Preferences for and barriers to gender affirming surgeries in transgender and non-binary individuals (original) (raw)
Abstract
Background: The transgender/non-binary community continues to be an underserved population in medicine, and our understanding of their interests, disinterests, and barriers to transition-related healthcare is quite limited, especially among the diverse gender identities within the transgender/non-binary umbrella.
Aim: To determine the interests, disinterests and barriers to gender affirming surgeries for transgender men, transgender women and non-binary individuals of any birth-assigned sex.
Methods: An anonymous, online survey using REDcap was applied across all 50 states and advertised through social media, healthcare organization websites and flyers. The responses of individuals greater than 18 years of age who identified as transgender or non-binary were analyzed.
Results: Compared to the 2015 US Transgender Survey, interest in gender affirming surgeries was higher across all gender identities surveyed and for all procedures, by an average of 38%. Interest overall in gender affirming procedures varied greatly among gender identity groups as well as with age differences. Barriers were found to be a mixture of lack of resources for recovery, financial, and a fear of complications.
Discussion: Our results highlight that a desire for these procedures is unique for each individual and should never be assumed for transgender/non-binary patients. In order to better aid this underserved population, the medical community must further work to mitigate the barriers to gender affirming procedures by decreasing cost, investigating ways to increase access to resources for recovery, and improving outcomes for each of the gender affirming surgeries.
Keywords: Facial feminization, gender affirming surgery, non-binary preferences, survey, transgender
Introduction
The population of transgender adults in the United States is estimated to be between 1 and 1.4 million (Flores et al., 2016; Meerwijk & Sevelius, 2017). As this number continues to rise, so does the availability of gender affirming therapies for those experiencing gender dysphoria (Cai et al., 2019; Roehr, 2015; Unger, 2017). These interventions, as outlined by the World Professional Association for Transgender Health (WPATH) Standards of Care, include hormone therapy, counseling, voice therapy, and gender affirming surgeries (GAS) (Coleman et al., 2012). In the nation’s largest transgender survey conducted by the National Center for Transgender Equality (NCTE), the 2015 US Transgender Survey (USTS), 49% of the 27,715 respondents reported having received hormone therapy, and 25% reported having some form of transition related surgery (James et al., 2016). Not every person with gender dysphoria desires surgical interventions, yet the incidence of trans-related surgeries has increased over time (Canner et al., 2018). The American Society of Plastic Surgeons reported a 115% increase in the number of gender affirming surgeries from 2016 to 2017 (American Society of Plastic Surgeons, 2017). Studies have shown overwhelmingly that transgender individuals who receive GAS experience improved quality of life, high satisfaction rates, few regrets, and improvements in self-confidence and social interactions (Cai et al., 2019; Nelson et al., 2009; Terrier et al., 2014). However, the cost of gender therapies is high, as is the rate of denials for coverage by insurance companies (Unger, 2017). This is despite literature showing insurance coverage to be cost effective and coverage refusal to result in poor health outcomes (Padula & Baker, 2017; Padula et al., 2016). Even though progress has been made in providing gender affirming therapy for people with gender dysphoria, significant barriers in accessing both general and transition related care persist (El-Hadi et al., 2018; Gridley et al., 2016; Lerner & Robles, 2017; Sanchez et al., 2009; Sineath et al., 2016; White Hughto et al., 2017).
Barriers to GAS reported in the literature include a combination of financial, emotional, and interpersonal factors, as well as a deficiency of well-trained medical professionals (Puckett et al., 2018). Even with recent improvements in healthcare insurance policy to increase coverage and access to GAS, transgender patients still report financial barriers to be the largest hurdles to receiving care (Puckett et al., 2018). Financial hurdles include cost of procedures, insurance loopholes, and unemployment. The next biggest barrier has been reported to be a lack of professionals trained to give gender-affirming care (Puckett et al., 2018). However, little is known about how these barriers differ among the spectra of gender identities. Furthermore, little is known about varying interests in procedures across gender identity. Medical professionals must expand upon their understanding of non-binary and transgender patients’ identities and desires or risk decreasing their patients’ agencies and forcing them into a box (Linander et al., 2019). It is important to increase awareness in the medical community about the highly individualized interests and needs of these patient populations. The goal of this study was to understand how barriers to GAS differ among various gender identities, as well as to further elucidate the preferences for specific GAS.
Methods
An anonymous, national survey directed at trans/non-binary individuals was designed with 146 multiple choice and free response questions built into the REDCap application. The survey was reviewed by the healthcare professionals in our group, a Lesbian, Gay, Bisexual, Transgender (LGBT) representative within our research group, and the director of the LGBT Resource Center at the University of Utah. The survey focused on experience with transition related surgeries, mental health and demographic questions of employment level, race/ethnicity, gender identity, age and relationship status. It was designed based on knowledge gaps from the 2015 U.S. Transgender Survey by the National Center for Transgender Equality, specifically with regards to why individuals desire certain procedures and why they experience certain barriers (James et al., 2016). It was advertised through social media, healthcare organization websites, and flyers. Social media channels included Facebook, Instagram, and Twitter. Survey participants were not provided compensation. Inclusion criteria were at least 18 years of age, U.S. residency, identifying as trans/non-binary, and completing the full survey. For purposes of clarity to the participants, we used the term “bottom surgery” to refer to gender-affirming genital surgeries and “top surgery” to refer to gender-affirming chest surgery (including breast reduction, mastectomy with or without nipple-areolar reconstruction or positioning, and breast augmentation). For consistency with our survey, we used the terms top and bottom surgery throughout the article.
Categorical variables were compared against gender identities using a Pearson’s chi-square test. Multiple comparative analyses of mental health outcomes by GAS were performed using a false discovery rate (FDR) <5%, with p values adjusted by the Benjamini–Hochberg correction. A p value of <0.05 was used for statistical significance. Analysis was done with four groups of gender identities: transgender men, transgender women, non-binary individuals assigned female at birth (AFAB), and non-binary individuals assigned male at birth (AMAB). The outcomes measured were the responses to multiple choice questions and differences among these four groups. Respondents were also split into two age groups, 40 years and above and under 40 years for separate analyses. We used these differences to analyze the different needs, desires, and barriers for each group with regards to GAS.
