Objective and subjective reduction of cellulite volume using a localized vibrational massage device in a 24‐week randomized intra‐individual single‐blind regression study (original) (raw)
Show available content in
Abstract
Cellulite occurs in females and is a common condition of altered connective tissue matrix and increased adipogenicity with visible dimples and orange‐peel appearance on the skins surface. Whilst advancements in methods continue to help our understanding, attempts to correct the appearance of cellulite topically have yielded limited success. Various kinds of non‐invasive body contouring methods such as whole body vibration have been reported with demonstrable visible improvements in the cellulite condition. The aim of this study was to evaluate volume reduction and improvement of the visible appearance of cellulite as judged both objectively (AEVA‐HE phase‐shift 3‐D fringe projection, macrophotography image grading) and subjectively (questionnaires) after application of a hand‐held localized vibrational device over 24‐weeks. The study was conducted on 40 healthy female volunteers who were instructed how to use the device on defined areas of cellulite of the outside and rear of the thighs (iliotibial band, and over biceps femoris region respectively). The initial 12 weeks of continuous massage application of the study were followed by a 12 week phase in which volunteers were split into 2 subgroups – one for assessment of regression effects and one for continuous application effects. AEVA (skin surface volume) measurements of cellulite‐related dimples correlated with questionnaires and visual image evaluation scoring, in that in the iliotibial region cellulite was significantly reduced at 12 weeks. In the regression subgroup cellulite returned to initial values soon after cessation of treatment, whereas in the continuous application subgroup, cellulite remained diminished. The effect of this device to reduce cellulite as observed in this study proves that continuous use of vibrational massage is beneficial to mitigate visible signs of cellulite.
Keywords: cellulite, claim substantiation in vivo, image analysis, skin profilometry, vibrational massage
The aim of this study was to evaluate volume reduction and improvement of the visible appearance of cellulite as judged both objectively (AEVA‐HE phase‐shift 3‐D fringe projection, macrophotography image grading) and subjectively (questionnaires) after application of a hand‐held localized vibrational device over 24 weeks. AEVA (skin surface volume) measurements of cellulite‐related dimples correlated with questionnaires and visual image evaluation scoring, in that in the iliotibial region cellulite was significantly reduced at 12 weeks. In the regression, subgroup cellulite returned to initial values soon after cessation of treatment, whereas in the continuous application subgroup, cellulite remained diminished.

Introduction
Commonly known as ‘cellulite’, gynoid lipodystrophy (GLD) is a structural, hormonally sensitive and biochemical disorder of the subcutaneous tissue causing alterations in the visual topography of the skin [1, 2]. In females, bands of connective tissue at the buttocks and posterior and lateral thighs are oriented longitudinally. These bands form fibrous septae that localize adipose deposits into channels, and in manifest cellulite, the skin surface changes via a reactive process to sustained hypodermal pressure caused by fat accumulation [3, 4]. The condition affects up to 75–90% of post‐pubescent females, and as a clinical condition, it can considerably affect their quality of life. Cellulite, localized fat deposits and skin flaccidity are common concerns being frequently localized on the thigh and buttock regions, visually characterized by an ‘orange peel’ appearance. Furthermore, cellulite is influenced by female sex hormones, ageing processes, and the subcutaneous fat localized in these areas is metabolically more stable [1, 2, 5].
Advanced methods such as magnetic resonance imaging and spectroscopy have been applied in vivo to improve the understanding of cellulite [6]. Deep indentations of adipose tissue into the dermis and a great increase in the thickness of the inner fat layer in women with cellulite were observed and quantified. A higher percentage of fibrous septae perpendicular to the skin surface was also observed. In other investigations, similar observations have also been made [7]. In vivo confocal reflectance microscopy has been employed to evaluate the epidermal condition in cellulite [8]. Compared with male skin, striae were seen penetrating within the epidermis. The collagen had a dense appearance and stretched in one direction, and the epidermis was thin. It was also suggested that the tissue matrix fibres in cellulite had ‘aged’ with an inability to bind water [8, 9] and since the observed dark fluid spaces index‐matched to water [8], these findings support the issues with oedema and flaccidity. Clearly, cellulite is a condition of altered connective tissue matrix as well as increased adipogenicity. Other investigative methods have been used to characterize cellulite, such as histology [1, 10], ultrasound [11], thermography [12], fringe projection [13] and macrophotography [14].
Attempts to correct the appearance of cellulite have yielded limited success. A plethora of cosmetic formulations are currently available for the treatment of cellulite, yet with a lack of sound scientific and clinical substantiation of so‐called ‘active ingredients’ supporting these products, and most studies conducted are only short term in design. Interestingly, advances in visual methods such as standardized macrophotography have improved non‐invasive evaluation techniques to quantify at least the ‘visible’ efficacy of cosmetic anti‐cellulite products [14]. However, they do not add to any consensus surrounding the actual causes of cellulite despite an understanding that cellulite tissue is characterized by oedema, vasoconstriction, adiposity and a thick unyielding fibrosis [6, 7, 8] all of which are difficult to treat. Some treatments are directed through pharmacological restoration [3], and although topical treatments are wide‐ranging, and often rational, their mechanisms of action still remain elusive. Despite the lack of consensus on the exact mechanisms of cellulite formation, it is clear that removing or diminishing the ‘visual’ aspects of the condition so readily seen on the skin surface makes for a marked improvement in overall skin appearance and thus overall subject well‐being.
Various kinds of non‐invasive body contouring methods, including cryolipolysis, radio‐frequency (RF), low‐level laser therapy (LLLT) and high‐intensity focused ultrasound (HIFU), are available for reducing the volume of subcutaneous adipose tissue or cellulite. [15, 16, 17, 18, 19]. Each procedure has distinct mechanisms for stimulating apoptosis or necrosis of adipose tissue [19]. Other investigations are reported such as whole‐body vibration (WBV) and extra‐corporeal shockwave therapy (ESWT) [19, 20, 21]. WBV demonstrated an improvement in visible cellulite when assessed by blind reviewers [20]. In some adipose conditions, it is reported that vibrational evidence exists for the breakdown of adipose tissue in studies investigating obesity and diabetes [22], and significant correlations exist between changes in percent body fat and blood flow. WBV is also considered an effective means to increase leg blood flow and to reduce adiposity in patients with type II diabetes [23]. WBV treatment has also been shown to be effective in reducing and preventing adiposity with increasing age, and changes in body composition induced by WBV were associated with a stimulation of hepatic lipid metabolism [24]. Such findings could be of value in the understanding of the causes of cellulite in females. Since WBV is, as yet, widely unavailable to the average consumer, hand‐held devices for partial body vibration would be deemed more accessible and practical.
