings. While education is important, lack of exposure to transgender people represents a barrier to provider comfort and expertise (Lurie, 2005). Inter-group contact is effective in reducing prejudice among diverse populations (Pettigrew & Tropp, 2006). Thus, interventions aimed at increasing provider contact with transgender people may be beneficial in eliminating biases and discomfort (Pettigrew & Tropp, 2006; Walch et al., 2012); although such interventions could prove burdensome to transgender people.
To our knowledge no empirical studies testing the efficacy of provider contact interventions exist for transgender patients; however, a recent study with college students showed that exposure to a transgender speaker panel on transgender stigma yielded greater immediate decreases in stigma compared to a lecture led by non-transgender people (Walch et al., 2012). Healthcare entities have also begun to institute training programs aimed at increasing transgender medical and cultural competency through exposure to transgender patients and trainings led by transgender people (Hanssmann et al., 2008; Makadon, 2008). While these interventions represent efforts to reduce transgender stigma in healthcare settings, they require significant time and resources, with positive effects only extending to those who participate in the intervention and often only sustained for a limited time (Hanssmann et al., 2008). Given that stigma is socially constructed, efforts to reduce transgender stigma at the population-level and improve health outcomes for all transgender people are needed.
Structural Stigma Interventions
Changes to policies that reduce stigma and provide equal opportunities for transgender people have the potential to improve the health of transgender individuals. Recent years have witnessed a movement to be more inclusive of transgender people in non-discrimination policies, with numerous states having passed laws to provide transgender people with equal protections in employment, housing, and education (Transgender Law and Policy Institute, 2012). While empirical work has not assessed whether these policies had an effect on the lived realities of transgender people, studies in other populations suggest that even changes to distal stigma structures (i.e., state-level policies) can improve the health of stigmatized groups (Hatzenbuehler & Keyes, 2013; Hatzenbuehler et al., 2009). For example, Hatzenbuehler et al. (2009) examined state-level policies that provided protections against hate crimes and employment discrimination based on sexual orientation and found that state-level protective policies led to a reduction in the association between LGB status and mood disorders. Similarly, a study of anti-bullying laws in Oregon found that inclusive anti-bullying policies were significantly associated with a reduced risk for suicide attempts and exposure to peer victimization among gay youth (Hatzenbuehler & Keyes, 2013). These findings suggest that policies can positively impact the lives of stigmatized individuals by providing greater protections and access to resources under the law.
As noted previously, access to gender transition-related care represents an important structural factor that can impact the mental and physical health of transgender people. In 2010, the Affordable Care Act made it illegal for insurance companies to deny individuals on the basis of pre-existing conditions and gender identity (ACA, 2010). The law also provides low-income people with access to gender affirmation therapies through Medicaid. Protections for older and disabled adults came with the 2014 repeal of the Medicare policy of excluding coverage for transition-related surgery, thus allowing care decisions to be made on an individual basis (NCTE, 2015). While other structural factors, such as untrained providers could still bar access to care for transgender patients, extended coverage under the law may encourage medical schools and healthcare institutions to increase training for transgender care as gender affirmation surgeries will become reimbursable (Khan, 2013). Such policy changes serve as structural interventions that engender immediate health benefits through increased access to care and also have the potential to shift societal attitudes by increasing public awareness of transgender issues.
