Regulation of nitric oxide signaling by thrombospondin-1: implications for anti-angiogenic therapies (original) (raw)
. Author manuscript; available in PMC: 2009 Dec 18.
Published in final edited form as: Nat Rev Cancer. 2009 Feb 5;9(3):182–194. doi: 10.1038/nrc2561
Abstract
In addition to long term regulation of angiogenesis, angiogenic growth factor signaling through nitric oxide (NO) acutely controls blood flow and hemostasis. Inhibition of this pathway may account for the hypertensive and prothrombotic side effects of vascular endothelial growth factor antagonists currently used for cancer treatment. The first identified endogenous angiogenesis inhibitor, thrombospondin-1, also controls tissue perfusion, hemostasis, and radiosensitivity by antagonizing NO signaling. We examine the role of these and other emerging activities of thrombospondin-1 in cancer. Clarifying how endogenous and therapeutic angiogenesis inhibitors regulate vascular NO signaling could facilitate development of more selective inhibitors.
The insight that tumor growth requires angiogenesis led to the development and clinical use of angiogenesis inhibitors as cancer therapeutics. The drugs bevacizumab, sorafenib, and sunitinib, which are approved by the US Food and Drug Administration for the treatment of several cancers, act specifically or in part by blocking the angiogenic activity of the vascular endothelial growth factor (VEGF) pathway. These targeted drugs significantly extend survival of cancer patients but have cardiovascular side effects that include hypertension[G] and thrombosis[G]1–3. Although most attempts to define the etiology of their hypertensive activity have focused on long term changes in vessel architecture, VEGF signaling via nitric oxide (NO) also has acute effects on vessel tone[G]4, 5, and hypertension induced by the experimental VEGF receptor kinase inhibitor cediranib was recently shown to be caused by acute disruption of NO synthesis in vascular endothelium6. Recent studies of the first identified endogenous angiogenesis inhibitor, thrombospondin-1 (TSP1), reveal that it also inhibits NO-mediated signaling to acutely control tissue perfusion[G] and hemostasis[G]7, 8.
Interestingly, the pioneering work of Folkman and colleagues showed that tumors can produce circulating angiogenesis inhibitors9, and circulating TSP1 levels are elevated in people and mice with certain cancers10–12. The benefit to the tumor of circulating angiogenesis inhibitors, which in some cases are produced by stromal rather than tumor cells, is unclear. We propose that elevated plasma TSP1 can enhance tumor perfusion through its hypertensive activity. This review synthesizes emerging evidence that hemostasis and tissue blood flow are acute targets of both endogenous and therapeutic angiogenesis inhibitors and explores ways that this insight can be used to improve anti-angiogenic therapy.
Nitric oxide
Physiological activity of NO was first described by Davy in 180013, but its production by mammalian tissues and role as a signaling molecule in vascular cells was not discovered until the 1980s14. The primary endogenous source of NO in endothelial cells is the endothelial isoform of nitric oxide synthase[G] (eNOS, also known as NOS3). eNOS is a highly regulated enzyme that is controlled by varying its expression, post-translational modification, subcellular localization, and binding of several regulatory proteins15. NO diffuses rapidly through tissue and across cell membranes and binds to its most sensitive known target soluble guanylate cyclase (sGC) to stimulate production of cGMP16, which regulates a number of signaling pathways that affect vascular cell function (Fig. 1a). NO at low concentrations promotes vascular cell survival, proliferation, and migration. Higher levels of NO directly or following conversion to other reactive nitrogen species trigger additional signaling pathways17, but the control of NO signaling in vascular cells appears to be specific for the NO/cGMP pathway, thus this is the focus of this Review18.
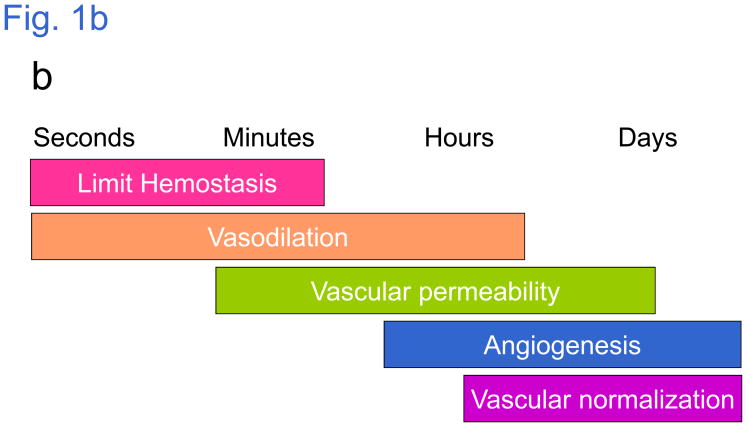
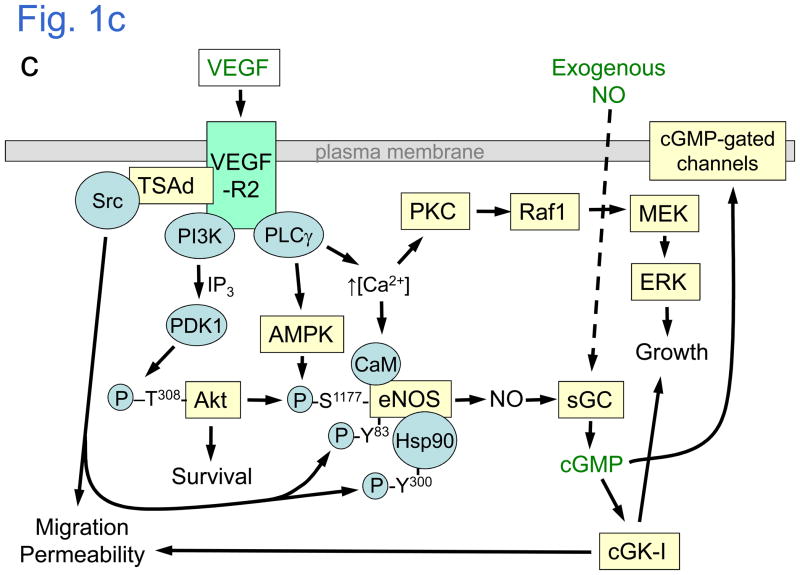
Figure 1. The central role of nitric oxide (NO) signaling in angiogenesis, vascular tone, and hemostasis.
a | Vascular endothelial growth factor (VEGF) binding to its receptor on endothelial cells activates nitric oxide synthase (eNOS) to produce the diffusible signaling molecule NO. NO acts in an autocrine manner to stimulate endothelial cell growth and motility leading to angiogenesis. VEGF signaling via NO also contributes to increasing vascular permeability. NO diffuses into vessel walls, causing arterial vessels to relax and increase blood flow. NO also acts in a paracrine manner to prevent thrombosis by inhibiting platelet adhesion and aggregation. b | Different vascular activities of NO occur on different time scales. c | In endothelial cells, VEGF signaling through VEGFR2 activates the phosphatidyinositol 3-kinase (PI3K) pathway; Akt then phosphorylates human eNOS at Ser1177 157, 158, activating eNOS and decreasing its calcium dependence. The kinase Src, which is activated by VEGF, also activates eNOS through two mechanisms: phosphorylation of Tyr83, 159 and phosphorylation of heat shock protein 90 (Hsp90), which then binds to eNOS and activates NO synthesis 160. Simultaneously, VEGFR2 signaling through phospholipase-Cγ (PLCγ) mobilizes intracellular Ca2+, which further activates eNOS in a calmodulin (CaM)-dependent manner, and increases AMP kinase (AMPK)-mediated eNOS phosphorylation at Ser1177161. NO produced by eNOS binds to the prosthetic heme on soluble guanylate cyclase (sGC) to stimulate cGMP synthesis, activating cGMP-dependent protein kinase (cGK-I) and cGMP-gated channels to regulate downstream targets that increase endothelial cell proliferation, migration, survival, and permeability14. Additional parallel signaling through Src, Akt, and the protein kinase C-mitogen-activated protein kinase pathway (PKC-Raf1-MEK-ERK) synergizes with NO/cGMP signaling to support each of these endothelial cell responses. In VSMC and platelets, the same downstream pathways are activated by exogenous NO diffusing from endothelium.
In the cardiovascular system NO/cGMP signaling has several important physiological functions (Fig. 1a). NO produced by endothelium diffuses into the vessel wall and relaxes vascular smooth muscle cells (VSMC) in arteries, thereby increasing vessel diameter, lowering resistance, and enhancing blood flow to tissues. Endothelial cell-derived NO thereby mediates acute local self-regulation of arterial tone in response to changes in mechanical shear[G] sensed by the endothelium and to circulating factors such as VEGF or acetylcholine[G]. NO also diffuses into the lumen of vessels, where it regulates hemostasis by limiting platelet aggregation19. Finally, NO acts in an autocrine manner to regulate endothelial permeability and angiogenesis20. These vascular responses to NO occur over different time scales (Fig. 1b). Hemostasis and vessel tone are regulated acutely, whereas angiogenesis requires sustained elevation of NO levels.
Angiogenic factors stimulate NO synthesis
NO/cGMP signaling is required for angiogenesis in tumor and wound healing environments, and several angiogenesis factors stimulate this signaling node20. VEGF activates eNOS through several pathways (Fig. 1c). The key role of eNOS in VEGF signaling is supported by deficiencies in both angiogenesis and acute permeability responses to VEGF in _eNOS_-null mice21. Angiogenic responses to angiopoietin-1 and angiopoietin-related factor are similarly deficient in _eNOS_-null mice22, 23. Proangiogenic signaling by adrenomedullin, estrogens, insulin, lysophosphatidic acid, sphingosine-1-phosphate, and fibroblast growth factor-2 also involve NO15, 24–26. Therefore, the NO/cGMP pathway is an important signaling node for a number of angiogenic factors.
Based on its important role in tumor angiogenesis, inhibition of eNOS has been considered as an approach to inhibit tumor growth. Accordingly, tumor growth rates and angiogenesis decrease in animals treated with NOS inhibitors27, and angiogenesis and metastasis correlate with the level of eNOS expression28. However, NO also has stimulatory and inhibitory roles in anti-tumor immunity29. Inhibiting NOS delayed immune rejection of tumors30, and stromal cell production of NO suppressed growth31. Therefore, general inhibition of NOS may not be an effective strategy to control tumor growth. At higher levels, NO is metabolized into reactive nitrogen species that have enhanced cytotoxic activities32.
What limits physiological NO signaling?
While the downstream biochemical and physiological targets of NO that mediate its positive effects on vascular cells are well understood, less attention has been given to negative regulation of NO/cGMP signaling. The distance NO diffuses in vascular tissues and the duration of its signaling are limited by its binding to heme-containing proteins, especially to the abundant hemoglobin in red blood cells33. NO bound to hemoglobin is converted to nitrite, which serves as a reservoir to regenerate NO under hypoxic conditions such as occur in solid tumors33. Following metabolism to reactive nitrogen species, NO can also react with protein thiols or glutathione to form adducts that can regenerate nitrite or NO34.
A family of cGMP phosphodiesterases play important roles in certain tissues to limit NO signaling by degrading the product of NO-driven sGC activation35. Yet, the sustained physiological activity of inhaled NO gas36, 37, the limited ability of phosphodiesterase inhibitors to dramatically alter blood pressure38, 39, and the number of major human diseases associated with states of “NO insufficiency” of undefined origin40, 41 are compelling evidence that additional regulatory pathways must limit NO/cGMP signaling. One of these pathways is mediated by the secreted protein thrombospondin-1 (TSP1).
TSP1 blocks NO-driven angiogenesis
Thrombospondins are a family of 5 secreted proteins that play distinct roles in development and physiology42. TSP3–5 are pentameric proteins that are most abundant in bone and cartilage extracellular matrix. Specific mutations in TSP5 (cartilage oligomeric matrix protein) cause two inherited forms of dwarfism43. To date, associations of TSP3–5 with cancer are limited to isolated reports of altered expression44–49.
TSP1 and TSP2 constitute a subfamily of trimeric TSPs, and both are angiogenesis inhibitors50. TSP1 is the most abundant protein in α-granules[G] of platelets, from which it is rapidly released during hemostasis51. Platelets may also serve as a buffer to control circulating TSP1 levels52, 53. TSP2 is not found in platelets but is expressed by other vascular cells. Polymorphisms in THBS1 and THBS2, which encode TSP1 and TSP2, have been associated with increased risk of cardiovascular disease54–56 but not to date with cancer57.
Altered TSP1 and/or TSP2 expression has been observed in a number of human and murine cancers (for illustrative examples see Table 1). TSP1 expression in human cancers is inversely correlated with progression, and in a few cases was found to be an independent prognostic indicator58, 59. One of the more consistent inverse relationships has been observed in colon cancer60. However, lack of correlation with progression and a few positive correlations have also been reported.61. Careful examination of some tumors that showed a positive correlation, however, revealed that the increased TSP1 originated not from tumor cells but rather from stromal cells in the tumor62–64. Induction of stromal TSP1 expression appears to be a paracrine effect of growth factors released by tumor cells. Studies of chemical-induced and spontaneous carcinogenesis in TSP1 or TSP2 transgenic mice support the hypothesis that paracrine induction of TSP1 and TSP2 expression plays an important inhibitory role in tumor progression65, 66.
Table 1.