Given reports of the benefits of WBV on cellulite appearance [20], hand‐held vibrating electrical massage devices have come to the fore in the management of cellulite directly by the consumer. Utilizing both objective (AEVA‐HE phase‐shift 3‐D fringe volume and macrophotography image grading) and subjective (questionnaire) methods, the aim of this study was to investigate the performance of a hand‐held localized vibrational device in the reduction of visually assessed cellulite volume over 24 weeks (6 months). The study was a randomized intra‐individual single‐blind regression investigation on healthy female volunteers. The visual evaluation of photographs by trained graders was performed in a blinded manner.
Materials and methods
Test materials
Materials comprised an electric vibrational (cellulite releaZer; Beurer GmbH, Ulm, Germany) massage device in conjunction with an inert silicone oil (cyclopentasiloxane, dimethicone, dimethiconol and ethylhexyl stearate) to prevent skin friction during rubbing of the instrument over the skins surface.
Volunteers
Ethical review board
Approval for this long‐term study was granted by an Ethics Review Board (Institutional Review Board; proDERM GmbH, Hamburg, Gemany).
Study inclusion criteria
Inclusion onto the study required written informed consent to participate and a willingness to comply with instructions; females aged 30–55 years; a body mass index (BMI) of 18–30; having cellulite in the outside of the thigh (iliotibial band) and the rear of the thigh (over the biceps femoris muscle); in these 2 regions having a proDERM cellulite score of 4–6 [14].
Study exclusion criteria
Subjects with a body weight over 100 kg were excluded from the study as well as pregnant/lactating females; drug addicts/alcoholics; subjects with infectious diseases including active skin diseases and neuropathies; diabetics; moles and tattoos on the study area; subjects with conditions which exclude a participation or might influence the test reaction evaluation; involvement with another study; systemic/topical anti‐phlogistic/analgesics within the last 3 days (except for minor pain relief); systemic/topical immunosuppressive drugs and/or antihistamines/anti‐allergics and/or retinoids, in the test area within the last 7 days prior to the start of the study; any topical medication on test area within the last 7 days prior to study commencement and throughout the entire study.
All inclusion and exclusion criteria were checked by a questionnaire during the screening phase and during the course of the study.
Safety criteria and adverse event reporting
Adverse events (AE's) were recorded and documented.
Instructions prior to study commencement
Subjects were instructed not to apply any leave on cosmetics (e.g. creams, lotions and oily cleansing products) or detergents (e.g. soaps, shampoos, bath and shower products) in the test area in the morning prior to the start of the study; use any products with the same indication as the test product in the test areas within the last 4 weeks prior to the start of the study; wear tight clothing such as jeans, that could leave pressure marks on the skin's surface on the day of the study.
Instructions during study
Subjects were instructed to only use the silicone oil provided in the test area throughout the entire course of the study, and no other anti‐cellulite or contouring products; treat only the designated area with the test product and use according to application instructions throughout the study; allowed normal cosmetic products in the test area, without changing brand or using different products; to only carefully shower in the test area (without scrubbing); refrain from contact with water in the test area within the last 2 h prior to instrumental measurements; wear the same (black) undergarments to assure standardized photographs on the measurement days.
Product application
Subjects were instructed how to use the massage device and silicone oil on the outside of the thigh (iliotibial region) and the rear of the thigh (biceps femoris region) as shown in Fig. 1. Product usage was performed every second day on the assigned thigh area for 15 min.
Figure 1.
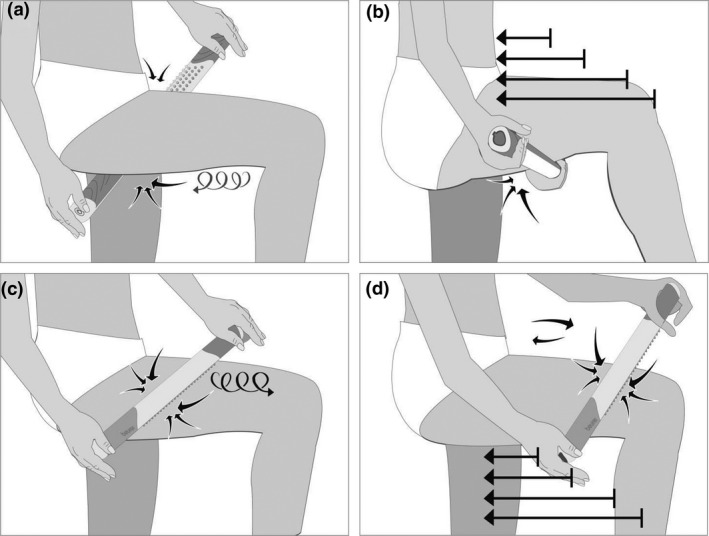
Diagram of mode of use and site of application of the massage device on the biceps femoris (a and b) and the iliotibial region (c and d).
Study design
The study consisted of two phases: In the first phase between Day 1 and Day 85, all 40 subjects applied the device on one leg (B) whereas leaving the other leg untreated (A) (data from 36 subjects were obtained for the biceps femoris region and from 37 subjects for the iliotibial area). In the second phase between Day 85 and Day 168 (regression phase), the study population was divided into two subgroups: Subgroup D which discontinued device application, but followed the other instructions (data from 18 subjects were obtained for both, biceps femoris and iliotibial areas) and subgroup F which continued application on both legs to avoid plolonged assymetric treatment (data from 17 subjects were obtained for biceps femoris and from 16 subjects for iliotibial region). For the regression analysis, the area treated until Day 85 and untreated thereafter until Day 168 (regression subgroup, D) was compared with the corresponding area treated throughout the study (continuous application subgroup, F). The study design is illustrated in Fig. 2.
Figure 2.
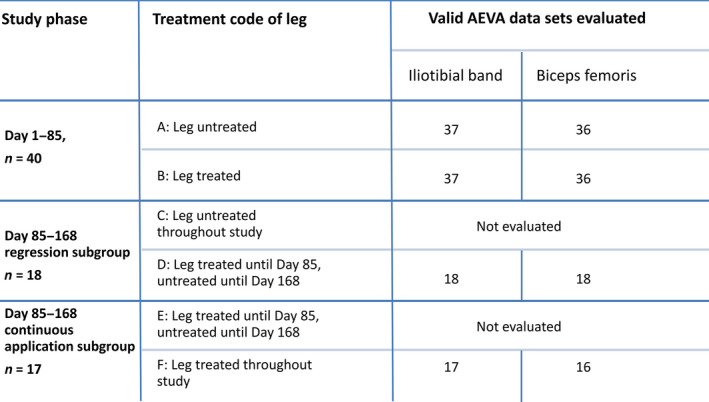
Study design: Study phases, (sub‐) populations, corresponding treated and untreated areas and valid AEVA data sets evaluated.
Measurements
Study schedule
The study was broken down according to the schedule summarized in Table I and performed according to the study protocol and principles and standards of GCP.
Table I.
