THE ROLE OF THE SCAPULA (original) (raw)
Abstract
Previously, the scapular musculature was often neglected in designing a rehabilitation protocol for the shoulder. In the past two decades a significant amount of research has been performed in order to help identify the role of the scapula in upper extremity function. Weakness of the scapular stabilizers and resultant altered biomechanics could result in: 1) abnormal stresses to the anterior capsular structures of the shoulder, 2) increased possibility of rotator cuff compression, and 3) decreased shoulder complex neuromuscular performance. This clinical commentary presents facts about the anatomy and biomechanics of the scapula and surrounding musculature, and describes the pathomechanics of scapular dysfunction. The focus is upon the assessment of dysfunction and retraining of the scapular musculature.
Level of Evidence:
5
Keywords: scapular musculature, scapular biomechanics, shoulder rehabilitation, scapular strengthening
INTRODUCTION
The understanding of and interest in the role of the scapula in upper extremity function has grown considerably in the past two decades. As understanding of the shoulder and surrounding structures has increased it has become well accepted that the scapula plays several roles in facilitating optimal shoulder complex function when scapulohumeral anatomy and biomechanics interact to produce efficient movement.1 In normal upper quarter function, the scapula provides a stable base from which glenohumeral mobility occurs.1,2 Stability of the scapulothoracic joint depends on coordinated activity of the surrounding musculature. The scapular muscles must dynamically position the glenoid so that efficient glenohumeral movement can occur. When weakness or dysfunction of the scapular musculature is present, normal scapular positioning and mechanics may become altered.1,2 When the scapula fails to perform its stabilization role, shoulder complex function is inefficient, which can result not only in decreased neuromuscular performance but also may predispose the individual to injury of the glenohumeral joint.1,2
FUNCTIONAL ANATOMY AND BIOMECHANICS
It is important that the clinician have a thorough understanding of the muscles that control the scapula and normal scapular mechanics. Only through an understanding of normal biomechanics can the pathomechanics of injury or dysfunction be understood.2 The scapulothoracic articulation is one of the least congruent joints in the body. No actual bony articulation exists between the scapula and thorax, which allows tremendous mobility in many directions including protraction, retraction, elevation, depression, anterior/posterior tilt, and internal/external and upward/downward rotation. When describing scapular positions, the point of reference is the glenoid. The lack of an actual bony articulation in the scapulothoracic region predisposes it to pathologic movement, rendering the glenohumeral joint highly dependent on its for stability and normal motion.1,3–6 The scapula is only attached to the thorax by ligamentous attachments at the acromioclavicular joint and through a suction mechanism provided by the muscular attachments of the serratus anterior and subscapualaris.3 This suction mechanism holds the scapula in close proximity to the thorax and allows it to glide during movements of the joint.3
While many muscles serve to stabilize the scapula, the main stabilizers are the serratus anterior, rhomboid major and minor, levator scapulae, and trapezii. The glenohumeral “protectors” include the muscles of the rotator cuff: the supraspinatus, infraspinatus, teres minor, and subscapularis.5–9 These muscle groups function through synergistic co‐contraction to anchor the scapula and guide movement.3 Specifically, the muscles of the scapula function as follows:
Serratus Anterior
The serratus anterior is an important scapular stabilizing muscle. It originates from the first eight ribs and courses along the rib cage to insert along the anterior medial aspect of the scapula. The upper portion of the serratus anterior insertion is spread along the medial border of the scapula, while the lower portion inserts into the inferior angle of the scapula. Innervation of the serratus anterior is provided by the long thoracic nerve, which arises from the ventral rami of the fifth and seventh cranial nerves. Due to the multiple attachment sites, the primary role of the serratus anterior is to stabilize the scapula during elevation and to pull the scapula forward and around on the thoracic cage. Advancement of the scapula to an anterior position on the thoracic cage is termed protraction or scapular abduction. The term protraction is more frequently used in describing this anterior movement in order to avoid confusion with shoulder abduction. The movement of protraction is involved with pushing or punching type activities. Three‐dimensional studies have shown that the serratus anterior contributes to all components of 3‐D scapular movements during arm elevation, which includes upward rotation, posterior tilt, and external rotation.10,11
Rhomboids
