Associations of sedentary time and physical activity with adverse health conditions: Outcome-wide analyses using isotemporal substitution model (original) (raw)
Summary
Background
As one of the most common lifestyles today, sedentary behaviour is a risk factor for many health conditions. To inform potential behavioural guideline development, we aimed to estimate the theoretical effects of replacing sedentary behaviour with different intensity of physical activity on risks of 45 common non-communicable diseases (NCDs).
Methods
A total of 360,047 participants (aged 37-73 years) in the UK Biobank free of the 45 common non-communicable diseases (NCDs) were included. Information on sedentary time (sum of television watching, computer using and driving behaviour) and physical activity (measured by International Physical Activity Questionnaire questionnaire) were collected by self-reported at baseline. Participants were followed up for 45 NCDs diagnosis according to the ICD-10 code using linkage to national health records until 2020. Isotemporal substitution models were used to investigate substituting sedentary time with light physical activity (LPA), moderate physical activity (MPA) and vigorous physical activity (VPA) after adjusting for potential confounders.
Finding
Participants who reported > 6 h/day compared with ≤ 2 h/day sedentary time had higher risks of 12 (26.7%) of 45 NCDs, including ischemic heart disease, diabetes, chronic obstructive pulmonary disease, asthma, chronic kidney disease, chronic liver disease, thyroid disorder, depression, migraine, gout, rheumatoid arthritis and diverticular disease. Theoretically, replacing sedentary time with equivalent LPA, MPA and VPA was associated with risk reductions in 4, 6 and 10 types of NCDs, respectively. Among long sedentary time (> 6 h/day), replacing 1 h/day sedentary time with equivalent VPA showed stronger associations with 5 NCDs (diabetes, depression, chronic liver disease, diverticular disease and sleep disorder), with a larger risk reduction of 11%-31%.
Interpretation
Sedentary time is associated with multiple adverse health conditions, replacing sedentary time with any equivalent amounts of VPA than LPA and MPA could be associated with risk reductions of more types of NCDs.
Funding
National Natural Science Foundation of China.
Keywords: Sedentary behaviour, Physical activity, Chronic non-communicable diseases, Isotemporal substitution model
Research in context.
Evidence before the study
We searched PubMed for full-text original studies and review articles written in English published up to October 30, 2021, to identify papers on physical activity, sedentary behaviour and adverse health outcomes. The search terms used were “physical activity”, “sedentary behaviour”, together with “health outcome”. The most reference lists of the identified papers showed that sedentary behaviour and physical activity are independently associated with risk of some health outcomes; however, there was no study to date to systematically examine theoretical effects of replacing sedentary behavior with different intensity of physical activity on risk of multiple health outcomes.
Added value of the study
To the best of our knowledge, this is one of the largest single cohort studies of its kind to date that quantifies the replacing effect of sedentary behaviour with physical activity on health outcomes. We provide evidence that sedentary behaviour of > 6 h/day was associated with higher risks of 12 of 45 non-communicable diseases (NCDs) compared with ≤ 2 h/day sedentary behaviour, and replacing sedentary behaviour with equivalent light physical activity (LPA), moderate physical activity (MPA) and vigorous physical activity (VPA) was associated with risk reduction in 4, 6 and 10 types of NCDs, respectively.
Implications of all the available evidence
These findings have relevant individual, clinical, and public health implications as the results suggest that replacing sedentary behaviour with VPA could be a more beneficial way of reducing the risks of more NCDs.