Study schedule. *, First application of test materials was performed after the instrumental measurements; **, Visual ranking by expert graders was performed at the study site approximately 7 days after Day 85 and after the end of the study; ***, Voluntary subject decision to be included in regression or continuous application subgroup; ****, Before and after the first usage of the test product
| | Screening | Day 1 | Day 2 to 28 | Day 29 | Day 30 to 56 | Day 57 | Day 58 to 84 | Day 85 | Day 86 to 167 | Day 168*** | After Day 168 | | | --------------------------------------------------- | ----- | ----------- | ------ | ------------ | ------ | ------------ | ------ | ------------- | ------------- | ------------- | - | | Informed consent | X | | | | | | | | | | | | In‐/exclusion criteria | X | | | | | | | | | | | | Acclimatization | | X | | | | | | X | | X | | | Capturing of macrophotographs | | X | | | | | | X | | X | | | AEVA measurement | | X | | | | | | X | | X | | | Application of test materials | | X* | X | X | X | X | X | X | X*** | X | | | Compliance check of application | | | | X | | X | | | | | | | Questionnaire (product traits) | | | | | | | | X | | X | | | Questionnaire (pre‐/post‐sensitivity and sensation) | | X**** | | | | | | | | | | | Visual ranking (photos) | | | | | | | | | X | | X |
Climatic conditions
Instrumental measurements took place in an air‐conditioned room at a temperature of 21 ± 1°C and at 50 ± 5% relative humidity. Prior to all measurements, subjects remained in this room for 30 min.
Test procedure
Following subject screening, informed consent and evaluations according to all inclusion/exclusion criteria, subjects were then treated as follows:
Day 1: Subjects were acclimatized for 30 min and completed a questionnaire. Macrophotographs were taken (Baseline) under standardized illumination on the biceps femoris region, and on the iliotibial region of the thighs (iliotibial band) and the rear of the thigh (over the biceps femoris muscle). AEVA measurements were performed, in the same areas. Test products were issued to subjects with instructions for use on the designated areas, and initial product application was performed under guidance. Subjects documented product usage in a diary provided. After the initial use of the massage device, subjects completed a second questionnaire.
Days 2–28: Subjects used the test product as instructed and documented usage in the diary provided.
Day 29: Study compliance evaluation of product usage was undertaken, and correction of usage was made when necessary.
Days 30–56: As days 2–28.
Day 57: As day 29.
Days 58–84: As days 2–28.
Day 85: Subjects were weighed and remained in a climatized room for at least 30 min with thighs uncovered. Image capture and instrumental measurements of the test areas were performed, and subjects completed a questionnaire addressing product traits and sensitivity/sensation of the test areas.
Days 85–167: Following 3 months of usage, subjects were given the option of continuing for a further 3 months. Those which agreed were instructed to use the product on both thighs according to previous usage instructions including diary and were assigned to the continuous application subgroup (F). Those which stopped treatment were identified as the regression subgroup (D). All subjects continued to adhere to all other restrictions.
Day 168: As day 85. In addition, macrophotographs were evaluated by 6 trained graders assessing the ‘degree of cellulite’ after Day 85 and Day 168.
AEVA‐HE measurement(s)
AEVA‐HE (EO Tech SA, Marcoussis France): Using phase‐shifted in vivo measurements of human skin, the three‐dimensional surface structure of the investigated skin site was captured (Fig. 3a) – two measurements of each thigh (biceps femoris and iliotibial region of the thighs separately) per assessment time. The measuring principle is based on digital fringe projection and stereometry. The fringes that were projected under the so‐called triangulation angle onto the surface of the measured target with a sinus‐like intensity of brightness were detected with two cameras. The three‐dimensional structure (cellulite‐related dimple) was assessed from the position of the fringes. For each area, a region of interest of 8 × 7 cm was selected (Fig. 3b) and a plane was computationally projected into the assessed three‐dimensional structure (Fig. 3d). Domains extruding from the plane yielded positive and negative volume, respectively. Their absolute sum was calculated accounting for the cellulite‐related dimple volume [mm3].
Figure 3.
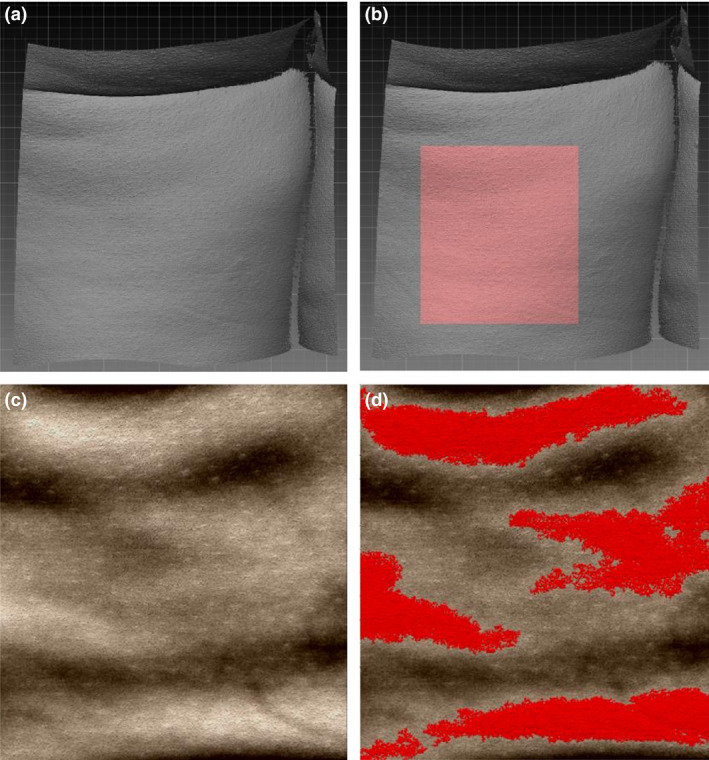
Captured three‐dimensional surface of the biceps femoris region (a) and a suitable region of interest (ROI) for analysis (b); ROI (c) and volume extruding from a computationally projected plane within the ROI (d).
Cellulite macrophotography and imaging
_S_tandardized Macrophotographs were captured with a Cellulite Photography Stand comprising an individually designed platform, with a fixed computer‐controlled Canon 21 Megapixel camera (Canon EOS 5D MkIII; Canon Deutschland GmbH, Krefeld, Germany) camera, and neon ring light for illumination. The ring light positioned at knee height, produced varying shadows on the subjects' skin according to their degree of cellulite (Fig. 4). The camera position was recorded on two defined axes with the orientation between the camera and the ring light remained fixed at any time. Thus, quality cellulite photography of high definition and same illumination at different assessment times could be enabled. Camera settings were defined and saved for each subject for each assessment and each thigh area. Photographic images (2 images) of each thigh (biceps femoris and iliotibial regions separately) per assessment time were taken. Images were stored for photograph documentation and evaluation.
Figure 4.
