US life expectancy stalls due to cardiovascular disease, not drug deaths (original) (raw)
Abstract
After decades of robust growth, the rise in US life expectancy stalled after 2010. Explanations for the stall have focused on rising drug-related deaths. Here we show that a stagnating decline in cardiovascular disease (CVD) mortality was the main culprit, outpacing and overshadowing the effects of all other causes of death. The CVD stagnation held back the increase of US life expectancy at age 25 y by 1.14 y in women and men, between 2010 and 2017. Rising drug-related deaths had a much smaller effect: 0.1 y in women and 0.4 y in men. Comparisons with other high-income countries reveal that the US CVD stagnation is unusually strong, contributing to a stark mortality divergence between the US and peer nations. Without the aid of CVD mortality declines, future US life expectancy gains must come from other causes—a monumental task given the enormity of earlier declines in CVD death rates. Reversal of the drug overdose epidemic will be beneficial, but insufficient for achieving pre-2010 pace of life expectancy growth.
Keywords: life expectancy, mortality, cardiovascular disease, drug-related mortality, opioid epidemic
Life expectancy in the United States increased at a phenomenal pace throughout the twentieth century, by nearly 2 y per decade (1). A major driver of the improvement after 1970 was the decline in cardiovascular disease (CVD) mortality. This “CVD revolution” has been attributed to improved pharmacological management, advances in surgical techniques, and healthier lifestyles (2). US death rates from CVD halved between 1970 and 2002 (3).
After 2010, however, US life expectancy growth stalled and has most recently been declining. A critical question for American health policy is how to return US life expectancy to its pre-2010 growth rate. While much attention is being directed at drug-related deaths (4–6), we demonstrate that the changing trajectory of CVD deaths has been the most consequential cause-specific trend for the post-2010 US life expectancy stall. This link has not been empirically demonstrated, in part, because past analyses have focused on the very recent period in which CVD mortality had already stalled. For example, Ho and Hendi (5) was concerned with the year-over-year life expectancy decline that occurred during 2014–2015, and concluded that the US decline was mainly attributable to drug-related mortality; and Barbieri (4) focused on drug-related mortality in an analysis of causes of deaths that have contributed to the US shortfall in life expectancy relative to 12 other high-income countries in 2014. Consistent with our findings, Barbieri (4) found that drug-related mortality accounted for only about 10% of the US shortfall in 2014, and concluded, “Overall, the largest [reduction in the US life expectancy shortfall] would be achieved by reducing the US disadvantage in mortality not from drug use, alcohol and chronic liver diseases or suicide, but from other broad cause-of-death categories.” In this paper, we show that CVD is the key cause-of-death category for understanding the US life expectancy stagnation.
A Cause-of-Death Accounting of the Post-2010 US Life Expectancy Stall
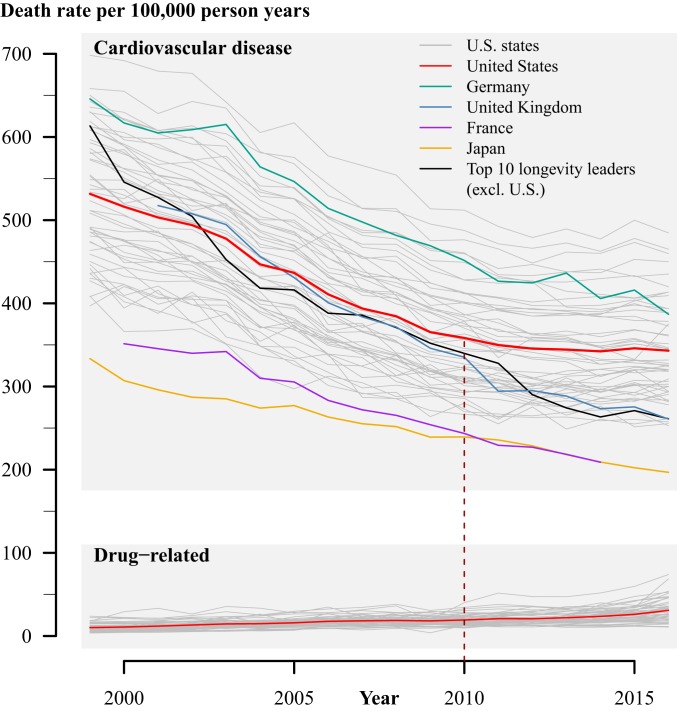
Fig. 1 compares the death rates from drug-related causes and CVD since 1999 on the same _y_-axis scale. At its peak, drug-related deaths reached a level of 30 deaths per 100,000 person-years in 2017. CVD mortality is on a level that is an order of magnitude higher, ranging between 350 and 550 deaths per 100,000 person-years during 1999–2017. Importantly, since 2010, declines in US CVD death rates have slowed dramatically. In 2010, US CVD mortality was similar to the mean of 10 high-ranking life expectancy countries, including the United Kingdom (Fig. 1). In 2016, the US CVD mortality rate exceeded that of the mean of 10 high life expectancy countries by a staggering 30%, or 80 deaths per 100,000 person-years. This stagnation—and, in some cases, reversal—has occurred for men and women, for most age groups, and in high and low life expectancy states in the United States (additional information linked at ref. 7).