Results
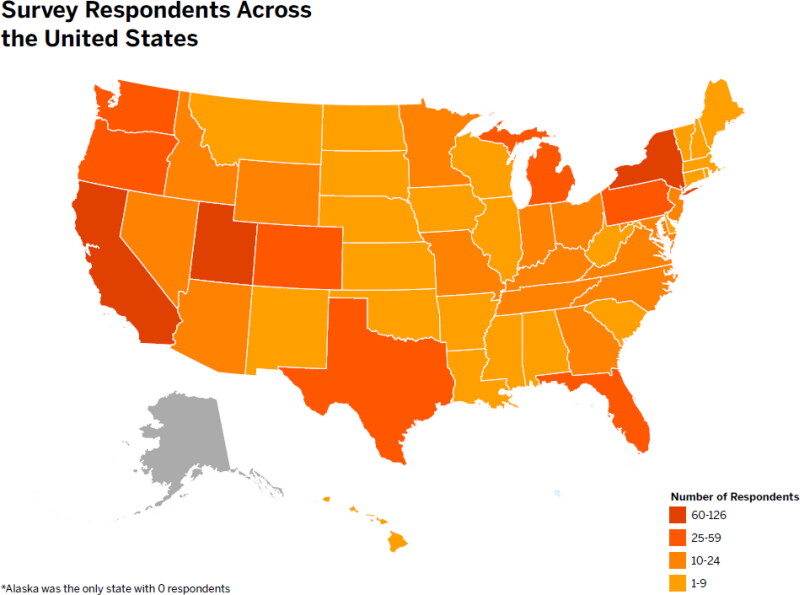
1092 responses from across the United States were collected. After eliminating partial responses or duplicates, a total of 887 individuals were included in the study who represented 49 states (Figure 1). 383 identified as transgender women, 49 as non-binary people AMAB, 298 as transgender men, and 158 non-binary people AFAB.
Figure 1.
Number of respondents from each state. This is a heat map visually representing the number of respondents from each state, with darker colors indicating more respondents from that state as per the legend key.
The majority of responses came from individuals in their late 20s to early 40s (range 18–74 years, average age 34 years). There were statistically significant differences in age across the groups (p < 0.001) with transgender women having the highest average age at 42 years and non-binary AFAB individuals having the lowest at 27 years (p < 0.001). Predominantly Caucasian identifying people filled out the survey (82%). Most of the respondents were insured (88%), with 69% having private insurance and 19% having Medicare/Medicaid. Forty-five percent of the respondents had full-time employment (Table 1). Over half the respondents across all gender identities reported mental illness diagnoses, predominantly anxiety (59%) and depression (64%). Nearly half (45%) reported a suicide attempt in their life.
Table 1.
Demographic data of respondents.
| Demographic | All | Transmen | Non-binary AFAB | Transwomen | Non-binary AMAB | p value | |
|---|---|---|---|---|---|---|---|
| Total respondents | 887 | 298 | 158 | 383 | 49 | ||
| Average Age | 34 | 28 | 27 | 42 | 37 | <0.001 | |
| Race | White | 82% | 80% | 80% | 85% | 80% | 0.37 |
| Non-white | 18% | 20% | 20% | 15% | 20% | ||
| Education | High school or below | 16% | 20% | 13% | 14% | 10% | 0.06 |
| College and above | 84% | 80% | 87% | 86% | 90% | ||
| Employment | Full time | 45% | 46% | 36% | 47% | 45% | <0.001 |
| Student | 18% | 22% | 32% | 9% | 14% | ||
| Other | 38% | 32% | 31% | 44% | 41% | ||
| Relationship | No partner | 46% | 47% | 41% | 47% | 47% | 0.58 |
| Partnered | 54% | 53% | 59% | 53% | 53% | ||
| Insurance | Uninsured | 12% | 11% | 8% | 15% | 4% | 0.002 |
| Private Insurance | 69% | 74% | 77% | 62% | 71% | ||
| Medicare/Medicaid/VA | 19% | 15% | 15% | 24% | 24% | ||
| Mental Health | Anxiety | 59% | 69% | 71% | 48% | 49% | <0.001 |
| Depression | 64% | 69% | 72% | 57% | 55% | <0.001 | |
| Other diagnosisa | 32% | 30% | 47% | 27% | 35% | <0.001 | |
| Suicide attempt | 45% | 46% | 51% | 43% | 43% | <0.001 |
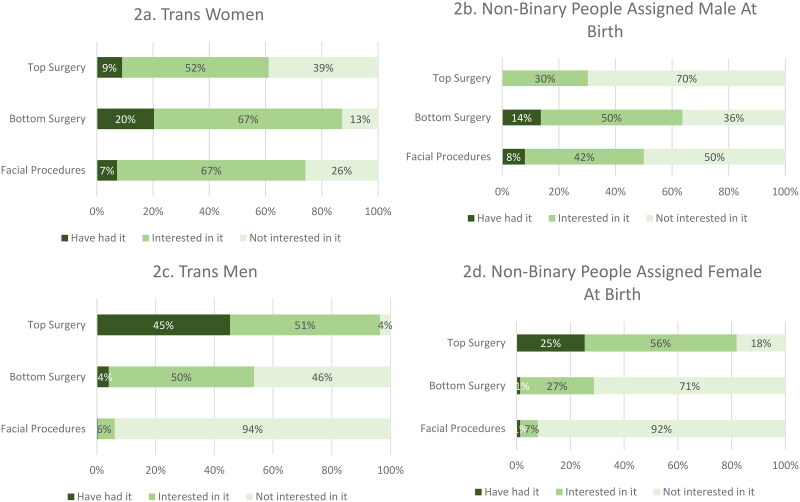
The majority of transgender women expressed interest in GAS. Bottom surgery in the form of vaginoplasty or vulvoplasty was highly desired, with 20% having had the surgery and an additional 67% wanting it. For top surgery, 9% had undergone breast enhancement and 52% more wanted it. While only 7% of transgender women had undergone facial feminizing surgery, an additional 67% expressed wanting it (Figure 2a).
Figure 2.
Percentage of respondents who have had, or are interested, in gender affirming procedures. Each bar represents a different surgery, reading top surgery, bottom surgery, and facial procedures from top down. Dark green represents having had the procedure, light green represents being interested in the procedure, and lightest green indicates no interest in the procedure. Top left corner shows data for transgender women (n = 383), top right shows data for non-binary respondents assigned male at birth (n = 49), bottom left corner shows data for transgender men (n = 298), and bottom right corner shows data for non-binary respondents assigned female at birth (n = 158).
