Exploring Predictors of Sleep State Misperception in Women with Posttraumatic Stress Disorder (original) (raw)
. Author manuscript; available in PMC: 2024 Jan 1.
Abstract
Insomnia is a common symptom of posttraumatic stress disorder (PTSD) that is resistant to first-line cognitive behavioral interventions. However, research suggests that, among individuals with PTSD, self-reported sleep impairment is typically more severe than what is objectively observed, a phenomenon termed sleep state misperception. Relatively little research has examined which individuals with PTSD are most likely to exhibit sleep state misperception. This study explored clinical predictors of sleep state misperception in a sample of 43 women with PTSD and clinically significant sleep impairment. During a baseline assessment, participants’ PTSD symptoms were assessed using a clinical interview and their sleep was assessed using the Pittsburgh Sleep Quality Index (PSQI). Objective sleep, self-reported sleep, and PTSD symptoms were then assessed over a 1-week period using actigraphy and daily diaries. Consistent with previous research, women in the study exhibited total sleep time (TST), sleep efficiency (SE), and sleep onset latency (SOL) sleep state misperception. For TST and SE, but not SOL, discrepancies between actigraphy and the PSQI were associated with each clinician-rated PTSD symptom cluster, whereas discrepancies between actigraphy and daily diary were only associated with clinician-rated re-experiencing symptoms. The only self-reported PTSD symptom that was uniquely associated with sleep state misperception was nightmares. This association was no longer significant after controlling for sleep-related anxiety. Results suggest that women with more severe re-experiencing symptoms of PTSD, particularly nightmares, may be more likely to exhibit TST and SE sleep state misperception, perhaps due to associated sleep-related anxiety.
Keywords: Paradoxical Insomnia, Subjective Insomnia, Trauma, Fear of Sleep
Approximately 80-90% of individuals with posttraumatic stress disorder (PTSD) endorse clinically significant insomnia, including difficulty falling and/or staying asleep (Koffel et al., 2016). Notably, insomnia is resistant to first-line treatments for PTSD, including cognitive processing therapy and prolonged exposure (Belleville et al., 2011; Larsen et al., 2019). As many as 80% of people continue to endorse clinically significant insomnia following treatment (Pruiksma et al., 2016). A better understanding of PTSD-related insomnia may, thus, improve PTSD interventions.
Sleep disturbance is often assessed using self-report measures (e.g., daily sleep diaries, global self-reports), but can also be assessed objectively using polysomnography (PSG) or actigraphy. Importantly, self-reported and objectively assessed sleep disturbance appear to be discrete constructs with only low to moderate degrees of concordance (Slightam et al., 2018; Werner et al., 2016). The concordance between daily sleep diaries and concurrent objective assessments appears to be stronger than the concordance between global self-reports and objective assessments, perhaps due to greater biases when recalling sleep over an extended period (Lipinska & Thomas, 2017; Slightam et al., 2018).
Most research on sleep in PTSD suggests that self-reported sleep disturbance is more severe than what is objectively observed. Meta-analytic findings indicate large differences in self-reported sleep disturbance between individuals with PTSD and healthy controls (Cox & Olatunji, 2020). In contrast, the same meta-analysis found only a medium effect for worse sleep continuity, a small effect for decreased sleep depth, and non-significant effects for shorter total sleep time (TST) and rapid eye movement (REM) pressure in PTSD (Cox & Olatunji, 2020). Another recent meta-analysis on sleep measured with actigraphy found that individuals with and without PTSD did not differ in their TST, sleep onset latency (SOL), waking after sleep onset (WASO), or sleep efficiency (SE; Lewis et al., 2020). The tendency to report greater sleep disturbance than what is objectively observed has been termed sleep state misperception; it is also referred to as subjective insomnia or, clinically, as paradoxical insomnia (American Academy of Sleep Medicine, 2005). Of the few studies that have examined sleep state misperception in PTSD, almost all have documented the presence of this phenomenon and/or more pronounced sleep state misperception in participants with PTSD vs. trauma- and non-trauma exposed control participants (Ghadami et al., 2015; Hurwitz et al., 1998; Klein et al., 2003; Slightam et al., 2018, Kobayashi et al., 2012).
Notably, sleep state misperception is not unique to PTSD. It has been observed in individuals with primary insomnia and linked to other psychiatric conditions, including major depressive disorder and schizophrenia (Rezaie et al., 2018). Within the primary insomnia literature, research has found evidence for distinct pathophysiology in individuals with, vs. without, sleep state misperception. As reviewed by Edinger and Krystal (2003), individuals with sleep state misperception demonstrate better objectively assessed sleep, but greater levels of motor activity during sleep and poorer daytime cognitive functioning than individuals with objective insomnia. The latter finding regarding cognitive functioning highlights the importance of elucidating the subgroup(s) of individuals who are most likely to experience sleep state misperception and its sequelae. A better understanding of why sleep state misperception occurs is also critical to avoid inadvertently trivializing patient reports of insomnia and associated distress (Harvey & Tang, 2012).
Within the context of PTSD, very little research has examined who is most likely to experience sleep state misperception and why. We can begin, however, by considering how specific symptoms of PTSD are linked to insomnia symptoms, more generally. Recently, Werner, Riemann, and Ehring (2021) proposed a conceptual model linking specific PTSD symptoms to chronic trauma-related insomnia. According to this model, hyperarousal symptoms may contribute to insomnia by increasing maladaptive insomnia-related processes. Separately, insomnia may be maintained by fear of sleep due to nightmares or maladaptive beliefs about safety and the loss of control that occurs during sleep. Avoidance symptoms may contribute to both insomnia- and fear of sleep-related processes. Based on this model, we may expect specific PTSD symptoms, including hyperarousal symptoms, nightmares, maladaptive beliefs about safety, and/or avoidance to also be associated with greater sleep state misperception.