Fig. 1.
Age-standardized death rates (per 100,000 person-years) from drug-related causes and CVD. Gray shaded lines are trends for individual US states and Washington, DC. US data are from the CDC Wonder Database. Longevity leaders is the average of countries that had the highest life expectancy at birth in year 2010 (Japan, Switzerland, Singapore, Australia, Spain, Iceland, Italy, Israel, Sweden, and France). Non-US data are from WHO Cause of Death Database. Sexes are combined. CVD deaths include deaths from heart attacks and strokes (ICD 10: I00 to I78). Drug-related causes include ICD 10: X40 to X44, X60 to X64, X85, and Y10 to Y14.
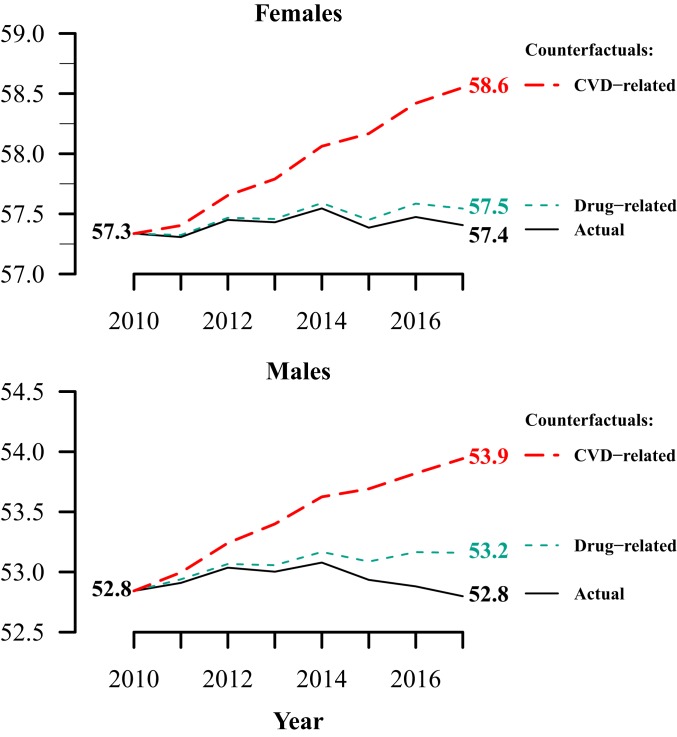
What would life expectancy be if drug-related deaths had not increased since 2010? And, what would life expectancy be if declines in CVD mortality had not stalled after 2010? We simulated life expectancies based on these counterfactual scenarios. The drug-related counterfactual held sex- and age-specific drug-related mortality fixed at its 2010 level, and estimated life expectancy at age 25 y (e25) for subsequent years. This simulation provides a trajectory of e25 under the counterfactual scenario of no rise in drug-related death rates since 2010. The CVD scenario simulated the e25 trajectory under the counterfactual that CVD death rates continued their 2000–2009 pace of decline. We applied the average annual decline in CVD death rates by sex at each single year of age (and for ages 85+ y) during 2000–2009 to each year in 2010–2017.