As a group, non-binary AMAB respondents were less interested in GAS than transgender women. Similar to transgender women, the largest interest was in bottom surgery (14% of non-binary AMAB respondent had it and 50% wanted it in comparison with 20% of transgender women having already had bottom surgery and 67% desiring it). The frequency of facial procedures in this identity group was similar to transgender women (8% had it and 42% wanting it). Interestingly, there were no non-binary AMAB participants who had undergone top surgery, and only 30% expressed interest in having it (Figure 2b).
Among transgender men, the vast majority indicated they either had undergone top surgery (45%) or were interested in pursuing it (51%). In contrast, only 4% of transgender men had undergone bottom surgery, including phalloplasty or metoidioplasty, but an additional 50% expressing interest in undergoing the procedures. Overwhelmingly, transgender men expressed little interested in facial procedures (94%) (Figure 2c).
Non-binary AFAB respondents had a high interest in top surgery (25% had it and 56% were interested in it). AFAB non-binary respondents indicated disinterest in bottom surgery at a higher frequency out of all four gender categories (71%). Similar to transgender men, nearly all non-binary AFAB respondents were disinterested in facial procedures (92%) (Figure 2d).
Barriers to gender affirming procedures
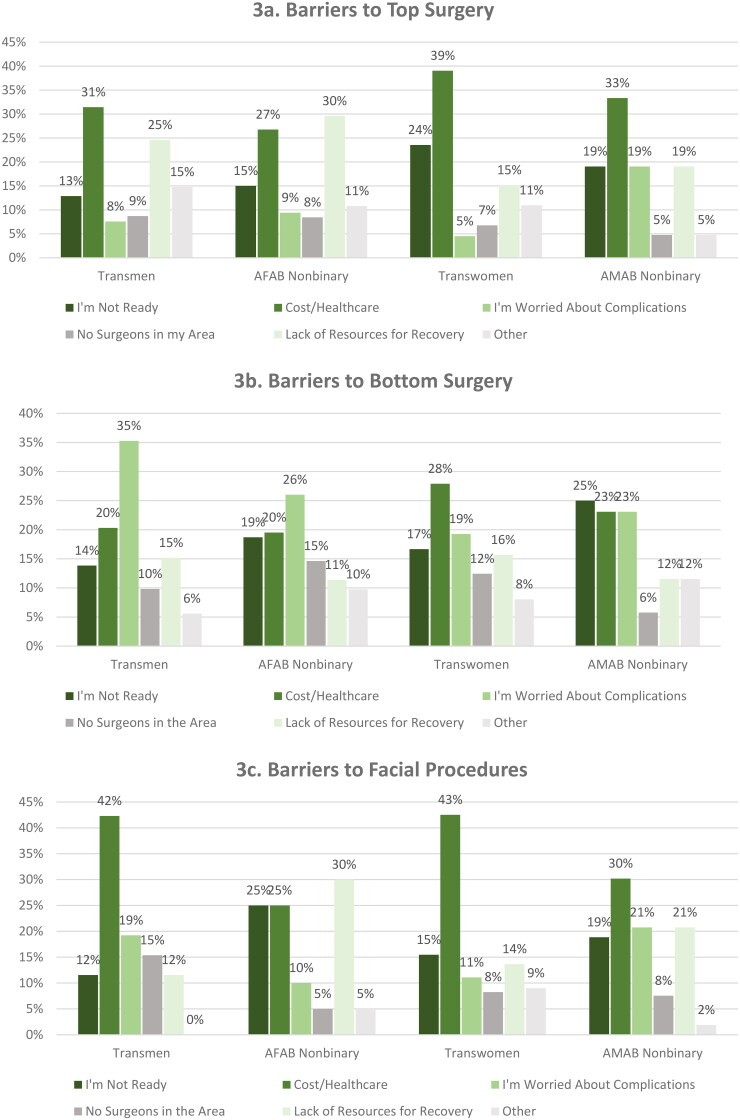
For respondents who indicated they were interested in a type of GAS but had not yet undergone a procedure, there were distinct barriers associated with different procedures. For top surgery, the largest barrier across all groups was financial. For transgender men and non-binary AFAB individuals who were interested in top surgery, healthcare limitations and lack of resources for recovery were listed as principal barriers. Most common barriers to top surgery for transgender women were cost (39%) and lack of readiness (24%) (Figure 3a).
Figure 3.
Barriers to each gender affirming procedure for the four gender identities surveyed. Participants interested in a specific surgery who had not had it yet were asked to list their barriers to that procedure. Each barrier is listed as a different bar, with percentages of how frequently each option was selected. (a) The barriers to top surgery, with transgender men (n = 143), non-binary AFAB (n = 85), transgender women (n = 237), and non-binary AMAB (n = 13) reading left to right. (b) The barriers to bottom surgery, with transgender men (n = 160), non-binary AFAB (n = 42), transgender women (n = 247), and non-binary AMAB (n = 22) reading left to right. (c) The barriers to facial procedures, with transgender men (n = 16), non-binary AFAB (n = 10), transgender women (228), and non-binary AMAB (n = 21) reading left to right.
For bottom surgery, cost and lack of healthcare resources were the principal barriers for all gender groups, but it was the greatest barrier for transgender women and non-binary AMAB respondents (28% and 25%, respectively). For transgender men and non-binary AFAB respondents, concern for complications was the most frequent barrier (35% and 26%, respectively). Non-binary AMAB individuals listed not being ready for the procedure as the most common barrier to bottom surgery (25%) (Figure 3b).
For facial procedures, cost and lack of healthcare resources was listed as the biggest barrier across most gender categories (30%, 42%, 43% for non-binary AMAB, transgender men, and transgender women respectively). For AFAB non-binary respondents, lack of resources for recovery was the largest barrier (30%) (Figure 3c).
