Vein Size and Disease Severity in Chronic Venous Diseases (original) (raw)
Abstract
Given the high prevalence of chronic venous diseases (CVD), defining criteria to screen patients who are in need for intervention is attaining primacy. An important clinical criterion for treating CVD is incompetence of larger veins. We have assessed the association of size of afflicted veins with disease severity in patients with CVD to define an acceptable criterion to identify patients who need intervention. Demographic characteristics and risk factors were recorded from 6350 patients. Based on physical examination and venous duplex ultrasound study, patients were classified into clinical severity, etiology, anatomy, and pathophysiology (CEAP) classes and grouped according to the size of the veins which had varicosities. Patients with reflux in smaller veins (vein size <4 mm diameter) were considered as type I and those with varicosities in truncal veins (>4 mm diameter) as type II. Risk ratio was determined by multivariate regression analysis. About 47.67% of patients in this study were found to have CEAP class 3 disease. Compared with varicose veins of large truncal veins, patients with varicosities in smaller superficial veins had 2.85-fold (p < 0.01) more risk of edema and 5.71-fold (p < 0.01) higher prevalence of hyperpigmentation. Varicosities in small superficial veins were associated with higher risk of ulceration (odds ratio 3.93, 95% confidence interval 2.51–6.18) compared with truncal vein reflux. Our study reveals that presence of small varicose veins in patients without truncal saphenous reflux involvement is associated with severe manifestations of venous insufficiency such as edema and skin lesions even in the absence of varicosities in truncal saphenous veins.
Keywords: chronic venous disease, varicose veins, CEAP classification, venous ulcers, great saphenous vein, small saphenous vein, vein reflux
Chronic venous disease (CVD) of lower limbs is characterized by the presence of spider veins, varicose veins, edema, skin hyperpigmentation, and venous ulcers in the affected areas. Progressive venous insufficiency in great saphenous vein (GSV) or small saphenous vein (SSV) is an underlying feature of this disease.1Until recently it was considered that small superficial veins including tributaries and reticular veins are harmless and are not involved. Recent studies based on retrograde resin venography demonstrated that venous incompetence in small superficial veins can take place in the absence of reflux in GSV and SSV.2Reflux in these small veins is currently considered to be associated with clinical severity of venous insufficiency.
Increasing incidence of CVD and the substantial treatment cost contribute to a heavy burden on health care resources. Public health care systems restrict treatment to those who have high prevalence of varicose veins and thus qualify for treatment and those who are likely to benefit from intervention.3 4Reflux in larger veins is considered as a key factor for morbid manifestations of CVD. Based on a retrospective study in 330 patients with CVD, Lane et al have reported that there was no significant association between larger vein diameter and clinical severity, etiology, anatomy, and pathophysiology (CEAP) classes of CVD.3The role of reflux in veins with smaller diameter in the development of skin changes and leg ulceration is unknown. We have analyzed the relationship between the size of veins with blood reflux and clinical manifestations such as hyperpigmentation, thrombophlebitis, cellulitis, and ulceration. We have also analyzed other risk factors for varicose veins in our study population.
Methods
Study Population and Design
A retrospective study comprising 6,350 patients with CVD (age range 18–89 years) was undertaken. Study subjects were consecutive patients who were assessed, treated, and followed up at specialized referral vascular clinic, St. Thomas Institute of Research on Venous Diseases, Changanassery, Kerala, India, between the year 2007 and 2013. Principles of the Helsinki declaration were strictly followed. The study and protocols were approved by institutional ethics committee of Rajiv Gandhi Centre for Biotechnology, Thiruvananthapuram. All study participants gave their written consent for participation in the study.
Data Collection
Demographic and clinical data regarding symptoms such as pain or throbbing sensation in legs, hemorrhage, lower limb edema, itching, hyperpigmentation, thrombophlebitis, cellulitis, ulceration, and history of deep vein thrombosis were collected from each patient. Details regarding family history and occupational risk factors were collected by interviewing patients and their relatives, using a specific questionnaire. The questionnaire aimed at demographic details such as age, gender, body weight, height, smoking, drinking, medical history, and family history of varicose veins or spider veins; and disease-related queries such as pain, throbbing, and number of pregnancy and occupation-related details.