Thrombospondin expression and cancer progression*
| Study Design | Outcome | Cancer sites | References |
|---|---|---|---|
| Trp53 null × Thbs1 null mice | Decreased survival; decreased incidence of osteosarcomas | Various | 163 |
| MMTV-THBS1 × MMTV-neu mice | Delays and prevents tumors | Mammary gland | 164 |
| K14-THBS1 mice: over-expression in skin: chemical carcinogenesis | delays squamous carcinogenesis but not malignant conversion | Skin | 66 |
| UPII-SV40T transgenic mice | Castration delays bladder carcinoma and increases TSP1 | Bladder | 165 |
| polyomavirus middle Tag × Thbs1 null mice | Larger primary tumors but fewer lung metastases | Mammary gland | 125 |
| Thbs1 null mice | Antitumor effects of low- dose continuous cyclophosphamide lost in _Thbs1_-null | Syngeneic LL/2 tumors s.c. | 166 |
| Thbs2 null mice: chemical carcinogenesis | Accelerated and increased tumor formation | skin | 65 |
| Human pathological studies | TSP1 or 2 decrease with progression | Colon carcinoma, penile squamous cell carcinoma, cervical carcinoma, leiomyosarcoma, melanoma, prostate cancer, neuroblastoma, breast ductal carcinoma in situ | 58, 59, 63, 68, 167–174 |
| TSP1 or TSP2 increase with progression | non-Hogkin’s lymphoma, colorectal liver metastases, vulvar squamous cell carcinoma, hepatocellular carcinoma | 61, 175–177 | |
| TSP1 and TSP2 not correlated with progression | stage III ovarian carcinoma, breast cancers | 178, 179 | |
| TSP1 expression attributed to tumor is actually from stroma | Melanoma, breast ductal carcinoma in situ, Pancreatic ductal carcinoma | 62–64 |
Loss of expression in cancers does not result from mutation or deletion of the THBS1 and THBS2 genes, so these are not classic tumor suppressors. Rather, expression is lost due to epigenetic silencing through hypermethylation59, 67, 68 or decreased by loss of positive regulation by tumor suppressors such as p5369 or gain of negative regulation by oncogenes such as Ras, ID1, and MYC70–72. Decreased levels of circulating TSP1 in certain inbred mouse strains are also associated with increased circulating endothelial precursors and susceptibility to cancers73. Re-expressing TSP1 or TSP2 in cancers suppresses tumor growth and angiogenesis74–77. Furthermore, recent evidence shows that TSP1 and TSP2 can also limit tumor growth by modulating innate anti-tumor immunity (Box 1).
Box 1. Expanding the role of TSP1 in cancer to innate immunity[G].
In addition to suppression of angiogenesis and acute blood flow regulation, down-regulation of TSP1 and TSP2 during tumor progression and inhibition of growth by re-expression of the proteins in murine models can also result from modulation of innate anti-tumor immunity137. Over-expression of TSP1 in melanoma cells causes delayed growth and increased tumor-associated macrophage (TAM) recruitment into xenograft tumors grown in nude mice74. However, TAM can differentiate into either cytotoxic (M1) or tumor growth-promoting (M2) states. Increased iNOS is a hallmark of M1 macrophages138, and although M1 cytotoxic macrophages are a minor fraction of the TAM in MDA-MB-435 tumors, their recruitment or differentiation is increased when those tumors express TSP1. In vitro, TSP1 acutely induces expression of PAI-1, an important regulator of macrophage migration139, 140, by human and mouse macrophages. PAI-1 is strongly expressed by TAM in TSP1-overexpressing tumors in vivo, suggesting that TSP1-induced macrophage recruitment is at least partially mediated by PAI-1137. Moreover, TSP1 and TSP2 cause a significant increase in phorbol ester-mediated superoxide generation by M1-differentated human monocytic cells, which mediates tumor cell killing, by interacting with α6β1 integrin through their NH2-terminal domains. TSP1 stimulates killing of breast carcinoma and melanoma cells by M1-polarized macrophages in vitro via this release of ROS. Taken together, these data suggest that TSP1 plays an important role in innate anti-tumor immunity by enhancing recruitment and activation of M1 TAM. Thus, avoiding this innate immune surveillance could provide an additional selective pressure for loss of TSP1 and TSP2 expression during tumor progression.
iNOS, inducible nitric oxide synthase; PAI-1, plasminogen activator inhibitor-1;
ROS, reactive oxygen species; TAM, tumor-associated macrophages.
The above findings have spurred efforts to identify active domains or peptides from TSP1 and TSP2 that could be developed as therapeutic inhibitors of angiogenesis and tumor growth50, 78, 79. A peptide sequence in the anti-angiogenic type 1 repeats of TSP1 was used to design the TSP1 mimetic ABT-510 80. This drug showed efficacy for cancer therapy in animal models and recently completed two phase II clinical trails81, 82. ABT-510 also synergizes with chemotherapy in murine models83, prompting the initiation of combination trials for cancer84–86.
Despite clear evidence that TSP1 potently inhibits angiogenesis in vivo, relatively high concentrations of TSP1 are typically required to inhibit endothelial cell proliferation and migration in vitro87, 88. One reason for this discrepancy is the absence of NO in such assays. TSP1 becomes a 100-fold more potent inhibitor in the presence of exogenous NO18. NO-stimulated vascular cell outgrowth into a 3D collagen matrix is dramatically greater in skeletal muscle explants from _Thbs1_-null compared to wild type mice. As little as 10 picomolar TSP1 blocks NO-stimulated increases in primary murine and human endothelial cell proliferation, matrix adhesion and migration. This concentration is less than that found in plasma52, indicating that circulating TSP1 levels are sufficient to limit physiological NO/cGMP signaling in endothelium.
TSP1 inhibits NO/cGMP signaling in other vascular cells
Inhibition of NO/cGMP signaling by TSP1 is not restricted to endothelial cells. TSP1 potently inhibits NO/cGMP signaling in VSMC and platelets8, 89. As discussed below, VSMC are an important target through which TSP1 controls tissue perfusion. By suppressing the antithrombotic activity of NO, TSP1 released during platelet activation play an important role in hemostasis8. In contrast, TSP1 cannot regulate cGMP synthesis in most tumor cell lines90, suggesting that inhibition of NO/cGMP signaling by TSP1 is specific to vascular cells.
TSP1 receptors mediating inhibition of NO/cGMP signaling
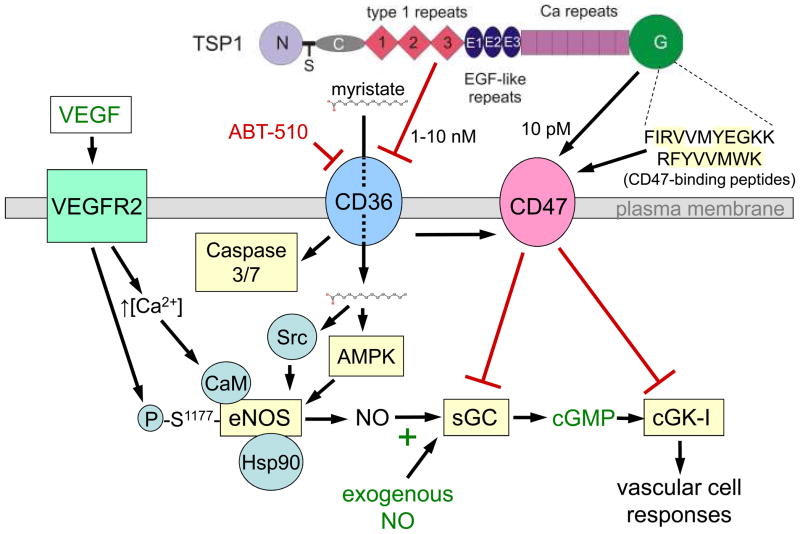
Two receptors (CD36 and CD47) mediate TSP1 inhibition of NO/cGMP signaling (Fig. 2). Vascular cells express at least 9 TSP1 receptors (Box 2)91, but initial studies focused on CD36 for inhibiting angiogenesis. Chemotaxis of CD36-deficient endothelial cells and corneal angiogenesis[G] in _CD36_-null mice were resistant to inhibition by TSP192, 93. Re-expression of CD36 in the endothelial cells restored inhibition by TSP1, indicating that this activity of TSP1 requires CD36 binding. Recombinant type 1 repeats of TSP1 that engage CD36, synthetic peptides derived from the same, and some CD36 antibodies mimic TSP1 to inhibit angiogenesis79, 92. Consistent with these results, the same agents inhibited NO-stimulated responses in vascular cells8, 18, 89. Thus, engaging CD36 is sufficient to inhibit NO/cGMP signaling. However, TSP1 remains a potent inhibitor of NO signaling in vascular cells lacking CD3694. Therefore, CD36 is not necessary for TSP1 to inhibit NO/cGMP signaling. The corneal angiogenesis assay may over-emphasize the role of CD36 due to high concentrations of soluble VEGF receptor-1 that blocks VEGF signaling via NO in this tissue95. Recent evidence suggests that the potent anti-angiogenic activity of ABT-510 may also be independent of CD36.96
Figure 2. CD47 and CD36 mediate inhibition of NO/cGMP signaling by thrombospondin-1.
Thrombospondin-1 (TSP1) redundantly inhibits cGMP signaling driven by exogenous or endogenous NO in vascular cells via 2 receptors. The C-terminal G-module of TSP1 contains two peptide motifs that have been shown to bind CD47106. The yellow highlighted residues in these peptides are conserved across all 5 TSPs, but studies using recombinant domains of TSP2 and TSP4 indicate that high affinity binding to CD47 is specific to TSP1108. Binding of TSP1 or the peptides signals via CD47 to inhibit both NO-mediated activation of soluble guanylate cyclase (sGC) in endothelial cells, VSMC, and platelets and cGMP-mediated activation of cGMP-dependent protein kinase (cGK-I) in platelets. At elevated levels, TSP1 also interacts with CD36 via its central type 1 repeats and thereby inhibits its fatty acid translocase activity105, limiting myristate uptake into the cytoplasm and thereby inhibiting membrane translocation of Src family kinases in endothelial cells. CD36-dependent myristate uptake activates two known eNOS kinases: Src and AMP kinase (AMPK)96, 103, but the relative importance of these two pathways in controlling eNOS activation through CD36 has not been established. The TSP1 mimetic drug ABT-510 also binds to CD36 and inhibits angiogenesis via both translocase-dependent and caspase-dependent mechanisms96, 162.
Box 2. TSP1 receptors that regulate angiogenesis.
Although intact TSP1 is a potent angiogenesis inhibitor, its N-terminal domains have pro-angiogenic activities141, 142. These are mediated by interactions with several TSP1-binding integrins: α3β1, α4β1, α6β1, and α9β1 141, 143–145. The N-terminal domain of TSP1 also modulates endothelial cell focal adhesions and vascular permeability by engaging calreticulin and low density lipoprotein receptor-related protein-1146, 147.
The central type 1 repeats of TSP1 and TSP2 inhibit angiogenesis by engaging the receptor CD3692, 148. CD36, a class B scavenger receptor and fatty acid translocase104, is expressed on microvascular endothelium and VSMC. Peroxisome proliferator-activated receptor-γ ligands increase vascular expression of CD36 and correspondingly increase tumor responses to the CD36-targeted drug ABT-510149. A coding polymorphism in CD36 was associated with increased risk of colorectal carcinoma in a Japanese population150.
CD47 is a high affinity cell surface receptor for the C-terminal domain of TSP1 and a low affinity receptor for this domain of TSP2 108, but the specific residues in TSP1 that mediate binding to CD47 is currently a subject of debate 151–153. CD47 is ubiquitously expressed and also plays an important role in regulating phagocytosis through engaging its counter-receptor SHPS1154. In some hematologic malignancies and breast cancer, antibody targeting of CD47 can kill tumor cells155, 156.
CD47 is the necessary receptor, based on the absence of TSP1 inhibitory activity in vascular cells from _CD47_-null mice94. TSP1 engages CD47 via its C-terminal domain97, and recombinant C-terminal domain and related CD47-binding peptides potently inhibit NO signaling94. Thus, TSP1 blockade of physiological NO-signaling in vascular cells requires CD47. CD36 engagement is sufficient to activate the inhibitory signal, but only in cells that also express CD4794. Furthermore, 100-fold lower concentrations of TSP1 are sufficient to inhibit NO signaling in vascular cells via CD47 versus CD36 (Fig. 2). The physiological importance of endogenous TSP1/CD47 signaling is shown by the elevated basal cGMP levels in vascular cells and muscle tissue from _Thbs1_- and _CD47_-null mice, which _CD36_-null cells lack94, 98.
TSP1 inhibits NO/cGMP signaling at multiple levels
sGC is clearly one target of inhibitory TSP1 signaling through CD47 (Fig. 2)91, 99. In addition to activation by NO binding to its heme moiety, sGC can be activated by post-translational modifications, drugs, and interactions with activating proteins100, but the signal transduction pathway through which CD47 ligation by TSP1 inhibits sGC activation is currently unknown. It will be important to determine whether this inhibitory signaling extends to pharmacological activators of sGC to assess whether pathological elevation of TSP1 levels would obviate the activity of sGC-activating drugs currently under development for treating cardiovascular diseases associated with NO-insufficiency101.