Disinterest in gender affirming procedures
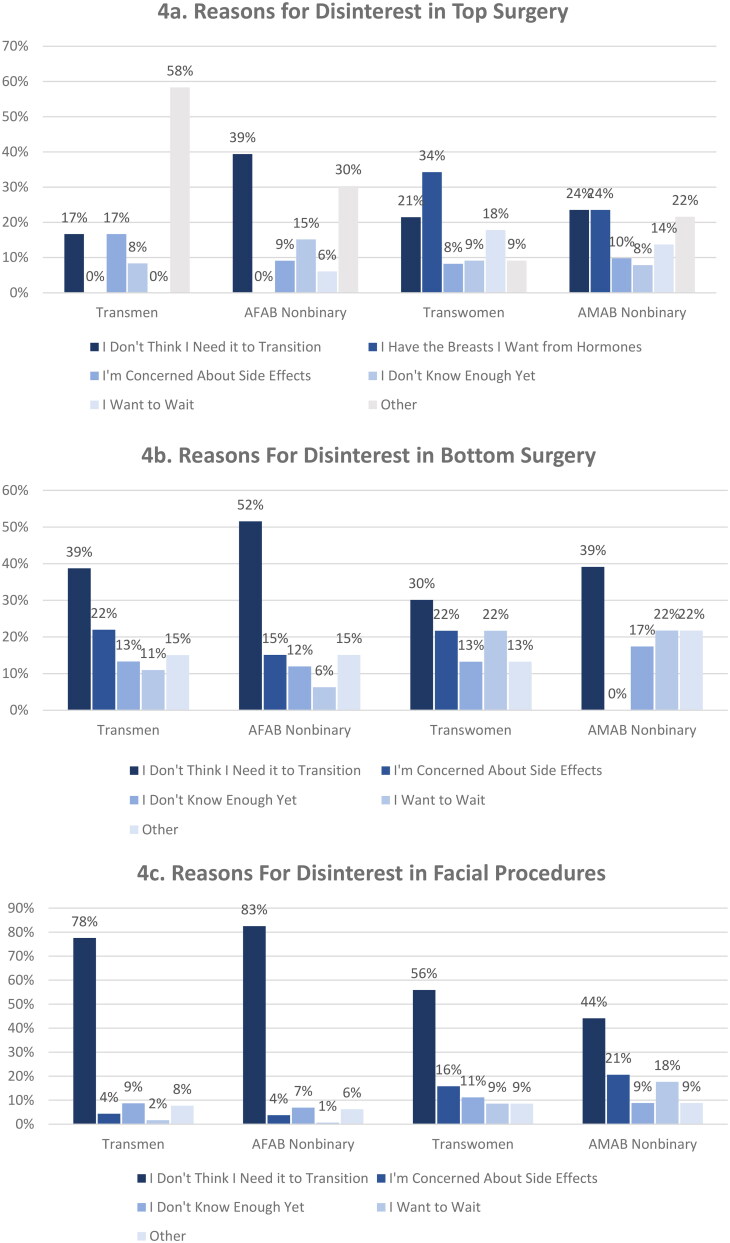
For each of the respondents who indicated they were not interested in a particular procedure, we asked them about the reasons for their disinterest. Of the 39% of transwomen not interested in top surgery, 34% indicated that they had enough breast development from hormone therapy and 21% stated that they did not need it for their transition. For the non-binary AMAB respondents, of which a large number (70%) did not want top surgery, 24% said this was due adequate breast development with hormones and 24% stated that they did not need it for their transition. While the vast majority of transgender men (96%) and non-binary AFAB (81%) desired top surgery, for those who did not want it, the most common reason among the non-binary group was “not needing it for my transition” (39%) and “other” (58%) for the transmen not wanting surgery (Figure 4a).
Figure 4.
Reasons that each respondent was not interested each gender affirming procedure for the four gender identities surveyed. Participants who were not interested in a particular procedure were asked to list their reasons. Each reason is listed as a different bar, with percentages of how frequently each option was selected. There are 4 separate bar graphs for each gender identity. From top to bottom, data is shown for top surgery, bottom surgery, and facial procedures. (a) The reasons for disinterest in top surgery, with transgender men (n = 10), non-binary AFAB (n = 28), transgender women (n = 147), and non-binary AMAB (n = 33) reading left to right. (b) The reasons for disinterest in bottom surgery, with transgender men (n = 105), non-binary AFAB (n = 109), transgender women (n = 47), and non-binary AMAB reading left to right (n = 18). (c) The reasons for disinterest in facial procedures, with transgender men (n = 262), non-binary AFAB (n = 141), transgender women (n = 111), and non-binary AMAB (n = 25) reading left to right.
Across all gender categories, those who lacked interest in bottom surgery indicated the primary reason as “not needed” for their transition. This was seen most dramatically in the non-binary AFAB group, where, in the 71% who did not want bottom surgery, over half stated they did not need it for their transition. Of the 46% of transmen who did not want bottom surgery, the most common reasons were not needing it to transition (39%) and concern for side effects (22%). While the majority of transgender women (77%) and non-binary AMAB (64%) desired vaginoplasty or vulvoplasty, those not interested stated not needing it for their transition (30%, 39% respectively) as the most common reason (Figure 4b).
For facial procedures, the most common reason for disinterest was “not needing it for transition” (78% for transgender men, 85% for non-binary AFAB, 56% for transgender women, and 44% for non-binary AMAB). An important concern for transgender women and non-binary AMAB respondents was the potential side effects (16%, 21% respectively) (Figure 4c).
By age
Respondents were additionally considered by age as the demographics between groups were noted to be different by age. Younger (39 and below) as well as older (40 and above) participants varied in their responses. Older respondents were more likely to have already had top surgery (p = 0.01) bottom surgery (p = 0.04) or facial procedures (p < 0.0001) regardless of gender identity. Younger respondents were also more interested in top surgery (p < 0.0001) whereas older respondents showed greater interest in bottom surgery (p = 0.01) and facial procedures (p = 0.0001) (Table 2).
Table 2.
