Sleep Medicine: Parasomnias (original) (raw)
. 2018 Mar-Apr;115(2):169–175.
Abstract
Parasomnias are abnormal and undesirable behaviors during sleep and are thought to be due to the sleep state instability. Some of them are benign, while some of them point to a possible underlying neurodegenerative process. This article briefly discusses the clinical characteristics, demographics, and pathophysiology of major parasomnias and associated disorders. The classification outlined in this article conforms to the current version of International Classification of Sleep disorders.
Introduction
The word parasomnia is derived from the Greek prefix ‘_Para_’ (meaning alongside of) and the Latin noun ‘_Somnus_’ (meaning sleep). In clinical terms, parasomnia refers to an abnormal or unusual behavior during sleep. Parasomnias encompass a broad spectrum of events including abnormal motor, behavioral, and sensory experiences. Excessive motor activity and abnormal motor behaviors, when present, adversely affect the patient or the bed partner resulting in sleep fragmentation, psychosocial effects, and even injuries.
In general, most parasomnias are more common in children and become less prevalent as they get older. Approximately 4% of adult population have been reported to have parasomnias.1 Parasomnias are also more frequent in psychiatric disorders.2 Other risk factors include sleep disorders, medical comorbidities and substance abuse.
Parasomnias are mainly categorized based on the sleep state in which they are observed. The ‘Other Parasomnias’ in the ICSD-third edition are sleep state independent.
Pathophysiology
The three states of human behavior are Wakefulness, NREM sleep and REM sleep, and are previously thought to be mutually exclusive. NREM sleep in turn is divided into three stages (N1, N2, and N3) Transitions from one behavioral state to another is not a quick switch but involves reorganization and transition of various neural centers before a specific state manifests unequivocally. Recent research has shown that combinations of one or more of these states can result in unstable states, and an arousal out of these unstable states can give rise to abnormal behaviors manifesting as parasomnias.3,4 It is also suggested that deafferentation of locomotor centers in the spinal and at supraspinal levels, from the generators of different sleep states may result in motor activity in the setting of arousals.5
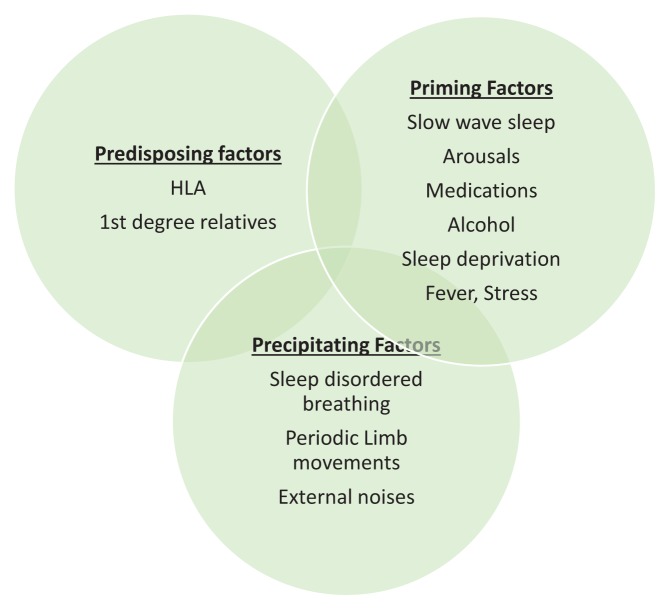
Most of the NREM parasomnias arise out of N3 NREM sleep. Any condition that promotes NREM sleep fragmentation (such as pain conditions, restless legs syndrome, periodic limb movements, sleep-related breathing disorders, etc.) increase the risk of parasomnias. Also, conditions of increased sleep drive including sleep deprivation and sedative medications are risk factors for parasomnias. Certain HLA haplotypes like HLA DQ B1*05:01 and HLA DQ B1*04 are considered risk factors for the development of parasomnias. First-degree relatives of patients with parasomnias have a higher prevalence of similar parasomnias. (Figure 1)
Figure 1.
Model for the pathogenesis of Parasomnias.
