Habit Reversal versus Object Manipulation Training for Treating Nail Biting: A Randomized Controlled Clinical Trial (original) (raw)
Abstract
Objective
This is a parallel, three group, randomized, controlled clinical trial, with outcomes evaluated up to three months after randomization for children and adolescents with chronic nail biting. The current study investigates the efficacy of habit reversal training (HRT) and compares its effect with object manipulation training (OMT) considering the limitations of the current literature.
Method
Ninety one children and adolescents with nail biting were randomly allocated to one of the three groups. The three groups were HRT (n = 30), OMT (n = 30), and wait-list or control group (n = 31). The mean length of nail was considered as the main outcome.
Results
The mean length of the nails after one month in HRT and OMT groups increased compared to the waiting list group (P < 0.001, P < 0.001, respectively). In long term, both OMT and HRT increased the mean length of nails (P < 0.01), but HRT was more effective than OMT (P < 0.021). The parent-reported frequency of nail biting did show similar results as to the mean length of nails assessment in long term. The number of children who completely stopped nail biting in HRT and OMT groups during three months was 8 and 7, respectively. This number was zero during one month for the wait-list group.
Conclusion
This trial showed that HRT is more effective than wait-list and OMT in increasing the mean length of nails of children and adolescents in long terms.
Keywords: Nail biting, behavior therapy, object manipulation, clinical trial
Nail biting is a very common behavior among children and adolescents; however, it is not well studied (1). The prevalence of nail biting in primary school boys and girls is 20.1% (95% confidence interval 15.9 to 24.2) and 24.4% (95% confidence interval 20.1 to 28.7), respectively (2). Nail biting is not associated with gender (2). Also, there is not any preference for biting of any finger nails (1).
Children with nail biting might be punished for their behavior (1). Moreover, nail biting can have medical consequences such as the damage of nail beds (3), temporomandibular dysfunction (4), and giardia infection (5).
Adults with nail biting usually bite their nail in the two conditions of boredom and frustration (6). Randomized controlled pharmacological therapy for the treatment of nail biting is rarely conducted. The efficacy of N-acetylcysteine is limited (7). Another study indicated that clomipramine is more effective than desipramine hydrochloride (8).
There are some published studies about the role of behavior therapy for treatment of nail biting. A study examined the role of wearing a non-removable wristband to quit nail biting. It was less effective than the aversion-based method, but it decreased nail biting (9). Another study showed that a self-help technique was more effective than progressive muscle relaxation (10).
The concept of habit reversal is suggested by Azrin et al. (11). The effect of habit reversal has been reported in several studies (12, 13). In addition, both mild aversion and competing response therapies improve nail length. However, the competing response improves it more than mild aversion (14).
Nevertheless, another study reported that the efficacy of mild aversion is more than competing response for treating nail biting (15). Meanwhile, no study included nail biting behavior exclusively in children. Some other studies investigated whether social support should be included for habit reversal. While some authors reported that social support is not necessary to be included (16), others opposed it (17). Habit reversal includes different parts; and competing response is part of habit reversal.
Anxiety, stress, loneliness, and inactivity are reported as the etiological factors for nail biting (18). Moreover, nail biting is reported as a co-morbid problem in some psychiatric disorders such as tic disorder (19). Those with nail biting have lesser prosocial abilities. Also, there is a marked trend for association of nail biting and emotional problems (2). A study including a clinical sample of children and adolescents with nail biting reported that many of these children suffer from co-morbid psychiatric disorders. The rates of attention deficit hyperactivity disorder (74.6%), oppositional defiant disorder (36%), and separation anxiety disorder (20.6%) were considerably high (20). Moreover, nail biting can guide us for a better pharmacological management of psychiatric problems (21). Meanwhile, mental health of children with nail biting as a covariate factor has not been considered in previous studies for its treatment (13).
In addition to mental health of children with nail biting, parent's mental health is also considerable. More than half of the mothers and 45.9% of the fathers of a clinical sample of children with nail biting had at least one psychiatric disorder (20). Given that habit reversal needs the involvement of parents, parental mental health should be considered in any intervention. No previous published study included these covariates.