Alt-text: Unlabelled box
Introduction
Sedentary time represents a major public health problem considering its high prevalence and health cost.1,2 In the UK, each adult spends an average 5 h/day of sedentary activities, 30% adults are sedentary for at least 6 h/day during the week, which rises to 37% on the weekend.1 Previous studies have reported that a person's waking day involves sedentary activities ubiquitously associated with prolonged sitting, such as watching television and using computer.3 Recent Canadian 24 h Movement Guidelines recommended that sedentary time limited to 8 h or less for adults, which includes no more than 3 h of recreational screen time for adults.4
Current guidelines and overviews systemically summarized the evidence regarding the effect of sedentary time on health conditions.4, 5, 6 For instance, it is suggested that longer sedentary time was associated with increased risk of all-cause mortality.7, 8, 9 Sedentary time was also an established risk factor for several non-communicable diseases (NCDs), such as cardiovascular disease (CVD),10 diabetes,11 and cognitive decline.12 Moderate evidence indicated an increased risk of colorectal, endometrial and lung cancer.13 However, most of the existing evidence have emerged from separate and heterogeneous studies. Therefore, this warrants investigation in one large-scale study oriented by outcomes-wide analyses.
Although sedentary time, physical activity, and sleeping are common behaviours that occupy a 24 h day, most previous studies have typically examined each behaviour without considering what time-dependent behaviours are being displaced. Isotemporal substitution model (ISM) uniquely enables examination of the potential effect on health outcomes of substituting one type of activity with another.14 A recent systematic review of compositional data analysis that included 1 prospective and 7 cross-sectional studies revealed associations between sleep, sedentary time, and physical activity with health outcomes in adults.15 A recent UK Biobank study found that time spent in moderate-vigorous physical activity was associated with lower mortality, irrespective of whether it replaced time spent sleeping, sedentary, or in light activity.16 However, there is less comprehensive evidence about the replacement effect of sedentary time with different intensity physical activity and sleeping on various health outcomes in a large longitudinal study.
To strengthen the existing evidence about the influence of sedentary time and to inform the development and evaluation of physical activity interventions, we examined the comprehensive associations of sedentary time with the risks of 45 NCDs, and our primary objectives were to assess whether substituting periods of daily sedentary time with light physical activity (LPA), moderate physical activity (MPA), vigorous physical activity (VPA) and sleeping were associated with lower risks of some NCDs.
Methods
Study design and population
This was a prospective, population-based cohort study of participants enrolled in the UK Biobank. Between April 2006 and December 2010, the UK Biobank recruited 502,528 adults (37–73 years old) from the general population. Participants attended one of 22 assessment centers across England, Scotland, and Wales, where they completed touchscreen and nurse-led questionnaires, had physical measurements taken, and provided biological samples.17 In the current study, sedentary time, physical activity and sleep duration were used as exposures and 45 types of NCDs as outcomes. Participants were excluded if they had any of history of NCDs before recruitment, missing information on exposures or covariates, leaving 360,047 participants included in final study (Supplemental Figure S1). All participants gave written informed consent prior data collection. This study was performed under generic ethical approval obtained by the UK Biobank from the National Health Service National Research Ethics Service (approval letter ref 11/NW/0382, dated 17 June 2011).
Exposure variables
Sedentary behaviours in leisure time were self-reported and collected using questionnaires at baseline. Participants were asked in a typical day how many hours they spent watching television, using computer and driving. This information was used as an indicator of sedentary behaviours as television watching, time spent using computers and driving are three of the most wide-spread leisure-time sedentary behaviours in adults.18
The questions on physical activity that were included in the UK Biobank baseline questionnaire were adapted from the International Physical Activity Questionnaire (IPAQ) short form, a validated survey instrument.19 The questions captured the frequency and duration of three different intensity of activities (light, moderate, and vigorous). The number of days per week that participants engaged in each level of physical activity was multiplied by the number of minutes spent per day doing that activity. This gave the total number of minutes spent per week engaged in each activity category, then we calculate the mean hours spent per day.
Sleep duration was collected by self-reported. Participants were asked the following: “About how many hours sleep do you get in every 24 h? (please include naps).” The answer could only contain integer values. We treated sleeping as a piecewise variable with a breakpoint at 7 h (≤ 7 h/day and > 7 h/day), where each of the two sleeping variables had an approximately linear association with mortality.20
Outcome ascertainment
The primary outcomes for this study were the incidence of 45 types of NCDs. All residents in England, Scotland, and Wales have a unique National Health Service (NHS) identification number, which we used to link all participants to electronic health records. Participants were followed starting at inclusion until the incidence of first NCDs, the date of death, or the end of the follow-up (September 30, 2020), whichever came first. The diagnosis for incident NCDs was coded according to the WHO International Classification of Diseases Tenth Revision (ICD-10). We focused on eight ICD-10 disease chapters that concern neoplasms, endocrine, nutritional, and metabolic diseases, mental and behavioural disorders, diseases of the nervous system, the circulatory system, the respiratory system, the digestive system, the musculoskeletal system. Detailed information on ICD-10 was presented in Supplemental Table S1.