Remarkably, TSP1 also inhibits functional responses driven by 8Br-cGMP, a cell-permeable analog of cGMP, including a delay in platelet aggregation18. TSP1 inhibits 8Br-cGMP-stimulated phosphorylation of platelet VASP[G] at Ser239, a direct target of cGMP-dependent protein kinase (cGK)102. 8Br-cGMP-induced phosphorylation of a defined cGK peptide substrate in platelet lysates is inhibited by pretreatment of platelets with TSP1. Therefore, cGK is a second target of inhibitory TSP1 signaling (Fig. 2).
Further studies revealed a third site at which TSP1 controls physiological NO signaling. Extracellular myristate stimulates eNOS activity in a CD36- and AMP kinase-dependent manner103 (Fig. 2). CD36 is a known transporter of free fatty acids104, and TSP1 and a CD36 antibody known to mimic its anti-angiogenic activity potently block radiolabeled myristate uptake via CD36 into endothelial cells105. TSP1 blocks myristate-stimulated cGMP synthesis in an eNOS-dependent manner. Thus, inhibition of myristate uptake via CD36 and consequent blocking of eNOS activation is a third mechanism by which TSP1 limits NO/cGMP signaling in vascular cells (Fig. 2). Because 1–10 nM TSP1 is required to inhibit myristate uptake, whereas 10 pM TSP1 is sufficient for blocking sGC and cGK activation via CD47, the latter targets should be dominant for cell-autonomous inhibition of NO signaling. However, the ability to inhibit endothelial NO synthesis through CD36 provides a mechanism by which circulating TSP1 could also limit the paracrine effects of endothelium-produced NO on platelets and VSMC (Fig. 1a).
Do other TSPs inhibit NO/cGMP signaling?
Given the potent and redundant regulation of vascular NO/cGMP signaling by TSP1, it is important to know whether this activity is shared by other members of the TSP family. All 5 TSPs have conserved sequence motifs in their C-terminal G-module that are known to bind to CD47 as synthetic peptides (Fig. 2)106, and one study provided correlative evidence that both TSP1 and TSP2 regulate inflammatory responses via CD47107. However, we found that the C-terminal signature domains[G] of TSP2 and TSP4 bind much less avidly to CD47-expressing cells than does the signature domain of TSP1108. Consistent with their decreased binding avidities, the signature domains of TSP2 and TSP4 are less active for inhibiting NO-stimulated cGMP synthesis in vascular cells. Therefore, potent antagonism of NO signaling is relatively specific for TSP1. As discussed below, this selectivity is reflected in several phenotypes of _Thbs1_- versus _Thbs2_-null mice.
TSP1 acutely regulates blood flow
The activity of TSP1 via CD47 to block NO-stimulated relaxation of contracting VSMC in vitro89 translates directly to regulation of blood flow in vivo. Challenging _Thbs1_- or _CD47_-null mice with NO results in twice the increase in regional blood flow as in wild type animals7. Thus, endogenous TSP1 engaging CD47 constantly limits the dynamic blood flow response of healthy tissue to NO.
Antagonism of NO/cGMP signaling by TSP1 becomes more pronounced under ischemic conditions. This is relevant to cancer because of the transient and persistent hypoxic conditions found in solid tumors109. Ischemic soft tissue survival and blood flow are significantly enhanced in mice lacking TSP1 or CD47. This is true for partial fixed ischemia[G] models employing skin flaps or femoral artery ligation in hindlimbs and for total ischemia[G] in full thickness skin grafts7, 110, 111. Conversely, loss of tissue blood flow and tissue necrosis in wild type mice can be prevented by blocking TSP1/CD47 signaling using antibodies or antisense techniques98, 99, 110, 111. Consistent with its weak binding to CD47108, _Thbs2_-null mice show no advantage in the same ischemic injury models108, further indicating that this is a specific function of TSP1.
Reperfusion of ischemic tissue results in an additional stress mediated by recruitment and activation of immune inflammatory cells. These in turn release inflammatory mediators and reactive oxygen species, yielding an ischemia-reperfusion (I/R) injury112. Increasing NO decreases I/R injury by improving return of blood flow and limiting inflammatory cell activation. Following liver I/R, _Thbs1_- and _CD47_-null mice show better preservation of liver cytoarchitecture and lower serum levels of released liver enzymes than wild type mice113. Furthermore, pre-treating wild type animals with a function-blocking CD47 antibody decreases liver I/R injury. Therefore, endogenous TSP1 augments both fixed ischemic and I/R injury responses. Given that solid tumors are constantly subject to cycles of I/R109, the loss of TSP1 expression in some tumors could offer a selective advantage by maximizing the anti-inflammatory activity of NO produced in the tumor.
Does flow regulation select for loss of TSP1 in cancer?
Although TSP1 clearly has acute effects on tissue perfusion in addition to its long term regulation of angiogenesis, it was unclear whether such acute regulation extends to blood flow in tumors. On the one hand, the tumor vasculature is anatomically abnormal114. The tortuous channels and poor organization of tumor vasculature creates turbulent flow and transient interruptions in perfusion, both of which increase overall resistance and limit the degree to which flow could increase in response to dilation of arteries and arterioles feeding the tumor vascular bed. The characteristic leakiness of tumor vasculature also results in increased interstitial pressure115, which further limits the ability of tumor perfusion to increase in response to increased pressure in the perfusing vessels following upstream vasodilation by NO.
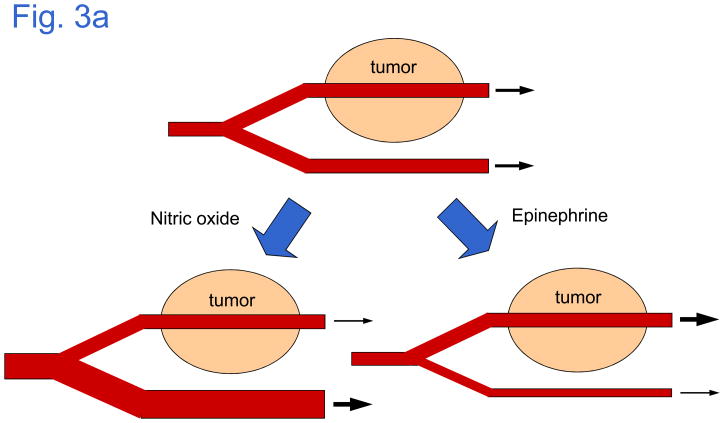
An ability to acutely regulate the perfusion of tumors is desirable for cancer treatment, for example to enhance hyperthermia therapy[G] by decreasing tumor blood flow, or to increase intravenous delivery of cytotoxic therapeutics by increasing flow. In many but not all tumors, vasodilators such as NO diminish flow through the tumor, while vasoconstrictors increase flow116, 117. This paradoxical outcome has given rise to the concept of a “vascular steal phenomenon,”118 which is based on evidence that healthy tissue is more responsive to vasoactive agents than are vessels in the tumor (Fig. 3a). Thus, systemic vasodilation would “steal” blood flow from the tumor by selectively decreasing resistance in the healthy tissues.
Figure 3. Vascular responses outside the tumor primarily determine effects of TSP1 on tumor perfusion.
a | Tumor vasculature is much less responsive than normal vasculature to physiological regulation by vasodilators such as NO and vasoconstrictors such as epinephrine. Thus, vasodilation indirectly decreases blood flow through the tumor, and vasoconstriction increases flow through the tumor. b | These responses to vasoactive agents are not sensitive to endogenous TSP1 in the tumor vasculature, but over-expression of TSP1 in the tumor either locally or by release into the circulation tempers responses to vasoactive agents in the host vasculature and decreases the “steal” phenomenon in mice bearing TSP1-expressing tumors. The relative contribution of local versus systemic effects of TSP1 on tumor vascular resistance remains to be defined.
We recently examined the ability of TSP1 to acutely regulate tumor blood flow using syngeneic melanomas grown in wild type and _Thbs1_-null mice90. Blood flow in tumor versus normal tissue was imaged using blood oxygen level-dependent (BOLD)-MRI[G]. Consistent with BOLD-MRI data in healthy mice at rest7, flow through normal soft tissue increased when tumor-bearing mice were challenged using a rapidly releasing NO donor, and the increase was greater in _Thbs1_-null mice. In contrast, flow through the tumor decreased immediately following NO challenge and did not differ between the _Thbs1_-null and wild type mice. This decrease in tumor flow is consistent with a steal effect, indicating that the tumor vasculature is less able to acutely dilate in response to NO. Because tumors in wild type and _Thbs1_-null mice showed similar resistance, this inability to respond to NO is not dependent on TSP1 expression in the tumor vasculature. Therefore, the tumor vasculature has a limited ability to acutely alter its perfusion, due to either its abnormal vascular architecture or an absence of functional smooth muscle119. Rather, vasoactive agents indirectly alter tumor perfusion by either increasing or decreasing the hydrostatic pressure in major vessels supplying the tumor (Fig. 3a).
Acute flow changes following vascular challenge were also examined in a melanoma xenograft model90. The parental melanoma cell line MDA-MB-435 lacks significant TSP1 expression and is tumorigenic in athymic mice74. Like the syngeneic melanoma, NO challenge decreased flow through this xenograft tumor while increasing flow in the contralateral leg, and injection of the vasoconstrictor epinephrine increased flow through the tumor while decreasing flow elsewhere. However, when the same tumor cells were engineered to express TSP1, which decreases growth, angiogenesis, and spontaneous lung metastasis74, the acute decrease in flow following NO challenge was diminished, and epinephrine challenge did not increase flow. Therefore, TSP1 secretion by a tumor can limit its acute responsiveness to blood flow regulation. This could involve local effects of TSP1 on the tumor vasculature, but a more likely explanation is that TSP1 released into the circulation from the tumor tempers acute responses of vascular beds outside of the tumor to vasodilator or vasoconstrictor challenge (Fig. 3b).
The concept that TSP1 can temper acute regulation of tumor blood flow has several implications. Although TSP1 expression is frequently suppressed in tumors, elevated circulating TSP1 levels derived from stromal cells have been reported in certain human cancers11, 12. Our data suggest that such increased circulating TSP1 could increase tumor perfusion if it selectively vasoconstricts and thereby limits perfusion of healthy tissues. This hypothesis is consistent with the known ability of endogenous TSP1 to limit blood flow through normal muscle and in ischemic tissues7. A second implication of this data concerns the use of angiogenesis inhibitors in conjunction with chemotherapy or radiotherapy. To enhance radiotherapy and chemotherapy responses, agents have been sought that temporarily increase tumor perfusion. Our results suggest that a TSP1 mimetic administered prior to irradiation could temporarily increase tumor perfusion and thereby enhance responses to radiotherapy. Similarly, TSP1 mimetics could improve tumor delivery of chemotherapeutics by selective vasoconstriction of extratumoral vessels (Fig. 3b). However, such mimetics should be used with caution since they would be expected to also have similar prothrombotic activity as TSP18. Indeed, we found that ABT-510 is a weak inhibitor of myristate uptake via CD36 (Fig. 2), and ABT-510 has corresponding prothrombotic activities in platelets96 and some patients86.
Do therapeutic angiogenesis inhibitors resemble TSP1?
Analogous to TSP1 and ABT-510, the hypertensive activity of therapeutic angiogenesis inhibitors may contribute to their efficacy. Bevacizumab, sunitinib, and sorafinib block VEGF-dependent activation of eNOS (Fig. 4). In addition to inhibiting NO/cGMP signaling in endothelial cells, these inhibitors decrease the flux of NO released by endothelial cells to act on other vascular targets. This can explain the acute regulation of blood pressure by intravenous VEGF and cediranib6. By analogy, we argue that the prothrombotic and hypertensive activities reported for clinical angiogenesis inhibitors have a similar basis (Fig. 4, Table 2). A similar explanation was recently proposed for the renal side effects of these drugs120.
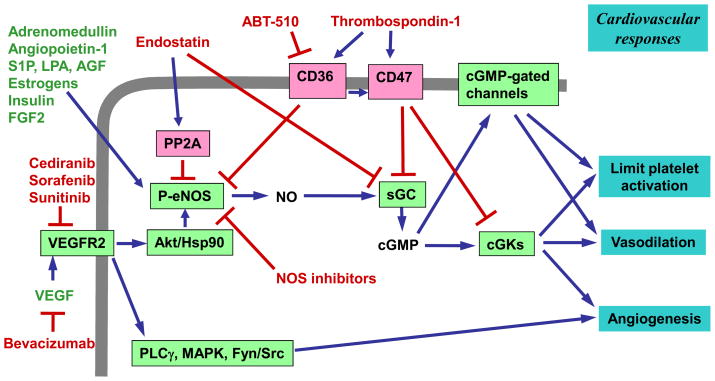
Figure 4. Convergence of angiogenesis inhibitor signaling on the nitric oxide (NO)/cGMP cascade.