Diagnosis
The size of veins involved and related clinical signs and complications of CVD such as varicosities, edema, eczema, hyperpigmentation of the skin, and ulceration were assessed by physical examination and color duplex ultrasound scanning (Doppler ultrasound machine, Philips HD 15 and Philips Envisor, with high-frequency linear probe 3–12 MHz, wide band) by experienced ultrasonologists. Clinical examination was done with patient in standing position in all cases, to detect reflux in patients.
Inclusion and Exclusion Criteria
Reflux cutoff was decided to be ≥ 0.5 seconds5and was considered inclusion criteria. Six patients were diagnosed to have varicose veins and concomitant deep vein thrombosis and they were excluded from the current study. Patients who had prior truncal reflux and undergone GSV ablation and who presented with smaller varicosities were also excluded from the current study.
Patients with CVD were classified according to CEAP clinical classification (C0: no visible or palpable signs of venous disease; C1: telangiectasia; C2: varicose veins; C3: edema; C4: skin damage such as pigmentation, eczema, or lipodermatosclerosis; C5: healed venous ulcer; C6: nonhealing venous ulcer).6
We grouped all patients according to the size of the afflicted veins. Diameter of the incompetent reticular veins was between 2 and 3 mm and incompetent vein tributaries were 3 to 4 mm.7Diameter of incompetent truncal saphenous veins was found to be above 4 mm.8Truncal saphenous veins consisted of both GSV and SSV. The mean diameters of normal GSV and GSV with blood reflux have been reported to be ∼5 ± 2.4 mm and 6.4 ± 2.0 mm, respectively. The mean diameters of healthy SSV and refluxed SSV are reported to be 3.1 ± 1.3 mm and 5.2 ± 2.7 mm, respectively.9Patients with reflux and varicosities in small veins and tributaries were grouped as type I (vein size <4 mm diameter) and those with varicosities in truncal veins (GSV and SSV) involvement were grouped as type II (veins > 4 mm diameter). Several patients had varices in both type of veins and they were not included in the detailed analysis pertaining vein size and clinical severity.
Statistical Analysis
Data collected through questionnaires and medical records were entered into MS Excel and analyzed using STATA IC/11.2 software package. The demographic information and risk factors were compared between male and female patients by proportions and the significance was tested using chi-square test. Clinical manifestations of CVD in different age groups were also compared using chi-square test. The proportions of different clinical symptoms were compared between type I and type II patients. Risk of disease was calculated based on odds ratios which were estimated using logistic regression model with patients having truncal varicosities as the reference group. The adjusted odds ratios were calculated for each clinical symptom by including age and gender in the model.
Results
Demographic Data Analysis, Family History, and Lifestyle Factors
Six thousand three hundred fifty patients with CVD were evaluated in the current study. Our study revealed a preponderance of females with varicose veins (2,930 men and 3,420 women). There was no significant difference between males and females with respect to prevalence of CVD complications.
About 53.8% of the patients were between 40 and 59 years of age (mean age 49.4 ± 13 years). A positive family history of varicose veins was reported by 85.23% of patients. There was no significant gender difference with regard to family history for CVD (p = 0.661). Ninety two percent of the patients were involved in occupations involving prolonged periods of standing (Table 1).
Table 1. Demographic profile of patients with chronic venous diseases.
| Patient details | Male | Female | Total | _p_Value | |||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | ||
| Total number of patients | 2,930 | 3,420 | 6,350 | ||||
| Age in years | |||||||
| < 40 | 891 | (30.43) | 557 | (16.28) | 1448 | (22.80) | |
| 40–59 | 1434 | (48.98) | 1982 | (57.92) | 3,416 | (53.80) | |
| ≥ 60 | 603 | (20.59) | 883 | (25.80) | 1,486 | (23.40) | < 0.001 |
| Family history (Yes) | 2,491 | (85.02) | 2,921 | (85.41) | 5,412 | (85.23) | 0.661 |
| Prolonged standing | 2,845 | (97.10) | 2,985 | (87.28) | 5,830 | (91.81) | < 0.001 |
Hypertension and type 2 diabetes mellitus are considered to exacerbate varicose veins.10Type 2 diabetes mellitus was present in 493 patients and 817 patients in our study had hypertension. Three-hundred forty three patients had both type 2 diabetes mellitus and hypertension.