Moreover, previous studies included very small samples size (22). The other study included 9 participants in each group (13). Furthermore, some studies investigated the habit reversal in adults rather than children and adolescents (23–25). All of these items justified the need to investigate the effects of habit reversal behavior therapy to treat nail biting in children and adolescents. Moreover, no published study has compared habit reversal training and object manipulation training for the treatment of nail biting.
The aim of this study was to determine whether habit reversal training is effective for the treatment of nail biting behavior in the community sample of children and adolescents with nail biting. This study also aimed to examine whether object manipulation is effective for the treatment of nail biting in short and long term, and to find whether object manipulation is as effective as habit reversal training for the treatment of nail biting. Finally, in this study, we tried to survey whether the acceptability of object manipulation training and habit reversal training is different.
Material and Methods
Study Design and Participants
This study was a parallel, three group, randomized, controlled trial, with outcomes evaluated up to three months after the onset of intervention for children and adolescents. We announced our study to schools in Shiraz, Iran.
After contacting schools, the nail biting children and adolescents and their parents were invited to contact us for participation in a clinical trial. Two hundred ninety nine parents contacted us, and they were all invited to participate in our study. However, only 91 children and adolescents referred to the clinic at the set date. To participate in the study, the subjects must have been without any serious medical condition such as epilepsy, and psychiatric disorders (psychosis, bipolar disorder, substance misuse disorder). Moreover, being able to attend appointments was necessary. Nail biting had to be chronic and severe enough to cause observable damage or emotionally distressing to the individual. Moreover, children and adolescents or their parents should have requested any intervention for the treating nail biting behavior. Those with mild transient nail biting or those whose nail biting started after taking any medication were excluded. Participation in any current psychological therapy or pharmacotherapy for nail biting was another exclusion criterion. All the patients were examined medically by one of the researchers (A.B.).
Providing written informed consent for assessment and entry into the trial was required. The Ethics Committee of Shiras University of Medical Sciences approved the study.
After obtaining the consent form, the children and adolescents were randomly allocated to treatment groups. Participants and therapists were not masked to treatment allocation and it was also impractical to mask the research assessor. The primary outcome was rated by a researcher (A.B.). Parents reported the frequency of their children's nail biting behavior.
Procedures
Assessments were undertaken at baseline, 4 weeks, and 12 (post-therapy) weeks after the onset of intervention. There were only two assessments in the waiting-list group (Baseline and week 8). The research assessor assessed them face-to-face in the clinic through the evaluation of nails' length. The parents reported the frequency of nail biting, completed parent-reported version of SDQ. As it was impractical to mask the research assessor to treatment allocation after randomization, we also included parent reported frequency of nail biting to keep the observer bias to a minimum. One of the researchers (A.G.) trained another researcher (A.B.) until he was deemed competent to provide trial treatments. All of the children and adolescents were trained by one researcher (A.B.).
Interventions
There were three groups of Habit Reversal Treatment group (HR) (n = 30), Object manipulation group (n = 30), and wait-list or control group (n = 31) in this study. All the three groups were assessed at baseline. However, both HR and Object manipulation groups received intervention while the wait-list group did not receive any intervention. The children in the wait-list group were assessed in two sessions. They were not followed up for the last session of the assessment.
HRT and Object manipulation training groups were educated in the first session of the intervention. There was a booster session after one month.
HR treatment was conducted according to a protocol provided by Woods (26). In this protocol, the possible functions of nail biting as well as the feelings experienced before, during and after nail biting were identified. According to this protocol, habit reversal includes awareness training, competing response training, and social support training. These trainings were conducted in a 30-minute session. In fact, the next sessions were booster sessions to monitor the progress and develop solutions to problems which occurred during the implementation of the intervention. In awareness training, children were trained to recognize their nail biting behavior and its warning signs. For competing response, children were trained to exhibit a behavior which was incompatible with nail biting immediately after the occurrence of nail biting or one of its warning signs. They were asked to hold a pencil or a toy with their hands. Finally, a person was identified to support children to increase their treatment compliance, and remind their competing response, and reward them for their compliance.
