Increased Pathogenicity of a Reassortant 2009 Pandemic H1N1 Influenza Virus Containing an H5N1 Hemagglutinin (original) (raw)
Abstract
A novel H1N1 influenza virus emerged in 2009 (pH1N1) to become the first influenza pandemic of the 21st century. This virus is now cocirculating with highly pathogenic H5N1 avian influenza viruses in many parts of the world, raising concerns that a reassortment event may lead to highly pathogenic influenza strains with the capacity to infect humans more readily and cause severe disease. To investigate the virulence of pH1N1-H5N1 reassortant viruses, we created pH1N1 (A/California/04/2009) viruses expressing individual genes from an avian H5N1 influenza strain (A/Hong Kong/483/1997). Using several in vitro models of virus replication, we observed increased replication for a reassortant CA/09 virus expressing the hemagglutinin (HA) gene of HK/483 (CA/09-483HA) relative to that of either parental CA/09 virus or reassortant CA/09 expressing other HK/483 genes. This increased replication correlated with enhanced pathogenicity in infected mice similar to that of the parental HK/483 strain. The serial passage of the CA/09 parental virus and the CA/09-483HA virus through primary human lung epithelial cells resulted in increased pathogenicity, suggesting that these viruses easily adapt to humans and become more virulent. In contrast, serial passage attenuated the parental HK/483 virus in vitro and resulted in slightly reduced morbidity in vivo, suggesting that sustained replication in humans attenuates H5N1 avian influenza viruses. Taken together, these data suggest that reassortment between cocirculating human pH1N1 and avian H5N1 influenza strains will result in a virus with the potential for increased pathogenicity in mammals.
INTRODUCTION
In 1997, the first reported cases of human infection with a wholly avian influenza virus occurred in Hong Kong (9, 31). This initial outbreak with a highly pathogenic H5N1 virus caused only 18 documented infections and six deaths, but raised concerns that avian influenza viruses could become the next influenza pandemic. A new outbreak of H5N1 influenza began in 2003, with continual westward spread and human infection, resulting in 549 infections and 320 deaths (World Health Organization; http://www.who.int). Severe H5N1 disease in both humans and animal models is associated with increased virus replication and an exacerbated innate immune response characterized by elevated levels of proinflammatory cytokines and an increased pulmonary infiltration of macrophages (2, 8, 12, 24). Although the human H5N1 infections have largely been in patients who had close contact with infected birds, with little evidence of human-to-human spread, the enzootic disease in poultry, particularly in Southeast Asia, raises the possibility of continued human infections (5).
In the spring of 2009, a novel influenza virus of swine origin (pH1N1) emerged and rapidly spread across the globe, and it was recognized by the World Health Organization as the first influenza pandemic of the 21st century (3, 11). We are currently in the recovery phase of this pandemic, but pH1N1 virus is now the dominant H1N1 virus circulating in humans. While the pH1N1 virus caused fewer deaths than previous pandemics, it is highly transmissible and can establish infection in a wide range of hosts, including poultry (3). This last point is quite surprising, given the rigid species specificity displayed by most influenza strains. Additionally, pH1N1 has already begun to show a tendency for reassortment. A reassortant pH1N1 encoding the NA gene of a swine influenza virus has recently been isolated from pigs in Thailand (17). Of further concern, in some parts of the world pH1N1 is cocirculating with H5N1 viruses, creating the potential for reassortment between pH1N1 and H5N1 viruses.
The potential risk posed by the reassortment of circulating human influenza strains with H5N1 highly pathogenic avian influenza (HPAI) viruses necessitates a better understanding of the specific genetic factors that increase the pathogenicity of human influenza viruses. Recent studies have demonstrated a high level of genetic compatibility between currently circulating human influenza viruses and contemporary avian H5N1 strains, suggesting that the reassortment of these viruses in nature is possible (1, 6, 23). The pathogenicity of a number of these reassortant viruses was tested in mice, and a range of phenotypes was observed (1, 6). Additionally, Sun et al. demonstrated genetic compatibility and increased pathogenicity of several reassortant viruses derived from avian H9N2 and pH1N1 strains (32). However, the pathogenicity of reassortant viruses derived from the pH1N1 virus and HPAI H5N1 viruses and their potential for transmission has not been addressed.
To determine the phenotype of pH1N1-H5N1 reassortant viruses in vitro and in vivo, we used reverse genetics to create a strain of A/California/04/2009 pH1N1 (CA/09) virus expressing individual genes from the HPAI H5N1 A/Hong Kong/483/1997 virus (HK/483). Although HK/483 virus is no longer circulating in avian species, we chose this strain as a representative H5N1 virus on the advice of the St. Jude Children's Research Hospital biosafety committee. Previous studies have looked at the replication kinetics of many possible reassortment combinations between two influenza strains (1, 6, 28, 32). Our rationale for choosing to create single-gene reassortants was based on a desire to extend those studies and to learn more about the potential of individual H5 genes to influence the pathogenicity of pH1N1 virus in vivo. The coinfection of MDCK cells with pH1N1 and HPAI H5N1 influenza viruses does result in single-gene reassortant viruses in vitro, suggesting that these viruses can arise in nature (23). Indeed, it has been suggested that single-gene reassortment is common among H1N1 and H3N2 influenza viruses, and that the hemagglutinin (HA) gene is frequently involved in the reassortment event (33).
The expression of individual HK/483 genes on the background of CA/09 influenza virus resulted in variable pathogenicity in vitro and in vivo. However, the expression of the HA gene from HK/483 virus significantly increased the pathogenicity of CA/09 virus. This reassortant virus (CA/09-483HA) replicated more efficiently in differentiated, primary human respiratory epithelial cells grown at the air-liquid interface than both parental strains and caused 100% mortality in mice. In vivo infection with CA/09-483HA was associated with extrapulmonary dissemination, and mice were unable to clear the virus from the lungs. These results confirm previous reports demonstrating variable pathogenicity associated with reassortant viruses derived from human and avian influenza strains and show, for the first time, that reassortment between HPAI H5N1 and pH1N1 viruses could give rise to an influenza virus strain with enhanced pathogenicity.
MATERIALS AND METHODS
Ethics statement.