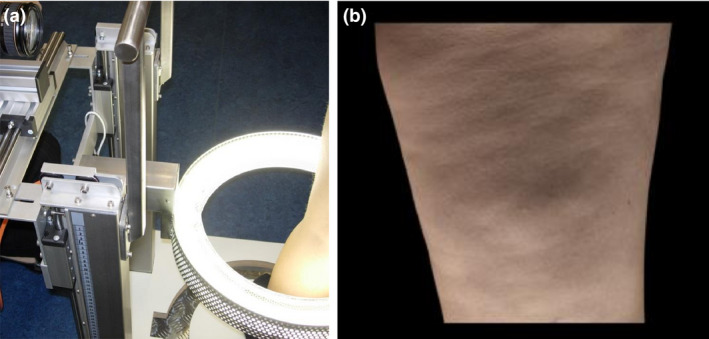
Cellulite Photography Stand (a) and exemplary image of the biceps femoris region (b).
Image evaluation
At study completion, six trained graders (male or female, 18–70 years of age) evaluated all macrophotographs assessing the ‘degree of cellulite’. Evaluation was performed on colour‐calibrated rating monitors (NEC SpectraView 30903090WQX, 30 inch) by comparing and grading photographs taken at Baseline and after 85 days of product application for each subject and each area. For the regression analysis, photographs taken on Day 85 were compared to photographs taken on Day 168. Assessments were performed blind against treatment assignment and time of photograph capture. Graders ranked images against the scale: 1 = less visible cellulite and 2 = more visible cellulite.
Subject questionnaires
Questionnaires for ‘sensitivity and sensation of the test area’ were completed before and after the first usage of the test product on Day 1. Questionnaires for product acceptance were completed on Days 85 and 168. The usage of the test product throughout the course of the study was documented in a diary provided.
Data managements and statistics
Valid subjects were defined as enrolled subjects who had finished the study without any major deviations from the protocol and who had not withdrawn their consent. No replacement of missing data was performed, de‐randomization was made by merging data to the randomization list using a unique identifier variable, and no unblinding was necessary. The assessment time before product application was defined as Baseline alongside the Day 85 and Day 168 time points.
Volume (AEVA)
Per area (biceps femoris and iliotibial region), treatment and assessment time, the cellulite‐related dimple volume was used as raw data for further analysis. The raw data of all valid subjects and the differences to Baseline values were listed by area, treatment and assessment time.
Image evaluation (trained graders)
The raw data of all valid subjects were listed per grader by area, treatment and assessment time. Mean scores over all raters were given per subject by area, treatment and assessment time and used for the statistical analysis.
Questionnaires
Results of the questionnaire were listed for valid subjects.
Statistical data analysis
A significance level of 0.05 (alpha) was chosen for statistical analysis. Due to the explorative character of the study, no adjustment for multiplicity was done.
Volume (AEVA)
All statistical analyses were performed for both assessed areas (biceps femoris and iliotibial region). Efficacy analysis on Day 85 of product application was performed by pairwise comparisons of differences to Baseline values of Day 85 for untreated and treated areas (A vs. B) with a paired _t_‐test. The biceps femoris region for 36 and the iliotibial region for 37 subjects were analysed. Furthermore, both, the regression (D) and the continuous application (F) subgroups were analysed by pairwise comparison of the difference to Baseline values of Day 85 vs. Day 168 using a paired _t_‐test. In the regression subgroup, the biceps femoris and the iliotibial region of 18 subjects were analysed for either region. In the continued application subgroup, the biceps femoris region of 17 and the iliotibial region of 16 subjects were analysed.
Image evaluation (trained graders)
Efficacy analysis on Day 85 was performed by pairwise (A vs. B). The comparisons were performed on mean scores of Day 85 vs. Baseline over all graders per area (biceps femoris and iliotibial region) with a Wilcoxon signed‐rank test. The score qualifies the comparison of Day 85 to Baseline.
The regression analyses were done on mean scores of subgroups D and F over all graders per area (biceps femoris and iliotibial region) and compared to the Benchmark Score1.5 (equivalent to no visible change) using a Wilcoxon signed‐rank test. The score qualifies the comparison between Day 168 and Baseline, as well as between Day 168 and Day 85.
Questionnaire (sensitivity and sensation of the test area, pre/post)
Pairwise comparisons of assessment times were done on mean scores for the treated thigh with a Wilcoxon signed‐rank test.
The computation of the statistical data throughout was carried out with commercially available statistics software (SAS for Windows, SAS Institute Cary, NC, USA).
Results
Only one subject withdrew from the study, and data were excluded from the overall analysis. Of 40 volunteers enrolled, 37 completed the 6‐month period of investigation without any major deviations (mean age: 47.0 ± 5.8 years, mean BMI: 24.8 ± 3.6). No adverse reactions or events were reported.
AEVA‐HE measurements
The changes in cellulite‐related dimple volume changes measured with AEVA on both test areas, biceps femoris and iliotibial region, respectively, are presented in Fig. 5. Mean values of differences to Baseline and 95% confidence intervals after 12‐week treatment (Day 85) are shown.
Figure 5.
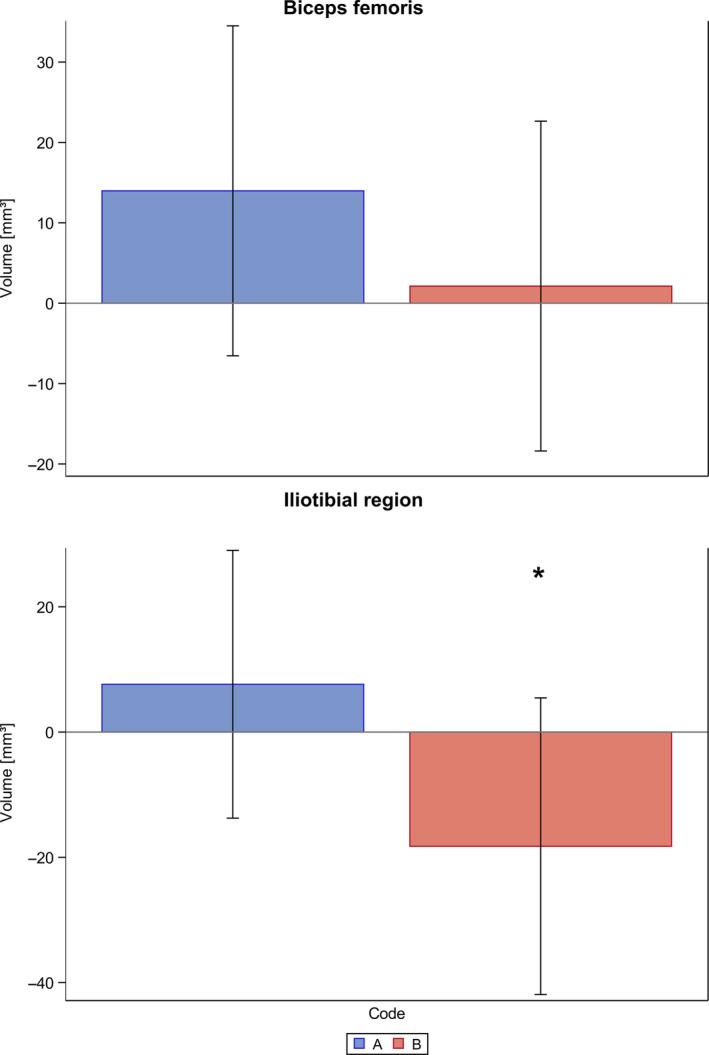
AEVA measurement results of the total population on Day 85 (12 weeks of massage device application); Bar chart with mean values and 95% confidence intervals of differences to baseline for change of cellulite‐related dimple volume [mm3]; biceps femoris region (n = 36); iliotibial region (n = 37); _P_‐value of difference between untreated (A) and treated (B) area of the iliotibial region: P = 0.049 (*).