CEAP-Based Classification of Patients
A significant number of patients (71.43%) had varicosities in both legs, while 28.57% patients had afflicted veins in single leg. Gender difference was not present with respect to which leg was predominantly involved. The frequencies of disease symptoms in 6,350 patients are given inFig. 1. Throbbing sensation or pain (71%) and hyperpigmentation (70%) were observed as the most frequent complaints/symptoms of patients. Itching was reported by 41.92%, edema by 39.35%, and ulceration by 28.9% of study subjects. The least common symptom was thrombophlebitis (1.32%). A majority of the study population (47.67%) comprised of patients in CEAP clinical class 3 (Fig. 2).
Fig. 1.
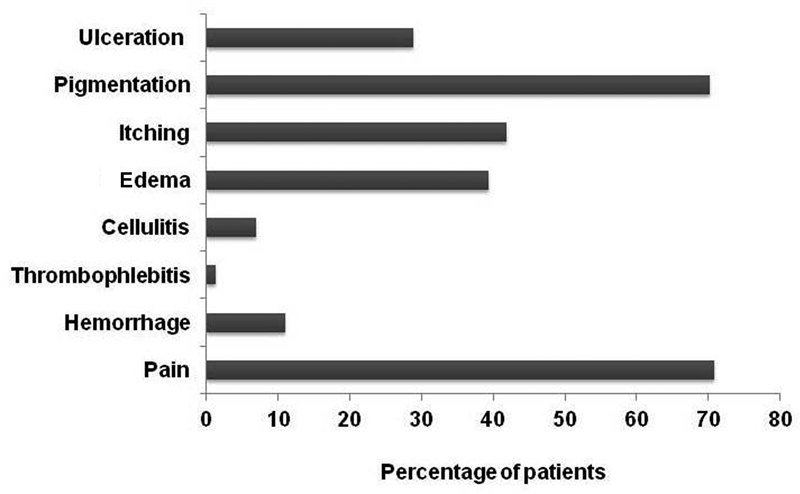
Frequencies of symptoms in 6,350 patients with chronic venous diseases. Throbbing sensation or pain in legs and hyperpigmentation of skin were observed to be highly prevalent compared with other symptoms in study participants.
Fig. 2.
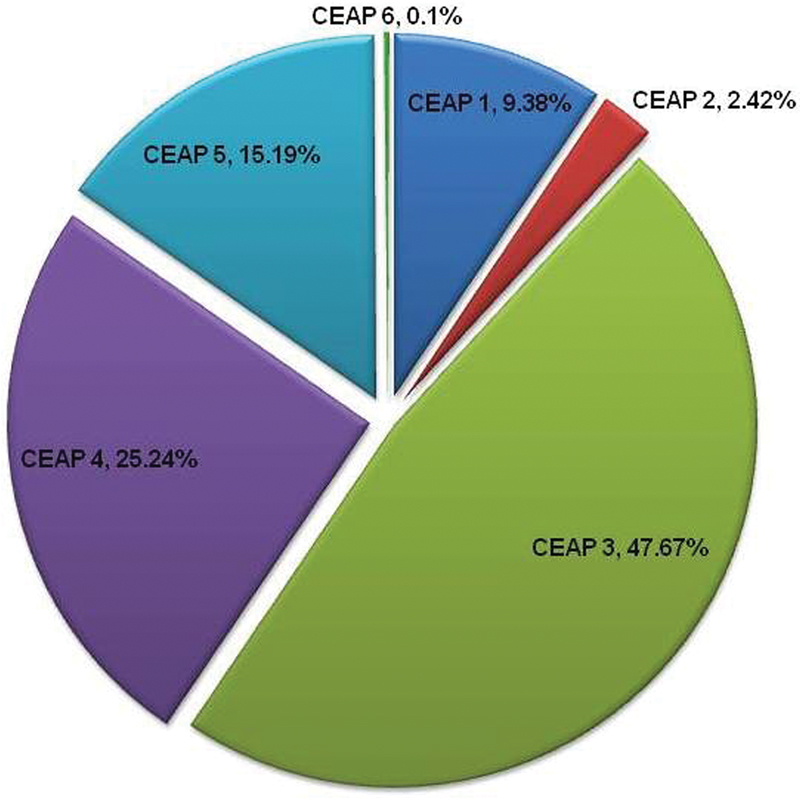
Clinical severity, etiology, anatomy, and pathophysiology (CEAP) classification of 6,350 patients with chronic venous diseases. Majority of patients in the study subjects belonged to CEAP clinical class 3.