This study explored the associations between PTSD symptoms and sleep state misperception among women with PTSD and clinically elevated insomnia symptoms. Examining these associations in women meaningfully extends previous research, which has been conducted using predominantly male samples (Ghadami et al., 2015; Hurwitz et al., 1998; Klein et al., 2003; Slightam et al., 2018), despite the fact that women are at increased risk of developing PTSD and insomnia following trauma exposure (Kobayashi & & Delahanty, 2013).
The study had three aims. First, we sought to replicate previous research documenting sleep state misperception in PTSD. We examined discrepancies between self-reported sleep on the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989) and daily sleep diaries and objective sleep assessed with actigraphy. We hypothesized participants would report poorer sleep than what was objectively observed, and that the PSQI-actigraphy discrepancy would be larger than the daily diary-actigraphy discrepancy. The second aim was to explore PTSD symptoms as predictors of sleep state misperception. It was hypothesized that re-experiencing and hyperarousal symptoms would be most strongly associated with sleep state misperception. Finally, we examined the association between sleep-related anxiety and sleep state misperception, predicting that participants experiencing greater sleep-related anxiety would exhibit greater sleep state misperception.
Method
Participants
Participants were women with PTSD secondary to interpersonal violence enrolled in a larger (_N_=92) randomized controlled trial (Arditte Hall et al., 2020; Galovski et al., 2016). Forty-five participants from the trial consented to participate in an auxiliary actigraphy study. Women opting into the study did not differ from women who declined participation on demographic or clinical variables of interest (_p_s>.05). Analyses presented here reflect cross-sectional data collected at baseline. Due to technical difficulties, two participants were missing actigraphy data. Thus, the full sample was _n_=43.
Participants were 18 years or older, currently diagnosed with PTSD, and endorsed sleep impairment (i.e., score ≥3 for frequency and intensity on symptom D1 - Trouble Initiating or Falling Asleep on the Clinician-Administered PTSD Scale for DSM-IV; Blake et al., 1995). Exclusion criteria included current psychosis, substance abuse/dependence, or suicidal ideation, and living in an ongoing traumatic situation. See Table 1 for sample characteristics.
Table 1.
Descriptive statistics for demographic and clinical variables.
| Variable | M (SD) | n (%) |
|---|---|---|
| Age | 36.51 (11.68) | |
| Race | ||
| White | 23 (53.5%) | |
| Black/African American | 20 (46.5%) | |
| Ethnicity | ||
| Hispanic or Latina | 1 (2.3%) | |
| Not Hispanic or Latina | 41 (95.3%) | |
| Years of Education | 13.91 (2.70) | |
| Income | ||
| Under $20,000 | 28 (65.1%) | |
| $20,000 or more | 15 (34.9%) | |
| Relationship Status | ||
| Single | 24 (55.8%) | |
| Married/Cohabitating | 8 (18.6%) | |
| Separated/Divorced/Widowed | 11 (25.6%) | |
| CAPS Total Score | 78.70 (16.45) | |
| Cluster B (Re-experiencing) | 21.42 (8.13) | |
| Cluster C (Avoidance/Emotional Numbing) | 31.79 (8.82) | |
| Cluster D (Hyperarousal) | 25.49 (4.99) |
Objective Sleep Assessment
Sleep was assessed objectively using actigraphy. Although PSG is the gold-standard for objective sleep assessment, actigraphy is more economical and less invasive (Smith et al., 2018). The current study focused on TST, SE, and SOL as indicators of sleep disturbance.
Actigraphy data were collected over seven nights using an actometer with basic motion-logger technology (Ambulatory Monitoring Inc., Ardsley, NY). Participants were instructed to press an event button when getting into bed at night and out of bed in the morning. Using similar procedures, research has found that TST, SE, and SOL are valid and reliable indicators relative to PSG (Withrow et al., 2019).
Actigraphy measurements were collected in 30s epochs using the proportional integrating mode (PIM). The Action-W analysis software (v 2.0) provided by Ambulatory Monitoring Inc. allowed for automated scoring by computing a down interval and estimates of normal sleep and wake time parameters. Additionally, the University of California – San Diego algorithm (Cole et al., 1992) was used to calculate sleep metrics for each night of recording. PIM data collection procedures and the UCSD scoring algorithm have been validated as robust analysis tools of actigraphy recordings as compared to PSG (Ancoli-Israel et al., 2003; Blackwell et al., 2008). Relative to the Cole-Kripke and Sadeh algorithms, the UCSD algorithm has been found to yield the least bias and strongest correlations with PSG in a related, sleep-impaired sample (Kim et al., 2013). All available nights of actigraphy data were averaged to create a mean score for each sleep variable.
Self-Reported Sleep Assessments
Daily Diaries
Daily diaries were adapted from previous research (Galovski & Blanchard, 1998; 2002). Each day, participants reported on their sleep the previous night. Responses were used to obtain nightly TST, SE, and SOL values. Notably, TST was reported in hours and was thus multiplied by 60 to obtain a value that could be compared against actigraphy. Diaries also assessed three aspects of sleep-related anxiety: “anxiety during the night when trying to sleep,” “disruptions during sleep time (scary noises),” and “leaving bed during night due to concerns/anxiety.” These items were rated on a 6-point scale from 0 (Not at all) to 5 (Debilitating, unable to function/continuous) and were summed to create a measure of daily sleep-related anxiety. All available nights of sleep diary data were averaged to create a mean score for each sleep variable.