The current US Food and Drug Administration (FDA)-approved angiogenesis inhibitors for cancer therapy block vascular endothelial growth factor (VEGF) binding to the VEGF receptor (VEGFR2) (the inhibitor bevacizumab) or inhibit the tyrosine kinase activity of VEGFR2 (the inhibitors sorafenib and sunitinib). VEGFR2 activates several parallel signaling pathways that control angiogenesis, but inhibiting NO/cGMP signaling blocks most of these responses. Therapeutic responses to VEGF inhibitors may be limited by parallel activation of the downstream pathways by additional angiogenic factors produced by tumors that can activate NO/cGMP signaling independent of the VEGF receptor such as adrenomedullin, angiopoietin-1, sphingosine 1-phosphate (S1P), lysophosphatidic acid (LPA), angiopoietin-related growth factor (AGF), estrogens, insulin, and fibroblast growth factor-2 (FGF2)15, 22–24. Therefore, inhibitors that act on essential downstream pathways may be more effective than the existing VEGF/VEGFR antagonists for controlling tumor angiogenesis. Endostatin is one such agent that acts via the phosphatase PP2A to inhibit nitric oxide synthase (eNOS) activation121 and downstream to inhibit soluble guanylate cyclase (sGC) expression122. Thrombospondin 1 (TSP1) is a redundant inhibitor of the NO/cGMP cascade, and the experimental drug ABT-510, a TSP1 mimetic, inhibits angiogenesis via the TSP1 receptor CD3696. However, native TSP1 also acts through the more potent inhibitory pathway mediated by CD47. Proangiogenic factors and signaling pathways are shown in green, and anti-angiogenic factors and pathways are in red.
Table 2.
Hypertensive and prothrombotic activities of angiogenesis inhibitors
| Drug | Side-effect (incidence) | Study design | Reference |
|---|---|---|---|
| Bevacizumab | Hypertension (35%) | 154 patients: 20% new onset and 80% an exacerbation of pre-existing hypertension | 1 |
| Bevacizumab | Hypertension (15%) | Phase II trial in unresectable hepatocellular carcinoma | 180 |
| Thrombosis (6%). | |||
| Bevacizumab | Venous thromboembolism (11.9%) | Meta-analysis of 7956 patients from 15 randomized controlled trials | 181 |
| Bevacizumab | Hypertension (23–34%) | Review of clinical data for several cancers | 182 |
| Sorafenib | Hypertension (11–75%) | ||
| Sunitinib | Hypertension (19%) | ||
| Sorafenib | Hypertension (23.4%) | Meta-analysis of 4599 patients with renal cell carcinoma | 2 |
| Sorafenib | Hypertension and proteinuria (7 patients) | Noted to resemble preeclampsia | 183 |
| Sunitinib | |||
| Cedifanib | Acute hypertension in rats | NO signaling proposed to be responsible | 6 |
| Telatinib | Hypertension and Proteinuria (18 patients) | Phase I trial: noted decreased response to nitroglycerin | 184 |
| Various inhibitors | Hemostasis and thrombosis | Review of clinical study and trial data | 3 |
| Various inhibitor | Hypertension and proteinuria | Editorial proposes key role for NO depletion in renal vasculature | 120 |
TSP1 and cancer evolution
The elevated circulating TSP1 levels typical of certain cancers may provide a selective advantage to the tumor by maximizing tumor perfusion at the expense of other vascular beds. If circulating TSP1 in cancer does serve to increase perfusion of the tumor, could the discovery of other circulating angiogenesis inhibitors such as endostatin9, which inhibits eNOS activation via PP2A121 and inhibits sGC expression122 (Fig. 4), indicate that their release into the host circulation generally confers an advantage to the tumor by increasing perfusion? This could be viewed as a competitive evolutionary adaptation of tumors to maximize the nutrients they can obtain123. Conversely, platelet interactions with tumor cells play a critical role in metastasis124, so the activity of TSP1 to increase platelet adhesion8 could provide a selective advantage to account for the observed increased metastatic spread of some tumors that induce higher levels of circulating TSP1125. Both of these hypotheses merit further study to define what selective pressures drive these changes in TSP1 expression.
TSP1 and radiosensitivity
Angiogenesis inhibitors are increasingly being tested in combination with radiotherapy. Empirical evidence from animal tumor models and human clinical trials indicates that this combination is beneficial126, but the mechanism remains controversial. On the one hand, tumors have hypoxic regions, and based on their ability to “normalize” the tumor vasculature, angiogenesis inhibitors may improve the overall oxygenation of tumors in an NO-dependent manner127. Increased tissue oxygenation can increase radiosensitivity109, 128. This scenario predicts that prior treatment with angiogenesis inhibitors would produce the best enhancement. However, some studies have shown enhanced radiosensitivity when angiogenesis inhibitors are administered either immediately before or after irradiation129. In this case, mechanisms other than vascular normalization must account for their efficacy. Based on the radioresistance of tumors grown in mice lacking Bax or acid sphingomyelinase, which protect the tumor vasculature from radiation-induced apoptosis, tumor endothelial cells were proposed to be the critical radiosensitive component of tumors130. Thus, combining angiogenesis inhibitors with radiation could enhance apoptosis within the tumor vasculature and thereby starve the tumor of nutrients. This could account for some acute radiosensitization by angiogenesis inhibitors. However, other studies have questioned the limiting role of tumor vasculature in tumor radioresistance131, 132.
Given the many variables that can influence tumor tissue responses to radiation, it is important to first understand how angiogenesis inhibitors influence radiosensitivity in normal tissue. In addition to shedding light on cancer radiosensitivity, any manipulation that improves radioresistance of normal tissue could be exploited to locally protect surrounding healthy tissue and thereby maximize the radiation dose that can be delivered to an underlying tumor. If tumor radiosensitivity indeed proves to be more important than that of the tumor vasculature, systemic administration of a vascular radioprotectant could prevent radiation damage to healthy tissue without compromising tumor ablation.
Assessing the radiosensitivity of healthy soft tissue in mice, we recently found that _Thbs1_-null mice are remarkably resistant to high dose (25 Gy) hindlimb irradiation133. In the skin, alopecia[G] and wet desquamation[G] were decreased compared to that observed in wild type mice, and histological examination after 2 months confirmed preservation of skin architecture and function. Remarkably, underlying skeletal muscle in _Thbs1_-null mice showed essentially no signs of necrosis or fibrosis following irradiation. Not only was muscle mitochondrial function preserved, but the null mice tended to have greater muscle mass in the irradiated hindlimb compared to nonirradiated control limbs. Responses to irradiation in _CD47_-null mice paralleled those of the _Thbs1_-null, indicating that this TSP1 receptor is critical to the radiosensitizing activity of endogenous TSP1. _Thbs2_-null mice showed no protection from radiation injury, however, indicating that this activity is specific for TSP1.
Shortly following irradiation, apoptosis was also decreased in muscle and bone marrow of _Thbs1_- and _CD47_-null mice. Because CD47 and TSP1 are also implicated in recruitment of inflammatory cells at sites of infection or injury97, 134, we considered whether the apparent radioprotection could be secondary to a decreased inflammatory response in the irradiated null limbs. To eliminate this variable, radiosensitivity was assessed in vascular cells isolated from the respective mice. Remarkably, _Thbs1_- and _CD47_-null cells in culture replicated the radioresistance of their hosts133. The null cells exhibited less death following irradiation, and over time in culture, maintained proliferative capacity that was progressively lost by irradiated wild type cells. Thus, eliminating the signal from secreted TSP1 engaging its receptor CD47 dramatically protects the viability and proliferative capacity of cells following high dose irradiation. Cell-autonomous radioprotection in the null cells indicates that blocking this pathway in vivo could be protective independent of any effect of these proteins on the immune system. Although elevating NO is known to be radioprotective for whole body irradiation135, ongoing experiments indicate that regulation of NO/cGMP signaling only partially explains this radioprotection. Additional molecular mechanisms are under investigation.
Returning to the controversy concerning the relative contribution of tumor cells versus host vasculature to radiosensitivity, we compared radiation growth delays for syngeneic B16 melanomas implanted in wild type versus _Thbs1_-null mice133. No decrease in irradiation-induced regrowth delay was observed in the _Thbs1_-null mice. Therefore, antagonists of TSP1/CD47 interaction merit testing as selective radioprotectants and could permit higher radiation doses to be delivered to tumors while preserving critical adjacent tissue and organ function.
Conclusions and perspectives
Several common themes are emerging from studies of the endogenous inhibitor TSP1 and therapeutic angiogenesis inhibitors. First, we must not allow the name “angiogenesis inhibitor” to limit how we view the physiological pathways influenced by these agents. NO/cGMP signaling is an important component of pro-angiogenic signaling downstream of VEGF and other vascular growth factors, but the same pathway also mediates acute effects of VEGF signaling on vascular smooth muscle tone and regulates platelet homeostasis (Fig. 4). Just as VEGF has both long term and acute effects on vascular physiology and thrombosis, endogenous and therapeutic angiogenesis inhibitors should be expected to acutely affect the same pathways. TSP1 is an acute vasoconstrictor136, and bevacizumab and VEGFR kinase inhibitors exhibit similar hypertensive activities. TSP1 and the therapeutic VEGF pathway antagonists also share similar prothrombotic activities. Because NO rapidly diffuses between cells, blocking NO synthesis by endothelial cells using VEGF pathway antagonists lowers the level of NO seen by platelets and VSMC.
This concept is beginning to be recognized in attempts to overcome the side effects of therapeutic VEGF antagonists6. If NO/cGMP signaling is critical for both angiogenesis and acute cardiovascular regulation, then manipulation of other pathways unique to acute vascular regulation may compensate for loss of NO signaling. Thus, use of antihypertensive drugs (an angiotensin-converting enzyme inhibitor or a calcium channel blocker) overcame the hypertensive activity of the VEGF signaling inhibitor cediranib without blocking its inhibition of tumor growth6, 120.
What does this teach us about designing a better angiogenesis inhibitor? One scenario would be to selectively target components of the NO/cGMP signaling cascade that mediate long term regulation of angiogenesis but not acute cardiovascular responses. The current FDA-approved angiogenesis inhibitors all are expected to inhibit eNOS activation and thus lower the level of NO available for its paracrine regulation of VSMC and platelets. TSP1 signaling via CD47 inhibits sGC and cGK activation. Drugs that selectively inhibit at this level in endothelium could potentially block the autocrine pro-angiogenic activity of NO without blocking physiological NO paracrine signaling to the underlying VSMC. Antibodies that engage CD47 and mimic TSP1 binding would be one such approach. These would engage CD47 on the endothelium but be too large to cross the basement membrane to inhibit signaling in the VSMC. CD47 antagonists may also provide an advantage over VEGF antagonists by their ability to also block NO/cGMP signaling induced by other tumor-derived angiogenic factors (Fig. 4).
As we learn more about the specific downstream targets of NO/cGMP signaling that are critical for long term angiogenic responses versus acute vasoregulation and hemostasis, additional targets may be identified that can selectively block the pro-angiogenic aspects of NO/cGMP signaling. Achieving this goal will require further efforts to map the signaling networks mediating acute and chronic responses to NO in each vascular cell type.
Studies of TSP1 are also teaching us that angiogenesis inhibitors can profoundly affect other aspects of tumor biology including anti-tumor immunity and radiotherapy responses. Although TSP1 potently inhibits NO/cGMP signaling, additional signaling pathways controlled by TSP1 may be important for these other activities. Investigating these may identify additional targets for controlling tumor growth and improving responsiveness to ablative therapies.
Display items
At-a-glance
- Nitric oxide (NO) mediates pro-angiogenic activities of vascular endothelial growth factor and a number of additional angiogenic factors that support the neovascularization of tumors. This signaling involves activation of soluble guanylate cyclase and downstream targets of cGMP.
- Thrombospondin-1 (TSP1) and TSP2 are endogenous angiogenesis inhibitors. Their expression is frequently lost during cancer progression, and over-expression suppresses tumor growth. TSP1 is a potent antagonist of NO signaling in vascular endothelial cells, vascular smooth muscle cells, and platelets. TSP2 is substantially less active.
- Antagonism of NO signaling can be mediated by TSP1 binding to two of its receptors, CD36 and CD47, but CD47 mediates inhibition at much lower concentrations of TSP1, and CD47 is also required for signaling through CD36.
- TSP1 signaling through CD47 redundantly inhibits NO signaling at the level of soluble guanylate cyclase and cGMP-dependent protein kinase.
- In addition to long term inhibition of angiogenesis, antagonism of NO signaling by TSP1 results in acute inhibition of tissue perfusion and acceleration of platelet hemostasis. Consequently, TSP1 and CD47 limit recovery of blood flow and tissue survival following ischemic injuries. In contrast, tumor vasculature is resistant to acute vasodilation by NO, and increased circulating TSP1 produced by tumor stroma may instead indirectly increase tumor perfusion by limiting blood flow elsewhere.
- These activities of TSP1 parallel the hypertensive and prothrombotic activities that are emerging as frequent side effects of therapeutic angiogenesis inhibitors, and both can be explained by inhibition of NO signaling.
- TSP1 signaling through CD47 also limits soft tissue survival after radiation injury. Disruption of this pathway is a possible strategy to permit delivery of higher therapeutic radiation doses to tumors while selectively protecting surrounding healthy tissues.
Acknowledgments
This work was supported by the Intramural Research Program of the NIH, NCI, Center for Cancer Research (DDR). Gema Martin-Manso is recipient of a grant BEFI from Instituto de Salud Carlos III (Spanish Ministry of Heath).