Covariates
Covariates of our analysis included exact age, sex, ethnicity (White, Black, South Asian, Mixed background), socioeconomic status (Townsend Deprivation Index, quintiles), employment status (worked, unemployed, retired, others), education attainment (college or university degree, professional qualifications, others), smoking status (never, former, current), consumption of alcohol intaking (continuous, g/day), and body mass index (BMI, kg/m2). Further details for each variable are available on the UK Biobank Website (https://www.ukbiobank.ac.uk/).
Statistical analysis
We summarized baseline characteristics by sedentary behaviour using descriptive statistics, reporting the mean and standard deviation (SD) of normal distribution or median and interquartile ranges of non-normal distribution for continuous variables, and proportions for categorical variables. We compared the baseline characteristics by sedentary behaviour using Chi-square test for categorical or One-Way ANOVA for continuous variables.
Cox proportional hazards models with age as timescale were used to estimate the hazard ratio (HR) and 95% confidence interval (CI) of individual NCDs for sedentary time. All models were adjusted for sex, ethnicity, Townsend Deprivation Index, employment status, educational attainment, smoking status, alcohol intake and BMI. Specially, multivariable models of NCDs related to female (breast, cervix, endometrium and ovary cancer) were additionally adjusted for menopause status and hormone replacement therapy. The proportional hazard assumption was checked by tests based on Schoenfeld residuals, and the results indicated that the assumptions had not been violated. The non-linear associations were tested by restricted cubic spline functions. Likelihood ratio tests were used to examine the non-linearity of sedentary time by comparing models including spline or not. Moreover, to quantify the contribution of longer sedentary time to the burden of individual NCDs, we calculated population attributable fraction (PAF), which can be interpreted as the proportional reduction in population incidence that would have occurred during follow-up if all participants had adopted a shorter sedentary time.
ISM was used to estimate the effects of replacing sedentary time as a continuous variable with different intensity of physical activity (light, moderate and vigorous) and sleep duration on risk of individual NCD. Compared with conventional regression modelling, ISM can provide a more accurate estimation of the potential effects of different activities.14,21,22 The ISM analyses make a more realistic assumption that an increase in one behaviour will be accompanied by a decrease of equivalent duration (isotemporal) in another behaviour while total time in all behaviours is kept constant.
In the sensitivity analysis, we undertook a series of analyses to test the robustness of our findings. First, partition models that additionally adjusted for different intensity of physical activity and sleeping were fitted to examine the statistically independent roles of other activities in the associations between sedentary time and individual NCD. Second, to minimize the potential contribution of reverse causality to these findings, we did a landmark analysis excluding NCDs occurring within the two years after recruitment. Third, to investigate the extent to which any attrition bias from the missing data affected our results, we repeated the main analyses in a full cohort with imputed data. The missing data were estimated by multiple imputation models by chained equations. Finally, to investigate residual confounding by smoking, we repeated the analyses after excluding current and former smokers.
All analyses were performed using STATA 15 statistical software (StataCorp) and R i386 3.4.3 (R Foundation for Statistical Computing). Because of potentially inflated type I errors due to multiple tests, all analyses were corrected for multiple testing using Bonferroni's method (for 45 tests, P < 0.0011).23
Role of the funding source
The sponsor had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to the data in the study and had final responsibility for the decision to submit for publication.
Results
We included 360,047 participants (54.5% female) who took part in the 2006–2010 examination. The mean age of participants was 55.8±8.1 (range 37-73) years, with all participants being followed up to 2020. There were 67,034 (18.6%) participants reported a sedentary time of over 6 h/day. Supplemental Figure S2 shows the distribution of sedentary time among participants. Table 1 shows the baseline characteristics of the study population by sedentary time.
