The Revised Direct Assessment of Functional Status for Independent Older Adults (original) (raw)
Abstract
Purpose: The original version of the Direct Assessment of Functional Status (DAFS), a measure of instrumental activities of daily living (IADLs), was found to have a ceiling effect in older adults living independently in the community. This suggested that the tasks measured, although relevant, do not require full use of this population’s abilities, and thus, the instrument may not be sensitive to the early decrements in IADLs that can signal initial cognitive impairment and may not detect improvements in IADLs over time, which is especially important in intervention research. Design and Methods: By removing items with little to no variation and adding more difficult subscales that emphasized medication management skills, we designed the DAFS-Extended (Direct Assessment of Functional Status-Revised [DAFS-R]) to be more challenging for elders living independently. Results: Analysis with a sample of 45 older adults suggested that scores on the DAFS-R appear to be more normally distributed than on the original version. The DAFS was able to differentiate individuals with varying standard profile scores on the Rivermead Behavioural Memory Test memory performance instrument (normal, poor, and impaired). In addition, the reliability and validity of the DAFS-R were supported in this sample. Implications: Given the large number of older adults who regularly take multiple prescription medications, deficits in medication management skills can have serious consequences. A performance measure that emphasizes these higher level daily living skills can help providers screen for initial signs of functional decline.
Keywords: Older adults, Methodological, Performance-based instrumental activities
Successful performance of instrumental activities of daily living (IADLs) such as taking medications, managing money, and using a telephone requires intact executive function to sequence tasks, make appropriate judgments, and organize abilities (Bell-McGinty, Podell, Franzen, Baird, & Williams, 2002; Bertrand, Willis, & Sayer, 2001; Burton, Strauss, Hultsch, & Hunter, 2006; Dodge, Du, Saxton, & Ganguli, 2006; Insel, Morrow, Brewer, & Figueredo, 2006). In addition to executive function, physical disabilities, sensory impairment, medical conditions, emotional status, and perceived health status are also important predictors of functional capacity (Cahn-Weiner, Malloy, Boyle, Marran, & Salloway, 2000; Marcopulos, McLain, & Guiliano, 1997). Early measures of instrumental activities were self-reported; however, with concerns about the accuracy of these self-reports, actual observation of performance has increased (Diehl, Marsiske, Horgas, & Saczynski, 1998; Diehl, Willis, & Schaie, 1995; Lawton, 1988; Lawton & Brody, 1969).
Managing medications is an important daily task for older adults. In fact, 90% of adults aged 65 years and older take at least 1 prescription medication per week, 40% take at least 5 different medications, and 12% are taking more than 10 types of medications per week (Gurwitz et al., 2003; Zhan et al., 2001). Several available measures of IADL include medication management; however, many are self-report and require only recall (Diehl et al., 1998; Mahurin, DeBettignies, & Pirozzolo, 1991). For example, in the Physical Functioning Inventory, participants are asked how they would obtain medication and whether they have any difficulty taking them (Whetstone et al., 2001), and the timed IADL test requires participants to correctly identify and read the label on a medication bottle in a limited time (Edwards et al., 2005). Assessment of medication skills is limited on most performance measures; however, a measure is needed that more clearly reflects the skills required to manage multiple medications.
The Direct Assessment of Functional Status
The Direct Assessment of Functional Status (DAFS; Loewenstein et al., 1989) has been used to assess the functional status of older adults and their ability to successfully complete IADLs. The 85-item DAFS measures participants’ time orientation, communication abilities, transportation knowledge, financial skills, shopping skills, eating skills, and dressing/grooming skills and is administered in outpatient settings. The DAFS has been shown to have high interrater and test–rest reliability among patients identified as possibly having memory disorders and among normal controls. Validity was supported by the significant differences in scores between patients diagnosed with Alzheimer’s disease and individuals without cognitive impairment (CI). In addition, DAFS scores were negatively related to scores on the Blessed Dementia Rating Scale among 30 patients with memory impairment. A modified version of the DAFS tested with community elders has been found sensitive to level of cognitive function and dementia (Rankin & Keefover, 1998).
