Tobacco and the lung cancer epidemic in China (original) (raw)
Abstract
China is in the midst of a lung cancer epidemic on an unprecedented scale. In 2015, there were an estimated 733,000 new lung cancer cases (17% of total cancer incidence) and 610,000 deaths (21.7% of total cancer mortality) in China. Lung cancer is the most commonly diagnosed cancer and the leading cause of cancer mortality in China. Tobacco smoke exposure is the primary factor driving current lung cancer trends. In 2015, smoking prevalence was 27.7% (52.1% among men and 2.7% among women). China has taken substantial steps to control tobacco use in recent years, including 19 cities implementing comprehensive smoke free laws and expansion of cessation services. However, significant challenges remain in order to meet the 2030 Healthy China goal of reducing smoking prevalence to 20%. In particular, ongoing attention is needed to continuing to control secondhand smoke exposure, to further enhance smoking cessation services, and to address novel alternative nicotine delivery devices (ANDS).
Keywords: Lung cancer, tobacco, health policy, epidemiology, behavioral research
China is in the midst of a lung cancer epidemic on an unprecedented scale. In 2015, there were an estimated 733,000 new lung cancer cases (17% of total cancer incidence) and 610,000 deaths (21.7% of total cancer mortality) in China. Lung cancer is the most commonly diagnosed cancer and the leading cause of cancer mortality in China. While 70% of lung cancer cases occur in men (1), among women lung cancer is second to breast cancer in frequency of diagnosis and remains the leading cause of cancer death. As lung cancer incidence and mortality have been decreasing in most high-income countries, age-standardized lung cancer incidence and mortality rates in China have been steadily increasing since 1990 (2,3).
The most substantial factor driving recent lung cancer trends in China is tobacco smoke exposure. China has the largest smoking population in the world, with around 316 million adult smokers, and accounts for nearly one-third (30%) of smokers and 40% of tobacco consumption worldwide (4). In 2015, smoking prevalence was 27.7% (52.1% among men and 2.7% among women) (5). Although the prevalence of smoking among women in China is relatively low, exposure to secondhand smoke is high. China has taken some important steps for tobacco control, including ratifying the World Health Organization Framework Convention on Tobacco Control (FCTC) and implementing comprehensive smoke free workplace laws in a number of cities. However, smoking prevalence has remained relatively stable over the past decade (6). At the same time, new developments, such as the introduction of alternative nicotine delivery systems (ANDS) and rising disparities in tobacco use, pose new challenges for the future.
This paper reviews trends in lung cancer and tobacco use in China, along with progress in tobacco control efforts. Overall, tobacco smoking causes over 1 million deaths annually in China and this number is projected to rise to 2 million in 2030 and 3 million by 2050 (7). While tobacco smoke exposure is associated with several cancers as well as cardiovascular and lung disease, the strength of the association with lung cancer and the high lung cancer burden in China warrant a particular focus on lung cancer.
Tobacco and lung cancer in China
Tobacco is a major contributor to the overall cancer burden in China, accounting for the largest share of the cancer burden among major risk factors (8,9). According to a recent analysis based on data from China’s cancer registration system, in 2014, an estimated 383,167 cancer deaths in adults 30 years or older in were attributable to cigarette smoking (both active and passive smoking), with 342,854 of these deaths occurring in men (23.8% of male cancer deaths) and 40,313 in women (4.8% of female cancer deaths). For lung cancer alone, active smoking accounts for 54.7% of lung cancer mortality among men and 6.4% among women. Secondhand smoke exposure is estimated to account for another 10% of female lung cancer deaths (10).
The burden of tobacco use in China has increased over the past two decades and has become more similar to the pattern seen in high income countries where cigarette smoking began earlier. Chen and colleagues compared data from two nation-wide prospective studies initiated in 1991 and 2006. Among men, the excess mortality risk associated with smoking doubled over this period. Patterns of smoking behavior were changing in the 1980s and 1990s with increasing urbanization and economic development. Smokers born after 1970, compared with those born a generation before, started smoking earlier (at 20 rather than 25 years), primarily smoked manufactured cigarettes, and smoked with greater intensity. As a result, the relative risk of lung cancer, comparing smokers with nonsmokers, increased from 1.95 to 2.58 between the two cohorts, and increase of about 50% in the excess risk. Relative risks were also higher for urban versus rural male smokers, likely because rural smokers smoked less or started later. In the later study, urban male smokers had a relative risk of lung cancer of 3.78 compared with non-smokers (7).
Nevertheless, the population attributable fraction of lung cancer due to smoking remains lower in China compared with some other countries. While cigarette smoking accounts for around 55% of male lung cancer mortality in China, figures from other countries are much higher (11). For example, among Korean men, cigarette smoking was estimated to account for 71% of lung cancer mortality (12). Similarly, while tobacco smoking accounts for around 21% of cancer deaths in China, that proportion is lower than what has been estimated for a number of other Asian countries (13). Additionally, estimates of the relative risk of lung cancer associated with cigarette smoking are much greater in high income countries, such as the U.S., compared with China (14). This difference may be due to differences in smoking behavior. For example, in the U.S. and other countries where the tobacco epidemic is in an advanced stage, smoking behavior tends to begin in adolescence (15). While in China, male smoking typically begins after age 20 (though that number has been decreasing). Later initiation reduces lifetime years of exposure and, in turn, lifetime risk. A similar phenomenon has been described in Japan where smoking initiation also occurs later and relative risks associated with smoking are lower than in the U.S (16).
