Thymic Fatness and Approaches to Enhance Thymopoietic Fitness in Aging (original) (raw)
. Author manuscript; available in PMC: 2011 Aug 1.
Published in final edited form as: Curr Opin Immunol. 2010 Aug;22(4):521–528. doi: 10.1016/j.coi.2010.06.010
Summary
With advancing age, the thymus undergoes striking fibrotic and fatty changes that culminate in its transformation into adipose tissue. As the thymus involutes, reduction in thymocytes and thymic epithelial cells precede the emergence of mature lipid-laden adipocytes. Dogma dictates that adipocytes are ‘passive’ cells that occupy non-epithelial thymic space or ‘infiltrate’ the non cellular thymic niches. The provenance and purpose of ectopic thymic adipocytes during aging in an organ that is required for establishment and maintenance of T cell repertoire remains an unsolved puzzle. Nonetheless, tantalizing clues about elaborate reciprocal relationship between thymic fatness and thymopoietic fitness are emerging. Blocking or bypassing the route towards thymic adiposity may complement the approaches to rejuvenate thymopoiesis and immunity in elderly.
Keywords: Fibroblast, T cells, TCR, Adipogenesis, Adipocyte, Dietary Restriction, Nutrition, Ghrelin, PAPPA, Leptin, GH, IGF-1, Hormones, FoxN1, EMT, Obesity, Mesenchymal
Introduction
A characteristic feature of immunological aging in humans is the progressive loss of thymic T cell production. Consistent with critical role of the thymus in adult life, recent studies demonstrate that resection of thymus in children undergoing cardiac surgeries results in loss of naïve T cells (1). The peripheral T cell repertoire of 22-year old thymectomized patients is similar to that of 75-year old subjects (1). In all vertebrates studied to date, aging of the thymus is accelerated compared to aging of many other organs. Thymic aging is characterized by dramatic reduction in thymocyte numbers and marked perturbations in the thymic stromal cell microenvironment. In contrast to a young thymus where thymocytes are the major contributors to the thymic microenvironment, adipocytes constitute the bulk of an aged thymic cellular space (2, 3). The adipogenic transformation of thymus by middle-age is puzzling especially since the purpose of thymus is to produce naïve T cells while adipocytes regulate energy homeostasis and have no direct role in T cell development.
According to current estimates, approximately 3 × 109 T cells have to be generated everyday to replenish the total pool of existing 3 × 1011 T cells in human body (4). By 50 years of age approximately 80% of thymic stromal space is dysfunctional and composed of adipose tissue (2, 3) (Figure 1). During aging, the total peripheral T cell pool is maintained by homeostatic expansion of preexisting T cells rather than replenishment by thymic export (4–7). The ongoing exposure to pathogens and antigenic challenge across the life-span progressively erodes the integrity of the naïve T cell pool. Consequently, the T cell repertoire is restricted with an expansion of memory T cells and thus limits the host’s ability to mount responses against new antigenic challenges (4–7). Age-related thymic involution is associated with reduced immune-surveillance, increased risk and severity of emerging infections, certain cancers, vaccination failures and delayed T cell reconstitution in patients undergoing hematopoietic stem cell transplantations (HSCT) (8–10). In sum, the progressive loss of thymic function leads to a decline in adaptive immunity. Therefore, the ability to enhance thymopoiesis is central to the rejuvenation of T cell mediated immune-surveillance in elderly.
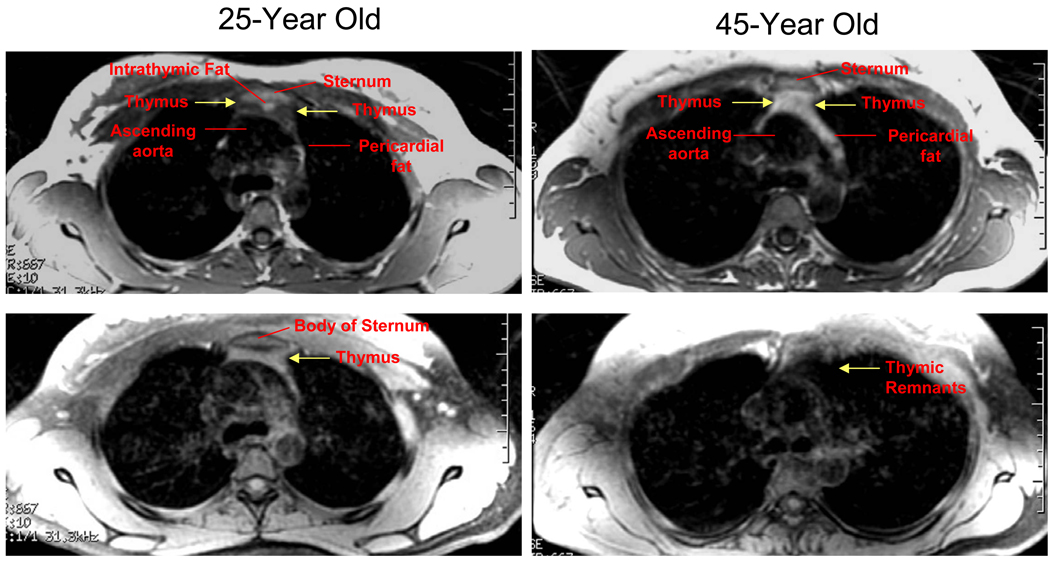
Figure 1. Thymic adiposity in humans.
The magnetic resonance imaging of thymus in metabolically healthy humans reveals age-related thymic adiposity. The Region of Interest (ROIs) depicting the thymus is highlighted by yellow arrows. The fat in the thymus appears whitish (upper panel) while thymic remnants are visible as pale area within the ROI. Lower panel shows thymic imaging in same subjects at similar locations after fat saturation. Since lipid appears as a high signal on T1 weighted images, the fat saturation sequences were applied to render the signal from fat null at the tracheal bifurcation. Upon application of fat-sat sequence, thymic tissue is visible (lower panel) in 25-year old individuals while in 45-year old subjects the area between sternum and ascending aorta is largely devoid of lymphoid tissue.
