Association between digestive symptoms and sleep disturbance: a cross-sectional community-based study (original) (raw)
Abstract
Background
This study was conducted to analyze the association between digestive symptoms and sleep disturbance, and to determine if any digestive symptoms are related to sleep disturbance.
Methods
This was a cross-sectional study of 5792 subjects surveyed in a community-based cohort. Subjects provided information regarding the quality of sleep as assessed by the Pittsburgh Sleep Quality Index (PSQI), as well as digestive symptoms as assessed by the Gastrointestinal Symptom Rating Scale (GSRS). Logistic regressions were used to examine factors associated with sleep quality.
Results
The mean PSQI global score of the no sleep disturbances group (n = 4948) was 3.92 (SD = 2.14), while that of the sleep disturbance group (n = 844) was 11.18 (SD = 2.17). The association between digestive symptoms and sleep disturbance was evaluated by logistic regression after adjusting for cofounding factors. The results revealed that sleep disturbances were associated with digestive symptoms (aOR = 1.29, 95% CI = 1.22–1.36), especially abdominal pains (aOR = 1.63, 95% CI = 1.19–2.25), acid regurgitation (aOR = 1.48, 95% CI = 1.17–1.86), abdominal distension (aOR = 1.80, 95% CI = 1.42–2.28), and eructation (aOR = 1.59, 95% CI = 1.24–2.03).
Conclusions
Digestive symptoms and sleep disturbances seem to be associated. These results will help medical professionals to effectively diagnose and manage patients with sleep disturbance. Furthermore, subsequent studies using comprehensive longitudinal data should be conducted to confirm the results of the present study.
Keywords: Digestive symptoms, Sleep disturbances, The Korean Genome and Epidemiology Study_Ansan and Ansung cohort, The Korean Medicine Data Center
Background
Sleep disturbance encompasses various sleep disorders including insomnia, hypersomnia, circadian rhythm sleep-wake disorders, sleep apnea, narcolepsy and cataplexy, parasomnia and sleep related movement disorders [1, 2].
Many people experience sleep disturbances worldwide, the most common of which is insomnia [3]. According to the American Psychiatric Association, 10–20% of people complain of significant sleep problems to their primary care physician [4]. Moreover, 16.6% of adults aged 50 years or older reported having nocturnal sleep problems in a prior study [5]. The finding that many older adults are commonly dissatisfied with sleep quality and report sleep-related diseases indicates that the prevalence of sleep disturbances increases as the population ages [6].
These sleep disturbances are associated with the occurrence of various diseases. Specifically, it has been reported that sleep disturbances may be associated with psoriasis, suicidal ideation, alcohol use disorders, mental health difficulties, and nocturnal acid reflux [7–10]. There have also been reports of sleep disturbances being associated with functional gastrointestinal disorders (FGID). In a systematic review of patients with irritable bowel syndrome (IBS), there was evidence of a positive correlation between subjectively, but not objectively, reported sleep disturbances and gastrointestinal symptom exacerbation among people with IBS [11]. In a study of 3600 Chinese patients, FGID were significantly associated with excessive daytime sleepiness [12]. Moreover, a 2002 study of Japanese people who underwent annual health checkups at a hospital revealed positive associations between gastroesophageal reflux disease and sleep disturbances [13]. Furthermore, a population-based study of 25,844 Norwegians revealed that sleep disturbances and gastroesophageal reflux symptoms (GERS) were bidirectionally associated, suggesting that sleep disturbances may lead to GERS and vice versa [14].
In the Neijing, which is an ancient oriental medical text, stomach disharmony is the major cause of the sleep disturbance [15]. Although stomach disharmony is a general term referring to various functional disorders of the stomach [16], it is uncertain if specific digestive symptoms are related to stomach disharmony.
Despite studies conducted to date, there is a lack of research regarding the relationship between sleep disturbances and digestive symptoms using large population datasets. Furthermore, we are aware of no studies that have examined the interaction between sleep disturbances and specific digestive symptoms. Therefore, this community-based study was conducted to: (a) investigate the association between digestive symptoms and sleep disturbance, and (b) analyze whether any digestive symptoms are related to sleep disturbance.