Understanding trends of lung cancer and tobacco smoke exposure in China is also complicated by the role of competing risks, particularly indoor and outdoor air pollution. In particular, high lung cancer mortality among non-smoking women in China has been attributed to household air pollution from cooking and the use of coal for heating (17,18). Lung cancer among women in China has historically been higher in the northeast of the country, where indoor heating exposure would be expected to be higher (19). Geographic studies have also linked ambient air pollution levels to lung cancer mortality in China (20). A recent analysis also estimated that (based on 2,005 figures) 13.7% of lung cancer deaths (10% for men and 18% for women) could be attributed to PM2.5 exposure (21).
The potential role of air pollution in lung cancer has received increasing attention recently in China. Several studies have identified a rise in adenocarcinoma relative to other lung cancer subtypes since 2000, though these studies have so far been limited to specific cities or institutions where historical lung cancer histology records exist. For example, at the National Cancer Hospital in Beijing, among male lung cancer patients, the frequency of adenocarcinomas, as a proportion of all lung cancers diagnosed, almost doubled (from 21.96% to 43.36%) from 2002 to 2012, while the proportion of squamous cell carcinomas decreased. This trend may be partly (though not wholly) due to improved diagnosis, as the proportion of unclassified cancers also decreased (22). Meanwhile, reports in popular media have highlighted “a surge in ‘non-smoking’ lung cancer” and expert opinions that the risk in adenocarcinoma is evidence of a growing impact of air pollution on lung cancer (23,24).
While squamous cell carcinoma is almost exclusively linked to cigarette smoking, adenocarcinoma has multiple causes (including air pollution and cigarette smoking). Additionally, the relative risks differ substantially for different lung cancer subtypes in relation to tobacco exposure (25). However, adenocarcinoma is also strongly linked with cigarette smoking (26). Moreover, a similar shift in lung cancer histology was seen earlier in the U.S. and European countries (27,28). Epidemiologic studies suggest that the increase in adenocarcinoma in Western countries is due to changes in cigarette design and smoking behavior. During the 1960s and 1970s, tobacco companies increasingly marketed “light” and low-tar cigarette brands with lower machine-measured levels of tar and nicotine, and these brands came to dominate the market in large part due to the perception that they were less harmful than other cigarettes. As smokers switched to low-tar cigarettes, they tended to inhale more deeply, transporting carcinogens more distally into the lungs where adenocarcinomas arise; At the same time, greater use of reconstituted tobacco, with higher concentrations of nitrosamines, may have also contributed to a shift towards adenocarcinomas (27).
China has experienced a similar shift towards ‘low tar’ cigarettes, though more recently. Average machine-measured tar content per cigarette decreased from about 27 milligrams in 1983 to 17 milligrams in 2000 and 12 milligrams in 2010 (29). Thus, it is likely that the increase in adenocarcinomas relative to other lung cancer subtypes is attributable, at least in part, to changes in cigarette design and smoking behavior. At the same time, long term air pollution exposure may also account for some portion of adenocarcinomas. However, it is also important to note that lung cancer risk is the result of long-term exposure and, thus, long cancer trends today reflect exposures in previous decades, not current air pollution levels reported recently in Beijing and other cities. Ambient air pollution exposure may have an increasing impact on lung cancer in the future, but long term tobacco smoke exposure remains the primary risk factor in current lung cancer trends.
Tobacco use in China
Smoking prevalence has been consistently high among Chinese men since the 1980s. Male smoking prevalence reached a peak of 63% in 1990 but has declined somewhat since then (Figure 1). According to the 2015 China Adult Tobacco Survey, current adult smoking prevalence is 27.7% (52.1% among men and 2.7% among women), showing little change in recent years (5). However, smoking prevalence and behavior varies by age and other demographic factors. For example, for men, smoking prevalence ranges from 36.5% among those 15–24 years of age to 60% among those 45–64 years. Similarly, for women smoking prevalence ranges from 0.5% in the 15–24 age group to 6.9% in those 65 years and older. Smoking prevalence is also higher among those with only a primary or secondary school education compared to those with a university education. Additionally, the survey also reports that the majority (80%) of Chinese adults are aware that smoking causes lung cancer, though awareness for other health effects is lower, such as stroke (31%) and myocardial infarction (42.6%) (30).
Figure 1.
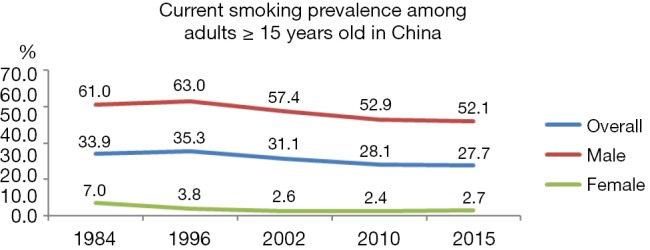
Smoking prevalence from 1984 to 2015 among Chinese adults.