All procedures were approved by the St. Jude Children's Research Hospital Institutional Biosafety Committee (IBC) and IACUC and were in compliance with the Guide for the Care and Use of Laboratory Animals. These guidelines were established by the Institute of Laboratory Animal Resources and approved by the Governing Board of the U.S. National Research Council.
Laboratory facilities.
All experiments using parental H5N1 and CA/09 viruses containing H5 HA were conducted in a biosafety level 3 enhanced containment laboratory (26). Investigators were required to wear appropriate respirator equipment (RACAL; Health and Safety Inc., Frederick, MD). Mice were housed in HEPA-filtered, negative-pressure, vented isolation containers. All other viruses were used under enhanced biosafety level 2 conditions by vaccinated personnel.
Viruses.
A/California/04/2009 pH1N1 virus was propagated in the allantoic cavity of 10-day-old specific-pathogen-free embryonated chicken eggs at 37°C. Allantoic fluid was harvested, cleared by centrifugation, and stored at −80°C. A/Hong Kong/483/1997 H5N1 virus was propagated in Madin Darby canine kidney (MDCK) cells as described previously (4, 16).
Cells and culture media.
MDCK cells were cultured in Eagle's minimum essential medium (MediaTech, Manassas, VA) supplemented with 2 mM glutamine and 10% fetal bovine serum (FBS; Gemini BioProducts, West Sacramento, CA) and grown at 37°C under 5% CO2. A549 cells were cultured in Dulbecco's minimum essential medium (DMEM; Lonza, Walkersville, MD) supplemented with 4.5 g/liter glutamine and 10% FBS and grown at 37°C under 5% CO2. Well-differentiated (transepithelial resistance of greater than 1,000 Ω), primary normal human bronchial epithelial cells (NHBE) were purchased from MatTek Corp (Ashland, MA), maintained by daily washes with 0.9% sodium chloride solution (Sigma, St. Louis, MO), and incubated at the air-liquid interface at 37°C under 5% CO2. The basal surface was in contact with AIR 100 growth medium (MatTek Corp), with complete growth medium being replaced every 24 h.
Reverse genetics.
The CA/09 viruses expressing HK/483 genes were generated using the eight-plasmid system as described previously (14) and were confirmed by sequence analysis. Viral titers were determined by 50% tissue culture infectious dose (TCID50) analysis in MDCK cells as described previously (25). The limit of detection for the TCID50 assay was 101 TCID50 units/ml. All in vitro experiments were performed with at least two different preparations of the reassortant virus.
In vitro infections.
A549 and MDCK cells were infected at a multiplicity of infection (MOI) of 0.01 for 1 h at 37°C. Cells were washed three times to remove unbound virus, and infected cells were cultured in appropriate medium containing 0.075% bovine serum albumin (BSA) and 1 μg/ml l-1-tosylamido-2-phenylethyl chloromethyl ketone (TPCK)-treated trypsin, except the parental HK/483 and CA/09-483 viruses, which were cultured in the absence of trypsin. Aliquots of culture supernatants were collected at 6, 24, 48, and 72 hours postinfection (hpi) and immediately stored at −80°C for the determination of virus titers. For the infection of NHBE cells, basal medium was removed and replaced with DMEM. The apical surface was washed twice and incubated with fresh, serum-free DMEM-containing virus for 2 h at 37°C, after which both apical and basal media were removed, and fresh growth medium added to the basal chamber. At 6, 24, 48, and 72 hpi, DMEM was added to the apical surface and incubated for 30 min at 37°C. This medium was collected and stored at −80°C for the determination of virus titers.
Serial passage of viruses.
NHBE cells cultured at the air-liquid interface were infected with CA/09, HK/483, or CA/09-483HA virus at an MOI of approximately 0.03. At 24, 48, and 72 hpi, DMEM was added to the apical surface and collected as described above. Virus titers in the samples (passage 1 [p1]) were determined by TCID50 analysis, and equivalent TCID50 units of each sample taken at 72 hpi were used to inoculate a new well of NHBE cells. This process was repeated until a third passage was obtained.
Immunofluorescent microscopy.
To determine viral spread in NHBE cells, inserts from passage 2 virus-infected cells at 48 hpi were fixed in cold 1:1 methanol/acetone for 5 min, washed with phosphate-buffered saline (PBS), and incubated in 0.1% Triton X-100-PBS for 10 min at room temperature. After blocking with PBS containing 1% BSA for 30 min at room temperature, inserts were incubated with a mouse monoclonal anti-influenza NP antibody as described previously (19). The cells then were incubated with Alexa 488-conjugated goat anti-mouse IgG (Invitrogen, 1:200) and 4′,6′-diamidino-2-phenylindole (DAPI) (1:1,000) at 4°C for 24 h and mounted with Permount. Confocal microscopy was performed on a Nikon TE2000 E2 microscope equipped with a Nikon C1Si confocal scan head. Excitation was with 404- and 488 nm diode-pumped solid-state lasers, and the emission was collected through 450/35 and 515/60 band pass filters. Images were acquired with a Nikon 40×, 1.3-numeric-aperture Plan Fluor objective and Nikon EZC1 software.
Animal experiments.
Six- to 8-week-old female BALB/c mice (Jackson Laboratory, Bar Harbor, ME) were lightly anesthetized with isofluorane and intranasally inoculated with PBS or 103 TCID50 units of parental or reverse-genetic reassortant viruses in 25 μl PBS. Mice were monitored daily for clinical signs of infection and weighed every 48 hpi (21). At different times postinfection, three control and three infected mice were euthanized by CO2 asphyxiation, and tissues were harvested. Tissues were either washed and immediately stored in 10% buffered formalin for histological analysis or homogenized in 1 ml PBS, and viral titers were determined by TCID50 analysis (16).