NREM Parasomnias
The common feature of these parasomnias is recurrent episodes of incomplete awakening from NREM sleep along with amnesia for the event. Clinical phenotypes of this incomplete arousal from NREM sleep include sleepwalking, sleep terrors, confusional arousals, and sleep-related eating disorder. They usually arise out of slow wave sleep but can also arise from N2 sleep and are more frequent in the first half of the night. These parasomnias are more frequently seen in children. Factors that impair sleep consolidation and increase sleep fragmentation (eg, pain, restless legs syndrome, sleep apnea) can result in these parasomnias. Similarly, sleep deprivation and sedating medications can also increase the emergence of these abnormal behaviors by enhancing sleep inertia and by hindering normal sleep-wake transition. Consequently, these disorders manifest as arousals associated with disorientation, amnesia, and confusion.
Immaturity of sleep-wake boundary regulation may be the reason why these occur more commonly in pediatric population. Studies have shown a higher prevalence of HLA DQB1*05:01 and HLA DQB1*04 alleles in various NREM parasomnias6. Sleepwalking also shows an autosomal dominant trait involving chromosome 20.7
Sleepwalking
Ambulatory behavior is the primary manifestation of this disorder of arousal. In a systematic review analyzing 51 different studies, Stallman et al. reported a lifetime prevalence of sleepwalking of 6.9% (95% CI 4.6% to 10.3%)8 which did not change significantly between childhood and adulthood. This number increased to 47.4% for children with one parent with history of sleepwalking and up to 61.5% for children with both parents with history of sleepwalking.9
The behaviors can range from aimless wandering to complex, prolonged, and inappropriate episodes that involve driving an automobile, urinating, walking naked, etc. Sleepwalkers typically do not respond to redirection during the episode. In adults, sleepwalking is frequently associated with other disorders like sleep apnea, RLS and usage of hypnotic medications. Multiple different medications like benzodiazepine receptor agonists, antidepressants (amitriptyline, paroxetine, mirtazapine, bupropion), antipsychotics (Olanzapine, quetiapine), antihypertensives (Propranolol, metoprolol), fluoroquinolones, montelukast, topiramate have been implicated as triggers for sleepwalking.10,11
Sleep Terrors
Sleep terrors consist of episodes of intense fear accompanied by very loud ‘piercing’ screams and loud crying during which the patient appears terrified. The associated autonomic activation results in increase in heartrate, breathing, pupillary dilatation, and sweating. The typical duration of sleep terrors is 3–5 minutes. The prevalence of sleep terrors varies widely in children from 14.7% to 56%9,10 and they almost always resolve by late childhood. Sleep terrors in adults are rare, and are more likely to be associated with medications or psychopathology.
Confusional Arousals
These are partial arousals from NREM sleep that results in a state of disorientation and occasionally, automatic behavior like vocalizations and motor activity. Ambulation and significant sympathetic over-activity is typically absent. Confusional arousals are more common in pediatric population with a prevalence of up to 17%.12 They are brief, lasting for a few minutes, but may sometimes be prolonged, particularly with sedative hypnotic usage. The individuals with confusional arousals show diminished responsiveness to external stimuli during the episode, and have a partial or complete amnesia of the episode afterward.
Sleep-Related Eating Disorder (SRED)
This parasomnia is more common in women and is characterized by recurrent episodes of binge eating after a partial arousal from NREM sleep.13 During these episodes patients show a predilection for high carbohydrate food and other peculiar inedible items including raw meat, pet foods etc. This parasomnia is closely related to and is thought to be a variant of sleepwalking. Patients are completely amnestic of their eating behavior, and can have adverse consequences due to their nocturnal eating including weight gain, worsening of diabetes, etc. This parasomnia is different from nocturnal eating disorder/night eating syndrome where patients are aware of their eating behavior, and is associated with anxiety in most cases. Ambien is the most common medication that induces SRED though several other psychotropic medications are known to precipitate it. Certain other factors like smoking cessation, alcohol consumption, and acute stress are also associated with SRED. Treatment should begin with elimination of precipitating factors like hypnotic medications and treating the comorbid sleep disorders. Medications that can be used to treat SRED include dopamine agonists and Topiramate.