Multi-Level Community-Based Stigma Interventions
As shown in this review, stigma works at multiple levels to impact the health of transgender people; thus, interventions that target stigma at multiple levels are likely to achieve the maximum benefit (Cook et al., 2014). Once such campaign is the I AM Trans People Speak campaign developed by the Massachusetts Transgender Political Association (MTPC, 2013), which features videos of transgender people sharing their stories and the multiple identities they hold. The videos act as a self-affirmation intervention (Walton & Cohen, 2011) that aids transgender people in coping with stigma. The campaign also features videos of family members, partners, and other transgender allies telling their narratives of heartbreak, acceptance, and unconditional love. While the project has not been rigorously evaluated, dissemination of the videos to non-transgender audiences aims to reduce transgender stigma by educating the public about transgender people’s lives and eliminating stereotypes through exposure. Similar programs have also been developed to address mental illness stigma and homophobia with positive results (Corrigan & Gelb, 2006; Vinney, 2014). The I Am campaign is just one strategy MTPC uses to combat transgender stigma and discrimination at multiple levels. The organization also advocates for the passage of supportive legislation, engages in community education by delivering “Transgender 101” trainings, supports transgender people in responding to discrimination, and encourages community empowerment through collective action. Interventionists looking to reduce transgender stigma should consider collaboratively engaging in research with communityled organizations, as community-based participatory research can yield measurable, significant, and sustainable results (Corrigan & Shapiro, 2010).
Summary and Future Directions
Changing attitudes have allowed transgender people to become more visible in society. However, the increased visibility of transgender people also highlights the high prevalence of adverse health outcomes that exist in some transgender communities – health inequities linked to the societal stigma attached to gender nonconforming identities and expressions. While recent US non-discrimination policies may reflect greater acceptance of transgender people, widespread interpersonal stigma ultimately impacts the health of transgender individuals.
This review paves a path for a transgender health research agenda that includes three primary domains: 1) Stigma Determinants: Stronger evidence—using population-based, longitudinal, and experimental designs—is needed to document the causal relationship between stigma and adverse health in US transgender populations. 2) Stigma Mechanisms and Moderators: Future studies should simultaneously and interactively examine the structural, interpersonal, and individual pathways through which stigma operates to jeopardize the health of transgender people in the US. Such research will permit examination of the pathways that mediate the stigma-health relationship for this population and the investigation of moderators that may help to identify subgroups at greatest risk for poor health (e.g., by age, race/ethnicity, poverty) or protective factors that can be levied as future modifiable intervention targets (e.g., transgender peer support, community involvement). 3) Stigma Interventions: Interventions are needed to reduce stigma toward transgender people at the individual, interpersonal, and structural levels. Multi-level interventions that concurrently address individual responses to stigma (e.g., stigma management and coping), implicit and explicit biases that contribute to enacted stigma at the interpersonal level (e.g., provider attitudes), and systems that restrict access to essential resources as the structural level (e.g., restrictive policies) also warrant future development and testing. Regardless of intervention level, these approaches should meaningfully enlist the input of transgender communities to ensure intervention acceptability, engagement, and long-term implementation.
Research Highlights.
- Stigma contributes to widespread health inequities in US transgender communities.
- We review the multiple levels at which stigma towards transgender people operates.
- The stress mechanisms through which stigma contributes to health are discussed.
- Intervention strategies to reduce transgender stigma are outlined at each level.
- Multi-level interventions are needed to reduce transgender stigma in the US.
Acknowledgments
Jaclyn White Hughto is supported by grants T32MH020031 and P30MH062294 from the National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- ACA. Law P, editor. Patient protection and affordable care act. 2010;124:111–148. [Google Scholar]
- Ahmed O, Jindasurat C. Lesbian, Gay, Bisexual, Transgender, Queer and HIV-Affected Hate Violence in 2013. 2014 http://www.avp.org/storage/documents/2013_ncavp_hvreport_final.pdf.