The three main causes of age-related thymic involution include – (a) a reduction in numbers and intrinsic defects in hematopoietic stem cells (HSCs) (11, 12) (b) Loss of thymic epithelial cells (TECs) and deterioration of stromal microenvironment (3, 13, 14) (c) extrinsic circulating factors affecting the aged microenvironment, e.g. alterations in hormones/growth factors/cytokines (15). Accordingly, several promising strategies to rejuvenate thymic function in aging have demonstrated the potential of targeting the mechanisms that correct the defects in HSCs and TECs (9, 10, 16, 17). Given that the thymus in middle-aged healthy humans is replaced by adipocytes (Figure 1), this review highlights the importance of thymic stromal microenvironment with emphasis on ectopic thymic adipocyte development in aging. Reviewed below are studies illustrating that pro-longevity interventions such as caloric restriction (CR) and neuroendocrine factors that regulate energy balance and thymic adipogenesis can forestall thymic aging and may rejuvenate thymopoiesis.
Thymic Adipocytes: Passive aggressive or active instigators of immunosenescence?
Thymic stromal cell composition as well as organization is severely disrupted with advancing age (3, 13, 18). This includes reduction in thymic epithelial cells (TECs), increase in fibroblasts, disruption of thymic perivascular space (PVS) and the emergence of adipocytes (2, 3, 13). The thymic stromal compartment is divided into (a) thymopoietic niches – which are mainly composed of epithelial cells and antigen presenting cells that sustain T cell development and (b) non-thymopoietic niches –which includes connective tissue capsule, interlobular trabeculae, septae and intricate network of thymic blood vessels.
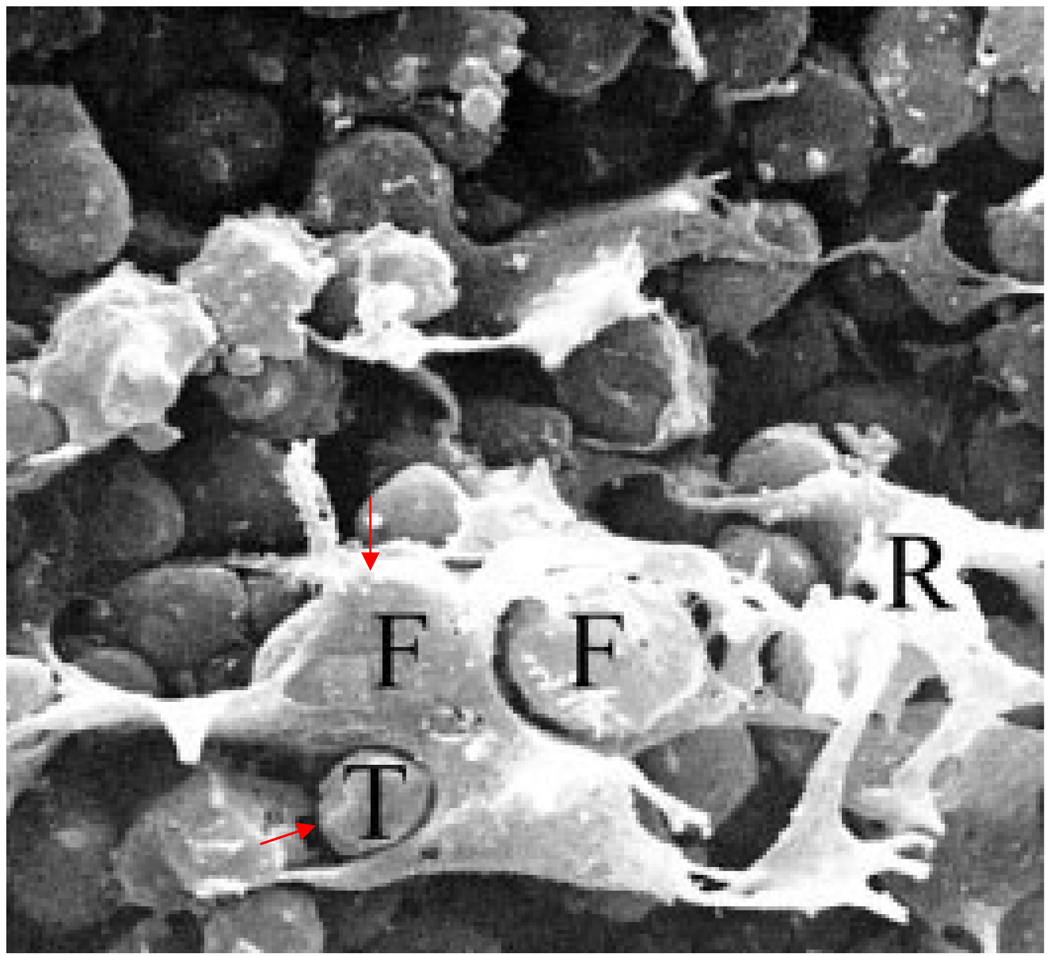
Loss of thymocytes precedes the formation of adipocytes during thymic involution. If emergence of adipocytes in thymus would simply be a consequence of loss of thymocytes then one might expect lymphopenic mouse models to have fatty thymi. This simple assumption, however, is not supported by histological evidence from RAG knock outs, severe combined immune deficiency (SCID), IL-2 receptor γ chain knockouts, in which there is loss of thymocytes but little spontaneous accumulation of thymic adipocytes at younger ages (19, 20). It is also believed that thymic adipocytes ‘infiltrate’ the perivascular space (PVS); however, evidence that large lipid filled adipocytes can migrate through tight intercellular spaces in PVS or thymic parenchyma is so far unavailable. Since PVS is not an active thymopoietic zone, the emergence of adipose tissue in these areas is believed to be incidental to the process of thymic aging. However, previous studies have demonstrated that the adipocytes and thymocytes can come in close cell-cell contact in the human thymus during aging (21) (Figure 2). It is also established that adipocytes are not inert cells and, depending upon their location, can secrete distinct cytokines and hormones that influence the local and systemic environment and immune function (22). No compelling or direct experimental evidence currently exists that would argue in favor of the dogmatic contention that thymic adipocytes are passive cells; therefore the prevailing view of adipocyte trafficking in the thymus may be overly simplistic. On the other hand, several studies over the past few years support the hypothesis that adipocytes differentiate through specific adipogenic mechanisms, and this process can compromise hematopoietic (23) and thymic function (24–26).
Figure 2. Scanning electron microscopy of thymus of 68 year old subject.
Thymus from a 68-year-old patient observed by scanning electron microscopy. A large number of fatty cells (F) and reticular epithelial cells (R), with a small number of thymocytes (T), can be observed in elderly subjects. (previously published as figure 5 by Cavalotti et al 2008, Microsc Res Tech. 71: 573–578.)
