Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? (original) (raw)
Abstract
The pathogenesis of tendinopathy and the primary biological change in the tendon that precipitates pathology have generated several pathoaetiological models in the literature. The continuum model of tendon pathology, proposed in 2009, synthesised clinical and laboratory-based research to guide treatment choices for the clinical presentations of tendinopathy. While the continuum has been cited extensively in the literature, its clinical utility has yet to be fully elucidated. The continuum model proposed a model for staging tendinopathy based on the changes and distribution of disorganisation within the tendon. However, classifying tendinopathy based on structure in what is primarily a pain condition has been challenged. The interplay between structure, pain and function is not yet fully understood, which has partly contributed to the complex clinical picture of tendinopathy. Here we revisit and assess the merit of the continuum model in the context of new evidence. We (1) summarise new evidence in tendinopathy research in the context of the continuum, (2) discuss tendon pain and the relevance of a model based on structure and (3) describe relevant clinical elements (pain, function and structure) to begin to build a better understanding of the condition. Our goal is that the continuum model may help guide targeted treatments and improved patient outcomes.
Keywords: Tendon
The continuum of tendon pathology1 has been cited over 250 times since publication in 2009. The original paper condensed clinical and laboratory-based research into a model of tendon pathology designed to help clinicians understand the various presentations of tendinopathy and to allow rational placement of interventions based on the continuum. Although the continuum was based on evidence from lower limb tendons, it has been adapted for rotator cuff2 and equine tendon pathology.3 The original paper suggested that the model should be tested against further developments in the clinical and research environment to assess its relevance. Seven years later, we reflect on the relevance of the model to sports medicine and physiotherapy. The main questions that have been raised since the continuum was proposed are:
- What is the relevance of tendon structure and pathology in what is primarily a painful condition?
- What is the relationship between structure, pain and function?
- How should tendon pain be considered as part of the continuum?
- Is the response to load normal adaptation or a pathological process?
- How can the continuum guide clinical treatment?
Three categories of pathoaetiology models and the relation of structure to pain
The continuum model is one of several models on the pathoaetiology of tendon pathology.1 4–7 These tendon pathology models can be divided into three groups depending on the primary or key event in the pathology ‘cascade’: (1) collagen disruption/tearing, (2) inflammation or (3) tendon cell response. Several other models have attempted to integrate pain and the central nervous system with pathology.8 9
The complexity of normal tendon structure, the multifaceted nature and magnitude of the tendon’s response to injury, and the difficulty in creating an experimental model that mimics load-related tendon pathology in humans make it difficult to construct a simple and robust model that accommodates all aspects and phases of the condition. There are key arguments for and against all these models, as well as commonalities among models (http://tinyurl.com/zkzza9x).
Collagen disruption/tearing model
The collagen tearing hypothesis is the oldest and perhaps the most open to challenge because normal collagen fibres cannot tear in vivo without substantial alterations in the non-collagenous matrix.10 The longevity of normal tendon collagen suggests that collagen tearing and remodelling does not occur as a result of loading.11 12 Recent publications cite early changes more as fibre kinking and a ‘loosening’ of the collagenous matrix.13–15 As such, in vivo animal models of tendinopathy based on collagen disruption theory (collagenase injection, tendon laceration) have limited relevance to human tendinopathy.
On the basis of the collagen disruption/tearing concept, Arnoczky et al5 proposed that tendon pathology may be driven by understimulation of the tendon cell due to a lack of load transmission through the torn collagen fibres. While collagen tearing may not be the primary event in tendon pathology, understimulation of the tendon cell may play a role in degenerative pathology. Regions of the degenerative tendon may be mechanically silent (ie, unable to transmit and sense tensile load) and thus potentially unresponsive to load due to fibrillar disorganisation. This lack of tendon cell stimulus may explain the limited reversibility of degenerative tendon pathology16 and lack of remodelling following exercise-based interventions.17
Inflammatory model
The role of inflammation in the tendon's response to overuse is complex.18 A classic inflammatory response in the tendon is seen when a tendon (and its blood supply) is ruptured or lacerated. The tissue response to such an insult is profound19—a large immune cell and tenocyte response increases protein production and tendon size.
While inflammatory cells have been observed in pathological tendons,20–23 the response does not seem to be a traditional inflammatory response.24 25 Increases in inflammatory cytokines (eg, COX-2, PGE-2, interleukin (IL)-6, IL-1β, transforming growth factor (TGF)-β) have been reported in overuse tendinopathy;26–29 however, the presence of these substances does not necessarily support the contention that inflammation is the primary event or key driver of tendon pathology (figure 1). Changes in the levels of inflammatory markers (vascular endothelial growth factor, COX-2, TGF-α and TGF-β, PGE-2, IL-1, IL-6) occur in response to cyclic load; tendon cell culture studies suggest that these cytokines are expressed by the resident tenocytes.29–33
Figure 1.
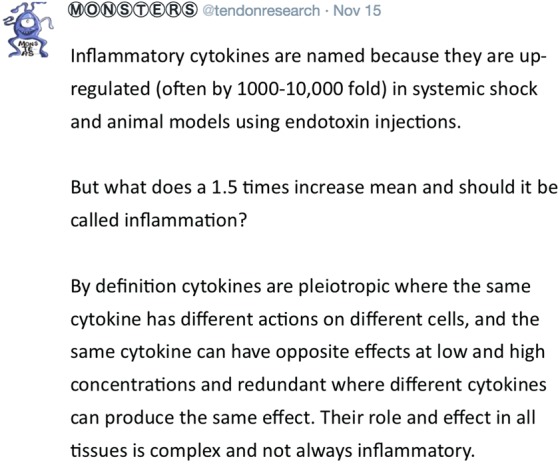
What is inflammation? Courtesy Dr James Gaida.