Table 1.
Baseline characteristics of participants by sedentary time.
| Characteristics | Total | Sedentary time (h/day) | P value | |||
|---|---|---|---|---|---|---|
| ≤ 2.0 | 2.1-4.0 | 4.1-6.0 | >6 | |||
| Total | 360,047 | 42,336 (11.8) | 135,486 (37.6) | 115,191 (32.0) | 67,034 (18.6) | |
| Sex | <0.001 | |||||
| Male | 163,732 (45.5) | 14,454 (34.1) | 52,927 (39.1) | 55,582 (48.3) | 40,769 (60.8) | |
| Female | 196,315 (54.5) | 27,882 (65.9) | 82,559 (60.9) | 52,927 (39.1) | 26,265 (39.2) | |
| Age (mean, SD) | 55.8 (8.1) | 54.7 (8.1) | 55.5 (8.1) | 56.7 (8.0) | 56.0 (8.1) | <0.001 |
| Townsend deprivation index | <0.001 | |||||
| 1 (Least deprived) | 72,330 (20.1) | 6986 (16.5) | 28,362 (20.9) | 24,642 (21.4) | 12,340 (18.4) | |
| 2 | 71,775 (19.9) | 7224 (17.1) | 27,607 (20.4) | 24,240 (21.0) | 12,704 (18.9) | |
| 3 | 72,131 (20.0) | 7724 (18.2) | 27,274 (20.1) | 23,792 (20.7) | 13,341 (19.9) | |
| 4 | 72,043 (20.0) | 9177 (21.7) | 27,156 (20.0) | 22,181 (19.3) | 13,529 (20.2) | |
| 5 (Most deprived) | 71,768 (19.9) | 11,225 (26.5) | 25,087 (18.5) | 20336 (17.6) | 15,120 (22.6) | |
| Ethnicity | <0.001 | |||||
| White | 342,787 (95.2) | 39,734 (93.8) | 129,928 (95.9) | 110,523 (95.9) | 62,602 (93.4) | |
| Black | 5153 (1.4) | 626 (1.5) | 1370 (1.0) | 1432 (1.2) | 1725 (2.6) | |
| South Asian | 7052 (2.0) | 1156 (2.7) | 2501 (1.8) | 1853 (1.6) | 1542 (2.3) | |
| Mixed background | 5055 (1.4) | 820 (1.9) | 1687 (1.3) | 1383 (1.2) | 1165 (1.7) | |
| Employment status | <0.001 | |||||
| Worked | 223,180 (62.0) | 29,323 (69,3) | 88,241 (65.1) | 65,525 (56.9) | 40,091 (59.8) | |
| Retired | 110,024 (30.6) | 9519 (22.5) | 38,229 (28.2) | 41,431 (36.0) | 20,845 (31,1) | |
| Unemployed | 21,629 (6.0) | 2759 (6.5) | 7183 (5.3) | 6668 (5.8) | 5019 (7.5) | |
| Others | 5214 (1.5) | 735 (1.7) | 1833 (1.4) | 1567 (1.4) | 1079 (1.6) | |
| Education level | <0.001 | |||||
| College or university degree | 130,303 (36.2) | 21,334 (50.4) | 53,830 (39.7) | 36,394 (31.6) | 18,745 (28.0) | |
| Professional qualifications | 180,471 (50.1) | 16,972 (40.1) | 65,929 (48.7) | 60,987 (52.9) | 36,583 (54.6) | |
| Others | 49,273 (13.7) | 4030 (9.5) | 15,727 (11.6) | 17,810 (15.5) | 11,706 (17.5) | |
| Smoking status | <0.001 | |||||
| Never | 204,100 (56.7) | 26,546 (62.7) | 80,612 (59.5) | 63,268 (54.9) | 33,674 (50.2) | |