Glossary
Hypertension
A condition in which blood pressure is chronically elevated
Thrombosis
Formation of a blood clot (thrombus) inside a blood vessel that obstructs blood flow
Vessel tone
An assessment of vessel resistance to blood flow. Vessel tone is decreased by NO-mediated vasodilation and increased by activity of autonomic innervation and the presence of vasopressors
Tissue perfusion
The volume of blood that flows through a unit quantity of tissue
Hemostasis
Physiological process that arrests bleeding at a site of injury by formation of a hemostatic plug, resolves this plug during healing, and maintains circulating blood in a fluid state in the absence of injury
Nitric oxide synthase
Mammalian genomes encode three nitric oxide synthases: NOS1 or nNOS is constitutively expressed in neuronal tissues, NOS2 or iNOS is an inducible enzyme in phagocytic cells that can also be induced by inflammatory mediators in vascular cells, and NOS3 or eNOS is a constitutively expressed but highly regulated enzyme in endothelium and platelets
Mechanical shear
A physical force exerted on endothelial cells in blood vessels as a result of blood flow, which regulates the activity of eNOS in endothelium
Acetylcholine
A neurotransmitter in the autonomic nervous system that activates eNOS in endothelial cells by increasing cytoplasmic calcium levels
α-Granules
A major secretory organelle in platelets. The primary source for purification of thrombospondin-1
Corneal angiogenesis assay
A standard method to assess pro- and anti-angiogenic factors by implanting slow-releasing polymer pellets containing the factors into the avascular cornea, usually of mice, rats, or rabbits
VASP
Vasodilator-stimulated phosphoprotein is a protein that controls actin polymerization. It is a well characterized substrate for phosphorylation by cGMP-dependent protein kinase
Signature domain
Conserved C-terminal region of thrombospondins that includes EGF-like repeats, calcium-binding repeats and the C-terminal globular domain. Contains the binding site for CD47 in TSP1
Partial fixed ischemia
A partial but sustained loss of tissue blood flow
Total ischemia
Sustained total loss of tissue blood flow
Hyperthermia therapy
The use of heat to damage or kill cancer cells and to make cancer cells more sensitive to the effects of radiation and certain anticancer drugs
Blood oxygen level-dependent magnetic resonance imaging (BOLD-MRI)
An imaging technique that assesses blood oxygenation by detecting oxygen bound to hemoglobin
Alopecia
A temporary or permanent loss of hair. Typically occurs several weeks following high dose irradiation for tumor treatment
Wet desquamation
Skin damage leading to broken skin or infection due to a fluid filled abscess created by a blocked ducts or capillaries. A characteristic side effect of high dose irradiation
Innate immunity
Cells and mechanisms that defend the host from pathogens or tumors in a non-specific manner. Innate anti-tumor immunity involves primarily macrophages and natural killer cells
Biographies
JEFF S. ISENBERG
Jeff S. Isenberg is an Associate Professor of Medicine and a principal investigator of the Hemostasis and Vascular Biology Research Institute, University of Pittsburgh School of Medicine. He received his B.A. from the University of Pennsylvania (1982) and his medical training at Tulane University School of Medicine (M.D., M.P.H, 1986). Following general surgery residency he specialized in reconstructive, hand and microsurgery training at Yale University and the University of Southern California. He completed postdoctoral training in the Laboratory of Pathology with Dr. Roberts. His research interests include selective control of tissue perfusion/survival, blood flow, and cardiovascular responses through enhancing NO signaling.
GEMA MARTIN-MANSO
Gema Martin-Manso is a graduate student at the Universidad Complutense of Madrid and a Predoctoral Visiting Fellow with Dr. Roberts in the Laboratory of Pathology. She received her B.D. in Biology (Neurobiology) from the Complutense University, Madrid, Spain (2000). Her research focuses on regulation of innate immunity in cancer.
JUSTIN B. MAXHIMER
Justin B. Maxhimer is a Resident in General Surgery at The Johns Hopkins Hospital and a Cancer Research Training Award fellow with Dr. Roberts in the Laboratory of Pathology. He received his B.A in Biological Sciences from Northwestern University (1998) and his M.D. from Rush Medical College (2005). He was a Howard Hughes Medical Institute-NIH Research Scholar (2003-4). His research interests are wound healing, signaling, and hemodynamics in surgical models.
DAVID D. ROBERTS
David D. Roberts is Chief of the Biochemical Pathology Section, Laboratory of Pathology in the Center for Cancer Research, National Cancer Institute, National Institutes of Health in Bethesda. He received his B.S. in Chemistry from Massachusetts Institute of Technology (1976) and his Ph.D. in Biological Chemistry from The University of Michigan (1983). His research has focused on extracellular matrix and the role of thrombospondins in regulating tumor growth, redox signaling, angiogenesis, tissue perfusion, and anti-tumor immunity.
References
- 1.Pande A, Lombardo J, Spangenthal E, Javle M. Hypertension secondary to anti-angiogenic therapy: experience with bevacizumab. Anticancer Res. 2007;27:3465–3470. [PubMed] [Google Scholar]
- 2.Wu S, Chen JJ, Kudelka A, Lu J, Zhu X. Incidence and risk of hypertension with sorafenib in patients with cancer: a systematic review and meta-analysis. Lancet Oncol. 2008;9:117–123. doi: 10.1016/S1470-2045(08)70003-2. [DOI] [PubMed] [Google Scholar]
- 3.van Heeckeren WJ, et al. Complications from vascular disrupting agents and angiogenesis inhibitors: aberrant control of hemostasis and thrombosis. Curr Opin Hematol. 2007;14:468–480. doi: 10.1097/MOH.0b013e3282a6457f. [DOI] [PubMed] [Google Scholar]
- 4.Ku DD, Zaleski JK, Liu S, Brock TA. Vascular endothelial growth factor induces EDRF-dependent relaxation in coronary arteries. Am J Physiol. 1993;265:H586–592. doi: 10.1152/ajpheart.1993.265.2.H586. First report that VEGF is an acute vasodilator. [DOI] [PubMed] [Google Scholar]
- 5.Yang R, et al. Effects of vascular endothelial growth factor on hemodynamics and cardiac performance. J Cardiovasc Pharmacol. 1996;27:838–844. doi: 10.1097/00005344-199606000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Curwen JO, et al. Inhibition of vascular endothelial growth factor-a signaling induces hypertension: examining the effect of cediranib (recentin; AZD2171) treatment on blood pressure in rat and the use of concomitant antihypertensive therapy. Clin Cancer Res. 2008;14:3124–3131. doi: 10.1158/1078-0432.CCR-07-4783. In vivo demonstration of acute blood pressure regulation by VEGF and the opposing acute hypertensive activity of a VEGF kinase inhibitor. [DOI] [PubMed] [Google Scholar]
- 7.Isenberg JS, et al. Thrombospondin-1 limits ischemic tissue survival by inhibiting nitric oxide-mediated vascular smooth muscle relaxation. Blood. 2007;109:1945–1952. doi: 10.1182/blood-2006-08-041368. First demonstration that thrombospondin-1 acutely regulates tissue blood flow in vivo by antagonizing nitric oxide signaling and limits tissue survival of ischemic injury. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Isenberg JS, et al. Thrombospondin-1 stimulates platelet aggregation by blocking the antithrombotic activity of nitric oxide/cGMP signaling. Blood. 2008;111:613–623. doi: 10.1182/blood-2007-06-098392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Folkman J. Endogenous angiogenesis inhibitors. Apmis. 2004;112:496–507. doi: 10.1111/j.1600-0463.2004.apm11207-0809.x. [DOI] [PubMed] [Google Scholar]
- 10.Volpert OV, Lawler J, Bouck NP. A human fibrosarcoma inhibits systemic angiogenesis and the growth of experimental metastases via thrombospondin-1. Proc Natl Acad Sci U S A. 1998;95:6343–6348. doi: 10.1073/pnas.95.11.6343. Identified thrombospondin-1 as a circulating angiogenesis inhibitor that limits growth of metastases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamashita Y, Kurohiji T, Tuszynski GP, Sakai T, Shirakusa T. Plasma thrombospondin levels in patients with colorectal carcinoma. Cancer. 1998;82:632–638. doi: 10.1002/(sici)1097-0142(19980215)82:4<632::aid-cncr3>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 12.Nathan FE, et al. Plasma thrombospondin levels in patients with gynecologic malignancies. Cancer. 1994;73:2853–2858. doi: 10.1002/1097-0142(19940601)73:11<2853::aid-cncr2820731131>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 13.Davy H, Davy J. The collected works of Sir Humphry Davy. Smith, Elder and Co; London: 1839. [Google Scholar]
- 14.Ignarro LJ. Nitric oxide as a unique signaling molecule in the vascular system: a historical overview. J Physiol Pharmacol. 2002;53:503–514. [PubMed] [Google Scholar]
- 15.Dudzinski DM, Michel T. Life history of eNOS: partners and pathways. Cardiovasc Res. 2007;75:247–260. doi: 10.1016/j.cardiores.2007.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roy B, Garthwaite J. Nitric oxide activation of guanylyl cyclase in cells revisited. Proc Natl Acad Sci U S A. 2006;103:12185–12190. doi: 10.1073/pnas.0602544103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas DD, et al. The chemical biology of nitric oxide: implications in cellular signaling. Free Radic Biol Med. 2008;45:18–31. doi: 10.1016/j.freeradbiomed.2008.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isenberg JS, et al. Thrombospondin-1 inhibits endothelial cell responses to nitric oxide in a cGMP-dependent manner. Proc Natl Acad Sci U S A. 2005;102:13141–13146. doi: 10.1073/pnas.0502977102. First demonstration that thrombospondin-1 blocks nitric oxide/cGMP signaling in endothelial cells and tissue explants. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radomski MW, Palmer RM, Moncada S. An L-arginine/nitric oxide pathway present in human platelets regulates aggregation. Proc Natl Acad Sci U S A. 1990;87:5193–5197. doi: 10.1073/pnas.87.13.5193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fukumura D, Kashiwagi S, Jain RK. The role of nitric oxide in tumour progression. Nat Rev Cancer. 2006;6:521–534. doi: 10.1038/nrc1910. [DOI] [PubMed] [Google Scholar]
- 21.Fukumura D, et al. Predominant role of endothelial nitric oxide synthase in vascular endothelial growth factor-induced angiogenesis and vascular permeability. Proc Natl Acad Sci U S A. 2001;98:2604–2609. doi: 10.1073/pnas.041359198. Established the critical role in vivo for eNOS in VEGF-stimulated angiogenesis and vascular permeability. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Babaei S, et al. Angiogenic actions of angiopoietin-1 require endothelium-derived nitric oxide. Am J Pathol. 2003;162:1927–1936. doi: 10.1016/S0002-9440(10)64326-X. Extends the critical role of eNOS in angiogenesis beyond VEGF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Urano T, et al. Angiopoietin-related growth factor enhances blood flow via activation of the ERK1/2-eNOS-NO pathway in a mouse hind-limb ischemia model. Arterioscler Thromb Vasc Biol. 2008;28:827–834. doi: 10.1161/ATVBAHA.107.149674. [DOI] [PubMed] [Google Scholar]
- 24.Shindo T, et al. Hypotension and resistance to lipopolysaccharide-induced shock in transgenic mice overexpressing adrenomedullin in their vasculature. Circulation. 2000;101:2309–2316. doi: 10.1161/01.cir.101.19.2309. [DOI] [PubMed] [Google Scholar]
- 25.Babaei S, et al. Role of nitric oxide in the angiogenic response in vitro to basic fibroblast growth factor. Circ Res. 1998;82:1007–1015. doi: 10.1161/01.res.82.9.1007. [DOI] [PubMed] [Google Scholar]
- 26.Rikitake Y, et al. Involvement of endothelial nitric oxide in sphingosine-1-phosphate-induced angiogenesis. Arterioscler Thromb Vasc Biol. 2002;22:108–114. doi: 10.1161/hq0102.101843. [DOI] [PubMed] [Google Scholar]
