Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System (original) (raw)
Abstract
Our understanding of pressure injury etiology and development has grown in recent years through research, clinical expertise, and global interdisciplinary expert collaboration. Therefore, the National Pressure Ulcer Advisory Panel (NPUAP) has revised the definition and stages of pressure injury. The revision was undertaken to incorporate the current understanding of the etiology of pressure injuries, as well as to clarify the anatomical features present or absent in each stage of injury. An NPUAP-appointed Task Force reviewed the literature and created drafts of definitions, which were then reviewed by stakeholders and the public, including clinicians, educators, and researchers around the world. Using a consensus-building methodology, these revised definitions were the focus of a multidisciplinary consensus conference held in April 2016. As a result of stakeholder and public input, along with the consensus conference, important changes were made and incorporated into the new staging definitions. The revised staging system uses the term injury instead of ulcer and denotes stages using Arabic numerals rather than Roman numerals. The revised definition of a pressure injury now describes the injuries as usually occurring over a bony prominence or under a medical or other device. The revised definition of a Stage 2 pressure injury seeks to clarify the difference between moisture-associated skin damage and injury caused by pressure and/or shear. The term suspected has been removed from the Deep Tissue Pressure Injury diagnostic label. Each definition now describes the extent of tissue loss present and the anatomical features that may or may not be present in the stage of injury. These important revisions reflect the methodical and collaborative approach used to examine the available evidence and incorporate current interdisciplinary clinical expertise into better defining the important phenomenon of pressure injury etiology and development.
Keywords: Deep tissue pressure injury, Shear, Pressure injury, Pressure, Pressure ulcer, Stage 1-4, Staging System
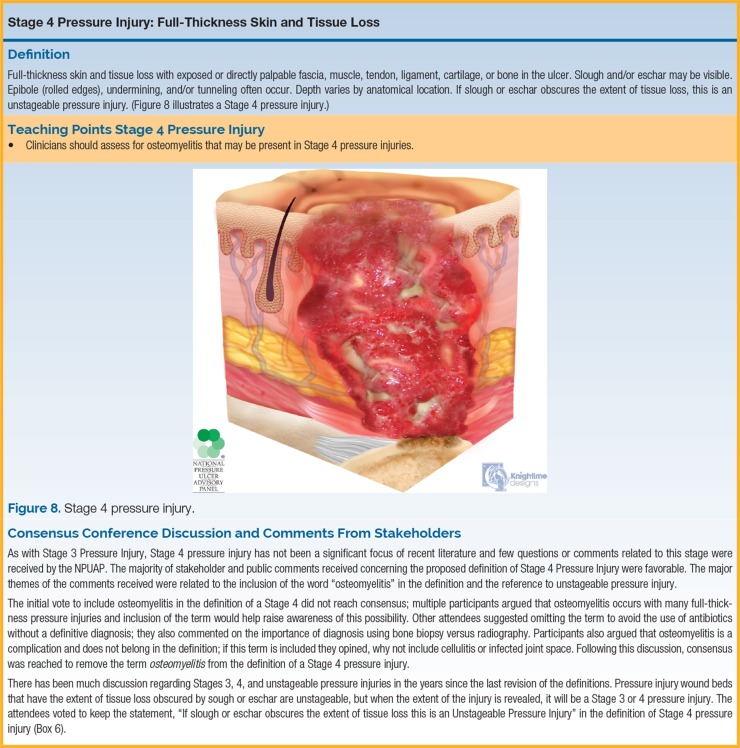
INTRODUCTION
The National Pressure Ulcer Advisory Panel (NPUAP) has revised the definition and stages of pressure injury. The revision was undertaken to incorporate the current understanding of the etiology of pressure injuries and to clarify the anatomical features present or absent in each stage of injury. An NPUAP-appointed Task Force reviewed the literature and created drafts of definitions, which were then reviewed by stakeholders and the public, including clinicians, educators, and researchers around the world. Using consensus-building methodology, these revised definitions were the focus of a multidisciplinary consensus conference held in April 2016. As a result of stakeholder and public input, along with the consensus conference, important changes were made and incorporated into the new staging definitions. The new revised staging system uses the term injury instead of ulcer and denotes stages using Arabic numerals rather than Roman numerals.