The elevation in inflammatory cytokines observed in tendon pathology may reflect tendon cell signalling in response to mechanical stimuli resulting in an alteration in tendon synthesis and degradation.34 An imbalance between synthesis and degradation may lead to tendon disorganisation.11 35 While it may appear that the inflammatory models and the continuum of pathology are distinct, they may not be mutually exclusive. A tendon cell is mechanoresponsive, releasing cytokines in response to overload that then stimulate matrix remodelling (degradation and synthesis).
Tendon cell response model
The tenocyte is primarily responsible for maintaining the extracellular matrix in response to its environment. Thus, changes in tendon load and biochemical milieu will be sensed by the tendon cell and result in a cascade of responses (cell activation, proteoglycan expression and changes in collagen type).36 37 Similarly, a tendon cell-based response logically explains the tendon's adaptation to compressive loads that occurs in the development of fibrocartilage within wrap-around tendons,38 or with transient (direct blow)39 or chronic (entheseal pathology) overload.40 It is unclear how collagen disruption/tearing models of tendon pathology account for these features.
What is the relationship between structure, pain and function?
The aim of the 2009 continuum model was threefold: (1) to express the varied capability of pathological tendons to recover structure, (2) to discuss the structural factors that limit return to pain-free function and (3) to propose interventions tailored to the stage of pathology. While the stages of the continuum are primarily based on structural features, it does not suggest that there is a direct relationship between structure, pain and dysfunction. In conceptualising the relationship between pain and structural change, intratendinous pathology may best be regarded as a risk factor for tendinopathy (defined as the clinical presentation of pain and dysfunction independent of structural pathology). Various prospective (relative risk 14.6; 95% CI 1.9 to 111.4)41 and cross-sectional studies (OR ranging from 3.9 to 16.2)42 43 have demonstrated that underlying structural pathology increases the risk of developing symptoms. Interestingly, progression and worsening of tendon pathology over time appears to be a greater risk factor for the development of pain than the absolute extent of pathology itself.44
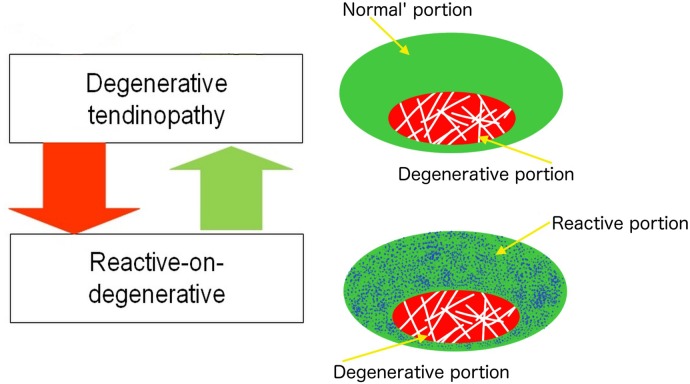
While not represented in the schematic of the continuum model, the concept that ‘some tendons may have discrete regions that are in different stages at the one time’.1 In revisiting the continuum, we have emphasised the important clinical presentation that is a hybrid of reactive and degenerative pathology, which is ‘reactive-on-degenerative tendinopathy’ (figure 2). This refers to clinical cases where the structurally normal (to conventional imaging modalities at least) portion of the tendon may drift in and out of a reactive response (figure 2).45 As discussed above, the degenerative portions of the tendon appear mechanically silent and structurally unable to transmit tensile load, which may result in overload in the normal portion of the tendon.46 Better imaging modalities and prospective studies are needed to identify the structural factors (ie, amount of disorganisation, variability in structure over time) that are important in the development of pain.
Figure 2.
Schematic representation of ‘reactive-on-degenerative’ tendinopathy. A representation an example of the presentation on (ultrasound tissue characterisation is presented by Rudavsky and Cook.45
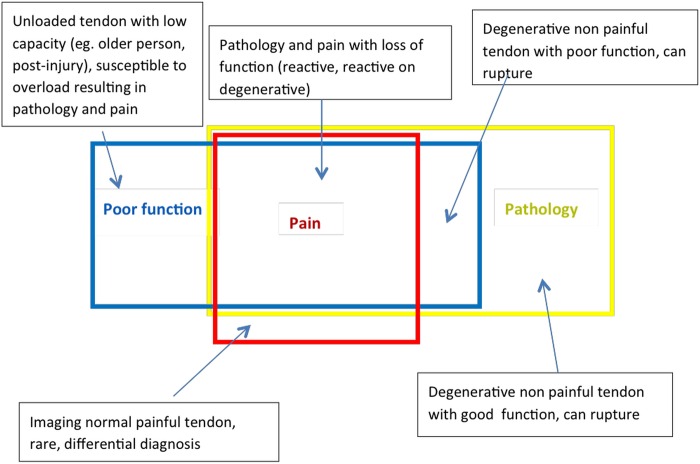
There are clear associations and dissociations between structure, pain and function, and a number of reviews have focused on this complex relationship in tendons.8 9 Tendon pain is partly related to function, with tendinopathy decreasing muscle strength and motor control, which in turn reduces function.47 48 Function in this context refers to the ability of the muscle to repeatedly generate appropriate force that enables the tendon to store and release energy for athletic movement. However, changes in function also occur in the presence of structural pathology, independent of pain. This highlights the complex interplay among structure, pain and function.49 50 The clinical presentation and quiescent changes in pain, structure and function can be linked as depicted in figure 3.
Figure 3.