This group of children was trained for all the items reported for HR training. They were trained to play with something (such as a toy, pencil) instead of biting their nail. In fact, nail biting was replaced by playing with something. All other parts including awareness training and social support were similar to habit reversal treatment group. In fact, the object manipulation condition and HR condition were identical. However, children in object manipulation condition manipulated an object instead of doing a competing response.
Measurements
Strengths and Difficulties Questionnaire
Strengths and Difficulties Questionnaire (SDQ) is a well-known questionnaire for screening psychiatric symptoms in children and adolescents (27). The parent-reported form was used in this study; its psychometric properties have already been reported; and its validity and reliability are satisfactory (28).
SDQ consists of five subscales including conduct problems, hyperactivity-inattention, emotional symptoms, peer problems and pro-social behaviors. It is a Likert type response. The parents reported their children's general mental health through completing this questionnaire.
General Mental Health of Parents
The parents' current mental health was assessed using the General Health Questionnaire (GHQ-28) (29)which is a Likert response type questionnaire (1-not at all, 2-no more than usual, 3-rather more than usual, 4-much more than usual).
Visual Analogue Scale
The parents reported the frequency of nail biting through a Visual Analogue Scale (VAS). It is an instrument in which the score ranges from 0 to 100. If fact, it is a continuum of behavior score. Operationally, it is a horizontal line, with zero indicating no nail biting behavior, and score of 100 implying extreme nail biting.
Meter
Nail length was measured in millimeter. The length of all the fingernails of children and adolescents was measures. The length was defined as the longest distance from the base of nail to its tip (23). Then, these lengths were summed up and its mean was considered as the nail length outcome measure.
Treatment Evaluation Inventory-Short Form (TEI-SF) It is a Likert response type questionnaire including 9 questions which evaluates the acceptability of intervention by the parents (30). The parents completed this questionnaire in the last visit of patients.
Statistical Analysis
Separate analyses of variance were used to compare the children's age, mean length of nails, parental age and educational level among the three different groups. Chi-Square test was used to compare gender ratio among the three groups. Also, an ANCOVA with post hoc analysis was performed to examine the mean of nail length after the first session of the intervention. The variable of the mean length of nails at baseline was considered as a covariate factor.
A repeated measures MANOVA was performed to compare the mean length of nails between the two intervention groups over time.
Another repeated measures ANCOVA was performed to compare the parent reported frequency of nail biting after the first session of intervention between the two groups.
A repeated measures MANOVA was performed to compare the parent-reported frequency of nail biting between the two groups over time. The parent-reported frequency of nail biting at the first session was considered as a covariate factor. Kolmogorov–Smirnov tests were used to test the distribution of data. P value less than 0.05 was considered as statistical significance.
None of the participants cut their nail during the first month of intervention. There were two children who cut their nails after the second session of assessment. The mean of increased length of nails during the first month was added to the length of nails at the third session.
A second round of analysis was performed after dealing with missing data using the method of EM (expectation-maximization) based on the initial treatment intent.
Result
Baseline Characteristics
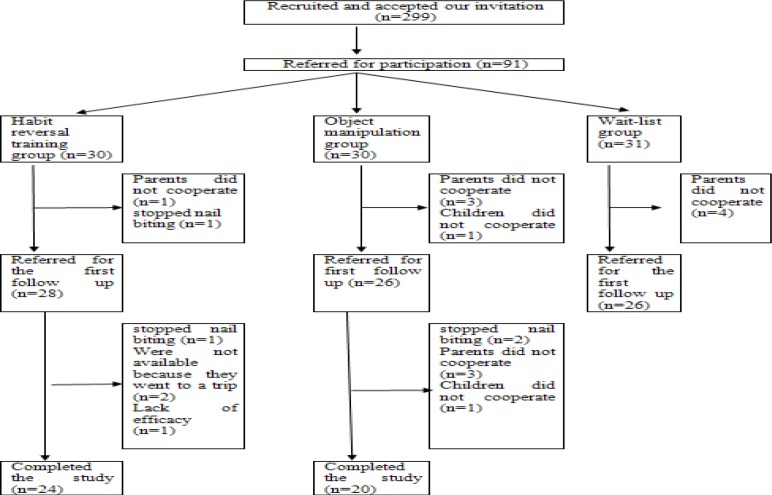
Out of 91 children and adolescents, 31 were in the wait-list group, 30 in HR group, and 30 in the object manipulation group. The rate of drops and its reasons are indicated in Figure 1. The mean age and gender ratio of children were not different among the three groups (Table 1). The age range of children was 6 to 17 years. In addition, parental age and educational level were not statistically different among the three groups (Table 1). The pretreatment mean length of nails among the three groups was not statistically different.