Smoking prevalence also varies across cities and provinces within China. According to the 2013–2014 China City Adult Tobacco Survey, prevalence among a select group of cities ranged from 17.7% in Qingdao to 24.5 in Shenyang (31). While in large, cosmopolitan cities like Beijing and Shanghai, smoking bans have been implemented and public support for tobacco control has grown recently (32), in more traditional provinces and those where tobacco is grown, such as Yunnan province, tobacco use remains high (33,34). In general, smoking is much less accepted for women in China and smoking prevalence among women remains relatively low, especially in more traditional, rural areas in the south of China (35). However, smoking among women is higher in Northeast China and in urban areas like Beijing and Tianjin, where female smoking is more socially acceptable (36,37). Thus, attitudes towards and cultural acceptability of smoking, along with socioeconomic status and education level, contribute to patterns of smoking prevalence.
Prevalence of smoking among Chinese youth remains low (6.9% among middle school students) in relation to adult prevalence. Additionally, smoking initiation tends to occur later; only about 32% of daily smokers start smoking before the age of 18 (6). However, youth smoking prevalence is higher among some population subgroups. According to the most recent China Global Youth Tobacco Survey (GYTS), prevalence was higher among boys (11.2%) compared with girls (2.2%) and among those living in rural areas (7.8%) compared with urban areas (4.8%). Students in western China had the highest tobacco use prevalence (10.3%), followed by the students in central (6.4%) and eastern China (4.5%). Other factors associated with tobacco use included having smoking parents (especially mother), friends or teachers, having more pocket money, being exposed to tobacco advertising, and positive attitudes towards smoking behavior (38). An earlier survey including both adolescents in school and not in school found smoking prevalence to be over 50% higher for those out of school compared with those in school (39). Additionally, the perceived acceptability of female smoking and female smoking prevalence may be increasing, particularly among young women in urban areas, which poses a challenge for the future (40-42). In general, the factors associated with youth smoking in China are similar to those seen elsewhere.
Progress and pitfalls
Tobacco control in China
China has taken important steps for tobacco control. China ratified the World Health Organization international public health treaty, the Framework Convention on Tobacco Control (FCTC), in 2003 and enacted it in January 2006. In 2009 and 2010, the Ministry of Health and the Ministry of Education both established regulations requiring hospitals and schools to implement smoke free policies (43). The National People’s Congress included statements in support of controlling tobacco use in China’s 12th and 13th Five-Year Plans (44). For example, the 13th Five-Year Plan, covering 2016–2020, asserts that “We will make a major push to prohibit smoking in public places” (45). Additionally, in 2015 new regulations imposed a ban on tobacco advertising in mass media, public places, public transport, and outdoors, as well as on tobacco advertising targeting youth.
An important “tipping point” came with a December 29, 2013, notice from the General Offices of the Central Committee of the Communist Party of China and the State Council titled “Notice on Officials Shall Take the Lead in Making Public Places Smoke Free”. The notice states that government officials should become role models and take the lead in promoting smoke free spaces and obeying smoking restrictions. Additionally, the notice prohibits the use of official funds to purchase tobacco products and prohibits smoking and gifting of cigarettes at official functions. In addition to damaging health, the text notes, officials’ smoking in public places “also damages the image of the government and the officials, bringing in negative impact”. This notice received broad attention in the international media and was applauded by tobacco control advocates (46).
However, in the absence of a comprehensive national smoke free law, municipalities have taken the lead in enacting smoke-free legislation for public places in China. Before the 2008 Olympic Games, Beijing enacted smoking bans in a range of public places, including medical institutions, child care centers, transport stations, cultural sites, and sporting venues. Shanghai followed in preparation for the 2010 World Expo, banning smoking in schools, hospitals, sports stadiums, and other specific public spaces. These early policies fell short of banning smoking within all indoor workplaces, but more recently a new wave of comprehensive smoke free policies have been implemented by at least 19 cities in China. Beijing (June 2015), Shanghai (March 2017), Shenzhen (January 2017), Xi’an (November 2018) and other cities have implemented comprehensive smoking bans in indoor public places (47). These comprehensive policies have been effective in reducing smoking in public spaces. For example, the success of the Beijing smoke free policy has provided a model for successful efforts in other cities (48). The national Tobacco Control Office of the Chinese Center for Disease Control and Prevention has provided support for the implementation and evaluation of local smoke free policies, national and local mass media campaigns to help to raise awareness about the risks of secondhand smoke and prompt some restaurants and private companies to implement their own smoke-free policies (49). Surveys also show considerable public support for smoke free laws (50).
Nevertheless, there remain ongoing challenges to long-term progress in tobacco control, and reducing lung cancer, in China. The following section focuses on three current topics or issues in tobacco control in China: protection from secondhand smoke exposure, promotion of tobacco cessation, and the potential impact of novel products. Each of these areas requires ongoing attention in order to reduce the burden of lung cancer in China.
Protection from secondhand smoke exposure
Past surveys have documented the high prevalence of secondhand smoke exposure in China. An estimated 70% of the Chinese population, or more than 740 million people, are regularly exposed to secondhand smoke at work or home, a proportion higher than that seen in other high-burden low- and middle-income countries (51). According to data from the International Tobacco Control Policy Evaluation Project, more than 90% of smokers and former smokers surveyed in China reported observing smoking in restaurants and bars, far more than in any of the other 15 countries surveyed (52). This situation is exacerbated by the fact that social norms in China are more favorable toward smoking compared with other high- and middle-income countries. One national survey found that 53% of smokers believed that Chinese society disapproves of smoking, compared with 79% in the United States and 80% in Thailand (53).