Diameter of Afflicted Vein and Clinical Manifestations
We assessed the diameter of veins with reflux and analyzed their association with disease symptoms (Table 2). The most common symptom of CVD, namely pain or throbbing in legs, was associated with varicosity of truncal veins (> 4 mm in diameter). Only six patients had thrombophlebitis and these patients also had reflux in smaller veins especially minor tributaries. These patients were excluded from our analysis. Complications such as hemorrhage, cellulitis, edema, itching, pigmentation, and ulceration were commonly associated when smaller veins such as small superficial tributaries of major saphenous veins and reticular veins were involved.
Table 2. Clinical symptoms and signs versus venous involvement in patients with chronic venous diseases.
| Clinical symptoms | Type II (n = 223) n(%) | Type I (n = 1,277) n(%) | OR, 95%CI | ||
|---|---|---|---|---|---|
| Pain | 179 | (80.27) | 918 | (71.89) | 0.63 (0.44–0.90) |
| Hemorrhage | 18 | (8.07) | 118 | (9.24) | 1.15 (0.68–1.95) |
| Thrombophlebitis | 0 | (0.00) | 6 | (0.47) | Omitted |
| Cellulitis | 12 | (5.38) | 108 | (8.46) | 1.57 (0.84–2.91) |
| Edema | 34 | (15.25) | 449 | (35.16) | 2.85 (1.94–4.20) |
| Itching | 45 | (20.18) | 520 | (40.72) | 2.61 (1.84–3.70) |
| Pigmentation | 31 | (13.90) | 619 | (48.47) | 5.71 (3.84–8.51) |
| Ulceration | 23 | (10.31) | 402 | (31.48) | 3.93 (2.51–6.18) |
After adjusting for all confounding factors, we observed that there is a 3.93-fold risk (p < 0.01) for developing ulceration in those patients who had blood reflux and varices only in smaller veins and when varices were absent in truncal veins. Edema and pigmentation in lower limb are known to be important indicators of morbidity in CVD and these symptoms were significantly associated with reflux in veins with smaller diameter (< 4 mm). Risk of developing edema was 2.85-fold (p < 0.01) and risk of pigmentation was as high as 5.71-fold (p < 0.01) in patients with varicosities in smaller veins compared with patients with truncal varices.
Discussion
In this study, we systematically analyzed patients with CVD and found that severity of disease is significantly associated with varicosities in veins with smaller diameter. There was a strong relationship between clinical features such as cellulitis, lower limb edema, itching, hyperpigmentation, and ulceration with varicosities of reticular veins and tributaries of superficial veins of legs.
Pain was significantly associated with varicosities of truncal veins such as GSV and SSV. Pain or throbbing sensation is possibly due to the tension created by blood stasis which is likely to be more in large truncal veins. Patients with varices in smaller veins reported incidence of hemorrhage more frequently compared with those with involvement of truncal veins, though the difference was not highly significant. Other severe symptoms of CVD such as edema, hyperpigmentation, and ulceration were significantly associated with varices in veins with < 4 mm diameter, that is, smaller superficial tributaries of major veins and reticular veins.
In our study population, 1,277 patients had reflux and varices only in reticular and tributaries with no reflux in truncal saphenous veins. Our observation corroborates an earlier finding that reflux and ensuing varices can occur in any vein and not necessarily depend on incompetence in truncal saphenous veins.7An earlier study by Carpentier et al reported an association of nonsaphenous varicose veins with female gender in French population.11In our study, however, varicosities of reticular veins and tributaries of superficial veins of legs were found to be not associated with any gender.