- Alegria CA. Transgender identity and health care: Implications for psychosocial and physical evaluation. Journal of the American Academy of Nurse Practitioners. 2011;23(4):175–182. doi: 10.1111/j.1745-7599.2010.00595.x. [DOI] [PubMed] [Google Scholar]
- Anderson NB. Racial differences in stress-induced cardiovascular reactivity and hypertension: current status and substantive issues. Psychological Bulletin. 1989;105(1):89–105. doi: 10.1037/0033-2909.105.1.89. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and statistical manual of mental disorders, (DSM-II) Washington, D.C: American Psychiatric Association; 1968. [Google Scholar]
- APA. The Diagnostic and Statistical Manual of Mental Disorders: DSM 5. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- Ashmore RD, Deaux K, McLaughlin-Volpe T. An organizing framework for collective identity: articulation and significance of multidimensionality. Psychological Bulletin. 2004;130(1):80–114. doi: 10.1037/0033-2909.130.1.80. [DOI] [PubMed] [Google Scholar]
- Baker HJ. Transsexualism-problems in treatment. American Journal of Psychiatry. 1969;125(10):1412–1418. doi: 10.1176/ajp.125.10.1412. [DOI] [PubMed] [Google Scholar]
- Bockting WO. Gender Dysphoria and Disorders of Sex Development. New York, NY: Springer; 2014. The impact of stigma on transgender identity development and mental health; pp. 319–330. [Google Scholar]
- Bockting WO, Knudson G, Goldberg JM. Counseling and mental health care for transgender adults and loved ones. International Journal of Transgenderism. 2006;9(3–4):35–82. [Google Scholar]
- Bockting WO, Miner MH, Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. American Journal of Public Health. 2013;103(5):943–951. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein K, Bergman SB. Gender outlaws: The next generation. Berkeley, CA: Seal Press; 2010. [Google Scholar]
- Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. American Journal of Public Health. 2013;103(10):1820–1829. doi: 10.2105/AJPH.2012.300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broad K. Coming out for parents, families and friends of lesbians and gays: From support group grieving to love advocacy. Sexualities. 2011;14(4):399–415. [Google Scholar]
- Broad KL, Alden H, Berkowitz D, Ryan M. Activist parenting and GLBTQ families. Journal of GLBT Family Studies. 2008;4(4):499–520. [Google Scholar]
- Bryant K, Schilt K. Transgender people in the US military: Summary and analysis of the 2008 transgender American Veterans Association survey. 2008 http://www.palmcenter.org/system/files/TGPeopleUSMilitary.pdf.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: Lessons from social-cognitive psychology. Journal of General Internal Medicine. 2007;22(6):882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byne W, Bradley SJ, Coleman E, Eyler AE, Green R, Menvielle EJ, et al. Report of the American Psychiatric Association task force on treatment of gender identity disorder. Archives of Sexual Behavior. 2012;41(4):759–796. doi: 10.1007/s10508-012-9975-x. [DOI] [PubMed] [Google Scholar]
- CDC. Acute renal failure associated with cosmetic soft-tissue filler injections–North Carolina, 2007. Morbidity and Mortality Weekly Report. 2008;57(17):453–456. [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. Journal of Homosexuality. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- Cohen-Kettenis PT, van Goozen SH. Adolescents who are eligible for sex reassignment surgery: Parental reports of emotional and behavioural problems. Clinical Child Psychology and Psychiatry. 2002;7(3):412–422. [Google Scholar]
- Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. International Journal of Transgenderism. 2012;13(4):165–232. [Google Scholar]
- Conrad P, Schneider JW. Deviance and medicalization: From badness to sickness. Philadelphia, PA: Temple University Press; 2010. [Google Scholar]
- Conron KJ, Scott G, Stowell GS, Landers SJ. Transgender health in Massachusetts: Results from a household probability sample of adults. American Journal of Public Health. 2012;102(1):118–122. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JE, Purdie-Vaughns V, Meyer IH, Busch JT. Intervening within and across levels: A multilevel approach to stigma and public health. Social Science and Medicine. 2014;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- Corrigan P, Gelb B. Three programs that use mass approaches to challenge the stigma of mental illness. Psychiatric Services. 2006;57(3):393–398. doi: 10.1176/appi.ps.57.3.393. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clinical Psychology Review. 2010;30(8):907–922. doi: 10.1016/j.cpr.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz TM. Assessing access to care for transgender and gender nonconforming people: A consideration of diversity in combating discrimination. Social Science and Medicine. 2014;110(0):65–73. doi: 10.1016/j.socscimed.2014.03.032. [DOI] [PubMed] [Google Scholar]