Figure 1.
Flowchart for the clinical trial of habit reversal versus object manipulation versus wait-list treatment groups
Table 1.
The characteristics of children and their parents in the three groups of waiting-list group, habit reversal group, and object manipulation group
| Variable | Group | Significance | ||
|---|---|---|---|---|
| Habit reversal | Object manipulation | Wait-list | ||
| Mean(SD) years of age | 10.3(2.1) | 10.1(1.8) | 9.9(1.7) | F (2, 88) = 0.4, P = 0.648 |
| Frequency of boy (%) | 46.7 | 43.3 | 29.0 | X2 = 2.2, df = 2, P = 0.325 |
| Fathers mean(SD) of age | 42.8(5.8) | 40.4(5.1) | 41.6(5.4) | F (2, 86) = 1.3, P = 0.163 |
| Fathers mean (SD) years of education | 12.8(3.4) | 12.1(3.4) | 11.4(3.3) | F (2, 87) = 1.2, P = 0.302 |
| Mother mean(SD) of age | 37.1(4.6) | 36.0(5.4) | 35.5(5.6) | F (2, 86) = 0.6, P = 0.352 |
| Mother mean (SD) years of education | 12.1(3.2) | 11.6(3.4) | 11.0(2.8) | F (2, 88) = 0.9, P = 0.378 |
| Parent-reported frequency of nail biting | 72.3(19.8) | 74.0(18.5) | 66.6(21.2) | F (2, 88) = 1.13, P = 0.326 |
| Pretreatment mean(SD) length of nails | 8.3(1.3) | 7.3(1.3) | 7.8(1.3) | F (2, 86) = 2.2, P = 0.112 |
| Mean(SD) length of nails after first session | 9.2(1.8) | 8.1(1.3) | 7.7(1.5) | F (2, 78) = 5.5, P < 0.006 |
| Mean(SD) length of nails three months after first intervention session | 9.6(2.2) | 8.7(1.7) | - | - |
The scores of emotional symptoms conduct problems, hyperactivity, peer problems, and pro-social behaviors were not significantly different among the three groups (Table 2). For the patients who cut their nails after one month, their mean length of increase in the first month was added to their mean length of nails after one month.
Table 2.
The mean scores of general mental health of children in the three groups of waiting-list, habit reversal, and object manipulation group
| Mental health variables | Group | Significance | ||
|---|---|---|---|---|
| Habit reversal | Object manipulation | Wait-list | ||
| Emotional Symptoms | 4.07(2.2) | 4.06(2.4) | 4.6(2.3) | F (2, 83) = 0.5, P = 0.555 |
| Conduct Problems | 3.5(1.5) | 3.2(1.3) | 3.5(2.7) | F (2, 84) = 0.4, P = 0.679 |
| Hyperactivity scale | 6.1(2.3) | 5.5(2.8) | 5.7(2.5) | F (2, 85) = 0.7, P = 0.628 |
| Peer Problem scale | 2.8(1.7) | 2.2(1.4) | 3.0(1.0) | F (2, 84) = 0.6,P = 0.628 |
| Pro-social scale | 7.7(1.3) | 7.6(2.1) | 7.592.0) | F (2, 80) = 0.1, P = 0.854 |
Regarding the parents’ mental health, none of the scores of GHQ subscales including somatic symptoms, anxiety/insomnia, social dysfunction, and depression were different among the three groups at baseline (all of P values were more than 0.05).