However, new data from the 2015 China Adult Tobacco Survey indicates that secondhand smoke exposure has decreased since 2010, though still remains high in some settings (5). From 2010 to 2015, secondhand smoke exposure among nonsmokers decreased in restaurants, government buildings, health-care facilities, schools, and public transportation. However, the change was greater in some areas than others. The proportion of people who reported being exposed to secondhand smoke in restaurants dropped only modestly from 87.6% to 76.3%, and continues to be high. Similarly, the proportion who reported exposure at home or in the workplace decreased only slightly and remains close to 50% in both settings. However, the proportion reporting exposure in primary and secondary schools (both indoors and outdoors) dropped from 34.6% to 17.2%, a decrease of 50%. Additionally, reported exposure on public transport decreased from 29% to 16.4%. About a quarter of respondents reported exposure to secondhand smoke in medical institutions, despite efforts to make such spaces smoke free. Nevertheless, public support for smoke free policies remains high. Even for restaurants, where support for smoke-free policies was lowest, 75.1% of nonsmokers and 55.3% of smokers supported smoke-free policies.
Promoting tobacco cessation
Attention to tobacco cessation has increased in China over the past several years. According to the 2015 China Adult Tobacco Survey, 58.2% smokers received advice to quit smoking from a health professional during the past 12 months, compared with only 33.2% in 2010. However, quitting behavior remains relatively low. Among ever smokers, 18.7% had quit smoking, 25.6% attempted to quit in the past 12 months but relapsed, and 55.7% did not make a quit attempt in the past 12 months. Quit intentions are also low. Only 7.0% of current smokers have plan to quit in next month and 17.6% in the next 12 months.
There are substantial challenges to increasing cessation in Chinese smokers. Among 20 countries in the International Tobacco Control Policy Evaluation project, China reported the third highest percentage of male smokers (59%) who said that they have no plans to quit smoking. Additionally, Chinese smokers show high levels of tobacco dependence compared with other countries, though they are less likely to perceive themselves as addicted. Only 8% of Chinese male smokers say they are addicted to smoking “a lot”, compared with 62% of US smokers reporting they are “very addicted” to cigarettes (54). China also has fewer former smokers compared with other nations. An analysis of Global Adult Tobacco Survey data from 16 countries showed that, in China, about 13% of people who were ever daily smokers have quit compared with 49% in the United States (55). Studies have found that the level of interest in quitting among smokers in China is very low compared with some high- and middle-income countries, including the United States, where a majority of smokers are interested in quitting. Among those who had made a quit attempt in the past 12 months, 92% reported not using any method (such as medication or counseling) to assist with cessation in China (56) compared with 68% not using any method in the United States (57).
However, there are also some promising trends in relation to tobacco cessation in China as well. The Tobacco Control Office of the China Centers for Disease Control and Prevention provides support and technical assistance to provincial health departments in developing tobacco cessation activities. Government funds support the development of three smoking cessation clinics annually in each province, along with the development of smoking cessation hotlines. Additionally, the use of mobile health interventions to support cessation, through the use of text messaging or social media apps like WeChat, may have substantial promise in China, given widespread use of mobile technology. Numerous apps are already available to Chinese consumers, though most have not been evaluated and may not be evidence-based (58). Some pilot studies have shown promising results (59,60). But more research is needed to evaluate the effectiveness of mobile health interventions for tobacco cessation in China.
Novel products and regulation
While the vast majority of tobacco use in China is in the form of conventional cigarettes, alternative nicotine delivery devices (ANDS), such as e-cigarettes, are in use by a segment of the population. According to the 2015 China Adult Tobacco Survey, 40.5% of Chinese adults have heard of e-cigarettes, 3.1% have used them, and 0.5% are current users. Marketing of e-cigarettes has expanded rapidly in China in recent years (61). Retail e-cigarette shops appear in rural counties as well as large cities and e-cigarettes can be easily purchased online (62). Unlike conventional cigarettes, advertising of e-cigarettes is not regulated in China. Online advertisements are prevalent and include claims about health benefits (63). In some places, e-cigarette promotions have taken place on school campuses (64).
According to the China Global Youth Tobacco Survey, 1.2% of middle school students reported they used an e-cigarette in past 30 days, higher than adult prevalence. Almost half (45.0%) of students have heard of e-cigarettes. Factors associated with e-cigarette awareness and/or use include having experimented with cigarette smoking, having parents or close friends who smoke, exposure to tobacco advertising and anti-tobacco messages, positive attitudes toward smoking, and having more pocket money. Additionally, findings suggest a relationship between e-cigarette use and conventional cigarettes. Students who were aware of or using e-cigarettes had more positive views about tobacco use in general, such as saying that tobacco helps people feel comfortable in social situations or that smoking makes young people look more attractive. They were also more likely to say they would use a tobacco product in the next 12 months or use a tobacco product if offered by a friend. No significant relationship was seen in this study between use of e-cigarettes and wanting to stop smoking or having tried stopping in the past 12 months. Thus, the data do not show any indication that e-cigarettes are being used as smoking cessation devices among Chinese youth (65).