Methods
Study design and data source
We conducted a cross-sectional analysis of the community-based cohort survey of the Korean Medicine Data Center (KDC) that was conducted from June 2012 to December 2014. The KDC is a consortium project consisting of hospital, clinic, and community-based cohort data collected in the Republic of Korea and hospital data collected in Japan, China, Vietnam and the United States of America [17–19]. The KDC community-based cohort data was collected as part of a follow-up survey of the “The Korean Genome and Epidemiology Study (KoGES)_Ansan and Ansung cohort,” which is an ongoing, community-based cohort study that started in 2001 [17, 20]. The participants in the KoGES_Ansan and Ansung cohort were residents aged 40 to 69 who were extracted by two-stage cluster sampling based on gender, age distribution, and information regarding the governing district obtained in the 2000 census [21].
These survey data were collected through face-to-face interviews with participants using structured questionnaires after the interviewers were trained according to a pre-established protocol. During interviews, information was obtained regarding the participants’ characteristics, results of physical examinations and laboratory analyses, symptoms, etc.
Variables definition
Sleep disturbances
The quality and disturbance of sleep was evaluated by the PSQI, a self-administered questionnaire that assesses usual sleep habits during the previous month [22, 23]. The individual items generate seven component scores pertaining to subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medicine, and daytime dysfunction [22]. The sum of these seven components yields a global PSQI score that ranges from 0 to 21 [22]. The PSQI is useful for distinguishing between sleep disorders and good sleepers. The cutoff score of the original English version of the PSQI is 5 points and the diagnostic sensitivity and specificity of good or poor sleepers are 89.6 and 86.5%, respectively [22]. However, the cutoff score of the Korean version of the PSQI is 8.5, and the diagnostic sensitivity and specificity are 94.3 and 84.4%, respectively [23]. Therefore, we defined a PSQI of 8.5 or more as having sleep disturbance.
Digestive symptoms
The digestive conditions of each subject were assessed by the digestion component portion of the Gastrointestinal Symptom Rating Scale (GSRS) [24, 25]. The GSRS is a disease specific instrument consisting of 15 items combined into five Gastrointestinal (GI) symptom clusters that depict reflux, abdominal pain, indigestion, diarrhea and constipation [25]. Among the GSRS, we used the digestion component portion, which consists of seven items, abdominal pains, heartburn, acid regurgitation, sucking sensations in the epigastrium, nausea and vomiting, borborygmus, abdominal distension and eructation.
Statistical analysis
We selected gender, age, marital status, education level and lifestyle (tobacco use, alcohol use, physical activity and obesity) as covariates because we could obtain this information from our data based on previously published studies of the risk factors for sleep disturbances [26–29]. Baseline characteristics were summarized using descriptive statistics such as the proportion, mean and standard deviation. Continuous variables were categorized as appropriate categorical variables. The association between several factors and sleep disturbance was investigated using logistic regression after adjusting for confounding factors, then analyzed using two models. Model 1 was adjusted for demographic characteristics (gender, age, marital status, education level, tobacco use, alcohol use, physical activity and obesity) and total score of GSRS digestion. Model 2 was adjusted for demographic characteristics and seven items of GSRS digestion (abdominal pains, heartburn, acid regurgitation, sucking sensations in the epigastrium, nausea and vomiting, borborygmus, abdominal distension and eructation). A two-sided _p_-value < 0.05 was considered to indicate statistical significance. All data manipulations and statistical analyses were performed using Stata/MP version 15 (StataCorp LP, College Station, TX, USA).
Results
Demographic characteristics of participants
The total number of participants in the KDC community-based survey from 2012 to 2014 was 5805, all of whom signed an informed consent form. Among the participants, 5792 completed the Pittsburgh Sleep Quality Index (PSQI) and the Gastrointestinal Symptom Rating Scale (GSRS) (Fig. 1). The mean PSQI global score of the no sleep disturbances group (n = 4948) was 3.92 (SD = 2.14), while that of the sleep disturbance group (n = 844) was 11.18 (SD = 2.17). Demographic information describing the participants is presented in Table 1. Overall, 67.77 and 76.66% of the sleep disturbance group were female and married, respectively. (Table 1).
Fig. 1.