For transmission studies, two male ferrets (9 to 15 weeks old; Triple F Farms, Sayre, PA) were inoculated intranasally with 104 TCID50 units of parental or reverse-genetic reassortant virus in 1 ml PBS. Twenty-four hours postinoculation, two naïve ferrets were introduced into the same cage and housed with the inoculated ferrets for the duration of the experiment. Body weight and temperature were assessed every 48 h, and the ferrets were monitored for the following clinical signs: anorexia, sneezing, nasal discharge, and lethargy. Nasal washes were collected at 1 day pi (dpi) for infected ferrets only, at 3, 5, and 7 dpi for all ferrets, and at 10 dpi for contact ferrets only. To collect nasal washes, the ferrets were anesthetized intramuscularly with 0.4 ml of a ketamine-xylazine mixture (30 mg/kg of body weight ketamine and 3 mg/kg xylazine) to induce sneezing, and 0.5 ml of sterile PBS containing antibiotics (100 U/ml penicillin, 100 μg/ml streptomycin, and 50 μg/ml gentamicin) was added dropwise to each nostril. Nasal washes were collected in a sterile specimen cup, and viral titers were determined by TCID50 analysis.
Histopathology.
Tissues were fixed in 10% buffered formalin, processed, and paraffin embedded. Four-micron-thick sections were stained with hematoxylin and eosin by the St. Jude Veterinary Pathology Core Facility.
Statistical analysis.
Statistical analyses were performed using JMP statistical software (SAS Institute, Cary, NC). Nonparametric data were analyzed using a Kruskal-Wallis test (α = 0.05). Normally distributed data were analyzed by two-way analysis of variance (ANOVA) with virus type and day postinfection as the main effects. Student's t test was used for post hoc comparisons between the virus groups and for post hoc comparisons between the days postinfection. Differences were considered significant at P < 0.05.
RESULTS
Replicative ability of pH1N1-H5N1 reassortant viruses in vitro.
Given that the pH1N1 virus is cocirculating with H5N1 viruses in many parts of the world, the replicative ability and pathogenicity of H1-H5 reassortant viruses were assessed. Specifically, we asked how individual genes from an H5N1 virus affect the virulence of pH1N1 CA/09 virus. Thus, CA/09 virus expressing individual genes from HK/483 virus, a highly pathogenic avian influenza strain, were created by reverse genetics, and the replicative capacity of these viruses first was tested in vitro in MDCK cells (Fig. 1A). Briefly, cells were infected at an MOI of 0.01 with the parental or reassortant viruses, and viral titers were determined at several times postinfection by TCID50 analysis. Compared to both parental strains, CA/09 viruses expressing the HK/483 PB1, PB2, PA, NP, NA, M, or NS gene were significantly reduced at all time points. The CA/09 virus expressing the HK/483 H5 HA gene (CA/09-483HA) replicated without the addition of exogenous trypsin to higher titers in MDCK cells than both parental strains.
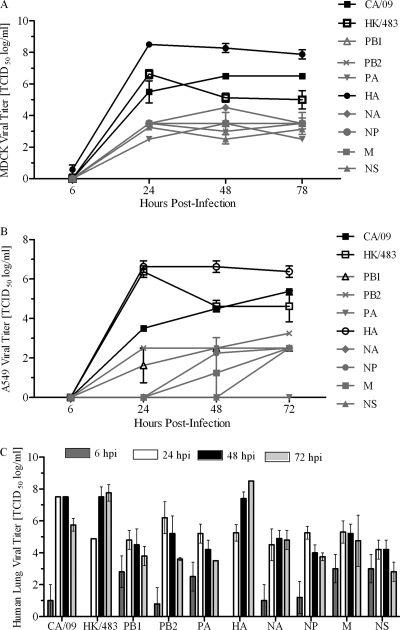
Fig. 1.
Replicative capacity of reassortant pH1N1-H5N1 viruses in vitro. MDCK (A) and A549 (B) cells were infected at an MOI of 0.01, cell culture supernatants were collected at 6, 24, 48, and 72 hpi, and viral titers were determined by TCID50 analysis. (C) NHBE cells were infected at an MOI of 0.03 for 2 h at 37°C. Following infection, the cells were maintained in culture at an air-liquid interface. At 6, 24, 48, and 72 hpi, medium was added to the apical surface for 30 min and collected, and viral titers were determined by TCID50 analysis in triplicate. Data are representative of at least two experiments. Error bars represent the standard errors of the means. Individual influenza virus genes indicate reassortant CA/09 virus expressing a single gene from HK/483 virus.
While MDCK cells represent the standard for analyzing the replicative capacity of influenza strains, influenza viruses preferentially infect cells of the respiratory tract of humans. Thus, the replication of the reassortant viruses was tested in human A549 cells (Fig. 1B). Similarly to the results with MDCK cells, CA/09 viruses expressing the HK/483 PB1, PB2, PA, NA, NP, M, and NS genes had significantly decreased titers in A549 cells compared to those of both parental strains at all time points postinfection (P < 0.05). Indeed, for several of the strains (NA, NP, M, and NS), virus was not detected in the supernatant until 48 hpi. No virus was detected at any time point for the CA/09 virus expressing the PA gene of HK/483. As seen with the MDCK cells, the CA/09-483HA virus replicated to the highest titers relative to those of all other strains.
While A549 cells are a better representation of the primary target cell type infected by influenza viruses, these cells are a pulmonary adenocarcinoma cell line and may not be the best model of viral replication in the lung epithelium. Therefore, the panel of reassortant viruses was tested in well-differentiated, normal human bronchial epithelial cells (NHBE) cultured at an air-liquid interface (Fig. 1C). Similarly to the observations in MDCK and A549 cells, in NHBE cells CA/09 viruses expressing the HK/483 PB1, PB2, PA, NA, NP, M, or NS gene were attenuated compared to the parental strains, while CA/09-483HA replicated to peak titers (∼108 TCID50/ml) and with kinetics similar to those of the parental HK/483.
In vivo pathogenicity of pH1N1-H5N1 reassortant viruses.