Relationship between structure, function and pain. The relative sizes of the boxes may vary from tendon to tendon.
Where does tendon pain fit in the continuum model?
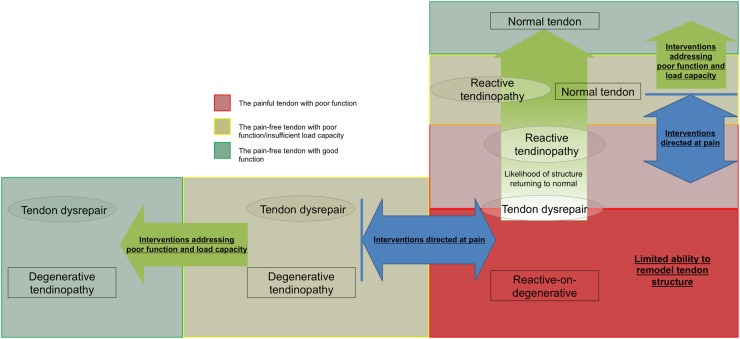
Clinically, tendon pain presentations fall into two categories in the continuum model: (1) reactive tendon with a first presentation of tendon pain following acute overload and (2) reactive-on-late dysrepair/degenerative tendon pathology (figure 4). This strongly suggests that reactive tendon pathology has a local nociceptive driver.
Figure 4.
Schematic representation of how we may phenotype patients with tendinopathy in relation to the continuum and target treatments. The aim of treatment is to push the tendon into the green section with relatively little pain and good function. Tendon structure can be normalised in the early stages of the continuum where rehabilitation can push the tendon ‘up the continuum’. In the latter stages of the continuum, ‘moving up the continuum’ may not be possible, so interventions should be focused in ‘moving the tendon sideways’. It is important to note that interventions directed solely at pain will not drive the tendon to a positive outcome as they do not address dysfunction, such as motor inhibition, strength and power deficits, or tendon load capacity. Interventions that target structure may improve tendon structure and direct the tendon ‘upwards along the continuum’; however, it will not address functional deficits (effect on pain is inconclusive) or load capacity and may leave the tendon vulnerable to reinjury.
The identity of the nociceptive driver in tendinopathy remains elusive. The strong relationship between tendon pain and mechanical load, together with the mechanoresponsiveness of tenocytes and lack of sensory innervation of the deep tendon tissue, may implicate paracrine signalling by the tendon cells as a potential driver of nociception51 These substances may sensitise peripheral mechanoreceptors near or in the peritendon52 stimulating the peripheral nerve and be interpreted as pain. This may explain why pathology can occur deeper in tendons without tendon pain as this region is remote to the nerve supply. Theoretically, a painful reactive or reactive-on-degenerative tendon may increase expression of nociceptive substances and their receptors, stimulating the peripheral nerve and be interpreted as pain. Diffuse reactive pathology may also irritate the peritendon due to an increase in tendon size.
The pain-free tendon may contain substantial matrix and cell abnormalities, but limited nociceptive substance production, signalling ability or receptor activation, which is in summary an insufficient nociceptive stimulus. The role of the central nervous system in the modulation of nociception and output of pain is acknowledged and well described by others;8 53 however, it is beyond the scope of this paper.
Loading a painful tendon perpetuates nociceptive stimuli, and it is plausible that secondary hyperalgesia in tendinopathy is a response to ongoing nociception. Hyperalgesia by itself does not define tendinopathy as a pathophysiological pain state or centrally driven phenomenon.51 Several clinical features support this concept; tendon pain remains localised and temporally linked to tissue loading,54 with little evidence of spontaneous tendon pain (stimulus-independent pain) that is a feature of other pathophysiological pain states.
Some consider tendinopathy to be centrally driven, while also questioning the relevance of local changes in tendon structure. While there is evidence of contralateral sensory perception changes in people with tendinopathy,55 this can equally reflect persistent nociceptive drive from the local tissue. Acute pain conditions, such as acute inversion ankle sprain, also caused secondary hyperalgesia;56 however, this can be reversed instantaneously with an anaesthetic. This suggests that the nociceptive input from the periphery maintains sensitisation.57 Unilateral isometric exercises in patellar tendinopathy have no effect on contralateral pain,58 suggesting that local factors or pathways are critical in pain production. In summary, we acknowledge that there is good evidence for adaptations (both motor and sensory) in tendinopathy, yet we cannot dismiss the role of local nociceptively driven pain.
Is a response to load part of an adaptive or pathological process?
Normal tendon tissue responds to load with both synthesis and degradation of the matrix; however, turnover rates vary depending on the protein.59–61 Collagen turnover is minimal after skeletal maturity,11 12 whereas non-collagenous substances, such as proteoglycans, are synthesised and degraded much more quickly (days), suggesting that they may be a critical component in early pathological or adaptive changes.12
We proposed that reactive pathology (as defined in the model) results in an increase in large proteoglycans but further consideration and recent studies suggest that there must be an earlier phase that is less intense and potentially transient. The Achilles tendon62 and superficial digital flexor tendon in the horse63 undergo a definite but subtle structural response on imaging 2 days after high loads that returned to normal by day 4. The time course of these changes in imaging appearance (ultrasound tissue characterisation (UTC) echopattern) is similar to that of the 2–3 days it takes to express and break down large proteoglycans such as aggrecan.64–67 A similar response is seen using MRI—this suggests an increase in large proteoglycans and associated bound water in response to high load exercise.68 It is unclear whether these changes are adaptive or pathological and whether they have a lasting effect on the health of the tendon (in reference to pain).