The rhomboids (major and minor) function to stabilize the medial border of the scapula. The rhomboids are very active in scapular adduction or retraction, which can be defined as backward rotation of the scapula toward the vertebral column. The rhomboid minor originates from the spinous process of the seventh cervical and first thoracic vertebrae and inserts into the medial border of the scapula near the base of the scapular spine. The rhomboid major originates from the second through fifth thoracic vertebrae and inserts into the medial scapular border of the scapula just below the insertion of the minor. Innervation to both the rhomboid major and minor is provided by the dorsal scapular nerve. If rhomboid weakness is present, the scapula will be unable to achieve full retraction. Full retraction is essential not only for overhead throwing motion but also for swimming strokes such as the crawl. The inability to achieve the fully retracted position during the throwing or overhead motion can lead to increased stress on the anterior structures of the shoulder.12 Activities that involve a pulling motion may be affected by lack of rhomboid strength. Electromyographic (EMG) analysis has demonstrated a high level of rhomboid activity during the acceleration phase of pitching.13 This EMG data suggests that the rhomboids are contracting eccentrically during the follow‐through phase of throwing as the muscle continues to contract eccentrically to “brake” the energy released during acceleration.12 Therefore, rhomboid strength is vital in throwing and overhead arm movement. Strengthening this muscle group should be emphasized when rehabilitating patients with anterior instability.2
Trapezius (Upper/Middle/Lower)
The trapezius functions include upward rotation and elevation for the upper trapezius, retraction for the middle trapezius, and upward rotation and depression for the lower trapezius. In addition, the inferomedial‐directed fibers of the lower trapezius may also contribute to posterior tilt and external rotation of the scapula during arm elevation.10 The trapezius takes originates from the medial third of the superior nuchal line, external occipital protuberance, nuchal ligament, and spinous processes of C7 to T12 vertebrae and attach distally at the lateral third of the clavicle, acromion and spine of the scapula. Innervation to the trapezius is provided by the spinal accessory nerve.
Levator Scapulae
The levator scapulae originates from the posterior tubercles of the transverse processes of cervical vertebrae 1–4. The insertion of the levator scapulae is along the medial border of the scapula at the level of the scapular spine. Innervation is provided by the cervical plexus (C3, C4) with frequent contribution from the dorsal scapular nerve. The levator scapulae functions to elevate the scapula and tilt the glenoid cavity inferiorly by rotating the scapula downward. Exercises used to strengthen rotator cuff and scapulothoracic musculature are also effective in eliciting activity of the levator scapulae, making specific exercises to target this muscle often unnecessary.14
Normal Biomechanics
Mechanically, the coordinated coupled motion between the scapula and humerus, often termed scapulohumeral rhythm, is needed for efficient arm movement and allows for glenohumeral alignment in order to maximize joint stability.15 Studies examining the mechanics and role of the scapula in shoulder function have progressed over time, with the earliest studies examining two dimensional scapular motion with the use of radiographs, dating back to Inman et al in 1944.16 Inman et al16 found an overall 2:1 relationship between glenohumeral elevation and scapular upward rotation, which has remained the classic description of the so‐called scapulohumeral rhythm.11 A more clinically relevant analysis of scapular motion has been conducted in several three‐dimensional studies using surface markers and indwelling bone pins.10,11,15,17–19 McClure et al.11 found that during scapular plane elevation of the arm in normal subjects, there was a consistent pattern of scapular upward rotation, posterior tilting, and external rotation along with clavicular elevation and retraction.11 Scapular upward rotation is the predominant scapulothoracic motion. The motion of the scapula with regard to changes in scapular internal rotation angles shows more variability across subjects, investigations, planes of elevation, and point in the range of motion of elevation.11,20,21 It has generally been found that end range elevation involves some scapulothoracic external rotation, however, some studies report internal rotation during elevation and limited data are available.11
PATHOMECHANICS
The role of the scapula in shoulder injuries has been widely investigated with the majority of studies in the area of shoulder impingement and rotator cuff disease, and fewer studies researching the role of the scapula in shoulder instability and adhesive capsulitis or glenohumeral joint stiffness.15,21 Among the research there is significant variability in subjects, study design, kinematic description and outcomes. However, most of the abnormal biomechanics and overuse injuries that occur about the shoulder girdle can be traced to alterations in the function of the scapular stabilizing muscles.22,23 Altered scapular motion and position have been termed scapular dyskinesis. The definition of dyskinesis is the alteration of normal scapular kinematics.15 Many factors may contribute to the development of scapular dyskinesis including but not limited to bony causes, including posture or previous fracture. Joint causes including acromioclavicular joint instability, acromioclavicular joint arthrosis, and glenohumeral joint internal derangement. Neurological causes including cervical radiculopathy or nerve palsy. Soft tissue factors including inflexibity (tightness) or intrinsic muscle problems, and alterations in periscapular muscle activation.15
