A Mutation in the Human Immunodeficiency Virus Type 1 Gag Protein Destabilizes the Interaction of the Envelope Protein Subunits gp120 and gp41 (original) (raw)
Abstract
The Gag protein of human immunodeficiency virus type 1 (HIV-1) associates with the envelope protein complex during virus assembly. The available evidence indicates that this interaction involves recognition of the gp41 cytoplasmic tail (CT) by the matrix protein (MA) region of Pr55Gag. Here we show that substitution of Asp for Leu at position 49 (L49D) in MA results in a specific reduction in particle-associated gp120 without affecting the levels of gp41. Mutant virions were markedly reduced in single-cycle infectivity despite a relatively modest defect in fusion with target cells. Studies with HIV-1 particles containing decreased levels of envelope proteins suggested that the L49D mutation also inhibits a postentry step in infection. Truncation of the gp41 tail, or pseudotyping by vesicular stomatitis virus glycoprotein, restored both the fusion and infectivity of L49D mutant virions to wild-type levels. Truncation of gp41 also resulted in equivalent levels of gp120 on particles with and without the MA mutation and enhanced the replication of the L49D mutant virus in T cells. The impaired fusion and infectivity of L49D mutant particles were also complemented by a single point mutation in the gp41 CT that disrupted the tyrosine-containing endocytic motif. Our results suggest that an altered interaction between the MA domain of Gag and the gp41 cytoplasmic tail leads to dissociation of gp120 from gp41 during HIV-1 particle assembly, thus resulting in impaired fusion and infectivity.
Human immunodeficiency virus type 1 (HIV-1) particles assemble and bud from the plasma membrane of infected cells as immature virions that are incapable of infecting target cells (79). During HIV-1 assembly, envelope glycoproteins of HIV-1 are incorporated as a trimer of heterodimers on the surface of the viral particle (65, 70, 86). The transmembrane (TM) glycoprotein gp41, which catalyzes fusion, consists of an ectodomain found on the exterior of the virion surface, a hydrophobic transmembrane anchor, and a long cytoplasmic tail (CT) (5, 73). The gp120 protein associates with the ectodomain of gp41 through noncovalent interactions (73) and mediates attachment to cell surface receptors. Initial interactions between HIV-1 particles and target cells occur between gp120 and CD4 (68). CD4 binding elicits a conformational change within gp120 that reveals a binding site for the viral coreceptor, typically the chemokine receptor CCR5 or CXCR4 (13, 19). Subsequent engagement of coreceptor initiates further conformational changes in gp41 that lead to membrane fusion (33).
Unlike simple retroviruses, lentiviruses characteristically encode transmembrane glycoproteins with cytoplasmic tails greater than 100 amino acids in length. Simian immunodeficiency virus (SIV) and HIV-2 are tolerant of CT truncation in vitro (31, 50, 87), but passage of CT-truncated SIV in macaques quickly selects for wild-type virus (42). Additionally, the CT is highly conserved in HIV-1, suggesting that this domain is functionally relevant. The 150-amino-acid CT of HIV-1 gp41 appears to be crucial for viral entry in many cell types (11, 16, 59) and for an early postentry step in infection in a cell-type-specific manner (26). The CT is not required for fusion as measured in cell-to-cell fusion assays, nor is it required for HIV-1 replication in selected cell types, including HeLa and MT-4 cells (32, 44, 53). However, in primary T cells and many other transformed T-cell lines, the gp41 CT is required for efficient Env incorporation during HIV-1 particle assembly (4, 53).
Following release, particles undergo proteolytic cleavage of the internal Gag and Gag-Pol polyproteins, resulting in structural morphogenesis termed maturation (77). The matrix (MA) protein is released upon processing of the amino-terminal segment of Pr55Gag (Gag) during an early step of HIV-1 maturation. MA performs diverse roles in the virus life cycle. During HIV-1 assembly, Gag associates with cellular membranes via its amino-terminal myristic acid and basic residues in the MA domain (28). MA is also important for the incorporation of the viral envelope glycoproteins (Env) gp41 and gp120 into nascent particles, as shown by the identification of HIV-1 MA mutants exhibiting low levels of particle-associated Env (7, 15, 23, 24, 52, 53, 55, 83, 84). During maturation, a fraction of MA localizes to the viral core (39, 75), where it may participate in early postentry events in infection, including uncoating (82), reverse transcription (7, 35, 36, 61, 62), and possibly nuclear import (6, 29, 66, 72), although the latter conclusion has been disputed (21, 22, 38).
Three lines of evidence indicate that the MA region of Gag interacts with gp41 during HIV-1 assembly. First, MA mutations that impair envelope incorporation can be rescued by subsequent truncation of the CT (23, 44), and deletions and mutations in the CT can be complemented by compensatory changes in MA (52, 76). Second, expression of Env targets the budding of HIV-1 particles to the basolateral surfaces of polarized epithelial cells; this activity depends on the gp41 CT and is blocked by mutations in MA (41, 57). Third, biochemical studies have demonstrated that gp41 is tightly associated with immature HIV-1 particles via the CT (80). Immature virions fuse poorly with target cells, but truncation of the CT relieves the fusion impairment, probably by releasing gp41 from Gag in the immature viral core (51, 80). Thus, binding of Gag to the gp41 CT appears to inhibit the function of the viral envelope proteins on immature HIV-1 particles.
Here we report a detailed analysis of an HIV-1 mutant containing a substitution of Asp for Leu at position 49 (L49D) in MA, which was previously shown by Freed and coworkers to be impaired for replication (25). We show that L49D mutant virions assemble efficiently, but are markedly impaired in infectivity. Quantitative assays of fusion and virion protein composition revealed a modest decrease in fusion capacity and a specific reduction of gp120 associated with the mutant particles. Truncation of the gp41 CT, or pseudotyping by vesicular stomatitis virus glycoprotein (VSV-G), restored both the fusion efficiency and infectivity of the L49D mutant particles to wild-type levels. Remarkably, mutation of the tyrosine-based endocytic motif in the gp41 CT also relieved the L49D mutant fusion and infectivity impairments. We conclude that the L49D substitution in MA results in reduced HIV-1 fusion capacity by destabilizing the association of gp120 with gp41 during particle assembly.
MATERIALS AND METHODS
Cell lines.
293T, P4R5, and Z-24/Rec-1 cells were cultured at 37°C and 5% CO2 in Dulbecco's modified Eagle's medium (Cellgro) supplemented with 10% fetal bovine serum, penicillin, and streptomycin. Z-24/Rec-1 cells are CD4-negative HeLa/long terminal repeat (LTR)-lacZ reporter cells expressing the ecotropic murine leukemia virus (MLV) receptor (85). MT-4 cells were cultured at 37°C and 5% CO2 in RPMI 1640 (Cellgro) medium supplemented with 10% fetal bovine serum and antibiotics (Cellgro).
Plasmid constructs.
Wild-type HIV-1 was generated from the pNL4-3 clone that carries full-length open reading frames for all HIV-1 genes (1). pNL4-3.L49D and pNL-CTdel144-2 were previously described (24, 25). All mutants were created in the pNL4-3 viral background. (Since the amino-terminal methionine is removed prior to Gag myristoylation, the L49D MA mutation corresponds to codon 50 in the Gag sequence.) pNL4-3ΔE and pNL4-3.L49DΔE were constructed by replacing the 2.6-kbp SalI-BamHI fragment with the corresponding fragment from R9ΔE (2). pNL4-3.L49D-CT144 was created by transfer of the SalI-BamHI fragment from pNL4-3.CTdel144-2 (24), containing a stop codon at bp 8341 of Env. Mutations created in the gp41 CT domain were named according to their location based on the initial methionine in the pNL4-3 sequence. The Y710S mutation was created by PCR mutagenesis segment overlap extension using sense primer 5′-AGGCAGGGCTCCTCACCATTATCG-3′ and antisense primer 5′-AGTATCCGTATCCAGAGGG-3′. These primers introduced a BamII restriction enzyme site into the proviral sequence. The Y710S mutation was introduced into the L49D proviral plasmid by transfer of the SalI-BamHI fragment into pNL4-3.L49DΔE. Mutant clones were verified by restriction digestion or DNA sequencing as appropriate. Plasmids pHCMV-G (81) (encoding the glycoprotein of vesicular stomatitis virus) and pCEET (60) (encoding a CT-truncated ecotropic murine leukemia virus Env protein) were generous gifts from Jane Burns and Jack Ragheb, respectively.
Virus production.
HIV-1 stocks were produced by calcium phosphate transfection of subconfluent 293T cells by a standard protocol (10). VSV-G-pseudotyped viruses were created by transfecting subconfluent 293T cell monolayers with pHCMV-G (2 μg) and proviral DNA (20 μg), as previously described (2). Virus was harvested 48 h later; supernatants were clarified and filtered through a 0.45-μm syringe filter to removal cellular debris and frozen in aliquots at −80°C. Viral yields were quantified by a p24 antigen capture enzyme-linked immunosorbent assay (ELISA) (74).
For MLV envelope titrations, 293T cells were transfected with equal levels of proviral DNA (4 μg) and various amounts of MLV ecotropic envelope containing a truncated envelope glycoprotein (pCEET; 6 μg, 4 μg, and 2 μg). Virus particles were harvested, clarified, and filtered through a 0.45-μm filter. Dilutions of virus were then tested for single-cycle infectivity as described below using Z-24/Rec-1 reporter cells that express the MLV receptor but lack CD4.
Single-cycle infection assay.
P4R5 cells, a HeLa-CD4/LTR-_lac_Z indicator cell line expressing both CXCR4 and CCR5, were employed to assess viral infectivity (3, 9). To determine virus titers, cells were plated in 48-well plates at a density of 20,000 cells/well. Ten-fold serial virus dilutions, supplemented with DEAE-dextran (20 μg/ml), were applied to wells in triplicate. Cells were fed with complete medium (0.5 ml) 24 h after infection. Forty-eight hours after infection, cells were fixed with a solution containing paraformaldehyde (1%) and glutaraldehyde (0.2%) and stained with 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside (X-Gal), as previously described (37). Images were captured using a charge-coupled device camera equipped with a macro lens and quantified using NIH Image software. The infectious titer units were normalized for virus concentration by normalizing for CA by p24 ELISA.