In the biceps femoris region, no significant differences were measured after 12‐week treatment with the massage device (B), in comparison with the untreated test area (A).
However, in the iliotibial region of the thighs the volume of cellulite significantly (P = 0.049) decreased after 12‐week treatment with the massage device (B) in comparison with the untreated test area (A).
On Day 85, following 12 weeks usage of the massage device by all 37 subjects, 18 subjects (regression subgroup, D) discontinued treatment for the following 12 weeks, and 17 subjects (continuous application subgroup, F) continued the use of the massage device until Day 168 (24 weeks).
Figure 6 presents the changes in cellulite‐related dimple volume on both test areas, as measured with AEVA. Mean values of the differences to Baseline and 95% confidence intervals of the regression subgroup (D) and the continuous application subgroup (F) are presented for Day 85 and after 12 further weeks (Day 168).
Figure 6.
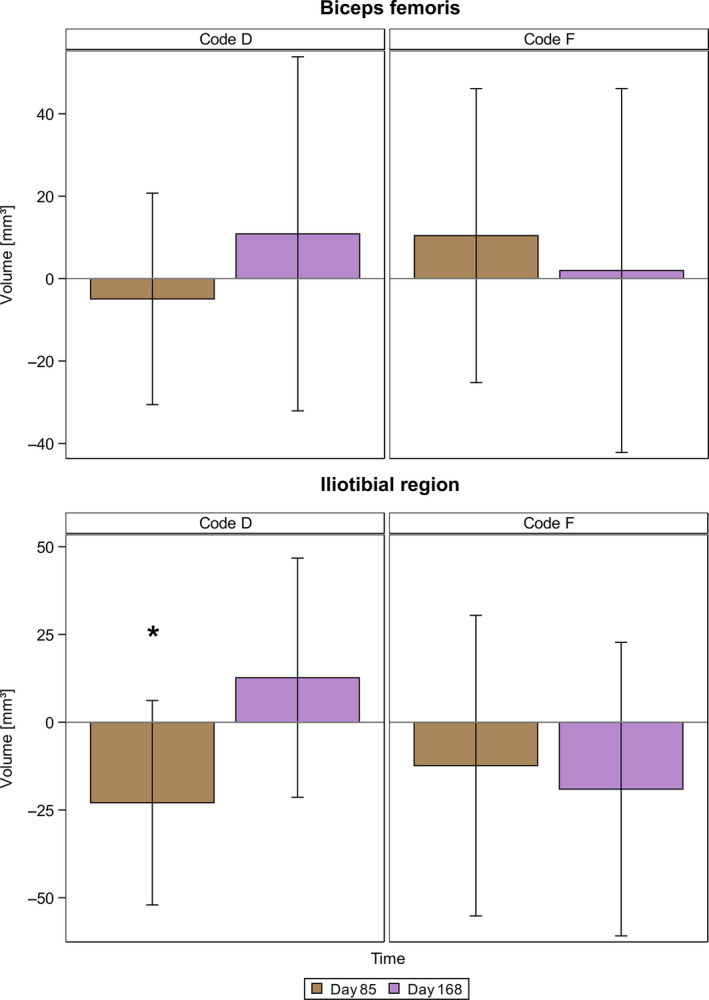
AEVA measurement results of the regression and the continuous application subgroups (D and F, respectively) on Day 168; condense Bar chart with mean values and 95% confidence intervals of differences to baseline for change of cellulite‐related dimple volume [mm3]; regression subgroup (D): biceps femoris and iliotibial region (n = 18 each); continuous application subgroup (F): biceps femoris and iliotibial region (n = 17 and n = 16, respectively).
On the biceps femoris region of the thighs, no significant differences regarding the volume were found on Day 168, neither after discontinued treatment (D) nor with continuous treatment with the massage device (F).
However, in the iliotibial region the discontinued treatment resulted in a statistically significant (P = 0.037) increase of cellulite‐related dimple volume on Day 168 in comparison with Day 85 Meanwhile, continued treatment with the massage device until Day 168 yielded a small, albeit statistically non‐significant decrease of cellulite‐related dimple volume on Day 168 in comparison with Day 85.
Macrophotography image evaluation
Table II shows the median scores of the degree of cellulite by ranking of macrophotographs, as evaluated by trained graders, as well as the results of comparison the medians by a Wilcoxon signed‐rank test. On both the biceps femoris and the iliotibial region of the thighs, significantly less cellulite was evaluated after 12‐week treatment with the massage device (B), in comparison with the untreated test area (A).
Table II.
Macro‐photographic analysis of visual cellulite in the biceps femoris and iliotibial region on Day 85 (12 weeks of treatment); comparison of untreated (A) to treated area (B); medians and _P_‐values of comparison of treatments of all graders by Wilcoxon signed‐ranks test (n = 37); Score: 1 = less visible cellulite compared to Baseline; 2 = more visible cellulite compared to Baseline
| Test area | Time | Treatment | Median | _P_‐values |
|---|---|---|---|---|
| Biceps femoris | Day 85 vs. baseline | A | 1.67 | 0.022* |
| B | 1.33 | |||
| Iliotibial region | Day 85 vs. baseline | A | 1.67 | 0.002* |
| B | 1.50 |
The evaluation of the regression and continuous application subgroups showed no statistically significant difference to the Bechmark score of 1.5 (equivalent to no change observed between Day 168 and Day 85). However, the tendency in the values indicates a further visual improvement of cellulite on the continually treated fields (F) on Day 168 in comparison with Day 85, as opposed to the discontinued treatment (D), which remain unchanged (Table III).
Table III.