Pressure injuries are classified and described through the use of staging systems. Staging systems describe the extent of tissue loss and the physical appearance of the injury caused by pressure and/or shear. In 1975, J. D. Shea developed a staging system for the classification of pressure injuries, and in 1988, the International Association of Enterostomal Therapy (now the Wound, Ostomy and Continence Nurses Society), created a 4-stage system based on these classifications.1,2 In 1989, the NPUAP developed a pressure injury staging system, using a consensus conference model; this taxonomy was based on the International Association of Enterostomal Therapy system. In 2007, the NPUAP revised their staging system to incorporate suspected Deep Tissue Injury (sDTI) again using the consensus conference model. The first NPUAP-EPUAP International Pressure Ulcer Prevention and Treatment Guidelines (2009) further revised the staging system for international use by adding the term category/stage, which is frequently used outside the United States.3 The NPUAP's staging system has been widely adopted internationally. Pressure injury staging has become the basis for treatment, comparison of outcomes, and, if applicable, reimbursement. The NPUAP Staging System was evaluated and revised to reflect current scientific and clinical understanding of the etiology of pressure injuries, as well as to clarify and make the system more accurate and easier to use.
Only pressure injuries should be staged with the NPUAP Pressure Injury Staging System. Non–pressure-related ulcers and wounds are subject to unique staging or classification systems based upon wound type: diabetic foot ulcers (Wagner Classification System), venous leg ulcers (Clinical Etiology Anatomy Pathophysiology), skin tears (International Skin Tear Advisory Panel), adhesive or tape injuries (Medical Adhesive Related Skin Injury categories, MARSI), and burn classification (total body surface area). It is essential that the intended staging or classification system be used for each type of injury to ensure appropriate treatment. Prior to using any pressure injury staging or classification system, it is necessary to assess the patient and wound type; for example, when diagnosing a pressure injury, it is essential to confirm the presence of pressure and/or shear as a causative factor. Since the NPUAP staging system is based on the extent of tissue damage, an understanding of anatomy is essential when evaluating the type of tissue present in the wound. In order to perform an accurate visual assessment, pressure injury staging should take place only after the wound bed has been cleansed. The purpose of this article was to describe issues associated with accurate staging of pressure injuries, to report the methods undertaken to revise the NPUAP staging system, and to present the new NPUAP Staging System definitions. In addition, injuries commonly mistaken for pressure injuries are described and important teaching points are included that can be used to further explain and differentiate pressure injuries from other wounds or injuries.
Literature Review and Preliminary Revisions
In January 2015, the NPUAP Board of Directors (BOD) approved a review of the staging system. A task force was appointed to examine the current system and to review literature relevant to staging. The work of the task force resulted in a revision of the staging definitions and artwork to clarify and refine the staging system. This work also led to development of new nomenclature relevant to pressure-related soft tissue injury. The Task Force comprised Drs Laura Edsberg and Joyce Black as cochairs; Margaret Goldberg, Laurie McNichol, Lynn Moore, and Mary Sieggreen served as task force members. Task Force members have expertise, education, and credentials in the areas of nursing practice, nursing education, dietetics (nutrition), and engineering.
The interdisciplinary Task Force worked with a university-based, professional reference librarian to generate a list of search terms that identified literature related to staging pressure injuries. Multiple search terms and combinations of terms were employed. An extensive literature review was conducted to summarize the state of the science in the area of pressure injury staging, pathology, and etiology. Following the initial searches, additional terms were added based on key words identified within the references. References were limited to those published in English. They included clinical practice guidelines, randomized controlled trials, nonrandomized studies, case studies, multiple case series, in vitro studies, and in vivo (animal) studies. National and international conference findings and government Web site information were also included. There was no publication year limit and all ages of individuals from premature infants through geriatrics were included. The CINAHL and MEDLINE electronic databases were searched individually; this search yielded 3652 articles. Task Force members completed title and abstract reviews, along with full text review. Two hundred forty-two articles were deemed relevant to the task at hand. In addition, references submitted by stakeholders and the public during the comment period were retrieved and reviewed for relevance to the goals of the Task Force. This multistage literature searches revealed a dearth of literature focused on pressure injury staging definitions, supporting the need for the review.