- Davidson M. Seeking refuge under the umbrella: Inclusion, exclusion, and organizing within the category transgender. Sexuality Research & Social Policy. 2007;4(4):60–80. [Google Scholar]
- Dewey JM. Knowledge legitimacy: How trans-patient behavior supports and challenges current medical knowledge. Qualitative Health Research. 2008;18(10):1345–1355. doi: 10.1177/1049732308324247. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. The role of adversity and stress in psychopathology: Some evidence and its implications for theory and research. Journal of Health and Social Behavior. 2000:1–19. [PubMed] [Google Scholar]
- Drescher J. Gender dysphoria and disorders of sex development: Progress in care and knowledge. New York, NY: Springer Science + Business Media; US; 2014. Gender identity diagnoses: History and controversies; pp. 137–150. [Google Scholar]
- Fabbre VD. Gender transitions in later life: The significance of time in queer aging. Journal of Gerontological Social Work. 2014;57(2–4):161–175. doi: 10.1080/01634372.2013.855287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Factor RJ, Rothblum ED. A study of transgender adults and their non-transgender siblings on demographic characteristics, social support, and experiences of violence. Journal of LGBT Health Research. 2008;3(3):11–30. doi: 10.1080/15574090802092879. [DOI] [PubMed] [Google Scholar]
- Gaber Y. Secondary lymphoedema of the lower leg as an unusual side-effect of a liquid silicone injection in the hips and buttocks. Dermatology. 2004;208(4):342–344. doi: 10.1159/000077845. [DOI] [PubMed] [Google Scholar]
- Gagné P, Tewksbury R. Conformity pressures and gender resistance among transgendered individuals. Social Problems. 1998;45:81–101. [Google Scholar]
- Gamarel KE, Reisner SL, Laurenceau JP, Nemoto T, Operario D. Gender minority stress, mental health, and relationship quality: A dyadic investigation of transgender women and their cisgender male partners. Journal of Family Psychology. 2014;28(4):437–447. doi: 10.1037/a0037171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. Journal of Adolescent Health. 2006;38(3):230–236. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Gates GJ. How many people are lesbian, gay, bisexual and transgender? 2011 http://www.ciis.edu/Documents/PDFs/PublicPrograms/ExpandingtheCircle/How-many-people-are-LGBT-Final.pdf.
- Geronimus AT, Hicken MT, Pearson JA, Seashols SJ, Brown KL, Cruz TD. Do US black women experience stress-related accelerated biological aging? Human Nature. 2010;21(1):19–38. doi: 10.1007/s12110-010-9078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Englewood Cliffs, N.J: Prentice-Hall; 1963. [Google Scholar]
- Grant JM, Lisa A, Mottet Justin, Tanis Jack, Harrison Jody, Herman L, Keisling Mara. Injustice at every turn: A report of the National Transgender Discrimination Survey. Washington, DC; National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011. [Google Scholar]
- Green R. Attitudes toward transsexualism and sex-reassignment procedures. Transsexualism and sex reassignment. 1969:235–251. [Google Scholar]
- Grollman EA. Multiple disadvantaged statuses and health the role of multiple forms of discrimination. Journal of Health and Social Behavior. 2014;55(1):3–19. doi: 10.1177/0022146514521215. [DOI] [PubMed] [Google Scholar]
- Grossman AH, D’augelli AR. Transgender youth: Invisible and vulnerable. Journal of Homosexuality. 2006;51(1):111–128. doi: 10.1300/J082v51n01_06. [DOI] [PubMed] [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychology. 2001;20(5):315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Hanssmann C, Morrison D, Russian E. Talking, gawking, or getting it done: Provider trainings to increase cultural and clinical competence for transgender and gender-nonconforming patients and clients. Sexuality Research & Social Policy. 2008;5(1):5–23. [Google Scholar]
- Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Social Science and Medicine. 2014a;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM. Inclusive anti-bullying policies and reduced risk of suicide attempts in lesbian and gay youth. Journal of Adolescent Health. 2013;53(1, Supplement):S21–S26. doi: 10.1016/j.jadohealth.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. American Journal of Public Health. 2009;99(12):2275–2281. doi: 10.2105/AJPH.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: A prospective study. American Journal of Public Health. 2010;100(3):452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: results from a prospective study of bereaved gay men. Health Psychology. 2008;27(4):455–462. doi: 10.1037/0278-6133.27.4.455. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Slopen N, McLaughlin KA. Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Health Psychology. 2014b;33(10):1185–1194. doi: 10.1037/hea0000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellman RE, Klein E. A program for lesbian, gay, bisexual, and transgender individuals with major mental illness. Journal of Gay & Lesbian Psychotherapy. 2004;8(3–4):67–82. [Google Scholar]
- Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Professional Psychology Research and Practice. 2012;43(5):460. [Google Scholar]
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: A systematic review. AIDS and Behavior. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- Huft M. Statistically speaking: The high rate of suicidality among transgender youth and access barriers to medical treatment in a society of gender dichotomy. Children’s Legal Rights Journal. 2008;28:53. [Google Scholar]
- Johnson VR, Yarhouse MA. Shame in sexual minorities: Stigma, internal cognitions, and counseling considerations. Counseling and Values. 2013;58(1):85–103. [Google Scholar]
- Khan L. Transgender health at the crossroads: Legal norms, insurance markets, and the threat of healthcare reform. Yale Journal of Health Policy, Law, and Ethics. 2013;11(2):375–418. [PubMed] [Google Scholar]
- Koken JA, Bimbi DS, Parsons JT. Experiences of familial acceptance-rejection among transwomen of color. Journal of Family Psychology. 2009;23(6):853–860. doi: 10.1037/a0017198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Link BG, Phelan J. Stigma power. Social Science and Medicine. 2014;103:24–32. doi: 10.1016/j.socscimed.2013.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001:363–385. [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. The Lancet. 2006;367(9509):528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Lombardi EL, Wilchins RA, Priesing D, Malouf D. Gender violence: Transgender experiences with violence and discrimination. Journal of Homosexuality. 2002;42(1):89–101. doi: 10.1300/j082v42n01_05. [DOI] [PubMed] [Google Scholar]
- Lurie S. Identifying training needs of health-care providers related to treatment and care of transgendered patients: A qualitative needs assessment conducted in New England. International Journal of Transgenderism. 2005;8(2–3):93–112. [Google Scholar]
- MacNish M, Gold-Peifer M. Critical Topics in Family Therapy. Cham: Springer; 2014. Families in transition: Supporting families of transgender youth; pp. 119–129. [Google Scholar]
- Major B, Mendes WB, Dovidio JF. Intergroup relations and health disparities: A social psychological perspective. Health Psychology. 2013;32(5):514–524. doi: 10.1037/a0030358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makadon HJ. The Fenway guide to lesbian, gay, bisexual, and transgender health. Philadelphia, PA: ACP Press; 2008. [Google Scholar]
- Massachusetts Family Institute. Bathroom Bill. 2011 http://www.mafamily.org/category/statelegislation/bathroom-bill/
- MassResistance. PART 3: Public Accommodations. Boston, MA: 2008. [Google Scholar]
- McEwen BS, Stellar E. Stress and the individual: Mechanisms leading to disease. Archives of Internal Medicine. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of Personality and Social Psychology. 2002;83(4):896–918. doi: 10.1037//0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- Menvielle E, Hill DB. An affirmative intervention for families with gender-variant children: A process evaluation. Journal of Gay & Lesbian Mental Health. 2010;15(1):94–123. doi: 10.1080/00926230903375560. [DOI] [PubMed] [Google Scholar]
- Menvielle EJ, Tuerk C. A support group for parents of gender-nonconforming boys. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(8):1010–1013. doi: 10.1097/00004583-200208000-00021. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice as stress: Conceptual and measurement problems. American Journal of Public Health. 2003a;93(2):262–265. doi: 10.2105/ajph.93.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003b;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerowitz JJ, Meyerowitz JJ. How sex changed: A history of transsexuality in the United States. Cambridge, MA: Harvard University Press; 2009. [Google Scholar]
- Mizock L, Mueser KT. Employment, mental health, internalized stigma, and coping with transphobia among transgender individuals. Psychology of Sexual Orientation and Gender Diversity. 2014;1(2):146–158. [Google Scholar]
- Movement Advancement Project. A Broken Bargain for Transgender Workers. 2013 http://www.lgbtmap.org/file/a-broken-bargain-for-transgender-workers.pdf.