Of the possible contributors to scapular dysfunction or dyskinesis, most commonly, muscles are either injured via macrotrauma, have microtrauma‐induced strain, or are inhibited by painful conditions of the shoulder such as labral lesions, arthrosis, or instability.8 Weakness of the scapulothoracic muscles potentially leads to abnormal positioning of the scapula, disturbances in scapulohumeral rhythm, and generalized shoulder complex dysfunction.5 The serratus anterior and lower trapezius are the most commonly weak or inhibited muscles of the scapulothoracic joint that may lead to abnormal movement.24,25 The serratus anterior and lower trapezius contribute to the important upward rotation force couple that produces acromial elevation. If part of that force couple is altered, for any reason, movement is abnormal. For example, paralysis of the serratus anterior results in reductions in both glenohumeral flexion and abduction. The medial border of the scapula is elevated off the rib cage, resulting in decreased acromial elevation. This problem manifests itself through decreased shoulder abduction and secondary impingement.5 This lack of acromial elevation and secondary impingement has been seen concomitant with many glenohumeral problems. Most shoulder complex injuries incurred as a result of sport activities can be traced to abnormal biomechanics, which, in turn, can be related to improper functioning of the scapular muscles.8 In fact, scapular instability is found in as many as 68% of rotator cuff problems and 100% of glenohumeral instability problems.8,26
The effects of muscle fatigue with regard to scapular stability have also been investigated. Thomson and Mitchell27 investigated the effect of repetitive exercise on the scapular stabilizers by studying the ability of the scapular musculature to stabilize the scapula after fatiguing exercise in the proprioceptive neuromuscular facilitation (PNF) D2 pattern as measured by the lateral scapular slide (LSS) test. Their results suggest that a fatigue‐induced strength deficit of the shoulder musculature can have an adverse effect on scapular positioning by allowing the scapula to glide more laterally during functional activities.27 The effect of fatiguing exercise on shoulder muscles has also been studied by Carpenter et al28 and Voight et al29, who investigated the effects of exercise and muscle fatigue on shoulder proprioception. Both groups found a significant decrease in joint kinesthesia, measured using the time threshold to detection of passive movement after fatiguing exercise.28 They hypothesized that a decrease in position sense as a result of fatigue of the shoulder girdle musculature could interfere with normal coordination and joint stability, thus impairing function around the shoulder girdle.28,29
Physical Exam and Assessment
It is well accepted that strengthening and motor control training of the scapular musculature is a vital component to most shoulder complex rehabilitation programs. The difficulty with validating such programs lies in the ability to measure changes in scapular position. It has been difficult to assess and track scapular motion secondary to the relatively deep position of the scapula and overlying muscles. This section on physical exam and assessment will present clinical examination tools for clinicians’ use in evaluating scapular asymmetry of weakness. Most methods for evaluating scapular dyskinesis involve some sort of tool, test, or observation in a single plane. This presents a problem due to the three‐dimensional nature of scapular movement. In addition, another difficult challenge with scapular evaluation is attempting to extrapolate how much weight to give a special test that shows a unilateral deficit. In many cases, such as overhead baseball throwers, unilateral asymmetry can be found in normal, asymptomatic subjects.30 Scapular dyskinesis is generally characterized by a lack of upward rotation, a lack of posterior tilting and increased internal or medial rotation of the scapula.21 Kibler has described a re‐location test of manually re‐positioning the scapula to reduce or eliminate a painful arc. This test was described by Kibler as the scapular dyskinesia test (SDT) test.15 Interrater reliability for Kibler’s test is moderate to fair at .42 and .32 for physical therapists and physicians. This test is a visual interpretation of scapular dyskinesia involving several subcategories. When this test was simplified as a “yes” or “no” for dyskinesis, the reliability scores were improved. A similar reliability study was performed by McClure and Tate. They found interrater reliability among visual observers of .57 for the active SDT.31 indicating moderate reliability. Criterion was based on normal, subtle, or obvious scapular dyskinesia. It appears that loading the shoulder by performing a forward flexion lift with a dumbbell seems to be the best position to reveal any lack of scapular control. Another method to reveal scapular stability is a wall push (Figure 1a). This test was described in the authors original article.2 This test is performed in a similar method to the dumbbell lift performed in forward flexion (Figure 1b). Figure 2 illustrates scapular asymmetry, with prominence of the right medial scapular border. Clearly, rehabilitation professionals are still searching for a reliable method of scapular physical examination techniques. As a comparison, the KT‐1000 knee ligament arthrometer demonstrates very high intertester reliability. This instrument is used for diagnosing an ACL tear, by measuring millimeters of anterior tibial translation of the tibia on the femur. Myer found interclass correlation coefficients (ICC) between examiners to be .92 for absolute millimeters of displacement.32 The authors applaud all authors’ efforts to provide the sports medicine community with answers to objectifying measurements of scapular position.