While prevalence of past 30-day e-cigarette use among youth in China remains relatively low, given the lack of regulations on e-cigarette sales and marketing in China and widespread tobacco advertising in retail tobacco shops, there is reason for concern that e-cigarette use may increase among Chinese adolescents, as seen in other countries (66,67). Additionally, the factors identified in youth e-cigarette use and experimentation in China are similar to those associated with conventional cigarette smoking in China (38). This trend raises concern because studies have shown e-cigarette use to be associated with greater intention to smoke and with subsequent initiation of conventional cigarette smoking (66). As in other countries, it is unclear how ANDS use will develop in the future or how it might impact use of other tobacco products.
Tobacco control and the future of lung cancer in China
As part of its Health China 2030 strategy, China has established a goal of reducing adult smoking prevalence from 27.7% to 20% by 2030 (68). This is an ambitious goal that will require implementation of strong comprehensive tobacco control measures (69). Substantial progress has been made in controlling tobacco use in China to date. The implementation of local smoke free laws and related health campaigns and media attention have led to increased awareness of the health effects of cigarette smoking. However, some significant challenges remain in achieving long term reductions in tobacco use. As described above, implementation of smoke free laws and the development of tobacco cessation services are ongoing but remain underdeveloped. Additionally, the introduction of novel, unregulated tobacco products, including e-cigarettes, may impact smoking initiation and behavior, particularly among youth.
One of the notable features of tobacco use and lung cancer in China is the wide disparities seen across cities, regions, and rural versus urban settings. As noted previously, cigarette smoking prevalence among a select group of cities included in the China City Adult Tobacco Survey ranged from 17.7% in Qingdao to 24.5 in Shenyang (31). An analysis of the provincial level cancer burden due to tobacco use found that the population attributable fraction for male lung cancer due to smoking ranged from 50.8% in Quizhou to 30.8 in Xinjiang (10). Tobacco use behavior also varies by socioeconomic characteristics. As in many other countries, smoking prevalence in China is associated with lower socioeconomic status and educational levels. Additionally, lower income smokers tend to start earlier and are less likely to successfully quit, which further increases their risk of lung cancer and other diseases (70,71). At the same time, as China has undergone dramatic economic growth in recent years, the distribution of wealth and resources varies across regions, and these differences have contributed to considerable disparities in cancer control and treatment outcomes (72).
In the U.S. and other countries where the tobacco epidemic is in a mature stage, progress in reducing tobacco use and related disease and death has not been equally distributed across population groups (73). Indeed, tobacco use, and the resultant health effects have become increasingly concentrated in low-income populations. A similar phenomenon may be occurring in China, as tobacco use is decreasing and tobacco control measures are being strengthened in some provinces and large urban areas, but other parts of the country and rural area are not experiencing the same changes. Findings from the ITC surveys show that awareness of the health effects of smoking and exposure to information about the harms of smoking are lower in rural areas, compared with urban areas, in China (54). Cigarettes are still regarded as a common gift and form of social currency in China, especially in rural areas where awareness of the health effects of tobacco use is lower (74).
The tobacco epidemic remains at an earlier stage in China compared with North American and Europe, and the full impact of tobacco smoking patterns in recent decades on cancer mortality may have not yet been realized. There is a substantial lag time between tobacco use and lung cancer diagnosis or death (13). Thus, tobacco control measures taken now may not substantially impact cancer rates for another decade or more. Indeed, a recent analysis projected that even if all risk reduction targets are met under the United Nations Agenda for Sustainable Development, which sets a target to reduce premature mortality from non-communicable diseases by one-third by 2030, this goal could be met for cardiovascular disease and chronic respiratory diseases, but not for cancer (75). Nevertheless, if no action is taken to reduce tobacco use, the burden for cancer and other NCDs will surely continue to grow into the future. Thus, the sooner additional actions are taken to control tobacco use and promote tobacco cessation, the sooner a reduction in the burden from lung cancer can be achieved. While China faces as large burden of lung cancer, it also has a great opportunity to reduce the global burden of lung cancer.
Acknowledgments
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 2.Fang JY, Dong HL, Wu KS, et al. Characteristics and Prediction of Lung Cancer Mortality in China from 1991 to 2013. Asian Pac J Cancer Prev 2015;16:5829-34. 10.7314/APJCP.2015.16.14.5829 [DOI] [PubMed] [Google Scholar]
- 3.Cao M, Chen W. Epidemiology of lung cancer in China. Thorac Cancer 2019;10:3-7. 10.1111/1759-7714.12916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Cancer Institute. The Economics of Tobacco and Tobacco Control. National Cancer Institute Tobacco Control Monograph 21. NIH Publication No 16-CA-8029A. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, 2016.