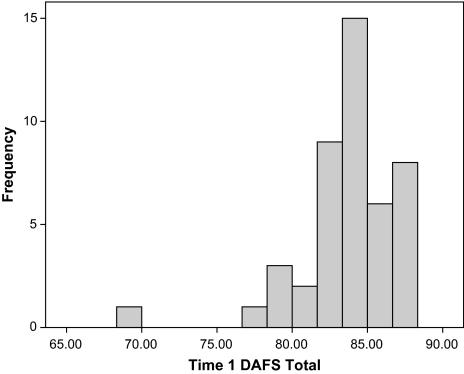
In our SeniorWISE study (McDougall et al., in press) with 265 independent older adults who were screened out for dementia, we found that the DAFS (even excluding the eating and dressing/grooming skills subscales) had a nonnormal distribution on the first administration before intervention or opportunity to practice completing the instrument and also showed a ceiling effect. We used the modified version to take into account the lack of kitchen and bathroom facilities in the evaluation rooms at study sites. The domains measured from the DAFS in this study were time orientation, communication abilities, transportation, financial skills, and shopping skills. A fifth domain, medication skills, was added for the study. Medication skills with three sections (identifying, refilling, and managing medications) was added to more fully capture cognitive tasks that are important for living independently in older age (Table 1 shows the mean, minimum, and maximum scores when administered at baseline in the SeniorWISE study). That is, scores on the DAFS were skewed to the upper end of the distribution (see Figure 1). Furthermore, item analysis of the DAFS showed that many of the items had little to no variation, and participants scored very high despite the fact that two thirds scored in the poor or impaired ranges on the Rivermead test of everyday memory performance (Wilson, Cockburn, & Baddeley, 1991). This pattern of results suggested that the DAFS might not be sensitive to the early deficits in functioning exhibited by older adults experiencing poor memory performance but are still living independently in the community.
Table 1.
Subscale and Total Score Information for the Modified DAFS Subscale used in the SeniorWISE Study
| Number of items | M | SD | Minimum–maximum | |
|---|---|---|---|---|
| Telling timea | 4 | 7.79 | 0.79 | 2–8 |
| Time orientationa | 4 | 7.60 | 0.92 | 2–8 |
| Phone usage | 8 | 7.37 | 0.66 | 5–8 |
| Preparing a letter | 6 | 5.63 | 0.87 | 2–6 |
| Transportation | 13 | 12.17 | 1.30 | 2–13 |
| Counting currency | 11 | 10.89 | 0.39 | 9–11 |
| Writing a check | 5 | 4.89 | 0.51 | 0–5 |
| Making change | 1 | 0.89 | 0.32 | 0–1 |
| Balancing a checkbook | 4 | 3.12 | 1.18 | 0–4 |
| Shopping recall | 6 | 3.37 | 1.14 | 0–6 |
| Shopping recognition | 10 | 8.58 | 1.14 | 4–10 |
| Medication management | 10 | 9.69 | 0.74 | 4–10 |
| T1 DAFS total score | 82/12b | |||
| Alpha = .73 | 81.99 | 5.34 | 46–89 |
Figure 1.
Frequency histogram of scores on the 85-item Direct Assessment of Functional Status (DAFS) at Time 1 of the SeniorWISE study for the 45 individuals in the present study.
We concluded that a more challenging assessment was needed to test the upper limit of the older adults’ skills and detect initial deficits in IADLs that might signal the need for more extensive testing of cognitive function. Also, because correct use of medications is so important for remaining independent, we decided that medication management skills should receive greater emphasis. Consequently, we modified the DAFS and tested the modified version with a subset of SeniorWISE participants approximately 2 years after they completed the study. We revised the instrument with the approval of Dr. David Lowenstein and then examined the psychometric properties of the Direct Assessment of Functional Status-Revised (DAFS-R). This article describes our revision of the DAFS and presents our initial findings on the score distribution, reliability, and validity of the new instrument.