Superficial venous system comprises of reticular veins as well as GSV and SSV and their tributaries. The reticular veins drain deoxygenated blood from subcutaneous tissues in the lower extremity and communicate to either tributaries of saphenous veins or the deep veins through perforator.1Reflux in reticular veins or smaller superficial veins results in venous hypertension forcing fluid into the lymphatic and interstitial spaces.12Fluid accumulation in tissue spaces with failure of the lymphatic channels to drain the massive quantity of tissue fluid can result in lower limb edema. Edema marks initiation of lymphatic failure and is the initial stage in the development of other morbidities in patients with CVD.13Progressive fluid accumulation leads to decreased tissue perfusion as well. Following red blood cell leakage into tissues around blood vessels, hemosiderin pigments are released and result in pigmentation and irritation.14Dysregulated apoptosis at tissue level, fibrin cuff formation in capillaries, decreased oxygen saturation, release of oxidants, etc. can contribute to tissue destruction and eventually ulcer formation.15
While analyzing the other risk factors in our study population, age and gender were not found to be significant in association with CVD. Interestingly, we found that a significant number of patients (85.23%) had a positive family history for venous insufficiency. To avoid possible bias in reporting family history, data was considered “positive” only if varicosities are present in close relatives of the study participants. The majority of study subjects (92%) had to stand for longer periods as part of their occupation. These findings suggest that activities or occupations with prolonged standing may contribute to varicosities in the presence of other factors such as genetic susceptibility.
The majority of patients (76.4%) in our study had involvement of tributaries of both superficial veins and truncal veins. Complications were severe in such patients. As the aim of the study was to identify differences in morbidity based on the diameter or size of the afflicted veins, such patients were removed from our final analysis.
CVD affects a large proportion of the population possibly because of susceptibility and lifestyle factors which increase the risk. Prevalence of CVD in adult population is reported to be between 10% and 60% among different populations.16 17The high prevalence necessitates the need for treatment rationing in the public health sector. In several countries such as UK, health care professionals consider a threshold of > 3 mm or even 4.5 mm diameter of afflicted veins to qualify the patient for treatment.3 4 18The treatment approach for reflux in smaller veins is different and difficult when compared with truncal veins.19 20The currently followed screening approach is inappropriate in several instances when patients have symptomatic varicose veins without truncal reflux. To address the above concern, Lane et al assessed the association of maximum vein diameter and clinical severity score with quality of living score in 330 patients.3They did not observe any significant association between maximum vein diameter and clinical stage of the disease. Our study had a large population of 6,350 patients and included patients with varicosities of all vein sizes. In consistent with the observations by Lane et al, we found that varicosity of veins with smaller diameter leads to complicated skin lesions and severe morbidity in patients with CVD. Morbidity is less when the involvement is limited to large truncal veins such as great, small, and accessory saphenous veins. Such patients were treated by modified technique of microfoam sclerotherapy focusing on smaller veins. No significant complications were recorded in patients during the 2 to 6 years of follow-up.21
Our findings thus do not support a role for treatment rationing only for patients with varicosities of veins of large diameter.
Conclusion
Pathogenesis of varicose veins and mechanisms of progression are not fully understood. Intervention based on vein diameter alone results most often in the treatment of patients with asymptomatic disease. Such a criterion could also result in delay in initiating the treatment of patients with afflicted veins with smaller diameter who have a higher chance of clinical complications. Our study indicates that thorough clinical review and Doppler scans to assess the size of veins involved in CVD are necessary in identifying patients who need early intervention to prevent complication of the disease.
Acknowledgments
The authors thank Director, Rajiv Gandhi Centre for Biotechnology, Thiruvananthapuram, and Director, St. Thomas Hospital, Changanassery, for providing facilities for conducting this study. We acknowledge Dr N. Radhakrishnan Foundation Trust for the support.
Competing Interests The authors have no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions
NR, CCK, and SS contributed to the conception and design of the study, acquisition of data, analysis, and drafting of the paper. SS and CCK analyzed, interpreted the results, and critically reviewed the manuscript, and DG and RJ contributed to the acquisition of data and drafting of the paper. All authors have read and approved the final manuscript.