During weekly meetings held between January 2015 and April 2016, the Task Force drafted definitions and descriptions based on new scientific findings, with the intention to clarify issues with current nomenclature. These issues are reflected in comments and questions received by the NPUAP. While regulatory compliance, documentation, and legal issues were considered, the proposed changes were based on science and expert opinion. Proposed definitions were revised based on feedback from the NPUAP BOD and expert Panel members during a panel meeting in August 2015. They were made available for feedback and comment from stakeholder organizations and individuals. More than 1800 comments were received and reviewed. Following the comment period, the definitions were again revised based on the feedback received; these revised definitions were reviewed by the full NPUAP Panel and approved by its BOD. The NPUAP has historically held a consensus conference to invite discussion of draft staging definitions. As in 1989 and 2007, the consensus conference model was used to present the 2016 draft definitions and facilitate discussion of those parts of the definitions that needed clarification or revision, based on stakeholder and public comments; it was held April 2016.
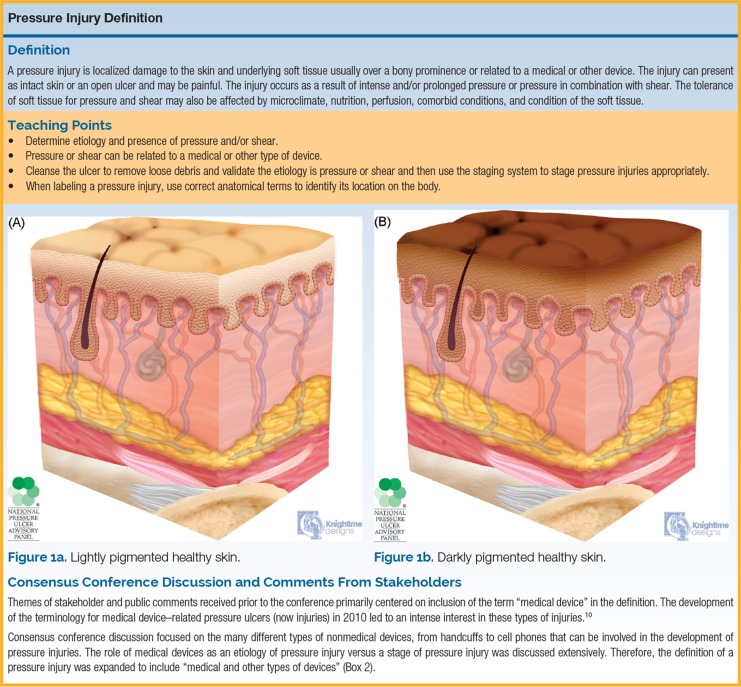
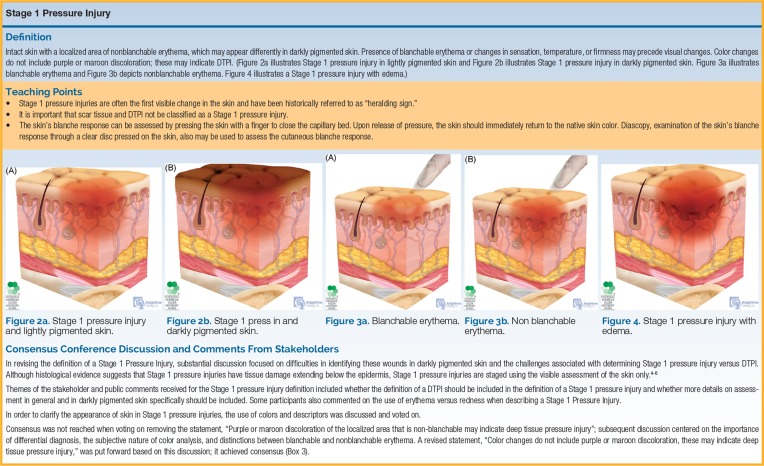
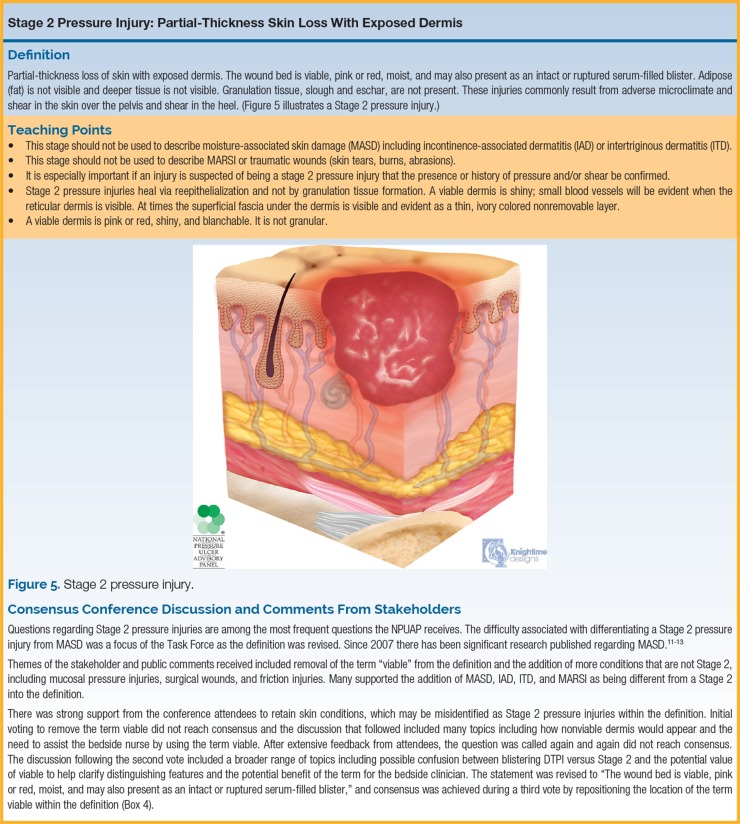
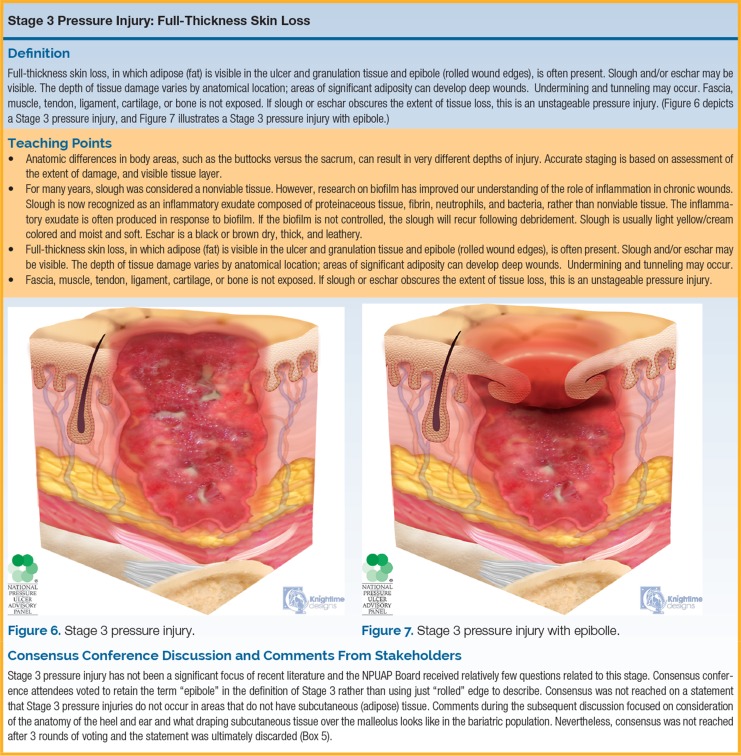