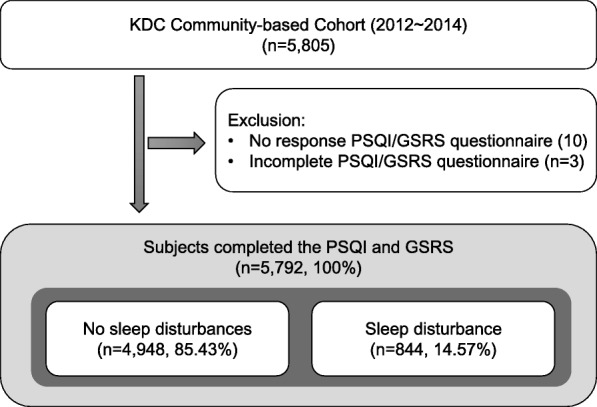
Selection of the cohort population. Among the participants, 5792 completed the Pittsburgh Sleep Quality Index (PSQI) and the Gastrointestinal Symptom Rating Scale (GSRS)
Table 1.
Demographic characteristics of 5,792 subjects
| No sleep disturbances (n = 4,948) | Sleep disturbance (n = 844) | p | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Gender | < 0.001 | ||||
| Male | 2,418 | 48.87 | 272 | 32.23 | |
| Female | 2,530 | 51.13 | 572 | 67.77 | |
| Age (year) | |||||
| Mean (SD) | 61.99 | 9.64 | 64.06 | 10.15 | < 0.001 |
| < 65 | 3,180 | 64.27 | 459 | 54.38 | < 0.001 |
| 65≤ | 1,768 | 35.73 | 385 | 45.62 | |
| Marital status | < 0.001 | ||||
| Spouselessa | 696 | 14.07 | 197 | 23.34 | |
| Married | 4,252 | 85.93 | 647 | 76.66 | |
| Education level | < 0.001 | ||||
| Elementary school (≤6 years) | 1,649 | 33.33 | 380 | 45.02 | |
| Middle school (6-9 years) | 990 | 20.01 | 178 | 21.09 | |
| High school or above (≥9 years) | 2,309 | 46.67 | 286 | 33.89 | |
| Tobacco | < 0.001 | ||||
| No | 4,274 | 86.38 | 767 | 90.88 | |
| Yes | 647 | 13.62 | 77 | 9.12 | |
| Alcohol | 0.001 | ||||
| No | 2,842 | 57.44 | 537 | 63.6 | |
| Yes | 2,106 | 42.56 | 307 | 36.37 | |
| Physical activity | 0.005 | ||||
| No | 1,749 | 35.10 | 341 | 40.40 | |
| Yes | 3,199 | 64.65 | 503 | 59.60 | |
| Obesityb | 0.468 | ||||
| No | 2,883 | 58.27 | 503 | 59.60 | |
| Yes | 2,065 | 41.73 | 341 | 40.40 |
Correlation between digestive symptoms and sleep disturbances
The sleep disturbances group reported significantly more intense and frequent symptoms than the no sleep disturbances group for all GSRS digestion items (Table 2). Moreover the overall magnitude of the difference between the digestive symptoms and the sleep disturbances was moderate except for the nausea and vomiting symptoms.
Table 2.
