Unique skin manifestations of COVID-19: Is drug eruption specific to COVID-19? (original) (raw)
Highlights
- •
COVID-19 is associated with specific skin manifestations and drug eruption. - •
This case shows COVID-19–related drug eruption and specific clinical features. - •
Drug eruption preceding COVID-19 symptoms may facilitate early diagnosis.
COVID-19 is associated with specific skin manifestations and drug eruption in some affected patients. Here, we report a case of suspected COVID-19–related drug eruption and specific clinical features.
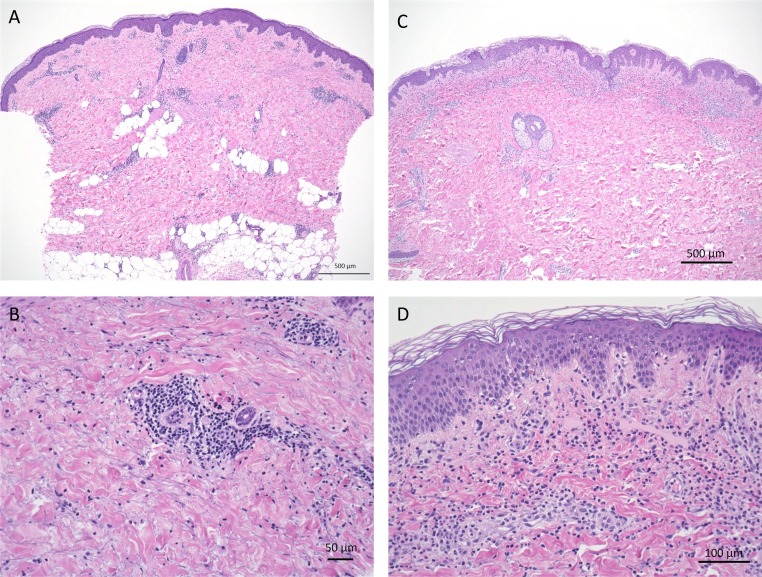
A 52-year-old woman visited our dermatology clinic with itchy erythematous lesions on her limbs and erosions on her lips and buccal mucosa. She had no flu symptoms or fever. She had been treated at a dental clinic 3 days prior (Day −3) and given antibiotics (cefcapene pivoxil hydrochloride hydrate) and the non-steroid anti-inflammatory drug (NSAID) loxoprofen sodium hydrate. Erythematous lesions and erosions on the lips appeared 2 days later (Day −1). Her blood counts were normal. The skin lesions were clinically diagnosed as a drug eruption (Day 0). Pathologic analysis of a skin biopsy sample obtained from an indurated erythematous lesion (Fig. 1) on her leg revealed slight liquefaction with perivascular and periadnexal mixed cell infiltrations from the papillary dermis to the deep subcutaneous tissue (Fig. 2A–B). Deep lymphocytic infiltrations are not typical for drug eruptions. Lymphocyte stimulation tests were performed for cefcapene pivoxil hydrochloride hydrate (stimulation index [SI]: 151%) and loxoprofen sodium hydrate (SI: 300%). Oral prednisolone (20 mg/day) was started immediately to treat oral lesion worsening. On Day 2, well-demarcated infiltrated erythema was observed on her trunk. The erosions of her lower lips and buccal mucosa gradually improved. The prednisolone was reduced to 10 mg/day.
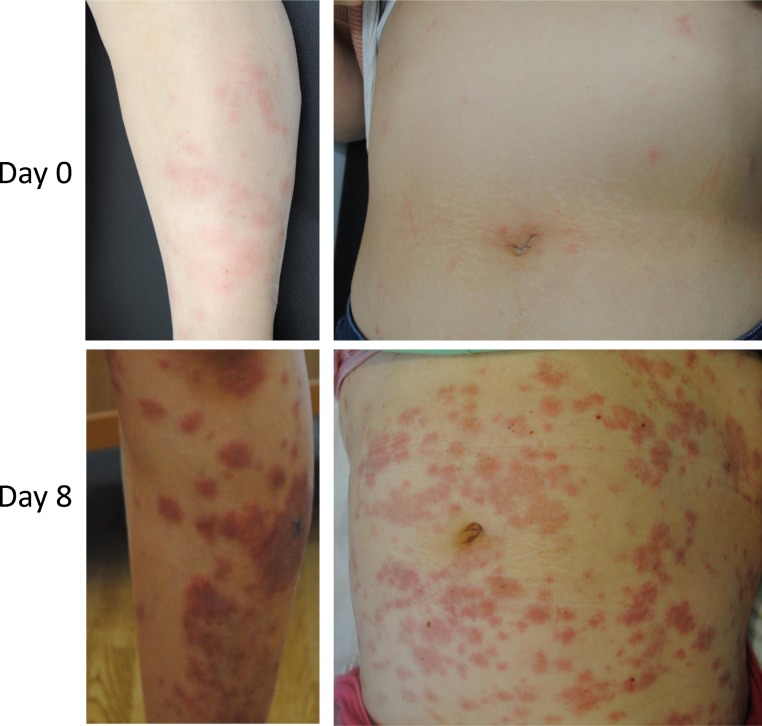
Fig. 1.