Figure 1.
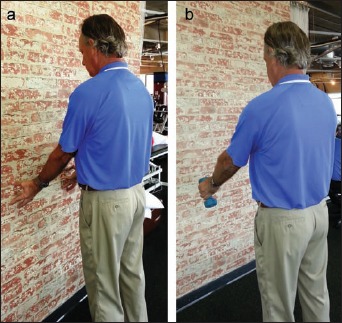
(a) Wall push – press into wall using fingertips. Avoid leaning into wall with body. Observe backward winging of the scapula. (b) Lift 3–5# dumbbell and lower to position shown (45 degrees). Observe backward winging of scapula.
Figure 2.

Notice prominence of the medial border of the right scapula during only a fingertip press into wall.
Evaluation of other soft tissue structures around the shoulder should be included during scapular examination. Posterior shoulder tightness is thought to be a contributing cause of the anterior tilted scapula. Borich et al showed a correlation between decreased internal rotation and anterior tilted scapula in normal subjects.33 Laudner showed a moderate correlation to posterior shoulder tightness and forward scapular posture in baseball players.34 Launder believes that increased laxity in baseball pitchers may contribute to a downwardly rotated scapula. In his study, pitchers were shown to have a more downwardly rotated scapula when compared to position players. Laudner theorized that increased laxity in pitchers creates a lack of capsular tension that allows the scapula to drift inferiorly.35
Figure 3 demonstrates the “genie” stretch described by Paine.36 This stretch focuses on the posterior soft tissue restriction of the shoulder. When performing this stretch, external rotation is controlled, placing the tight posterior rotator cuff and capsule on tension. This technique is believed to impart a more focused stretching rather than pulling into horizontal adduction with no control of external rotation. Wilk (personal communication) has described a sidelying version of this stretch to help reduce scapular movement. The patient is sidelying on the affected side and rolls onto the scapula while performing the movement of the “genie” stretch.
Figure 3.
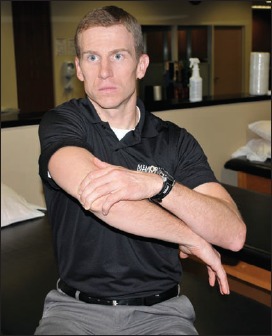
Genie Stretch – Begin stretch in “Genie Position” with involved arm below normal. Limit external rotation using top arm as the control arm. Lift the elbow slightly then pull across chest in a diagonal movement. Make sure that subject perceives stretch on top and or posterior aspect of shoulder. Coracoid impingement will occur if subject feels pinching in front. This can be avoided by lowering angle towards opposite hip.
Therapeutic Exercise Design
The rehabilitation program for scapular dyskinesis should address all of the contributory impairments found during the evaluation process. By doing so, the clinician should be able to restore the balance of musculature that allow for normal static scapular position and dynamic motion. Before beginning a corrective strengthening program, the clinician must regain normal flexibility of the muscles about the scapula if identified, as tightness or adaptive shortening can inhibit activation of opposing muscle groups. It is common to find tightness of the pectoralis minor and posterior glenohumeral capsule in patients with scapular dyskinesis. Borstad and Ludewig found increased internal rotation and anterior tilting of the scapula in subjects with a short pectoralis minor.20 Therefore manual therapy and stretching of tight structures can be employed early in the rehabilitative process. Once normal flexibility has been achieved, a conscious motor control‐strengthening program can be initiated to help normalize the scapular resting posture. As the patient is progressed through the program, emphasis will shift to dynamic control in order to restore muscle balance with various arm movements. Once muscle balance is achieved, the final emphasis is on scapular muscle strengthening within sports specific movement patterns. The following is an outline describing a typical phased implementation of various scapular strengthening exercises. This exercise routine was designed based upon muscular activation identified in prior EMG studies.37–42
Phase I
The beginning phase of scapular strengthening is designed to initiate firing of the muscles that control the scapula. Depending on the type of scapular dyskinesia or weakness present, select the appropriate exercise to address the physical exam findings. Please see figures for all exercise descriptions.