Sexsomnia
Sexsomnia refers to sleep-related abnormal sexual behaviors. It is classified as a subtype of NREM parasomnia disorders of arousal in ICSD-3 with abnormal sexual behaviors emerging from partial arousals during slow-wave sleep. It is more common in young males. A wide range of behaviors have been reported including sexual intercourse, attempted intercourse, masturbation, assaultive sexual behavior, sexual vocalizations, etc. Like other parasomnias, other causes of sleep fragmentation should be investigated before initiating pharmacotherapy. Nocturnal seizures, medications like SSRIs and pramipexole have been reported to be some of the other causes for sexsomnia. Treatment data is limited but Clonazepam might be helpful in bothersome cases.14
REM Parasomnias
REM Sleep Behavior Disorder
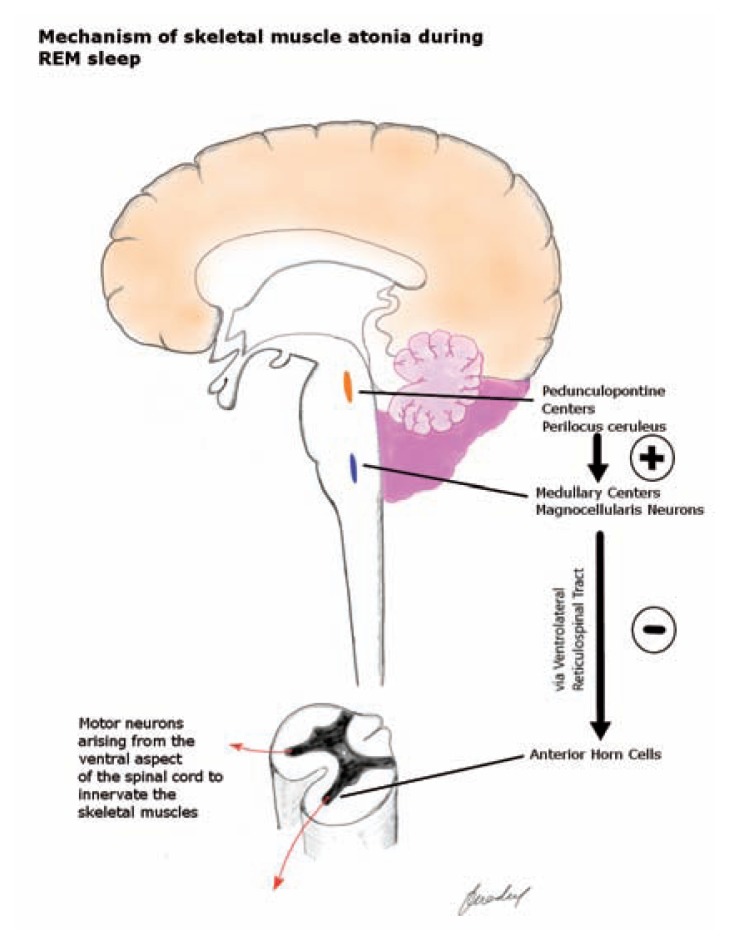
REM sleep is characterized by rapid eye movements and skeletal muscle atonia. Respiration is diaphragm–based during REM sleep. Dreaming during REM sleep tends to be vivid and detailed, compared to the vague dream content of non-REM sleep. Muscle atonia mediated by brainstem centers, pedunculopontine nucleus and locus coeruleus, serves as a protective mechanism preventing dream enactment during REM sleep. (Figure 2) However, conditions resulting in disruption of this protective mechanism can lead to physical enactment of dream content during REM sleep. This phenomenon is called REM Sleep Behavior Disorder (RBD)
Figure 2.
The Perilocus Coeruleus region of the pons exerts an excitatory influence on the medullary ‘Magnocellularis’ neurons via lateral tegmentoreticular tract. These neurons project on to the spinal alpha motor neurons in the ventral horn via ventrolateral reticulospinal tract and cause hyperpolarization. This results in reduced muscle tone during the REM sleep. In RBD, the brainstem mechanisms that generate REM sleep related muscle atonia are disrupted.