Virus-cell fusion assay.
Quantitative HIV-1 fusion assays were performed as described previously (8, 79). Briefly, P4R5 cells were plated at 20,000 cells/well using black 96-well plates with clear bottoms (Packard). HIV-1 particles containing a β-lactamase-Vpr (BlaM-Vpr) reporter protein were produced by transient transfection of 293T cells with the expression construct pMM310 (obtained from Mike Miller, Merck Research Laboratories). Viruses were diluted serially into complete medium supplemented with 10 mM HEPES (pH 7.3) and 20 μg/ml DEAE-dextran. Dilutions of viruses (100 μl volumes) were applied to the cells and incubated at 37°C in 5% CO2 for 2 h. The BlaM substrate CCF2-AM (20 μM; Panvera) was prepared per the manufacturer's “enhanced loading protocol” and applied to the cells (88). Cells were incubated overnight at room temperature in the dark. Prior to reading fluorescence, the CCF2-AM was removed and phosphate-buffered saline (PBS) was added to each well. Fluorescence was quantified at 450 nm (blue) and 520 nm (green) using excitation at 410 nm in a microplate fluorometer (BMG FluoStar). Fluorescence ratios were determined after subtracting blue fluorescence of wells containing cells but no virus and green fluorescence of wells containing neither cells nor virus. Triplicate determinations were performed for each virus dilution, and the values typically agreed to within 10%.
Immunoblot analysis.
Immunoblot analysis of viral proteins was performed as previously described (80). Briefly, virus produced by transient transfection of 293T cells was pelleted by ultracentrifugation (100,000 × g, 30 min in a Beckman TLA-55 rotor). Equivalent quantities of viral lysates, as determined by p24 ELISA, were subjected to electrophoresis on 4% to 20% Tris-HCl gradient gels (Bio-Rad) followed by transfer of protein to a nitrocellulose membrane (0.45-μm pore size; Perkin-Elmer). Blots were probed with HIV-1-specific antibodies for p24/CA (from D. Trono), p17/MA (from P. Spearman), gp41/TM (NIH AIDS Research and Reference Reagents Program, catalog no. 526 and 1475), gp120/SU (NIH AIDS Research and Reference Reagents Program, catalog no. 522), polyclonal antisera to VSV envelope (Lee Biomedical Research Laboratories), and polyclonal goat antiserum to MLV Env (ViroMed Safety Laboratories, Camden, NJ). β-Lactamase was detected using a monoclonal antibody (QED Biosciences, Inc.) (79). Following incubation with the appropriate species-specific AlexaFluor 680- or IRDye 800-conjugated secondary antibody, protein bands were visualized using the Odyssey Infrared Imaging system (LI-COR) and quantified using the instrument software. Quantification of individual band intensities was determined as kilocounts, where 1 kilocount = 1,000 pixels/mm3.
Quantitative ELISA for gp120.
gp120 levels on virions were determined by ELISA as previously described (43). Briefly, Immulon flat-bottom 96-well plates (Dynex) were coated with gp120-specific sheep polyclonal antibody (4 μg/ml; Cliniqa Inc.) for at least 6 h. Individual wells were blocked with 5% donor calf serum in PBS for 1 h, following washes. Dilutions of purified gp120 protein (IIIB; NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH) were used to construct a standard curve. Dilutions of virus lysates and standards were applied and incubated for 2 h at 37°C. A gp120-specific human monoclonal antibody (NIH AIDS Research and Reference Reagents Program, catalog no. 1476) was applied for 1 h at 37°C followed by addition of horseradish peroxidase-conjugated antihuman antibody (0.2 μg/ml; Pierce). Signals were quantified by spectrophotometry following the application of 3,3′,5,5′-tetramethylbenzidine (TMB) substrate (Kirkegaard & Perry Laboratories).
Assays of gp120 shedding.
Provirus-transfected 293T cells were washed with sterile PBS and fed with complete medium 16 h following transfection. Cells were cultured for an additional hour at 37°C. Virus-containing culture supernatants were harvested and clarified by filtration through a 0.45-μm filter. Virus samples were subsequently incubated at 37°C for various times (1, 2, 4, and 8 h). At each time point, a sample of each virus was collected and frozen at −80°C. The virus stocks were later thawed together and tested for single-cycle infectivity using P4 target cells. Virus samples were also pelleted by ultracentrifugation for 30 min through a cushion STE buffer (10 mM Tris-Cl [pH 7.4], 100 mM NaCl, 1 mM EDTA [39]) containing 20% sucrose in a Beckman TLA-55 rotor (45,000 rpm at 4°C). Virus pellets were dissolved with 1/10 original volume of p24 sample diluent (PBS, 0.2% Tween 20) and assayed for gp120 and p24 by ELISA. The relative levels of particle-associated gp120 were calculated as the ratio of the gp120 and p24 concentrations in each virus pellet.
HIV-1 replication assay.
Viruses derived from 293T cells (1 ng p24) were used to inoculate duplicate parallel cultures of MT-4 cells seeded at 300,000 cells/well. Samples of culture supernatants (300 μl) were collected every 1 to 2 days, and the original culture volumes were restored with fresh medium. Cultures were split 1:2 when necessary to prevent senescence due to overgrowth. HIV-1 particle production in culture supernatants was quantified by p24 ELISA.
RESULTS
L49D mutant particles assemble but are poorly infectious.
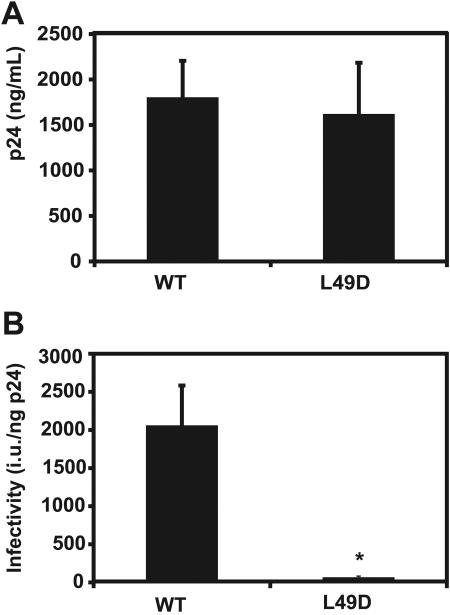
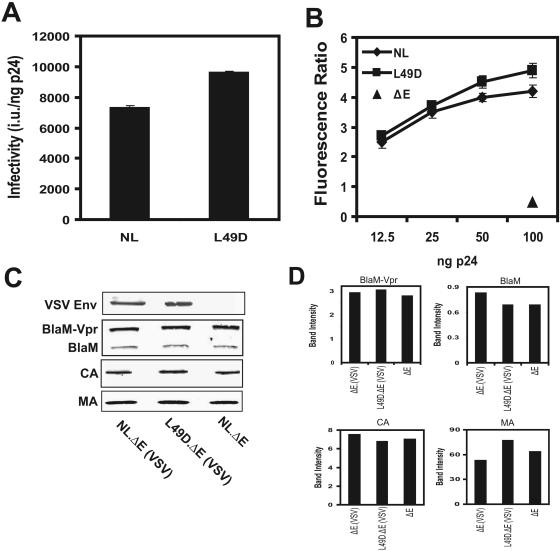
A previous study reported the initial characterization of a series of HIV-1 mutants containing engineered substitutions in MA (25). One of these mutants, L49D, was impaired for replication in T cells but was competent for viral assembly and release. To confirm and extend previous findings regarding this mutant, we quantified the levels of wild-type and mutant HIV-1 particles produced by transient transfection of 293T cells. L49D particles were released in quantities comparable to wild type (Fig. 1A). We sought to determine whether the L49D mutant was impaired for infection in a single-round reporter assay. The single-cycle assay requires completion of steps in the virus life cycle up to and including Tat expression and is therefore a useful tool to probe blocks during the early viral life cycle. Quantitation of virus infectivity using the P4R5 cell line (HeLa-CD4/LTR-_lacZ_-CCR5) revealed a 40-fold reduction in L49D particle infectivity relative to wild type (Fig. 1B). Because the single-cycle infection assay depends on expression of Tat from an integrated provirus, these results suggest that the mutant virus is impaired at a step in HIV-1 infection prior to integration.
FIG. 1.
L49D virus particles exhibit efficient assembly but are poorly infectious. (A) Transient transfection of 293T cells with proviral DNAs resulted in comparable levels of particle production for wild-type (WT; NL4-3) and MA mutant (L49D) particles. Particle yield was determined by p24 ELISA. The data represent the average of at least three independent transfections, with error bars corresponding to 1 standard deviation. (B) Single-cycle infectivity was assayed in P4R5 target cells which contain the lacZ gene under transcriptional control of the HIV-1 promoter. Cells were inoculated with 293T-derived viruses, and infected cells were identified microscopically after staining with X-Gal. Infectivity is presented as infectious units (i.u.)/ng of p24. This figure represents the average of at least three independent assays. *, P < 0.001 from two-tailed Student's t test.
L49D mutant particles are moderately impaired for fusion with target cells.