Pittsburgh Sleep Quality Index (PSQI)
The PSQI (Buysse et al., 1989) is a 19-item measure of past month sleep quality. Relevant to the current study was the TST item assessing average hours slept per night (multiplied by 60) and the SOL item assessing average minutes to fall asleep per night. SE was calculated as TST divided by time in bed, multiplied by 100. Five participants with values >100 were excluded from SE analyses.
Clinical Symptom Measures
Standardized Trauma Interview
All participants completed a standardized trauma interview to collect basic demographic information and to confirm exposure to a Criterion A trauma.
Clinician-Administered PTSD Scale for DSM-IV (CAPS)
The CAPS (Blake et al., 1995) was used to diagnose current PTSD and assess clinician-rated symptom severity. This 22-item clinical interview assesses the frequency and intensity of each DSM-IV PTSD symptom. Clinician ratings (0-4) were summed to create a total score and three symptom clusters scores (i.e., re-experiencing, avoidance/emotional numbing, and hyperarousal). Previous research indicates that this interview has strong psychometric properties (Weathers et al., 2001).
Daily Diary Assessment of PTSD Symptoms
Participants provided daily reports of specific PTSD symptoms including: intrusive thoughts; flashbacks; nightmares; dissociation; racing heart; trouble breathing/shortness of breath; trembling/shaking; feeling as if you are in danger; feeling easily startled or jumpy; outbursts of anger; avoidance of trauma memories; emotional numbing; difficulty relating to others; anhedonia; feeling as if your normal life’s course has changed; difficulty recalling parts of the trauma; and difficulty concentrating. Items were rated on a 6-point scale from, 0 (Not at all) to 5 (Debilitating, unable to function/continuous). Again, all available assessments were averaged to obtain a mean score for each PTSD symptom.
Procedure
Procedures were approved by the Institutional Review Board at the University of Missouri–St. Louis. Participants provided informed consent and were compensated $30 for their participation. During an in-person assessment, participants completed self-report measures and clinical interviews. Participants were then given daily diary measures and instructed to complete them each day for one week. Participants were also fitted with the actometer on their non-dominant wrist. Participants returned to the clinic within two weeks, at which point daily diary and actigraphy data were collected. Average days of data collection for actigraphy and daily diary were 6.33 (_SD_=2.97) and 5.61 (_SD_=1.90), respectively.
Data Analytic Plan
Data were analyzed using SPSS (v. 27). Valid actigraphy, daily diary, and PSQI data were collected from 100%, 83.7%, and 95.3% of participants, respectively. Missingness was unrelated to demographic or clinical variables of interest (all _p_s>.05). Thus, data were assumed to be missing completely at random and all available data were included in analyses.
To determine whether sleep state misperception was present in our sample, we conducted repeated-measures ANOVAs with follow-up paired samples _t_-tests to examine TST, SE, and SOL as a function of assessment method. The magnitude of effects was examined using partial eta squared (ηp2) and Cohen’s d.
Next, we examined the correlations between clinician-rated PTSD symptoms and sleep state misperception. TST misperception was measured with two misperception index scores: one examining daily diaries and the other examining the PSQI, relative to actigraphy. These scores were calculated as: (objective TST mean – self-reported TST mean)/objective TST mean (Manconi et al., 2010). Higher scores indicated greater underestimation of TST relative to what was objectively observed. Previous research on misperception of other sleep indices has typically relied on simple difference scores (e.g., Herbert et al., 2017). We, thus, examined SE and SOL discrepancies by subtracting self-reported scores from objective scores. Separate scores were calculated to examine daily diaries and the PSQI relative to actigraphy.
We then conducted a more fine-grained examination of the associations between participant-rated PTSD symptoms assessed with daily diary and sleep state misperception using both correlational and linear regression analyses. Because participant-rated PTSD symptoms were specific to the period of daily diary and actigraphy data collection, in these latter analyses, we only examined the daily diary-actigraphy sleep state misperception variables.
Finally, we examined the relationships between sleep-related anxiety, nightmares, and daily diary-actigraphy sleep-state misperception using both correlations and linear regressions.
Results
Results of analyses comparing sleep indices across assessment methods are presented in Table 2. Moderate to large significant differences among assessment methods emerged for all three sleep indices. Relative to actigraphy, participants reported shorter TST on diaries and on the PSQI; average past month TST on the PSQI was also shorter than the daily diary average (Figure 1a). Similarly, participants reported worse SE on diaries and on the PSQI than what was observed with actigraphy. SE on the PSQI was also significantly worse than what was reported on diaries (Figure 1b). Finally, participants reported longer SOLs on diaries and the PSQI relative to actigraphy. Participants’ report of their average SOL on the PSQI was longer than their average daily diary report (Figure 1c).
Table 2.