Methods
Revision of the Original DAFS
The four “telling time” items on the original DAFS exhibited relatively little variability on each of these items, between 253 and 263 people scored correctly, and the alpha reliability for the four items was .45. Because there was little variability in telling time, it was clearly a skill participants retained. The four “orientation to date” items as a group had low reliability of .23. The greatest variability came in “What is the date?” and “What month are we in?,” both of which were correlated negatively with the other three items. These items were not particularly related to the rest of the DAFS. These items were constants because they were too easy for this population. Most of the “preparing a letter” items performed reasonably well, except that correctly doing the return address part was not related to the rest of the items, and everyone stamped the envelope correctly. However, because including a return address is important and scoring the envelope stamping was trivial, we kept this item. The transportation items seemed to make a reasonable scale (alpha = .67). However, the “red light” and “stop sign” items were constants and on some other items, very few people (two to five) answered incorrectly. Only “no right turn,” “no U-turn,” “double yellow line,” and “passing line” exhibited much variation; alpha was .64 for these items. The shopping recall and recognition items were fine. Conventional alpha reliability did not apply here because although the specific items forgotten were somewhat random, the count of items forgotten was useful. The sum of items answered correctly was correlated with the total DAFS score and with other performance measures. Additionally, these shopping items had good “face validity.” No individual missed any of the 8 of the 11 items on “identifying currency.” This left three “counting currency” items that were acceptable. Few people missed any of the “writing a check” items except for the “written amount” item. But all the items were correlated about the same with the total DAFS. The “balancing a checkbook” items together with the “making change” item had good variability and reliability, and they correlated notably with other performance measures. Shopping from a written list was too easy—there was no variability. The medication items were very easy, but the ease of scoring, together with their face validity and overall alpha reliability, justified their retention.
The DAFS-R
We based our decision on what items or subscales to eliminate on these ceiling effects. As shown in Table 1, our aim was to create a measure that would reflect individuals’ functioning on key activities of daily living in as parsimonious a way as possible. Because there are a number of measures of basic activities such as time orientation, we chose to focus on higher level skills. However, in a few cases, we retained items that showed a ceiling effect because it would have been difficult to retain the remaining items on the subscale without those items.
To make the DAFS more appropriate for the population of interest, items with little to no variation were removed. Items related to time orientation and transportation were removed completely. In addition, items testing participants’ ability to pick up a receiver and hang up the phone were removed from the communication domain. All items testing participants’ ability to identify currency were removed from the financial domain, along with one item related to counting currency (counting six cents in coins). The DAFS-R thus assessed participants’ performance in the following domains: communication skills, financial skills, shopping skills, and medications skills. There are 55 items in the DAFS-R, 20 of which are in the medication skills domain, enlarged from 10 in the modified DAFS used in the SeniorWISE study.
In the identifying medications section of the medication skills domain, participants were presented with a medication bottle and asked to identify the prescription or over-the-coutner medication, the patient’s name, medication name, the prescribing doctor, and any special instructions. Therefore, there were five items in this section and scores could range from 0 to 5.
The prescription refill task made up the second section of the medication skills domain. Participants were presented with a phone and a bottle of medication and were told that the activity was designed to give them practice in refilling prescriptions using an automated phone system. As in a real automated phone system, the instructor read instructions from a script and asked the participants to respond by pushing numbers on the phone. The phone had a small screen where the instructor could read the numbers that the participant pushed. The first item asked participants to select from a list of options the purpose of their call, which was to refill a prescription. The second item asked them to key in the prescription number. The third item asked them to enter the last four digits of their home phone number. The fourth item asked if they wanted to pick up the prescription or wanted it mailed to them. Previously, participants had been told that they were to pick up the prescription from the pharmacy tomorrow at 10 a.m. Therefore, the correct answer was to indicate that they wanted to pick it up from the pharmacy. The fifth item asked participants to choose whether they wanted to pick up the prescription today or tomorrow (the latter being the correct answer). The sixth item asked them if they wanted to pick up the prescription before noon or afternoon (the former being the correct answer). Finally, the seventh item asked them to key into the phone the exact time they wanted to pick up the prescription (the correct answer was “1,000”). Scores could range from 0 to 7.