- 27.Jadeski LC, Lala PK. Nitric oxide synthase inhibition by N(G)-nitro-L-arginine methyl ester inhibits tumor-induced angiogenesis in mammary tumors. Am J Pathol. 1999;155:1381–1390. doi: 10.1016/S0002-9440(10)65240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jadeski LC, Hum KO, Chakraborty C, Lala PK. Nitric oxide promotes murine mammary tumour growth and metastasis by stimulating tumour cell migration, invasiveness and angiogenesis. Int J Cancer. 2000;86:30–39. doi: 10.1002/(sici)1097-0215(20000401)86:1<30::aid-ijc5>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 29.Hussain SP, et al. Nitric oxide is a key component in inflammation-accelerated tumorigenesis. Cancer Res. 2008;68:7130–7136. doi: 10.1158/0008-5472.CAN-08-0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hu DE, Dyke SO, Moore AM, Thomsen LL, Brindle KM. Tumor cell-derived nitric oxide is involved in the immune-rejection of an immunogenic murine lymphoma. Cancer Res. 2004;64:152–161. doi: 10.1158/0008-5472.can-03-1807. [DOI] [PubMed] [Google Scholar]
- 31.Wei D, et al. Direct demonstration of negative regulation of tumor growth and metastasis by host-inducible nitric oxide synthase. Cancer Res. 2003;63:3855–3859. [PubMed] [Google Scholar]
- 32.Ridnour LA, et al. Molecular mechanisms for discrete nitric oxide levels in cancer. Nitric Oxide. 2008;19:73–76. doi: 10.1016/j.niox.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim-Shapiro DB, Schechter AN, Gladwin MT. Unraveling the reactions of nitric oxide, nitrite, and hemoglobin in physiology and therapeutics. Arterioscler Thromb Vasc Biol. 2006;26:697–705. doi: 10.1161/01.ATV.0000204350.44226.9a. [DOI] [PubMed] [Google Scholar]
- 34.Ridnour LA, et al. The chemistry of nitrosative stress induced by nitric oxide and reactive nitrogen oxide species. Putting perspective on stressful biological situations. Biol Chem. 2004;385:1–10. doi: 10.1515/BC.2004.001. [DOI] [PubMed] [Google Scholar]
- 35.Omori K, Kotera J. Overview of PDEs and their regulation. Circ Res. 2007;100:309–327. doi: 10.1161/01.RES.0000256354.95791.f1. [DOI] [PubMed] [Google Scholar]
- 36.Lecour S, et al. Evidence for the extrapulmonary localization of inhaled nitric oxide. Heart Dis. 2003;5:372–377. doi: 10.1097/01.hdx.0000098613.53486.08. [DOI] [PubMed] [Google Scholar]
- 37.Gladwin MT, et al. Inhaled nitric oxide augments nitric oxide transport on sickle cell hemoglobin without affecting oxygen affinity. J Clin Invest. 1999;104:937–945. doi: 10.1172/JCI7637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghiadoni L, Versari D, Taddei S. Phosphodiesterase 5 inhibition in essential hypertension. Curr Hypertens Rep. 2008;10:52–57. doi: 10.1007/s11906-008-0011-4. [DOI] [PubMed] [Google Scholar]
- 39.Dony E, et al. Partial reversal of experimental pulmonary hypertension by phosphodiesterase-3/4 inhibition. Eur Respir J. 2008;31:599–610. doi: 10.1183/09031936.00002007. [DOI] [PubMed] [Google Scholar]
- 40.Voetsch B, Jin RC, Loscalzo J. Nitric oxide insufficiency and atherothrombosis. Histochem Cell Biol. 2004;122:353–367. doi: 10.1007/s00418-004-0675-z. [DOI] [PubMed] [Google Scholar]
- 41.Loscalzo J. Nitric oxide insufficiency, platelet activation, and arterial thrombosis. Circ Res. 2001;88:756–762. doi: 10.1161/hh0801.089861. [DOI] [PubMed] [Google Scholar]
- 42.Carlson CB, Lawler J, Mosher DF. Structures of thrombospondins. Cell Mol Life Sci. 2008;65:672–686. doi: 10.1007/s00018-007-7484-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Posey KL, Yang Y, Veerisetty AC, Sharan SK, Hecht JT. Model systems for studying skeletal dysplasias caused by TSP-5/COMP mutations. Cell Mol Life Sci. 2008;65:687–699. doi: 10.1007/s00018-007-7485-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiao Y, et al. Cartilage oligomeric matrix protein expression in hepatocellular carcinoma and the cirrhotic liver. J Gastroenterol Hepatol. 2004;19:296–302. doi: 10.1111/j.1440-1746.2003.03268.x. [DOI] [PubMed] [Google Scholar]
- 45.Li N, et al. Discovery of novel biomarkers in oral submucous fibrosis by microarray analysis. Cancer Epidemiol Biomarkers Prev. 2008;17:2249–2259. doi: 10.1158/1055-9965.EPI-07-2908. [DOI] [PubMed] [Google Scholar]
- 46.van Doorn R, et al. Epigenetic profiling of cutaneous T-cell lymphoma: promoter hypermethylation of multiple tumor suppressor genes including BCL7a, PTPRG, and p73. J Clin Oncol. 2005;23:3886–3896. doi: 10.1200/JCO.2005.11.353. [DOI] [PubMed] [Google Scholar]
- 47.Korkola JE, et al. Differentiation of lobular versus ductal breast carcinomas by expression microarray analysis. Cancer Res. 2003;63:7167–7175. [PubMed] [Google Scholar]
- 48.Sugimura J, et al. Gene expression profiling of mesoblastic nephroma and Wilms tumors--comparison and clinical implications. Urology. 64:362–368. doi: 10.1016/j.urology.2004.04.052. discussion 368 (2004) [DOI] [PubMed] [Google Scholar]
- 49.Dalla-Torre CA, et al. Effects of THBS3, SPARC and SPP1 expression on biological behavior and survival in patients with osteosarcoma. BMC Cancer. 2006;6:237. doi: 10.1186/1471-2407-6-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kazerounian S, Yee KO, Lawler J. Thrombospondins in cancer. Cell Mol Life Sci. 2008;65:700–712. doi: 10.1007/s00018-007-7486-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bonnefoy A, Moura R, Hoylaerts MF. The evolving role of thrombospondin-1 in hemostasis and vascular biology. Cell Mol Life Sci. 2008;65:713–727. doi: 10.1007/s00018-007-7487-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bergseth G, Lappegard KT, Videm V, Mollnes TE. A novel enzyme immunoassay for plasma thrombospondin. Comparison with beta-thromboglobulin as platelet activation marker in vitro and in vivo. Thromb Res. 2000;99:41–50. doi: 10.1016/s0049-3848(00)00226-7. [DOI] [PubMed] [Google Scholar]
- 53.Italiano JE, Jr, et al. Angiogenesis is regulated by a novel mechanism: pro- and antiangiogenic proteins are organized into separate platelet alpha granules and differentially released. Blood. 2008;111:1227–1233. doi: 10.1182/blood-2007-09-113837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stenina OI, Topol EJ, Plow EF. Thrombospondins, their polymorphisms, and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2007;27:1886–1894. doi: 10.1161/ATVBAHA.107.141713. [DOI] [PubMed] [Google Scholar]
- 55.Kato K, et al. Assessment of genetic risk factors for thoracic aortic aneurysm in hypertensive patients. Am J Hypertens. 2008;21:1023–1027. doi: 10.1038/ajh.2008.229. [DOI] [PubMed] [Google Scholar]
- 56.Koch W, Hoppmann P, de Waha A, Schomig A, Kastrati A. Polymorphisms in thrombospondin genes and myocardial infarction: a case-control study and a meta-analysis of available evidence. Hum Mol Genet. 2008;17:1120–1126. doi: 10.1093/hmg/ddn001. [DOI] [PubMed] [Google Scholar]
- 57.Sfar S, Saad H, Mosbah F, Gabbouj S, Chouchane L. TSP1 and MMP9 genetic variants in sporadic prostate cancer. Cancer Genet Cytogenet. 2007;172:38–44. doi: 10.1016/j.cancergencyto.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 58.Kodama J, et al. Thrombospondin-1 and -2 messenger RNA expression in invasive cervical cancer: correlation with angiogenesis and prognosis. Clin Cancer Res. 2001;7:2826–2831. [PubMed] [Google Scholar]
- 59.Guerrero D, et al. Hypermethylation of the thrombospondin-1 gene is associated with poor prognosis in penile squamous cell carcinoma. BJU Int. 2008;102:747–755. doi: 10.1111/j.1464-410X.2008.07603.x. [DOI] [PubMed] [Google Scholar]
- 60.Neal CP, et al. Molecular prognostic markers in resectable colorectal liver metastases: a systematic review. Eur J Cancer. 2006;42:1728–1743. doi: 10.1016/j.ejca.2006.01.056. [DOI] [PubMed] [Google Scholar]
- 61.Poon RT, et al. Clinical significance of thrombospondin 1 expression in hepatocellular carcinoma. Clin Cancer Res. 2004;10:4150–4157. doi: 10.1158/1078-0432.CCR-03-0435. [DOI] [PubMed] [Google Scholar]
- 62.Straume O, Akslen LA. Expresson of vascular endothelial growth factor, its receptors (FLT-1, KDR) and TSP-1 related to microvessel density and patient outcome in vertical growth phase melanomas. Am J Pathol. 2001;159:223–235. doi: 10.1016/S0002-9440(10)61688-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rice AJ, Steward MA, Quinn CM. Thrombospondin 1 protein expression relates to good prognostic indices in ductal carcinoma in situ of the breast. J Clin Pathol. 2002;55:921–925. doi: 10.1136/jcp.55.12.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tobita K, et al. Thrombospondin-1 expression as a prognostic predictor of pancreatic ductal carcinoma. Int J Oncol. 2002;21:1189–1195. [PubMed] [Google Scholar]
- 65.Hawighorst T, et al. Thrombospondin-2 plays a protective role in multistep carcinogenesis: a novel host anti-tumor defense mechanism. Embo J. 2001;20:2631–2640. doi: 10.1093/emboj/20.11.2631. Established a tumor suppressor activity for TSP2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hawighorst T, et al. Thrombospondin-1 selectively inhibits early-stage carcinogenesis and angiogenesis but not tumor lymphangiogenesis and lymphatic metastasis in transgenic mice. Oncogene. 2002;21:7945–7956. doi: 10.1038/sj.onc.1205956. [DOI] [PubMed] [Google Scholar]
- 67.Li Q, Ahuja N, Burger PC, Issa JP. Methylation and silencing of the Thrombospondin-1 promoter in human cancer. Oncogene. 1999;18:3284–3289. doi: 10.1038/sj.onc.1202663. [DOI] [PubMed] [Google Scholar]
- 68.Yang QW, et al. Methylation-associated silencing of the thrombospondin-1 gene in human neuroblastoma. Cancer Res. 2003;63:6299–6310. [PubMed] [Google Scholar]
- 69.Dameron KM, Volpert OV, Tainsky MA, Bouck N. Control of angiogenesis in fibroblasts by p53 regulation of thrombospondin-1. Science. 1994;265:1582–1584. doi: 10.1126/science.7521539. [DOI] [PubMed] [Google Scholar]
- 70.Janz A, Sevignani C, Kenyon K, Ngo CV, Thomas-Tikhonenko A. Activation of the myc oncoprotein leads to increased turnover of thrombospondin-1 mRNA. Nucleic Acids Res. 2000;28:2268–2275. doi: 10.1093/nar/28.11.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Volpert OV, et al. Id1 regulates angiogenesis through transcriptional repression of thrombospondin-1. Cancer Cell. 2002;2:473–483. doi: 10.1016/s1535-6108(02)00209-x. Established TSP1 as a target for the anti-angiogenic activity of Id1. [DOI] [PubMed] [Google Scholar]
- 72.Zabrenetzky V, Harris CC, Steeg PS, Roberts DD. Expression of the extracellular matrix molecule thrombospondin inversely correlates with malignant progression in melanoma, lung and breast carcinoma cell lines. Int J Cancer. 1994;59:191–195. doi: 10.1002/ijc.2910590209. [DOI] [PubMed] [Google Scholar]
- 73.Shaked Y, et al. Genetic heterogeneity of the vasculogenic phenotype parallels angiogenesis; Implications for cellular surrogate marker analysis of antiangiogenesis. Cancer Cell. 2005;7:101–111. doi: 10.1016/j.ccr.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 74.Weinstat-Saslow DL, et al. Transfection of thrombospondin 1 complementary DNA into a human breast carcinoma cell line reduces primary tumor growth, metastatic potential, and angiogenesis. Cancer Res. 1994;54:6504–6511. First demonstration that re-expressing thrombospondin-1 in a tumor xenograft model inhibits tumor growth and angiogenesis. [PubMed] [Google Scholar]
- 75.Sheibani N, Frazier WA. Thrombospondin 1 expression in transformed endothelial cells restores a normal phenotype and suppresses their tumorigenesis. Proc Natl Acad Sci U S A. 1995;92:6788–6792. doi: 10.1073/pnas.92.15.6788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Streit M, et al. Overexpression of thrombospondin-1 decreases angiogenesis and inhibits the growth of human cutaneous squamous cell carcinomas. Am J Pathol. 1999;155:441–452. doi: 10.1016/S0002-9440(10)65140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Streit M, et al. Thrombospondin-2: a potent endogenous inhibitor of tumor growth and angiogenesis. Proc Natl Acad Sci U S A. 1999;96:14888–14893. doi: 10.1073/pnas.96.26.14888. First demonstration that expressing thrombospondin-2 inhibits tumor angiogenesis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guo NH, Krutzsch HC, Inman JK, Shannon CS, Roberts DD. Antiproliferative and antitumor activities of D-reverse peptides derived from the second type-1 repeat of thrombospondin-1. J Pept Res. 1997;50:210–221. doi: 10.1111/j.1399-3011.1997.tb01187.x. [DOI] [PubMed] [Google Scholar]
- 79.Iruela-Arispe ML, Lombardo M, Krutzsch HC, Lawler J, Roberts DD. Inhibition of angiogenesis by thrombspondin-1 is mediated by two independent regions within the type 1 repeats. Circulation. 1999;100:1423–1431. doi: 10.1161/01.cir.100.13.1423. [DOI] [PubMed] [Google Scholar]
- 80.Haviv F, et al. Thrombospondin-1 mimetic peptide inhibitors of angiogenesis and tumor growth: design, synthesis, and optimization of pharmacokinetics and biological activities. J Med Chem. 2005;48:2838–2846. doi: 10.1021/jm0401560. Development of a potent thrombospondin-1 mimetic drug that inhibits tumor growth. [DOI] [PubMed] [Google Scholar]