The normal Achilles tendon improves in structure as seen using UTC69 over the course of an elite Australian football preseason; this supports the adaptive pathway suggested within the continuum.70 However, in this same cohort, 3 out of the 18 participants progressed to a reactive pathology, that is, structure deteriorated and pain developed. This highlights that the effect of load on tendon structure may vary depending on intrinsic risk factors (genetics, adiposity, age, etc) and other features within loading history.71 Load magnitude and recovery time, as well as numerous other factors (type and consistency of load stimulus), may influence tendon response and the progression along the continuum.35 Furthermore, it also highlights the difficulty in attempting to dichotomise the tendon's response as being pathological or adaptive, as these changes are likely to fall within a greater continuum.
How would the practitioner choose a treatment based on the continuum?
The continuum model suggested that management may be optimised by tailoring interventions to the stage of pathology and targeting the primary driver (cell activation) and inter-related alterations in matrix integrity. While exercise and load management are fundamental to management, a plethora of intratendinous and peritendinous interventions exist to ‘treat’ tendinopathy—this increases the complexity of the clinical decision-making process.
Tendinopathy is a heterogeneous clinical presentation due to the variable change in matrix structure, pain and dysfunction.9 Phenotyping of patients based on structure, pain, dysfunction and load capacity may allow the clinician to direct appropriate treatments at the critical limiting factors (figure 4).
Interventions targeting pain
Patients with tendinopathy present clinically primarily due to pain, with available interventions directed at the painful tendon including non-steroidal anti-inflammatory drugs, corticosteroid injections,72 extracorporeal shockwave therapy,73 extratendinous high volume injection74 and surgical scraping.75 While the majority of these treatments reduce pain in the short to medium term, the longer term efficacy of some has been questioned.72 Addressing pain is critical; however, interventions directed solely at pain have a minimal effect on the associated kinetic chain deficits or tissue capacity and may result in the recurrence of pain (figure 4).55
Interestingly, isometric quadriceps muscle contractions in patellar tendinopathy induce immediate analgesia and reduce cortical inhibition of the muscle, which in turn improves strength.58 Intervening with a loading programme also has the advantage of benefiting the tendon,76 the muscle,77 as well as the cortical control of that muscle, which may lead to improvements in function and a positive clinical outcome. An incremental load-based rehabilitation programme is capable of modifying the balance of excitability and inhibition in muscle control,78 thus altering the loads transmitted by the tendon.
Interventions addressing function and load capacity
There are few papers that investigate dysfunction in tendinopathy because pain and structure have been deemed to be more important. It is also difficult in the clinic to quantify function and the tendon's load capacity, where pure measures of strength may not reflect the whole picture (see separate paper on ‘Capacity’ in BJSM79). There can be alterations to the graded recruitment of muscles associated with tendinopathy leading to changes in function.58 Return to sport is potentially a measure of function and load capacity, though most research has been conducted outside of the competitive season. While addressing pain may remove a barrier for improving function, dysfunction including persistent deficits in muscle performance or the kinetic chain, as well as insufficient tendon load capacity, may well predispose the tendon to reinjury (figure 4). Further research is needed to better characterise the functional deficits associated with tendinopathy and develop useful tools for the clinician.
Interventions targeting structure
The continuum model1 provided a framework to understand the potential of the tendon to regain normal structure. This particularly applies to the reactive stage (figure 4) of the model where it remains possible for the tendon to regain its normal structure with optimal management.16 Treatments that may dampen tendon cell response at this stage (unloading, medication directed at inhibiting the cell and resultant matrix changes) may also reduce pain, although this is yet to be substantiated. Notably, heavy load eccentric exercises or intratendinous injections may be highly provocative and deleterious within this reactive stage.
In degenerative tendinopathy, interventions influencing tendon structure are less critical, as the pathology appears to have limited reversibility. Although the original continuum paper suggested that treatments should focus on stimulating the cell to produce collagen (in the degenerative region) and restructure the matrix, it has since been demonstrated that interventions designed to change structure do not necessarily result in these improvements.17
Furthermore, the pathological tendon appears to effectively compensate for areas of disorganisation by increasing in cross-sectional dimension to maintain sufficient volumes of aligned fibrillar structure.80 Since the degenerative tendon has sufficient levels of load-bearing tissue, and given the limited ability of the tendon to reverse the pathology, treatment strategies should be directed at optimising adaptation of the tendon as a whole (figure 4). Specifically, treatment at this stage should aim to build load capacity in the aligned fibrillar matrix portion of the tendon rather than attempting to stimulate healing in the degenerative portion.
While the continuum classifies tendons based on the extent/presence of structural disorganisation, targeting treatments at regenerating the area of disorganisation may be futile as the tendon may have already compensated, or be in the process of doing so. This conceptual shift may be explained by the metaphor, treat the doughnut (area of aligned fibrillar structure), not the hole (area of disorganisation). However, sufficient aligned tissue of itself will not protect from further episodes of reactive pathology; to achieve this, management must progress to improving the load capacity of the ‘doughnut’ through a progressive loading rehabilitation.
In this context, it is difficult to find relevance for treatments directed at repairing tendons and normalising structure through the addition of growth stimulants (eg, platelet-rich plasma),81 which do not appear appropriate for the pathological process at any of the continuum stages. It should also be recognised that there is a hyperactive tendon cell response, as well as an increase in tendon cell numbers, in all stages of tendinopathy, even in the degenerative stage.64 The addition of additional cells (stem or tenocytes) into a hypercellular environment would appear counter-intuitive, as the ability to recreate a viable cell–matrix relationship is limited in a frankly degenerative region of the tendon that is unable to transmit tension.