Mean Length of Nails
ANCOVA test revealed a statistically significant difference among the three groups at the second session of the intervention (Table 2) (F (2, 77) = 20.3, P < 0.001, Partial Eta Squared= 0.34). Post hoc analysis indicated that the mean length of nails in the HR group was statistically different with the wait-list group (P < 0.001). In addition, a difference was found between object manipulation group and wait list group (P < 0.001). However, no significant difference was found between HR and object manipulation groups (P = 0.230).
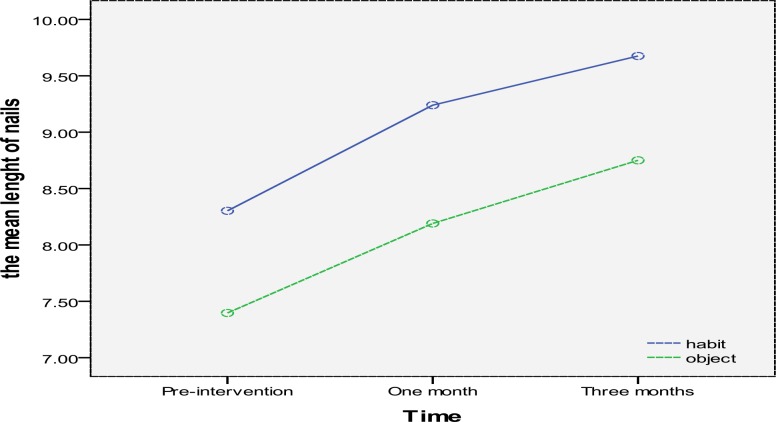
Repeated measures MANOVA showed that, in long term, the mean length of nails significantly increased in both groups and the time factor had a significant effect on the subjects' mean length of nails (F(2, 42)= 24.457, P < 0.001, Partial Eta Squared=.53) (Figure 2).
Figure 2.
The changes of mean length of nails during the trial in the habit reversal and object manipulation groups
However, the interactive effect of treatment type (group) and the time factor was not statistically significant (F(2, 42)= 0.145, P = 0.886). However, the mean length of nails was statistically higher in the HR group than object manipulation group (F (1, 43) =5.10, P < 0.02, Partial Eta Squared= 0.10) (Figure 2).
Parents Reported Frequency of Nail Biting
The parents also reported a significant difference among the three groups after one month (F (2, 76) = 8.4, P < 0.001, Partial Eta Squared= 0.18). This difference was between the HR and wait-list groups (P < 0.001). Moreover, the frequency in object manipulation group was statistically different from the wait-list group (P < 0.001). However, no difference was observed between the HR and object manipulation groups (P = 0.91).
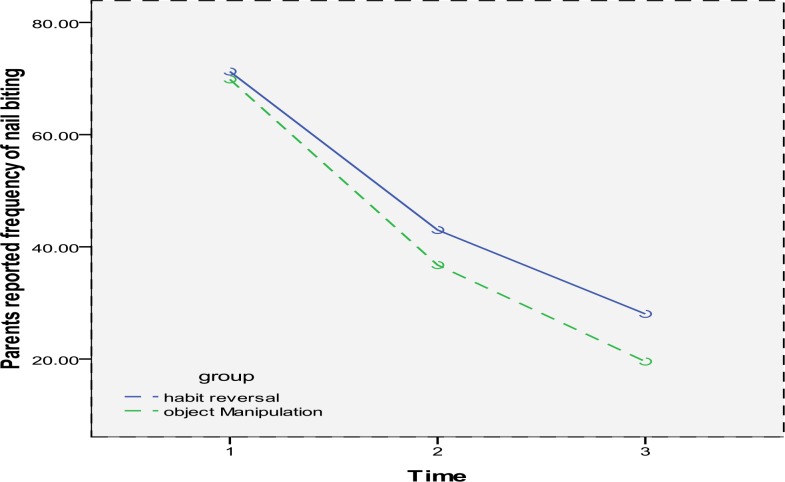
Repeated measures MANOVA showed that, in long term, the parent-reported frequency of nail biting was significantly decreased in both groups. The time factor had a significant effect on the frequency of nail biting (F(2, 41) = 60.897, P < 0.001, Partial Eta Squared=.66). However, the interactive effect of treatment type (group) and the time factor was not statistically significant (F(2, 41) = 0.349, P = 0.708) (Figure 3).