| Former | 121,038 (33.6) | 12,182 (28.8) | 43,229 (31.9) | 40,744 (35.4) | 24,883 (37.1) | |
| Current | 34,909 (9.7) | 3608 (8.5) | 11,645 (8.6) | 11,179 (9.7) | 8477 (12.7) | |
| Alcohol intake (g/day; mean, SD) | 15.2 (18.0) | 13.1 (17.0) | 14.4 (16.7) | 15.8 (18.2) | 17.1 (20.5) | <0.001 |
| Hypertension | 247,173 (68.7) | 25,282 (59.7) | 89,791 (66.3) | 82,487 (71.6) | 49,613 (74.0) | <0.001 |
| SBP (mmHg; mean, SD) | 138 (18) | 134 (19) | 137 (19) | 139 (19) | 139 (18) | <0.001 |
| DBP (mmHg; mean, SD) | 82 (10) | 80 (10) | 82 (10) | 83 (10) | 84 (10) | <0.001 |
| BMI (kg/m2; mean, SD) | 27.0 (4.5) | 25.3 (4.1) | 26.4 (5.3) | 27.5 (4.4) | 28.5 (4.8) | <0.001 |
| Sleep duration (h/day; mean, SD) | 7.15 (1.03) | 7.16 (1.01) | 7.16 (0.98) | 7.17 (1.03) | 7.11 (1.11) | <0.001 |
| LPA (h/day; mean, SD) | 0.80 (1.09) | 0.86 (1.19) | 0.83 (1.13) | 0.80 (1.10) | 0.68 (0.92) | <0.001 |
| MPA (h/day; mean, SD) | 0.58 (0.94) | 0.63 (1.03) | 0.61 (0.98) | 0.59 (0.94) | 0.49 (0.79) | <0.001 |
| VPA (h/day; mean, SD) | 0.20 (0.38) | 0.22 (0.40) | 0.21 (0.39) | 0.20 (0.37) | 0.18 (0.35) | <0.001 |
Estimated dose-response associations between sedentary time and individual NCD are presented from restricted cubic spline models (Supplemental Figure S3), and sedentary time was overall associated with risks of 17 types of NCDs. For 14 of the 17 NCDs, there was evidence of linear associations, including ischemic heart disease (IHD), lung cancer, chronic obstructive pulmonary disease (COPD), asthma, diabetes, thyroid disorder, migraine, sleep disorder, anxiety, chronic liver disease (CLD), chronic kidney disease (CKD), inflammatory bowel disease (IBD), diverticular disease and rheumatoid arthritis. In contrast, the associations between sedentary time and another 3 NCDs (dementia, depression, schizophrenia) were curvilinear.
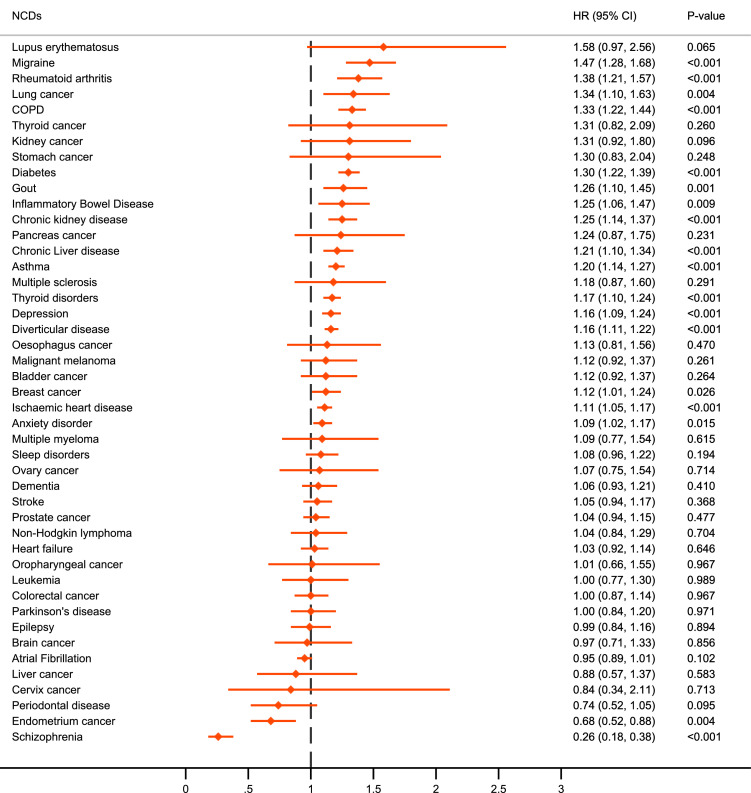
When sedentary time was categorized, we found that sedentary time was associated with higher risk of 12 of 45 types of NCDs comparing > 6 h/day to ≤ 2 h/day sedentary time (P < 0.0011) (Figure 1, Supplemental Table S2), including migraine, rheumatoid arthritis, COPD, diabetes, gout, CKD, CLD, asthma, thyroid disorder, depression, diverticular disease and IHD. Moreover, sedentary time was inversely associated with the risk of schizophrenia, with the HR that compared > 6 h/day to ≤ 2 h/day of sedentary time being 0.26 (95% CI: 0.18-0.38).