Discussion and future directions
Regardless of the initiating event (overstimulation of resident tenocyte, collagen disruption/tearing, inflammation), tendon pathology is characterised by a significant cell response to injury.7 82 It is unlikely that any one model fully explains all aspects of the pathoaetiology of tendon pathology and its links to pain and function, as these processes and relationships are complex.
Equivocal clinical intervention outcomes from research that may well be due to heterogeneity in the research cohorts. Subgrouping by tendon pathology for clinical trials may give clearer outcomes and better clinical guidance.
The capacity to test the continuum in humans is limited in part by the capacity of present imaging modalities to detect pathological and structural changes, along with the need for a deeper understanding and greater precision in the measurement of the various aspects of pain and associated dysfunction in tendinopathy. The requirement to better comprehend these inter-relationships in time should guide effective management through considered interventions across the spectrum of presentations. The history of biomedical research would remind us that this paper, as with many of our colleagues, are just a part of the very long and complex journey in the better understanding of this challenging condition.
Footnotes
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med 2009;43:409–16. 10.1136/bjsm.2008.051193 [DOI] [PubMed] [Google Scholar]
- 2.Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. Br J Sports Med 2010;44:918–23. 10.1136/bjsm.2008.054817 [DOI] [PubMed] [Google Scholar]
- 3.Patterson-Kane JC, Becker DL, Rich T. The pathogenesis of tendon microdamage in athletes: the horse as a natural model for basic cellular research. J Comp Pathol 2012;147:227–47. 10.1016/j.jcpa.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 4.Fu SC, Rolf C, Cheuk YC, et al. . Deciphering the pathogenesis of tendinopathy: a three-stages process. Sports Med Arthrosc Rehabil Ther Technol 2010;2:30 10.1186/1758-2555-2-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnoczky SP, Lavagnino M, Egerbacher M. The mechanobiological aetiopathogenesis of tendinopathy: is it the over-stimulation or the under-stimulation of tendon cells? Int J Exp Pathol 2007;88:217–26. 10.1111/j.1365-2613.2007.00548.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abate M, Gravare-Silbernagel K, Siljeholm C, et al. . Pathogenesis of tendinopathies: inflammation or degeneration? Arthritis Res Ther 2009;11:235 10.1186/ar2723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leadbetter WB. Cell-matrix response in tendon injury. Clin Sports Med 1992;11:533–78. [PubMed] [Google Scholar]
- 8.Littlewood C, Malliaras P, Bateman M, et al. . The central nervous system—an additional consideration in ‘rotator cuff tendinopathy’ and a potential basis for understanding response to loaded therapeutic exercise. Man Ther 2013;18:468–72. 10.1016/j.math.2013.07.005 [DOI] [PubMed] [Google Scholar]
- 9.Coombes BK, Bisset L, Vicenzino B. A new integrative model of lateral epicondylalgia. Br J Sports Med 2009;43:252–8. 10.1136/bjsm.2008.052738 [DOI] [PubMed] [Google Scholar]
- 10.Screen HRC, Shelton JC, Chhaya VH, et al. . The influence of noncollagenous matrix components on the micromechanical environment of tendon fascicles. Ann Biomed Eng 2005;33:1090–9. 10.1007/s10439-005-5777-9 [DOI] [PubMed] [Google Scholar]
- 11.Heinemeier KM, Schjerling P, Heinemeier J, et al. . Lack of tissue renewal in human adult Achilles tendon is revealed by nuclear bomb (14)C. FASEB J 2013;27:2074–9. 10.1096/fj.12-225599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thorpe CT, Streeter I, Pinchbeck GL, et al. . Aspartic acid racemization and collagen degradation markers reveal an accumulation of damage in tendon collagen that is enhanced with aging. J Biol Chem 2010;285:15674–81. 10.1074/jbc.M109.077503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fung DT, Wang VM, Laudier DM, et al. . Subrupture tendon fatigue damage. J Orthop Res 2009;27:264–73. 10.1002/jor.20722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shepherd JH, Riley GP, Screen HR. Early stage fatigue damage occurs in bovine tendon fascicles in the absence of changes in mechanics at either the gross or micro-structural level. J Mech Behav Biomed 2014;38:163–72. 10.1016/j.jmbbm.2014.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pingel J, Lu Y, Starborg T, et al. . 3-D ultrastructure and collagen composition of healthy and overloaded human tendon: evidence of tenocyte and matrix buckling. J Anat 2014;224:548–55. 10.1111/joa.12164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malliaras P, Purdam C, Maffulli N, et al. . Temporal sequence of greyscale ultrasound changes and their relationship with neovascularity and pain in the patellar tendon. Br J Sports Med 2010;44:944–7. 10.1136/bjsm.2008.054916 [DOI] [PubMed] [Google Scholar]
- 17.Drew BT, Smith TO, Littlewood C, et al. . Do structural changes (eg, collagen/matrix) explain the response to therapeutic exercises in tendinopathy: a systematic review. Br J Sports Med 2014;48:966–72. 10.1136/bjsports-2012-091285 [DOI] [PubMed] [Google Scholar]