- MTPC. I am Trans People Speak. Boston, MA: Massachusetts Transgender Political Coalition; 2013. [Google Scholar]
- Namaste V. Invisible lives: The erasure of transsexual and transgendered people. Chicago, IL: University of Chicago Press; 2000. [Google Scholar]
- National Gay and Lesbian Task Force. Scope of Explicitly Transgender-Inclusive Anti-Discrimination Laws. Transgender Law and Policy Institute; 2008. [Google Scholar]
- NCTE. Know Your Rights - Medicare. National Center for Transgender Equality; 2015. [Google Scholar]
- Nemoto T, Bodeker B, Iwamoto M. Social support, exposure to violence and transphobia, and correlates of depression among male-to-female transgender women with a history of sex work. American Journal of Public Health. 2011;101(10):1980–1988. doi: 10.2105/AJPH.2010.197285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoto T, Luke D, Mamo L, Ching A, Patria J. HIV risk behaviours among male-to-female transgenders in comparison with homosexual or bisexual males and heterosexual females. AIDS Care. 1999;11(3):297–312. doi: 10.1080/09540129947938. [DOI] [PubMed] [Google Scholar]
- Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, et al. Gender abuse and incident HIV/STI among transgender women in New York City: Buffering effect of involvement in a transgender community. AIDS and Behavior. 2015;19(8):1446–1453. doi: 10.1007/s10461-014-0977-7. [DOI] [PubMed] [Google Scholar]
- Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender–related content in undergraduate medical education. JAMA. 2011;306(9):971–977. doi: 10.1001/jama.2011.1255. [DOI] [PubMed] [Google Scholar]
- Operario D, Yang MF, Reisner SL, Iwamoto M, Nemoto T. Stigma and the syndemic of HIV-related health risk behaviors in a diverse sample of transgender women. Journal of Community Psychology. 2014;42(5):544–557. [Google Scholar]
- Pachankis JE, Goldfried MR. Expressive writing for gay-related stress: Psychosocial benefits and mechanisms underlying improvement. Journal of Consulting and Clinical Psychology. 2010;78(1):98–110. doi: 10.1037/a0017580. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology. 2015;83(5):875–889. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Brumer A, Hatzenbuehler ML, Oldenburg CE, Bockting W. Individual- and structural-level risk factors for suicide attempts among transgender adults. Behavioral Medicine. 2015;41(3):164–171. doi: 10.1080/08964289.2015.1028322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology. 2006;90(5):751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: One animal or two? Social Science and Medicine. 2008;67(3):358–367. doi: 10.1016/j.socscimed.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T, German D, Kerrigan D. Managing uncertainty: A grounded theory of stigma in transgender health care encounters. Social Science and Medicine. 2013;84:22–29. doi: 10.1016/j.socscimed.2013.02.019. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB. Monitoring the health of transgender and other gender minority populations: Validity of natal sex and gender identity survey items in a US national cohort of young adults. BMC Public Health. 2014a;14(1):1224–1234. doi: 10.1186/1471-2458-14-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender minority social stress in adolescence: Disparities in adolescent bullying and substance use by gender identity. Journal of Sex Research. 2014b;52(3):243–256. doi: 10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Pardo ST, Gamarel KE, White Hughto JM, Pardee DJ, Keo-Meier CL. Substance use to cope with stigma in healthcare among U.S. female-to-male trans masculine adults. LGBT Health. 2015a doi: 10.1089/lgbt.2015.0001. (ahead-of-print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, White Hughto J, Dunham E, Heflin K, Begenyi J, Coffey-Esquivel J, et al. Legal protections in public accommodations settings: A critical public health issue for gender minority people. Milbank Quarterly. 2015b;93(3):1–32. doi: 10.1111/1468-0009.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggle ED, Gonzalez KA, Rostosky SS, Black WW. Cultivating positive LGBTQA identities: An intervention study with college students. Journal of LGBT Issues in Counseling. 2014;8(3):264–281. [Google Scholar]