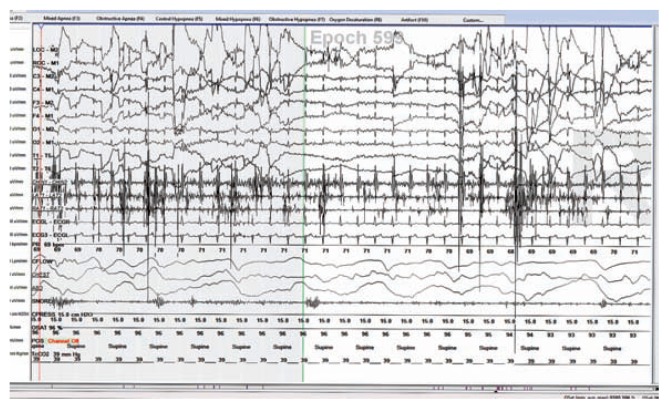
Parkinson disease (PD) is strongly associated with RBD. (Figure 3) In fact, RBD can predate the initial motor symptoms by years, and is one of the best-known biomarkers for PD. RBD is present in 25–50% of PD patients and is even more frequent in other neurodegenerative disorders such as Multiple System Atrophy and Lewy body dementia. Forty percent of the patients with idiopathic RBD develop parkinsonian syndrome within a decade and two-thirds within two decades.
Figure 3.
Increased EMG activity in the chin and the leg EMG leads suggestive of RBD in a patient with Parkinson disease.
Secondary RBD can also be seen in the setting of pontine tegmental lesions, withdrawal from alcohol, medication usage (SSRIs, SNRIs, TCAs, MAO inhibitors), Type 1 narcolepsy, and other neurodegenerative disorders like fronto-temporal dementia, Alzheimer’s dementia. Patients experiencing RBD may have mild, low amplitude limb movements that are often overlooked. Some patients have vocalizations. These movements can be significant and violent with apparent goal directed behaviors that can cause injury with lacerations. Curiously, the motor activity in RBD in patients with PD appears smoother, faster, and stronger than the patient’s daytime motor performance. Patients experiencing RBD may report falling from their beds during the night. Their bed partners may sometimes be able to understand the dream content based on the patient’s behavior. Some episodes result in arousal from sleep. Usually, RBD episodes do not cause significant sleep disruption. Nocturnal REM sleep without atonia is found to be strongly associated with pediatric narcolepsy15.
Nightmare Disorder
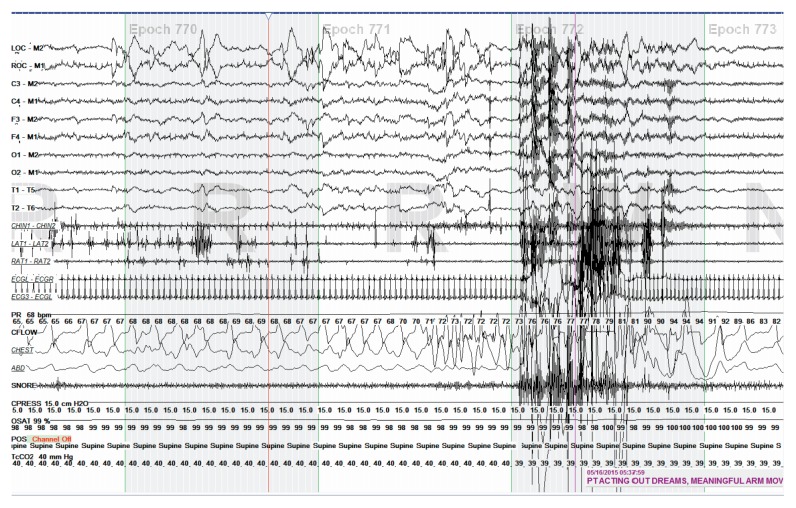
This disorder is characterized by recurrent dysphoric dreams of disturbing mental experiences. These nightmares mostly occur during REM sleep and result in awakening. The theme of the nightmare is usually distressing to the individual and result in a variety of emotions including anxiety, fear, rage, embarrassment, and disgust. Nightmares are very common in children and the child that wakes up from a nightmare usually can give a good description of the dream. They are also common in patients with increased anxiety levels and in those with posttraumatic stress. Childhood nightmares usually resolve spontaneously. Diagnosis of nightmare disorder should only be given in patients that are experiencing persistent distress and impairments. (Figure 4)
Figure 4.
A two-minute window of polysomnogram showing nightmare arising out of REM sleep.