Figure 3.
Parents reported frequency of nail biting in the habit reversal and object manipulation group
According to parents’ report, the number of children who completely stopped nail biting in habit reversal group and object manipulation group during the 3-month follow up was 8 and 7 children, respectively. However, nobody stopped nail biting in wait-list group during the one month follow up.
Treatment Evaluation Inventory Short Form
The acceptability of treatment measured by TEI-SF showed that the mean score for the HR group and object manipulation group was 33.3(3.8) and 34.7(4.3). There was no statistically significant difference between the two groups (F (1, 43) =1.2, P = 0.489).
Second Round of Analysis after Dealing with Missing Data
We also conducted a second round of analysis after dealing with missing data using the method of EM (expectation-maximization). Again, the interactive effect of treatment type (group) and the time factor was not statistically significant (F (2, 57) = 0.281, P = 0.756). It showed that the mean length of nails increased in both groups (F (2, 57) =42.31, P < 0.001). However, there was a statistically significant difference between the two groups regarding their outcomes (F(1,58) = 5.021, P = 0.029).
Discussion
Overall, the current results confirmed that HR significantly increases the mean length of nails more than the other two groups in long term. This confirms that HR is an effective treatment for the management of nail biting for the community sample -of children and adolescents. Moreover, nail length increased during the trial in both groups of intervention while the mean length of nails in the wait-list group decreased during the trial. It is consistent with and supports the results of Woods et al.'s study (13). However, there is a lot of covariate factors considered in the current study that were not considered in the study by Woods et al. (1999). Moreover, the study by Woods et al. (1999) was conducted on children with thumb sucking. Only some of their participants had nail biting problem. In addition, we did not find any study on the effect of object manipulation on nail biting behavior. Therefore, the current study seems to be unique.
Regarding our second aim, the obtained results showed that object manipulation was more effective than wait-list in short term. Moreover, object manipulation significantly decreased nail biting in long term. However, the number of children who completely stopped nail biting was very close to each other. Therefore, further studies with longer duration are recommended.
Our third aim was to compare the effectiveness of object manipulation training and habit reversal training. The results showed that, in long term, both object manipulation training and habit reversal training are significantly effective for treating nail biting behavior. However, habit reversal training is more effective than object manipulation training.
Concerning our aim to understand the acceptability of object manipulation training and habit reversal training, the current results showed no significant difference between the two groups regarding their acceptability.
However, the drop-out rate was higher in the object manipulation group than the habit reversal group.
To the best of our knowledge, this is the first study that included a considerable large sample of children and adolescents with nail biting. It also considered the covariate factors including mental health of children and their parents. Emotional score, hyperactivity score, conduct score, pro-social score, and peer problems score were not associated with groups. Moreover, no study investigated the possible role of object manipulation for the treatment of nail biting. However, further studies with larger sample size are recommended.
Limitations
In this study, the assessor was not blind to the groups. However, it does not seem to be a fatal flaw. We measured the length of nail which is not the subject of assessor bias. However, future studies may consider a second assessor. This study included children and adolescents from a community sample. Therefore, generalization of these findings to other communities or clinical samples is not warranted. In addition, further studies with longer duration are recommended. Furthermore, it is not clear whether treating concurrent psychiatric problems in children with nail biting leads to stopping nail biting.
Conclusion
Habit reversal more than object manipulation increases the mean length of nails in long term.
Acknowledgements
This study was the post graduate thesis of Dr. Amir Bazrafshan toward the Iranian board of psychiatry. This study was supported by a grant from Shiraz University of Medical Sciences (88-5074) to Professor Ahmad Ghanizadeh. The authors would like to thank Dr. Nasrin Shokrpour at Center for Development of Clinical Research of Nemazee Hospital for editorial assistance.