Perivascular space (PVS) and adipocytes
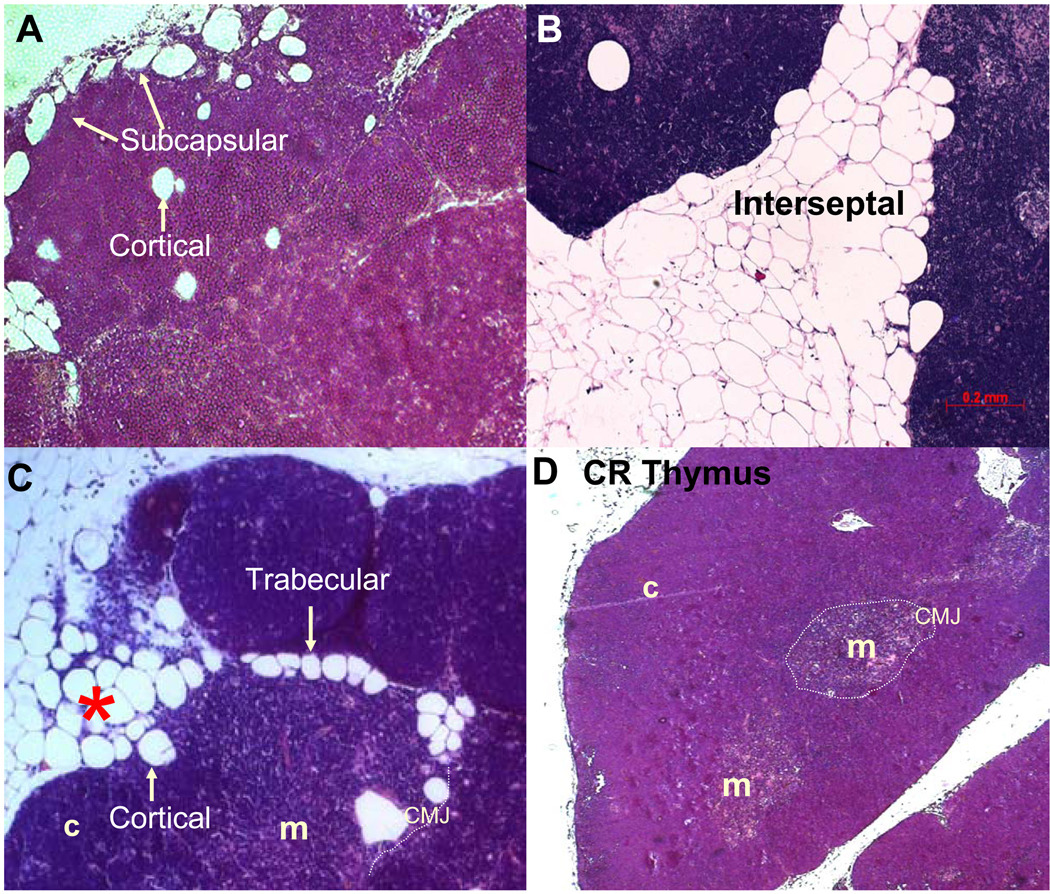
In addition to PVS, thymic adipocytes are also present in several thymic zones which include interlobular septae, capsular region, subcapsular cortex and medulla (Figure 3). Since several prior histological studies of aging thymus refer to expansion of PVS and ‘infiltration’ of adipocytes within this region, the role of thymic vasculature in thymic involution process merits revisiting.
Figure 3. Thymic Adipocytes.
Location of thymic adipocytes in 18mo old thymi of C57/B6 mice. (A) Subcapsular cortical adipocytes, (B) Interseptal adipocytes (C) Trabecular adipocytes, * denotes cortical areas of thymus undergoing adipogenic involution. Dotted line indicates corticomeduallry junction and adjacent ectopic adipocytes which could be in the PVS. Cortex (c) and Medulla (m). (D) Thymus from 18m old mouse maintained on 40% caloric restriction shows absence of adipocytes and maintenance of thymic architecture during aging.
In young mice, thymic vascular supply is primarily characterized by entry of one artery and exit of one vein at the hilus on the dorsolateral surface of thymus (27). Importantly, migration of T cell progenitors in thymus and selective export of mature thymocytes to the periphery occurs via the post capillary venules (PCVs) at the corticomedullary junction (CMJ). In young mice, the PCVs appear ‘double walled’ because of the presence of perivascular space (PVS) between inner endothelial cell vessel wall and outer layer of thin epithelial like cells (21, 28–30). The PVS is a typical feature of PCVs at the CMJ; whereas, in thymic capillaries, the endothelial vessel wall is anchored with the outer epithelial basal lamina leaving no PVS between vessels and adjacent parenchyma (21, 27–30). The PVS in young mice contains migrating progenitors, T cells and pericytes (28–30). Aging is known to cause disruption of PVS, which include gaps in outer epithelial cell layer of PCVs (27) and presence of adipogenic cells in the PVS (2).
Elegant lineage-tracing studies provide strong evidence that neural crest derived mesenchymal cells are ancestors of thymic pericytes and some perivascular cells (29, 30). Additionally, the neural crest derived cells in adult thymus express the mesenchymal cell markers PDGFR-α and PDGFR-β (29, 30). The PDGFR-α+ mesenchymal cells have the potential to differentiate into adipocyte lineage and are known to give rise to ectopic adipocytes in skeletal muscle (31). Consistent with this, in middle-aged thymus, several PDGFR-α+ cells express PPARγ, a master proadipogenic transcription factor (26). Furthermore, PDGFR-β+ mesenchymal cells derived from the vasculature of adipose tissue differentiate into adipocytes through the activation of PPARγ (32). Previous studies indicate that perivascular cells and pericytes exhibit multipotency including the ability to differentiate into fibroblasts and adipocytes (32, 33). Considering that PVS is among the sites for accumulation of fibro-adipogenic cells in thymus, it is possible that specific perivascular cells differentiate and serve as adipocyte precursors during aging. Such a hypothesized mechanism remains to be formally tested, but the emerging evidence argues against oft stated ‘adipocyte infiltration’ view of PVS. Instead, it is likely that within PVS, precursor cells undergo adipogenic commitment with advancing age through specific molecular mechanisms. Given a critical role played by PCVs in selective import and export of cells in thymus through the expression of chemokines and chemokine receptors, the mechanisms that compromise the perivascular stromal cell microenvironment in aging are likely to contribute towards the process of thymic dysfunction.