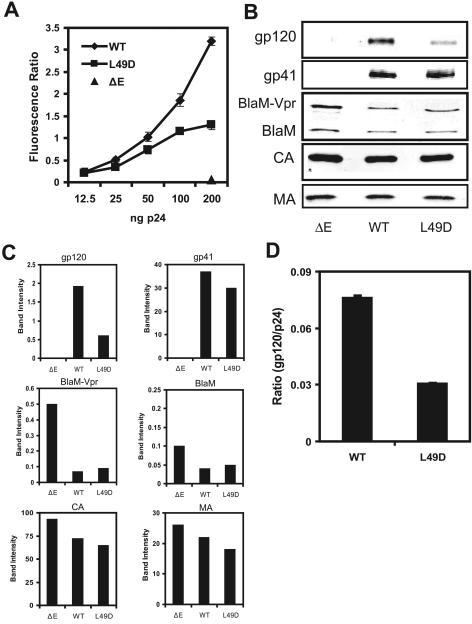
To determine whether the reduced infectivity of L49D particles is a consequence of impaired cell entry, we quantified the fusion capacity of wild-type and L49D particles using a specific assay of HIV-1 virus-cell fusion (8). This assay utilizes β-lactamase (BlaM) packaged into viral particles as a fusion with Vpr. P4R5 target cells were inoculated with HIV-1 particles containing BlaM; cells were subsequently loaded with CCF2-AM, a cell-permeable fluorescent substrate for BlaM. The emission spectrum of CCF2 shifts from green to blue upon cleavage by BlaM, the extent of which is subsequently quantified by spectrofluorimetry. We have previously shown that a positive signal in this assay requires fusion-competent virus and functional receptors on cells (79). Furthermore, the signal is inhibited by coreceptor antagonists and the HIV-1 inhibitor T-20 (8, 79). Thus, signals obtained with this assay are dependent on virus-cell interactions that result in fusion. Inoculation with wild type HIV-1 reporter particles produced a dose-dependent increase of the blue/green fluorescent ratio (Fig. 2A). The L49D mutant also exhibited a linear dose response of fusion; however, the fusion was approximately one-half that of the wild type over a range of virus dilutions (Fig. 2A). Similar results were observed when SupT1 and MT-4 cells were used as targets (data not shown). Mutant HIV-1 particles lacking envelope glycoproteins exhibited only background signals (Fig. 2A). These results indicated that the MA mutation moderately reduced the efficiency of HIV-1 fusion with target cells.
FIG. 2.
L49D mutant HIV-1 particles are moderately impaired for fusion. (A) HIV-1 particles were tested for fusion with P4R5 cells. Ratios represent the average of triplicate wells ± standard deviation and are representative of at least three independent assays. WT, wild type; ΔE, Env defective. (B) Virus particles were pelleted through 20% sucrose and analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis. Following protein transfer to nitrocellulose, immunoblots were probed for p24/CA, gp41/TM, gp120/SU, p17/MA, and β-lactamase. (C) Band intensities were quantified by LI-COR Odyssey software. (D) ELISA quantitation of gp120 on virus particles. Viruses were pelleted and then dissolved in lysis buffer, and gp120 and p24 were quantified by ELISA. Shown is the mean ratio of gp120 to p24 from three independent assays, with error bars representing 1 standard deviation.
L49D particles exhibit a reduction in the level of gp120 but not gp41.
Mutations within the MA protein can impair HIV-1 envelope incorporation (15, 23, 83). Thus, the reduced fusion capacity of the L49D virions could result from impaired Env glycoprotein incorporation. We therefore analyzed Env levels on mutant and wild-type HIV-1 particles by immunoblotting and quantification with the LI-COR Odyssey imaging system. The signals obtained using this system are linear over a wide range of band intensities. Samples were normalized for CA levels by p24 ELISA prior to sodium dodecyl sulfate-polyacrylamide gel electrophoresis. The results revealed that wild-type and mutant particles contained similar levels of gp41, suggesting that the L49D mutation did not inhibit overall envelope incorporation (Fig. 2B and C). We also considered the possibility that the reduced fusion of L49D particles might be an artifact of reduced levels of BlaM-Vpr incorporation. Therefore, we concurrently tested particles used in the fusion assay by immunoblotting for the presence of β-lactamase, which is released from the BlaM-Vpr fusion protein upon cleavage by the viral protease (PR) during particle maturation (79). The wild-type and mutant particles contained equivalent levels of cleaved and uncleaved BlaM-Vpr, as well as MA (Fig. 2B and C). Control HIV-1 particles lacking Env contained slightly higher levels of reporter protein, yet exhibited minimal signals in the fusion assay (Fig. 2B and C). We conclude that L49D particles efficiently incorporate gp41 during their assembly.
The presence of gp41 on L49D mutant particles demonstrated that they were able to incorporate envelope during viral assembly. However, altered interactions between gp41 and MA could affect the structure of the gp41 ectodomain, potentially modulating the noncovalent association of gp120 and gp41 on the viral surface. To test this, we quantified gp120 levels on virus particles by immunoblotting. While the mutant particles efficiently incorporated gp41 during assembly, the level of gp120 on the virion surface was significantly reduced (Fig. 2B and C). The reduction in gp120 was consistently observed in multiple experiments, although its magnitude varied somewhat between experiments. To further confirm that gp120 levels were reduced on L49D particles, we quantified gp120 and p24 levels on pelleted virions by ELISA. Mutant particles retained only 40% as much gp120 as wild-type HIV-1, after being normalized by p24 core antigen (Fig. 2D). We conclude that L49D mutant particles exhibit a specific deficit in the gp120 subunit of Env.
The impaired infectivity of L49D particles is likely due to defects in both entry and postentry steps.
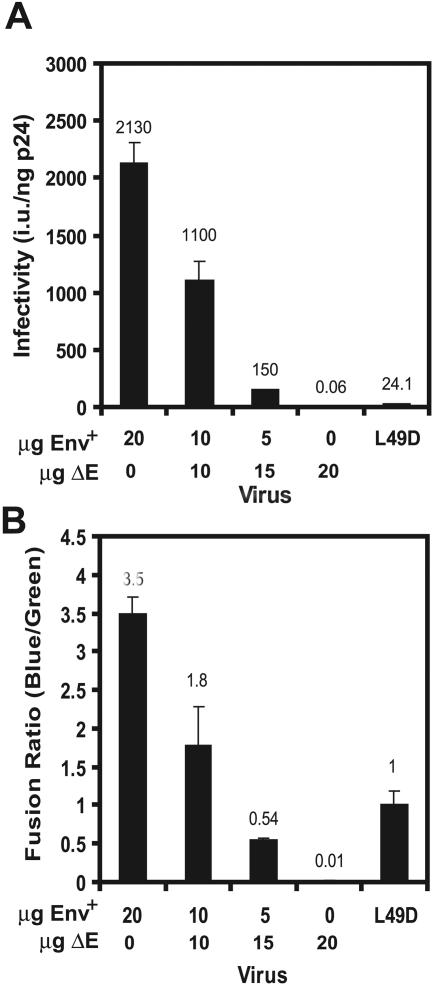
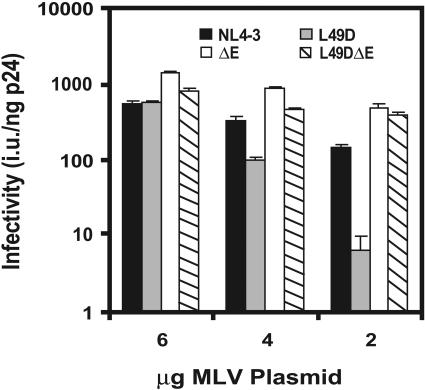
L49D mutant particles are strongly impaired in infectivity despite a modest reduction in virus-cell fusion. This apparent discrepancy suggested the possibility that the L49D mutant particles could also be impaired for early postentry steps in infection. Alternatively, viral infectivity might not exhibit a linear correspondence to virus-cell fusion. To determine if the observed reduction in fusion fully accounts for the 40-fold decrease in infectivity of the L49D particles, we compared mutant particles to virus containing various levels of HIV-1 envelope in single-cycle infectivity and virus-cell fusion assays (Fig. 3A and B). To this end, we produced wild-type HIV-1 fusion reporter particles containing decreasing quantities of Env by cotransfection of pNL4-3 and pNL4-3ΔE plasmids at various ratios, together with a fixed quantity of the BlaM-Vpr expression vector. We then compared the fusion and infectivity of the resulting viruses (Fig. 3). Immunoblot analysis of viral lysates revealed similar levels of BlaM protein (data not shown). In this experiment, the infectivity of L49D particles was decreased by nearly 100-fold relative to normal wild-type particles (Fig. 3A). Cotransfection of wild-type and Env-defective proviruses at a 1:1 ratio resulted in particles that were approximately one-half as infectious as the wild-type control (Fig. 3A); these particles also exhibited approximately 50% of wild-type fusion activity (Fig. 3B). Cotransfection of wild-type and Env-defective proviruses at a 1:3 ratio resulted in particles that were 7% as infectious as the wild type and exhibited 15% of wild-type fusion activity. Although these particles were less active for fusion than the L49D mutant particles, they were six times as infectious. These results suggest that the 50% reduction in fusion observed for the L49D mutant does not fully account for the strong infectivity impairment exhibited by this virus. Therefore, it is likely that a second, postentry impairment exists for this mutant.
FIG. 3.
Envelope titration reveals a second block to L49D infectivity. (A) Infectivity assays. 293T cells were transfected with various ratios of wild-type and Env-defective (ΔE) proviruses with a fixed quantity of the BlaM-Vpr reporter construct. The resulting particles were then assayed for infectivity. Shown are the mean values for triplicate determinations, with error bars representing 1 standard deviation. i.u., infectious units. (B) Assays of virus-cell fusion. Shown are the fusion signals resulting from 100-ng p24 inocula. The data shown are the mean values from triplicate determinations. Results are representative of three independent experiments.
The L49D infectivity and fusion impairments are relieved by truncating the gp41 cytoplasmic tail.