The managing medications task section of the medication skills domain was composed of eight items. Participants were presented with a pillbox and eight bottles of medications commonly used by older adults that had labels and candy pills inside. Participants were instructed to fill the pillbox according to the labels on the different bottles. For example, they were instructed to take two Lipitor tablets every evening with dinner and one Levaquin tablet every morning for 3 more days. If any mistake was made on an item, it was scored as incorrect; otherwise, the participants got 1 point. Scores could range from 0 to 8.
Psychometric Testing
Subjects.—
Participants for this pilot test of the psychometric properties of the DAFS-R were recruited from a sample of older adults who had participated in an earlier study of a memory intervention for older adults living independently in the community. The SeniorWISE study has been described elsewhere (Austin-Wells, McDougall, & Becker, 2006). Participants for that study were recruited via print and TV media as well as direct recruitment at city-run senior activity centers, churches, health fairs, and festivals. They were screened for sensory loss and dementia. Other eligibility criteria included age (≥65 years), ability to speak and understand English, and reliable transportation. In that study, participants’ memory functioning and ability to perform IADLs were assessed five times for a period of 2 years.
Memory performance on the Rivermead Behavioural Memory Test (RBMT) of subjects at Time 5 in the SeniorWISE study (24 months into the study) was used as a basis for enrollment into this pilot study (Cockburn & Smith, 1989). Participants’ previous Rivermead scores were also used to assess the criterion validity of the DAFS-R. Following institutional review board approval, 105 participants split evenly into those who previously scored in the “normal” (≥22) or “impaired” (≤16) category on the Rivermead Memory test were selected from the final SeniorWISE sample and mailed a recruitment letter. Of those contacted, 60 agreed to participate (response rate = 57%) and 45 eventually completed the study. Among those, 34 were women and 11 men; 3 were African Americans, 36 Caucasians, and 6 Hispanics. Furthermore, 14 were in the “impaired” category and 31 were in the “normal” category. Their average age was 77.11 years, and their average numbers of years of education was 15.33. The Mini-Mental State Examination (MMSE) was used in this study to assess concurrent validity of the DAFS-R. Approximately 20 months had passed on average from the administration of the Rivermead and administration of the DAFS-R.
The MMSE, an 11-item screening instrument, was used to assess cognitive function and rule out those whose CI would preclude their participation in SeniorWISE (Folstein, Folstein, & McHugh, 1975). MMSE scores can range from 0 to 30, with a value of 23 or less indicating CI. A score between 18 and 22 usually indicates mild CI, and a score between 0 and 17 indicates severe CI. Those with scores below 20 were excluded.
Participants’ previous Rivermead scores were also used to assess the criterion validity of the DAFS-R. At Time 5 of the SeniorWISE study, mean MMSE scores were 27.79 and 29.16, respectively, for the impaired and normal Rivermead groups. In the present study, participants in the impaired and normal Rivermead categories averaged 28.00 and 29.03, respectively. A 2 × 2 repeated measures analysis of variance revealed that although neither the change over time (p = .88) nor the interaction of Rivermead group with time of administration (p = .54) was statistically significant, the main effect of Rivermead group was statistically significant (p < .01).
Participants came to a centrally located site. Cab fairs were reimbursed for participants who needed transportation. The study was described to participants, and they signed a consent form. A trained psychologist who had administered the DAFS and MMSE in the original SeniorWISE study administered the instruments to participants in the following order: MMSE and DAFS-R. Participants were paid $20 for participating.