Results from ANOVAs and paired samples t-tests examining total sleep time (TST), sleep efficiency (SE), and sleep onset latency (SOL) as a function of assessment method.
| Total Sleep Time (TST): F (2, 68) = 20.96, p < .001, ηp2 = .38 | ||||
|---|---|---|---|---|
| t | df | p | Cohen’s d | |
| Actigraphy vs. Daily Diary | 3.70 | 35 | .001 | .54 |
| Actigraphy vs. PSQI | 6.41 | 40 | < .001 | 1.00 |
| Daily Diary vs. PSQI | 3.63 | 34 | .001 | .61 |
| Sleep Efficiency (SE): F (2, 50) = 17.30, p < .001, ηp2 = .41 | ||||
| t | df | p | Cohen’s d | |
| Actigraphy vs. Daily Diary | 3.62 | 25 | .001 | .71 |
| Actigraphy vs. PSQI | 7.32 | 34 | < .001 | 1.26 |
| Daily Diary vs. PSQI | 2.27 | 25 | .03 | .44 |
| Sleep Onset Latency (SOL): F (2, 64) = 15.32, p < .001, ηp2 = .32 | ||||
| t | df | p | Cohen’s d | |
| Actigraphy vs. Daily Diary | −3.08 | 34 | .004 | −.52 |
| Actigraphy vs. PSQI | −5.06 | 41 | < .001 | −.74 |
| Daily Diary vs. PSQI | −2.90 | 32 | .007 | −.50 |
Figure 1.
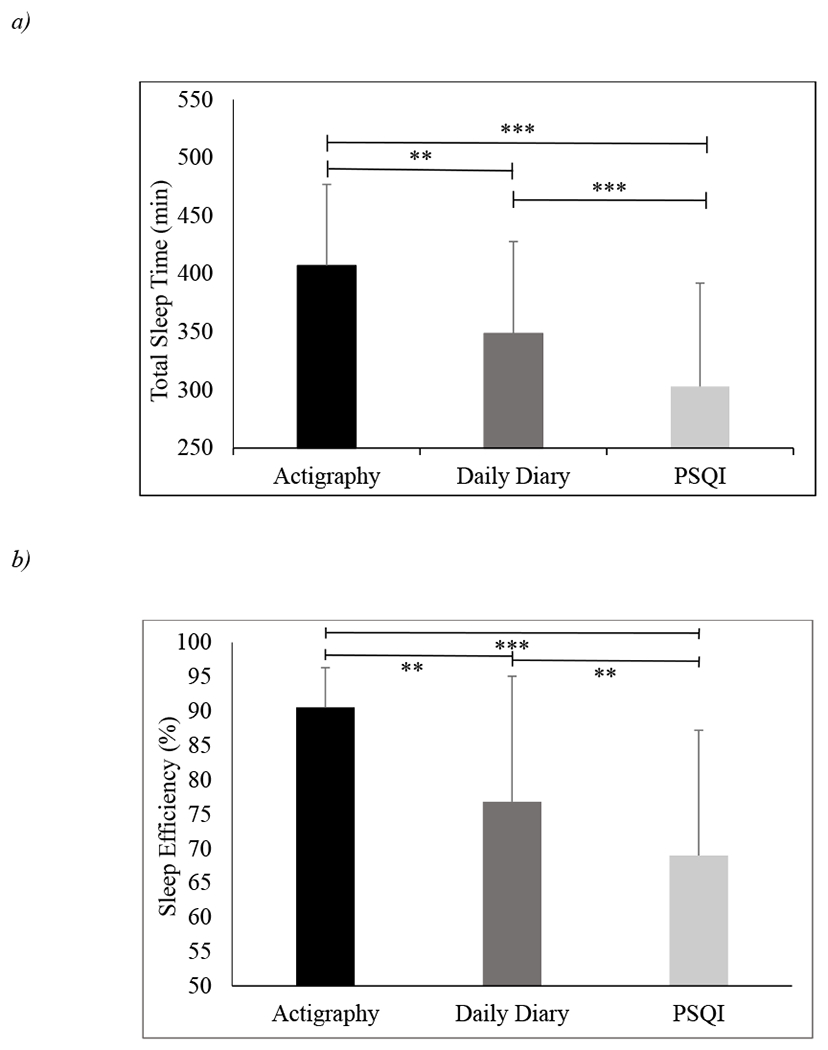
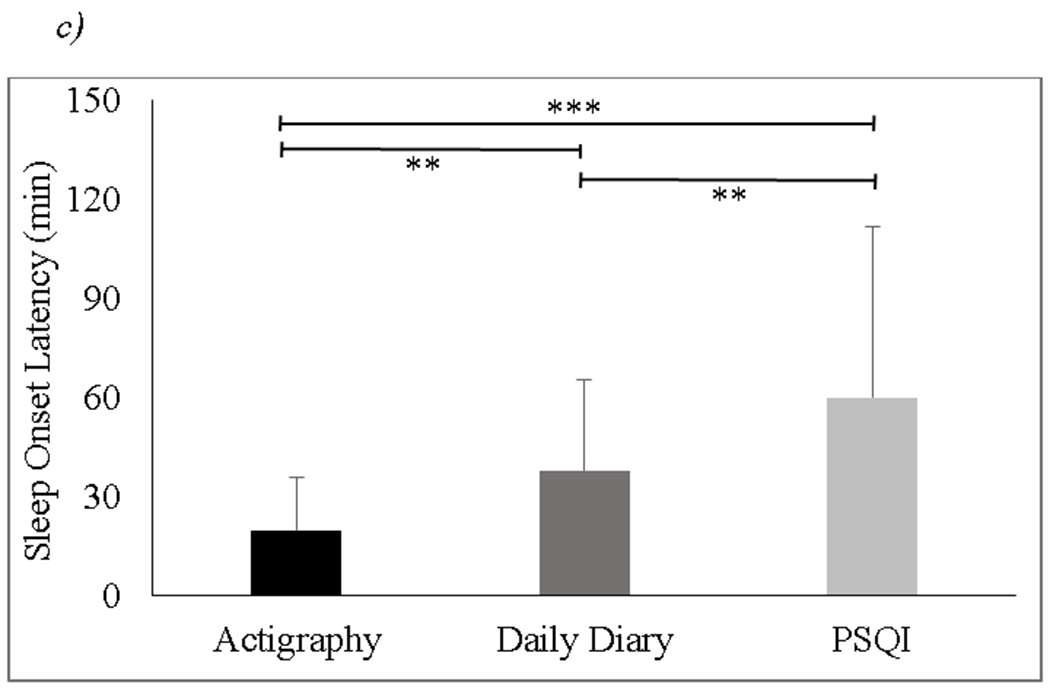
Differences in a) total sleep time (TST), b) sleep efficiency (SE), and c) sleep onset latency (SOL) across three assessment methods: actigraphy, daily diary, and the Pittsburgh Sleep Quality Index (PSQI).