Artwork was created to illustrate the features of each stage of pressure injuries. The artwork is a graphic representation of the tissues present and is to be used for teaching about the extent of injury and the tissues present or absent within each stage of a pressure injury. The artwork was developed in parallel with the staging revisions and was subject to multiple revisions. The NPUAP BOD approved the final artwork prior to the Consensus Conference.
INITIAL REVISIONS TO STAGING SYSTEM
Ulcer Versus Injury
The 2016 NPUAP Pressure Injury Staging System uses the term injury instead of ulcer. The decision to change the term ulcer to the term injury was based on months of discussion, vigorous debate, comments received from stakeholders and individuals, and the intensive literature review described previously. As a result, it was determined that the term ulcer does not accurately describe the physical presentation of a Stage 1 Pressure Injury or a Deep Tissue Pressure Injury (DTPI). Furthermore, histopathological work indicates that small changes in pressure-related injuries start in the tissue prior to the changes being visible on physical examination.4–6 An ulcer cannot be present without an injury, but an injury can be present without an ulcer. An ulcer is defined as a break in skin or mucous membrane with loss of surface tissue, disintegration and necrosis of epithelial tissue, and often, purulent exudate.7 Langley and Brenner8 define an injury as bodily damage caused by transfer of energy and also the absence of energy. Examples of injuries caused by absence of energy are hypothermia and asphyxia. Examples of injuries caused by exposure to low energy are pressure injuries and carpel tunnel syndrome; these injuries occur without a sudden discernable effect.