Isometrics
Isometric squeezing exercise may begin with many post‐operative patients or those that are having significant pain with active elevation exercises.
- Scapular pinches: Squeeze shoulder blades together and hold for 3 seconds
- Robbery pinches: Squeeze shoulder blades together and hold for 3 seconds in a position described by Kibler37 (see Figure 6: Swiss Ball Robbery exercise for position).
- Low Row Wall isometrics: With back against wall, arms to side and extended, push fingertips into wall, holding 3 seconds.
Figure 6.

Swiss Ball “Robbery” – Prone on a Swiss Ball, assume “robbery” position, cuing patient to point elbows to back pockets. Target muscle, lower trapezius.
Isotonics
Advancement to active glenohumeral/scapular joint movement occurs when painful arc symptoms are diminished. These exercises use light resistance with emphasis on proper technique. The authors suggest 3 sets of 10 to 20 repetitions, with 3 second holds.
- Scapular pinches using theraband: Using tensioned theraband in front of body, spread theraband by pinching shoulder blades together. It is very important to keep elbows tucked to side during entire routine.
- Low Row Theraband: Standing with arms to side, loop theraband around stable object, and pull both arms into extension behind body squeezing lower scapular muscles.
- Dynamic Hug: (Figure 4) Place single theraband around back grasping band with both hands in front, perform hugging motion to perform protraction of scapula
- Scapular Punches: Affix theraband to door approximately shoulder height. With back to door grab theraband and mimic punching motion making sure to achieve full protraction.
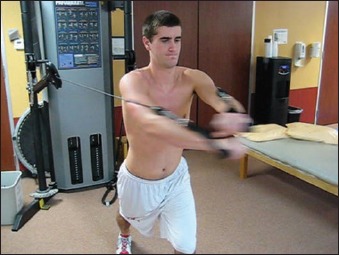
- Cheerleader Exercise: (Figure 5) Using single piece of theraband held with both hands in front of body, elbows completely extended, pull theraband apart in bilateral horizontal abduction. Return to starting position, then pull theraband in D2 diagonal position with right arm up, then alternate into D2 diagonal with left arm up.
Figure 4.
Dynamic Hug – using cable column, can also be performed using Theraband. Instruct the patient to reach forward as if “hugging a tree”. Target muscle, serratus anterior.
Figure 5.

Cheerleader Exercise – Using Theraband, perform alternating diagonal patterns with one bilateral horizontal abduction motion between each diagonal. Target muscles, lower trapezius, rhomboids.
Phase II
This phase of scapular strengthening is usually instituted when there is minimal/no pain in the shoulder complex with lifting arm overhead, although some exercises could be used at an earlier time frame if non‐painful.
- Seated Rows: Seated on a bench, using a cable column or row machine, pull handles into sternum while pinching scapulae together, toward the spine. Pinch and hold scapulae then extend arms and allow scapulae to assume a fully protracted position and repeat. It is very important to keep elbows tucked during entire exercise. Note, this exercise can also be performed unilaterally.
- High Rows: same exercise as above, raising cable column to higher position and pulling handles downward into chest.
- Swiss Ball Robbery: (Figure 6) While lying on stomach on Swiss ball, place dumbbells in front of body on floor. Grasp dumbbells and retract scapula to achieve the “robbery position” while maintaining spine extension. This allows posterior chain strengthening along with lower trapezius strengthening.
- Standing D2 Cocking Cable Column: (Figure 7) While in standing position, using either theraband or cable column, starting hand in position across the body and around shin height, pull upward at a diagonal to achieve “Statue of Liberty” position. Return, with control, to start position and repeat.
- Latissimus Pull Downs: Keeping bar in front of the body, pull down handle to chest level, flexing elbows, in order to exercise lower scapular musculature (downward rotators).
- Manually Resisted Scapular Strengthening: (Figure 8) Manual resistance from therapist in sidelying position to attempt to isolate scapular movements. Can emphasize pro/retraction, elevation/depression, upward/downward rotation, and PNF diagonals.
Figure 7.

Cocking Cable Column – Perform D2 diagonal pattern pulling into a cocked position, then slowly lower to decelerate. Target muscles, lower trap, rhomboid, posterior cuff.
Figure 8.