Note. ** p < .01, *** p < .001; error bars reflect +1 standard deviation (SD).
Correlations between clinician-rated PTSD symptoms and misperception indices are presented in Table 3. Underestimation of TST and SE on diaries relative to actigraphy was associated with greater re-experiencing symptoms (Cluster B), but not with avoidance/emotional numbing (Cluster C) or hyperarousal symptoms (Cluster D). Underestimation of TST and SE on the PSQI relative to actigraphy was associated with greater re-experiencing, avoidance/emotional numbing, and hyperarousal symptoms. No significant associations emerged from these analyses examining clinician-rated PTSD symptoms and SOL difference scores.
Table 3.
Associations between clinician-rated PTSD symptoms and sleep state misperception variables.
| CAPSTotal Score | CAPSCluster B | CAPSCluster C | CAPSCluster D | |
|---|---|---|---|---|
| Total Sleep Time (TST) | ||||
| Daily Diary-Actigraphy | .47** | .46** | .27 | .31 |
| PSQI-Actigraphy | .46** | .35* | .34* | .36* |
| Sleep Efficiency (SE) | ||||
| Daily Diary-Actigraphy | .30 | .40* | .17 | .08 |
| PSQI-Actigraphy | .50* | .48** | .47** | .34* |
| Sleep Onset Latency (SOL) | ||||
| Daily Diary-Actigraphy | −.03 | −.10 | −.01 | .05 |
| PSQI-Actigraphy | −.19 | −.29 | .03 | −.20 |
Several specific PTSD symptoms assessed via daily diary were associated with a tendency to underestimate TST and SE, but not SOL, on diaries relative to actigraphy (Supplement Table 1). However, nightmares was the only symptom that was uniquely associated with daily diary-actigraphy TST misperception index scores, demonstrating a positive association of medium magnitude (Table 4)1. A similar pattern was found for SE misperception difference scores (Table 5).
Table 4.
Unique associations between PTSD symptoms assessed with daily diary and the daily-diary-actigraphy total sleep time (TST) misperception index score.
| PTSD Symptom | B | SE | β | t | p |
|---|---|---|---|---|---|
| Intrusive Thoughts | −.03 | .04 | −.17 | −.69 | .49 |
| Nightmares | .08 | .03 | .42 | 2.22 | .04 |
| Feelings of Danger | .02 | .04 | .12 | .51 | .62 |
| Startle/Jumpiness | .03 | .05 | .14 | .52 | .61 |
| Avoidance | −.04 | .03 | −.24 | −1.02 | .32 |
| Emotional Numbness | .02 | .05 | .14 | .40 | .69 |
| Relate to Others | −.003 | .06 | −.02 | −.05 | .96 |
| Enjoy Activities | .02 | .06 | .15 | .33 | .75 |
| Change in Life Course | .003 | .06 | .02 | .04 | .97 |
| Concentration Difficulty | .06 | .04 | .34 | 1.57 | .13 |
Table 5.
Unique associations between PTSD symptoms assessed with daily diary and the daily-diary-actigraphy sleep efficiency (SE) misperception index score.
| PTSD Symptom | B | SE | β | t | p |
|---|---|---|---|---|---|
| Intrusive Thoughts | 5.03 | 3.67 | .36 | 1.37 | .18 |
| Flashbacks | −1.47 | 3.63 | −.10 | −.40 | .69 |
| Nightmares | 8.49 | 2.96 | .53 | 2.87 | .009 |
| Trembling/Shaking | 3.78 | 3.69 | .23 | 1.03 | .32 |
| Startle/Jumpiness | −4.05 | 3.30 | −.27 | −1.23 | .23 |
| Concentration Difficulty | 1.66 | 2.74 | .11 | .61 | .55 |
Finally, sleep-related anxiety was positively and significantly associated with nightmares (_r_=.51, _p_=.002), TST (_r_=.56, p<.001) and SE (_r_=.65, p<.001) misperception, but not SOL misperception (_r_=−.25, _p_=.14). After controlling for sleep-related anxiety, nightmares were no longer associated with TST misperception (β=.18, _p_=.34), but remained significantly associated with SE misperception (β=.18, _p_=.045).
Discussion
This study sought to increase understanding of sleep state misperception in women with PTSD. Consistent with previous research with predominantly male samples, sleep state misperception was present in our sample of women with PTSD; on average, participants reported sleeping less, sleeping less efficiently, and taking longer to fall asleep than what was objectively observed. As hypothesized, sleep state misperception was also greater when assessed with the PSQI vs. daily diaries.