To determine the in vivo phenotype of the pH1N1-H5N1 reassortant viruses, mice were infected with each virus at a dose of 103 TCID50 units, and weight loss and survival were monitored for 10 to 12 dpi (Fig. 2). Mice infected with the parental CA/09 virus experienced mild disease resulting in ∼10% weight loss by 4 dpi, with all mice fully recovering by 10 dpi. In contrast, mice infected with the parental HK/483 virus lost ∼25% of their preinfection weight by 6 dpi, with 100% of the mice requiring euthanasia due to hind-limb paralysis (Fig. 2A). Mice infected with the reassortant viruses experienced a range of illness. The CA/09 virus expressing the PA, NP, NA, or M gene of HK/483 experienced no weight loss, while the expression of the HK/483 PB1, PB2, or NS gene on the CA/09 background resulted in 10 to 15% weight loss; however, these mice fully recovered from infection (Fig. 2A). Of these three reassortant viruses, mice infected with CA/09-483PB1 had a prolonged recovery period marked by significant weight loss (P < 0.05) at 8 and 10 dpi relative to that of the CA/09 parental virus (Fig. 2A).
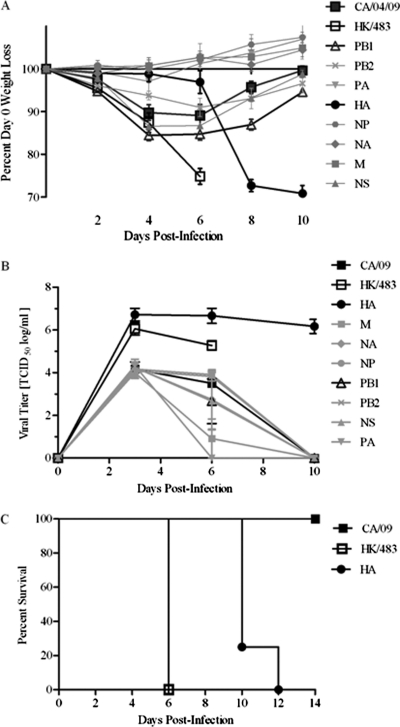
Fig. 2.
Pathogenicity of reassortant pH1N1-H5N1 viruses in vivo. Female 6- to 8-week-old BALB/c mice (n = 10) were intranasally infected with 103 TCID50 units of the indicated viruses, and weight loss (A) and survival (B) were monitored for 14 dpi. (C) At 3, 6, and 10 dpi, lungs were collected from three mice per group, and viral titers were determined in homogenates by TCID50 analysis. Data are representative of at least two experiments, and error bars represent the standard errors of the means. Individual influenza virus genes indicate reassortant CA/09 virus expressing a single gene from HK/483 virus.
We next asked whether the increased morbidity in the mice infected with the CA/09 virus expressing the PB1, PB2, or NS gene of HK/483 was associated with elevated virus titers in the lungs (Fig. 2B). At 3 dpi there was no differences in the levels of virus in the lungs of mice infected with the parental CA/09 virus or CA/09 expressing the PB1, PB2, PA, NA, NP, M, or NS gene of HK/483. By 6 dpi, the mice infected with CA/09 expressing the HK/483 NA or M gene had almost completely cleared the virus from the lungs, which is consistent with the observation that these mice did not lose any weight. Virus titers in the mice infected with CA/09 expressing the PB1, PB2, PA, NP, or NS genes of HK/483 still were not statistically different at 6 dpi than those of mice infected with the parental CA/09 virus. By 10 dpi, all of the mice had cleared the virus from the lungs. These data are consistent with the morbidity that was observed during infection and demonstrates that the more severe morbidity associated with the CA/09-483PB1 virus was independent of increased virus replication.
In contrast, mice infected with the CA/09-483HA virus exhibited the most severe phenotype. While they maintained their preinfection weight longer than mice infected with either the parental CA/09 virus or any of the other reassortant viruses, between 6 and 8 dpi there was a rapid and dramatic weight loss comparable to that caused by the parental HK/483 virus. As a result, 80% of the CA/09-483HA-infected mice had to be euthanized by 10 dpi, increasing to 100% by 12 dpi (Fig. 2C). This dramatic morbidity was associated with elevated viral titers. CA/09-483HA-infected mice had significantly increased viral titers in the lungs compared to mice infected with parental CA/09 at 3 (6.7 ± 0.3 versus 4.2 ± 0.2; P < 0.05) and 6 dpi (6.7 ± 0.4 versus 3.5 ± 0; _P_ < 0.05) or parental HK/483 at 6 dpi (6.7 ± 0.4 versus 5.3 ± 0.2; _P_ < 0.05). Even at 10 dpi, there was no significant decrease in lung titers in the CA/09-483HA-infected mice (6.2 ± 0.3) (Fig. 2B), suggesting a problem with viral clearance. Given the enhanced morbidity, the 50% mouse lethal dose (MLD50) was determined. These studies showed that the addition of the HK/483 HA gene caused a significant increase in virulence, going from an MLD50 of >105 TCID50 units with the parental CA/09 virus to 102.5 with the CA/09-483HA virus. The MLD50 of the parental HK/483 virus is 101.5 (data not shown).
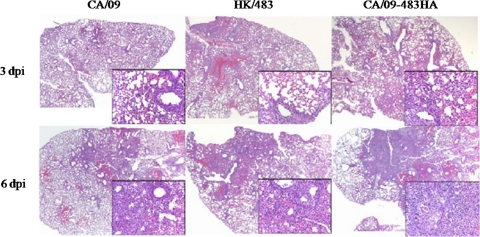
The CA/09-483HA-infected mice also had the most severe pulmonary disease, consisting of extensive bronchiole and alveolar lesions at both 3 and 6 dpi (Fig. 3). This contrasts with the CA/09- and HK/483-infected mice, which had less overall alveolar involvement in both groups. Although the HK/483-infected mice had more extensive bronchiolar involvement than the CA/09 virus-infected group, it remained less than that of the CA/09-483HA-infected mice. Regardless of the viral strain, the lung lesions primarily consisted of bronchiole epithelial necrosis, alveolitis with pneumocyte hyperplasia and mixed inflammatory cell infiltrates, interstitial thickening, and perivascular mononuclear cell aggregates with more extensive pathology at 6 dpi than at 3 dpi (Fig. 3).
Fig. 3.
Histological analysis of CA/09-483HA infection. Female 6- to 8-week-old BALB/c mice (n = 3) were inoculated with 103 TCID50 units of the indicated viruses. Lung tissue was collected at 3 or 6 dpi, fixed in 10% buffered formalin, processed, and embedded in paraffin. Four-micron-thick sections were stained with hematoxylin and eosin.