References
- 1.Meissner M H. Lower extremity venous anatomy. Semin Intervent Radiol. 2005;22(03):147–156. doi: 10.1055/s-2005-921948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent J R, Jones G T, Hill G B, van Rij A M.Failure of microvenous valves in small superficial veins is a key to the skin changes of venous insufficiency J Vasc Surg 201154(6, Suppl):62S-9S.e1–e3. [DOI] [PubMed] [Google Scholar]
- 3.Lane T RA, Varatharajan L, Fiorentino F et al. Truncal varicose vein diameter and patient-reported outcome measures. Br J Surg. 2017;104(12):1648–1655. doi: 10.1002/bjs.10598. [DOI] [PubMed] [Google Scholar]
- 4.Harris M R, Davies R J, Brown S, Jones S M, Eyers P S, Chester J F. Surgical treatment of varicose veins: effect of rationing. Ann R Coll Surg Engl. 2006;88(01):37–39. doi: 10.1308/003588406X82998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joh J H, Kim W S, Jung I M, Park K H, Lee T, Kang J M; Consensus Working Group.Consensus for the treatment of varicose vein with radiofrequency ablation Vasc Spec Int 20143004105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eklöf B, Rutherford R B, Bergan J J et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(06):1248–1252. doi: 10.1016/j.jvs.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 7.Seidel A C, Miranda F, Jr, Juliano Y, Novo N F, dos Santos J H, de Souza D F. Prevalence of varicose veins and venous anatomy in patients without truncal saphenous reflux. Eur J Vasc Endovasc Surg. 2004;28(04):387–390. doi: 10.1016/j.ejvs.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Khilnani N M, Min R J. Imaging of venous insufficiency. Sem Interv Radiol. 2005;22:178–184. doi: 10.1055/s-2005-921950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joh J H, Park H C. The cutoff value of saphenous vein diameter to predict reflux. J Korean Surg Soc. 2013;85(04):169–174. doi: 10.4174/jkss.2013.85.4.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lionis C, Erevnidou K, Antonakis N, Argyriadou S, Vlachonikolis I, Katsamouris A; CVI Research Group.Chronic venous insufficiency. A common health problem in general practice in Greece Int Angiol 2002210186–92. [PubMed] [Google Scholar]
- 11.Carpentier P H, Maricq H R, Biro C, Ponçot-Makinen C O, Franco A. Prevalence, risk factors, and clinical patterns of chronic venous disorders of lower limbs: a population-based study in France. J Vasc Surg. 2004;40(04):650–659. doi: 10.1016/j.jvs.2004.07.025. [DOI] [PubMed] [Google Scholar]
- 12.Perrin M, Ramelet A A. Pharmacological treatment of primary chronic venous disease: rationale, results and unanswered questions. Eur J Vasc Endovasc Surg. 2011;41(01):117–125. doi: 10.1016/j.ejvs.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 13.Mortimer P S, Pearson I C. Lymphatic function in severe chronic venous insufficiency. Phlebolymphology. 2004;44:253–257. [Google Scholar]
- 14.Nicholls S C. Sequelae of untreated venous insufficiency. Sem Interv Radiol. 2005;22:162–168. doi: 10.1055/s-2005-921960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown J. The role of the fibrin cuff in the development of venous leg ulcers. J Wound Care. 2005;14(07):324–327. [PubMed] [Google Scholar]
- 16.Ahti T M, Mäkivaara L A, Luukkaala T, Hakama M, Laurikka J O. Effect of family history on the incidence of varicose veins: a population-based follow-up study in Finland. Angiology. 2009;60(04):487–491. doi: 10.1177/0003319709335510. [DOI] [PubMed] [Google Scholar]
- 17.Robertson L, Evans C, Fowkes F GR. Epidemiology of chronic venous insufficiency. Phlebology. 2008;11:2–5. doi: 10.1258/phleb.2007.007061. [DOI] [PubMed] [Google Scholar]
- 18.Aetna Insurance Inc.Varicose Veins; 2015http://www.aetna.com/cpb/medical/data/1_99/0050.html. Accessed August 10, 2017
- 19.Subramonia S, Lees T A. The treatment of varicose veins. Ann R Coll Surg Engl. 2007;89(02):96–100. doi: 10.1308/003588407X168271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carradice D, Wallace T, Gohil R, Chetter I. A comparison of the effectiveness of treating those with and without the complications of superficial venous insufficiency. Ann Surg. 2014;260(02):396–401. doi: 10.1097/SLA.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 21.Radhakrishnan N, Jayakrishnan R, Deepu G.Microfoam sclerotherapy for varicose veins: a retrospective analysis of a modified technique Indian J Surg 201577(Suppl 3):816–821. [DOI] [PMC free article] [PubMed] [Google Scholar]