- 81.Ebbinghaus S, et al. Phase 2 study of ABT-510 in patients with previously untreated advanced renal cell carcinoma. Clin Cancer Res. 2007;13:6689–6695. doi: 10.1158/1078-0432.CCR-07-1477. [DOI] [PubMed] [Google Scholar]
- 82.Markovic SN, et al. A phase II study of ABT-510 (thrombospondin-1 analog) for the treatment of metastatic melanoma. Am J Clin Oncol. 2007;30:303–309. doi: 10.1097/01.coc.0000256104.80089.35. [DOI] [PubMed] [Google Scholar]
- 83.Yap R, et al. Metronomic low-dose chemotherapy boosts CD95-dependent antiangiogenic effect of the thrombospondin peptide ABT-510: a complementation antiangiogenic strategy. Clin Cancer Res. 2005;11:6678–6685. doi: 10.1158/1078-0432.CCR-05-0621. [DOI] [PubMed] [Google Scholar]
- 84.Gietema JA, et al. A phase I study assessing the safety and pharmacokinetics of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 with gemcitabine and cisplatin in patients with solid tumors. Ann Oncol. 2006;17:1320–1327. doi: 10.1093/annonc/mdl102. [DOI] [PubMed] [Google Scholar]
- 85.Hoekstra R, et al. Phase I study of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 with 5-fluorouracil and leucovorin: a safe combination. Eur J Cancer. 2006;42:467–472. doi: 10.1016/j.ejca.2005.08.040. [DOI] [PubMed] [Google Scholar]
- 86.Baker LH, et al. Randomized, phase II study of the thrombospondin-1-mimetic angiogenesis inhibitor ABT-510 in patients with advanced soft tissue sarcoma. J Clin Oncol. 2008;26:5583–5588. doi: 10.1200/JCO.2008.17.4706. [DOI] [PubMed] [Google Scholar]
- 87.Taraboletti G, Roberts D, Liotta LA, Giavazzi R. Platelet thrombospondin modulates endothelial cell adhesion, motility, and growth: a potential angiogenesis regulatory factor. J Cell Biol. 1990;111:765–772. doi: 10.1083/jcb.111.2.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tolsma SS, et al. Peptides derived from two separate domains of the matrix protein thrombospondin-1 have anti-angiogenic activity. J Cell Biol. 1993;122:497–511. doi: 10.1083/jcb.122.2.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Isenberg JS, Wink DA, Roberts DD. Thrombospondin-1 antagonizes nitric oxide-stimulated vascular smooth muscle cell responses. Cardiovasc Res. 2006;71:785–793. doi: 10.1016/j.cardiores.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 90.Isenberg JS, et al. Thrombospondin-1 and vasoactive agents indirectly alter tumor blood flow. Neoplasia. 2008;10:886–896. doi: 10.1593/neo.08264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Isenberg JS, Frazier WA, Roberts DD. Thrombospondin-1: a physiological regulator of nitric oxide signaling. Cell Mol Life Sci. 2008;65:728–742. doi: 10.1007/s00018-007-7488-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dawson DW, et al. CD36 mediates the In vitro inhibitory effects of thrombospondin-1 on endothelial cells. J Cell Biol. 1997;138:707–717. doi: 10.1083/jcb.138.3.707. Established the role of CD36 as a receptor that mediates anti-angiogenic responses to thrombospondin-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jimenez B, et al. Signals leading to apoptosis-dependent inhibition of neovascularization by thrombospondin-1. Nat Med. 2000;6:41–48. doi: 10.1038/71517. [DOI] [PubMed] [Google Scholar]
- 94.Isenberg JS, et al. CD47 is necessary for inhibition of nitric oxide-stimulated vascular cell responses by thrombospondin-1. J Biol Chem. 2006;281:26069–26080. doi: 10.1074/jbc.M605040200. Established that CD47, not CD36, is the critical receptor for inhibition of nitric oxide/cGMP signaling in vascular cells. [DOI] [PubMed] [Google Scholar]
- 95.Ambati BK, et al. Corneal avascularity is due to soluble VEGF receptor-1. Nature. 2006;443:993–997. doi: 10.1038/nature05249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Isenberg JS, Yu C, Roberts DD. Differential effects of ABT-510 and a CD36-binding peptide derived from the type 1 repeats of thrombospondin-1 on fatty acid uptake, nitric oxide signaling, and caspase activation in vascular cells. Biochem Pharmacol. 2008;75:875–882. doi: 10.1016/j.bcp.2007.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brown EJ, Frazier WA. Integrin-associated protein (CD47) and its ligands. Trends Cell Biol. 2001;11:130–135. doi: 10.1016/s0962-8924(00)01906-1. [DOI] [PubMed] [Google Scholar]
- 98.Isenberg JS, et al. Blocking thrombospondin-1/CD47 signaling alleviates deleterious effects of aging on tissue responses to ischemia. Arterioscler Thromb Vasc Biol. 2007;27:2582–2588. doi: 10.1161/ATVBAHA.107.155390. [DOI] [PubMed] [Google Scholar]
- 99.Isenberg JS, et al. Gene silencing of CD47 and antibody ligation of thrombospondin-1 enhance ischemic tissue survival in a porcine model: implications for human disease. Ann Surg. 2008;247:860–868. doi: 10.1097/SLA.0b013e31816c4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pyriochou A, Papapetropoulos A. Soluble guanylyl cyclase: more secrets revealed. Cell Signal. 2005;17:407–413. doi: 10.1016/j.cellsig.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 101.Jackson EB, Jr, Mukhopadhyay S, Tulis DA. Pharmacologic modulators of soluble guanylate cyclase/cyclic guanosine monophosphate in the vascular system - from bench top to bedside. Curr Vasc Pharmacol. 2007;5:1–14. [PubMed] [Google Scholar]
- 102.Butt E, et al. cAMP- and cGMP-dependent protein kinase phosphorylation sites of the focal adhesion vasodilator-stimulated phosphoprotein (VASP) in vitro and in intact human platelets. J Biol Chem. 1994;269:14509–14517. [PubMed] [Google Scholar]
- 103.Zhu W, Smart EJ. Myristic acid stimulates endothelial nitric-oxide synthase in a CD36- and an AMP kinase-dependent manner. J Biol Chem. 2005;280:29543–29550. doi: 10.1074/jbc.M501238200. [DOI] [PubMed] [Google Scholar]
- 104.Febbraio M, Silverstein RL. CD36: implications in cardiovascular disease. Int J Biochem Cell Biol. 2007;39:2012–2030. doi: 10.1016/j.biocel.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Isenberg JS, et al. Thrombospondin-1 inhibits nitric oxide signaling via CD36 by inhibiting myristic acid uptake. J Biol Chem. 2007;282:15404–15415. doi: 10.1074/jbc.M701638200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gao A-G, et al. Integrin-associated protein is a receptor for the C-terminal domain of thrombospondin. J Biol Chem. 1996;271:21–24. doi: 10.1074/jbc.271.1.21. Identified CD47 as a thrombospondin-1 receptor. [DOI] [PubMed] [Google Scholar]
- 107.Lamy L, et al. Interactions between CD47 and thrombospondin reduce inflammation. J Immunol. 2007;178:5930–5939. doi: 10.4049/jimmunol.178.9.5930. [DOI] [PubMed] [Google Scholar]
- 108.Isenberg JS, et al. Differential interactions of thrombospondins-1, -2 and -4 with CD47 and effects on cGMP signaling and ischemic injury responses. J Biol Chem. 2009;284:1116–1125. doi: 10.1074/jbc.M804860200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Dewhirst MW, Cao Y, Moeller B. Cycling hypoxia and free radicals regulate angiogenesis and radiotherapy response. Nat Rev Cancer. 2008;8:425–437. doi: 10.1038/nrc2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Isenberg JS, et al. Blockade of thrombospondin-1-CD47 interactions prevents necrosis of full thickness skin grafts. Ann Surg. 2008;247:180–190. doi: 10.1097/SLA.0b013e31815685dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Isenberg JS, et al. Increasing survival of ischemic tissue by targeting CD47. Circ Res. 2007;100:712–720. doi: 10.1161/01.RES.0000259579.35787.4e. [DOI] [PubMed] [Google Scholar]
- 112.Lien YH, Lai LW, Silva AL. Pathogenesis of renal ischemia/reperfusion injury: lessons from knockout mice. Life Sci. 2003;74:543–552. doi: 10.1016/j.lfs.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 113.Isenberg JS, et al. Treatment of ischemia/reperfusion injury by limiting thrombospondin-1/CD47 signaling. Surgery. 2008;144:752–761. doi: 10.1016/j.surg.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Baluk P, Hashizume H, McDonald DM. Cellular abnormalities of blood vessels as targets in cancer. Curr Opin Genet Dev. 2005;15:102–111. doi: 10.1016/j.gde.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 115.Jain RK. Haemodynamic and transport barriers to the treatment of solid tumours. Int J Radiat Biol. 1991;60:85–100. doi: 10.1080/09553009114551621. [DOI] [PubMed] [Google Scholar]
- 116.Dewhirst MW, et al. The use of hydralazine to manipulate tumour temperatures during hyperthermia. Int J Hyperthermia. 1990;6:971–983. doi: 10.3109/02656739009140980. [DOI] [PubMed] [Google Scholar]
- 117.Shankar A, Loizidou M, Burnstock G, Taylor I. Noradrenaline improves the tumour to normal blood flow ratio and drug delivery in a model of liver metastases. Br J Surg. 1999;86:453–457. doi: 10.1046/j.1365-2168.1999.01045.x. [DOI] [PubMed] [Google Scholar]
- 118.Jirtle RL. Chemical modification of tumour blood flow. Int J Hyperthermia. 1988;4:355–371. doi: 10.3109/02656738809016490. [DOI] [PubMed] [Google Scholar]
- 119.Morikawa S, et al. Abnormalities in pericytes on blood vessels and endothelial sprouts in tumors. Am J Pathol. 2002;160:985–1000. doi: 10.1016/S0002-9440(10)64920-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thachil J. Nitric oxide depletion is responsible for the adverse effects of vascular endothelial growth factor inhibitors. Nat Clin Pract Nephrol. 2008 doi: 10.1038/ncpneph0907. [DOI] [PubMed] [Google Scholar]
- 121.Urbich C, et al. Dephosphorylation of endothelial nitric oxide synthase contributes to the anti-angiogenic effects of endostatin. Faseb J. 2002;16:706–708. doi: 10.1096/fj.01-0637fje. [DOI] [PubMed] [Google Scholar]
- 122.Schmidt A, et al. Endostatin down-regulates soluble guanylate cyclase (sGC) in endothelial cells in vivo: influence of endostatin on vascular endothelial growth factor (VEGF) signaling. Endothelium. 2005;12:251–257. doi: 10.1080/10623320500476690. [DOI] [PubMed] [Google Scholar]
- 123.Goymer P. Natural selection: The evolution of cancer. Nature. 2008;454:1046–1048. doi: 10.1038/4541046a. [DOI] [PubMed] [Google Scholar]
- 124.Ludwig RJ, Schon MP, Boehncke WH. P-selectin: a common therapeutic target for cardiovascular disorders, inflammation and tumour metastasis. Expert Opin Ther Targets. 2007;11:1103–1117. doi: 10.1517/14728222.11.8.1103. [DOI] [PubMed] [Google Scholar]
- 125.Yee KO, et al. The effect of thrombospondin-1 on breast cancer metastasis. Breast Cancer Res Treat. 2008 Apr 13; doi: 10.1007/s10549-008-9992-6. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nieder C, Wiedenmann N, Andratschke NH, Astner ST, Molls M. Radiation therapy plus angiogenesis inhibition with bevacizumab: rationale and initial experience. Rev Recent Clin Trials. 2007;2:163–168. doi: 10.2174/157488707781662733. [DOI] [PubMed] [Google Scholar]
- 127.Kashiwagi S, et al. Perivascular nitric oxide gradients normalize tumor vasculature. Nat Med. 2008;14:255–257. doi: 10.1038/nm1730. [DOI] [PubMed] [Google Scholar]
- 128.Moeller BJ, Richardson RA, Dewhirst MW. Hypoxia and radiotherapy: opportunities for improved outcomes in cancer treatment. Cancer Metastasis Rev. 2007;26:241–248. doi: 10.1007/s10555-007-9056-0. [DOI] [PubMed] [Google Scholar]
- 129.Dings RP, et al. Scheduling of radiation with angiogenesis inhibitors anginex and Avastin improves therapeutic outcome via vessel normalization. Clin Cancer Res. 2007;13:3395–3402. doi: 10.1158/1078-0432.CCR-06-2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Garcia-Barros M, et al. Tumor response to radiotherapy regulated by endothelial cell apoptosis. Science. 2003;300:1155–1159. doi: 10.1126/science.1082504. [DOI] [PubMed] [Google Scholar]
- 131.Ogawa K, et al. Influence of tumor cell and stroma sensitivity on tumor response to radiation. Cancer Res. 2007;67:4016–4021. doi: 10.1158/0008-5472.CAN-06-4498. [DOI] [PubMed] [Google Scholar]
- 132.Gerweck LE, Vijayappa S, Kurimasa A, Ogawa K, Chen DJ. Tumor cell radiosensitivity is a major determinant of tumor response to radiation. Cancer Res. 2006;66:8352–8355. doi: 10.1158/0008-5472.CAN-06-0533. [DOI] [PubMed] [Google Scholar]