Epithelial-mesenchymal transition (EMT) and fibroadipogenesis in aging thymus
The primary EMT occurs during embryonic development when epiblast cells give rise to mesenchymal and neural crest cells (34). The primary mesenchymal cells transition to secondary epithelial cells via the mesenchymal-epithelial transition (MET) process and initiate organ development. (34). It is now well documented that with progressive aging, thymic epithelial cells (TECs) decline with a concomitant increase in thymic fibroblasts (3, 13, 26). Recent studies employing genetic fate-mapping, suggest that subset of FoxN1 origin TECs can transition into fibroblasts during aging via the activation of epithelial-mesenchymal transition (EMT) process in thymus (24). Importantly, secondary EMT, also referred as type 2 EMT, occurs during adult life when epithelial and endothelial cells transition to give rise to tissue resident fibroblasts leading to fibrosis (34–36). The secondary mesenchymal cells generated through the process of EMT are identified by the expression of fibroblast specific protein-1 (FSP1) also called S100A4/Mts1/calvasculin (35). The FSP1 gene contains a position and promoter-dependent proximal element between −187 and −88 bp called fibroblast transcription site-1 (FTS-1), which is active in fibroblasts but not in epithelium (35). FSP1 is not expressed in primary mesenchymal cells but is present in fibroblasts derived from secondary epithelium and is therefore a strong indicator of EMT (35). The process of thymic involution is associated with an increase in pro-EMT transcripts including FSP1/S100A4 (24, 26). The secondary mesenchymal cells retain multipotency in vitro (37). Importantly, certain EMT cells in aging thymus express PPARγ and unilocular lipid droplet and appear to commit to adipocyte lineage (3, 24, 26). In addition, activation of PPARγ in mesenchymal cells induces ectopic adipogenesis in bone marrow and thymus leading to reduced thymopoiesis and restricted TCR repertoire diversity (25). Thus, the loss of TEC phenotype and emergence of fibro-adipogenic precursors from a subset of thymic stromal cells may have direct implications in compromising thymopoiesis.
Novel strategies for thymic rejuvenation: Inhibitors of EMT and thymoadipogenesis
Several experimental approaches for thymic and T cell reconstitution during aging have been the subject of excellent review articles (7, 9, 10). This review summarizes the strategies that target the EMT and ectopic adipogenesis mechanism as complementary strategies to rejuvenate thymopoiesis or forestall thymic aging.
1. Caloric Restriction (CR) and CR mimetics
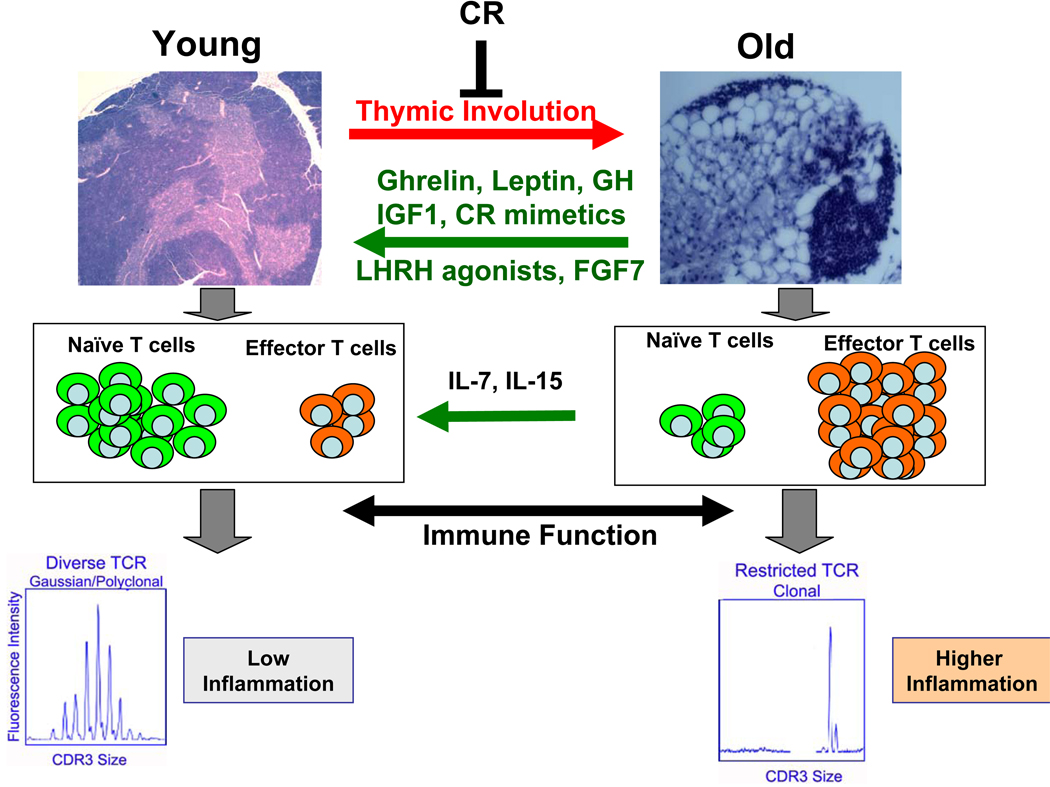
Induction of negative energy balance via CR remains one of the most robust non-genetic means of extending healthspan and lifespan across several species (38). Chronic CR in mice and monkeys sustains T cell receptor repertoire diversity and enhances thymopoiesis (3, 26, 39). Conversely, chronic caloric excess seen during obesity accelerates thymic aging and restricts TCR repertoire (40). Recent data suggest that CR efficiently blocks EMT and age-related increase in pro-adipogenic machinery in thymus (26). This includes reduction in PPARγ expression on PDGFRα+ mesenchymal cells (26). In addition, chronic CR prevents age-related changes in the thymic transcriptome (41).
Although CR has been a very effective experimental approach to prolong healthy life-span in experimental animals, it is unclear if CR is relevant to human immune function. The impact of CR on T cell function, thymopoiesis and thymic adipogenesis in humans is being investigated in an ongoing multi-center, parallel-group, randomized control trial called Comprehensive Assessment of Long-Term Effects of Reducing Intake of Energy (CALERIE). It is however, well recognized that long-term adherence to a strict CR diet in humans for enhancing immunity and longevity is a significant challenge in the current ‘obesogenic’ environment. In several chronic illnesses or BMT conditioning regimens where elderly patients already have loss of appetite and frailty, recommending CR to enhance naïve T cell production is not advisable. Therefore, identification and development of compounds that mimic the positive biologic effects of calorie restriction could help unravel novel pathways to enhance thymopoiesis.