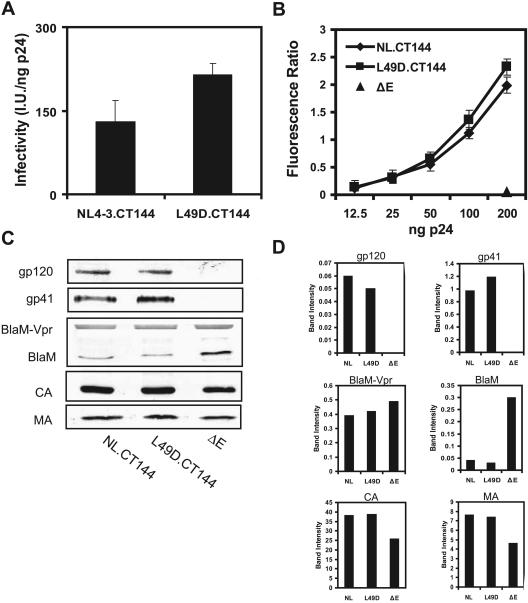
The altered gp120/gp41 ratio exhibited by the L49D mutant virions suggested that the L49D MA mutation results in altered interaction of Gag and/or MA with the gp41 CT, resulting in impaired infectivity. One prediction of this model is that truncation of the gp41 CT might suppress the L49D fusion and infectivity defects. To test this hypothesis, we determined the infectivity of L49D mutant and control particles lacking the gp41 CT (CT144) in single-cycle infection assays. The results revealed that infectivity of the MA mutant was slightly elevated over control particles lacking the mutation (Fig. 4A). This result indicated that removal of the gp41 CT relieved the infectivity impairment resulting from the L49D MA mutation.
FIG. 4.
Truncation of the gp41 CT complements the L49D mutant. (A) Single-cycle infectivity of mutant virus particles lacking the gp41 cytoplasmic tail. Shown are the mean values of three independent experiments, with error bars representing 1 standard deviation. I.U., infectious units. (B) Assays of virus-cell fusion. Shown are the mean values of quadruplicate assays, with error bars representing 1 standard deviation. ΔE, Env defective. (C) Immunoblots of pelleted virus particles for CA, gp41, gp120, MA, and BlaM. (D) Quantification of the protein signals from the immunoblots shown in panel C using the LI-COR Odyssey imaging system and software.
The restored infectivity of L49D mutant particles resulting from the gp41 CT truncation suggested that the ability of these particles to fuse with cells would be similar to that of control particles lacking the L49D mutation. BlaM reporter fusion assays revealed that NL.CT144 and L49D.CT144 reporter particles exhibited equivalent fusion signals with P4R5 cells (Fig. 4B). In SupT1 cells, truncation of CT actually resulted in a twofold enhancement of the L49D mutant particles relative to the control NL.CT144 virus (data not shown). Quantitative immunoblotting of the CT144 particles demonstrated that similar levels of both gp120 and the truncated gp41 envelope protein were incorporated into wild-type and L49D particles (Fig. 4C and D). The enhanced fusion exhibited by L49D.CT144 particles was not due to elevated incorporation of the BlaM-Vpr reporter protein, as shown by quantitation of β-lactamase band intensities (Fig. 4C and D). These results indicated that the reduced fusion capacity and infectivity of L49D mutant particles are both dependent on the gp41 cytoplasmic tail.
Fusion and infectivity of L49D mutant particles are restored upon pseudotyping with VSV-G.
Previous studies have shown that pseudotyping HIV-1 particles with the VSV-G can relieve defects at both entry and postentry steps in HIV-1 infection (2, 79). VSV-G targets HIV-1 entry to an endocytic pathway and enhances HIV-1 fusion and infectivity (2). HIV-1 MA mutants presumed to be blocked for early postentry events have also been rescued by pseudotyping (7, 35, 36). To determine whether pseudotyping by VSV-G would restore normal infectivity to L49D mutant particles, we titrated pseudotyped particles on P4R5 indicator cells. HIV-1 infectivity was enhanced by VSV-G pseudotyping by approximately sevenfold, as previously reported (2). Pseudotyping by VSV-G resulted in equivalent infectivity of wild-type and L49D particles (Fig. 5A).
FIG. 5.
Pseudotyping by VSV-G suppresses the phenotype of the HIV-1 L49D mutation. (A) Infectivity of pseudotyped HIV-1 particles. Shown are mean values from triplicate determinations, with error bars representing 1 standard deviation. i.u., infectious units. (B) Assays of virus fusion with P4R5 cells. Shown are mean values of triplicate determinations, with error bars representing one standard deviation. Results are representative of at least three independent experiments. ΔE, Env defective. (C) Immunoblots of pelleted virus particles for VSV-G, BlaM, CA, and MA. (D) Quantification of the bands shown in panel C using the Odyssey imaging system.
To determine if VSV-G pseudotyping would also suppress the L49D fusion impairment, we tested VSV-pseudotyped particles for virus-cell fusion efficiency. Pseudotyped viruses containing BlaM-Vpr were produced by transfection of 293T cells and titrated onto P4R5 cells. As expected, levels of fusion were higher when pseudotyped particles were employed, although Env-deficient particles lacking VSV-G remained at background levels (compare Fig. 5B and Fig. 2A). The fusion of wild-type and L49D mutant particles containing VSV-G was equivalent at all dilutions tested (Fig. 5B). Immunoblot analysis of viral lysates demonstrated that pseudotyped L49D and control virions contained similar quantities of VSV-G and BlaM (Fig. 5C and D). Collectively, these results demonstrate that pseudotyping by VSV-G overcomes the fusion and infectivity defects resulting from the L49D mutation and further support the conclusion that impaired fusion exhibited by L49D mutant virions is dependent on the gp41 CT.
The HIV-1 Env protein exerts a dominant inhibitory effect on the infectivity of particles containing the L49D mutation.
The discordance between the fusion and infectivity impairments exhibited by L49D mutant particles suggested that this mutation results in an additional postentry defect. Truncation of the gp41 CT appears to suppress both impairments, indicating that the putative postentry defect may also depend on the CT. Based on these observations, we hypothesized that the L49D mutation results in an altered interaction of MA with the gp41 CT. One prediction of this hypothesis is that the gp41 CT would inhibit the infectivity of L49D mutant particles even when entry is mediated by a heterologous Env protein that rescues the infectivity defect. To test this hypothesis, we generated HIV-1 particles containing the wild-type HIV-1 Env as well as an ecotropic murine leukemia virus Env protein and determined the infectivity of the resulting particles on reporter target cells lacking CD4 but expressing the receptor for ecotropic MLV. The MLV Env TM protein is normally activated by cleavage of the CT by the viral protease; therefore, we employed an MLV Env lacking the cytoplasmic tail to avoid complications that might result from the requirement for cleavage of the CT. Virus particles were produced by transfection of wild-type and L49D mutant proviral clones with various quantities of the MLV Env expression plasmid. The resulting particles were assayed for p24 concentrations and titrated onto CD4-negative reporter target cells expressing Rec-1, the receptor for ecotropic MLV. At the highest dose of the MLV Env expression plasmid (6 mg), the wild-type and L49D mutant particles infected the target cells with similar efficiencies (Fig. 6). However, as the quantity of MLV Env was reduced, the ecotropic MLV-pseudotyped L49D mutant particles became less infectious than the control virions. When the cotransfections were performed with 2 μg of MLV Env plasmid, the L49D mutant virions were less than 10% as infectious as the corresponding wild-type particles (Fig. 6). In contrast, when the experiment was performed with particles lacking the HIV-1 Env proteins, the pseudotyped control and L49D mutant particles were of similar infectivity, irrespective of the quantity of the MLV Env plasmid used in the transfection (Fig. 6). Analysis of the viral particles by immunoblotting demonstrated that the decreased infectivity of the L49D particles containing both HIV-1 and MLV Env proteins was not due to impaired incorporation of the MLV Env protein (data not shown). These results therefore suggest that the HIV-1 Env protein exerts a dominant inhibitory effect on the infectivity of the L49D mutant particles even when entry into target cells is mediated by an Env protein that rescues the infectivity impairment. This observation also provides further evidence for a postentry impairment in infection by the L49D mutant that is dependent on the gp41 CT.
FIG. 6.
HIV-1 Env protein inhibits the infectivity of L49D mutant particles when cell entry is mediated through a heterologous viral Env protein. Dual-enveloped wild-type and L49D mutant particles were generated by cotransfection of cells with Env+ or Env-defective (ΔE) proviral clones with the indicated quantities of plasmid pCEET encoding a CT-truncated ecotropic MLV Env protein. Virus particles were collected and assayed for infection on CD4-negative reporter cells expressing the ecotropic MLV receptor. Shown are the mean infectivity values of triplicate infections, with error bars representing 1 standard deviation. Results are representative of two independent experiments. i.u., infectious units.
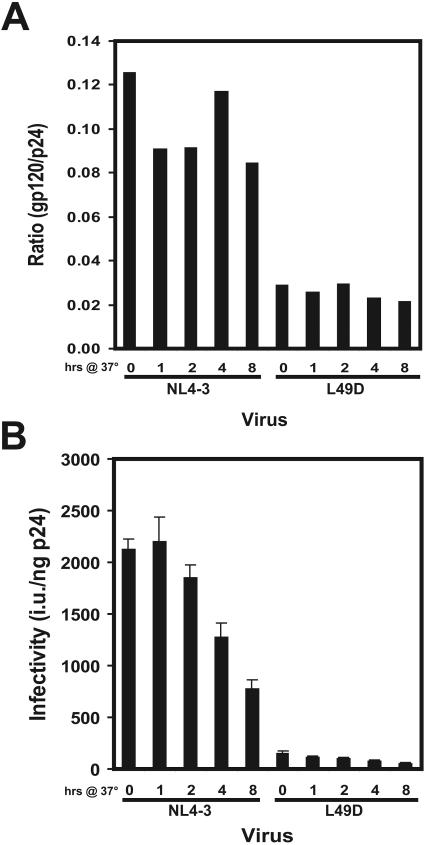
L49D particles do not exhibit accelerated gp120 shedding.