Gastrointestinal Symptom Rating Scale (GSRS)-digestive items of 5,792 subjects
| No sleep disturbances (n = 4,948) | Sleep disturbance (n = 844) | p | Effect Size (Cohen’s d) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Estimate | 95% CI | |||
| GSRS-total digestion score | 0.34 | 1.01 | 0.78 | 1.49 | < 0.001 | −0.40 | −0.48 | −0.33 |
| Abdominal pains | 0.02 | 0.17 | 0.08 | 0.30 | < 0.001 | −0.28 | −0.35 | −0.21 |
| Heartburn | 0.87 | 0.29 | 0.15 | 0.41 | < 0.001 | − 0.23 | − 0.30 | − 0.15 |
| Acid regurgitation | 0.06 | 0.26 | 0.13 | 0.38 | < 0.001 | −0.24 | − 0.32 | − 0.17 |
| Sucking sensations in the epigastrium | 0.02 | 0.17 | 0.06 | 0.30 | < 0.001 | −0.19 | −0.26 | − 0.11 |
| Nausea and vomiting | 0.02 | 0.14 | 0.03 | 0.20 | 0.0043 | −0.11 | −0.18 | − 0.03 |
| Borborygmus | 0.03 | 0.19 | 0.07 | 0.20 | < 0.001 | −0.19 | −0.27 | − 0.12 |
| Abdominal distension | 0.06 | 0.25 | 0.14 | 0.39 | < 0.001 | −0.30 | −0.38 | − 0.23 |
| Eructation | 0.05 | 0.24 | 0.13 | 0.35 | < 0.001 | −0.28 | −0.35 | − 0.21 |
Factors associated with sleep disturbances
The association between digestive symptoms and sleep disturbances was evaluated by logistic regression after adjusting for cofounding factors. In model 1, sleep disturbances were associated with being female (aOR = 1.66, 95% CI = 1.41–1.96), age (aOR = 1.02, 95% CI = 1.01–1.03), marital status (aOR = 0.72, 95% CI = 0.60–0.88), high school or above (aOR = 0.79, 95% CI = 0.66–0.94) and total score of GSRS digestion (aOR = 1.29, 95% CI = 1.22–1.36). In model 2, sleep disturbances were associated with being female (aOR = 1.66, 95% CI = 1.41–1.97), age (aOR = 1.02, 95% CI = 1.01–1.03), marital status (aOR = 0.72, 95% CI = 0.59–0.87), high school or above (aOR = 0.79, 95% CI = 0.66–0.94) and four digestive symptoms: abdominal pains (aOR = 1.63, 95% CI = 1.19–2.25), acid regurgitation (aOR = 1.48, 95% CI = 1.17–1.86), abdominal distension (aOR = 1.80, 95% CI = 1.42–2.28), eructation (aOR = 1.59, 95% CI = 1.24–2.03) (Table 3).
Table 3.
Factors associated with sleep disturbance
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p | aOR | 95% CI | p | |
| Female | 1.66 | 1.41–1.96 | < 0.001 | 1.66 | 1.41–1.97 | < 0.001 |
| Age | 1.02 | 1.01–1.03 | < 0.001 | 1.02 | 1.01–1.03 | < 0.001 |
| Marital status | 0.72 | 0.60–0.88 | 0.001 | 0.72 | 0.59–0.87 | 0.001 |
| High school or above (≥9 years) | 0.79 | 0.66–0.94 | 0.007 | 0.79 | 0.66–0.94 | 0.008 |
| Total score of GSRS digestion | 1.29 | 1.22–1.36 | < 0.001 | |||
| Abdominal pains | – | 1.63 | 1.19–2.25 | 0.003 | ||
| Acid regurgitation | – | 1.48 | 1.17–1.86 | 0.001 | ||
| Abdominal distension | – | 1.80 | 1.42–2.28 | < 0.001 | ||
| Eructation | – | 1.59 | 1.24–2.03 | < 0.001 | ||
| constant | 0.06 | 0.03–0.11 | < 0.001 | 0.05 | 0.03–0.10 | < 0.001 |
Discussion
In this study, we demonstrated that sleep disturbances were associated with digestive symptoms (abdominal pains, acid regurgitation, abdominal distension and eructation), with some being closely associated.
According to many previous studies, sleep disturbances comprise an independent disease and a risk factor for many other diseases, including GI disorders such as IBS, gastroesophageal reflux disease, gastric ulcer, and duodenal ulcer [11–14, 30–34]. Moreover, a few studies have attempted to identify the cause of the association between sleep disturbances and sereval diseases. For example, Reddy attempted to identify differences in GI symptoms among poor sleepers based on variations in genes and found that the brain-derived neurotrophic factor genotype may be related to the etiology of poor sleep quality and chronic abdominal pain [35]. In addition, sleep disturbances were significant predictors of somatic complaints [36].