- 5.China Center for Disease Control and Prevention 2015 China Adult Tobacco Survey Report. Beijing, 2015. Available online: http://www.tcrc.org.cn/UploadFiles/2016-03/318/201603231215175500.pdf
- 6.China Center for Disease Control and Prevention 2010 Global Adult Tobacco Survey (GATS) China Country Report. Beijing, 2010. Available online: http://www.who.int/tobacco/surveillance/survey/gats/en_gats_china_report.pdf
- 7.Chen Z, Peto R, Zhou M, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet 2015;386:1447-56. 10.1016/S0140-6736(15)00340-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Islami F, Chen WQ, Yu XQ, et al. Cancer deaths and cases attributable to lifestyle factors and infections in China, 2013. Ann Oncol 2017;28:2567-74. [DOI] [PubMed] [Google Scholar]
- 9.Chen W, Xia C, Zheng R, et al. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health 2019;7:e257-69. 10.1016/S2214-109X(18)30488-1 [DOI] [PubMed] [Google Scholar]
- 10.Xia C, Zheng R, Zeng H, et al. Provincial-level cancer burden attributable to active and second-hand smoking in China. Tob Control 2018. [Epub ahead of print]. 10.1136/tobaccocontrol-2018-054583 [DOI] [PubMed] [Google Scholar]
- 11.Tobacco smoke and involuntary smoking. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monogr Eval Carcinog Risks Hum 2004;83:1-1438. [PMC free article] [PubMed] [Google Scholar]
- 12.Park S, Jee SH, Shin HR, et al. Attributable fraction of tobacco smoking on cancer using population-based nationwide cancer incidence and mortality data in Korea. BMC Cancer 2014;14:406-17. 10.1186/1471-2407-14-406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kristina SA, Endarti D, Thavorncharoensap M. Burden of cancer attributable to tobacco smoking in member countries of the Association of Southeast Asian Nations (ASEAN), 2012. Cancer Epidemiol 2016;44:84-90. 10.1016/j.canep.2016.08.005 [DOI] [PubMed] [Google Scholar]
- 14.Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med 2013;368:351-64. 10.1056/NEJMsa1211127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elders MJ, Perry CL, Eriksen MP, et al. The report of the Surgeon General preventing tobacco use among young people. Am J Public Health 1994;84:543-7. 10.2105/AJPH.84.4.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Funatogawa I, Funatogawa T, Yano E. Trends in smoking and lung cancer mortality in Japan, by birth cohort, 1949-2010. Bull World Health Organ 2013;91:332-40. 10.2471/BLT.12.108092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xue Y, Jiang Y, Jin S, et al. Association between cooking oil fume exposure and lung cancer among Chinese nonsmoking women: a meta-analysis. Onco Targets Ther 2016;9:2987-92. 10.2147/OTT.S100949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao Y, Wang S, Aunan K, et al. Air pollution and lung cancer risks in China--a meta-analysis. Sci Total Environ 2006;366:500-13. 10.1016/j.scitotenv.2005.10.010 [DOI] [PubMed] [Google Scholar]
- 19.Xu ZY, Blot WJ, Fraumeni JF., Jr Geographic variation of female lung cancer in China. Am J Public Health 1986;76:1249-50. 10.2105/AJPH.76.10.1249-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao Q, Rui G, Liang Y. Study on PM2.5 pollution and the mortality due to lung cancer in China based on geographic weighted regression model. BMC Public Health 2018;18:925. 10.1186/s12889-018-5844-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo Y, Zeng H, Zheng R, et al. The burden of lung cancer mortality attributable to fine particles in China. Sci Total Environ 2017;579:1460-6. 10.1016/j.scitotenv.2016.11.147 [DOI] [PubMed] [Google Scholar]
- 22.Zou XN, Lin DM, Wan X, et al. Histological subtypes of lung cancer in Chinese males from 2000 to 2012. Biomed Environ Sci 2014;27:3-9. [DOI] [PubMed] [Google Scholar]
- 23.Surge in 'non-smoking' lung cancer in China. The Straits Times. August 12, 2017. Available online: https://www.straitstimes.com/asia/east-asia/surge-in-non-smoking-lung-cancer-in-china
- 24.Lung Cancer Cases Linked to Air Quality. China Daily. February 27, 2014. Available online: http://www.china.org.cn/environment/2014-02/27/content_31610749.htm
- 25.Pesch B, Kendzia B, Gustavsson P, et al. Cigarette smoking and lung cancer--relative risk estimates for the major histological types from a pooled analysis of case-control studies. Int J Cancer 2012;131:1210-9. 10.1002/ijc.27339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang P, Cerhan JR, Vierkant RA, et al. Adenocarcinoma of the lung is strongly associated with cigarette smoking: further evidence from a prospective study of women. Am J Epidemiol 2002;156:1114-22. 10.1093/aje/kwf153 [DOI] [PubMed] [Google Scholar]
- 27.Thun MJ, Lally CA, Flannery JT, et al. Cigarette smoking and changes in the histopathology of lung cancer. J Natl Cancer Inst 1997;89:1580-6. 10.1093/jnci/89.21.1580 [DOI] [PubMed] [Google Scholar]
- 28.Devesa SS, Bray F, Vizcaino AP, et al. International lung cancer trends by histologic type: male:female differences diminishing and adenocarcinoma rates rising. Int J Cancer 2005;117:294-9. 10.1002/ijc.21183 [DOI] [PubMed] [Google Scholar]