Recurrent Isolated Sleep Paralysis
The core feature of sleep paralysis is complete inability to move during wakefulness. Unlike RBD where muscle tone persists during REM sleep, sleep paralysis is characterized by the extension of REM sleep-related muscle atonia into wakefulness. Most cases of sleep paralysis are isolated and sporadic with about 7% of the general population reporting at least one episode of sleep paralysis.16 Sometimes, sleep paralysis can be associated with a sensation of difficult breathing and hallucinatory experiences. Isolated sleep paralysis is a benign condition but can contribute to significant distress when experienced for the first time. Sleep paralysis can happen either during falling asleep (hypnogogic sleep paralysis) or while when waking up (hypnopompic sleep paralysis). In some cases, triggers for sleep paralysis include sleep deprivation and comorbid sleep apnea. Though sleep paralysis is a benign problem, it can happen frequently causing a significant fear of initiating sleep at which time the more appropriate term for it would be recurrent isolated sleep paralysis (RISP).
Other Parasomnias
Sleep Enuresis
Sleep Enuresis (SE) is characterized by recurrent, involuntary voiding during sleep for at least three months. SE occurs in 15 to 20% of five-year olds, and is three times more common in boys. In primary SE, recurrent episodes of involuntary voiding happen at least twice a week during sleep after five years of age in a patient who was never consistently dry during sleep for six consecutive months. It is considered secondary SE if the patient was consistently dry for at least six months before and began wetting later. This condition is associated with difficulty waking up from sleep in response to an urge to urinate in the setting of a full urinary bladder. Though psychological problems are a rare cause of primary SE, secondary SE is more commonly seen in children who have recently experienced a significant psychosocial stress. Secondary SE is also commonly associated with chronic constipation and fecal soiling. There is often a high prevalence of enuresis among the parents, siblings and other relatives of children with primary enuresis.
Three important factors contribute to the risk of developing SE: large nocturnal urine volume production, nocturnal bladder over-activity and difficulty arousing from sleep. Multiple studies suggest that difficulty arousing from sleep is more important in primary enuresis while bladder overactivity is more important in secondary enuresis. Sleep fragmentation by disorders like sleep apnea is also highly correlated with SE and successful treatment of sleep apnea results in reduction or elimination of sleep enuresis. Typically, the spontaneous cure rate of primary SE is about 15% per year.
Sleep-Related Hallucinations
Sleep-related hallucinations are unreal experiences that occur at the onset of sleep or upon awakening from sleep. They are predominantly visual hallucinations but can also be auditory or even tactile in nature. Hallucinations occurring at sleep onset are called ‘Hypnogogic hallucinations’ while those occurring on awakening are called ‘Hypnopompic hallucinations.’ Sometimes, they can be very complex and can follow a sudden awakening without recall of a preceding dream. These ‘complex nocturnal hallucinations’ can result in injuries when patients jump out of bed in terror. Sleep-related hallucinations can be associated with other parasomnias including sleep talking or sleepwalking. They are also very common in narcolepsy but can also be seen in a high proportion of general population. They are more common in younger persons, and occur slightly more frequently in women. Large populations studies suggest that alcohol use, mood disorders, insomnia, and drug use increase the likelihood of sleep-related hallucinations. Complex nocturnal visual hallucinations, on the other hand, are very rare and may be seen in patients with narcolepsy, Parkinson disease, Lewy body dementia, midbrain and diencephalic pathology, and in the setting of beta-blocker medication usage.
Exploding Head Syndrome
Exploding Head Syndrome (EHS) is a condition where the affected individuals experience a sudden noise or a sense of explosion that results in abrupt arousal with a sense of fright and happens in the setting of either falling asleep or while waking up. This whole experience is not associated with significant complaints of pain. The term Exploding Head Syndrome was first coined by J.M.S Pearce17 and despite its memorable name, relatively little is known about this condition. It is not uncommon for patients suffering from EHS to interpret their condition to be far more serious and seek medical attention. The sounds reported during EHS are varied and include violent explosions, door slamming sounds, buzzing, nearby thunder, whip lash, etc.18 Some patients experience visual symptoms like light flashes, feelings of intense heat, epigastric sensations and an aura of electrical sensation that ascends from lower torso to the head.19 EHS should be differentiated from headache syndromes like cluster headache, thunderclap headaches, hypnic headache and from nocturnal seizures. Patient education and reassurance are the mainstay treatments, though medications like flunarizine, nifedipine, clomipramine, topiramate and carbamazepine have been tried with limited benefit. Stress and anxiety reduction has been found to be helpful.