The science regarding the etiology of pressure injuries has supported the role of tissue deformation, microclimate, nutrition, perfusion, and tissue tolerance.9 The pressure injury definition was revised in order to incorporate what is now understood regarding the etiology of these injuries.
Comments received from stakeholder organizations and individuals expressed overwhelming support in favor of the terminology change from ulcer to injury. The NPUAP BOD voted to change the term prior to the consensus conference based on the current science and support from the comments received. The term ulcer is used within the definition of those stages of pressure injuries that present as ulcers.
Roman Versus Arabic Numerals
Roman numerals were changed to Arabic numerals in the names of the different stages. This change was made to clarify and reduce the potential for confusion between similar terms used in health care such as a Stage IV and intravenous (IV).
Consensus Conference
The NPUAP hosted an interdisciplinary conference April 8 to 9, 2016, in Chicago, Illinois. Consensus statements were developed by the Task Force to further revise the definitions for pressure injury and the pressure injury stages, based on the most frequent comments and questions received during the comment period. All conference attendees were able to discuss and vote on each consensus statement. Approximately 400 individuals attended the conference. The interdisciplinary audience included nurses, physicians, physical therapists, dieticians, and researchers. Representatives of many national and international wound organizations participated. Mikel Gray, a Professor from the School of Medicine and School of Nursing at the University of Virginia, was invited by the NPUAP to serve as the consensus conference moderator. Dr Gray has expertise in moderating consensus conferences and is knowledgeable about, although not directly vested in, the issue of pressure injury staging.
Consensus Process
Each audience member was given a handheld audience response system device. At the start of the conference, the system was calibrated. All results from the conference reflect the positive or negative audience responses. A review of each proposed definition with rationale was presented by one of the Task Force members. The moderator then presented the consensus statements for discussion and a vote. Consensus was reached when 80% or more indicated agreement or disagreement with a particular statement. If the vote on a statement did not reach consensus, all attendees were invited to participate in a discussion moderated by Dr Gray. If needed, 2 additional votes were taken to try to reach consensus, either positively or negatively. If consensus was not reached after 3 votes, the original definition remained unchanged. Table 1 summarizes the statements that were voted on at the conference.
TABLE 1. Summary of Consensus Statements and Outcomes.
| Consensus Statement | Vote | Outcome |
|---|---|---|
| Pressure injury | ||
| Include medical device–related pressure injuries as a cause in the definition of a pressure injury. | Yes = 83%No = 17%354 votes | Consensus achieved |
| I prefer “medical device”Or “medical or other device” | 7%93%335 votes | Consensus achieved |
| Stage 1 pressure injury | ||
| Remove the statement “Purple or maroon discoloration of the localized area that is non-blanchable may indicate deep tissue pressure injury” from the description of Stage 1 pressure injury. | Yes = 44%No = 56%339 votes | Consensus not achieved |
| Remove the statement “Color changes do not include purple or maroon discoloration, these may indicate deep tissue pressure injury”. | Yes = 14%No = 86%337 votes | Consensus achieved |
| Stage 2 pressure injury | ||
| The wound bed is viable pink or red, moist, and may also present as an intact or ruptured serum-filled blister. | Yes = 97%No = 3%351 votes | Consensus achieved |
| Retain skin conditions that may be incorrectly identified as a Stage 2 pressure injury. | Yes = 92%No = 8%350 votes | Consensus achieved |