Macro‐photographic analysis of visual cellulite at 24 weeks post treatment compared tountreated site ‐ outer and backside of thigh comparison. Mean values, standard deviations, medians and comparison of mean scores over all graders with Benchmark 1.5 by Wilcoxon signed‐ranks test (Code D: n = 18, Code F: n = 17). ns, not significant; *, significant; P ≤ 0.05 Score: 1 = less visible cellulite compared to Day 168; 2 = more visible cellulite compared to Day 168
| Test area | Time | Treatment | Median | _P_‐values (vs. 1.5 benchmark) |
|---|---|---|---|---|
| Biceps femoris | Day 168 vs. Day 85 | D | 1.50 | 0.559 ns |
| F | 1.17 | 0.503 ns | ||
| Iliotibial region | Day 168 vs. Day 85 | D | 1.67 | 0.295 ns |
| F | 1.17 | 0.317 ns |
Questionnaire
Sensitivity and sensation of the test area
On Day 1, the subjects filled in a self‐assessment questionnaire regarding sensitivity and sensation of the test area directly before and after the intervention (i.e. first use of the massage device). Table IV presents the mean scores with standard deviations and the medians of the questionnaire regarding pre‐/post‐sensitivity and sensation of the test area, as well as the results for the comparison of times on raw data for the treated thigh by a Wilcoxon signed‐rank test.
Table IV.
Results of questionnaire on Day 1 ‐ mean scores, standard deviations, median scores and comparison of times on raw data by Wilcoxon signed‐ranks test (n = 37). ns, not significant; *, significant, P ≤ 0.05. Score: 0 = does not apply; 5 = neither nor; 10 = applies
| Question | Time | Mean scores (standard deviations) | Median scores | _P_‐values |
|---|---|---|---|---|
| 1. The part of the body to be treated/the treated part of the body feels RELAXED | Before intervention | 7.4 (2.6) | 8.0 | 0.613ns |
| After intervention | 7.5 (2.8) | 8.0 | ||
| 2. The part of the body to be treated/the treated part of the body feels STABLE | Before intervention | 6.2 (3.1) | 6.0 | 0.005* |
| After intervention | 7.7 (2.1) | 9.0 | ||
| 3. The part of the body to be treated/the treated part of the body feels STRONG | Before intervention | 5.8 (2.8) | 6.0 | <0.001* |
| After intervention | 7.3 (2.4) | 8.0 | ||
| 4. The part of the body to be treated/the treated part of the body feels LIGHT | Before intervention | 5.5 (2.6) | 5.0 | 0.043* |
| After intervention | 6.8 (2.9) | 7.0 | ||
| 5. The part of the body to be treated/the treated part of the body feels balanced in comparison with the opposite part of the body on opposite side | Before intervention | 7.4 (3.0) | 9.0 | 0.289ns |
| After intervention | 6.4 (3.5) | 7.0 |
Product acceptance
On Days 85 (12 weeks) and 168 (24 weeks), subjects filled in a further questionnaire relating to product acceptance. Disagreements and agreements to the product acceptance questions at Day 85 are presented in Fig. 7. After 12‐week application of the massage device, between 60% and 87% of subjects agreed with all statements relating to beneficial product traits of the massage device and the sensory and appearance aspects of the skin There was a 70% overall high acceptance of the test product.
Figure 7.
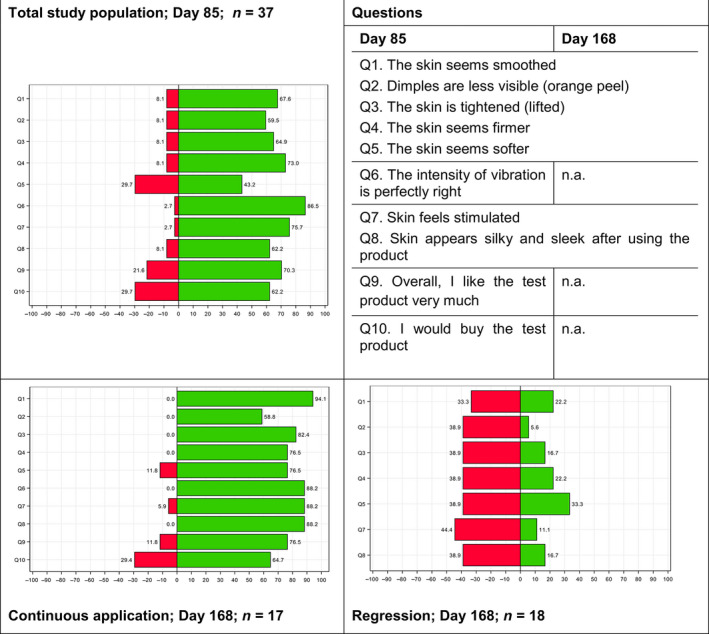
Product acceptance results based on self‐assessment questionnaires of the total population on Day 85 and the regression and continuous subgroups on Day 168; Butterfly Plots: Percentages for (dis‐)Agreement of Questionnaire [%]; dark grey = disagreement, light grey = agreement; total population on Day 85: n = 37; regression and continuous application subgroups: n = 17 and n = 18, respectively; _P_‐value of difference to Baseline of the treated area of the iliotibial region on Day 85 and the same area after treatment discontinuation on Day 168: P = 0.037 (significant).
Following 24 weeks (Day 168) application of the massage device, the vast majority of all subjects of the continuous application subgroup agreed with all statements concerning positive product traits of the massage device, and the sensory and appearance aspects of the skin as compared to 12 weeks (Day 85). There was a 76% overall high acceptance of the test product. Meanwhile, the regression subgroup noted decreased positive effects due to treatment discontinuation.
Discussion
Cellulite is difficult to manage for the consumer and difficult to prove the effectiveness of products addressing the need to reduce the visual appearance of its dimpled appearance. Furthermore, cellulite manifesting itself subcutaneously makes it nigh on impossible for topical cosmetic treatments to effectively address, since most topical cosmetic actives cannot reach the subcutis in a sufficient dose and other actives might be forbidden by law, as they are drugs and fall out of the scope of ‘cosmetic’ definition. Lubricant oil was used in this study to facilitate and improves the massage. Such oils can be defined as indirect cosmetic anti‐cellulite actives as they are essential for the functioning of massage tools. Given reports of benefits of WBV on the appearance of cellulite [19, 20], hand‐held electrical vibrating massage devices have come to the fore in the management of cellulite.
Utilizing both objective (AEVA‐HE phase‐shift 3‐D fringe volume, and macrophotography) and subjective (questionnaire) methods this study investigated the performance of a consumer hand‐held localized vibrational device in reducing visually assessed cellulite volume over 24 weeks (6 months). The study was a randomized intra‐individual single‐blind regression investigation on healthy female volunteers.
Following 12‐week treatment with the massage device, the volume of cellulite dimples determined by AEVA on the iliotibial region of the thighs significantly decreased in comparison with non‐massaged skin. On the biceps femoris region of the thighs, this effect was less pronounced and not statistically significant. This finding, however, might be explained by more ease of use of the massage device on the side of the thigh as compared to the biceps femoris region, especially in terms of an easier reach and better visibility, given that it would be more difficult to observe the biceps femoris region of the thighs. This suggestion may also contribute to a more effective massaging effect on the side than on the biceps femoris region. Another suggestion could be that the structural aspects of cellulite differ in morphology on the iliotibial region of the thighs and on the biceps femoris region of the thighs [1, 25, 26, 27].