- Samuel L, Zaritsky E. Communicating effectively with transgender patients. American Family Physician. 2008;78(5):648–650. [PubMed] [Google Scholar]
- Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. American Journal of Public Health. 2009;99(4):713–719. doi: 10.2105/AJPH.2007.132035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilder AJ, Kennedy C, Goldstone IL, Ogden RD, Hogg RS, O’Shaughnessy MV. “Being dealt with as a whole person.” Care seeking and adherence: the benefits of culturally competent care. Social Science and Medicine. 2001;52(11):1643–1659. doi: 10.1016/s0277-9536(00)00274-4. [DOI] [PubMed] [Google Scholar]
- Schilt K. Just one of the guys?: Transgender men and the persistence of gender inequality. Chicago, IL: University of Chicago Press; 2010. [Google Scholar]
- Schilt K, Westbrook L. Doing gender, doing heteronormativity “gender normals,” transgender people, and the social maintenance of heterosexuality. Gender & Society. 2009;23(4):440–464. [Google Scholar]
- Schilt K, Wiswall M. Before and after: Gender transitions, human capital, and workplace experiences. The BE Journal of Economic Analysis & Policy. 2008;8(1):1–28. [Google Scholar]
- Schrock D, Holden D, Reid L. Creating emotional resonance: Interpersonal emotion work and motivational framing in a transgender community. Social Problems. 2004;51(1):61–81. [Google Scholar]
- Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–689. doi: 10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons L, Schrager SM, Clark LF, Belzer M, Olson J. Parental support and mental health among transgender adolescents. Journal of Adolescent Health. 2013;53(6):791–793. doi: 10.1016/j.jadohealth.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart L, Wegner DM. Covering up what can’t be seen: Concealable stigma and mental control. Journal of Personality and Social Psychology. 1999;77(3):474–486. doi: 10.1037//0022-3514.77.3.474. [DOI] [PubMed] [Google Scholar]
- Snelgrove J, Jasudavisius A, Rowe B, Head E, Bauer G. “Completely out-at-sea” with “two-gender medicine”: A qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Services Research. 2012;12(1):110–113. doi: 10.1186/1472-6963-12-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solursh D, Ernst J, Lewis R, Prisant LM, Mills T, Solursh L, et al. The human sexuality education of physicians in North American medical schools. International Journal of Impotence Research. 2003;15(5):S41. doi: 10.1038/sj.ijir.3901071. [DOI] [PubMed] [Google Scholar]
- Spicer SS. Healthcare needs of the transgender homeless population. Journal of Gay & Lesbian Mental Health. 2010;14(4):320–339. [Google Scholar]
- Stotzer RL. Violence against transgender people: A review of United States data. Aggression and Violent Behavior. 2009;14(3):170–179. [Google Scholar]
- Sullivan C, Sommer S, Moff J. Youth in the margins: A report on the unmet needs of lesbian, gay, bisexual, and transgender adolescents in foster care. New York, NY: Lambda Legal Defense and Education Fund New York; 2001. [Google Scholar]