| Stage 3 pressure injury | ||
| Retain the term “epibole” in the definition of Stage 3. | Yes = 80%No = 20%345 votes | Consensus achieved |
| Include the sentence describing anatomical locations: “The bridge of the nose, ear auricle, and occiput, and malleolus do not have subcutaneous adipose/fat tissue and Stage 3 pressure injuries do not occur in these areas.” | Yes = 75%No = 25%289 votes | Consensus not achieved |
| Stage 4 pressure injury | ||
| Remove the term osteomyelitis from the definition of Stage 4. | Yes = 80%No = 20%335 votes | Consensus to remove the phrase was achieved |
| Remove the statement “If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury” from Stage 4. | Yes = 20%No = 80%341 votes | Consensus achieved |
| Unstageable pressure injury | ||
| Change “depth” to “extent” in unstageable. | Yes = 96%No = 4%321 votes | Consensus achieved |
| Stable eschar (ie, dry, adherent, intact without erythema or fluctuance) on the heel or ischemic limb should not be softened or removed. | Yes = 81%No = 19%296 votes | Consensus achieved |
| Deep tissue pressure injury | ||
| Add the phrase in italic to the definition: Wounds may evolve rapidly to reveal the actual extent of tissue injury, or may resolve without tissue loss. | Yes = 86%No = 14%346 votes | Consensus achieved |
| Place the definition of DTPI between Stage 1 and Stage 2. | Yes = 16%No = 84%353 votes | Consensus achieved |
| Add: “Do not use DTPI to describe vascular, traumatic, neuropathic, or dermatologic conditions”. | Yes = 85%No = 15%319 votes | Consensus achieved |
| Mucosal membrane pressure injury | ||
| Add the statement “The staging system for pressure injury of the skin cannot be used to stage mucosal membrane pressure injury.” to the definition of mucosal membrane pressure injury. | Yes = 98%No = 2%325 votes | Consensus achieved |
Revised NPUAP Pressure Injury Staging System
Below is a summary of the moderated and detailed discussions that occurred during the NPUAP consensus conference. The following sections summarize statements voted on at the consensus conference, key points raised during discussion, and important teaching points associated with each of the pressure injury stages. In addition, artwork for each stage is shown, as well as the final definition for each stage. Figures 1a and 1b illustrate lightly and darkly pigmented healthy skin; they provide a foundation for the additional artwork used to illustrate each of the pressure injury stages (Box 1).
BOX 1.
BOX 2.
BOX 3.
BOX 4.
BOX 5.
BOX 6.
BOX 7.
BOX 8.
BOX 9.
Validation of Staging System
After achieving consensus on the revised Staging System, photographs of various wounds were shown to the participants along with a focused patient history and physical examination findings. The audience voted on the appropriate stage represented by the photo. The results were used to determine which of the photographs provided a clear representation of the stage, and which did not; results are summarized in Table 2.
TABLE 2. Validation of Revised Staging System.
| Stage of Injury | Total Number of Responses | Stage 1a | Stage 2a | Stage 3a | Stage 4a | DTPIa | Unstageable PIa | MDRPIa | MMPIa | Not a PIa |
|---|---|---|---|---|---|---|---|---|---|---|
| 4 | 314 | 0 | 0 | 0 | 94%a | 0 | 3% | 0 | 0 | 3% |
| 4 | 290 | 0 | 19 | 2 | 56%a | 0 | 0 | 0 | 0 | 21% |
| 9 | 312 | >1% | 1% | 0 | 0 | 0 | >1% | >1% | 0 | 95%a |
| 5 | 307 | >1% | >1% | >1% | 0 | 97%a | >1% | 0 | 0 | >1% |
| 9 | 306 | 0 | 0 | 0 | 0 | 0 | 0 | 5% | >1% | 92%a |
| 4 | 316 | 0 | 0 | 3% | 86%a | 0 | 6% | 2% | 0% | 0% |
| 2 | 304 | 0 | 70%a | 22% | 0 | 0 | 0 | 0 | 0 | 4% |
| 3 | 314 | 0 | 8% | 88%a | >1% | 0 | 1% | >1% | 0 | >1% |
| 9 | 309 | 1% | 0 | 0 | 0 | >1% | 0 | 0 | >1% | 97%a |
| 1 | 311 | 97%a | 0 | 0 | 0 | 2% | 0 | 0 | 0 | 0 |
| 9 | 310 | 0 | 0 | 0 | 0 | >1% | 0 | 0 | 0 | 99%a |
| 6/7 | 303 | 0 | >1% | >1% | >1% | >1% | 33%a | 62%a | 0 | 2% |
| 9 | 302 | 0 | 0 | 0 | 0 | 2% | 0 | 0 | 0 | 97%a |
| 2 | 298 | 4% | 72%a | >1% | 0 | >1% | 0 | 0 | 1% | 21% |
| 9 | 309 | 0 | 0 | 0 | 0 | >1% | >1% | 0 | 0 | 98%a |