A hallmark of HPAI H5N1 viruses is the ability to replicate in extrapulmonary tissues (15, 36). Mice infected with HK/483 had virus in the kidneys at 3 dpi (3.3 ± 2.0 TCID50/ml) and the brain at 6 dpi (3.2 ± 0.5 TCID50/ml), which accounts for the hind-limb paralysis; CA/09-483HA-infected mice had virus in the kidney on both 3 and 6 dpi (2.2 ± 0.4 and 1.2 ± 0.5 TCID50/ml, respectively) but not in the brain (data not shown). Virus was not recovered from any extrapulmonary tissue in the CA/09 virus-infected mice. Thus, while the expression of several genes from an HPAI H5 virus on the genetic background of CA/09 is capable of causing increased morbidity in vivo, only the expression of the HA gene is sufficient to cause lethal disease in mice similar to that seen with a wild-type H5N1 infection. Given these results, the remainder of the experiments focused on the CA/09-483HA virus.
Virus adaptation in primary human lung epithelial cells.
Given the increased replicative ability and pathogenicity of the CA/09-483HA virus in vitro and in vivo, we next asked whether this virus could sustain replication in primary human bronchial epithelial cells. To test this, the parental and CA/09-483HA viruses were serially passaged three times in differentiated NHBE cells cultured at the air-liquid interface. Both the parental and CA/09-483HA viruses replicated to high titers with passaging, indicating a good sustainment of replicative capacity during subsequent transfer to new NHBE cells (Fig. 4). The parental HK/483 virus replicated well during the first passage, up to 107.75 TCID50/ml by 72 hpi, but became significantly attenuated during the subsequent two passages, reaching a maximum of 105.5 TCID50/ml (Fig. 4A). Differences in their growth kinetics also were noted between the viral strains. Viral titers in NHBE cells consistently peaked for the parental CA/09 virus at 48 hpi, while titers peaked for the parental HK/483 virus between 48 and 72 hpi with increased time to peak titers with each subsequent passage. The CA/09-483HA virus appears to have switched replication kinetics after three passages. During the first passage, replication kinetics are similar to those of the parental HK/483 virus, with titer peak at 72 hpi. However, after three passages, the CA/09-483HA virus replication kinetics are similar to those of the parental CA/09 virus, with peak titers at 48 hpi with titers almost 100-fold higher than those of the parental strain, from 107.5 to 109.25 TCID50/ml, respectively. This suggests that a CA/09 virus that acquires the HA gene from an H5 strain is capable of sustained replication in human lung cells.
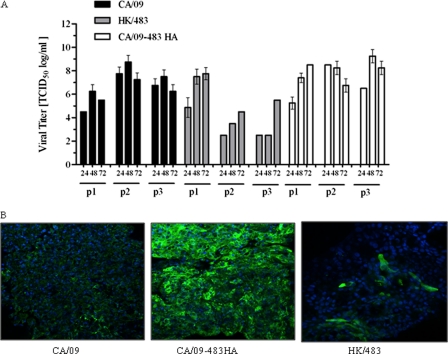
Fig. 4.
Replication of serially passaged viruses in vitro. (A) NHBE cells were inoculated with the indicated viruses at an MOI of 0.03 at 37°C for 2 h. At 24, 48, and 72 hpi medium was added to the apical surface for 30 min and collected, and viral titers were determined by TCID50 analysis in triplicate. This represents one passage (p1). Equal TCID50 doses of each virus from the sample of p1 at 72 h was used to infect another monolayer of NHBE cells at an MOI of 0.03. This procedure was repeated until p3 virus was collected. Error bars represent the standard errors of the means. (B) At 48 hpi, inserts from NHBE cells infected with the p2 viruses were fixed, stained for the viral NP (green) and nuclei by DAPI (blue), and visualized by confocal microscopy.
To ensure that the decreased replication of the parental HK/483 virus observed after passaging in NHBE cells was not due to changes leading to decreased growth in the MDCK cells, which were used to determine viral titers, the inserts from NHBE cells infected with the different passage 2 viruses were monitored for viral NP levels by immunofluorescent staining at 48 hpi (Fig. 4B). Consistent with the MDCK cell results, there was less NP staining in the NHBE cells infected with the HK/483 passage 2 virus than with the CA/09 or CA/09-483HA virus (Fig. 4B).
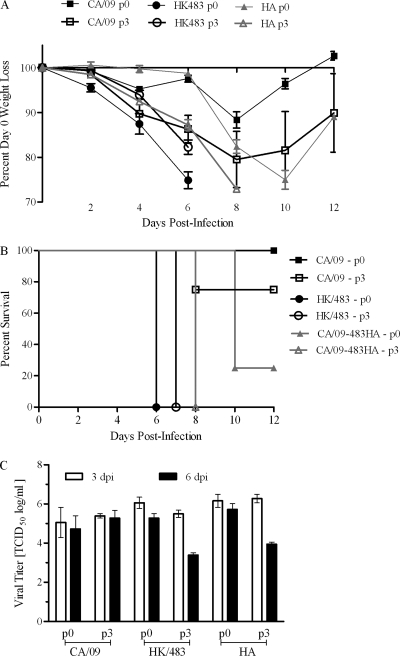
Pathogenicity of the NHBE-passaged viruses in mice.