The second aim was to examine PTSD symptoms as predictors of sleep state misperception. Across analyses, specific PTSD symptoms were predictive of TST and SE, but not SOL, misperception. Indeed, despite SOL misperception being present in our sample, it was unrelated to PTSD or fear of sleep. Future research should identify other individual differences and/or methodological factors associated with the discrepancy between self-reported and objective SOL.
Within TST and SE analyses examining clinician-rated symptoms, differences between the actigraphy-daily diary and actigraphy-PSQI misperception emerged. Whereas actigraphy-PSQI misperception indices were positively associated with all three symptom clusters, actigraphy-daily diary misperception indices were only associated with re-experiencing symptoms. The reason for these differences is not entirely clear. Perhaps the broader associations between clinician-rated PTSD symptoms and actigraphy-PSQI misperception are driven by more pronounced effects of memory biases on sleep estimates on the PSQI (a global, more distally retrospective recollection of sleep quality) vs. daily diaries (a more recent recollection of previous night’s sleep; Slightam et al., 2018). PTSD is associated with memory biases, including a tendency to remember negative or trauma-related content and to forget positive or neutral content (Bomyea et al., 2017). It seems plausible that such biases extend to enhanced memory for poor sleep and deteriorated memory for high sleep quality. Alternatively, it is possible that, as compared to daily diaries, the PSQI is more susceptible to the effects of general distress, which is associated with greater sleep state misperception in other populations (Harvey & Tang, 2012).
We also examined the associations between participant-rated symptoms of PTSD and actigraphy-daily diary misperception. Consistent with hypotheses, more severe re-experiencing symptoms, including intrusive thoughts, flashbacks, and nightmares, were associated with greater TST/SE misperception. In contrast, the majority of hyperarousal symptoms assessed, including racing heart, trouble breathing, dissociation, and anger, were not significantly related to sleep state misperception. When all significant zero-order predictors were examined simultaneously, the only symptom that remained uniquely associated with TST/SE sleep state misperception was nightmares. Integrating these results with Werner and colleagues’ conceptual model (2021), it appears that sleep state misperception may be less closely associated with the path from hyperarousal symptoms to insomnia-related maladaptive processes and more closely associated with the path from re-experiencing symptoms to fear of sleep and related processes.
Analyses examining sleep-related anxiety provided additional support for the relevance of fear of sleep to sleep state misperception. Sleep-related anxiety was positively associated with both nightmare severity and TST/SE misperception. Further, after controlling for sleep-related anxiety, the association between nightmares and TST misperception was no longer significant. It is possible that sleep-related anxiety is one factor associated with previously observed PTSD-related sleep patterns, including decreased sleep depth and continuity (Cox & Olatunji, 2020). Results also suggests a pathway from nightmares to TST misperception through fear of sleep, though future research will need to confirm the direction of association between variables and more closely examine the mechanisms underlying such a pathway.
Several limitations should be noted. This exploratory study relied on a relatively small sample with some missing data. In addition, there were differences in how TST was assessed across measures. Actometers measured TST in minutes, while self-reported TST scores were reported in hours and then converted to minutes. It is possible that this methodological difference exacerbated the discrepancies between objective and self-report measures, though it seems unlikely that it fully explains the relatively large observed differences. Though adapted from previous research (Galovski & Blanchard, 1998; 2002), the daily diary assessments of PTSD symptoms and sleep-related anxiety have not been validated, which may have influenced study results. Finally, because data were collected prior to the publication of the DSM-5, the study utilized the CAPS-IV to assess clinician-rated PTSD symptoms. Given that the DSM-5 included changes to the PTSD symptom clusters (APA, 2013), it will be necessary to replicate results in persons meeting DSM-5 criteria for the disorder.
There are also several directions for future research. This study focused on differences between self-reported and objectively observed TST, SE, and SOL. However, there are other aspects of sleep that may also be disturbed among individuals with PTSD, including number of nighttime awakenings and time spent awake during the night. Actigraphy measures sleep indirectly via movement and, as such, can sometimes miscategorize wakefulness in the absence of movement as sleep or movement during sleep as wakefulness. Perhaps because of these methodological limitations, actigraphy has been found to be a less reliable objective assessment of these sleep indicators (Withrow et al., 2019). Still, future studies should examine possible misperception of these aspects of sleep and to explore clinical predictors of potential discrepancies which could provide a more complete understanding of PTSD-related sleep disturbances. Given methodological limitations of actigraphy, it may be beneficial to extend research on sleep state misperception in PTSD to include comparisons of self-reported sleep to sleep that is objectively observed using PSG. With repeated assessments of self-reported and objectively observed sleep, it would also be interesting to conduct a more fine-grained analysis of how daily PTSD symptoms and nightly sleep state misperception are associated using a linear mixed models approach. Finally, future research may benefit from including both women and men, and a trauma-exposed control group or participants with subclinical PTSD symptoms to broaden our understanding of sleep state misperception across individuals with PTSD and more varied trauma-related sequelae.