- Taylor CB, Conrad A, Wilhelm FH, Neri E, DeLorenzo A, Kramer MA, et al. Psychophysiological and cortisol responses to psychological stress in depressed and nondepressed older men and women with elevated cardiovascular disease risk. Psychosomatic Medicine. 2006;68(4):538–546. doi: 10.1097/01.psy.0000222372.16274.92. [DOI] [PubMed] [Google Scholar]
- Testa RJ, Jimenez CL, Rankin S. Risk and resilience during transgender identity development: The effects of awareness and engagement with other transgender people on affect. Journal of Gay & Lesbian Mental Health. 2014;18(1):31–46. [Google Scholar]
- Thomas DD, Safer JD. A simple intervention raised resident-physician willingness to assist transgender patients seeking hormone therapy. Endocrine Practice. 2015 doi: 10.4158/EP15777.OR. (Ahead of Print) [DOI] [PubMed] [Google Scholar]
- Townsend SS, Major B, Gangi CE, Mendes WB. From “in the air” to “under the skin”: Cortisol responses to social identity threat. Personality and Social Psychology Bulletin. 2011;37(2):151–164. doi: 10.1177/0146167210392384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Transgender Law and Policy Institute. US jurisdictions with laws prohibiting discrimination on the basis of gender identity or expression. Transgender Law and Policy Institute; 2012. [Google Scholar]
- Valentine D. Imagining transgender: An ethnography of a category. Durham, NC: Duke University Press; 2007. [Google Scholar]
- Vinney C. Gay adolescent development and the It Gets Better Project: Instilling hope through a new media campaign. Media Psychology Review. 2014;4(4) [Google Scholar]
- Walch SE, Sinkkanen KA, Swain EM, Francisco J, Breaux CA, Sjoberg MD. Using intergroup contact theory to reduce stigma against transgender individuals: Impact of a transgender speaker panel presentation. Journal of Applied Social Psychology. 2012;42(10):2583–2605. [Google Scholar]
- Wallace PM. Finding self: A qualitative study of transgender, transitioning, and adulterated silicone. Health Education Journal. 2010;69(4):439–446. [Google Scholar]
- Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science. 2011;331(6023):1447–1451. doi: 10.1126/science.1198364. [DOI] [PubMed] [Google Scholar]
- West C, Zimmerman DH. Doing gender. Gender & Society. 1987;1(2):125–151. [Google Scholar]
- Westbrook L, Schilt K. Doing gender, determining gender transgender people, gender panics, and the maintenance of the sex/gender/sexuality System. Gender & Society. 2013;28(1):32–57. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson C. Providing care to transgender persons: A clinical approach to primary care, hormones, and HIV management. Journal of the Association of Nurses in AIDS Care. 2010;21(3):221–229. doi: 10.1016/j.jana.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Worden FG, Marsh JT. Psychological factors in men seeking sex transformation: A preliminary report. Journal of the American Medical Association. 1955;157(15):1292–1298. doi: 10.1001/jama.1955.02950320022007. [DOI] [PubMed] [Google Scholar]
- Wren B. ‘I can accept my child is transsexual but if I ever see him in a dress I’ll hit him’: Dilemmas in parenting a transgendered adolescent. Clinical Child Psychology and Psychiatry. 2002;7(3):377–397. [Google Scholar]
- Xavier J. Passing as privilege. Part Two of a Series on Transfeminism. 1999 http://learningtrans.files.wordpress.com/2010/11/jxavier_passing_as_privilege.pdf.
- Xavier J, Bradford J, Hendricks M, Safford L, McKee R, Martin E, et al. Transgender health care access in Virginia: A qualitative study. International Journal of Transgenderism. 2013;14(1):3–17. [Google Scholar]
- Ziguras S, Klimidis S, Lewis J, Stuart G. Ethnic matching of clients and clinicians and use of mental health services by ethnic minority clients. Psychiatric Services. 2003;54(4):535–541. doi: 10.1176/appi.ps.54.4.535. [DOI] [PubMed] [Google Scholar]