Parasomnias Due to Medical Disorder
The primary feature of this diagnosis is the presence of a parasomnia that can be explained by an underlying medical or neurological disorder. Charles Bonnet syndrome (CBS) is characterized by vivid visual imagery in the setting of partial or complete visual loss. Peduncular hallucinosis is a syndrome of hallucinations that can happen in the setting of brainstem and diencephalic pathology.20 Sleep-related hallucinations, seen in the setting of CBS and peduncular hallucinosis, are good examples of parasomnias due to medical disorder. Though REM sleep behavior disorder is technically a parasomnia that occurs in the setting of an underlying neurological disorder (α-synucleopathy), it is considered as a separate parasomnia and discussed above.
Parasomnia Due to Medication or Substance Abuse
The essential feature of this diagnosis is dependent upon the onset or worsening of a parasomnia in the setting of usage of a medication or bioactive substance. Multiple medications including selective serotonin reuptake inhibitors, venlafaxine, tricyclic antidepressants, MAO inhibitors have been associated with worsening of RBD. Beta-adrenergic blocking agents can be associated with sleep-related hallucinations. Zolpidem and Zopiclone are associated with a variety of parasomnias including sleep driving and sleep-related eating disorder.
Parasomnia in the Setting of IgLON5 Autoimmunity
Sabater, et al.21 described a case series of patients showing a unique NREM and REM parasomnia in the setting of autoantibodies against IgLON5, a neuronal cell adhesion protein. This syndrome is characterized by breathing dysfunction, gait instability and brainstem symptoms. Despite being described as a unique parasomnia, this disease has some features of agrypnia excitata and may not be a true parasomnia.22
Sleep Talking
Sleep talking is highly prevalent with a lifetime prevalence up to 66%.23,24 Due to its high prevalence and the benign nature of this parasomnia, it is typically considered a normal variant. It is characterized by varying degrees of comprehensibility, and can happen both, during REM and NREM sleep. It rarely causes problems but sometimes can be frequent and loud disrupting the sleep of bed partners or roommates.
Catathrenia is another sleep-related phenomenon consisting of loud groaning sounds during episodes of prolonged expiration. It was first reported in 1983 by De Roeck et al. Initially, it was classified among Parasomnias in the ICSD– 2nd edition but was later included among respiratory disorders in the ICSD-3rd edition.
Diagnostic Evaluation
The approach to a patient presenting with abnormal nocturnal behaviors should start with a good history and if possible, an account from a firsthand witness. A comprehensive video polysomnography (PSG) with expanded EEG and EMG channels should be considered if the parasomnia is presenting with an unusual phenotype or an atypical age and if it is happening frequently. The main purpose of polysomnographic evaluation is to identify triggers of parasomnias like sleep apnea, periodic limb movements and mimics of parasomnias like nocturnal seizures.
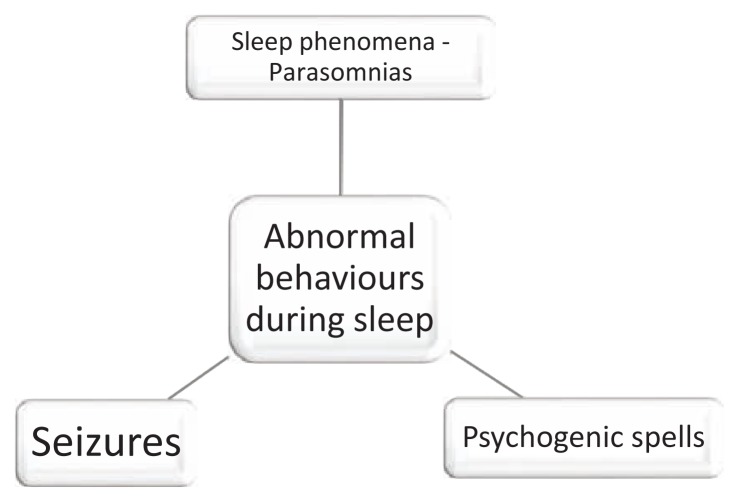
It should be noted that not all nocturnal abnormal behaviors are parasomnias. Nocturnal seizures can be sometimes confused with parasomnias. Both temporal lobe and frontal lobe seizures can present during sleep. Similarly, psychogenic/psychiatric conditions like PTSD and nocturnal panic attacks also mimic parasomnias. (Figure 5)
Figure 5.