Conflict of interest
There is no conflict of interest to be declared.
References
- 1.Ghanizadeh A. Nail biting; etiology, consequences and management. Iran J Med Sci. 2011;36:73–79. [PMC free article] [PubMed] [Google Scholar]
- 2.Ghanizadeh A, Shekoohi H. Prevalence of Nail Biting and Its Association with Mental Health in a Community Sample of Children. BMC research notes. 2011;4:116. doi: 10.1186/1756-0500-4-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sousa D, Pinto D, Araujo R, Rego RO, Moreira-Neto J. Gingival Abscess Due to an Unusual Nail-Biting Habit: A Case Report. The journal of contemporary dental practice. 2010;11:085–091. [PubMed] [Google Scholar]
- 4.Pereira LJ, Pereira-Cenci T, Del BelCury AA, Pereira SM, Pereira AC, Ambosano GM, et al. Risk Indicators of Temporomandibular Disorder Incidences in Early Adolescence. Pediatric dentistry. 2010;32:324–328. [PubMed] [Google Scholar]
- 5.Bello J, Nunez FA, Gonzalez OM, Fernandez R, Almirall P, Escobedo AA. Risk Factors for Giardia Infection among Hospitalized Children in Cuba. Annals of tropical medicine and parasitology. 2011;105:57–64. doi: 10.1179/136485911X12899838413385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams TI, Rose R, Chisholm S. What Is the Function of Nail Biting: An Analog Assessment Study. Behaviour research and therapy. 2007;45:989–995. doi: 10.1016/j.brat.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Ghanizadeh A, Derakhshan N, Berk M. N-Acetylcysteine Versus Placebo for Treating Nail Biting, a Double Blind Randomized Placebo Controlled Clinical Trial. Anti-inflammatory & anti-allergy agents in medicinal chemistry. 2013 doi: 10.2174/1871523011312030003. [DOI] [PubMed] [Google Scholar]
- 8.Leonard HL, Lenane MC, Swedo SE, Rettew DC, Rapoport JL. A Double-Blind Comparison of Clomipramine and Desipramine Treatment of Severe Onychophagia (Nail Biting) Archives of general psychiatry. 1991;48:821–827. doi: 10.1001/archpsyc.1991.01810330045007. [DOI] [PubMed] [Google Scholar]
- 9.Koritzky G, Yechiam E. On the Value of Nonremovable Reminders for Behavior Modification: An Application to Nail-Biting (Onychophagia) Behavior modification. 2011;35:511–530. doi: 10.1177/0145445511414869. [DOI] [PubMed] [Google Scholar]
- 10.Moritz S, Treszl A, Rufer M. A Randomized Controlled Trial of a Novel Self-Help Technique for Impulse Control Disorders: A Study on Nail-Biting. Behavior modification. 2011;35:468–485. doi: 10.1177/0145445511409395. [DOI] [PubMed] [Google Scholar]
- 11.Azrin NH, Nunn RG. Habit-Reversal: A Method of Eliminating Nervous Habits and Tics. Behaviour research and therapy. 1973;11:619–628. doi: 10.1016/0005-7967(73)90119-8. [DOI] [PubMed] [Google Scholar]
- 12.Long ES, Miltenberger RG, Ellingson SA, Ott SM. Augmenting simplified habit reversal in the treatment of oral-digital habits exhibited by individuals with mental retardation. J Appl Behav Anal. 1999;32:353–65. doi: 10.1901/jaba.1999.32-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woods DW, Murray LK, Fuqua RW, Seif TA, Boyer LJ, Siah A. Comparing the Effectiveness of Similar and Dissimilar Competing Responses in Evaluating the Habit Reversal Treatment for Oral-Digital Habits in Children. Journal of behavior therapy and experimental psychiatry. 1999;30:289–300. doi: 10.1016/s0005-7916(99)00031-2. [DOI] [PubMed] [Google Scholar]
- 14.Silber KP, Haynes CE. Treating Nailbiting: A Comparative Analysis of Mild Aversion and Competing Response Therapies. Behaviour research and therapy. 1992;30:15–22. doi: 10.1016/0005-7967(92)90091-t. [DOI] [PubMed] [Google Scholar]