The specific deficit in gp120 on L49D mutant particles could be due to enhanced shedding of gp120 from particles. Alternatively, an alteration between Gag and Env may lead to dissociation of gp120 at a stage of assembly prior to particle release. To distinguish between these two hypotheses, we quantified the loss of gp120 from fresh virus particles during an 8-h incubation at 37°C. To generate the virus stocks for this assay, provirus-transfected 293T cells were washed and cultured with fresh medium for 1 h. Virus-containing supernatants were harvested and then incubated at 37°C for up to 8 h, after which the particles were pelleted, lysed, and assayed for gp120 and CA by ELISA. Freshly harvested wild-type particles exhibited a gp120/p24 ratio that was approximately three to four times greater than that of L49D virions (Fig. 7A), a result that is in rough agreement with the levels observed for viruses released during the 36- to 48-h culture periods (Fig. 2B to D). Particle-associated gp120 levels declined by approximately 25% during the 8-h incubation, indicating that the particles were not rapidly shedding gp120 (Fig. 7B). This apparent stability of the gp120/gp41 complex on the surface of HIV-1 particles is also consistent with a previous report that gp120 levels are relatively stable on the surface of HIV-1 particles (12). The gp120/p24 ratio of L49D particles was also fairly constant during the incubation period, indicating that the mutant particles did not exhibit accelerated gp120 shedding (Fig. 7B). The infectivities of wild-type and L49D particles both declined by approximately two-thirds during the 8-h incubation (Fig. 7B); thus the stability of the mutant particles was similar to that of the wild type under these conditions. Collectively, these results argue against an effect of the L49D mutant on gp120 shedding from viral particles and suggest that a significant fraction of the Env protein on L49D mutant particles is incorporated without gp120.
FIG. 7.
Assays of gp120 shedding and loss of infectivity during incubation of freshly-harvested HIV-1 particles. (A) Viruses were harvested from transfected 293T cells following a 1-h culture period and were then incubated at 37°C for the indicated time periods. Virus stocks were assayed for particle-associated gp120 and p24 by ELISA. Shown is the ratio of gp120 to p24 for each virus sample. (B) Infectivity of incubated HIV-1 particles. Virus stocks were assayed for infectivity with P4R5 cells. Shown are the mean values from triplicate determinations. The results in this figure are representative of two independent experiments, the results of which agreed well. i.u., infectious units.
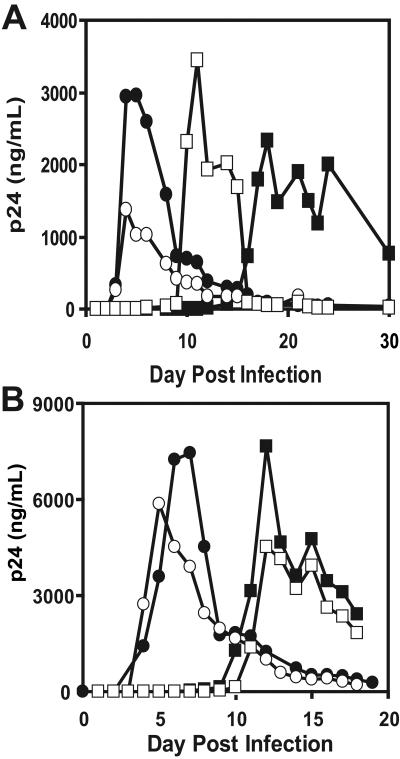
Replication of HIV-1 particles containing the L49D mutant is enhanced by truncation of the gp41 CT.
A previous study reported that replication of the L49D mutant was delayed by 2 weeks relative to wild-type HIV-1 in the human T-cell line CEM (25). Because the infectivity of the L49D.CT144 mutant particles was similar to that of the NL.CT144 control virus, we asked whether truncation of the gp41 CT would enhance the ability of L49D mutant particles to replicate in T cells. For this purpose, we chose MT-4 cells, a T-cell line that is permissive for replication of HIV-1 with CT deleted (63). A small quantity of each virus (1 ng p24) was used to inoculate independent cultures, and HIV-1 replication was monitored by quantifying p24 antigen accumulation in the culture supernatants. Replication of wild-type HIV-1 was apparent by day 3, with the peak occurring at 5 days postinfection (Fig. 8A). The L49D MA mutant emerged at day 15 and peaked at day 18 with a level of p24 comparable to that of the wild type (Fig. 8A). To determine whether truncation of the gp41 CT enhanced replication of the L49D mutant particles, we tested the replication of viruses lacking the gp41 CT. Control HIV-1 particles lacking the CT replicated with kinetics similar to those of the wild type (Fig. 8A). In contrast, L49D.CT144 replication was accelerated relative to L49D mutant particles, exhibiting a peak of p24 at day 11 with a yield comparable to that of the wild type (Fig. 8A). Assays of two independent cultures agreed well, thus confirming the reproducibility of the replication assays (data not shown).
FIG. 8.
Truncation of the gp41 CT enhances the replication of L49D mutant particles. (A) MT-4 cells were inoculated at low multiplicity with the indicated HIV-1 viruses (1 ng p24). Duplicate cultures were evaluated for virus replication every 1 to 2 days by p24 ELISA. The values shown are the averages of duplicate wells from two separate cultures. (B) Regrowth of viruses from cultures shown in panel A. Normalized quantities (1 ng p24) of viruses collected from the cultures shown in panel A were reinoculated onto fresh cultures of MT-4 cells. Duplicate cultures were analyzed, and samples were withdrawn daily. The data shown are the mean values from duplicate wells from two independent assays. •, wild type; ○, CT144; ▪, L49D; □, L49D.CT144.
To determine whether replication of the L49D.CT144 mutant particles was due to reversion to wild type, we inoculated fresh MT-4 cultures with viruses harvested from the original cultures (Fig. 8B). The replication kinetics of the wild-type and CT144 viruses were similar to those observed in the original assays (Fig. 8B). L49D.CT144 replication was also similar to that seen in the original cultures, indicating that the virus that had emerged in the first cultures was neither a contaminant nor a revertant (Fig. 8B). In contrast, virus particles derived from the L49D cultures replicated at an intermediate rate (Fig. 8B). The particles failed to spread through the MT-4 cultures with wild-type kinetics but instead demonstrated kinetics that were very similar to those of L49D.CT144 particles (Fig. 8B). We confirmed this result in two independent cultures (data not shown). We conclude that the enhanced replication of the L49D.CT144 is not a consequence of contamination by, or reversion to, wild-type HIV-1. Thus, truncation of the gp41 CT partially relieved the replication defect associated with the L49D MA mutation.
The impaired fusion and infectivity of the L49D mutant are relieved by a mutation in the gp41 endocytic motif.
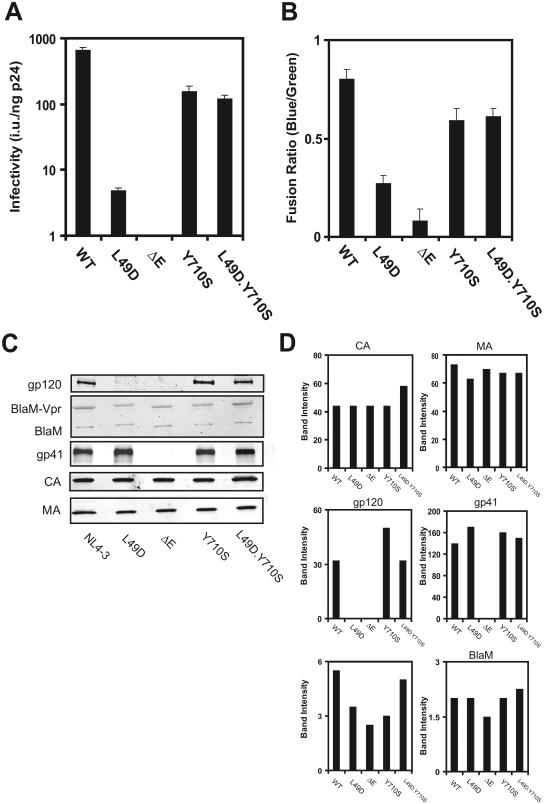
HIV-1 envelope protein is internalized from the plasma membrane via a tyrosine-based endocytic motif (64). The L49D mutant was rescued by truncating the CT domain of gp41 (see Fig. 4), resulting in the loss of the membrane-proximal endocytic sequence (18). Mutation of this sequence has also been shown to complement some MA mutations that impair Env incorporation into HIV-1 particles (76). To ask whether the L49D mutant phenotype depends on the gp41 endocytic motif, we mutated this tyrosine to serine (Y710S) (Fig. 9A). Virus particles were produced by 293T transfection and assessed for single-cycle infectivity and virus-cell fusion. In this experiment, the control L49D particles were approximately 100-fold less infectious than wild-type particles (Fig. 9A) and were approximately 30% as active for fusion (Fig. 9B). Particles containing the Y710S mutation were approximately one-fourth as infectious as wild-type particles (Fig. 9A) and were slightly less fusogenic. However, the double mutant L49D.Y710S particles were similar to the control Y710S particles in both infectivity and fusion (Fig. 9A and B). Immunoblot analyses revealed similar levels of BlaM in the particles. Furthermore, addition of the Y710S mutation restored normal levels of gp120 to L49D mutant particles (Fig. 9C). These results indicate that a specific mutation in the endocytosis motif located in gp41 overcomes the impaired fusion and infectivity of L49D mutant particles, most likely by complementing the gp120 deficit on the particles.
FIG. 9.
Mutation of the gp41 endocytic motif restores L49D fusion and infectivity. (A) Infectivity of HIV-1 particles was determined by titration on P4R5 cells. Values are the means of triplicate determinations, with error bars representing 1 standard deviation. The results are representative of three independent experiments. i.u., infectious units; WT, wild type. (B) Fusion of BlaM-Vpr reporter viruses with P4R5 target cells. The results shown are representative of two independent experiments. (C) Immunoblot analysis of pelleted particles normalized by p24 ELISA. Blots were probed with antibodies specific for BlaM, gp120/SU, p24/CA, p17/MA, and gp41/TM.
DISCUSSION
HIV-1 particle formation requires interaction of the nascent Gag protein with the cellular protein trafficking machinery (27). A growing body of evidence indicates that HIV-1 assembly utilizes cellular endosomal membranes (54, 67). Gag colocalizes with cellular markers for late endosomes (67), and budding into intracellular membranes has been visualized in macrophages (58). Release of HIV-1 particles from cells is dependent on the vacuolar protein-sorting pathway, and several vacuolar protein-sorting proteins interact functionally with Gag to promote particle release (27, 45, 71). Gag also interacts with components of adaptor protein complexes that control endocytic trafficking, including AP-2 and AP-3 subunits (14, 40). An unanswered question is where Env associates with Gag in the assembly pathway.