- 29.Zou XN, Lin D, Chao A, et al. Histological subtypes of lung cancer in Chinese women from 2000 to 2012. Thorac Cancer 2014;5:447-54. 10.1111/1759-7714.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheng HG, McBride O, Phillips MR. Relationship between knowledge about the harms of smoking and smoking status in the 2010 Global Adult Tobacco China Survey. Tob Control 2015;24:54-61. 10.1136/tobaccocontrol-2013-051163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liang X. editor. Report of China City Adult Tobacco Survey 2013–14: A 14-City Experience. Atlanta: CDC Foundation, 2015. [Google Scholar]
- 32.Kegler MC, Hua X, Solomon M, et al. Factors associated with support for smoke-free policies among government workers in Six Chinese cities: a cross-sectional study. BMC Public Health 2014;14:1130. 10.1186/1471-2458-14-1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cai L, Wu X, Goyal A, et al. Patterns and socioeconomic influences of tobacco exposure in tobacco cultivating rural areas of Yunnan Province, China. BMC Public Health 2012;12:842. 10.1186/1471-2458-12-842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang T, Barnett R, Rockett IR, et al. The impact of regional economic reliance on the tobacco industry on current smoking in China. Health Place 2015;33:159-71. 10.1016/j.healthplace.2014.12.015 [DOI] [PubMed] [Google Scholar]
- 35.Mao A, Bristow K, Robinson J. Caught in a dilemma: why do non-smoking women in China support the smoking behaviors of men in their families? Health Educ Res 2013;28:153-64. 10.1093/her/cys078 [DOI] [PubMed] [Google Scholar]
- 36.Li Z, Yao Y, Han W, et al. Smoking prevalence and associated factors as well as attitudes and perceptions towards tobacco control in Northeast China. Int J Environ Res Public Health 2015;12:8606-18. 10.3390/ijerph120708606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen X, Li X, Stanton B, et al. Cigarette smoking among rural-to-urban migrants in Beijing, China. Prev Med 2004;39:666-73. 10.1016/j.ypmed.2004.02.033 [DOI] [PubMed] [Google Scholar]
- 38.Xiao L, Feng GZ, Jiang Y, et al. Tobacco use rate and associated factors in middle school students in China. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:567-71. [DOI] [PubMed] [Google Scholar]
- 39.Yang G, Ma J, Chen AP, et al. Smoking among adolescents in China: 1998 survey findings. Int J Epidemiol 2004;33:1103-10. 10.1093/ije/dyh225 [DOI] [PubMed] [Google Scholar]
- 40.Han J, Chen X. A Meta-Analysis of Cigarette Smoking Prevalence among Adolescents in China: 1981-2010. Int J Environ Res Public Health 2015;12:4617-30. 10.3390/ijerph120504617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wan X, Shin SS, Wang Q, et al. Smoking among young rural to urban migrant women in China: a cross-sectional survey. PLoS One 2011;6:e23028. 10.1371/journal.pone.0023028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sansone N, Yong HH, Li L, et al. Perceived acceptability of female smoking in China. Tob Control 2015;24 Suppl 4:iv48-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiao D, Wang C, Chen H, et al. Making Hospitals in China smoke-Free: a Prospective study of implementing the new standard. Nicotine Tob Res 2013;15:2076-80. 10.1093/ntr/ntt098 [DOI] [PubMed] [Google Scholar]
- 44.The National People's Congress of the People's Republic of China. The Twelfth Five-Year Plan for National Economic and Social Development of the People's Republic of China. Beijing: 2011.
- 45.The National People's Congress of the People's Republic of China. The Thirteenth Five-Year Plan for Economic and Social Development of the People's Republic of China (2016-2020). Beijing: Central Compilation & Translation Press, 2016. Available online: http://en.ndrc.gov.cn/newsrelease/201612/P020161207645765233498.pdf
- 46.Mackay J. China: the tipping point in tobacco control. Br Med Bull 2016;120:15-25. 10.1093/bmb/ldw043 [DOI] [PubMed] [Google Scholar]
- 47.Hu Y, Sun X, Yuan Z, et al. Another step change for tobacco control in China? Lancet 2015;386:339-40. 10.1016/S0140-6736(15)61409-X [DOI] [PubMed] [Google Scholar]
- 48.Xiao L, Jiang Y, Liu X, et al. Smoking reduced in urban restaurants: the effect of Beijing Smoking Control Regulation. Tob Control 2017;26:e75-8. 10.1136/tobaccocontrol-2016-053026 [DOI] [PubMed] [Google Scholar]
- 49.Redmon P, Koplan J, Eriksen M, et al. The Role of Cities in Reducing Smoking in China. Int J Environ Res Public Health 2014;11:10062-75. 10.3390/ijerph111010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Q, Hyland A, O'Connor R, et al. Support for smoke-free policies among smokers and non-smokers in six cities in China: ITC China Survey. Tob Control 2010;19 Suppl 2:i40-6. 10.1136/tc.2009.029850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Song Y, Zhao L, Palipudi KM, et al. Global Adult Tobacco Survey (GATS) Collaborative Group Tracking MPOWER in 14 countries: results from the Global Adult Tobacco Survey, 2008-2010. Glob Health Promot 2016;23:24-37. 10.1177/1757975913501911 [DOI] [PubMed] [Google Scholar]