Figure 1.
The hazard ratios of NCDs for sedentary time higher than 6 h/day compared with less than 2 h/day. Each box of forest plot indicates the hazard ratios and confidence interval for individual NCD. The models were adjusted for age (timescale), sex, ethnicity, Townsend Deprivation Index, employment status, educational attainment, smoking status, alcohol intake and BMI. Multivariate models for specific disorders for female (breast, cervix, endometrium and ovary cancer) were additionally adjusted for menopause status and hormone replacement therapy. All P values were corrected for multiple testing by using the Bonferroni's method (P < 0.0011).
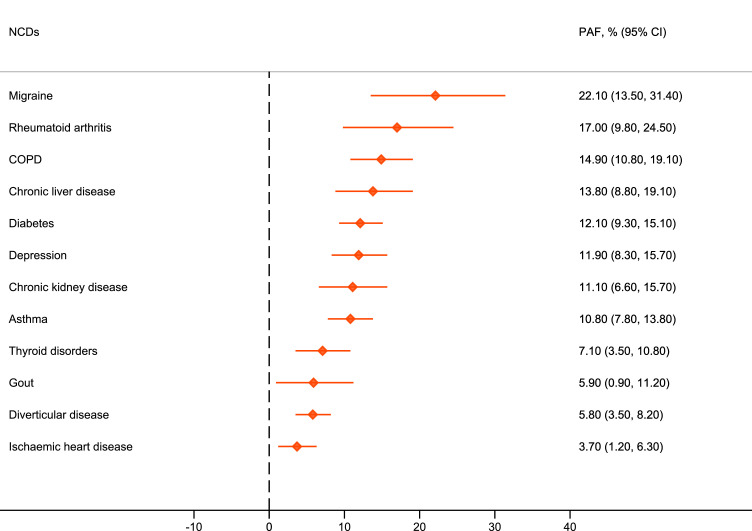
We estimated PAF for individual NCD that were significantly related to sedentary time (Figure 2). The contribution of > 6 h/day sedentary time to NCDs was orderly migraine, rheumatoid arthritis, COPD, CLD, diabetes, depression, CKD, asthma, thyroid disorders, gout, diverticular disease and IHD. These findings illustrated that 3.7%-22.1% NCDs cases would theoretically not have occurred if sedentary time of all participants had decreased to less than 6 h/day, assuming a causal relation.
Figure 2.
Multivariable-adjusted population attributable fraction (PAF) for NCDs by over 6 h/day sedentary time. Each box of forest plot indicates the population attributable fraction (PAF) and confidence interval for individual NCD, which can be interpreted as the proportional reduction in population incidence that would have occurred during follow-up if all participants had adopted a sedentary time with < 6 h/day. The models were adjusted for age (timescale), sex, ethnicity, Townsend Deprivation Index, employment status, educational attainment, smoking status, alcohol intake and BMI.