Interest/barriers by age.
| Variable | Under 40 | Over 40 | p value* | |
|---|---|---|---|---|
| N = 581 | N = 253 | |||
| Procedures FTM | Top surgery | 131 (34%) | 26 (52%) | 0.01 |
| Bottom surgery | 10 (3%) | 4 (8%) | 0.04 | |
| Facial procedures | 2 (0.5%) | 0 (0%) | n/s | |
| Other | 38 (10%) | 9 (18%) | 0.09 | |
| None | 236 (62%) | 23 (46%) | 0.03 | |
| Procedures MTF | Top surgery | 7 (3%) | 26 (13%) | 0.0005 |
| Bottom surgery | 18 (9%) | 59 (30%) | <0.0001 | |
| Facial procedures | 7 (3%) | 22 (11%) | 0.003 | |
| Other | 10 (5%) | 20 (10%) | 0.05 | |
| None | 171 (83%) | 115 (57%) | <0.0001 | |
| Challenges getting top surgery | Cost | 99 (71%) | 36 (69%) | 0.73 |
| Few surgeons | 54 (39%) | 16 (30%) | 0.29 | |
| Time off | 26 (19%) | 2 (4%) | 0.009 | |
| Recovery | 29 (21%) | 8 (15%) | 0.38 | |
| Other | 7 (5%) | 5 (10%) | **0.**25 | |
| Challenges getting bottom surgery | Cost | 15 (53%) | 35 (55%) | 0.86 |
| Few surgeons | 17 (60%) | 28 (44%) | 0.15 | |
| Time off | 9 (32%) | 6 (10%) | 0.007 | |
| Recovery | 12 (43%) | 18 (30%) | 0.18 | |
| Other | 3 (10%) | 9 (14%) | 0.64 | |
| Top surgery interest | Interested | 321 (71%) | 108 (54%) | <0.0001 |
| Not interested | 128 (29%) | 92 (46%) | ||
| Top surgery barriers | Not ready | 105 (32%) | 27 (25%) | 0.13 |
| Cost | 193 (60%) | 65 (60%) | 0.99 | |
| Fear of complications | 51 (16%) | 3 (3%) | 0.0003 | |
| No surgeons | 49 (15%) | 13 (12%) | 0.41 | |
| Time off | 84 (26%) | 8 (7%) | <0.0001 | |
| Recovery | 60 (19%) | 10 (10%) | 0.02 | |
| Other | 71 (22%) | 24 (22%) | 0.98 | |
| Disinterest top surgery | I do not need it | 55 (43%) | 20 (21%) | 0.001 |
| I have breasts I want from hormones | 35 (27%) | 47 (51%) | 0.0003 | |
| Fear side effects | 16 (13%) | 10 (11%) | 0.71 | |
| Not enough info | 24 (19%) | 5 (5%) | 0.003 | |
| Want to wait | 36 (28%) | 11 (12%) | 0.003 | |
| Other | 34 (26%) | 19 (21%) | 0.31 | |
| Bottom surgery interest | Interested | 327 (59%) | 130 (70%) | 0.01 |
| Not interested | 224 (41%) | 56 (30%) | ||
| Bottom barriers | Not ready | 136 (42%) | 40 (31%) | 0.03 |
| Cost | 193 (59%) | 68 (52%) | 0.19 | |
| Fear of complications | 117 (36%) | 20 (15%) | <0.0001 | |
| Sexual function | 109 (33%) | 19 (15%) | 0.000058 | |
| No surgeons | 87 (26%) | 33 (25%) | 0.79 | |
| Time off | 69 (21%) | 15 (12%) | 0.01 | |
| Recovery | 63 (19%) | 24 (18%) | 0.84 | |
| Other | 62 (19%) | 20 (15%) | 0.37 | |
| Disinterred bottom surgery | Do not need it | 115 (51%) | 28 (50%) | 0.86 |
| Side effects | 65 (29%) | 11 (20%) | 0.16 | |
| Not enough information | 50 (22%) | 4 (7%) | 0.01 | |
| Want to wait | 41 (18%) | 10 (18%) | 0.94 | |
| Other | 52 (23%) | 19 (33%) | 0.10 | |
| Facial interest | Interested | 154 (27%) | 115 (50%) | <0.0001 |
| Not interested | 418 (73%) | 114 (50%) | ||
| Facial barriers | Not ready | 52 (33%) | 24 (21%) | 0.02 |
| Cost | 109 (70%) | 83 (72%) | 0.80 | |
| Complications | 45 (30%) | 16 (14%) | 0.003 | |
| No surgeons | 26 (17%) | 14 (12%) | 0.28 | |
| Time off | 28 (18%) | 9 (8%) | 0.01 | |
| Recovery | 25 (16%) | 10 (9%) | 0.07 | |
| Other | 21 (14%) | 16 (14%) | 0.95 | |
| Facial disinterest | Do not need it | 370 (88%) | 83 (73%) | <0.0001 |
| Side effects | 31 (7%) | 18 (16%) | 0.006 | |
| Not enough info | 52 (12%) | 5 (4%) | 0.01 | |
| Want to wait | 17 (4%) | 9 (8%) | 0.09 | |
| Other | 36 (9%) | 17 (15%) | 0.047 |
Younger respondents indicated more difficulty with cost of top surgery (p = 0.007). They also reported being more likely to be worried about complications from both bottom surgery and facial procedures than the older cohort (p < 0.0001). Younger participants were also more likely to indicate they do not need top surgery for their transition than older participants (p = 0.003) (Table 2).
Discussion
While it is known that barriers to GAS include financial, emotional and interpersonal factors, as well as lack of trained medical professionals to perform the procedures (Puckett et al., 2018), little is known about how barriers vary among the fluid spectra of gender identities. Furthermore, reasons for not undergoing specific procedures have gone largely unstudied. This is the first survey of its kind that not only looks closely at specific barriers to GAS for across gender groups, but also looks into the reasons why individuals may not be interested in pursuing them. Additionally, there is a lack of data that looks specifically at older transgender/non-binary patients. This study further analyzes interests alongside younger and older respondents.
Interest in gender affirming procedures
The 2015 U.S. Transgender Survey (USTS) queried interest in GAS (James et al., 2016). While a direct comparison is not possible between our survey and that of the USTS due to varying demographics, it is interesting to look at the differences and trends between the two. Overall, we found a higher interest in every gender affirming surgery by an average of 38%. In no gender category was interest lower for any procedure. Though the comparison is not possible, the very large increase in interest may be somewhat explained by the continued rise of transgender rights and changes in healthcare access.
The percentage of transgender men who either had or wanted top surgery (96%) was comparable to 97% in the USTS group. With bottom surgery, interest was 25% from the 2015 USTS survey and 54% interested in our 2018 survey. For non-binary AFAB respondents, interest in top surgery was 48% in the USTS group and 81% in our group. Likewise, for bottom surgery, there was nearly 50% greater interest in our survey group.