2. Ghrelin and GH secretagogues
Ghrelin is predominantly secreted from the gut in response to negative energy balance and CR (42). Ghrelin binds to specific growth hormone secretaguge receptor (GHSR) to induce GH production and reduces pro-inflammatory cytokines from immune cells (42–45). Similar to CR, ghrelin reduces age-related inflammation (46) and partially reverses thymic involution process (47). On the contrary, deletion of ghrelin accelerates thymic involution, EMT and adipogenesis in thymus (24). Consistent with anti-fibrogenic effects of ghrelin in thymus, ghrelin also reduces fibrosis in liver (48). The synthetic long-acting small molecule ghrelin-receptor agonists can partially reverse age-related thymic involution (49). Importantly, such ghrelin-mimetic compounds have been shown to be safe in humans and effective in reducing frailty in the elderly (50). Therefore, long-acting synthetic ghrelin-receptor agonists may be ideal candidates for further clinical evaluation as potential therapeutic candidates for thymic regeneration in aging and HSCT.
Consistent with the complementary role of ghrelin and GH axis in reducing ectopic adipocytes in primary lymphoid organs (51), randomized clinical trials in middle-aged HIV patients have demonstrated that GH serves as a potent pro-thymopoietic agent (52). IGF-1, like ghrelin, also enhances thymopoiesis by expanding bone marrow Lin− Sca1+Kit+ progenitors and thymic epithelial niches while the disruption of IGF1 signaling in thymocyte, reduces thymocyte survival (53). These data demonstrate that activation of ghrelin-GH-IGF1 axis can regenerate thymus. Whether this can be clinically accomplished without elevating the risk of certain cancers remains to be established.
3. Leptin
Leptin is a potent adipokine that signals the state of positive energy balance and reduces food intake. Deficiency of leptin in mice induces severe obesity and marked thymic involution (54). Consistent with the importance of leptin in immunity, loss of function leptin mutations in humans lowers T cell mediated immunity (55). Administration of recombinant leptin to leptin-deficient humans reverses T cell dysfunction (55). Furthermore, loss of function mutation in leptin-receptor also results in development of childhood obesity that is characterized by T cell defects and premature death due to severe infections (56). Administration of leptin to aging mice increases peripheral IGF-1 levels (47) and despite leptin’s well documented pro-inflammatory effects (43), it can induce thymic regeneration and expand TCR repertoire diversity (47). These observations are consistent with pro-survival effects of leptin on thymocytes (57) and the ability of leptin treatment to augment thymopoiesis in models of aging, stress and endotoxemia (9, 47). Recent data from Louisiana Healthy Aging Study (LHAS) suggest that elevated levels of leptin and GH are associated with maintenance of the CD28+CD95− naïve T cell pool and presence of recent thymic emigrants in healthy nonagenarians (≥90-year-old) (58).
4. Pregnancy associated Plasma Protein A (PAPPA)
PAPPA is a metalloproteinase that cleaves IGF-binding proteins (IGFBPs) facilitating the bioavailability of IGF1 to IGF receptors. Interestingly, PAPPA deficiency in mice is associated with enhanced lifespan and maintenance of thymic and T cell function during aging (59). Compared to the thymi of aged wild type mice which contains cortical adipocytes, the PAPPA−/− animals lack ectopic adipocyte development with increased thymocyte numbers and thymopoiesis. The increased thymopoiesis in PAPPA knockout mice is proposed to be due to slower release of thymic IGF1, which increases the survival of T cell progenitors and thymocyte subsets (59).
Conclusions
Although the thymus undergoes rapid adipogenic transformation, the fibrosis and fatty changes with advancing age occur in several organs and are not unique to thymus. The mechanisms behind this age-associated phenomenon are still largely unknown. Several recent studies have greatly expanded the understanding of basic mechanisms of age-related thymic regeneration in mouse models. As new data emerge and future therapeutic approaches for thymic rejuvenation are developed, preventing the deterioration of thymic microenvironment or strategies for reversal of fibro-adipogenesis in thymus offer as-of-yet untapped opportunity for enhancing and maintaining thymopoiesis.
Figure 4. Approaches to reverse immunosenescence.
Approaches to reverse immunosenescence. CR and metabolic regulators such as ghrelin, leptin, GH and IGF-1 can partially reverse age-related thymic involution. Increased thymopoiesis by these agents (including LHRH and FGF7/KGF, IL7 and IL-15) increases naïve cells and enhanced T cell repertoire diversity.
Acknowledgements
I thank Yun-Hee Youm, Hyunwon Yang, Bolormaa Vandanmagsar and Anthony Ravussin in my laboratory for many exciting findings and discussions that have helped to shape this review. I also thank Don Ingram for pre-submission review of the manuscript. This research was supported by the National Institutes of Health grant NIA-R01-AG031797, the Pennington Biomedical Research Foundation and the Coypu Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
● of special interest
●● of outstanding interest
- 1.Sauce D, Larsen M, Fastenackels S, Duperrier A, Keller M, Grubeck-Loebenstein B, Ferrand C, Debré P, Sidi D, Appay V. Evidence of premature immune aging in patients thymectomized during early childhood. J Clin Invest. 2009;119:3070–3078. doi: 10.1172/JCI39269. This study demonstrates that removal of thymus during infancy results in premature onset of immunosenescence thus establishing the requirement of thymopoiesis in adult life for a healthy immune system. This study also shows that removal of thymus accelerates ‘inflammaging’. Compared to age-matched controls the thymectomized patients show higher levels of pro-inflammatory cytokines such as IL-1β.