In this study, we observed that substitution of Asp for Leu at position 49 of MA results in HIV-1 particles that are impaired for replication in T cells. The mutant particles exhibited no obvious impairments in assembly, budding, and maturation, yet were deficient in the viral Env protein subunit gp120, despite having normal quantities of gp41. Single-cycle infection and particle fusion assays demonstrated that L49D particles were moderately (∼60%) reduced in the ability to fuse with target cells, yet were profoundly impaired for infection of target cells (∼40-fold reduction relative to wild type). Both the fusion and infectivity defects were relieved by truncation of the gp41 cytoplasmic tail and by pseudotyping by VSV-G. Truncation of the gp41 CT also partially restored the ability of the L49D mutant to replicate in MT-4 cells. Collectively, these results indicate that the L49D mutation destabilizes the noncovalent association of gp120 with gp41, either during HIV-1 assembly or following particle budding from cells. To our knowledge, the selective loss of gp120 from HIV-1 particles containing a mutation in Gag has not been previously observed. This novel phenotype suggests that interactions between Gag and gp41 modulate the gp120/gp41 association on the surface of HIV-1 particles.
How would a mutation in MA result in a specific decrease in gp120 levels on HIV-1 particles without affecting gp41? gp120 has been considered to be loosely associated with gp41 on the surface of HIV-1 particles, particularly on laboratory-adapted virus strains (30, 47-49, 56, 78). Thus, one possibility is that the L49D mutation in MA triggers the release of gp120 from HIV-1 particles following maturation of the core. However, freshly isolated L49D mutant particles that were harvested following a 1-h culture period were also deficient in gp120. Furthermore, in our studies both wild-type and L49D mutant particles exhibited minimal shedding of gp120 during an 8-h incubation at 37°C. These results imply that the decrease in gp120 on L49D particles is not due to enhanced shedding following particle budding. However, they do not exclude the possibility of a rapid dissociation of gp120 during particle release.
Another potential explanation for the novel L49D phenotype is that the MA region of Gag may stabilize the association of gp120 with gp41 during particle assembly. In a previous study, we observed that HIV-1 particles lacking the gp41 cytoplasmic tail also exhibit a selective reduction of gp120 relative to gp41, suggesting that the CT stabilizes the association of gp120 and gp41 (80). This interpretation is also consistent with studies demonstrating that mutations in the cytoplasmic domain of gp41 can affect the conformation of gp120 on the virus surface (17, 34, 69). The Leu at position 49 of MA resides on an exposed loop on the surface of the protein, providing a potential binding site for the gp41 CT (46). We postulate that engagement of gp41 by the MA domain of Gag stabilizes the Env protein complex within an intracellular assembly compartment, such as the multivesicular body, where Gag may encounter Env following its endocytosis from the cell surface. In the absence of the gp41 CT, or with an altered interaction between Gag and gp41 (as may occur with the L49D substitution), this stabilization may be impaired, resulting in incorporation of Env trimers deficient in gp120. In this study, we also observed that a point mutation in the tyrosine-based gp41 endocytic motif (Y710S) relieved the fusion and infectivity impairments of the L49D mutant. Mutations in this tyrosine have also been reported to complement other MA mutants without restoring Env incorporation (76). In contrast, we found that the Y710S mutant restored normal gp120 levels to the L49D mutant particles. We speculate that by inhibiting gp41 endocytosis, the Y710S mutation restricts Gag-Env interactions to the plasma membrane, thereby relieving the destabilizing effect of the L49D mutation on gp120-gp41 interactions during engagement of Env by Gag within endosomal compartments. This model thus assumes that the consequences of the L49D mutation depend on the intracellular site of Gag-Env association.
In addition to the fusion impairment associated with L49D mutant particles, our results indicate that the mutation affects a postentry step in the virus life cycle. The reduction in infectivity associated with the L49D particles was significantly greater than the fusion impairment. Remarkably, both the modest fusion and strong infectivity defects were rescued by pseudotyping with VSV-G or by truncating the gp41 CT. Our data therefore suggest the existence of a conditional postentry defect of the L49D mutant virions that depends on the gp41 cytoplasmic tail. In support of this, we observed that control “wild-type” HIV-1 particles lacking the L49D mutation were significantly more infectious than the mutant particles, even when the wild-type particles were rendered less active for fusion by expression of decreased Env levels in the producer cells. Additionally, the full-length HIV-1 Env protein exerted a dominant inhibitory effect on the infectivity of L49D mutant particles when cell entry was mediated by a heterologous viral Env protein that rescued the L49D infectivity impairment when the particles lacked HIV-1 Env. Based on these results, we speculate that an altered interaction between the mutant MA and gp41 results in an atypical composition or stability of the mature viral core, which has been reported to contain a fraction of virion-associated MA protein (39, 75). We are currently testing these hypotheses.
Acknowledgments
We thank members of the Aiken laboratory for helpful suggestions during the course of this study and Paul Spearman for helpful comments on the manuscript. We also thank Mike Miller (Merck Research Laboratories) for pMM310, Jane Burns for pHCMV-G, and Jack Ragheb for pCEET. The following reagents were obtained through the NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH: HIV-1 gp41 monoclonal antibody (2F5), and gp120 monoclonal antibody (2G12) from Hermann Katinger; hybridoma 902 (anti-gp120) from Bruce Chesebro; pNL4-3 from Malcolm Martin; and recombinant baculovirus-produced HIV-1 gp120 from ImmunoDiagnostics, Inc.
This work was supported by grant AI47056 from the NIH.
REFERENCES
- 1.Adachi, A., H. E. Gendelman, S. Koenig, T. Folks, R. Willey, A. Rabson, and M. A. Martin. 1986. Production of acquired immunodeficiency syndrome-associated retrovirus in human and nonhuman cells transfected with an infectious molecular clone. J. Virol. 59**:**284-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aiken, C. 1997. Pseudotyping human immunodeficiency virus type 1 (HIV-1) by the glycoprotein of vesicular stomatitis virus targets HIV-1 entry to an endocytic pathway and suppresses both the requirement for Nef and the sensitivity to cyclosporin A. J. Virol. 71**:**5871-5877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aiken, C., and D. Trono. 1995. Nef stimulates human immunodeficiency virus type 1 proviral DNA synthesis. J. Virol. 69**:**5048-5056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akari, H., T. Fukumori, and A. Adachi. 2000. Cell-dependent requirement of human immunodeficiency virus type 1 gp41 cytoplasmic tail for Env incorporation into virions. J. Virol. 74**:**4891-4893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andreassen, H., H. Bohr, J. Bohr, S. Brunak, T. Bugge, R. M. Cotterill, C. Jacobsen, P. Kusk, B. Lautrup, S. B. Petersen et al. 1990. Analysis of the secondary structure of the human immunodeficiency virus (HIV) proteins p17, gp120, and gp41 by computer modeling based on neural network methods. J. Acquir. Immune. Defic. Syndr. 3**:**615-622. [PubMed] [Google Scholar]
- 6.Bukrinsky, M. I., S. Haggerty, M. P. Dempsey, N. Sharova, A. Adzhubel, L. Spitz, P. Lewis, D. Goldfarb, M. Emerman, and M. Stevenson. 1993. A nuclear localization signal within HIV-1 matrix protein that governs infection of non-dividing cells. Nature 365**:**666-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casella, C. R., L. J. Raffini, and A. T. Panganiban. 1997. Pleiotropic mutations in the HIV-1 matrix protein that affect diverse steps in replication. Virology 228**:**294-306. [DOI] [PubMed] [Google Scholar]
- 8.Cavrois, M., C. De Noronha, and W. C. Greene. 2002. A sensitive and specific enzyme-based assay detecting HIV-1 virion fusion in primary T lymphocytes. Nat. Biotechnol. 20**:**1151-1154. [DOI] [PubMed] [Google Scholar]
- 9.Charneau, P., G. Mirambeau, P. Roux, S. Paulous, H. Buc, and F. Clavel. 1994. HIV-1 reverse transcription. A termination step at the center of the genome. J. Mol. Biol. 241**:**651-662. [DOI] [PubMed] [Google Scholar]
- 10.Chen, C., and H. Okayama. 1987. High-efficiency transformation of mammalian cells by plasmid DNA. Mol. Cell. Biol. 7**:**2745-2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen, S. S., A. A. Ferrante, and E. F. Terwilliger. 1996. Characterization of an envelope mutant of HIV-1 that interferes with viral infectivity. Virology 226**:**260-268. [DOI] [PubMed] [Google Scholar]
- 12.Chertova, E., J. W. Bess, Jr., B. J. Crise, R. C. Sowder II, T. M. Schaden, J. M. Hilburn, J. A. Hoxie, R. E. Benveniste, J. D. Lifson, L. E. Henderson, and L. O. Arthur. 2002. Envelope glycoprotein incorporation, not shedding of surface envelope glycoprotein (gp120/SU), is the primary determinant of SU content of purified human immunodeficiency virus type 1 and simian immunodeficiency virus. J. Virol. 76**:**5315-5325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deng, H., R. Liu, W. Ellmeier, S. Choe, D. Unutmaz, M. Burkhart, P. Di Marzio, S. Marmon, R. E. Sutton, C. M. Hill, C. B. Davis, S. C. Peiper, T. J. Schall, D. R. Littman, and N. R. Landau. 1996. Identification of a major co-receptor for primary isolates of HIV-1. Nature 381**:**661-666. [DOI] [PubMed] [Google Scholar]