It should be noted that not all nocturnal abnormal behaviors are parasomnias.
Treatment
As parasomnias are more common in children, their presence tends to elicit anxiety and panic in the parents. Reassurance and education is very important as most kids grow out of these behaviors without any intervention. In general, for NREM parasomnias, the diagnostic evaluation should start with an attempt to find out potential triggers. One of the common risk factors for NREM parasomnias is sleep disruption, and so the clinician should use a combination of history and diagnostic testing to determine if there are any sleep disorders like sleep-related breathing disorder, periodic limb movements, etc. Similarly, a careful history should be able to identify any environmental stimulants like loud noise that can be contributing to sleep disruption. Patients should be educated about maintaining a good sleep hygiene. Medications (Z drugs, antidepressants, antipsychotics) that are associated with a variety of parasomnias should be evaluated for the possibility of causality.
Patients with RBD should be carefully assessed for risk of injury and safety measures should be undertaken. The first step is to make the sleeping environment safe – e.g. putting soft pads around the bed to minimize the impact of falls, using pillows, keeping distance from the bed partner, removing sharp and potentially injurious objects. Bed partner should be aware of these behaviors and try to have an alternative sleeping arrangement rather than sleeping on the same bed as the patient. Similar safety measures should be employed in cases of NREM parasomnias like sleepwalking. Bed or door alarms can help prevent patient wandering away in their sleep.
Pharmacological treatments for RBD include Clonazepam and Melatonin. Clonazepam is a benzodiazepine and acts at GABA receptors. Melatonin on the other hand is an over-the-counter dietary supplement in the United States and acts on melatonin receptors. Other medications that showed success in limited case series include pramipexole, levodopa, carbamazepine, and imipramine.
Conclusion
Much has been learned about the pathogenesis of parasomnias in the last few decades. RBD has shown to be strongly associated with an underlying neurodegenerative α-synucleopathy while many other parasomnias are benign. Despite the variety of pharmacological and non-pharmacological strategies, there are still no standard of practice guidelines. It is important for the sleep physician to understand the nature of the parasomnia and to differentiate it from nocturnal seizures. Understanding the phenomenology of parasomnias is important due to the forensic implications associated with them.
Abbreviations
NREM
Non-Rapid Eye Movement
REM
Rapid Eye Movement
ICSD
International Classification of Sleep Disorders -3
SSRI
Selective Serotonin Reuptake Inhibitors
SNRI
Serotonin Norepinephrine Reuptake inhibitors
MAOI
Monoamine Oxidase Inhibitors
EMG
Electromyography
Biography
Pradeep C. Bollu, MD, (left), Munish K. Goyal, MD, Mahesh Thakkar, PhD, and Pradeep Sahota, MD, (right), MSMA member since 2003, are in the Department of Neurology, University of Missouri - Columbia.
Contact: BolluP@health.missouri.edu

Footnotes
Disclosure
None reported.