Following a further 12 weeks without massage, the volume of cellulite measured on the iliotibial region of the thighs significantly increased, in comparison with 12‐week (24 weeks in total) treatment with the massage device. That is, the condition regressed to its visible cellulite state when massaging stopped. Interestingly, following the 24‐week treatment with the massage device, the volume of the cellulite decreased even further compared to after only 12 weeks. These findings were supported by visual grading of macrophotographs. After 12‐week treatment with the massage device, the degree of cellulite evaluated on macrophotographs taken on the biceps femoris region, as well as the iliotibial region of the thighs, was significantly decreased in comparison with untreated skin. Owing the reduced size of the subgroups (D and F: n = 17 each) as compared to the initial total study population (n = 37), the results of the subgroup analysis of the visual grading lack statistical significance and only indicate a trend. This trend, however, does confirm the results found for AEVA volume measurements – the regression subgroup showed an increase in cellulite, whereas the continuous application subgroup showed a further improvement of their cellulite at 24 weeks as compared to 12 weeks.
According to subject questionnaires (Table IV), their skin felt more ‘stable, stronger and lighter’ directly after the first use of the massage device than before study participation, indicating a subjective improvement in skin firmness. Most subjects in the continual application subgroup evaluated positive skin sensory properties, whereas most subjects in the regression subgroup evaluated their skin sensory properties to be worse – thus correlating with AEVA and visual grading results.
As with any skin treatment investigations involving a regression phase evaluation, most treatments will result in a ‘regression’ of measured parameters once that treatment has been stopped. However, it is the rate at which that regression occurs which is of importance. This has been the case in this investigation where a regression was noticeable upon massage termination. A limitation of this study was the number of participating subjects. Observed changes in either parameter – change in cellulite‐related dimple volume as well as macrophotography grading – proved to be subtle, possibly masking the treatment effect on the biceps femoris region. The division of the total study population into smaller subgroups exacerbated the problem leading to a loss of statistical significance in the macrophotography grading in an otherwise plausible trend.
Notwithstanding this study's limitations, investigations have been reported showing that whole‐body vibration (WBV) leads to an improvement in visible cellulite [20]. In other reports, vibrational treatment evidence exists for enhancing the breakdown of adipose tissue in studies investigating obesity and diabetes [22] and significant correlations exist between changes in percent body fat and blood flow. Furthermore, WBV is an effective means of increasing leg blood flow and reducing adiposity in type 2 diabetics [23], and such treatment was effective in reducing and preventing adiposity with increasing age associated with a stimulation of hepatic lipid metabolism [24].
The aim of this study was to evaluate a visual improvement in the appearance of cellulite as judged both objectively and subjectively – thus ultimately focusing on the ‘consumer’. Scientific arguments for other limitations of this study may not only rest with evaluating surface observations (important consumer traits) in terms of correlating with other non‐invasive evaluations, but also with obvious questions that although the massage device is reducing surface dimples, the mechanism remains unknown. Furthermore, consideration needs to be given to questions surrounding actual adiposity reduction [20, 23], and even improvement in connective tissue hydration/rehydration in the visually observed reduction of fascia bulging [8, 28].
Oxidative stress and deficiencies in lymphatic drainage and microvascular circulation also promote cellulite, and reported studies have indicated that cellulite depression is associated with the presence of the underlying thick fibrous septae, which are perpendicular to the skin surface and mostly ramified [29, 30]. In these studies, a tool‐assisted tissue manipulation in the form of a self‐help treatment revealed significant changes (P < 0.001) in stiffness, elasticity, local temperature and hydration. The observed decrease in stiffness and increase in elasticity indicated a loosening of the adhesions of the underlying ramified, thick, fibrous, myofascial septa. Increase in local temperature, as observed by the subjects, improved the microvascular circulation which possibly reduces oxidative stress [30]. A higher hydrated tissue state, better lymphatic drainage and microvascular circulation and a reduction of liquid accumulation are therefore assumed. These bio‐physiological effects may reduce the oedema and the following reduction of pressure in the tissue, thus possibly improving natural lipolysis.
Since our study, subjects did not report skin ‘sensitivity’ which is an occurrence in skin oedema, we could, however, at this juncture surmise that oedema may not be an important issue, even though any unperceived subcutaneous ‘sensitivity’ may not be apparent either. As a work in progress, it would be of interest to investigate the actual mechanisms by which vibrational devices such as these could correlate with WBV, thus providing a real consumer benefit.
Conclusions
The aim of this investigation was to demonstrate a visual improvement in the appearance of cellulite on the thighs of females through the use of a hand‐held vibrational massage device. This was achieved and effects persisted for 24 weeks with continual use. Limitations of the study, particularly the design of the regression phase, warrant further investigation as a step forward to help identify the mechanisms and thus benefits of vibrational massage in the management of cellulite.
Conflict of interest
All authors declare that they have no conflict of interest.
Acknowledgements
The authors thank Dr. Theresa Callaghan, Callaghan Consulting International, Hamburg, Germany for the preparation of this manuscript and helpful discussions. The study was completely financed by the Sponsor (Beurer GmbH).