To study the effects of adapting parental CA/09, HK/483, and CA/09-483HA viruses in primary lung epithelial cells on the in vivo phenotype, 6-week-old BALB/c mice were infected with 103 TCID50 units of either unpassaged virus (p0) or virus that had been passaged three times in NHBE cells (p3). The mice infected with the p0 viruses experienced morbidity and mortality levels similar to those previously observed (Fig. 1), with the exception that one animal survived infection with CA/09-483HA virus (Fig. 5B). In contrast, infection with CA/09 or CA/09-483HA p3 virus caused significantly more weight loss at earlier times postinfection (P < 0.05) (Fig. 5A). Surprisingly, one animal succumbed to infection with the CA/09 p3 virus, suggesting that the passage of this virus through human lung cells increases pathogenicity in mammals. However, this observation was not statistically significant (Fig. 5B). All of the mice infected with the CA/09-483HA p3 virus succumbed by 8 dpi, a time to death 2 days faster than that for the mice infected with the p0 virus (compare Fig. 1 to 5B). Similar to the p0 virus, mice infected with the HK/483 p3 virus became paralyzed and had to be euthanized. However, the mice survived 1 day longer. While this was not a significant delay in time to death, it is an interesting trend that warrants further investigation. Finally, lung viral titers were measured at 3 and 6 dpi. In spite of the increased morbidity, viral titers were identical in the CA/09 p0- and p3-infected mice at both days postinfection. In contrast, there was enhanced clearance at 6 dpi in the p3-infected HK/483 and CA/09-483HA-infected mice (Fig. 5C). This contrasts with the p0-infected mice, where no viral clearance was observed prior to the death of the animal (Fig. 2C and 5C). These studies suggest that adaptation through differentiated primary lung cells rapidly influences pathogenicity and viral replication in infected animals.
Fig. 5.
In vivo pathogenicity of serially passaged viruses. Female 6- to 8-week-old BALB/c mice (n = 10) were intranasally inoculated with 103 TCID50 units of the indicated viruses, and weight loss (A) and survival (B) were monitored for 12 dpi. (C) At 3 and 6 dpi, lungs were collected from three mice per group and viral titers were determined in homogenates by TCID50 analysis. Error bars represent the standard errors of the means.
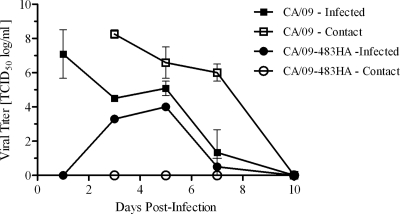
Transmissibility of CA/09-483HA.
One of the critical factors in the development of a pandemic influenza strain is the ability to transmit efficiently from human to human. The ability of pH1N1 to transmit in ferrets has been established (19). Thus, the transmissibility of the CA/09-483HA virus was assessed. Briefly, two ferrets were inoculated with 105 TCID50 of CA/09, HK/483, or CA/09-483HA virus, and 24 h later two naïve contact ferrets were introduced as cage mates. Viral titers were determined from nasal washes collected at various times postinfection. As previously shown, HK/483 virus infection caused significant weight loss (∼20%) and some decrease in activity level, but the virus did not transmit to the contact ferrets (data not shown; also see reference 37). In contrast, virus shedding in the CA/09-infected ferrets peaked at 1 dpi and was cleared by day 10 pi (Fig. 6). This virus transmitted to the contact ferrets with similar peak titers and clearance kinetics. Both the CA/09 virus-infected and contact ferrets lost weight during the course of infection, but no other clinical symptoms were observed. The CA/09-483HA virus also was shed from the infected ferrets, although shedding was delayed (3 versus 1 dpi) and peak titers were decreased relative to that of the CA/09 virus (103.3 versus 107.1 TCID50/ml). More importantly, despite replicative capacity similar to that of the parental CA/09 virus in a human lung cell, the CA/09-483HA virus did not transmit to contact ferrets (Fig. 6). Despite actively shedding the virus, CA/09-483HA virus-infected ferrets did not display any clinical symptoms during the course of infection. Overall, these data suggest that although a CA/09 virus containing an HPAI H5N1 HA is quite capable of enhanced growth in human lung cells and increased pathogenicity in an animal model, it does not transmit effectively.
Fig. 6.
Transmissibility of CA/09-483HA in ferrets. Male 9- to 15-week-old ferrets (n = 2) were intranasally inoculated with 104 TCID50 units of the indicated viruses. Twenty-four hpi, two naïve contact ferrets were introduced and housed together with the inoculated ferrets for the duration of the experiment. Nasal washes were collected, and viral titers were determined by TCID50 analysis at 1, 3, 5, and 7 dpi for the inoculated ferrets and at 3, 5, 7, and 10 days postexposure for the contact ferrets. Error bars represent standard errors of the means.
DISCUSSION
The evolutionary adaptation of influenza viruses by reassortment can result in antigenic shift and the development of novel, potentially pandemic strains (22). Given the documented promiscuity of pH1N1 to infect across the species barrier and to reassort with other circulating influenza viruses (3, 17), and that multiple lineages of avian H5N1 now are cocirculating with pH1N1 viruses, the potential exists for the emergence of mammalian-adapted strains incorporating genes from HPAI H5N1 viruses which could present a major public health threat. Previous studies demonstrated a high level of genetic compatibility between avian and human influenza strains and, in the event of a coinfection in a susceptible host, reassortment between seasonal or pandemic human strains and HPAI H5N1 viruses is possible (1, 6, 23). While increased pathogenicity was observed between human H3N2 and HPAI H5N1 viruses (1, 6), previous studies have not addressed the pathogenic potential of reassortant viruses derived from pH1N1 and HPAI H5N1 viruses in vivo, or the ability of these viruses to spread within the human population. Therefore, in this study we used reverse genetics to create a CA/09 virus expressing single genes from an HPAI H5N1 virus to evaluate their pathogenic potential both in vitro and in vivo and to observe the potential for these reassortant viruses to adapt and spread in the human population.
The in vitro inoculation of parental and reassortant viruses onto MDCK cells revealed differences in the replicative ability of the various viruses (Fig. 1). CA/09-483HA replicated to significantly higher titers than both parental CA/09 and parental HK/483 viruses, while the reassortant CA/09 viruses expressing the seven other genes of HK/483 had an attenuated phenotype. Similar observations were made in A549 and NHBE cells. In each case, CA/09-483HA replicated with similar or greater efficiency than the parental viruses. The level of attenuation for the reassortant viruses was most dramatic in the A549 cells. Octaviani et al. found that H5N1 viruses expressing PB1 and PB2, separately or in combination, from CA/09 showed enhanced growth in A549-M2 cells compared to that of the parental H5N1 strain (23). While these viruses showed a gain of function, our results show a loss of function with the opposite reassortment, suggesting an important role for these genes in the replication kinetics of H5N1 strains. Most interestingly about the in vitro data, striking differences were seen between the three in vitro models (Fig. 1). Several of the reassortant viruses (PA, NA, NP, M, and NS) were extremely attenuated in the A549 model, while they were able to replicate efficiently in the NHBE and MDCK cells. While the exact mechanisms for these differences are not yet known, there are obvious differences between MDCK, A549, and NHBE cell types and their abilities to support virus growth. These data suggest that the differences seen in replication in A549 cells compared to that in NHBE cells offer a good model to study host factors required for influenza replication in different types of human lung cells. Further, it is possible that the cellular factors required for optimal viral replication will differ among cells from different regions of the respiratory tract, making parallel studies in well-differentiated primary human lung, tracheal, and nasal epithelium of great interest.