Results
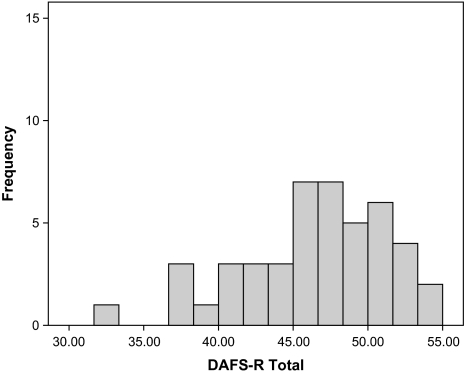
Figures 1 and 2 show the distributions of the original DAFS scores at Time 1 in the SeniorWISE study and the DAFS-R scores for the 45 participants in the present study. The distribution of the DAFS-R scores was more normal than that of the original DAFS (DAFS-R skewness = −0.69, SE = 0.35; kurtosis = 0.31, SE = 0.70 versus original DAFS skewness = −1.95, SE = 0.35; kurtosis = 7.06, SE = 0.70) and did not evidence a ceiling effect, as the original DAFS did. Furthermore, four of the participants in the current study had perfect scores on the DAFS at the fifth data collection in the SeniorWISE study, but only one individual had a perfect DAFS-R score.
Figure 2.
Frequency histogram of scores on the 55-item Direct Assessment of Functional Status-Revised (DAFS-R).
Table 2 presents basic information about each subscale and the total score of the 55-item DAFS-R. For each subscale, participants who had scored in the “normal” range on the Rivermead scored higher and displayed less variation as a group than those who were in the Rivermead “impaired” range, except for writing a check and prescription refill. The normal Rivermead group had significantly higher total scores on the total DAFS-R, t(17.42) = 2.19, p = .04 correcting for heterogeneous variances.
Table 2.
Subscale and Total Score Information for the DAFS-R
| MMSE | Impaired SPS | Normal SPS | |||||
|---|---|---|---|---|---|---|---|
| Subscale | Number of items | M | SD | Minimum–maximum | r | M (SD)a | M (SD)b |
| Phone | 4 | 3.40 | 0.69 | 2–4 | .28† | 3.29 (0.73) | 3.45 (0.68) |
| Letter | 6 | 5.56 | 0.69 | 3–6 | .26† | 5.43 (0.76) | 5.61 (0.67) |
| Money handling | 4 | 3.84 | 0.42 | 2–4 | −.03 | 3.57 (0.65) | 3.97 (0.18) |
| Writing a check | 5 | 5.00 | 0.00 | 5–5 | — | 5.00 (0.00) | 5.00 (0.00) |
| Balancing a checkbook | 4 | 3.40 | 0.86 | 1–4 | .54* | 3.14 (1.03) | 3.52 (0.77) |
| Shopping recall | 6 | 3.53 | 1.47 | 0–6 | .37* | 3.00 (1.75) | 3.77 (1.28) |
| Shopping recognition | 6 | 4.58 | 1.32 | 1–6 | .38* | 3.86 (1.46) | 4.90 (1.14) |
| Identifying medication | 5 | 4.93 | 0.33 | 3–5 | .17 | 4.79 (0.58) | 5.00 (0.00) |
| Pillbox | 8 | 6.53 | 1.55 | 2–8 | .39* | 5.93 (1.9) | 6.81 (1.30) |
| Refill | 7 | 5.56 | 1.34 | 3–7 | .25† | 5.57 (1.40) | 5.55 (1.34) |
| New DAFS total score | 10c/55 | 46.33 | 5.04 | 32–55 | .57* | 43.57 (6.35) | 47.58 (3.83) |
The Pearson’s correlations of the DAFS-R subscales and total score with the previously administered Rivermead and the concurrently administered MMSE are also shown in Table 2. These correlations provide estimates of the extent to which cognitive function was linearly associated with scores on the DAFS-R. In general, the amount of observed variation in a particular subscale was strongly related to its correlations with the MMSE and the Rivermead. The relationships between the MMSE and the Rivermead are positive associations. The near-zero correlations of the “money handling” and “identifying medication” subscales with these cognitive measures, however, must be interpreted in the context of the low variances in these subscales. A sample with more participants who performed poorly on these subscales would be required to assess the extent to which performance on these tasks is related to cognitive function.