Despite limitations and the need for additional research on this topic, the study offers valuable insight into the phenomenon of sleep state misperception in PTSD. Results indicate that women with re-experiencing symptoms, particularly nightmares, may be especially high risk of experiencing sleep state misperception. This may be due to fear of sleep/sleep-related anxiety that develops from nightmares. Sleep state misperception may represent a fruitful target of intervention for individuals with PTSD and associated sleep disturbance. Investigators may consider targeting sleep state misperception directly, perhaps though psychoeducation about the phenomenon or using data driven feedback (Tang & Harvey, 2006). Alternatively, if nightmares and associated fear of sleep are confirmed to play a causal role in the development and maintenance of sleep state misperception, it may be helpful to target these constructs using cognitive behavioral techniques, such as cognitive reappraisal and/or imagery rehearsal.
Supplementary Material
Supp 1
Acknowledgments
This research was supported by the National Center for Complementary and Alternative Medicine Grant 1R21AT004079 (PI: Galovski). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States Government. The authors have no conflicts of interest to disclose.
Footnotes
1
To assess for potential multicollinearity, we examined zero-order correlations among daily diary PTSD symptoms. Results are presented in Supplement Table 2. Strong correlations (≥.80) were found between difficulty relating to others and emotional numbing, anhedonia, and feeling like one’s life course has changed, as well as between anhedonia and feeling like one’s life course has changed. Rerunning the regression model including each of these symptoms without the other three (e.g., including difficulty relating to others, but excluding emotional numbing, anhedonia, and feeling like one’s life course has changed) did not alter the pattern of results.
References
- American Academy of Sleep Medicine. (2005). International Classification of Sleep Disorders: Diagnostic and Coding Manual (2nd Ed). Westchester, IL: American Academy of Sleep Medicine. [Google Scholar]
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association. [Google Scholar]
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W & Pollak C (2003). The role of actigraphy in the study of sleep and circadian rhythms. Sleep, 26(3), 342–392. doi: 10.1093/sleep/26.3.342 [DOI] [PubMed] [Google Scholar]
- Arditte Hall KA, Werner KB, Griffin MG, & Galovski TE (2020). The effects of cognitive processing therapy + hypnosis on objective sleep quality in women with posttraumatic stress disorder. Psychological Trauma: Theory, Research Practice and Policy. Advance online publication. doi: 10.1037/tra0000970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belleville G, Guay S, & Marchand A (2011). Persistence of sleep disturbances following cognitive-behavior therapy for posttraumatic stress disorder. Journal of Psychosomatic Research, 70(4), 318–327. doi: 10.1016/j.jpsychores.2010.09.022 [DOI] [PubMed] [Google Scholar]
- Blackwell T, Redline S, Ancoli-Israel S, Schneider JL, Surovec S, Johnson NL, … for the Study of Osteoporotic Fractures Research Group (2008). Comparison of sleep parameters from actigraphy and polysomnography in older women: The SOF Study. Sleep, 31(2), 283–291. doi: 10.1093/sleep/31.2.283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–90. doi: 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- Bomyea J, Johnson A, & Lang AJ (2017). Information processing in PTSD: Evidence for biased attentional, interpretation, and memory processes. Psychopathology Review, 4(3), 218–243. doi: 10.5127/pr.037214 [DOI] [Google Scholar]
- Buysse DJ, Reynolds CF III, Monk TH, Berman SR, & Kupfer DJ. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Journal of Psychiatric Research, 28(2), 193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Cole RJ, Kripke DF, Gruen W, Mullaney DJ, & Gillin JC (1992). Automatic sleep/wake identification from wrist activity. Sleep, 15(5), 461–469. doi: 10.1093/sleep/15.5.461 [DOI] [PubMed] [Google Scholar]
- Cox RC, & Olatunji BO (2020). Sleep in the anxiety-related disorders: A meta-analysis of subjective and objective research. Sleep Medicine Reviews, 51, 101282. doi: 10.1016/j.smrv.2020.101282 [DOI] [PubMed] [Google Scholar]
- Edinger JD, & Krystal AD (2003). Subtyping primary insomnia: Is sleep state misperception a distinct clinical entity? Sleep Medicine Reviews, 7(3), 203–214. doi: 10.1053/smrv.2002.0253 [DOI] [PubMed] [Google Scholar]
- Galovski TE, & Blanchard EB (1998). The treatment of irritable bowel syndrome with hypnotherapy. Applied Psychophysiology and Biofeedback, 23(4), 219–232. [DOI] [PubMed] [Google Scholar]
- Galovski TE, & Blanchard EB (2002). The effectiveness of a brief psychological intervention on court-referred and self-referred aggressive drivers. Behaviour Research and Therapy, 40(12), 1385–1402. doi: 10.1016/S0005-7967(01)00100-0 [DOI] [PubMed] [Google Scholar]