REFERENCES
- 1.Pierard, G. , Nizet, J. and Pierard‐Franchimont, C. Cellulite: from standing fat herniation to hypodermal stretch marks. Am. J. Dermatopathol. 22, 34–37 (2000). [DOI] [PubMed] [Google Scholar]
- 2.Friedmann, D. , Vick, G. and Mishra, V. Cellulite: a review with a focus on subcision. Clin. Cosmet. Investig. Dermatol. 10, 17–23 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hexsel, D. and Soirefmann, M. Cosmeceuticals for cellulite. Semin. Cutan. Med. Surg. 30, 167–170 (2011). [DOI] [PubMed] [Google Scholar]
- 4.Hexsel, D. , Abreu, M. , Rodrigues, T. , Soirefmann, M. , do Prado, D. and Gamboa, M. Side‐by‐side comparison of areas with and without cellulite depressions using magnetic resonance imaging. Dermatol. Surg. 35, 1471–1477 (2009). [DOI] [PubMed] [Google Scholar]
- 5.Rawlings, A. Cellulite and its treatment. Int. J. Cosmet. Sci. 28, 175–190 (2006). [DOI] [PubMed] [Google Scholar]
- 6.Querleux, B. , Cornillon, C. , Jolivet, O. and Bittoun, J. Anatomy and physiology of subcutaneous adi‐ pose tissue by in vivo magnetic resonance imaging and spectroscopy: relationships with sex and pres‐ ence of cellulite. Skin Res. Technol. 8, 118–124 (2002). [DOI] [PubMed] [Google Scholar]
- 7.Mirrashed, F. , Sharp, J. , Krause, V. , Morgan, J. and Tomanek, B. Pilot study of dermal and subcutaneous fat structures by MRI in individuals who differ in gender, BMI, and cellulite grading. Skin Res. Technol. 10, 161–168 (2004). [DOI] [PubMed] [Google Scholar]
- 8.Callaghan, T. Evaluating Cellulite – Reality Redirecting the Dream to Dispel the Myth. Proceedings International Federation of the Society of Cosmetic Chemists (IFSCC), Orlando, FL: (2004). [Google Scholar]
- 9.Callaghan, T. and Wilhelm, K.‐P. An examination of non‐invasive techniques in the analysis and review of cellulite. J. Cosmet. Sci. 56, 379–393 (2005). [PubMed] [Google Scholar]
- 10.Christman, M. , Belkin, D. , Geronemus, R. and Brauer, J. An anatomical approach to evaluating and treating cellulite. J. Drugs Dermatol. 16, 58–61 (2017). [PubMed] [Google Scholar]
- 11.Mlosek, R. , Dębowska, R. , Lewandowski, M. , Malinowska, S. , Nowicki, A. and Eris, I. Imaging of the skin and subcutaneous tissue using classical and high‐frequency ultrasonographies in anti‐cellulite therapy. Skin Res. Technol. 17, 461–468 (2011). [DOI] [PubMed] [Google Scholar]
- 12.Wilczyński, S. , Koprowski, R. , Deda, A. , Janiczek, M. , Kuleczka, N. and Błońska‐Fajfrowska, B. Thermographic mapping of the skin surface in biometric evaluation of cellulite treatment effectiveness. Skin Res. Technol. 23, 61–69 (2017). [DOI] [PubMed] [Google Scholar]
- 13.Yoo, M. , Seo, Y. , Ryu, J. , Back, J. and Koh, J. A validation study to find highly correlated parameters with visual assessment for clinical evaluation of cosmetic anti‐ cellulite products. Skin Res. Technol. 20, 200–207 (2014). [DOI] [PubMed] [Google Scholar]
- 14.Bielfeldt, S. , Buttgereit, P. , Brandt, M. , Springmann, G. and Wilhelm, K.P. Non‐invasive evaluation techniques to quantify the efficacy of cosmetic anti‐cellulite products. Skin Res. Technol. 14, 336–346 (2008). [DOI] [PubMed] [Google Scholar]
- 15.Ferraro, G. , De Francesco, F. , Cataldo, C. , Rossano, F. , Nicoletti, G. and D'Andrea, F. Synergistic effects of cryolipolysis and shock waves for noninvasive body contouring. Aesthetic Plast. Surg. 36, 666–679 (2012). [DOI] [PubMed] [Google Scholar]
- 16.Wanitphakdeedecha, R. , Sathaworawong, A. , Manuskiatti, W. and Sadick, N. Efficacy of multipolar radio‐frequency with pulsed magnetic field therapy for the treatment of abdominal cellulite. J. Cosmet. Laser Ther. 19, 205–209 (2017). [DOI] [PubMed] [Google Scholar]
- 17.Avci, P. , Nyame, T. , Gupta, G. , Sadasivam, M. and Hamblin, M. Low‐level laser therapy for fat layer reduction: a comprehensive review. Lasers Surg. Med. 45, 349–357 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savoia, A. , Landi, S. , Vannini, F. and Baldi, A. Low‐level laser therapy and vibration therapy for the treatment of localized adiposity and fibrous cellulite. Dermatol. Ther. (Heidelb) 3, 41–52 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alizadeh, Z. , Halabchi, F. , Mazaheri, R. , Abolhasani, M. and Tabesh, M. Review of the mechanisms and effects of noninvasive body contouring devices on cellulite and subcutaneous fat. Int J. Endocrinol. Metab. 14, e36727 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cristovam, D. , Botelho, S. , Andrade, M. , Marques, J. and Sousa, L. Whole‐body vibration in the reduction of the cellulite. J. Cosmet. Laser Ther. 9, 1–8 (2018). [DOI] [PubMed] [Google Scholar]
- 21.Knobloch, K. , Joest, B. , Krämer, R. and Vogt, P. Cellulite and focused extracorporeal shockwave therapy for non‐ invasive body contouring: a randomized trial. Dermatol. Ther. (Heidelb) 3, 143–155 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson, C. , Barreto, R. , Sbruzzi, G. and Plentz, R. The effects of whole body vibration in patients with type 2 diabetes: a systematic review and meta‐analysis of randomized controlled trials. Braz. J. Phys. Ther. 20, 4–14 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sañudo, B. , Alfonso‐Rosa, R. , Del Pozo‐Cruz, B. , del Pozo‐Cruz, J. , Galiano, D. and Figueroa, A. Whole body vibration training improves leg blood flow and adiposity in patients with type 2 diabetes mellitus. Eur J. Appl. Physiol. 113, 2245–2252 (2013). [DOI] [PubMed] [Google Scholar]
- 24.Reijne, A. , Ciapaite, J. , van Dijk, T._et al_Whole‐body vibration partially reverses aging‐induced increases in visceral adiposity and hepatic lipid storage in mice. PLoS One 11, e0149419 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.González‐Suárez, A. , Gutierrez‐Herrera, E. , Berjano, E. , Jimenez Lozano, J. and Franco, W. Thermal and elastic response of subcutaneous tissue with different fibrous septa architectures to RF heating: numerical study. Lasers Surg. Med. 47, 183–195 (2015). [DOI] [PubMed] [Google Scholar]
- 26.Leszko, M. Cellulite in menopause. Prz. Menopauzalny 13, 298–304 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quatresooz, P. , Xhauflaire‐Uhoda, E. , Piérard‐Franchimont, C. and Piérard, G. Cellulite histopathology and related mechanobiology. Int. J. Cosmet. Sci. 28, 207–210 (2006). [DOI] [PubMed] [Google Scholar]
- 28.Gniadecka, M. , Nielsen, O. , Wessel, S._et al_Water and protein structure in photoaged and chronically aged skin. J. Invest. Dermatol. 111, 1129–1133 (1998). [DOI] [PubMed] [Google Scholar]
- 29.Gordon, C. , Lindner, S. , Birbaumer, N. , Montoya, P. and Andrasik, F. Self‐help treatment with a myofascial manipulation tool. Fascia Research IV, Washington DC 9, 197 (2015). [Google Scholar]
- 30.Gordon, C. , Lindner, S. , Birbaumer, N. , Montoya, P and Andrasik, F. Correlation between hydration and fascia stiffness during a self‐help treatment with a myofascial manipulation tool. A bioimpedance controlled, clinical trial. Fascia Research IV, Washington DC. 5, 93 (2015). J Bodyw Mov Ther 19, 668 (2015). [Google Scholar]