Among transgender women, interest in top surgery was also greater in our survey group, with 51% in 2015 having had or wanting breast augmentation compared to 61% in our current survey. Interest in bottom surgery was greater in our survey group (66% versus 87%), and interest in facial feminization was also greater in our survey group (50% versus 74%). In non-binary AMAB respondents, there was a greater interest for breast augmentation in our group (17% versus 30%). Interest in bottom surgery was much greater in our group (24% versus 76%), along with interest in facial feminization in our group was much greater (12% versus 50%).
A direct comparison is not possible due to the different demographic cohorts of our survey group and the USTS group. However, differences between the two are interesting to note and perhaps signify increasing interest in procedures. It may suggest that more trans/non-binary individuals are thinking strongly about surgical transition as they become more accessible and outcomes improve. The greater interest was largest among the non-binary respondents, where in the 2015 group there was a much smaller percentage of individuals interested in top, bottom, or facial surgeries. We also see that the percentage of transgender men and non-binary AFAB respondents interested in top surgery is higher than for transgender women and non-binary AMAB. This could be explained by the fact that transfeminine individuals on estrogen therapy often develop sufficiently sized breasts for the individual’s preference. However, transmasculine individuals have a lower interest in bottom surgery than the transfeminine respondents, potentially due to phalloplasty having higher morbidity and higher complications rates.
Additionally, it is worth noting the differences in interest in procedures in the different age cohorts. The older respondents indicated higher rates of already having top, bottom, and facial surgeries, but also indicated greater interest in both bottom and facial surgeries. The largest reason for the older population not wanting feminizing top surgery was because they already had the breasts they desired from hormones. It is an encouraging sign to see that a large percentage of the older population of trans/non-binary respondents have had surgery, but more effort is needed to increase early access to these procedures for psychosocial benefit. The barriers to top and bottom surgery were also significantly different between the cohorts. The younger respondents indicated of fear of complications and not having time off from work were major barriers to accessing surgery. This could be explained by the younger population working more than the older cohort, and being unable to time off from work, or perhaps having less job stability having worked for a shorter amount of time. Cost was reported as a barrier at similar percentages between the cohorts. Finally, the younger population noted at a higher percentage that they didn’t feel they needed top surgery or facial feminization for their transition. This could be explained by the notion that as transgender rights have become a more common focus and acceptance increases, the diversity in ways to be transgender has increased as well. Surgical transition is only one aspect of being transgender, and one might feel a greater sense of liberty in being accepted as transgender without top surgery than in the past.
Barriers to gender affirming procedures
It is not surprising that one of the major barriers to GAS was financial. Trans/non-binary people uniquely face employment, educational and housing discrimination, greatly impacting the ability to obtain a steady revenue. Although the majority of the respondents had private insurance (69%) a number of insurance companies do not cover gender affirming procedures (Unger, 2017). The average out-of-pocket cost for a vaginoplasty or phalloplasty alone is between 10,000–30,000and10,000–30,000 and 10,000–30,000and20,000–50,000, respectively, placing these out of reach for most whose insurance does not provide coverage (Clary, 2018). It is concurrent with previous literature that the largest barrier is cost (Puckett et al., 2018).
Another major barrier cited for all procedures was the lack of resources for recovery. This category includes emotional care, fiscal ability to take time off work, or a space to recover in. One respondent quoted, “I want surgery, but the person I would be relying on for care can’t get time off work.” It is important for surgeons to be aware of these barriers in order to be aware of cost/recovery resources nearby to aid and inform their patients as to increase access to these procedures. Another challenge to surgical transition is the emotional toll or danger of coming out to others. One person specifically mentioned “work discrimination” as a main barrier to facial procedures. Many individuals listed their family as main barriers to surgical procedures.
Fear of complications was a major barrier for bottom surgery and facial procedures but less so for top surgery. This is not surprising as major complications for vaginoplasty and phalloplasty are reported as high as 16% and 33% respectively in the literature (Ascha et al., 2018; Ives et al., 2019). Not being ready for bottom surgery was nearly as important a barrier as cost and fear of complications. Many people interested in phalloplasty mentioned that although interested in bottom surgery, they were waiting until the surgical outcomes improve. One comment from a transgender man was, “I am waiting for advancement in surgery for more realistic appearance, better healing and reduced cost.” The fear of complications for all procedures was predominately listed as barriers by the younger generation of respondents.
Importantly, across all gender categories, the distribution of barriers for bottom surgery were the most varied, indicating there are more barriers to bottom surgery than for top or facial surgeries. This illustrates the need for more resources for bottom surgery, such as improved information about the outcomes and complications of the procedures, resources for recovery and an increased number of trained professionals to carry out the procedures in more varied locations. One individual expressed, “since there is no surgeon in the area, it’s hard to say how we will face complications with travel being a factor.” Lack of access to qualified surgeons is consistently mentioned within the trans/non-binary community as being a major barrier (Puckett et al., 2018).
Lack of interest in gender affirming procedures
There is some literature indicating that transgender women often prioritize facial procedures for their transition, whereas transgender men prioritize chest reconstructive surgery (Ginsberg et al., 2016). Still, an in-depth understanding of individualized preferences for or against specific procedures has been lacking. For example, some trans/non-binary individuals are not interested in undergoing any procedures at all, while others express anxiety over whether or not they are “transgender enough” (Garrison, 2018).
For the individuals who expressed no interest in having top surgery, reasons across gender categories varied greatly. While about 25% of transgender women and AMAB non-binary respondents indicated they already had the breasts they wanted from hormones, another 25% said they did not need the surgery for transition and 25% listed other a variety of other reasons such as age.
AFAB non-binary respondents listed not needing top surgery for transition as their major reason against surgery (39%). While the overwhelming number of transgender men either had or wanted top surgery, those that did not listed individualized reasoning, one being:
“I have found that therapies for trauma, anxiety, and dysmorphia are more helpful in reconciling with my body and alleviating dysphoria than HRT was or than I believe top surgery would be.” The fact that “other” was a frequently chosen option indicates that reasons for being uninterested in top surgery is quite varied and unique.