- 18.Rees JD, Stride M, Scott A. Tendons—time to revisit inflammation. Br J Sports Med 2014;48:1553–7. 10.1136/bjsports-2012-091957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedrich T, Schmidt W, Jungmichel D, et al. . Histopathology in rabbit Achilles tendon after operative tenolysis (longitudinal fiber incisions). Scand J Med Sci Sports 2001;11:4–8. 10.1034/j.1600-0838.2001.011001004.x [DOI] [PubMed] [Google Scholar]
- 20.Schubert TE, Weidler C, Lerch K, et al. . Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis 2005;64:1083–6. 10.1136/ard.2004.029876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kragsnaes MS, Fredberg U, Stribolt K, et al. . Stereological quantification of immune-competent cells in baseline biopsy specimens from Achilles tendons: results from patients with chronic tendinopathy followed for more than 4 years. Am J Sports Med 2014;42:2435–45. 10.1177/0363546514542329 [DOI] [PubMed] [Google Scholar]
- 22.Millar NL, Hueber AJ, Reilly JH, et al. . Inflammation is present in early human tendinopathy. Am J Sports Med 2010;38:2085–91. 10.1177/0363546510372613 [DOI] [PubMed] [Google Scholar]
- 23.Dean BJ, Gettings P, Dakin SG, et al. . Are inflammatory cells increased in painful human tendinopathy? A systematic review. Br J Sports Med 2016;50:216–20. 10.1136/bjsports-2015-094754 [DOI] [PubMed] [Google Scholar]
- 24.Khan KM, Bonar F, Desmond PM, et al. . Patellar tendinosis (jumper's knee): findings at histopathologic examination, US, and MR imaging. Victorian Institute of Sport Tendon Study Group. Radiology 1996;200:821–7. 10.1148/radiology.200.3.8756939 [DOI] [PubMed] [Google Scholar]
- 25.Scott A, Khan KM, Cook JL, et al. . What is “inflammation”? Are we ready to move beyond Celsus? Br J Sports Med 2004;38:248–9. 10.1136/bjsm.2003.011221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fenwick SA, Hazleman BL, Riley GP. The vasculature and its role in the damaged and healing tendon. Arthritis Res 2002;4:252–60. 10.1186/ar416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaida JE, Bagge J, Purdam C, et al. . Evidence of the TNF-alpha system in the human Achilles tendon: expression of TNF-alpha and TNF receptor at both protein and mRNA levels in the tenocytes. Cells Tissues Organs 2012;196:339–52. 10.1159/000335475 [DOI] [PubMed] [Google Scholar]
- 28.Gotoh M, Hamada K, Yamakawa H, et al. . Significance of granulation tissue in torn supraspinatus insertions: an immunohistochemical study with antibodies against interleukin-1 beta, cathepsin D, and matrix metalloprotease-1. J Orthop Res 1997;15:33–9. 10.1002/jor.1100150106 [DOI] [PubMed] [Google Scholar]
- 29.Legerlotz K, Jones ER, Screen HR, et al. . Increased expression of IL-6 family members in tendon pathology. Rheumatology (Oxford) 2012;51:1161–5. 10.1093/rheumatology/kes002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mousavizadeh R, Khosravi S, Behzad H, et al. . Cyclic strain alters the expression and release of angiogenic factors by human tendon cells. PLoS ONE 2014;9:e97356 10.1371/journal.pone.0097356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maeda T, Sakabe T, Sunaga A, et al. . Conversion of mechanical force into TGF-beta-mediated biochemical signals. Curr Biol 2011;21:933–41. 10.1016/j.cub.2011.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Devkota AC, Weinhold PS. Prostaglandin E(2), collagenase, and cell death responses depend on cyclical load magnitude in an explant model of tendinopathy. Connect Tissue Res 2010;51:306–13. 10.3109/03008200903318261 [DOI] [PubMed] [Google Scholar]
- 33.Li Z, Yang G, Khan M, et al. . Inflammatory response of human tendon fibroblasts to cyclic mechanical stretching. Am J Sports Med 2004;32:435–40. 10.1177/0095399703258680 [DOI] [PubMed] [Google Scholar]
- 34.Kjaer M, Bayer ML, Eliasson P, et al. . What is the impact of inflammation on the critical interplay between mechanical signaling and biochemical changes in tendon matrix? J Appl Physiol 2013;115:879–83. 10.1152/japplphysiol.00120.2013 [DOI] [PubMed] [Google Scholar]
- 35.Magnusson SP, Langberg H, Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Rev Rheumatol 2010;6:262–8. 10.1038/nrrheum.2010.43 [DOI] [PubMed] [Google Scholar]
- 36.Cook JL, Feller JA, Bonar SF, et al. . Abnormal tenocyte morphology is more prevalent than collagen disruption in asymptomatic athletes’ patellar tendons. J Orthop Res 2004;22:334–8. 10.1016/j.orthres.2003.08.005 [DOI] [PubMed] [Google Scholar]
- 37.Hamilton B, Purdam C. Patellar tendinosis as an adaptive process: a new hypothesis. Br J Sports Med 2004;38:758–61. 10.1136/bjsm.2003.005157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Benjamin M, Ralphs JR. Fibrocartilage in tendons and ligaments—an adaptation to compressive load. J Anat 1998;193(Pt 4):481–94. 10.1046/j.1469-7580.1998.19340481.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Docking S, Samiric T, Scase E, et al. . Relationship between compressive loading and ECM changes in tendons. Muscles Ligaments Tendons J 2013;3:7–11. 10.11138/mltj/2013.3.1.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cook JL, Purdam C. Is compressive load a factor in the development of tendinopathy? Br J Sports Med 2012;46:163–8. 10.1136/bjsports-2011-090414 [DOI] [PubMed] [Google Scholar]