References
- 1.Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. The Journal of clinical psychiatry. 1999;60(4):268–276. doi: 10.4088/jcp.v60n0413. quiz 277. [DOI] [PubMed] [Google Scholar]
- 2.Waters F, Moretto U, Dang-Vu TT. Psychiatric Illness and Parasomnias: a Systematic Review. Current psychiatry reports. 2017;19(7):37. doi: 10.1007/s11920-017-0789-3. [DOI] [PubMed] [Google Scholar]
- 3.De Lecea L, Kilduff T, Peyron C, et al. The hypocretins: hypothalamus-specific peptides with neuroexcitatory activity. Proceedings of the National Academy of Sciences. 1998;95(1):322–327. doi: 10.1073/pnas.95.1.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahowald M. Overview of parasomnias. American Academy of Sleep Medicine; 1999. [Google Scholar]
- 5.Tassinari C, Cantalupo G, Högl B, et al. Neuroethological approach to frontolimbic epileptic seizures and parasomnias: the same central pattern generators for the same behaviours. Revue neurologique. 2009;165(10):762–768. doi: 10.1016/j.neurol.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Heidbreder A, Frauscher B, Mitterling T, et al. Not Only Sleepwalking But NREM Parasomnia Irrespective of the Type Is Associated with HLA DQB1* 05:01. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine. 2016;12(4):565–570. doi: 10.5664/jcsm.5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Licis A, Desruisseau D, Yamada K, Duntley S, Gurnett C. Novel genetic findings in an extended family pedigree with sleepwalking. Neurology. 2011;76(1):49–52. doi: 10.1212/WNL.0b013e318203e964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stallman HM, Kohler M. Prevalence of sleepwalking: a systematic review and meta-analysis. PloS one. 2016;11(11):e0164769. doi: 10.1371/journal.pone.0164769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petit D, Pennestri M-H, Paquet J, et al. Childhood sleepwalking and sleep terrors: a longitudinal study of prevalence and familial aggregation. JAMA pediatrics. 2015;169(7):653–658. doi: 10.1001/jamapediatrics.2015.127. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. 2014. [Google Scholar]
- 11.Stallman HM, Kohler M, White J. Medication induced sleepwalking: A systematic review. Sleep Medicine Reviews. 2017 doi: 10.1016/j.smrv.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Wills L, Garcia J. Parasomnias. CNS drugs. 2002;16(12):803–810. doi: 10.2165/00023210-200216120-00002. [DOI] [PubMed] [Google Scholar]
- 13.Inoue Y. Sleep-related eating disorder and its associated conditions. Psychiatry and clinical neurosciences. 2015;69(6):309–320. doi: 10.1111/pcn.12263. [DOI] [PubMed] [Google Scholar]
- 14.Arino H, Iranzo A, Gaig C, Santamaria J. Sexsomnia: parasomnia associated with sexual behaviour during sleep. Neurología (English Edition) 2014;29(3):146–152. doi: 10.1016/j.nrl.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 15.Bin-Hasan S, Videnovic A, Maski K. Nocturnal REM Sleep Without Atonia Is a Diagnostic Biomarker of Pediatric Narcolepsy. Journal of Clinical Sleep Medicine. 2018;14(02):245–252. doi: 10.5664/jcsm.6944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharpless BA, Barber JP. Lifetime prevalence rates of sleep paralysis: a systematic review. Sleep medicine reviews. 2011;15(5):311–315. doi: 10.1016/j.smrv.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pearce J. Exploding head syndrome. The Lancet. 1988;332(8605):270–271. doi: 10.1016/s0140-6736(88)92551-2. [DOI] [PubMed] [Google Scholar]
- 18.Sharpless BA. Exploding head syndrome. Sleep medicine reviews. 2014;18(6):489–493. doi: 10.1016/j.smrv.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Kowey P, Marinchak R, Rials S. More things that go bang in the night. N Engl J Med. 1993;328:1570–1571. doi: 10.1056/NEJM199212243272614. [DOI] [PubMed] [Google Scholar]
- 20.Benke T. Peduncular hallucinosis. Journal of neurology. 2006;253(12):1561–1571. doi: 10.1007/s00415-0060-0254-4. [DOI] [PubMed] [Google Scholar]
- 21.Sabater L, Gaig C, Gelpi E, et al. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. The Lancet Neurology. 2014;13(6):575–586. doi: 10.1016/S1474-4422(14)70051-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Della Marca G, Iorio R, Losurdo A, Mirabella M, Frisullo G. Sleep disorder associated with antibodies to IgLON5: parasomnia or agrypnia? The Lancet Neurology. 2014;13(9):864. doi: 10.1016/S1474-4422(14)70127-9. [DOI] [PubMed] [Google Scholar]
- 23.Arkin AM, Toth MF, Baker J, Hastey JM. The frequency of sleep talking in the laboratory among chronic sleep talkers and good dream recallers. Journal of Nervous and Mental Disease. 1970 doi: 10.1097/00005053-197012000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Bjorvatn B, Grønli J, Pallesen S. Prevalence of different parasomnias in the general population. Sleep Medicine. 2010;11(10):1031–1034. doi: 10.1016/j.sleep.2010.07.011. [DOI] [PubMed] [Google Scholar]