- 15.Allen KW. Chronic Nailbiting: A Controlled Comparison of Competing Response and Mild Aversion Treatments. Behaviour research and therapy. 1996;34:269–272. doi: 10.1016/0005-7967(95)00078-x. [DOI] [PubMed] [Google Scholar]
- 16.Flessner CA, Miltenberger RG, Egemo K, Kelso P, Jostad C, Johnson B, Gatheridge BJ, Neighbors C. An evaluation of the social support element of simplified habit reversal. Behavior Therapy. 2005;36:35–42. [Google Scholar]
- 17.Woods DW, Miltenberger RG. Habit Reversal: A Review of Applications and Variations. Journal of behavior therapy and experimental psychiatry. 1995;26:123–131. doi: 10.1016/0005-7916(95)00009-o. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka OM, Vitral RW, Tanaka GY, Guerrero AP, Camargo ES. Nailbiting, or Onychophagia: A Special Habit. American journal of orthodontics and dentofacialorthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2008;134:305–308. doi: 10.1016/j.ajodo.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 19.Ghanizadeh A, Mosallaei S. Psychiatric Disorders and Behavioral Problems in Children and Adolescents with Tourette Syndrome. Brain & development. 2009;31:15–19. doi: 10.1016/j.braindev.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Ghanizadeh A. Association of Nail Biting and Psychiatric Disorders in Children and Their Parents in a Psychiatrically Referred Sample of Children. Child and adolescent psychiatry and mental health. 2008;2:13. doi: 10.1186/1753-2000-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ghanizadeh A. Can Behavioral Sensory Processing Problems Guide Us to a Better Pharmacological Management of Children with Attention Deficit Hyperactivity Disorder?: A Case Report. Psychiatry (Edgmont (Pa: Township)) 2009;6:40–43. [PMC free article] [PubMed] [Google Scholar]
- 22.Dufrene BA, Steuart Watson T, Kazmerski JS. Functional Analysis and Treatment of Nail Biting. Behavior modification. 2008;32:913–927. doi: 10.1177/0145445508319484. [DOI] [PubMed] [Google Scholar]
- 23.Twohig MP, Woods DW. Evaluating the Duration of the Competing Response in Habit Reversal: A Parametric Analysis. Journal of applied behavior analysis. 2001;34:517–520. doi: 10.1901/jaba.2001.34-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azrin NH, Nunn RG, Frantz SE. Habit Reversal Vs. Negative Practice Treatment of Nailbiting. Behaviour research and therapy. 1980;18:281–285. doi: 10.1016/0005-7967(80)90086-8. [DOI] [PubMed] [Google Scholar]
- 25.Twohig MP, Woods DW, Marcks BA, Teng EJ. Evaluating the Efficacy of Habit Reversal: Comparison with a Placebo Control. The Journal of clinical psychiatry. 2003;64:40–48. doi: 10.4088/jcp.v64n0109. [DOI] [PubMed] [Google Scholar]
- 26.Woods DW, Miltenberger RG. Tic Disorders, trichotillomania, and other repetitive behavior disorders. behavioral approaches to analysis and treatment. USA: Springer; 2006. [Google Scholar]
- 27.Goodman R. The Strengths and Difficulties Questionnaire: A Research Note. Journal of child psychology and psychiatry, and allied disciplines. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 28.Ghanizadeh A, Izadpanah A, Abdollahi G. Scale validation of the strengths and difficulties questionnaire in Iranian children. Iran J Psychiatry. 2007;2:65–71. [Google Scholar]
- 29.Goldberg DP, Hillier VF. A Scaled Version of the General Health Questionnaire. Psychological medicine. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 30.Kelley ML, Heffer RW, Gresham FM, Elliott SN. Development of a modified treatment evaluation inventory. Journal of Psychopathology and Behavioral Assessment. 1989;11:235–247. [Google Scholar]