Fig. 2 shows the results. Between 2010 and 2017, US e25 changed by +0.07 y in women and −0.04 y in men (Fig. 2). If drug-related mortality stayed fixed at its 2010 level, e25 in 2017 would have been 0.36 and 0.14 y higher in men and women, respectively. In contrast, if CVD mortality continued its past rate of decline after 2010, e25 in 2017 would have been 1.14 y higher in both women and men. This number closely matches the 1.2-y growth in the gap in life expectancy between the United States and the average of the 27 European Union countries that constituted the union in 2010 (EU-27) between 2010 and 2017. The counterfactual exercise confirms that the slowdown of CVD progress has been much more consequential to US life expectancy than has the increasing drug-related mortality.
Fig. 2.
Actual and simulated life expectancy at age 25 y during 2010–2017 in men and women. Drug-related counterfactual is estimated by holding age-specific drug-related mortality fixed at its 2010 level through 2017. CVD counterfactual is estimated by extrapolating average age-specific changes in CVD mortality from 2000 to 2009 forward to 2017. Data are from the CDC Wonder database.
Our counterfactual simulations retain observed levels of all other death causes, so as to isolate the effects of drug-related and CVD deaths. The simulation relies on a reasonable potential pace of CVD mortality decline that would have put the United States on a similar trajectory with the mean of 10 high-income countries and the United Kingdom (7). Alternate counterfactuals are possible. Halving the simulated pace of progress in CVD mortality, using year 2000 as the benchmark for drug-related mortality, or starting the simulations at age 15 y do not change the conclusions (7). Analysis of cancer and other death causes confirms that they have contributed less to the US life expectancy stall than has CVD (7).
Implications
Americans have enjoyed robust gains in life expectancy for more than a generation. A persistent stagnation in US life expectancy would require social, economic, and political institutions to adapt. The opioid epidemic has clearly contributed to recent stagnation. We do not wish to diminish its importance. The troubling trend in US CVD mortality, however, is the main culprit for longer-term US life expectancy stagnation.
Woolf and Schoomaker (6) recently concluded that drug-related deaths have played a central role in recent US life expectancy trends, drawing from a rich description of mortality trends and a review of the existing literature, including Ho and Hendi’s (5) findings. Woolf and Schoomaker (6) did not perform a formal decomposition of the contributory roles of various death causes, and the authors focused on trends under age 65 y, although mortality dynamics at older ages have also been important for the life expectancy stagnation (7). Our formal analysis demonstrates, starkly, that the reversal of the drug-related mortality epidemic would not return the United States to a life expectancy trajectory that it experienced prior to 2010.
It is important to emphasize that there is no logical inconsistency in our finding that the longer-run stagnation in US life expectancy is due to the CVD stagnation and that the shorter-term decline in life expectancy over 2014–2015 is attributable to drug-related deaths (5). If an analysis does not include the inflection point in CVD mortality that occurred around 2010—as prior papers did not—it would miss the massive effect and importance of CVD on the longer-run life expectancy trend.
The flattening of the CVD mortality trend has been documented elsewhere, and it has been shown to be occurring in other countries (8–12). The US CVD stagnation is unusually strong, however, and a quantification of the role of the CVD stagnation to the post-2010 stagnation in US life expectancy has not been previously demonstrated. One potential explanation is that the United States is experiencing a “floor effect” in CVD mortality—further improvements are not possible without medical innovations. Our international comparison shows that this is not true, as US CVD mortality is increasingly lagging behind the average of 10 high life expectancy countries, and countries with historically low CVD mortality, such as Japan, continue to improve.
Alternative hypotheses need to be considered. Rising obesity is a worthy candidate. The US obesity epidemic started in the mid-1980s, ahead of other high-income countries. Recent cohorts have experienced obesity at a younger age than their predecessors. Moreover, the United States has a higher prevalence of diabetes compared to its peer countries. The timing of the cigarette smoking epidemic and, particularly, its recession may also be important. The United States was a leader in both the rise and fall of the smoking epidemic, and the United States may have already benefitted from most of the gains from declining smoking. European countries, in contrast, may still be enjoying robust mortality benefits from their more recent declines (8).
The United States has performed well in detecting and treating major CVD risk factors (13). Cholesterol, triglyceride, and low-density lipoprotein (LDL) levels did not worsen between 1999 and 2014, thanks to effective management and public awareness (14). Systolic blood pressure levels were also relatively stable from 1999 to 2016 (15). Thus, the stagnation may be less related to treatment failures and more due to unfavorable trends in the prevalence of underlying risk factors that require treatment.