Similar to our findings, recent studies have commonly regarded female and age as risk factors related to sleep disturbances [26, 27]. For example, Dalmases reported that sleep health in a European population was associated with increasing age and being female [37]. Additionally, Choi reported that the incidence of GI diseases among sleep disturbance patients was much higher in females, as well as individuals of older age and with higher income in a multivariable analysis conducted using the National Health Insurance Service–National Sample Cohort [30]. In contrast to our findings, Mullane showed that obesity and smoking were risk factors for sleep disturbances [38], while Miller found interactive effects between insomnia and alcohol use among young adult veterans [39]. Accordingly, much more research is needed to investigate the relationship between demographic factors and sleep disturbances.
It should be noted that it was difficult to compare our findings with those of previous studies because we could not locate prior investigations that examined the relationship between specific digestive symptoms and sleep disturbance. However, the specific digestive symptoms presented in patients with sleep disturbance may be related to stomach disharmony, and these can be helpful to diagnosis of disease patterns in Traditional Chinese and Korean medicine.
Several limitations need to be considered while interpreting the results of this study. First, our findings were based on an association between digestive symptoms and sleep disturbance. To accurately evaluate the causal relationships, longitudinal data should be assessed. Second, there is the potential for self-reporting bias because we used perceived digestive symptoms tools and sleep quality tools; however, the GSRS and PSQI are good tools that have been shown to be reliable and valid in many studies. Third, we did not determine why only certain digestive symptoms among several digestive symptoms may be related to poor sleep quality. Accordingly, additional research is needed to investigate the genes, pain, and other mechanisms of digestive symptoms and sleep disturbances.
Conclusions
Digestive symptoms and sleep disturbances seem to be associative. These results will help medical professionals to effectively diagnose and manage patients with sleep disturbance. Furthermore, future studies using comprehensive longitudinal data should be conducted to confirm the results of the present study.
Acknowledgements
Not applicable.
Funding
This work was supported by the “Establishment of Korean medicine genome and epidemiology infrastructure” of the Korea Institution of Oriental Medicine grant funded by the Korean Government [grant numbers K18091]. The role of the funding body was data collection.
Availability of data and materials
The datasets analyzed during the current study are available from a public database of the KDC upon reasonable request.
- - E-mail: kdc@kiom.re.kr
- - Website: https://www.kiom.re.kr/eng/
Abbreviations
FGID
Functional Gastrointestinal Disorders
GERS
Gastroesophageal Reflux Symptoms
GI
Gastrointestinal
GSRS
Gastrointestinal Symptom Rating Scale
KDC
Korean Medicine Data Center
KoGES
Korean Genome and Epidemiology Study
PSQI
Pittsburgh Sleep Quality Index
Authors’ contributions
MKH conceptualized and designed the study, performed the statistical analysis and wrote the manuscript. SWL designed and built the Korean Medicine Data Center (KDC). SWL and YHB obtained this research data. MKH and SWL revised the manuscript. All authors approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Dongguk University, Gyeongju s (DRG IRB 20160009). Patient consent was exempted because of the total anonymity of this study data extracted from Korean Medicine Data Center (KDC) (Bioethics and safety act. Article 16).
Consent for publication
Not applicable.
Competing interests
The author has no conflicts of interest to declare with respect to the authorship and/or publication of this article.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Min Kyung Hyun, Email: mk3three@gmail.com.
Younghwa Baek, Email: aori79@kiom.re.kr.
Siwoo Lee, Phone: +82-42-868-9555, Email: bfree@kiom.re.kr.
References
- 1.AASM. International classification of sleep disorders, revised: Diagnostic and coding manual. Chicago, Illinois: American Academy of Sleep Medicine; 2001.
- 2.Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–1394. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 3.Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimäki M. Sleep epidemiology—a rapidly growing field. In: Oxford University Press. 2011. [DOI] [PMC free article] [PubMed]
- 4.What Are Sleep Disorders? [https://www.psychiatry.org/patients-families/sleep-disorders/what-are-sleep-disorders] or [https://www.psychiatry.org/].