While Octaviani et al. showed that H5N1 and pH1N1 had a high level of genetic compatibility and were able to reassort into viable strains in a coinfection model, the pathogenicity of these reassortants was not addressed (23). Therefore, we compared the pathogenicity of all eight reassortant viruses to those of their parental strains using the BALB/c mouse model. Consistently with our in vitro observations, CA/09-483HA was highly pathogenic, resulting in increased mortality, reduced viral clearance in the lungs, and increased pulmonary pathology (Fig. 2 and 3). The insertion of the H5N1 HA into pH1N1 also resulted in extrapulmonary spread in mice, which is a hallmark of the H5N1 viruses (15, 36). It is unknown why the CA/09-483HA virus, unlike the parental HK/483 virus, was unable to spread to the brain despite replication in the kidney.
Apart from the CA/09-483HA virus, the majority of the pH1N1-H5N1 reassortant viruses exhibited equivalent or attenuated pathogenicity compared to that of the parental CA/09 virus, which also is consistent with the in vitro data. The CA/09 virus expressing the HK/483 PB1 gene caused significantly increased weight loss compared to that caused by the parental CA/09 virus. However, this reassortant virus did not grow to higher titers in the lungs of infected mice, indicating that HK/483 PB1 was driving an increased inflammatory response. Many strains of PB1 encode a second protein, PB1-F2, from an alternative open reading frame that is involved in cell death regulation and viral pathogenesis (7, 10, 20). Specifically, the N66S mutation in the PB1-F2 protein of several H5N1 influenza strains, including HK/483, has been associated with the high pathogenicity observed for these viruses (10). The pH1N1 virus does not express a functional PB1-F2 (13). Thus, the increased morbidity observed for the CA/09 virus expressing the PB1 gene of HK/483 may be due to effects of the PB1-F2 protein. Studies are under way to address the contribution of PB1-F2 and exacerbated inflammation to increased morbidity associated with infection with this virus.
Aside from increased pathogenicity, the development of a potentially pandemic influenza strain requires this pathogenicity to be retained in newly infected hosts. To ask whether the CA/09-483HA virus, as well as the parental strains, retain their replicative capability over time in primary human lung cells, the viruses were serially passaged in differentiated NHBE cells. Both the parental CA/09 virus and CA/09-483HA replicated to higher titers in NHBE cells after three passages than after the first round of replication (Fig. 4). These changes in replicative capacity were relevant, as the passaged viruses had increased pathogenicity and mortality in BALB/c mice compared to that of the unpassaged strains (Fig. 5). These results suggest that the reassortant HA virus not only has the capacity for increased pathogenicity and replication but it also could retain, and even augment, this ability when going from one host to the next. Surprisingly, in contrast to the other two viruses, the parental HK/483 virus lost replicative ability following serial passage (Fig. 4). This correlated with significantly less weight loss in vivo, and death occurred 1 day later than for the unpassaged virus (Fig. 5). Although this slight delay in time to death was not statistically significant, the decreased morbidity is intriguing and warrants further studies to investigate whether this virus can be further attenuated by continued serial passage. This is the first evidence that an HPAI H5N1 virus loses replicative capacity over time in human lung cells. This is an important observation for public health and may explain why these viruses have not yet to become firmly established in humans. Full genomic sequence analysis is under way to determine if specific mutations lead to enhanced/decreased pathogenicity during passaging in primary human lung cells.
The combination of viral genes that accommodate transmission in humans, a critical step in the development of a pandemic strain, is not completely understood. In our study, the CA/09-483HA virus, despite displaying increased pathogenicity in mice, was unable to transmit in a ferret model (Fig. 6). The HA molecule of HPAI H5N1 influenza viruses preferentially recognizes α2,3-linked sialic acid receptors, and it is thought that this restricts the transmission of avian influenza viruses in mammals (27, 30, 35). However, others have demonstrated that transmissibility is a multigenic trait, involving the PB2 gene as well, and cannot be predicted based on HA sequence alone (18, 29, 34, 37). Thus, there is likely a combination of genes, working in tandem, which permits efficient transmission. Ongoing studies are focused on exploring the transmissibility of the other pH1N1-H5N1 reassortant viruses, with particular interest in the CA/09 virus expressing polymerase components from HPAI H5N1 influenza viruses.
H5N1 viruses continue to circulate in domestic bird populations throughout much of the world and pose a serious health risk to humans. We have demonstrated that the reassortment of an HPAI H5N1 virus strain with 2009 pH1N1 has the potential to result in a highly pathogenic virus in mammals, confounding the host's ability to control virus replication. These results support ongoing public health efforts to monitor the evolution of influenza viruses in nature and warrant future work to continue to elucidate the mechanisms of influenza virus transmission in humans.
ACKNOWLEDGMENTS
We thank Ashley Webb and Jeri Carol Crumpton for expert technical assistance; Jennifer Peters at the St. Jude Cell and Tissue Imaging Center; Alexander Klimov at the Centers for Disease Control and Prevention for the A/Hong Kong/483/97 (HK/483) H5N1 influenza virus; Yoshihiro Kawaoka at the University of Wisconsin and Subrata Barman from St. Jude Children's Research Hospital for the HK/483 and CA/09 reverse genetics plasmids; Robert Webster and Pamela McKenzie for the critical review of the manuscript; Paul Thomas, Andrew Burnham, and Kevin O'Brien for insightful discussions; and the St. Jude Veterinary Pathology Core.