For both bottom surgery and facial procedures, the most common reason for disinterest across all gender categories was: “I don’t think I need it for transition.” For bottom surgeries concern for side effects was a factor in 25% of respondents. Another unique reason was:
Facial surgery is not important to my identity or to relieving the dysphoria I experience.
Approximately 1 in 4 trans/non-binary people who were uninterested in gender affirming procedures reasoned that the procedures were “not needed” for affirming their gender identity. It is crucial to remember that each trans/non-binary individual is unique in their gender expression preferences and desires.
The mental health data obtained in the survey highlights the vulnerability of this population. Over half of the respondents indicated being diagnosed with anxiety and depression. 45% reported having a suicide attempt at least once in their life, which is 75 times higher than the average population (0.6%) (Substance Abuse and Mental Health Services Administration, 2017). For many trans/non-binary individuals, treatment of their gender dysphoria is intimately linked to treatment of their mental health conditions (Dhejne et al., 2016). Surgical procedures such as top, bottom, and facial feminization procedures have been shown to decrease gender dysphoria and improve body satisfaction for trans/non-binary individuals (Van de Grift et al., 2017). These procedures are medically necessary and given the strong evidence that interest for them is increasing, more effort must be made to make these therapies safe and accessible. Thus, understanding their needs for and barriers to gender affirming surgery an important step to ensure that appropriate care is made available for this population.
Limitations
Several limitations of this study warrant caution in interpretation and generalizability of our results. There was a relatively small sample size with limited distribution geographically as well as across gender groups. Additionally, the majority of the responses came from white identifying individuals. This responder bias limits the accuracy of expanding interpretations to trans/non-binary individuals of other ethnicities. There are a few issues with selection bias. Because the survey was conducted online, only participants with internet access could complete it. It is estimated that 1 in 5 trans/non-binary peoples are homeless, meaning that our study likely lacked representation of a significant portion of the population (James et al., 2016). The survey’s length of 146 questions, which may have led to some declining to participate and survey fatigue in those who did participate. We cannot be sure that those who chose not to participate or those who did not finish do not represent different populations than those who completed the survey. Some barriers such as lack of readiness are not easily defined. They were provided as choices to allow participants to have a voice to state any reason the healthcare system may have failed to give them support. While our study did not directly ask, it is important to note that one barrier to getting top and bottom surgery for trans/non-binary people is the WPATH requirements for having a certified letter from a therapist to have access to the surgery. Cost of seeing a therapist and finding a local therapist willing to write letters could be a major barrier for many. Barrier such as this could have been added in the open-ended portions of our survey sections, but we could not expect to capture all barriers. Additionally, the survey was only available to English speakers, eliminating non-English speakers from the transgender population we captured. Finally, as with any survey-based methodology, there are inherent limitations due to uncertainty in the interpretation of questions and accuracy of responses.
Conclusion
To better aid a drastically underserved population in medicine, we must fully understand the desires for and barriers to trans/non-binary people’s healthcare. While a direct comparison to the 2015 USTS is not possible, our data suggests that since 2015 interest in surgical transition has increased across all gender identities for all procedures, most dramatically for non-binary individuals. This study also demonstrated that barriers to the procedures are varied and diverse. It is not only the cost that must be mitigated to increase access, but there must be more resources for recovery on a broader societal level, meaning less stigma of taking time off work for a gender affirming procedure, as well as more research into improving outcomes for specific surgeries. It is further critical to keep in mind that transition means different things for each individual. Given that the interest to GAS varied considerably within each gender identity, is it important never to assume that any one trans/non-binary person wants or needs a particular procedure for their transition. Recognizing that not all trans/non-binary people wish to partake in all GAS is an important step toward improving healthcare for this community. With the high risk of mental illness in this population, it is especially critical that we improve our understanding of trans/non-binary patients’ needs and desires to work at improving their healthcare experiences. This article takes a step toward that aim by shedding light on the diverse array of identities, desires, and barriers to healthcare that trans/non-binary communities face.
Author contributions
(I) Conception and design: C. Agarwal, A. Simpson, K. Hoerger, A. Rivera; (II) administrative support: none; (III) provision of study materials or patients: none; (IV) collection and assembly of data: all authors; (V) data analysis and interpretation: B. Tristani-Firouzi, J. Veith, C. Agarwal; (VI) manuscript writing: B. Tristani-Firouzi, J. Veith, K. Hoerger, C. Agarwal; (VII) final approval of manuscript: all authors.
Figure 1 was designed and created by Emma Veith according to requested specifications from the authors of this manuscript.
Acknowledgments
The statistical analysis was performed in consultation with the University of Utah Biostatistics Core, which is supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding Statement
This work was supported in part by grants from the BW Bastian Foundation, Orem, UT, and the Summer Undergraduate Research Grant from Pomona College, CA.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- American Society of Plastic Surgeons . (2017). 2017 Plastic Surgery Statistics Report.
- Ascha, M., Massie, J. P., Morrison, S. D., Crane, C. N., & Chen, M. L. (2018). Outcomes of single stage phalloplasty by pedicled anterolateral thigh flap versus radial forearm free flap in gender confirming surgery. The Journal of Urology, 199(1), 206–214. 10.1016/j.juro.2017.07.084 [DOI] [PubMed] [Google Scholar]
- Cai, X., Hughto, J. M., Reisner, S. L., Pachankis, J. E., & Levy, B. R. (2019). Benefit of gender-affirming medical treatment for transgender elders: Later-life alignment of mind and body. LGBT Health, 6(1), 34–39. 10.1089/lgbt.2017.0262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canner, J. K., Harfouch, O., Kodadek, L. M., Pelaez, D., Coon, D., Offodile, A. D., 2nd, Haider, A. H., & Lau, B. D. (2018). Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surgery, 153(7), 609–616. 10.1001/jamasurg.2017.6231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clary, S. (2018). Bottom surgery: What you need to know. Healthline. https://www.healthline.com/health/transgender/bottom-surgery.
- Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., Decuypere, G., Feldman, J., Fraser, L., Green, J., Knudson, G., Meyer, W. J., Monstrey, S., Adler, R. K., Brown, G. R., Devor, A. H., Ehrbar, R., Ettner, R., Eyler, E., Garofalo, R., Karasic, D. H., Lev, A. I., … Zucker, K. (2012). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. World Professional Association for Transgender Health.