Results of the ISM are shown in Table 2. There were beneficial associations with diabetes and CKD for replacing 1 h/day sedentary time with equivalent any activities, including sleeping in those sleeping for ≤ 7 h/day, sleeping for >7 h/day, LPA, MPA and VPA. Substituting 1 h/day of sedentary time with equivalent LPA was associated with a small reduction in diabetes, CKD, diverticular disease and depression, with a 2%-5% risk reduction. Substituting 1 h/day of sedentary time with equivalent MPA was associated with a lower risk of 6 types of NCDs (including diabetes, CKD, COPD, diverticular disease, CLD and dementia), with a 2%-12% risk reduction. In contrast, replacing 1 h/day sedentary time with equivalent VPA was associated with a lower risk of 6 types of 10 types of NCDs (diabetes, CKD, COPD, diverticular disease, depression, CLD, IHD, lung cancer, IBD and sleep disorder), with a relatively large reduction of 7%–19%.
Table 2.
Hazard ratios for NCDs that was related to sedentary time when substituting 1 h/day of sedentary time with equivalent duration of other types of activity using isotemporal substitution model.
| NCDs | Sleeping (≤7 h) | Sleeping (>7 h) | LPA | MPA | VPA |
|---|---|---|---|---|---|
| Diabetes | 0.97 (0.96–0.98) | 1.09 (1.05–1.12) | 0.98 (0.96–0.99) | 0.94 (0.92–0.96) | 0.85 (0.81–0.89) |
| CKD | 0.97 (0.96–0.99) | 1.10 (1.05–1.16) | 0.95 (0.93–0.98) | 0.94 (0.92–0.97) | 0.89 (0.83–0.95) |
| COPD | 0.96 (0.95–0.98) | 1.04 (0.99–1.08) | 1.00 (0.98–1.02) | 0.96 (0.94–0.98) | 0.81 (0.76–0.86) |
| Diverticular disease | 0.98 (0.97–0.99) | 1.01 (0.98–1.04) | 0.98 (0.97–0.99) | 0.98 (0.97–0.99) | 0.93 (0.90–0.96) |
| Depression | 0.99 (0.98–1.00) | 1.23 (1.20–1.27) | 0.98 (0.96–0.99) | 0.98 (0.96–1.01) | 0.91 (0.87–0.96) |
| CLD | 0.98 (0.96–1.00) | 1.05 (0.99–1.11) | 1.01 (0.99–1.03) | 0.94 (0.91–0.97) | 0.88 (0.81–0.95) |
| IHD | 0.99 (0.98–1.00) | 1.03 (1.00–1.07) | 1.00 (0.99–1.02) | 0.99 (0.98–1.01) | 0.91 (0.87–0.94) |
| Lung cancer | 0.98 (0.95–1.01) | 1.06 (0.96–1.19) | 0.98 (0.93–1.03) | 0.97 (0.91–1.02) | 0.86 (0.74–0.99) |
| IBD | 0.99 (0.96–1.02) | 1.00 (0.89–1.12) | 0.99 (0.95–1.03) | 0.97 (0.92–1.02) | 0.85 (0.95–0.96) |
| Sleep disorder | 0.99 (0.97–1.01) | 1.07 (1.00–1.15) | 0.98 (0.95–1.01) | 0.98 (0.95–1.02) | 0.85 (0.77–0.93) |
| Dementia | 0.99 (0.96–1.01) | 1.12 (1.04–1.21) | 1.03 (0.99–1.06) | 0.88 (0.85–0.92) | 1.09 (1.00–1.19) |
| Anxiety disorder | 1.00 (0.98–1.01) | 1.17 (1.12–1.22) | 0.99 (0.97–1.01) | 0.99 (0.96–1.01) | 0.96 (0.90–1.01) |
| Rheumatoid arthritis | 0.98 (0.96–1.01) | 1.10 (1.02–1.18) | 0.98 (0.95–1.02) | 0.98 (0.94–1.02) | 0.92 (0.83–1.02) |
| Migraine | 0.95 (0.93–0.98) | 1.01 (0.92–1.10) | 0.99 (0.95–1.02) | 0.97 (0.93–1.01) | 0.90 (0.81–1.01) |