| 5 | 303 | 0 | 4% | 11% | 2% | 79%a | 1% | 0 | 0 | >1% |
| 2/7 | 293 | 2% | 42%a | 0 | 0 | 1% | 0 | 46%a | 0 | 8% |
| 9 | 299 | >1% | 0 | 0 | >1% | 0 | 3% | 0 | 0 | 95% |
| 6/7 | 292 | >1% | 0 | 0 | 0 | >1% | 22%a | 73%a | 0 | 2% |
| 7/8 | 275 | 0 | 2% | 1% | 0 | 0 | 0 | 53%a | 42%a | 0% |
| 1/7 | 287 | 79% | 2% | 0 | 0 | 3% | 0 | 5% | 0 | 9% |
| 7/8 | 284 | 0 | 0 | 0 | 0 | 0 | 1% | 19%a | 77%a | 2% |
| 5 | 296 | 0 | 0 | 0 | 0 | 97%a | .1% | 0 | 0 | >1% |
| 9 | 272 | >1% | 41% | 2% | 0 | 4% | 0 | 5% | 0 | 45%a |
| 6 | 287 | 0 | 1% | 5% | 0 | 0 | 90%a | 0 | 0 | 1% |
| 9 | 278 | 1% | 0 | 0 | 0 | 1% | 0 | 0 | 0 | 96%a |
| 9 | 284 | 0 | 0 | 0 | 0 | 0 | >1% | 0 | 0 | 99%a |
| 4 | 277 | 0 | 0 | 0 | 91%a | 1% | >1% | 0 | 0 | 6% |
| 2 | 272 | 4% | 90%a | 1% | 0 | 0 | 0 | >1% | 0 | 2% |
| 2 | 279 | 0 | 19%a | 61% | 17% | 0 | 0 | 0 | 0 | >1% |
| 4 | 276 | 0 | 0 | 2% | 86%a | 0 | 3% | 1% | 0 | 6% |
| 5 | 272 | 0 | 0 | 0 | 0 | 93%a | 6% | 0 | 0 | 0 |
The nonpressure injuries were most frequently scored correctly (92%-97%). The ulcers that were due to medical devices were scored most incorrectly, with respondents choosing both the stage of the injury and the label Medical Device–Related Pressure Injury. It became clear that the etiology of the injury, medical device–related, was chosen instead of the stage of the injury. To address this issue, the phrase medical or device related was defined clearly as an etiology and not a pressure injury stage during this conference. The revised medical device–related pressure injury definition now includes the directive that the injury should be staged using the staging system. Other areas of incorrect responses were deep Stage 2 ulcers with viable dermis or exposed fascia with visible capillary buds, reulcerated scar in a patient with a history of a Stage 4 ulcer in the area and chronic friction injury. Teaching points will be included in NPUAP materials to address these aspects.
CONCLUSIONS
The NPUAP Pressure Ulcer Staging System was refined, beginning with the change in terminology from pressure injury to pressure injury in order to include soft tissue injury without ulceration (Stage 1 and DTPI). Advances in the scientific understanding of how pressure injuries occur, from intense and/or prolonged pressure, were reflected in the new definition and resulted in the inclusion of medical and nonmedical devices as one of the etiologies. Arabic numbers were also incorporated to reduce confusion. Nevertheless, while the various pressure injury stages are assigned numbers, and numbers imply progression, the deterioration of a pressure injury does not predictably follow a linear evolution from Stage 1 to Stage 4. Until more clinical evidence is available, especially about the impact of pressure on levels of soft tissue and the tolerance of soft tissue for pressure and shear, clinicians cannot steadfastly state, for example, that a stage 3 had its beginnings as a stage 1 or that a stage 1 will inevitably evolve into a stage 4. Consensus was used to further clarify aspects of each of the definitions. Finally, each stage of pressure injury was validated using photographs and the new staging definitions. The revisions of the NPUAP Pressure Injury Staging System are intended to improve accuracy of pressure injury staging. The teaching points and artwork will provide clarity and added resources for clinicians.
GLOSSARY
Biofilm: Complex microbial communities containing bacteria and fungi. The microorganisms synthesize and secrete a protective matrix that attaches the biofilm firmly to a living or nonliving surface.
Blanchable: Quickly regains redness when pressure is lifted from skin (2-3 seconds)
Erythema: Redness of the skin or mucous membranes, caused by hyperemia (increased blood flow) in superficial capillaries
Eschar: Dead tissue appearing black or brown dry, thick, and leathery
Fascia: Band or sheet of connective tissue, primarily collagen, beneath the skin that attaches, stabilizes, encloses, and surrounds and separates muscles and internal organs.