Clinical features of her trunk and leg Day 0, indurated erythema on her leg, and red papules and erythema on her trunk Day 8, dark red colored papules and indurated erythema were largely observed on her leg and trunk.
Fig. 2.
Pathologic findings (Day 0 and Day 8). (A, B): Pathologic analysis of a skin biopsy sample obtained from an indurated erythematous lesion (Day 0). The size of bar is indicated in the figure. (C, D): Pathologic analysis of a skin biopsy sample from an abdominal lesion. Interface changes with liquefaction and perivascular mixed cell infiltrations in the papillary dermis are observed. There are histiocytic infiltrations around the capillary vessels and neutrophils are scattered in the upper dermis (C–D). The size of bar is indicated in the figure.
Five days after decreasing the prednisolone (Day 7), she returned to our clinic with high fever, cough, chills, fatigue, and shortness of breath. She reported no travel history, but worked at a healthcare facility for elderly people. Computed tomography (CT) revealed slight ground glass opacity in the lower lung lobes. Blood tests revealed a high white blood cell count (22,300/μl) with lymphocytopenia (490/μl) and increased neutrophils (20,449/μl), high C-reactive protein (12·8 mg/dl), and normal lactic acid dehydrogenase (196 U/l). She was diagnosed with pneumonia and admitted to an isolation ward with suspicion of COVID-19. Lymphocytopenia is a COVID-19 severity factor [1]. On admission (Day 7), her erythematous lesions worsened precipitously. Serious infection led us to discontinue the oral prednisolone, and ampicillin/sulbactam and clarithromycin were administered. On Day 8, new macular papules and erythematous lesions appeared on her face and trunk with some petechiae (Fig. 1). A biopsy specimen was obtained from an indurated erythematous skin lesion on her abdomen. Pathologic analysis revealed interface changes with liquefaction and perivascular mixed cell infiltrations, including histiocytes and neutrophils, in the papillary dermis (Fig. 2C–D). The ampicillin/sulbactam was changed to levofloxacin. On Day 10, the erythematous lesions peaked and gradually pigmented. Polymerase chain reaction (PCR) analysis for COVID-19 on Day 1 of admission was negative, but computed tomography showed progression of the ground glass opacity. Repeat PCR for COVID-19 was positive on Day 3 of admission and the patient was diagnosed with COVID-19 and transferred to an intensive care unit at another hospital.
In this case, COVID-19 infection was suspected 10 days before onset. Drug eruption might develop during the latency period. COVID-19 is associated with drug eruptions, but the details remain unclear [2,3]. Drug hypersensitivity (11.4%) and urticaria (1.4%) have been self-reported by several patients. Drug eruption might not be merely incidental, but possibly related to COVID-19-induced cytokine storm with Th17 dysregulation [4]. NSAIDs may exacerbate symptoms of COVID-19, but no evidence has yet been provided [5]. Drug hypersensitivity may be due to aggravated inflammation. Drug eruption caused by NSAIDs preceding other symptoms of COVID-19 may facilitate early diagnosis based on specific features. In this case, the macular papule lesions and pathologic findings might be unique exacerbations of COVID-19.
Funding
None
Declaration of Competing Interest
No conflict of interest.
Acknowledgements
We declare no competing interests. We acknowledge SciTechEdit International, LLC (Highlands Ranch, CO, USA) for providing pro bono professional English-language editing of this article.
References
- 1.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng Y., Lai W. Dermatology staff participate in fight against Covid-19 in China. J. Eur. Acad. Dermatol. Venereol. 2020 doi: 10.1111/jdv.16390. [Epub ahead of print: Mar 23, 2020] [DOI] [PubMed] [Google Scholar]
- 3.Zhang J.J., Dong X., Cao Y.Y., Yuan Y.D., Yang Y.B., Yan Y.Q., Akdis C.A., Gao Y.D. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1111/all.14238. [Epub ahead of print: Feb 19, 2020] [DOI] [PubMed] [Google Scholar]
- 4.Wu D., Yang X.O. TH17 responses in cytokine storm of COVID-19: an emerging target of JAK2 inhibitor fedratinib. J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.03.005. [Epub ahead of print: Mar 11, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Russell B., Moss C., Rigg A., Van Hemelrijck M. COVID-19 and treatment with NSAIDs and corticosteroids: should we be limiting their use in the clinical setting? Ecancermedicalscience. 2020;14:1023. doi: 10.3332/ecancer.2020.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]