- 5.Stranges S, Tigbe W, Gomez-Olive FX, Thorogood M, Kandala NB. Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep. 2012;35(8):1173–1181. doi: 10.5665/sleep.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: 1. Sleep disorders commonly found in older people. Can Med Assoc J. 2007;176(9):1299–1304. doi: 10.1503/cmaj.060792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaines KK. Sleepless in America: burning the candle at both ends? At what cost? Urol Nurs. 2016;36(3):109–110. doi: 10.7257/1053-816X.2016.36.3.109. [DOI] [PubMed] [Google Scholar]
- 8.Franic T, Kralj Z, Marcinko D, Knez R, Kardum G. Suicidal ideations and sleep-related problems in early adolescence. Early Interv Psychiatry. 2014;8(2):155–162. doi: 10.1111/eip.12035. [DOI] [PubMed] [Google Scholar]
- 9.Hunt EJ, Greenberg N, Jones N. Poor sleep after military deployment: associations with mental health difficulties. Occupational Medicine. 2016;66:669–675. [DOI] [PubMed]
- 10.Henry AL, Kyle SD, Chisholm A, Griffiths CE, Bundy C. A cross-sectional survey of the nature and correlates of sleep disturbance in people with psoriasis. Br J Dermatol. 2017;177(4):1052-1059. [DOI] [PubMed]
- 11.Tu Q, Heitkemper M, Jarrett M, Buchanan D. Sleep disturbances in irritable bowel syndrome: a systematic review. Neurogastroenterol Motil. 2017;29:e12946. [DOI] [PubMed]
- 12.Wu S, Chen S, Zhao Y, Ma X, Wang R, He J. Associations Between Excessive Daytime Sleepiness and Functional Gastrointestinal Disorders: A Population-based Study in China. J Neurogastroenterol Motil. 2017;23(2):298-305. [DOI] [PMC free article] [PubMed]
- 13.Okuyama M, Takaishi O, Nakahara K, Iwakura N, Hasegawa T, Oyama M, Inoue A, Ishizu H, Satoh H, Fujiwara Y. Associations among gastroesophageal reflux disease, psychological stress, and sleep disturbances in Japanese adults. Scand J Gastroenterol. 2016:1–6. [DOI] [PubMed]
- 14.Lindam A, Ness-Jensen E, Jansson C, Nordenstedt H, Åkerstedt T, Hveem K, Lagergren J. Gastroesophageal reflux and sleep disturbances: a bidirectional association in a population-based cohort study, the HUNT study. Sleep. 2016;39(7):1421. doi: 10.5665/sleep.5976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tessenow PUUaH . University of California Press. 2011. Huang Di nei jing su wen. [Google Scholar]
- 16.WHO. WHO international standard terminologies on traditional medicine in the Western Pacific region: World Health Organization; 2007.
- 17.Lee S-W. The guide book: Korean medicine data center (KDC) (2006-2014) Korea: Institute of Oriental Medicine; 2014. [Google Scholar]
- 18.Baek Y, Lee S. Development of Korean medicine data center(KDC) teaching dataset to enhance utilization of KDC. J Sasang Constitut Med. 2017;29(3):242–247. [Google Scholar]
- 19.Jin H-J, Baek Y, Kim H-S, Ryu J, Lee S. Constitutional multicenter bank linked to Sasang constitutional phenotypic data. BMC Complement Altern Med. 2015;15(1):46. doi: 10.1186/s12906-015-0553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim Y, Han BG. Cohort profile: the Korean genome and epidemiology study (KoGES) consortium. Int J Epidemiol. 2017;46(2):e20. doi: 10.1093/ije/dyv316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ifeacho S, Narula T. Association of snoring with chronic bronchitis. Arch Intern Med. 2008;168(17):1930. doi: 10.1001/archinte.168.17.1930-a. [DOI] [PubMed] [Google Scholar]
- 22.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 23.Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh sleep quality index. Sleep and Breathing. 2012;16(3):803–812. doi: 10.1007/s11325-011-0579-9. [DOI] [PubMed] [Google Scholar]
- 24.Kwon S, Jung H-K, Hong JH, Park HS. Diagnostic validity of the Korean gastrointestinal symptom rating scale (KGSRS) in the assessment of gastro-esophageal reflux disease. Ewha Med J. 2008;31(2):73–80. doi: 10.12771/emj.2008.31.2.73. [DOI] [Google Scholar]