(a) Manual Resisted protraction/retraction – Manual resistance applied to anterior shoulder and spine of scapula while patient performs protraction, retraction. Target muscles, serratus anterior and rhomboids. (b) Bilateral PNF – Manual resisted D2 bilateral PNF pattern. Target muscles, lower trap, rhomboid, posterior cuff.
Phase III
This phase is comprised of advanced scapular exercises and may not be necessary for all individuals. It incorporates closed chain activities and more aggressive, sport specific techniques.
- Super 6: (Figure 9) A series of scapular exercises that involve reciprocal movements of both arms.
- Standing Cable Column Punch: Using long bar attached to cable column, perform a punching (with protraction) type maneuver with cable column resistance.
- Bear Crawl on Swiss Ball: (Figure 10) With legs on Swiss Ball and trunk extended, maintaining neutral spine, walk out on hands and perform push‐up, then crawl back to start position using hands.
- Plyoball Deceleration: With subject kneeling, throw a small (2#) plyoball from behind asking patient to catch and decelerate into internal rotation.
- Seated Pike lift: (Figure 8) Using 2 boxes or large dumbbells, have patient place hands on boxes or grasp dumbells and lift buttocks off table or floor. Goal: 20 second holds.
- Standing “Snow Angels”: (Figure 12) With back against wall perform overhead pressing maneuver and touch hands together above head. Patient attempts to keep back of hands, forearms, and scapulae against wall. Light cuff weights are used for resistance.
Figure 9.

(Super 6 Scapular Routine (a‐f) Series of reciprocal scapular exercises that target scapular, rotator cuff, and trunk musculature. a. Upright Row, b. Dynamic Hug, c. Cocking/Deceleration, d. Cocking/Acceleration, e. Bilateral D2, f. Bilateral Pullover
Figure 10.
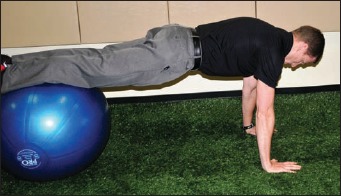
Bear Crawl – Walk out on hands while in a plank position on swiss ball, then perform push‐up with a plus. Target muscles, serratus anterior, pectoralis major.
Figure 12.
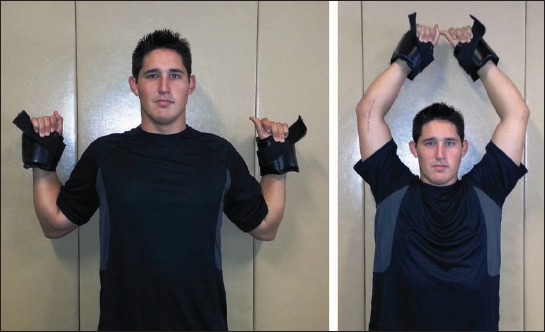
Standing “snow angels” – Stand with back against wall, keeping scapula, back of hands, and forearms touching wall. Move hands to overhead pressing motion then return with arms to side. Light cuff weights are used to provide additional resistance.
Figure 11.
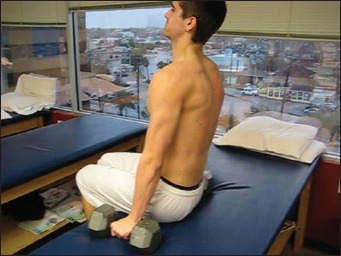
Seated Pike Lift – Using large dumbbells or blocks, lift buttocks off table and hold for 20 seconds. Target muscle, lower trapezius.
Supportive Devices
The need for increased awareness of scapular position and stability during movement, as well as correlation to positive clinical outcomes has led to the development of accessory tools to enhance scapular positioning with activity. Several manufacturers have developed “scapular shirts”, an external, tight fitting device, sewn in a manner that promotes an upright posture of scapular retraction and upward rotation. Scapular taping is used by some clinicians for proprioceptive feedback to the scapular musculature. The authors preferred method is use of the scapular shirt. (Figure 13)
Figure 13.

Scapular shirt – Scapular shirt used to help maintain proper posture and scapular positioning.