- 2.Flores KG, Li J, Sempowski GD, Haynes BF, Hale LP. Analysis of the human thymic perivascular space during aging. J Clin Invest. 1999;104:1031–1039. doi: 10.1172/JCI7558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang H, Youm YH, Rim JS, Galban C, Vandanmagsar B, Dixit VD. Axin expression in thymic stromal cells contributes to age-related increase in thymic adiposity and associated with reduced thymopoiesis independently of ghrelin signaling. J. Leukoc Biol. 2009;85:928–938. doi: 10.1189/jlb.1008621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goronzy JJ, Weyand CM. T cell development and receptor diversity during aging. Curr Opin Immunol. 2005;17:468–475. doi: 10.1016/j.coi.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 5.Maue AC, Yager EJ, Swain SL, Woodland DL, Blackman MA, Haynes L. T-cell immunosenescence: lessons learned from mouse models of aging. Trends Immunol. 2009;30:301–305. doi: 10.1016/j.it.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yager EJ, Ahmed M, Lanzer K, Randall TD, Woodland DL, Blackman MA. Age-associated decline in T cell repertoire diversity leads to holes in the repertoire and impaired immunity to influenza virus. J Exp Med. 2008;205:711–723. doi: 10.1084/jem.20071140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorshkind K, Montecino-Rodriguez E, Signer RA. The ageing immune system: is it ever too old to become young again? Nat Rev Immunol. 2009;9:57–62. doi: 10.1038/nri2471. [DOI] [PubMed] [Google Scholar]
- 8.McElhaney JE, Effros RB. Immunosenescence: what does it mean to health outcomes in older adults? Curr Opin Immunol. 2009;21:418–424. doi: 10.1016/j.coi.2009.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lynch HE, Goldberg GL, Chidgey A, Van den Brink MR, Boyd R, Sempowski GD. Thymic involution and immune reconstitution. Trends Immunol. 2009;30:366–373. doi: 10.1016/j.it.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holland AM, van den Brink MR. Rejuvenation of the aging T cell compartment. Curr Opin Immunol. 2009;21:454–459. doi: 10.1016/j.coi.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Min H, Montecino-Rodriguez E, Dorshkind K. Reduction in the developmental potential of intrathymic T cell progenitors with age. J Immunol. 2004;173:245–250. doi: 10.4049/jimmunol.173.1.245. [DOI] [PubMed] [Google Scholar]
- 12.Zediak VP, Maillard I, Bhandoola A. Multiple prethymic defects underlie age-related loss of T progenitor competence. Blood. 2007;110:1161–1167. doi: 10.1182/blood-2007-01-071605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gray DH, Seach N, Ueno T, Milton MK, Liston A, Lew AM, Goodnow CC, Boyd RL. Developmental kinetics, turnover, and stimulatory capacity of thymic epithelial cells. Blood. 2006;108:3777–3785. doi: 10.1182/blood-2006-02-004531. [DOI] [PubMed] [Google Scholar]
- 14.Chen L, Xiao S, Manley NR. Foxn1 is required to maintain the postnatal thymic microenvironment in a dosage-sensitive manner. Blood. 2009;113:567–574. doi: 10.1182/blood-2008-05-156265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nobori S, Shimizu A, Okumi M, Samelson-Jones E, Griesemer A, Hirakata A, Sachs DH, Yamada K. Thymic rejuvenation and the induction of tolerance by adult thymic grafts. Proc Natl Acad Sci U SA. 2006;103:19081–19086. doi: 10.1073/pnas.0605159103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Virts EL, Phillips JA, Thoman ML. A novel approach to thymic rejuvenation in the aged. Rejuvenation Res. 2006;9:134–142. doi: 10.1089/rej.2006.9.134. [DOI] [PubMed] [Google Scholar]
- 17.Aspinall R, Mitchell W. Reversal of age-associated thymic atrophy: treatments, delivery, and side effects. Exp Gerontol. 2008;43:700–705. doi: 10.1016/j.exger.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 18.Gui J, Zhu X, Dohkan J, Cheng L, Barnes PF, Su DM. The aged thymus shows normal recruitment of lymphohematopoietic progenitors but has defects in thymic epithelial cells. Int Immunol. 2007;19:1201–1211. doi: 10.1093/intimm/dxm095. [DOI] [PubMed] [Google Scholar]
- 19.Pearse G. Normal structure, function and histology of the thymus. Toxicol Pathol. 2006;34:504–514. doi: 10.1080/01926230600865549. [DOI] [PubMed] [Google Scholar]
- 20.Ohbo K, Suda T, Hashiyama M, Mantani A, Ikebe M, Miyakawa K, Moriyama M, Nakamura M, Katsuki M, Takahashi K, Yamamura K, Sugamura K. Modulation of hematopoiesis in mice with a truncated mutant of the interleukin-2 receptor gamma chain. Blood. 1996;87:956–967. [PubMed] [Google Scholar]
- 21.Cavallotti C, D'Andrea V, Tonnarini G, Cavallotti C, Bruzzone P. Age-related changes in the human thymus studied with scanning electron microscopy. Microsc Res Tech. 2008;71:573–578. doi: 10.1002/jemt.20588. [DOI] [PubMed] [Google Scholar]
- 22.Tilg H, Moschen AR. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol. 2006;6:772–783. doi: 10.1038/nri1937. [DOI] [PubMed] [Google Scholar]
- 23.Naveiras O, Nardi V, Wenzel PL, Hauschka PV, Fahey F, Daley GQ. Bone-marrow adipocytes as negative regulators of the haematopoietic microenvironment. Nature. 2009;460:259–263. doi: 10.1038/nature08099. Authors demonstrate that adipocytes do not simply fill the marrow space but are negatively impact hematopoietic stem cell function in bone marrow. Using A-ZIP/F1 mice that lack adipocytes and pharmacological treatment with PPARγ antagonist, authors demonstrate that by blocking marrow adipocyte development, hematopoiesis and engraftment after irradiation can be enhanced.
- 24.Youm YH, Yang H, Sun Y, Smith RG, Manley NR, Vandanmagsar B, Dixit VD. Deficient Ghrelin receptor mediated signaling compromises thymic stromal cell microenvironment by accelerating thymic adiposity. J Biol Chem. 2009;284:7068–7077. doi: 10.1074/jbc.M808302200. Utilizing genetic lineage-tracing by indelibly marking the FoxN1 thymic epithelial cells, this paper provides evidence that with aging, a subset of TECs can transition into fibroadipogenic cells. Deletion of ghrelin and ghrelin-receptors accelerates epithelial-mesenchymal transition and thymic adipogenesis.