IAD: incontinence-associated dermatitis
ITD: intertriginous dermatitis
MARSI: medical-adhesive–related skin injuries
MASD: moisture-associated skin damage
Microclimate: temperature, humidity, and airflow at patient/support surface
Re-epithelialization: Restoration of epithelium over a wound
Slough: Inflammatory exudate composed of proteinaceous tissue, fibrin, neutrophils, and bacteria, rather than nonviable tissue. Slough is usually light yellow/cream colored and moist and soft.
Viable dermis: Living dermal tissue
Vasopressive medication: Cause vasoconstriction (contraction of smooth muscle in blood vessels) and increase in blood pressure. They are used to treat hypotension, especially in critically ill patients.
ACKNOWLEDGMENTS
We thank Andrea Sullivan, MLS, for her expertise and guidance in searching the literature. The conference support was provided by the National Pressure Ulcer Advisory Panel.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Shea JD. Pressure sores: classification and management. Clin Orthop Relat Res. 1975;112:89–100. [PubMed] [Google Scholar]
- 2.International Association of Enterostomal Therapists. Dermal wound: pressure sores. Philosophy of the IAET. J Enterostomal Ther. 1988;15(1):4–17. [PubMed] [Google Scholar]
- 3.National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Washington, DC: National Pressure Ulcer Advisory Panel; 2009. [Google Scholar]
- 4.Witkowski JA, Parish LC. Histopathology of the decubitus ulcer. J Am Acad Derm. 1982;6:1014–1021. [DOI] [PubMed] [Google Scholar]
- 5.Arao H, Obato M, Shimada T, Hagisawa S. Morphological characteristics of the dermal papillae in the development of pressure sores. J Tissue Viability. 1998;8:17–23. [DOI] [PubMed] [Google Scholar]
- 6.Edsberg LE. Pressure ulcer tissue histology: an appraisal of current knowledge. Ostomy Wound Manage. 2007;53(10):40–49. [PubMed] [Google Scholar]
- 7.Merriam-Webster Dictionary. http://www.merriam-webster.com/dictionary/ulcer. Accessed March 15, 2016.
- 8.Langley J, Brenner R. What is an injury? Inj Prev. 2004;10(2):69–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Osborne Park, Western Australia: Cambridge Media; 2014. [Google Scholar]
- 10.Black JM, Cuddigan JE, Walko MA, Didier LA, Lander MJ, Kelpe MR. Medical device related pressure ulcers in hospitalized patients. Int Wound J. 2010;7(5):358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahoney M, Rozenboom B, Doughty D, Smith H. Issues related to accurate classification of buttocks wounds. J Wound Ostomy Continence Nurs. 2011;38(6):635–642. [DOI] [PubMed] [Google Scholar]
- 12.Doughty D, Junkin J, Kurz P, et al. Incontinence-associated dermatitis: consensus statements, evidence based guidelines for prevention and treatment, and current challenges. J Wound Ostomy Continence Nurs. 2012;39(3):303–315. [DOI] [PubMed] [Google Scholar]
- 13.McNichol L, Lund C, Rosen T, Gray M. Medical adhesives and patient safety: state of the science: consensus statements for the assessment, prevention, and treatment of adhesive-related skin injuries. J Wound Ostomy Continence Nurs. 2013;40(4):365–380. [DOI] [PubMed] [Google Scholar]
- 14.Zaratkiewicz S, Whitney JD, Baker MW, Lowe JR. Defining unstageable pressure ulcers as full-thickness wounds: are these wounds being misclassified? J Wound Ostomy Continence Nurs. 2015;42(6):583–588. 10.1097/WON.0000000000000175 [DOI] [PubMed] [Google Scholar]
- 15.Huang TT, Tseng CE, Lee TM, Yeh JY, Lai YY. Preventing pressure sores of the nasal ala after nasotracheal tube intubation: from animal model to clinical application. J Oral Maxillofac Surg. 2009;67(3):543–551. [DOI] [PubMed] [Google Scholar]
- 16.Kuo C, Wootten CT, Tyulor D, Werkhaven J, Huffman K, Goudy S. Prevention of pressure ulcers after pediatric tracheostomy using a Mepilex AG dressing. Laryngoscope. 2013;123(12):3201–3205. 10.1002/lary.24094 [DOI] [PubMed] [Google Scholar]
- 17.Weng M. The effect of protective treatment in reducing pressure ulcers for non-invasive ventilation patients. Intensive Crit Care Nurs. 2008;24(5):295–299. [DOI] [PubMed] [Google Scholar]