CONCLUSION
The shoulder complex must be considered a part of a larger kinetic chain made up of several joints. It is obvious that the glenohumeral joint and scapula cannot function independently. Clearly, dysfunction at either joint has a direct effect on the other. The function of the scapula and surrounding musculature is vital to the normal function of the glenohumeral joint. As knowledge regarding the role of the scapula continues to grow, improved evaluation and treatment approaches for dyskinesis continue to evolve. While rotator cuff strengthening has been an obvious treatment for various pathologies, the origins of the rotator cuff muscle arise from the scapula, therefore an effective exercise program for rehabilitation should include improving the strength and function of the muscles that control the position of the scapula. An effective scapular strengthening program is especially important for the overhead athlete or swimmer where normal scapular firing and control may have an effect on performance and may also relate to injury prevention. Weakness of these anchoring muscles may lead to altered biomechanics of the glenohumeral joint with resultant excessive stress imparted to the rotator cuff and anterior capsule. Implementation of the scapular program can begin early in the rehabilitation protocol and progress to more aggressive strengthening approaches. Scapular strengthening should be a part of all rehabilitation programs relating to the shoulder complex. Advancement in the knowledge of shoulder complex biomechanics and related EMG patterns has allowed for the development of strengthening exercises that maximally address these “anchor” muscles. As techniques evolve to objectively measure scapular position and dynamic function, the interaction between the scapula and glenohumeral joint can be further clarified.
REFERENCES
- 1.Voight ML, Thomson BC. The role of the scapula in the rehabilitation of shoulder injuries. J Athl Training. 2000;35(3):364–372 [PMC free article] [PubMed] [Google Scholar]
- 2.Paine RM, Voight ML. The role of the scapula. J Orthop Sports Phys Ther. 1993;18:386–391 [DOI] [PubMed] [Google Scholar]
- 3.Peat M. Functional anatomy of the shoulder complex. Phys Ther. 1986;66:1855–1865 [DOI] [PubMed] [Google Scholar]
- 4.Bigliani LU, Codd TP, Connor PM, Levine WN. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609–613 [DOI] [PubMed] [Google Scholar]
- 5.Kamkar A, Irrgang JJ, Whitney SL. Nonoperative management of secondary shoulder impingement syndrome. J Orthop Sports Phys Ther. 1993;17:212–224 [DOI] [PubMed] [Google Scholar]
- 6.Pink M, Jobe FW. Shoulder injuries in athletes. Clin Manage. 1991;11:39–47 [Google Scholar]
- 7.Jobe FW, Pink M. Classification and treatment of shoulder dysfunction in the overhead athlete. J Orthop Sports Phys Ther. 1993;18:427–432 [DOI] [PubMed] [Google Scholar]
- 8.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337 [DOI] [PubMed] [Google Scholar]
- 9.DiVeta J, Walker ML, Skibinski B. Relationship between performance of selected scapular muscles and scapular abduction in standing subjects. Phys Ther. 1990;70:470–476 [DOI] [PubMed] [Google Scholar]
- 10.Ludewig PM, Cook TM, Nawoczenski DA. Three‐dimensional scapular orientation and muscle activity at selected positions of humeral elevation. J Orthop Sports Phys Ther. 1996;24:57–65 [DOI] [PubMed] [Google Scholar]
- 11.McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3‐dimesional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269–277http://dx.doi.org/10.1067/mse.2001.112954 [DOI] [PubMed] [Google Scholar]
- 12.Kibler WB. Role of the scapula in the overhead throwing motion. Contemp Orthop. 1991;22:525–532 [Google Scholar]
- 13.DiGiovine NM, Jobe FW, Pink M, Perry J. An electromyographic analysis of the upper extremity in pitching. J Shoulder Elbow Surg. 1992;1:15–25 [DOI] [PubMed] [Google Scholar]
- 14.Reinold MM, Escamilla R, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39:105–117 [DOI] [PubMed] [Google Scholar]
- 15.Kibler WB, Ludewig PM, McClure PW, et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med. Published online first: 11 April 2013. 10.1136/bjsports‐2013–092425. [DOI] [PubMed] [Google Scholar]
- 16.Inman VT, Saunders M, Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg Am. 1944;26:1–30 [Google Scholar]
- 17.Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3‐dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–586 [DOI] [PubMed] [Google Scholar]