Our supplemental analyses indicate that stagnating CVD mortality is occurring across most states, not only in disadvantaged ones (7). It is possible, nonetheless, that the stagnation is driven by subpopulations within states, and further distillation of this variation is important. It is also plausible that some of the explanations for rising drug-related deaths and stagnating CVD mortality are common. For example, social and economic despair may contribute to both (12, 16). Opioid use is a risk factor for heart disease (17), and a portion of CVD deaths may be attributable to opioid use (18).
Future gains in US life expectancy are jeopardized in the absence of a renewed decline in CVD mortality. Without this resumption, gains must come from improvements in other causes—a monumental task given the enormity of earlier declines in CVD mortality. Reversal of the drug overdose epidemic will be beneficial but, as we demonstrate, insufficient to returning the United States to its pre-2010 pace of life expectancy growth.
Materials and Methods
US data are from the Centers for Disease Control (CDC) Wonder database. Non-US data are from World Health Organization (WHO) Cause of Death Database. Drug-related deaths include deaths from legal and illegal substances and intentional (e.g., suicides) and unintentional (e.g., accidents) drug-related causes (International Classification of Disease [ICD] 10: X40 to X44, X60 to X64, X85, and Y10 to Y14). CVD deaths include deaths from heart attacks and strokes (ICD 10: I00 to I78). The life expectancies at age 25 y (e25) in Fig. 2 were produced using conventional period life table techniques using single year of age death rates for ages 25 y to 84 y and an open-ended interval for ages 85+ y. For additional information, see ref. 7.
Acknowledgments
We thank Christina Bohk-Ewald and Peng Li for technical assistance.
Footnotes
The authors declare no competing interest.
References
- 1.National Center for Health Statistics, Health, United States, 2005 With Chartbook on Trends in the Health of Americans. https://www.cdc.gov/nchs/data/hus/hus05.pdf. Accessed 1 February 2020.
- 2.Ford E. S., et al. , Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N. Engl. J. Med. 356, 2388–2398 (2007). [DOI] [PubMed] [Google Scholar]
- 3.Jemal A., Ward E., Hao Y., Thun M., Trends in the leading causes of death in the United States, 1970-2002. JAMA 294, 1255–1259 (2005). [DOI] [PubMed] [Google Scholar]
- 4.Barbieri M., The contribution of drug-related deaths to the US disadvantage in mortality. Int. J. Epidemiol. 48, 1026 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ho J. Y., Hendi A. S., Recent trends in life expectancy across high income countries: Retrospective observational study. BMJ 362, k2562 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woolf S. H., Schoomaker H., Life expectancy and mortality rates in the United States, 1959-2017. JAMA 322, 1996–2016 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta N. K., Abrams L. R., Myrskyla M., Additional information for the analysis of CVD and drug related mortality in the U.S. https://osf.io/u6dzp/?view_only=bc78d18059b042cf8ca4c4ff8f4dfd95. Accessed 18 November 2019.
- 8.Lopez A. D., Adair T., Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int. J. Epidemiol. 48, 1815–1823 (2019). [DOI] [PubMed] [Google Scholar]
- 9.Sidney S., et al. , Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 1, 594–599 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Shah N. S., et al. , Trends in cardiometabolic mortality in the United States, 1999-2017. JAMA 322, 780–782 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma J., Ward E. M., Siegel R. L., Jemal A., Temporal trends in mortality in the United States, 1969-2013. JAMA 314, 1731–1739 (2015). [DOI] [PubMed] [Google Scholar]
- 12.Case A., Deaton A., Mortality and morbidity in the 21st century. Brookings Pap. Econ. Act. 2017, 397–476 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Preston S. H., Ho J., Low Life Expectancy in the United States: Is the Health Care System at Fault? (National Academies Press, 2010). [Google Scholar]
- 14.Rosinger A., Carroll M. D., Lacher D., Ogden C., Trends in total cholesterol, triglycerides, and low-density lipoprotein in US adults, 1999-2014. JAMA Cardiol. 2, 339–341 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dorans K. S., Mills K. T., Yang L., Jiang H., Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline. J. Am. Heart Assoc. 7, e008888 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Case A., Deaton A., Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U.S.A. 112, 15078–15083 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishimura M., et al. , The impact of substance abuse on heart failure hospitalizations. Am. J. Med. 133, 207–213.e1 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glei D. A., Preston S. H., Estimating the impact of drug use on US mortality, 1999-2016. PLoS One 15, e0226732 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]