- 14.Dong, X., H. Li, A. Derdowski, L. Ding, A. Burnett, X. Chen, T. R. Peters, T. S. Dermody, E. Woodruff, J. J. Wang, and P. Spearman. 2005. AP-3 directs the intracellular trafficking of HIV-1 Gag and plays a key role in particle assembly. Cell 120**:**663-674. [DOI] [PubMed] [Google Scholar]
- 15.Dorfman, T., F. Mammano, W. A. Haseltine, and H. G. Göttlinger. 1994. Role of the matrix protein in the virion association of the human immunodeficiency virus type 1 envelope glycoprotein. J. Virol. 68**:**1689-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubay, J. W., S. J. Roberts, B. H. Hahn, and E. Hunter. 1992. Truncation of the human immunodeficiency virus type 1 transmembrane glycoprotein cytoplasmic domain blocks virus infectivity. J. Virol. 66**:**6616-6625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards, T. G., S. Wyss, J. D. Reeves, S. Zolla-Pazner, J. A. Hoxie, R. W. Doms, and F. Baribaud. 2002. Truncation of the cytoplasmic domain induces exposure of conserved regions in the ectodomain of human immunodeficiency virus type 1 envelope protein. J. Virol. 76**:**2683-2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Egan, M. A., L. M. Carruth, J. F. Rowell, X. Yu, and R. F. Siliciano. 1996. Human immunodeficiency virus type 1 envelope protein endocytosis mediated by a highly conserved intrinsic internalization signal in the cytoplasmic domain of gp41 is suppressed in the presence of the Pr55gag precursor protein. J. Virol. 70**:**6547-6556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Feng, Y., C. C. Broder, P. E. Kennedy, and E. A. Berger. 1996. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science 272**:**872-877. [DOI] [PubMed] [Google Scholar]
- 20.Forshey, B. M., and C. Aiken. 2003. Disassembly of human immunodeficiency virus type 1 cores in vitro reveals association of Nef with the subviral ribonucleoprotein complex. J. Virol. 77**:**4409-4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fouchier, R. A., B. E. Meyer, J. H. Simon, U. Fischer, and M. H. Malim. 1997. HIV-1 infection of non-dividing cells: evidence that the amino-terminal basic region of the viral matrix protein is important for Gag processing but not for post-entry nuclear import. EMBO J. 16**:**4531-4539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freed, E. O., G. Englund, and M. A. Martin. 1995. Role of the basic domain of human immunodeficiency virus type 1 matrix in macrophage infection. J. Virol. 69**:**3949-3954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freed, E. O., and M. A. Martin. 1996. Domains of the human immunodeficiency virus type 1 matrix and gp41 cytoplasmic tail required for envelope incorporation into virions. J. Virol. 70**:**341-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freed, E. O., and M. A. Martin. 1995. Virion incorporation of envelope glycoproteins with long but not short cytoplasmic tails is blocked by specific, single amino acid substitutions in the human immunodeficiency virus type 1 matrix. J. Virol. 69**:**1984-1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freed, E. O., J. M. Orenstein, A. J. Buckler-White, and M. A. Martin. 1994. Single amino acid changes in the human immunodeficiency virus type 1 matrix protein block virus particle production. J. Virol. 68**:**5311-5320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gabuzda, D. H., A. Lever, E. Terwilliger, and J. Sodroski. 1992. Effects of deletions in the cytoplasmic domain on biological functions of human immunodeficiency virus type 1 envelope glycoproteins. J. Virol. 66**:**3306-3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garrus, J. E., U. K. von Schwedler, O. W. Pornillos, S. G. Morham, K. H. Zavitz, H. E. Wang, D. A. Wettstein, K. M. Stray, M. Cote, R. L. Rich, D. G. Myszka, and W. I. Sundquist. 2001. Tsg101 and the vacuolar protein sorting pathway are essential for HIV-1 budding. Cell 107**:**55-65. [DOI] [PubMed] [Google Scholar]
- 28.Gowda, S. D., B. S. Stein, and E. G. Engleman. 1989. Identification of protein intermediates in the processing of the p55 HIV-1 gag precursor in cells infected with recombinant vaccinia virus. J. Biol. Chem. 264**:**8459-8462. [PubMed] [Google Scholar]
- 29.Haffar, O. K., S. Popov, L. Dubrovsky, I. Agostini, H. Tang, T. Pushkarsky, S. G. Nadler, and M. Bukrinsky. 2000. Two nuclear localization signals in the HIV-1 matrix protein regulate nuclear import of the HIV-1 pre-integration complex. J. Mol. Biol. 299**:**359-368. [DOI] [PubMed] [Google Scholar]
- 30.Hammonds, J., X. Chen, L. Ding, T. Fouts, A. De Vico, J. zur Megede, S. Barnett, and P. Spearman. 2003. Gp120 stability on HIV-1 virions and Gag-Env pseudovirions is enhanced by an uncleaved Gag core. Virology 314**:**636-649. [DOI] [PubMed] [Google Scholar]
- 31.Johnston, P. B., J. W. Dubay, and E. Hunter. 1993. Truncations of the simian immunodeficiency virus transmembrane protein confer expanded virus host range by removing a block to virus entry into cells. J. Virol. 67**:**3077-3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jones, D. R., K. Suzuki, and S. C. Piller. 2002. A 100-amino acid truncation in the cytoplasmic tail of glycoprotein 41 in the reference HIV type 1 strain RF. AIDS Res. Hum. Retrovir. 18**:**513-517. [DOI] [PubMed] [Google Scholar]
- 33.Jones, P. L., T. Korte, and R. Blumenthal. 1998. Conformational changes in cell surface HIV-1 envelope glycoproteins are triggered by cooperation between cell surface CD4 and co-receptors. J. Biol. Chem. 273**:**404-409. [DOI] [PubMed] [Google Scholar]
- 34.Kalia, V., S. Sarkar, P. Gupta, and R. C. Montelaro. 2005. Antibody neutralization escape mediated by point mutations in the intracytoplasmic tail of human immunodeficiency virus type 1 gp41. J. Virol. 79**:**2097-2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaushik, R., and L. Ratner. 2004. Role of human immunodeficiency virus type 1 matrix phosphorylation in an early postentry step of virus replication. J. Virol. 78**:**2319-2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kiernan, R. E., A. Ono, G. Englund, and E. O. Freed. 1998. Role of matrix in an early postentry step in the human immunodeficiency virus type 1 life cycle. J. Virol. 72**:**4116-4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kimpton, J., and M. Emerman. 1992. Detection of replication-competent and pseudotyped human immunodeficiency virus with a sensitive cell line on the basis of activation of an integrated β-galactosidase gene. J. Virol. 66**:**2232-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kootstra, N. A., and H. Schuitemaker. 1999. Phenotype of HIV-1 lacking a functional nuclear localization signal in matrix protein of gag and Vpr is comparable to wild-type HIV-1 in primary macrophages. Virology 253**:**170-180. [DOI] [PubMed] [Google Scholar]
- 39.Kotov, A., J. Zhou, P. Flicker, and C. Aiken. 1999. Association of Nef with the human immunodeficiency virus type 1 core. J. Virol. 73**:**8824-8830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lindwasser, O. W., and M. D. Resh. 2004. Human immunodeficiency virus type 1 Gag contains a dileucine-like motif that regulates association with multivesicular bodies. J. Virol. 78**:**6013-6023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lodge, R., H. Göttlinger, D. Gabuzda, E. A. Cohen, and G. Lemay. 1994. The intracytoplasmic domain of gp41 mediates polarized budding of human immunodeficiency virus type 1 in MDCK cells. J. Virol. 68**:**4857-4861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luciw, P. A., K. E. Shaw, B. L. Shacklett, and M. L. Marthas. 1998. Importance of the intracytoplasmic domain of the simian immunodeficiency virus (SIV) envelope glycoprotein for pathogenesis. Virology 252**:**9-16. [DOI] [PubMed] [Google Scholar]
- 43.Lundquist, C. A., J. Zhou, and C. Aiken. 2004. Nef stimulates human immunodeficiency virus type 1 replication in primary T cells by enhancing virion-associated gp120 levels: coreceptor-dependent requirement for Nef in viral replication. J. Virol. 78**:**6287-6296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mammano, F., E. Kondo, J. Sodroski, A. Bukovsky, and H. G. Göttlinger. 1995. Rescue of human immunodeficiency virus type 1 matrix protein mutants by envelope glycoproteins with short cytoplasmic domains. J. Virol. 69**:**3824-3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martin-Serrano, J., T. Zang, and P. D. Bieniasz. 2003. Role of ESCRT-I in retroviral budding. J. Virol. 77**:**4794-4804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Massiah, M. A., M. R. Starich, C. Paschall, M. F. Summers, A. M. Christensen, and W. I. Sundquist. 1994. Three-dimensional structure of the human immunodeficiency virus type 1 matrix protein. J. Mol. Biol. 244**:**198-223. [DOI] [PubMed] [Google Scholar]
- 47.McKeating, J. A., A. McKnight, and J. P. Moore. 1991. Differential loss of envelope glycoprotein gp120 from virions of human immunodeficiency virus type 1 isolates: effects on infectivity and neutralization. J. Virol. 65**:**852-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moore, J. P., and P. J. Klasse. 1992. Thermodynamic and kinetic analysis of sCD4 binding to HIV-1 virions and of gp120 dissociation. AIDS Res. Hum. Retrovir. 8**:**443-450. [DOI] [PubMed] [Google Scholar]
- 49.Moore, J. P., J. A. McKeating, R. A. Weiss, and Q. J. Sattentau. 1990. Dissociation of gp120 from HIV-1 virions induced by soluble CD4. Science 250**:**1139-1142. [DOI] [PubMed] [Google Scholar]