- 25.Svedlund J, Sjödin I, Dotevall G. GSRS—a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988;33(2):129–134. doi: 10.1007/BF01535722. [DOI] [PubMed] [Google Scholar]
- 26.Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev. 2016;25:21–30. doi: 10.1016/j.smrv.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ohayon MM. Epidemiological overview of sleep disorders in the general population. Sleep Med Res. 2011;2(1):1–9. doi: 10.17241/smr.2011.2.1.1. [DOI] [Google Scholar]
- 28.Muscogiuri G, Barrea L, Annunziata G, Di Somma C, Laudisio D, Colao A, Savastano S. Obesity and sleep disturbance: the chicken or the egg? Crit Rev Food Sci Nutr. 2018:1–8. [DOI] [PubMed]
- 29.Lei WY, Chang WC, Wong MW, Hung JS, Wen SH, Yi CH, Liu TT, Chen JH, Hsu CS, Hsieh TC, et al. Sleep disturbance and its association with gastrointestinal symptoms/diseases and psychological comorbidity. Digestion. 2018:1–8. [DOI] [PubMed]
- 30.Choi WJ, Lee BW, Kim DW, Lee H, Lee S, Oh ST, Kim WJ, Park JY. A study on the status and characteristics of sleep disorders and comorbidities using national health insurance data. National Health Insurance Service (NJIS) Ilsan Hospital Institute of Health Insurance & Clinical Research: Ilsan, Republic of Korea; 2015.
- 31.Patel A, Hasak S, Cassell B, Ciorba MA, Vivio EE, Kumar M, Gyawali CP, Sayuk GS. Effects of disturbed sleep on gastrointestinal and somatic pain symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44(3):246–258. doi: 10.1111/apt.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Iwakura N, Fujiwara Y, Shiba M, Ochi M, Fukuda T, Tanigawa T, Yamagami H, Tominaga K, Watanabe T, Arakawa T. Characteristics of sleep disturbances in patients with gastroesophageal reflux disease. Internal medicine (Tokyo, Japan) 2016;55(12):1511. doi: 10.2169/internalmedicine.55.5454. [DOI] [PubMed] [Google Scholar]
- 33.Jansson C, Nordenstedt H, Wallander MA, Johansson S, Johnsen R, Hveem K, Lagergren J. A population-based study showing an association between gastroesophageal reflux disease and sleep problems. Clin Gastroenterol Hepatol. 2009;7(9):960–965. doi: 10.1016/j.cgh.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Khanijow V, Prakash P, Emsellem HA, Borum ML, Doman DB. Sleep dysfunction and gastrointestinal diseases. Gastroenterology & hepatology. 2015;11(12):817–825. [PMC free article] [PubMed] [Google Scholar]
- 35.Yamawaki H, Futagami S, Shimpuku M, Sato H, Wakabayashi T, Maruki Y, Kodaka Y, Nagoya H, Shindo T, Kawagoe T, et al. Impact of sleep disorders, quality of life and gastric emptying in distinct subtypes of functional dyspepsia in Japan. J Neurogastroenterol Motil. 2014;20(1):104–112. doi: 10.5056/jnm.2014.20.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schlarb AA, Classen M, Hellmann SM, Vogele C, Gulewitsch MD. Sleep and somatic complaints in university students. J Pain Res. 2017;10:1189–1199. doi: 10.2147/JPR.S125421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dalmases M, Benítez ID, Mas A, Garcia-Codina O, Medina-Bustos A, Escarrabill J, Saltó E, Buysse DJ, Roure N, Sánchez-de-la-Torre M, et al. Assessing sleep health in a European population: results of the Catalan health survey 2015. PLoS One. 2018;13(4):e0194495. doi: 10.1371/journal.pone.0194495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mullane N, Bradley C. An investigation into the association between demographic and morbidity factors, and sleep disturbance. Ir J Med Sci. 2018;187(1):163-175. [DOI] [PubMed]
- 39.Miller MB, DiBello AM, Carey KB, Pedersen ER. Insomnia moderates the association between alcohol use and consequences among young adult veterans. Addict Behav. 2017;75:59–63. doi: 10.1016/j.addbeh.2017.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from a public database of the KDC upon reasonable request.
- - E-mail: kdc@kiom.re.kr
- - Website: https://www.kiom.re.kr/eng/