- 18.Ludewig PM, Behrens SA, Meyer SM, Spoden SM, Wilson LA. Three‐dimensional clavicular motion during arm elevation: reliability and descriptive data. J Orthop Sports Phys Ther. 2004;34:140–149 [DOI] [PubMed] [Google Scholar]
- 19.Treece RM, Lunden JB, Lloyd AS, Kaiser AP, Cieminski CJ, Ludewig PM. Three‐dimensional acromioclavicular joint motions during elevation of the arm. J Orthop Sports Phys Ther. 2008;38:181–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borstad JD, Ludewig PM. Comparison of scapular kinematics between elevation and lowering of the arm in the scapular plane. Clin Biomech. 2002;17:650–659 [DOI] [PubMed] [Google Scholar]
- 21.Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39:90–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moseley JB Jr, Jobe FW, Pink M, Perry J, Tibone JE. EMG analysis of the scapular muscles during a scapular rehabilitation program. Am J Sports Med. 1992;20:128–134 [DOI] [PubMed] [Google Scholar]
- 23.Kuhn JE, Plancher KD, Hawkins RJ. Scapular winging. J Am Acad Orthop Surg. 1995;3:319–325 [DOI] [PubMed] [Google Scholar]
- 24.Pink M, Perry J. Biomechanics. In Jobe FW, ed. Operative Techniques in Upper Extremity Sports Injuries. St. Louis, MO: Mosby; 1996:109–123 [Google Scholar]
- 25.Glousman R, Jobe FW, Tibone JE, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70:220–226 [PubMed] [Google Scholar]
- 26.Warner JJ, Micheli LJ, Arslenian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome: a study using Moire topographic analysis. Clin Orthop. 1992;285:191–199 [PubMed] [Google Scholar]
- 27.Thomson BC, Mitcheli LJ. The effects of repetitive exercise of the shoulder on the lateral scapular stability. Presented at: American Physical Therapy Association Combined Sections Meeting; February 2000; New Orleans, LA [Google Scholar]
- 28.Carpenter JE, Blasier RB, Pellizon GG. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med. 1998;26:262–265 [DOI] [PubMed] [Google Scholar]
- 29.Voight ML, Hardin JA, Blackburn TA, Tippett SR, Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23:348–352 [DOI] [PubMed] [Google Scholar]
- 30.Koslow PA, Prosser LA, Strony GA, Suchecki SL, Mattingly GE. Specificity of the lateral scapular slide test in asymptomatic competitive athletes. J Orthop Sports Phys Ther. 2003;33(6):331–336 [DOI] [PubMed] [Google Scholar]
- 31.Philip McClure, Angela R. Tate, Stephen Kareha, Dominic Irwin, Erica Zlupko. (2009) A Clinical Method for Identifying Scapular Dyskinesis, Part 1: Reliability. J Athl Train 2009;(44)2:160–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Myrer JW, Schulthies SS, Fellingham GW. Relative and absolute reliability of the KT‐2000 arthrometer for uninjured knees: testing at 67,89, 134, and 178 N and manual maximum forces. Am J Sports Med. 1996;24:104–108 [DOI] [PubMed] [Google Scholar]
- 33.Borich MR, Bright JM, Lorello DJ, et al. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit J Orthop Sports Phys Ther. 2006;36:926–34 [DOI] [PubMed] [Google Scholar]
- 34.Laudner Kevin G, Moline Mike T, Meister Keith. The relationship between forward scapular posture and posterior shoulder tightness among baseball players. Am J Sports Med. 2010;(38):2106–2112 [DOI] [PubMed] [Google Scholar]
- 35.Laudner KG, Stanek JM, Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med 2007;(35)12:2091–2095 [DOI] [PubMed] [Google Scholar]
- 36.Paine RM, Johnson RJ. (2009) Conditioning, training, and rehabilitation for the golfer’s shoulder. In The Athlete’s Shoulder 2nd Edition. 465–491 Churchill Livingstone Elsevier; Philadelphia PA [Google Scholar]
- 37.Kibler WB, Sciascia AD, Uhl TL, et al. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med. 2008:(36)9:1789–1798 [DOI] [PubMed] [Google Scholar]
- 38.Ekstrom RA, Donatelli RA, Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther 2003;33:247–58 [DOI] [PubMed] [Google Scholar]
- 39.Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39:105–17 [DOI] [PubMed] [Google Scholar]
- 40.Decker MJ, Hintermeister RA, Faber KJ, et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med 1999;27:784–91 [DOI] [PubMed] [Google Scholar]
- 41.Hintermeister RA, Lange GW, Schultheis JM, et al. Electromyographic activity and applied load during shoulder rehabilitation exercises using elastic resistance Am J Sports Med 1998;26:210–20 [DOI] [PubMed] [Google Scholar]
- 42.Moseley JB Jr, Jobe FW, Pink M, et al. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med 1992;20:128–34 [DOI] [PubMed] [Google Scholar]