- Dhejne, C., Van Vlerken, R., Heylens, G., & Arcelus, J. (2016). Mental health and gender dysphoria: A review of the literature. International Review of Psychiatry, 28(1), 44–57. 10.3109/09540261.2015.1115753 [DOI] [PubMed] [Google Scholar]
- El-Hadi, H., Stone, J., Temple-Oberle, C., & Harrop, A. R. (2018). Gender-affirming surgery for transgender individuals: Perceived satisfaction and barriers to care. _Plastic Surgery (Oakville, Ont.)_26(4), 263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores, A. R., Herman, J. L., Gates, G. J., & Brown, T. N. T. (2016). _How many adults identify as transgender in the United States?_The Williams Institute. [Google Scholar]
- Garrison, S. (2018). On the limits of “transgender enough”: authenticating transgender identity narratives. Gender & Society, 32(5), 613–637. 10.1177/0891243218780299 [DOI] [Google Scholar]
- Ginsberg, B. A., Calderon, M., Seminara, N. M., & Day, D. (2016). A potential role for the dermatologist in the physical transformation of transgender people: A survey of attitudes and practices within the transgender community. Journal of the American Academy of Dermatology, 74(2), 303–308. 10.1016/j.jaad.2015.10.013 [DOI] [PubMed] [Google Scholar]
- Gridley, S. J., Crouch, J. M., Evans, Y., Eng, W., Antoon, E., Lyapustina, M., Schimmel-Bristow, A., Woodward, J., Dundon, K., Schaff, R., McCarty, C., Ahrens, K., & Breland, D. J. (2016). Youth and caregiver perspectives on barriers to gender-affirming health care for transgender youth. Journal of Adolescent Health, 59(3), 254–261. 10.1016/j.jadohealth.2016.03.017 [DOI] [PubMed] [Google Scholar]
- Ives, G. C., Fein, L. A., Finch, L., Sluiter, E. C., Lane, M., Kuzon, W. M., & Salgado, C. J. (2019). Evaluation of BMI as a risk factor for complications following gender-affirming penile inversion vaginoplasty. Plastic and Reconstructive Surgery Global Open, 7(3), e2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The report of the 2015 U.S. transgender survey. National Center for Transgender Equality. [Google Scholar]
- Lerner, J. E., & Robles, G. (2017). Perceived barriers and facilitators to health care utilization in the United States for transgender people: A review of recent literature. Journal of Health Care for the Poor and Underserved, 28(1), 127–152. 10.1353/hpu.2017.0014 [DOI] [PubMed] [Google Scholar]
- Linander, I., Alm, E., Goicolea, I., & Harryson, L. (2019). “It was like I had to fit into a category”: Care-seekers’ experiences of gender regulation in the Swedish trans-specific healthcare. Health, 23(1), 21–38. 10.1177/1363459317708824 [DOI] [PubMed] [Google Scholar]
- Meerwijk, E. L., & Sevelius, J. M. (2017). Transgender population size in the United States: A meta-regression of population-based probability samples. American Journal of Public Health, 107(2), e1–e8. 10.2105/AJPH.2016.303578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, L., Whallett, E. J., & McGregor, J. C. (2009). Transgender patient satisfaction following reduction mammaplasty. Journal of Plastic, Reconstructive & Aesthetic Surgery, 62(3), 331–334. 10.1016/j.bjps.2007.10.049 [DOI] [PubMed] [Google Scholar]
- Padula, W. V., & Baker, K. (2017). Coverage for gender-affirming care: Making health insurance work for transgender Americans. LGBT Health, 4(4), 244–247. 10.1089/lgbt.2016.0099 [DOI] [PubMed] [Google Scholar]
- Padula, W. V., Heru, S., & Campbell, J. D. (2016). Societal implications of health insurance coverage for medically necessary services in the U.S. transgender population: A cost-effectiveness analysis. Journal of General Internal Medicine, 31(4), 394–401. 10.1007/s11606-015-3529-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puckett, J. A., Cleary, P., Rossman, K., Newcomb, M. E., & Mustanski, B. (2018). Barriers to gender-affirming care for transgender and gender nonconforming individuals. Sexuality Research and Social Policy, 15(1), 48–59. 10.1007/s13178-017-0295-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehr, B. (2015). Comfortable in their bodies: The rise of transgender care. BMJ, 350, 3083. 10.1136/bmj.h3083 [DOI] [PubMed] [Google Scholar]
- Sanchez, N. F., Sanchez, J. P., & Danoff, A. (2009). Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. American Journal of Public Health, 99(4), 713–719. 10.2105/AJPH.2007.132035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sineath, R. C., Woodyatt, C., Sanchez, T., Giammattei, S., Gillespie, T., Hunkeler, H., Owen-Smith, A., Quinn, V. P., Roblin, D., Stephenson, R., Sullivan, P. S., Tangpricha, V., & Goodman, M. (2016). Determinants of and barriers to hormonal and surgical treatment receipt among transgender people. Transgender Health, 1(1), 129–136. 10.1089/trgh.2016.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . (2017). 2017 National Survey on Drug Use and Health annual national report. [PubMed]
- Terrier, J. E., Courtois, F., Ruffion, A., & Morel Journel, N. (2014). Surgical outcomes and patients’ satisfaction with suprapubic phalloplasty. The Journal of Sexual Medicine, 11(1), 288–298. 10.1111/jsm.12297 [DOI] [PubMed] [Google Scholar]
- Unger, C. A. (2017). Update on gender-affirming treatment for the transgender woman. Seminars in Reproductive Medicine, 35(5), 442–447. 10.1055/s-0037-1604454 [DOI] [PubMed] [Google Scholar]
- van de Grift, T. C., Elaut, E., Cerwenka, S. C., Cohen-Kettenis, P. T., De Cuypere, G., Richter-Appelt, H., & Kreukels, B. P. C. (2017). Effects of medical interventions of gender dysphoria and body image: A follow-up study. Psychosomatic Medicine, 79(7), 815–832. 10.1097/PSY.0000000000000465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Hughto, J. M., Rose, A. J., Pachankis, J. E., & Reisner, S. L. (2017). Barriers to gender transition-related healthcare: Identifying underserved transgender adults in Massachusetts. Transgender Health, 2(1), 107–118. 10.1089/trgh.2017.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]