- Galovski TE, Mott J, Blain LM, Elwood L, Gloth C, & Fletcher T (2016). Augmenting CPT to improve sleep impairment in PTSD: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 84(2), 167–177. doi: 10.1037/ccp0000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghadami MR, Khaledi-Paveh B, Nasouri M, & Khazaie H (2015). PTSD-related paradoxical insomnia: An actigraphic study among veterans with chronic PTSD. Journal of Injury and Violence Research, 7(2), 54–58. doi: 10.5249/jivr.v7i2.607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, & Tang N (2012). (Mis)perception of sleep in insomnia: A puzzle and a resolution. Psychological Bulletin, 138(1), 77–101. doi: 10.1037/a0025730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert V, Pratt D, Emsley R, & Kyle SD (2017). Predictors of nightly subjective-objective sleep discrepancy in poor sleepers over a seven-day period. Brain Science, 7(3), 29. doi: 10.3390/brainsci7030029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurwitz TD, Mahowald MW, Kuskowski M, & Engdahl BE (1998). Polysomnographic sleep is not clinically impaired in Vietnam combat veterans with chronic posttraumatic stress disorder. Biological Psychiatry, 44, 1066–1073. doi: 10.1016/S0006-3223(98)00089-4 [DOI] [PubMed] [Google Scholar]
- Kim MJ, Lee GH, Kim CS, Kim WS, Chung YS, Chung S, & Lee SA (2013). Comparison of three actigraphic algorithms used to evaluate sleep in patients with obstructive sleep apnea. Sleep and Breathing, 17(1), 297–304. doi: 10.1007/s11325-012-0689-z [DOI] [PubMed] [Google Scholar]
- Klein E, Koren D, Arnon I, & Lavie P (2003). Sleep complaints are not corroborated by objective sleep measures in post-traumatic stress disorder: A 1-year prospective study in survivors of motor vehicle crashes. Journal of Sleep Research, 12, 35–41. doi: 10.1046/j.1365-2869.2003.00334.x [DOI] [PubMed] [Google Scholar]
- Kobayashi I, & Delahanty DL (2013). Gender differences in subjective sleep after trauma and the development of posttraumatic stress disorder symptoms: A pilot study. Journal of Traumatic Stress, 26(4), 467–474. doi: 10.1002/jts.21828 [DOI] [PubMed] [Google Scholar]
- Kobayashi I, Huntley E, Lavela J, & Mellman TA (2012). Subjectively and objectively measured sleep with and without posttraumatic stress disorder and trauma exposure. Sleep, 35(7), 957–965. doi: 10.5665/sleep.1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffel E, Khawaja IS, & Germain A (2016). Sleep disturbances in posttraumatic stress disorder: Updated review and implications for treatment. Psychiatry Annals, 46(3), 173–176. doi: 10.3928/00485713-20160125-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen SE, Fleming CJE, & Resick PA (2019). Residual symptoms following empirically supported treatments for PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 11(2), 207–215. doi: 10.1037/tra0000384 [DOI] [PubMed] [Google Scholar]
- Lewis C, Lewis K, Kitchiner N, Isaac S, Jones I, & Bisson JI (2020). Sleep disturbance in post-traumatic stress disorder (PTSD): A systematic review and meta-analysis of actigraphy studies. European Journal of Psychotraumatology, 11(1), 1767349. doi: 10.1080/20008198.2020.1767349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipinska G, & Thomas KGF (2017). Better sleep in a strange bed? Sleep quality in South African women with posttraumatic stress disorder. Frontiers in Psychology, 8, 1555. doi: 10.3389/fpsyg.2017.01555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manconi M, Ferri R, Sagrada C, Punjabi NM, Tettamanzi E, Zucconi M, … Ferini-Strambi L (2010). Measuring the error in sleep estimation in normal subjects and in patients with insomnia. Journal of Sleep Research, 19(3), 478–486. doi: 10.1111/j.1365-2869.2009.00801.x [DOI] [PubMed] [Google Scholar]
- Pruiksma KE, Taylor DJ, Wachen JS, Mintz J, Young-McCaughan S, Peterson AL, … Resick PA (2016). Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychological Trauma: Theory, Research, Practice, and Policy, 8(6), 697–701. doi: 10.1037/tra0000150 [DOI] [PubMed] [Google Scholar]
- Rezaie L, Fobian AD, McCall WV, & Khazaie H (2018). Paradoxical insomnia and subjective-objective sleep discrepancy: A review. Sleep Medicine Reviews, 40, 196–202. doi: 10.1016/j.smrv.2018.01.002 [DOI] [PubMed] [Google Scholar]
- Slightam C, Petrowski K, Jamison AL, Keller M, Bertram F, Kim S, & Roth WT (2018). Assessing sleep quality using self-report and actigraphy in PTSD. Journal of Sleep Research, 27, 1–10. doi: 10.1111/jsr.12632 [DOI] [PubMed] [Google Scholar]
- Smith MT, McCrae CS, Cheung J, Martin JL, Harrod CG, Heald JL, & Carden KA (2018). Use of actigraphy for the evaluation of sleep disorders and circadian rhythm sleep-wake disorders: An American Academy of Sleep Medicine clinical practice guideline. Journal of Clinical Sleep Medicine, 14(7), 1231–1237. doi: 10.5664/jcsm.7230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang NKY, & Harvey AG (2006). Altering misperception of sleep in insomnia: Behavioral experiment vs. verbal feedback. Journal of Consulting and Clinical Psychology, 74(4), 767–776. doi: 10.1037/0022-006X.74.4.767 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT (2001). Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety, 13(3), 132–156. doi: 10.1002/da.1029 [DOI] [PubMed] [Google Scholar]
- Werner GG, Riemann D, & Ehring T (2021). Fear of sleep and trauma-induced insomnia: A review and conceptual model. Sleep Medicine Reviews, 55, 101383. doi: 10.1016/j.smrv.2020.101383 [DOI] [PubMed] [Google Scholar]
- Werner KB, Griffin MG, & Galovski TE (2016). Objective and subjective measurement of sleep disturbance in female trauma survivors with posttraumatic stress disorder. Psychiatry Research, 240, 234–240. doi: 10.1016/j.psychres.2016.04.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Withrow D, Roth T, Koshorek G, & Roehrs T (2019). Relation between ambulatory actigraphy and laboratory polysomnography in insomnia practice and research. Journal of Sleep Research, 28, e12854. doi: 10.1111/jsr.12854 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supp 1