- 25.Youm YH, Yang H, Amin R, Smith SR, Leff T, Dixit VD. Thiazolidinedione treatment and constitutive-PPARgamma activation induces ectopic adipogenesis and promotes age-related thymic involution. Aging Cell. 2010 Apr 1; doi: 10.1111/j.1474-9726.2010.00574.x. [Epub ahead of print] This paper demonstrates that widely used anti-hyperglycemic PPARγ-ligand drugs accelerate age-related thymic involution and immunosenescence. Genetic evidence is provided that shows that constitutive-active PPARγ fusion protein expression in adipogenic lineage cells in thymus and bone marrow promotes thymic aging, lowers Lin−Sca1+Kit+ pool and restricts TCR diversity.
- 26.Yang H, Youm YH, Dixit VD. Inhibition of thymic adipogenesis by caloric restriction is coupled with reduction in age-related thymic involution. J Immunol. 2009;183:3040–3052. doi: 10.4049/jimmunol.0900562. This study shows that CR blocks age-related increase in pro-EMT and pro-adipogenic programming and protects thymus from involution.
- 27.Kato S. Thymic microvascular system. Microsc Res Tech. 1997;38:287–299. doi: 10.1002/(SICI)1097-0029(19970801)38:3<287::AID-JEMT9>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 28.Mori K, Itoi M, Tsukamoto N, Kubo H, Amagai T. The perivascular space as a path of hematopoietic progenitor cells and mature T cells between the blood circulation and the thymic parenchyma. Int Immunol. 2007;19:745–753. doi: 10.1093/intimm/dxm041. [DOI] [PubMed] [Google Scholar]
- 29.Müller SM, Stolt CC, Terszowski G, Blum C, Amagai T, Kessaris N, Iannarelli P, Richardson WD, Wegner M, Rodewald HR. Neural crest origin of perivascular mesenchyme in the adult thymus. J Immunol. 2008;180:5344–5351. doi: 10.4049/jimmunol.180.8.5344. [DOI] [PubMed] [Google Scholar]
- 30.Foster K, Sheridan J, Veiga-Fernandes H, Roderick K, Pachnis V, Adams R, Blackburn C, Kioussis D, Coles M. Contribution of neural crest-derived cells in the embryonic and adult thymus. J Immunol. 2008;180:3183–3189. doi: 10.4049/jimmunol.180.5.3183. [DOI] [PubMed] [Google Scholar]
- 31.Uezumi A, Fukada S, Yamamoto N, Takeda S, Tsuchida K. Mesenchymal progenitors distinct from satellite cells contribute to ectopic fat cell formation in skeletal muscle. Nat Cell Biol. 2010;12:143–152. doi: 10.1038/ncb2014. [DOI] [PubMed] [Google Scholar]
- 32.Tang W, Zeve D, Suh JM, Bosnakovski D, Kyba M, Hammer RE, Tallquist MD, Graff JM. White fat progenitor cells reside in the adipose vasculature. Science. 2008;322:583–586. doi: 10.1126/science.1156232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brachvogel B, Moch H, Pausch F, Schlötzer-Schrehardt U, Hofmann C, Hallmann R, von der Mark K, Winkler T, Pöschl E. Perivascular cells expressing annexin A5 define a novel mesenchymal stem cell-like population with the capacity to differentiate into multiple mesenchymal lineages. Development. 2005;132:2657–2668. doi: 10.1242/dev.01846. [DOI] [PubMed] [Google Scholar]
- 34.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 35.Zeisberg M, Neilson EG. Biomarkers for epithelial-mesenchymal transitions. J Clin Invest. 2009;119:1429–1437. doi: 10.1172/JCI36183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zeisberg EM, Tarnavski O, Zeisberg M, Dorfman AL, McMullen JR, Gustafsson E, Chandraker A, Yuan X, Pu WT, Roberts AB, Neilson EG, Sayegh MH, Izumo S, Kalluri R. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis. Nat Med. 2007;13:952–961. doi: 10.1038/nm1613. Authors use genetic fate-mapping approached to demonstrate that endothelial cells can transition into fibroblasts and give rise to cardiac fibrosis.
- 37.Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, Campbell LL, Polyak K, Brisken C, Yang J, Weinberg RA. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barger JL, Walford RL, Weindruch R. The retardation of aging by caloric restriction: its significance in the transgenic era. Exp Gerontol. 2003;38:1343–1351. doi: 10.1016/j.exger.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 39.Messaoudi I, Warner J, Fischer M, Park B, Hill B, Mattison J, Lane MA, Roth GS, Ingram DK, Picker LJ, Douek DC, Mori M, Nikolich-Zugich J. Delay of T cell senescence by caloric restriction in aged long-lived nonhuman primates. Proc Natl Acad Sci U S A. 2006;103:19448–19453. doi: 10.1073/pnas.0606661103. This study demonstrate that chronic CR in primates can prevent the loss of naïve T cells and reduces senescent T cells. Using CDR3 polymorphism analysis, authors provide evidence that CR prevents age-related deterioration of TCR repertoire diversity in rhesus macaque.
- 40.Yang H, Youm YH, Vandanmagsar B, Rood J, Kumar KG, Butler AA, Dixit VD. Obesity accelerates thymic aging. Blood. 2009;114:3803–3812. doi: 10.1182/blood-2009-03-213595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lustig A, Weeraratna AT, Wood WW, 3rd, Teichberg D, Bertak D, Carter A, Poosala S, Firman J, Becker KG, Zonderman AB, Longo DL, Taub DD. Transcriptome analysis of age-, gender- and diet-associated changes in murine thymus. Cell Immunol. 2007;245:42–61. doi: 10.1016/j.cellimm.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kojima M, Kangawa K. Ghrelin: structure and function. Physiol Rev. 2005;85:495–522. doi: 10.1152/physrev.00012.2004. [DOI] [PubMed] [Google Scholar]
- 43.Dixit VD, Schaffer EM, Pyle RS, Collins GD, Sakthivel SK, Palaniappan R, Lillard Jr, JW, Taub DD. Ghrelin inhibits leptin- and activation-induced proinflammatory cytokine expression by human monocytes and T cells. J Clin Invest. 2004;114:57–66. doi: 10.1172/JCI21134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chorny A, Anderson P, Gonzalez-Rey E, Delgado M. Ghrelin protects against experimental sepsis by inhibiting high-mobility group box 1 release and by killing bacteria. J Immunol. 2008;180:8369–8377. doi: 10.4049/jimmunol.180.12.8369. [DOI] [PubMed] [Google Scholar]
- 45.Gonzalez-Rey E, Chorny A, Delgado M. Therapeutic action of ghrelin in a mouse model of colitis. Gastroenterology. 2006;130:1707–1720. doi: 10.1053/j.gastro.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 46.Dixit VD, Yang H, Cooper-Jenkins A, Giri BB, Patel K, Taub DD. Reduction of T cell-derived ghrelin enhances proinflammatory cytokine expression: implications for age-associated increases in inflammation. Blood. 2009;113:5202–5205. doi: 10.1182/blood-2008-09-181255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dixit VD, Yang H, Sun Y, Youm YH, Weeraratna AT, Smith RG, Taub DD. Ghrelin promotes thymopoiesis during aging. J. Clin. Invest. 2007;117:2778–2790. doi: 10.1172/JCI30248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moreno M, Chaves JF, Sancho-Bru P, Ramalho F, Ramalho LN, Mansego ML, Ivorra C, Dominguez M, Conde L, Millán C, Marí M, Colmenero J, Lozano JJ, Jares P, Vidal J, Forns X, Arroyo V, Caballería J, Ginès P, Bataller R. Ghrelin attenuates hepatocellular injury and liver fibrogenesis in rodents and influences fibrosis progression in humans. Hepatology. 2010;51:974–985. doi: 10.1002/hep.23421. This paper demonstrates that in humans, SNPs in ghrelin gene are associated with liver fibrosis. Loss of ghrelin function accelerates hepatic fibrosis while treatment of mice with ghrelin reduces inflammation and fibrosis.