Table 3 displays the intercorrelations among the DAFS-R subscales as well as their correlations with the corrected total score. In many instances, subscales were essentially uncorrelated with other subscales. Although all the subscales were positively correlated with the rest of the DAFS-R, the item–total correlations for money handling, letter, and identifying medication were weak and not significantly different from zero. As with the subscale correlations with the two cognitive measures, these low correlations were not surprising, given the low variances in the subscales.
Table 3.
Subscale and Total Score Intercorrelations for the DAFS-R Subscales
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| (1) Phone | 1 | ||||||||
| (2) Letter | −0.05 | ||||||||
| (3) Money handling | −0.02 | −0.09 | |||||||
| (4) Balancing a checkbook | 0.22 | 0.38† | 0.11 | ||||||
| (5) Shopping recall | 0.23 | 0.13 | −0.01 | 0.29 | |||||
| (6) Shopping recognition | 0.34† | 0.01 | 0.00 | 0.35† | 0.67* | ||||
| (7) Identifying medication | 0.02 | 0.07 | 0.41* | 0.33† | −0.02 | 0.09 | |||
| (8) Pillbox | 0.35† | 0.21 | 0.06 | 0.53* | 0.31† | 0.25 | 0.16 | ||
| (9) Refill | 0.27 | −0.22 | 0.04 | 0.22 | 0.32† | 0.21 | −0.02 | 0.19 | |
| DAFS-R total scorea | 39* | 0.10 | 0.06 | 0.58* | 0.56* | 0.53* | 0.17 | 0.48* | 0.29 |
Although each of the tasks of daily living represented in the DAFS-R might be considered fundamentally distinct, we were nevertheless interested in examining the reliability of the DAFS-R as a whole. Our sample size, however, did not permit calculation of Cronbach’s alpha across all individual items considered as a collection. Therefore, we treated each of the 10 subscales as “items” and found Cronbach’s alpha to be .67 or .68 if the writing a check subscale was disregarded because it was a constant.
A large number of individual items of the DAFS-R were either constants or near-constants. This is to be expected because it is a mastery test designed to assess several activities of daily living. For this reason, we do not report internal consistency reliability coefficients for the individual subscales. However, reliability is necessary for validity, and some preliminary evidence of the reliability of scores on the DAFS-R is provided by the numerous nonzero correlations of the subscales with the MMSE, the Rivermead, and each other as well as the correlations of the total DAFS-R score with the MMSE and the Rivermead (Kubiszyn & Borich, 2003).
Discussion
Assessing older adults’ ability to live independently is necessary to provide the diagnostic and prescriptive information to make informed health-related decisions. These preliminary analyses support the reliability and validity of the DAFS-R with this sample of elders living independently in the community. The internal consistency reliability (Cronbach’s alpha) of the 10 subscales was .68 when removing the writing a check subscale, which had no variation. Although the alpha coefficient was slightly lower than traditional standards, it should be noted that the DAFS-R tests skills from a variety of areas of functioning, including communication, financial, shopping, and medication management. Consequently, we might not expect to see high inter-item agreement. Future studies with a larger sample should be undertaken to test other aspects of reliability, particularly the temporal stability of scores on this measure.
The validity of the DAFS-R was supported by the moderate correlations of the total score and most of the subscales with the concurrently administered MMSE, which screens for CI. The DAFS-R total score also discriminated between those previously identified as having normal and impaired functioning, as measured by the previously administered Rivermead. However, future studies should explore other aspects of validity, particularly the relationship between scores on the subscales related to medication and other measures of medication skills.
There were individuals in our sample whose performance was poor enough to raise concerns about aspects of their daily functioning. Because individuals with MMSE scores less than 20 were excluded from participating in the study, our findings are limited to individuals exhibiting normal to poor memory performance and mild CI. The DAFS was able to differentiate individuals with varying standard profile scores on the RBMT memory performance instrument (normal, poor, and impaired). We would expect that cognitively impaired individuals will score lower on the DAFS-R because individuals with “poor” memory scores had difficulty with the complex tasks.