- 41.Malliaras P, Cook J. Patellar tendons with normal imaging and pain: change in imaging and pain status over a volleyball season. Clin J Sport Med 2006;16:388–91. 10.1097/01.jsm.0000244603.75869.af [DOI] [PubMed] [Google Scholar]
- 42.Khan KM, Forster BB, Robinson J, et al. . Are ultrasound and magnetic resonance imaging of value in assessment of Achilles tendon disorders? A two year prospective study. Br J Sports Med 2003;37:149–53. 10.1136/bjsm.37.2.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leung JL, Griffith JF. Sonography of chronic Achilles tendinopathy: a case-control study. J Clin Ultrasound 2008;36:27–32. 10.1002/jcu.20388 [DOI] [PubMed] [Google Scholar]
- 44.Mall NA, Kim HM, Keener JD, et al. . Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am 2010;92:2623–33. 10.2106/JBJS.I.00506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rudavsky A, Cook J. Physiotherapy management of patellar tendinopathy (jumper's knee). J Physiother 2014;60:122–9. 10.1016/j.jphys.2014.06.022 [DOI] [PubMed] [Google Scholar]
- 46.Thornton GM, Hart DA. The interface of mechanical loading and biological variables as they pertain to the development of tendinosis. J Musculoskelet Neuronal Interact 2011;11:94–105. [PubMed] [Google Scholar]
- 47.Silbernagel KG, Gustavsson A, Thomeé R, et al. . Evaluation of lower leg function in patients with Achilles tendinopathy. Knee Surg Sports Traumatol Arthrosc 2006;14:1207–17. 10.1007/s00167-006-0150-6 [DOI] [PubMed] [Google Scholar]
- 48.Silbernagel KG, Nilsson-Helander K, Thomeé R, et al. . A new measurement of heel-rise endurance with the ability to detect functional deficits in patients with Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc 2010;18:258–64. 10.1007/s00167-009-0889-7 [DOI] [PubMed] [Google Scholar]
- 49.Edwards S, Steele JR, McGhee DE, et al. . Landing strategies of athletes with an asymptomatic patellar tendon abnormality. Med Sci Sports Exerc 2010;42:2072–80. 10.1249/MSS.0b013e3181e0550b [DOI] [PubMed] [Google Scholar]
- 50.Mann KJ, Edwards S, Drinkwater EJ, et al. . A lower limb assessment tool for athletes at risk of developing patellar tendinopathy. Med Sci Sports Exerc 2013;45:527–33. 10.1249/MSS.0b013e318275e0f2 [DOI] [PubMed] [Google Scholar]
- 51.Rio E, Moseley L, Purdam C, et al. . The pain of tendinopathy: physiological or pathophysiological? Sports Med 2014;44:9–23. 10.1007/s40279-013-0096-z [DOI] [PubMed] [Google Scholar]
- 52.Danielson P, Alfredson H, Forsgren S. Immunohistochemical and histochemical findings favoring the occurrence of autocrine/paracrine as well as nerve-related cholinergic effects in chronic painful patellar tendon tendinosis. Microsc Res Tech 2006;69:808–19. 10.1002/jemt.20351 [DOI] [PubMed] [Google Scholar]
- 53.Moseley GL. Reconceptualising pain according to modern pain science. Phys Ther Rev 2007;12:169–78. 10.1179/108331907X223010 [DOI] [Google Scholar]
- 54.Ferretti A. Epidemiology of jumper's knee. Sports Med 1986;3:289–95. 10.2165/00007256-198603040-00005 [DOI] [PubMed] [Google Scholar]
- 55.Heales LJ, Lim EC, Hodges PW, et al. . Sensory and motor deficits exist on the non-injured side of patients with unilateral tendon pain and disability—implications for central nervous system involvement: a systematic review with meta-analysis. Br J Sports Med 2014;48:1400–6. 10.1136/bjsports-2013-092535 [DOI] [PubMed] [Google Scholar]
- 56.Ramiro-González MD, Cano-de-la-Cuerda R, De-la-Llave-Rincón AI, et al. . Deep tissue hypersensitivity to pressure pain in individuals with unilateral acute inversion ankle sprain. Pain Med 2012;13:361–7. 10.1111/j.1526-4637.2011.01302.x [DOI] [PubMed] [Google Scholar]
- 57.Verne NG, Robinson ME, Vase L, et al. . Reversal of visceral and cutaneous hyperalgesia by local rectal anesthesia in irritable bowel syndrome (IBS) patients. Pain 2003;105:223–30. 10.1016/S0304-3959(03)00210-0 [DOI] [PubMed] [Google Scholar]
- 58.Rio E, Kidgell D, Purdam C, et al. . Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med 2015;49:1277–83. 10.1136/bjsports-2014-094386 [DOI] [PubMed] [Google Scholar]
- 59.Olesen JL, Heinemeier KM, Gemmer C, et al. . Exercise-dependent IGF-I, IGFBPs, and type I collagen changes in human peritendinous connective tissue determined by microdialysis. J Appl Physiol 2007;102:214–20. 10.1152/japplphysiol.01205.2005 [DOI] [PubMed] [Google Scholar]
- 60.Langberg H, Skovgaard D, Petersen LJ, et al. . Type I collagen synthesis and degradation in peritendinous tissue after exercise determined by microdialysis in humans. J Physiol (Lond) 1999;521(Pt 1):299–306. 10.1111/j.1469-7793.1999.00299.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Miller BF, Olesen JL, Hansen M, et al. . Coordinated collagen and muscle protein synthesis in human patella tendon and quadriceps muscle after exercise. J Physiol (Lond) 2005;567 3):1021–33. 10.1113/jphysiol.2005.093690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rosengarten SD, Cook JL, Bryant AL, et al. . Australian football players’ Achilles tendons respond to game loads within 2 days: an ultrasound tissue characterisation (UTC) study. Br J Sports Med 2015;49:183–7. 10.1136/bjsports-2013-092713 [DOI] [PubMed] [Google Scholar]