- 52.ITC Project. Smoke-free Policies: ITC Cross-Country Comparison Report. University of Waterloo; Waterloo, Ontario, 2012. [Google Scholar]
- 53.ITC Project and Office of Tobacco Control, China CDC. ITC China Project Report. Findings from the Wave 1 to 3 Surveys (2006-2009). University of Waterloo, Waterloo, Ontario, Canada, and Office of Tobacco Control, Chinese Center for Disease Control and Prevention, Beijing, China. Beijing: China Modern Economic Publishing House, 2012. [Google Scholar]
- 54.ITC Project and Office of Tobacco Control, China CDC. ITC China Project Report. Findings from the Wave 1 to 5 Surveys (2006-2015). University of Waterloo, Waterloo, Ontario, Canada, and Office of Tobacco Control, Chinese Center for Disease Control and Prevention, Beijing, China. Beijing: China Modern Economic Publishing House, 2017. [Google Scholar]
- 55.Giovino GA, Mirza SA, Samet JM, et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet 2012;380:668-79. 10.1016/S0140-6736(12)61085-X [DOI] [PubMed] [Google Scholar]
- 56.Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. N Engl J Med 2011;364:2469-70. 10.1056/NEJMc1102459 [DOI] [PubMed] [Google Scholar]
- 57.Centers for Disease Control and Prevention Quitting smoking among adults—United States, 2001—2010. MMWR Morb Mortal Wkly Rep 2011;60;1513-9. [PubMed] [Google Scholar]
- 58.Cheng F, Xu J, Su C, et al. Content Analysis of Smartphone Apps for Smoking Cessation in China: Empirical Study. JMIR Mhealth Uhealth 2017;5:e93. 10.2196/mhealth.7462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liao Y, Wu Q, Kelly BC, et al. Effectiveness of a text-messaging-based smoking cessation intervention ("Happy Quit") for smoking cessation in China: A randomized controlled trial. PLoS Med 2018;15:e1002713. 10.1371/journal.pmed.1002713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Augustson E, Engelgau MM, Zhang S, et al. Text to Quit China: An mHealth Smoking Cessation Trial. Am J Health Promot 2017;31:217-25. 10.4278/ajhp.140812-QUAN-399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jiang N, Ho SY, Lam TH. Electronic cigarette marketing tactics in mainland China. Tob Control 2017;26:230-2. 10.1136/tobaccocontrol-2015-052824 [DOI] [PubMed] [Google Scholar]
- 62.Yao T, Jiang N, Grana R, et al. A content analysis of electronic cigarette manufacturer websites in China. Tob Control 2016;25:188-94. 10.1136/tobaccocontrol-2014-051840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Churk SS. E-cigarette Regulation and Harm Reduction: The Case of Hong Kong. Food Drug Law J 2016;71:634-57. [PubMed] [Google Scholar]
- 64.Peng Q. E-cigarettes are sold around the school and the pupils smoke e-cigarettes there. Guangxi News Network; 2015. Available online: http://news.china.com.cn/live/2015-04/05/content_32160855.htm
- 65.Xiao L, Parascandola M, Wang C, et al. Perception and Current Use of E-cigarettes Among Youth in China. Nicotine Tob Res 2018. [Epub ahead of print]. 10.1093/ntr/nty145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General Report. U.S. Department of Health and Human Services: Rockville, MD, 2016. [Google Scholar]
- 67.Lee JA, Lee S, Cho HJ. The relation between frequency of e-cigarette use and frequency and intensity of cigarette smoking among South Korean adolescents. Int J Environ Res Public Health 2017;14:305. 10.3390/ijerph14030305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tan X, Liu X, Shao H. Healthy China 2030: A Vision for Health Care. Value Health Reg Issues 2017;12:112-4. 10.1016/j.vhri.2017.04.001 [DOI] [PubMed] [Google Scholar]
- 69.Goodchild M, Zheng R. Tobacco control and Healthy China 2030. Tob Control 2018. [Epub ahead of print]. 10.1136/tobaccocontrol-2018-054372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guo H, Sa Z. Socioeconomic differentials in smoking duration among adult male smokers in China: result from the 2006 China Health and Nutrition Survey. PLoS One 2015;10:e0117354. 10.1371/journal.pone.0117354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Droomers M, Huang X, Fu W, et al. Educational disparities in the intention to quit smoking among male smokers in China: a cross-sectional survey on the explanations provided by the theory of planned behaviour. BMJ Open 2016;6:e011058. 10.1136/bmjopen-2016-011058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang Q, Jiao J. Health Disparity and Cancer Health Disparity in China. Asia Pac J Oncol Nurs 2016;3:335-43. 10.4103/2347-5625.195899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.National Cancer Institute. Monograph 22: A Socioecological Approach to Addressing Tobacco-Related Health Disparities Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, 2018. [Google Scholar]
- 74.Yang Y, Wang JJ, Wang CX, et al. Awareness of tobacco-related health hazards among adults in China. Biomed Environ Sci 2010;23:437-44. 10.1016/S0895-3988(11)60004-4 [DOI] [PubMed] [Google Scholar]
- 75.Li Y, Zeng X, Liu J, et al. Can China achieve a one-third reduction in premature mortality from non communicable diseases by 2030? BMC Med 2017;15:132. 10.1186/s12916-017-0894-5 [DOI] [PMC free article] [PubMed] [Google Scholar]