A comparison of the distributions of the DAFS and DAFS-R (Figures 1 and 2) suggests that the DAFS-R has a more normal distribution and is also relatively challenging, as evidenced by the lack of a ceiling effect. This preliminary evidence suggests that the DAFS-R may provide more information on this population’s functional status at the upper limit, which may be especially important for clinicians wanting to detect slight decrements in activities of daily living that might signal the onset of memory impairment. In addition, we reduced the number of items from 85 to 55, a 38% reduction, and this shorter version of the DAFS would be a more attractive screening measure to administer in a clinical setting.
Although the DAFS-R has fewer items than the original DAFS, the administration of the DAFS-R might take slightly longer than the original DAFS, primarily because the pillbox exercise is somewhat time-consuming. Future studies should compare the two versions to determine if the DAFS-R is markedly longer than the DAFS, because the decision of which version of the tool to use would be informed by the relative differences in administration time.
The limitations of this exploratory pilot study included its small convenience sample of primarily nonimpaired. Future studies should be undertaken with larger, more diverse samples. Such samples would support more complex psychometric analyses, such as confirmatory factor analysis. In addition, information from respondents with a wider range of cognitive abilities would more clearly elucidate the relationship between cognitive functioning and ability to perform activities of daily living. Future studies should also address the sensitivity of the DAFS-R to clinically meaningful changes in cognitive functioning that can affect elders’ ability to carry out activities of daily living such as those measured here.
Practice Implications
Although there are a number of self-reports of activities of daily living, there are fewer performance measures, particularly measures that assess higher level daily living skills, including proper medication management. Given the large number of older adults who regularly take multiple prescription medications, deficits in medication management skills can have serious consequences. These are areas that may be affected by subtle changes in cognitive functioning and may signal the onset of mild CI. Consequently, a measure that emphasizes these higher level daily living skills can help providers screen for initial signs of functional decline that can be followed up by more in-depth testing in specific functional areas.
Funding
Support for this research was provided by the National Institute of Aging (grant R01 AG 15384) and additional pilot funding from the Center for Health Promotion and Disease Prevention Research in Underserved Populations grant funded by the National Institute of Nursing Research (5P30 NR005051) in the School of Nursing at The University of Texas at Austin.
References
- Austin-Wells V, McDougall GJ, Becker H. Recruiting and retaining an ethnically diverse sample of older adults in a longitudinal intervention study. Educational Gerontology. 2006;32:159–170. doi: 10.1080/03601270500388190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell-McGinty S, Podell K, Franzen M, Baird AD, Williams MJ. Standard measures of executive function in predicting instrumental activities of daily living in older adults. International Journal of Geriatric Psychiatry. 2002;17:828–843. doi: 10.1002/gps.646. [DOI] [PubMed] [Google Scholar]
- Bertrand R, Willis SL, Sayer A. An evaluation of change over time in everyday cognitive competence among Alzheimer patients. Aging, Neuropsychology, and Cognition. 2001;8:192–212. [Google Scholar]
- Burton CL, Strauss E, Hultsch DF, Hunter MA. Cognitive functioning and everyday problem solving in older adults. Clinical Neurologist. 2006;20:432–452. doi: 10.1080/13854040590967063. [DOI] [PubMed] [Google Scholar]