- 49.Koo GC, Huang C, Camacho R, Trainor C, Blake JT, Sirotina-Meisher A, Schleim KD, Wu TJ, Cheng K, Nargund R, McKissick G. Immune enhancing effect of a growth hormone secretagogue. J Immunol. 2001;166:4195–4201. doi: 10.4049/jimmunol.166.6.4195. [DOI] [PubMed] [Google Scholar]
- 50.Smith RG, Sun Y, Jiang H, Albarran-Zeckler R, Timchenko N. Ghrelin receptor (GHS-R1A) agonists show potential as interventive agents during aging. Ann N Y Acad Sci. 2007;1119:147–164. doi: 10.1196/annals.1404.023. [DOI] [PubMed] [Google Scholar]
- 51.French RA, Broussard SR, Meier WA, Minshall C, Arkins S, Zachary JF, Dantzer R, Kelley KW. Age-associated loss of bone marrow hematopoietic cells is reversed by GH and accompanies thymic reconstitution. Endocrinology. 2002;143:690–699. doi: 10.1210/endo.143.2.8612. [DOI] [PubMed] [Google Scholar]
- 52.Napolitano LA, Schmidt D, Gotway MB, Ameli N, Filbert EL, Ng MM, Clor JL, Epling L, Sinclair E, Baum PD, Li K, Killian ML, Bacchetti P, McCune JM. Growth hormone enhances thymic function in HIV-1-infected adults. J Clin Invest. 2008;118:1085–1098. doi: 10.1172/JCI32830. This prospective, randomized control clinical study demonstrates that GH treatment of middle aged (average age 50.3 years) HIV patients for 1 year can regenerate the thymus. Authors show that GH-induced increased circulating IGF-1 levels were associated with increased thymic volumes, recent thymic emigrants and naïve T cells in the blood.
- 53.Chu YW, Schmitz S, Choudhury B, Telford W, Kapoor V, Garfield S, Howe D, Gress RE. Exogenous insulin-like growth factor 1 enhances thymopoiesis predominantly through thymic epithelial cell expansion. Blood. 2008;112:2836–2846. doi: 10.1182/blood-2008-04-149435. This study demonstrates that ablation of IGF1 signaling in thymocytes lowers thymic function. The 4 week long infusion of IGF1 via osmotic pumps increases thymic output by increasing thymocyte survival and TEC proliferation. Authors also demonstrate that IGF1 can enhance thymopoiesis in P-selectin ligand (PSGL1) knockout mice; overcoming the defects in progenitor homing into thymus by proving greater TEC niches for available T cell precursors to develop into mature naïve T cells.
- 54.Howard JK, Lord GM, Matarese G, Vendetti S, Ghatei MA, Ritter MA, Lechler RI, Bloom SR. Leptin protects mice from starvation-induced lymphoid atrophy and increases thymic cellularity in ob/ob mice. J Clin Invest. 1999;104:1051–1059. doi: 10.1172/JCI6762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Farooqi IS, Matarese G, Lord GM, Keogh JM, Lawrence E, Agwu C, Sanna V, Jebb SA, Perna F, Fontana S, Lechler RI, DePaoli AM, O'Rahilly S. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest. 2002;110:1093–1103. doi: 10.1172/JCI15693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Farooqi IS, Wangensteen T, Collins S, Kimber W, Matarese G, Keogh JM, Lank E, Bottomley B, Lopez-Fernandez J, Ferraz-Amaro I, Dattani MT, Ercan O, Myhre AG, Retterstol L, Stanhope R, Edge JA, McKenzie S, Lessan N, Ghodsi M, De Rosa V, Perna F, Fontana S, Barroso I, Undlien DE, O'Rahilly S. Clinical and molecular genetic spectrum of congenital deficiency of the leptin receptor. N Engl J Med. 2007;356:237–247. doi: 10.1056/NEJMoa063988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Trotter-Mayo RN, Roberts MR. Leptin acts in the periphery to protect thymocytes from glucocorticoid-mediated apoptosis in the absence of weight loss. Endocrinology. 2008;149:5209–5218. doi: 10.1210/en.2008-0476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen J, Li J, Lim FC, Wu Q, Douek DC, Scott DK, Ravussin E, Hsu HC, Jazwinski SM, Mountz JD. Louisiana Healthy Aging Study. Maintenance of naïve CD8 T cells in nonagenarians by leptin, IGFBP3 and T3. Mech Ageing Dev. 2010;131:29–37. doi: 10.1016/j.mad.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vallejo AN, Michel JJ, Bale LK, Lemster BH, Borghesi L, Conover CA. Resistance to age-dependent thymic atrophy in long-lived mice that are deficient in pregnancy-associated plasma protein A. Proc Natl Acad Sci U S A. 2009;106:11252–11257. doi: 10.1073/pnas.0807025106. This paper shows for the first time that long-lived PAPPA deficient animals have maintenance of thymic function with age and greater TCR repertoire diversity. Authors also provide initial evidence that PAPPA null mice are protected from age-related adipogenic transformation of thymus.