- 50.Mulligan, M. J., G. V. Yamshchikov, G. D. Ritter, Jr., F. Gao, M. J. Jin, C. D. Nail, C. P. Spies, B. H. Hahn, and R. W. Compans. 1992. Cytoplasmic domain truncation enhances fusion activity by the exterior glycoprotein complex of human immunodeficiency virus type 2 in selected cell types. J. Virol. 66**:**3971-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murakami, T., S. Ablan, E. O. Freed, and Y. Tanaka. 2004. Regulation of human immunodeficiency virus type 1 Env-mediated membrane fusion by viral protease activity. J. Virol. 78**:**1026-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Murakami, T., and E. O. Freed. 2000. Genetic evidence for an interaction between human immunodeficiency virus type 1 matrix and α-helix 2 of the gp41 cytoplasmic tail. J. Virol. 74**:**3548-3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Murakami, T., and E. O. Freed. 2000. The long cytoplasmic tail of gp41 is required in a cell type-dependent manner for HIV-1 envelope glycoprotein incorporation into virions. Proc. Natl. Acad. Sci. USA 97**:**343-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nydegger, S., M. Foti, A. Derdowski, P. Spearman, and M. Thali. 2003. HIV-1 egress is gated through late endosomal membranes. Traffic 4**:**902-910. [DOI] [PubMed] [Google Scholar]
- 55.Ono, A., M. Huang, and E. O. Freed. 1997. Characterization of human immunodeficiency virus type 1 matrix revertants: effects on virus assembly, Gag processing, and Env incorporation into virions. J. Virol. 71**:**4409-4418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Orloff, S. L., M. S. Kennedy, A. A. Belperron, P. J. Maddon, and J. S. McDougal. 1993. Two mechanisms of soluble CD4 (sCD4)-mediated inhibition of human immunodeficiency virus type 1 (HIV-1) infectivity and their relation to primary HIV-1 isolates with reduced sensitivity to sCD4. J. Virol. 67**:**1461-1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Owens, R. J., J. W. Dubay, E. Hunter, and R. W. Compans. 1991. Human immunodeficiency virus envelope protein determines the site of virus release in polarized epithelial cells. Proc. Natl. Acad. Sci. USA 88**:**3987-3991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pelchen-Matthews, A., B. Kramer, and M. Marsh. 2003. Infectious HIV-1 assembles in late endosomes in primary macrophages. J. Cell Biol. 162**:**443-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Piller, S. C., J. W. Dubay, C. A. Derdeyn, and E. Hunter. 2000. Mutational analysis of conserved domains within the cytoplasmic tail of gp41 from human immunodeficiency virus type 1: effects on glycoprotein incorporation and infectivity. J. Virol. 74**:**11717-11723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ragheb, J. A., and W. F. Anderson. 1994. pH-independent murine leukemia virus ecotropic envelope-mediated cell fusion: implications for the role of the R peptide and p12E TM in viral entry. J. Virol. 68**:**3220-3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reicin, A. S., A. Ohagen, L. Yin, S. Hoglund, and S. P. Goff. 1996. The role of Gag in human immunodeficiency virus type 1 virion morphogenesis and early steps of the viral life cycle. J. Virol. 70**:**8645-8652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reicin, A. S., S. Paik, R. D. Berkowitz, J. Luban, I. Lowy, and S. P. Goff. 1995. Linker insertion mutations in the human immunodeficiency virus type 1 gag gene: effects on virion particle assembly, release, and infectivity. J. Virol. 69**:**642-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reil, H., A. A. Bukovsky, H. R. Gelderblom, and H. G. Gottlinger. 1998. Efficient HIV-1 replication can occur in the absence of the viral matrix protein. EMBO J. 17**:**2699-2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rowell, J. F., P. E. Stanhope, and R. F. Siliciano. 1995. Endocytosis of endogenously synthesized HIV-1 envelope protein. Mechanism and role in processing for association with class II MHC. J. Immunol. 155**:**473-488. [PubMed] [Google Scholar]
- 65.Sanders, R. W., M. Vesanen, N. Schuelke, A. Master, L. Schiffner, R. Kalyanaraman, M. Paluch, B. Berkhout, P. J. Maddon, W. C. Olson, M. Lu, and J. P. Moore. 2002. Stabilization of the soluble, cleaved, trimeric form of the envelope glycoprotein complex of human immunodeficiency virus type 1. J. Virol. 76**:**8875-8889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sharova, N., and A. Bukrinskaya. 1991. p17 and p17-containing gag precursors of input human immunodeficiency virus are transported into the nuclei of infected cells. AIDS Res. Hum. Retrovir. 7**:**303-306. [DOI] [PubMed] [Google Scholar]
- 67.Sherer, N. M., M. J. Lehmann, L. F. Jimenez-Soto, A. Ingmundson, S. M. Horner, G. Cicchetti, P. G. Allen, M. Pypaert, J. M. Cunningham, and W. Mothes. 2003. Visualization of retroviral replication in living cells reveals budding into multivesicular bodies. Traffic 4**:**785-801. [DOI] [PubMed] [Google Scholar]
- 68.Smith, D. H., R. A. Byrn, S. A. Marsters, T. Gregory, J. E. Groopman, and D. J. Capon. 1987. Blocking of HIV-1 infectivity by a soluble, secreted form of the CD4 antigen. Science 238**:**1704-1707. [DOI] [PubMed] [Google Scholar]
- 69.Spies, C. P., G. D. Ritter, Jr., M. J. Mulligan, and R. W. Compans. 1994. Truncation of the cytoplasmic domain of the simian immunodeficiency virus envelope glycoprotein alters the conformation of the external domain. J. Virol. 68**:**585-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Srivastava, I. K., L. Stamatatos, H. Legg, E. Kan, A. Fong, S. R. Coates, L. Leung, M. Wininger, J. J. Donnelly, J. B. Ulmer, and S. W. Barnett. 2002. Purification and characterization of oligomeric envelope glycoprotein from a primary R5 subtype B human immunodeficiency virus. J. Virol. 76**:**2835-2847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Strack, B., A. Calistri, S. Craig, E. Popova, and H. G. Gottlinger. 2003. AIP1/ALIX is a binding partner for HIV-1 p6 and EIAV p9 functioning in virus budding. Cell 114**:**689-699. [DOI] [PubMed] [Google Scholar]
- 72.von Schwedler, U., R. S. Kornbluth, and D. Trono. 1994. The nuclear localization signal of the matrix protein of human immunodeficiency virus type 1 allows the establishment of infection in macrophages and quiescent T lymphocytes. Proc. Natl. Acad. Sci. USA 91**:**6992-6996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang, W. K., M. Y. Chen, C. Y. Chuang, K. T. Jeang, and L. M. Huang. 2000. Molecular biology of human immunodeficiency virus type 1. J Microbiol. Immunol. Infect. 33**:**131-140. [PubMed] [Google Scholar]
- 74.Wehrly, K., and B. Chesebro. 1997. p24 antigen capture assay for quantification of human immunodeficiency virus using readily available inexpensive reagents. Methods 12**:**288-293. [DOI] [PubMed] [Google Scholar]
- 75.Welker, R., H. Hohenberg, U. Tessmer, C. Huckhagel, and H. G. Kräusslich. 2000. Biochemical and structural analysis of isolated mature cores of human immunodeficiency virus type 1. J. Virol. 74**:**1168-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.West, J. T., S. K. Weldon, S. Wyss, X. Lin, Q. Yu, M. Thali, and E. Hunter. 2002. Mutation of the dominant endocytosis motif in human immunodeficiency virus type 1 gp41 can complement matrix mutations without increasing Env incorporation. J. Virol. 76**:**3338-3349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wiegers, K., G. Rutter, H. Kottler, U. Tessmer, H. Hohenberg, and H. G. Kräusslich. 1998. Sequential steps in human immunodeficiency virus particle maturation revealed by alterations of individual Gag polyprotein cleavage sites. J. Virol. 72**:**2846-2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Willey, R. L., M. A. Martin, and K. W. C. Peden. 1994. Increase in soluble CD4 binding to and CD4-induced dissociation of gp120 from virions correlates with infectivity of human immunodeficiency virus type 1. J. Virol. 68**:**1029-1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wyma, D. J., J. Jiang, J. Shi, J. Zhou, J. E. Lineberger, M. D. Miller, and C. Aiken. 2004. Coupling of human immunodeficiency virus type 1 fusion to virion maturation: a novel role of the gp41 cytoplasmic tail. J. Virol. 78**:**3429-3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wyma, D. J., A. Kotov, and C. Aiken. 2000. Evidence for a stable interaction of gp41 with Pr55Gag in immature human immunodeficiency virus type 1 particles. J. Virol. 74**:**9381-9387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yee, J. K., T. Friedmann, and J. C. Burns. 1994. Generation of high-titer pseudotyped retroviral vectors with very broad host range. Methods Cell Biol. 43**:**99-112. [DOI] [PubMed] [Google Scholar]
- 82.Yu, X., Q.-C. Yu, T.-H. Lee, and M. Essex. 1992. The C terminus of human immunodeficiency virus type 1 matrix protein is involved in early steps of the virus life cycle. J. Virol. 66**:**5667-5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yu, X., X. Yuan, Z. Matsuda, T. H. Lee, and M. Essex. 1992. The matrix protein of human immunodeficiency virus type 1 is required for incorporation of viral envelope protein into mature virions. J. Virol. 66**:**4966-4971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yuan, X., X. Yu, T.-H. Lee, and M. Essex. 1993. Mutations in the N-terminal region of human immunodeficiency virus type 1 matrix protein block intracellular transport of the Gag precursor. J. Virol. 67**:**6387-6394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhou, J., and C. Aiken. 2001. Nef enhances human immunodeficiency virus type 1 infectivity resulting from intervirion fusion: evidence supporting a role for Nef at the virion envelope. J. Virol. 75**:**5851-5859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhu, P., E. Chertova, J. Bess, Jr., J. D. Lifson, L. O. Arthur, J. Liu, K. A. Taylor, and K. H. Roux. 2003. Electron tomography analysis of envelope glycoprotein trimers on HIV and simian immunodeficiency virus virions. Proc. Natl. Acad. Sci. USA 100**:**15812-15817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zingler, K., and D. R. Littman. 1993. Truncation of the cytoplasmic domain of the simian immunodeficiency virus envelope glycoprotein increases Env incorporation into particles and fusogenicity and infectivity. J. Virol. 67**:**2824-2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zlokarnik, G., P. A. Negulescu, T. E. Knapp, L. Mere, N. Burres, L. Feng, M. Whitney, K. Roemer, and R. Y. Tsien. 1998. Quantitation of transcription and clonal selection of single living cells with beta-lactamase as reporter. Science 279**:**84-88. [DOI] [PubMed] [Google Scholar]