- Cahn-Weiner DA, Malloy PF, Boyle PA, Marran M, Salloway S. Prediction of functional status from neuropsychological tests in community-dwelling elderly individuals. Clinical Neuropsychologist. 2000;14:187–196. doi: 10.1076/1385-4046(200005)14:2;1-Z;FT187. [DOI] [PubMed] [Google Scholar]
- Cockburn J, Smith PT. The Rivermead Behavioural Memory Test. Supplement 3: Elderly people. Suffolk, UK: Thames Valley Test Company; 1989. [Google Scholar]
- Diehl M, Marsiske M, Horgas A, Saczynski J. Psychometric properties of the Revised Observed Tasks of Daily Living (OTDL-R) 1998, November. Poster session at the annual meeting of the Gerontological Society of America, Philadelphia, PA. [Google Scholar]
- Diehl M, Willis SL, Schaie KW. Everyday problem solving in older adults: Observational assessment and cognitive correlates. Psychology and Aging. 1995;10:478–491. doi: 10.1037//0882-7974.10.3.478. [DOI] [PubMed] [Google Scholar]
- Dodge HH, Du Y, Saxton JA, Ganguli M. Cognitive domains and trajectories of functional independence in nondemented elderly persons. Journal of Gerontology: Biological Sciences and Medical Sciences. 2006;61A:1330–1337. doi: 10.1093/gerona/61.12.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JD, Wadley VG, Vance DE, Wood K, Roenker DL, Ball KK. The impact of speed of processing training on cognitive and everyday performance. Aging and Mental Health. 2005;9:262–271. doi: 10.1080/13607860412331336788. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-Mental State’: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, et al. Incidence and preventability of adverse drug reactions among older persons in the ambulatory setting. Journal of the American Medical Association. 2003;289:1107–1116. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- Insel K, Morrow D, Brewer B, Figueredo A. Executive function, working memory, and medication adherence among older adults. Journal of Gerontology: Psychological Sciences and Social Sciences. 2006;61B:P102–P107. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- Kubiszyn T, Borich G. Educational testing and measurement: Classroom application and practice. 7th ed. Hoboken, NJ: John Wiley & Sons; 2003. [Google Scholar]
- Lawton MP. Scales to measure competence in everyday activities. Psychopharmacology Bulletin. 1988;24:609–614. [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Loewenstein DA, Amigo E, Duara R, Guterman A, Hurwitz D, Berkowitz N, et al. A new scale for the assessment of functional status in Alzheimer’s disease and related disorders. Journal of Gerontology. 1989;44:114–121. doi: 10.1093/geronj/44.4.p114. [DOI] [PubMed] [Google Scholar]
- Mahurin RK, DeBettignies BH, Pirozzolo FJ. Structured assessment of independent living skills: Preliminary report of performance measure of functional abilities in dementia. Journal of Gerontology. 1991;46:P58–P66. doi: 10.1093/geronj/46.2.p58. [DOI] [PubMed] [Google Scholar]
- Marcopulos BM, McLain CA, Guiliano AJ. Cognitive impairment or inadequate norms? A study of healthy, rural older adults with limited education. Clinical Neuropsychologist. 1997;11:111–131. [Google Scholar]
- McDougall GJ, Becker H, Pituch K, Acee TW, Vaughan PW, Delville CL. The SeniorWISE study: Cognitive training with a triethnic sample of community-residing older adults. in press [Google Scholar]
- Rankin ED, Keefover RW. Clinical cutoffs in screening functional performance for dementia. Journal of Clinical Geropsychology. 1998;4:31–43. [Google Scholar]
- Whetstone LM, Fozard JL, Metter J, Hisock BS, Burke R, Gittings N, Fried LP. The physical functioning inventory: Procedure for assessing physical function in adults. Journal of Aging and Health. 2001;13:467–493. doi: 10.1177/089826430101300402. [DOI] [PubMed] [Google Scholar]
- Wilson BA, Cockburn J, Baddeley AD. The Rivermead Behavioural Memory Test. Suffolk, UK: Thames Valley Test Company; 1991. [Google Scholar]
- Zhan C, Sangl J, Bierman AS, Miller MR, Friedman B, Wickizer SW, Meyer GS. Potentially inappropriate medication use in the community-dwelling elderly: Findings from the 1996 Medical Expenditure Panel Survey. Journal of the American Medical Association. 2001;286:2823–2829. doi: 10.1001/jama.286.22.2823. [DOI] [PubMed] [Google Scholar]