- 133.Isenberg JS, et al. Thrombospondin-1 and CD47 limit cell and tissue survival of radiation injury. Am J Pathol. 2008;173:1100–1112. doi: 10.2353/ajpath.2008.080237. Demonstrates key roles of thrombospondin-1 and CD47 in radiosensitivity of soft tissue in vivo and vascular cells in vitro. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Agah A, Kyriakides TR, Lawler J, Bornstein P. The lack of thrombospondin-1 (TSP1) dictates the course of wound healing in double-TSP1/TSP2-null mice. Am J Pathol. 2002;161:831–839. doi: 10.1016/S0002-9440(10)64243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Liebmann J, et al. In vivo radiation protection by nitric oxide modulation. Cancer Res. 1994;54:3365–3368. Established a radioprotective activity of nitric oxide. [PubMed] [Google Scholar]
- 136.Isenberg JS, et al. Thrombospondin-1 and CD47 regulate blood pressure and cardiovascular responses to vasoactive stress. Matrix Biol. 2009 in press. [Google Scholar]
- 137.Martin-Manso G, et al. Thrombospondin-1 promotes tumor macrophage recruitment and enhances tumor cell cytotoxicity by differentiated U937 cells. Cancer Res. 2008;68:7090–7099. doi: 10.1158/0008-5472.CAN-08-0643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Munder M, Eichmann K, Modolell M. Alternative metabolic states in murine macrophages reflected by the nitric oxide synthase/arginase balance: competitive regulation by CD4+ T cells correlates with Th1/Th2 phenotype. J Immunol. 1998;160:5347–5354. [PubMed] [Google Scholar]
- 139.Cao C, et al. Endocytic receptor LRP together with tPA and PAI-1 coordinates Mac-1-dependent macrophage migration. Embo J. 2006;25:1860–1870. doi: 10.1038/sj.emboj.7601082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Degryse B, et al. The low density lipoprotein receptor-related protein is a motogenic receptor for plasminogen activator inhibitor-1. J Biol Chem. 2004;279:22595–22604. doi: 10.1074/jbc.M313004200. [DOI] [PubMed] [Google Scholar]
- 141.Chandrasekaran L, et al. Cell contact-dependent activation of α3β1 integrin modulates endothelial cell responses to thrombospondin-1. Mol Biol Cell. 2000;11:2885–2900. doi: 10.1091/mbc.11.9.2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Taraboletti G, et al. The heparin binding 25 kDa fragment of thrombospondin-1 promotes angiogenesis and modulates gelatinase and TIMP-2 production in endothelial cells. FASEB J. 2000;14:1674–1676. doi: 10.1096/fj.99-0931fje. [DOI] [PubMed] [Google Scholar]
- 143.Calzada MJ, et al. Recognition of the N-terminal modules of thrombospondin-1 and thrombospondin-2 by α6β1 integrin. J Biol Chem. 2003;278:40679–40687. doi: 10.1074/jbc.M302014200. [DOI] [PubMed] [Google Scholar]
- 144.Calzada MJ, et al. α4β1 integrin mediates selective endothelial cell responses to thrombospondins in vitro and modulates angiogenesis in vivo. Circ Res. 2004;94:462–470. doi: 10.1161/01.RES.0000115555.05668.93. [DOI] [PubMed] [Google Scholar]
- 145.Staniszewska I, et al. Interaction of alpha9beta1 integrin with thrombospondin-1 promotes angiogenesis. Circ Res. 2007;100:1308–1316. doi: 10.1161/01.RES.0000266662.98355.66. [DOI] [PubMed] [Google Scholar]
- 146.Elzie CA, Murphy-Ullrich JE. The N-terminus of thrombospondin: the domain stands apart. Int J Biochem Cell Biol. 2004;36:1090–1101. doi: 10.1016/j.biocel.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 147.Liu A, Mosher DF, Murphy-Ullrich JE, Goldblum SE. The counteradhesive proteins, thrombospondin 1 and SPARC/osteonectin, open the tyrosine phosphorylation-responsive paracellular pathway in pulmonary vascular endothelia. Microvasc Res. 2008 Oct 1; doi: 10.1016/j.mvr.2008.08.008. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Simantov R, Febbraio M, Silverstein RL. The antiangiogenic effect of thrombospondin-2 is mediated by CD36 and modulated by histidine-rich glycoprotein. Matrix Biol. 2005;24:27–34. doi: 10.1016/j.matbio.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 149.Huang H, et al. Peroxisome proliferator-activated receptor gamma ligands improve the antitumor efficacy of thrombospondin peptide ABT510. Mol Cancer Res. 2004;2:541–550. [PubMed] [Google Scholar]
- 150.Kuriki K, et al. Increased risk of colorectal cancer due to interactions between meat consumption and the CD36 gene A52C polymorphism among Japanese. Nutr Cancer. 2005;51:170–177. doi: 10.1207/s15327914nc5102_7. [DOI] [PubMed] [Google Scholar]
- 151.McDonald JF, Dimitry JM, Frazier WA. An amyloid-like C-terminal domain of thrombospondin-1 displays CD47 agonist activity requiring both VVM motifs. Biochemistry. 2003;42:10001–10011. doi: 10.1021/bi0341408. [DOI] [PubMed] [Google Scholar]
- 152.Kvansakul M, Adams JC, Hohenester E. Structure of a thrombospondin C-terminal fragment reveals a novel calcium core in the type 3 repeats. Embo J. 2004;23:1223–1233. doi: 10.1038/sj.emboj.7600166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Floquet N, Dedieu S, Martiny L, Dauchez M, Perahia D. Human thrombospondin’s (TSP-1) C-terminal domain opens to interact with the CD-47 receptor: a molecular modeling study. Arch Biochem Biophys. 2008;478:103–109. doi: 10.1016/j.abb.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 154.van Beek EM, Cochrane F, Barclay AN, van den Berg TK. Signal regulatory proteins in the immune system. J Immunol. 2005;175:7781–7787. doi: 10.4049/jimmunol.175.12.7781. [DOI] [PubMed] [Google Scholar]
- 155.Kikuchi Y, et al. Apoptosis inducing bivalent single-chain antibody fragments against CD47 showed antitumor potency for multiple myeloma. Leuk Res. 2005;29:445–450. doi: 10.1016/j.leukres.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 156.Manna PP, Frazier WA. CD47 mediates killing of breast tumor cells via Gi-dependent inhibition of protein kinase A. Cancer Res. 2004;64:1026–1036. doi: 10.1158/0008-5472.can-03-1708. [DOI] [PubMed] [Google Scholar]
- 157.Dimmeler S, et al. Activation of nitric oxide synthase in endothelial cells by Akt-dependent phosphorylation. Nature. 1999;399:601–605. doi: 10.1038/21224. [DOI] [PubMed] [Google Scholar]
- 158.Fulton D, et al. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Fulton D, et al. Agonist-stimulated endothelial nitric oxide synthase activation and vascular relaxation. Role of eNOS phosphorylation at Tyr83. Circ Res. 2008;102:497–504. doi: 10.1161/CIRCRESAHA.107.162933. [DOI] [PubMed] [Google Scholar]
- 160.Duval M, Le Boeuf F, Huot J, Gratton JP. Src-mediated phosphorylation of Hsp90 in response to vascular endothelial growth factor (VEGF) is required for VEGF receptor-2 signaling to endothelial NO synthase. Mol Biol Cell. 2007;18:4659–4668. doi: 10.1091/mbc.E07-05-0467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Reihill JA, Ewart MA, Hardie DG, Salt IP. AMP-activated protein kinase mediates VEGF-stimulated endothelial NO production. Biochem Biophys Res Commun. 2007;354:1084–1088. doi: 10.1016/j.bbrc.2007.01.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Anderson JC, et al. ABT-510, a modified type 1 repeat peptide of thrombospondin, inhibits malignant glioma growth in vivo by inhibiting angiogenesis. Cancer Biol Ther. 2007;6:454–462. doi: 10.4161/cbt.6.3.3630. [DOI] [PubMed] [Google Scholar]
- 163.Lawler J, et al. Thrombospondin-1 gene expression affects survival and tumor spectrum of p53-deficient mice. Am J Pathol. 2001;159:1949–1956. doi: 10.1016/S0002-9440(10)63042-8. First demonstration that endogenous thrombospondin-1 limits tumor growth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Rodriguez-Manzaneque JC, et al. Thrombospondin-1 suppresses spontaneous tumor growth and inhibits activation of matrix metalloproteinase-9 and mobilization of vascular endothelial growth factor. Proc Natl Acad Sci U S A. 2001;98:12485–12490. doi: 10.1073/pnas.171460498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Johnson AM, et al. Androgenic dependence of exophytic tumor growth in a transgenic mouse model of bladder cancer: a role for thrombospondin-1. BMC Urol. 2008;8:7. doi: 10.1186/1471-2490-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bocci G, Francia G, Man S, Lawler J, Kerbel RS. Thrombospondin 1, a mediator of the antiangiogenic effects of low-dose metronomic chemotherapy. Proc Natl Acad Sci U S A. 2003;100:12917–12922. doi: 10.1073/pnas.2135406100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Maeda K, et al. Expression of vascular endothelial growth factor and thrombospondin-1 in colorectal carcinoma. Int J Mol Med. 2000;5:373–378. doi: 10.3892/ijmm.5.4.373. [DOI] [PubMed] [Google Scholar]
- 168.Maeda K, et al. Expression of thrombospondin-1 inversely correlated with tumor vascularity and hematogenous metastasis in colon cancer. Oncol Rep. 2001;8:763–766. doi: 10.3892/or.8.4.763. [DOI] [PubMed] [Google Scholar]
- 169.Kawakami T, et al. Interleukin 10 expression is correlated with thrombospondin expression and decreased vascular involvement in colon cancer. Int J Oncol. 2001;18:487–491. doi: 10.3892/ijo.18.3.487. [DOI] [PubMed] [Google Scholar]
- 170.Yoshida Y, et al. Expression of angiostatic factors in colorectal cancer. Int J Oncol. 1999;15:1221–1225. doi: 10.3892/ijo.15.6.1221. [DOI] [PubMed] [Google Scholar]
- 171.Kaio E, et al. Clinical significance of thrombospondin-1 expression in relation to vascular endothelial growth factor and interleukin-10 expression at the deepest invasive tumor site of advanced colorectal carcinoma. Int J Oncol. 2003;23:901–911. [PubMed] [Google Scholar]
- 172.Bodner-Adler B, et al. Expression of thrombospondin 1 (TSP 1) in patients with uterine smooth muscle tumors: an immunohistochemical study. Gynecol Oncol. 2006;103:186–189. doi: 10.1016/j.ygyno.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 173.Straume O, Akslen LA. Strong expression of ID1 protein is associated with decreased survival, increased expression of ephrin-A1/EPHA2, and reduced thrombospondin-1 in malignant melanoma. Br J Cancer. 2005;93:933–938. doi: 10.1038/sj.bjc.6602792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Vallbo C, Wang W, Damber JE. The expression of thrombospondin-1 in benign prostatic hyperplasia and prostatic intraepithelial neoplasia is decreased in prostate cancer. BJU Int. 2004;93:1339–1343. doi: 10.1111/j.1464-410x.2004.04818.x. [DOI] [PubMed] [Google Scholar]
- 175.Paydas S, et al. Thrombospondin-1 (TSP-1) and Survivin (S) expression in non-Hogkin’s lymphomas. Leuk Res. 2008;32:243–250. doi: 10.1016/j.leukres.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 176.Sutton CD, et al. Expression of thrombospondin-1 in resected colorectal liver metastases predicts poor prognosis. Clin Cancer Res. 2005;11:6567–6573. doi: 10.1158/1078-0432.CCR-05-0439. [DOI] [PubMed] [Google Scholar]
- 177.Tringler B, et al. Immunohistochemical expression of thrombospondin-1 in invasive vulvar squamous cell carcinoma. Gynecol Oncol. 2005;99:80–83. doi: 10.1016/j.ygyno.2005.05.038. [DOI] [PubMed] [Google Scholar]
- 178.Karavasilis V, et al. Clinicopathologic study of vascular endothelial growth factor, thrombospondin-1, and microvessel density assessed by CD34 in patients with stage III ovarian carcinoma. Int J Gynecol Cancer. 2006;16 (Suppl 1):241–246. doi: 10.1111/j.1525-1438.2006.00316.x. [DOI] [PubMed] [Google Scholar]
- 179.Linderholm B, Lindh B, Tavelin B, Grankvist K, Henriksson R. p53 and vascular-endothelial-growth-factor (VEGF) expression predicts outcome in 833 patients with primary breast carcinoma. Int J Cancer. 2000;89:51–62. [PubMed] [Google Scholar]
- 180.Siegel AB, et al. Phase II trial evaluating the clinical and biologic effects of bevacizumab in unresectable hepatocellular carcinoma. J Clin Oncol. 2008;26:2992–2998. doi: 10.1200/JCO.2007.15.9947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Nalluri SR, Chu D, Keresztes R, Zhu X, Wu S. Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. Jama. 2008;300:2277–2285. doi: 10.1001/jama.2008.656. [DOI] [PubMed] [Google Scholar]
- 182.Jain M, Townsend RR. Chemotherapy agents and hypertension: a focus on angiogenesis blockade. Curr Hypertens Rep. 2007;9:320–328. doi: 10.1007/s11906-007-0058-7. [DOI] [PubMed] [Google Scholar]
- 183.Patel TV, et al. A preeclampsia-like syndrome characterized by reversible hypertension and proteinuria induced by the multitargeted kinase inhibitors sunitinib and sorafenib. J Natl Cancer Inst. 2008;100:282–284. doi: 10.1093/jnci/djm311. [DOI] [PubMed] [Google Scholar]
- 184.Steeghs N, et al. Hypertension and rarefaction during treatment with telatinib, a small molecule angiogenesis inhibitor. Clin Cancer Res. 2008;14:3470–3476. doi: 10.1158/1078-0432.CCR-07-5050. [DOI] [PubMed] [Google Scholar]