- 63.Docking SI, Daffy J, van Schie HT, et al. . Tendon structure changes after maximal exercise in the Thoroughbred horse: use of ultrasound tissue characterisation to detect in vivo tendon response. Vet J 2012;194:338–42. 10.1016/j.tvjl.2012.04.024 [DOI] [PubMed] [Google Scholar]
- 64.Parkinson J, Samiric T, Ilic MZ, et al. . Change in proteoglycan metabolism is a characteristic of human patellar tendinopathy. Arthritis Rheum 2010;62:3028–35. 10.1002/art.27587 [DOI] [PubMed] [Google Scholar]
- 65.Robbins JR, Evanko SP, Vogel KG. Mechanical loading and TGF-beta regulate proteoglycan synthesis in tendon. Arch Biochem Biophys 1997;342:203–11. 10.1006/abbi.1997.0102 [DOI] [PubMed] [Google Scholar]
- 66.Samiric T, Ilic MZ, Handley CJ. Large aggregating and small leucine-rich proteoglycans are degraded by different pathways and at different rates in tendon. Eur J Biochem 2004;271:3612–20. 10.1111/j.0014-2956.2004.04307.x [DOI] [PubMed] [Google Scholar]
- 67.Samiric T, Ilic MZ, Handley CJ. Characterisation of proteoglycans and their catabolic products in tendon and explant cultures of tendon. Matrix Biol 2004;23:127–40. 10.1016/j.matbio.2004.03.004 [DOI] [PubMed] [Google Scholar]
- 68.Freund W, Weber F, Billich C, et al. . The foot in multistage ultra-marathon runners: experience in a cohort study of 22 participants of the Trans Europe Footrace Project with mobile MRI. BMJ Open 2012;2:e001118 10.1136/bmjopen-2012-001118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van Schie HT, de Vos RJ, de Jonge S, et al. . Ultrasonographic tissue characterisation of human Achilles tendons: quantification of tendon structure through a novel non-invasive approach. Br J Sports Med 2010;44:1153–9. 10.1136/bjsm.2009.061010 [DOI] [PubMed] [Google Scholar]
- 70.Docking SI, Rosengarten SD, Cook J. Achilles tendon structure improves on UTC imaging over a 5-month pre-season in elite Australian football players. Scand J Med Sci Sports 2015. [DOI] [PubMed] [Google Scholar]
- 71.Orchard JW, Blanch P, Paoloni J, et al. . Cricket fast bowling workload patterns as risk factors for tendon, muscle, bone and joint injuries. Br J Sports Med 2015;49:1064–8. 10.1136/bjsports-2014-093683 [DOI] [PubMed] [Google Scholar]
- 72.Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010;376:1751–67. 10.1016/S0140-6736(10)61160-9 [DOI] [PubMed] [Google Scholar]
- 73.Mani-Babu S, Morrissey D, Waugh C, et al. . The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. Am J Sports Med 2015;43:752–61. 10.1177/0363546514531911 [DOI] [PubMed] [Google Scholar]
- 74.Humphrey J, Chan O, Crisp T, et al. . The short-term effects of high volume image guided injections in resistant non-insertional Achilles tendinopathy. J Sci Med Sport 2010;13:295–8. 10.1016/j.jsams.2009.09.007 [DOI] [PubMed] [Google Scholar]
- 75.Alfredson H. Ultrasound and Doppler-guided mini-surgery to treat midportion Achilles tendinosis: results of a large material and a randomised study comparing two scraping techniques. Br J Sports Med 2011;45:407–10. 10.1136/bjsm.2010.081216 [DOI] [PubMed] [Google Scholar]
- 76.Kongsgaard M, Qvortrup K, Larsen J, et al. . Fibril morphology and tendon mechanical properties in patellar tendinopathy: effects of heavy slow resistance training. Am J Sports Med 2010;38:749–56. 10.1177/0363546509350915 [DOI] [PubMed] [Google Scholar]
- 77.Kubo K, Ikebukuro T, Yata H, et al. . Time course of changes in muscle and tendon properties during strength training and detraining. J Strength Cond Res 2010;24:322–31. 10.1519/JSC.0b013e3181c865e2 [DOI] [PubMed] [Google Scholar]
- 78.Latella C, Kidgell DJ, Pearce AJ. Reduction in corticospinal inhibition in the trained and untrained limb following unilateral leg strength training. Eur J Appl Physiol 2012;112:3097–107. 10.1007/s00421-011-2289-1 [DOI] [PubMed] [Google Scholar]
- 79.Cook JL, Docking SI. “Rehabilitation will increase the ‘capacity’ of your…insert musculoskeletal tissue here….” Defining ‘tissue capacity’: a core concept for clinicians. Br J Sports Med 2015;49:1484–5. 10.1136/bjsports-2015-094849 [DOI] [PubMed] [Google Scholar]
- 80.Docking SI, Cook J. Pathological tendons maintain sufficient aligned fibrillar structure on ultrasound tissue characterization (UTC). Scand J Med Sci Sports 2015. [DOI] [PubMed] [Google Scholar]
- 81.de Vos RJ, Windt J, Weir A. Strong evidence against platelet-rich plasma injections for chronic lateral epicondylar tendinopathy: a systematic review. Br J Sports Med 2014;48:952–6. 10.1136/bjsports-2013-093281 [DOI] [PubMed] [Google Scholar]
- 82.Cho NS, Hwang JH, Lee YT, et al. . Tendinosis-like histologic and molecular changes of the Achilles tendon to repetitive stress: a pilot study in rats. Clin Orthop Relat Res 2011;469:3172–80. 10.1007/s11999-011-2000-1 [DOI] [PMC free article] [PubMed] [Google Scholar]