Transient complete heart block in a patient with critical COVID-19 (original) (raw)
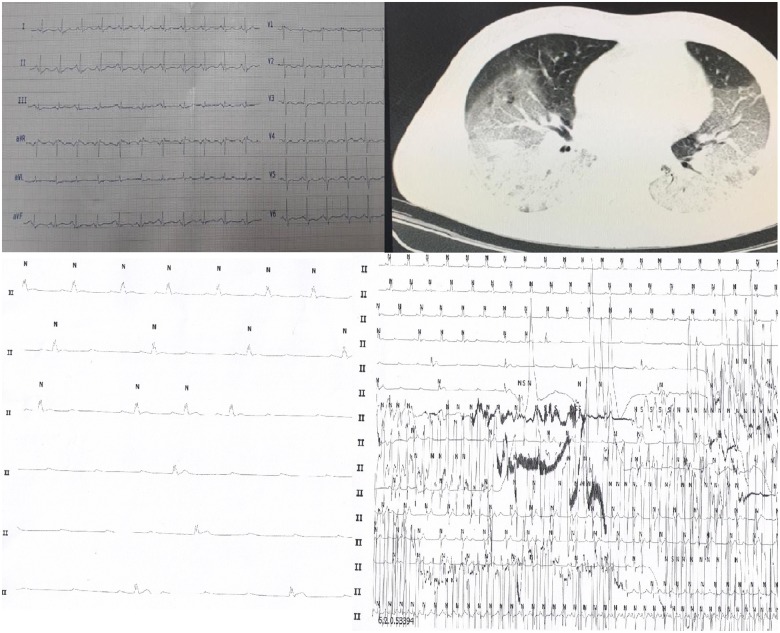
A 54-year-old man came to the Imam Khomeini hospital complex, Tehran, Iran due to shaking chills, dry cough, nausea, and vomiting during the outbreak of COVID-2019. In the emergency room, he had tachypnoea (respiratory rate 32/min), temperature 37.3°C, and O2 saturation of 76%, so he was admitted to the ward. Baseline ECG was normal (Panel A). High-resolution computed tomography showed bilateral ground-glass appearance (Panel B). PCR of the nasopharyngeal swab documented coronavirus infection. He was administered an antiviral and hydroxychloroquine. On the 13th day of hospital stay, due to aggravation of tachypnoea, he was intubated and transferred to the intensive care unit. Next morning, the patient suddenly developed complete heart block (CHB) (Panel C). Cardiopulmonary resuscitation (CPR) was performed for ∼10 min until resumption of normal sinus rhythm (Pancel D). Echocardiography showed normal left ventricular size and function with ejection fraction up to 50% without pericardial effusion. The patient remained in sinus rhythm until 30 March 30 when he died due to severe respiratory failure.
(A) A 12-lead ECG shows no atrioventricular block. (B) High-resolution computed tomography shows diffuse bilateral ground-glass opacities with some foci of consolidation formation in almost all lung lobes. (C) ECG of lead II shows CHB. (D) Acquired ECG of lead II at the rate of 6.25 cm/s. The upper part shows normal sinus rhythm, then proceeding to CHB. CPR was performed in the middle part of Holter monitoring with resultant artefacts. In the lower part of the Holter, the sinus rhythm returns.