This work was supported by NIH NIAID contract number HHSN266200700005C, the American Lebanese Syrian Associated Charities (ALSAC), and the St. Jude NIH Cancer Core facility (J.E.R.).
Footnotes
▿
Published ahead of print on 14 September 2011.
REFERENCES
- 1.Ashburn D. D., DeAntonio A., Reed M. J. 2010. Pulmonary system and obesity. Crit. Care Clin. 26:597–602 [DOI] [PubMed] [Google Scholar]
- 2.Baskin C. R., et al. 2009. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc. Natl. Acad. Sci. U. S. A. 106:3455–3460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berhane Y., et al. 2010. Molecular characterization of pandemic H1N1 influenza viruses isolated from turkeys and pathogenicity of a human pH1N1 isolate in turkeys. Avian Dis. 54:1275–1285 [DOI] [PubMed] [Google Scholar]
- 4.Carlson C. M., et al. 2010. Transforming growth factor-beta: activation by neuraminidase and role in highly pathogenic H5N1 influenza pathogenesis. PLoS Pathog. 6:e1001136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen H., et al. 2006. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc. Natl. Acad. Sci. U. S. A. 103:2845–2850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen L. M., Davis C. T., Zhou H., Cox N. J., Donis R. O. 2008. Genetic compatibility and virulence of reassortants derived from contemporary avian H5N1 and human H3N2 influenza A viruses. PLoS Pathog. 4:e1000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen W., et al. 2001. A novel influenza A virus mitochondrial protein that induces cell death. Nat. Med. 7:1306–1312 [DOI] [PubMed] [Google Scholar]
- 8.Cheung C. Y., et al. 2002. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet 360:1831–1837 [DOI] [PubMed] [Google Scholar]
- 9.Claas E. C., et al. 1998. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 351:472–477 [DOI] [PubMed] [Google Scholar]
- 10.Conenello G. M., Palese P. 2007. Influenza A virus PB1-F2: a small protein with a big punch. Cell Host Microbe 2:207–209 [DOI] [PubMed] [Google Scholar]
- 11.Dawood F. S., et al. 2009. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 360:2605–2615 [DOI] [PubMed] [Google Scholar]
- 12.de Jong M. D., et al. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 12:1203–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hai R., et al. 2010. PB1-F2 expression by the 2009 pandemic H1N1 influenza virus has minimal impact on virulence in animal models. J. Virol. 84:4442–4450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffmann E., Krauss S., Perez D., Webby R., Webster R. G. 2002. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine 20:3165–3170 [DOI] [PubMed] [Google Scholar]
- 15.Horimoto T., Kawaoka Y. 1994. Reverse genetics provides direct evidence for a correlation of hemagglutinin cleavability and virulence of an avian influenza A virus. J. Virol. 68:3120–3128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones J. C., Turpin E. A., Bultmann H., Brandt C. R., Schultz-Cherry S. 2006. Inhibition of influenza virus infection by a novel antiviral peptide that targets viral attachment to cells. J. Virol. 80:11960–11967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kitikoon P., et al. 2009. Vaccine efficacy and immune response to swine influenza virus challenge in pigs infected with porcine reproductive and respiratory syndrome virus at the time of SIV vaccination. Vet. Microbiol. 139:235–244 [DOI] [PubMed] [Google Scholar]
- 18.Maines T. R., et al. 2006. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc. Natl. Acad. Sci. U. S. A. 103:12121–12126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maines T. R., et al. 2009. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science 325:484–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAuley J. L., Zhang K., McCullers J. A. 2010. The effects of influenza A virus PB1-F2 protein on polymerase activity are strain specific and do not impact pathogenesis. J. Virol. 84:558–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morton D. B. 2000. A systematic approach for establishing humane endpoints. ILAR J. 41:80–86 [DOI] [PubMed] [Google Scholar]
- 22.Neumann G., Noda T., Kawaoka Y. 2009. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 459:931–939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Octaviani C. P., Ozawa M., Yamada S., Goto H., Kawaoka Y. 2010. High level of genetic compatibility between swine-origin H1N1 and highly pathogenic avian H5N1 influenza viruses. J. Virol. 84:10918–10922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perrone L. A., Plowden J. K., Garcia-Sastre A., Katz J. M., Tumpey T. M. 2008. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 4:e1000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reed L. J., Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. (London) 27:493–497 [Google Scholar]
- 26.Richmond J. Y., McKinney R. W., III 1993. Biosafety in microbiological and biomedical laboratories. U.S. Department of Health and Human Services, Centers for Disease Control, Atlanta, GA [Google Scholar]
- 27.Shinya K., et al. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436 [DOI] [PubMed] [Google Scholar]
- 28.Song M. S., et al. 2011. Virulence and genetic compatibility of polymerase reassortant viruses derived from the pandemic (H1N1) 2009 influenza virus and circulating influenza A viruses. J. Virol. 85:6275–6286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steel J., Lowen A. C., Mubareka S., Palese P. 2009. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 5:e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stevens J., et al. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404–410 [DOI] [PubMed] [Google Scholar]
- 31.Subbarao K., et al. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279:393–396 [DOI] [PubMed] [Google Scholar]
- 32.Sun Y., et al. 2011. High genetic compatibility and increased pathogenicity of reassortants derived from avian H9N2 and pandemic H1N1/2009 influenza viruses. Proc. Natl. Acad. Sci. U. S. A. 108:4164–4169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suzuki Y. 2010. A phylogenetic approach to detecting reassortments in viruses with segmented genomes. Gene 464:11–16 [DOI] [PubMed] [Google Scholar]
- 34.Van Hoeven N., et al. 2009. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc. Natl. Acad. Sci. U. S. A. 106:3366–3371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Riel D., et al. 2006. H5N1 virus attachment to lower respiratory tract. Science 312:399. [DOI] [PubMed] [Google Scholar]
- 36.Webster R. G., Rott R. 1987. Influenza virus A pathogenicity: the pivotal role of hemagglutinin. Cell 50:665–666 [DOI] [PubMed] [Google Scholar]
- 37.Yen H. L., et al. 2007. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J. Virol. 81:6890–6898 [DOI] [PMC free article] [PubMed] [Google Scholar]