| Asthma | 0.98 (0.97–0.99) | 1.01 (0.97–1.04) | 0.99 (0.98–1.00) | 0.99 (0.97–1.01) | 1.00 (0.96–1.04) |
| Thyroid disorders | 0.99 (0.91–1.09) | 1.26 (0.96–1.66) | 0.97 (0.85–1.12) | 0.89 (0.74–1.07) | 1.01 (0.68–1.50) |
While we replaced different duration of daily sedentary time with equivalent physical activity, we found that there were linear effects of replacing sedentary time with LPA, MPA and VPA on the several NCDs (Supplemental Table S3). For instance, replacing 0.5 h/day sedentary time with VPA was substantially associated with 10% and 8% lower risk of COPD and diabetes. Strikingly, the effects of sedentary time replacing another behaviour and of sedentary time being displaced by another behaviour are asymmetric. Substituting 1 h/day VPA with equivalent sedentary time was associated with 17% and 12% higher risk of diabetes and CKD (Supplemental Table S4). In addition, in participants with > 6 h/day sedentary time, replacing 1 h/day sedentary time with equivalent MPA was separately associated with 8% and 21% lower risks of COPD and dementia, and replacing 1 h/day sedentary time with equivalent VPA was associated with lower risk of 5 NCDs (diabetes, diverticular disease, depression, CLD and sleep disorder), with a larger reduction of 11%-31% (Table 3).
Table 3.
Hazard ratios for NCDs that was related to sedentary time when substituting 1 h/day of sedentary time with equivalent duration of other types of activity using isotemporal substitution model in participants with over 6 h/day sedentary time.
| NCDs | Sleeping (≤7 h) | Sleeping (>7 h) | LPA | MPA | VPA |
|---|---|---|---|---|---|
| Diabetes | 0.94 (0.92–0.96) | 1.00 (0.94–1.06) | 0.97 (0.93–1.00) | 0.96 (0.92–1.01) | 0.73 (0.66–0.81) |
| Chronic kidney disease | 0.96 (0.92–0.99) | 1.04 (0.94–1.15) | 0.94 (0.89–1.00) | 0.93 (0.87–1.00) | 0.93 (0.80–1.09) |
| COPD | 0.96 (0.93–0.98) | 1.00 (0.91–1.09) | 1.03 (0.98–1.08) | 0.92 (0.87–0.98) | 0.89 (0.78–1.01) |
| Diverticular disease | 0.98 (0.96–1.00) | 1.00 (0.94–1.06) | 0.99 (0.96–1.02) | 0.96 (0.93–1.00) | 0.89 (0.82–0.97) |
| Depression | 0.98 (0.95–1.01) | 1.21 (1.13–1.29) | 1.01 (0.97–1.06) | 0.95 (0.90–1.01) | 0.85 (0.75–0.97) |
| Chronic liver disease | 0.99 (0.95–1.03) | 0.98 (0.87–1.11) | 1.02 (0.96–1.08) | 0.93 (0.86–1.01) | 0.80 (0.66–0.97) |
| Ischaemic heart disease | 0.98 (0.96–1.00) | 1.02 (0.96–1.09) | 0.99 (0.96–1.02) | 0.96 (0.92–1.00) | 0.93 (0.85–1.02) |
| Lung cancer | 1.00 (0.92–1.08) | 1.01 (0.80–1.27) | 0.97 (0.85–1.09) | 0.89 (0.77–1.04) | 1.23 (0.94–1.60) |
| Inflammatory Bowel Disease | 0.87 (0.81–0.93) | 0.70 (0.53–0.92) | 0.98 (0.88–1.08) | 0.95 (0.84–1.08) | 0.75 (0.55–1.02) |
| Sleep disorder | 1.00 (0.96–1.04) | 1.08 (0.96–1.22) | 0.99 (0.93–1.06) | 1.06 (0.98–1.15) | 0.69 (0.56–0.86) |
| Dementia | 0.94 (0.88–0.99) | 1.08 (0.93–1.25) | 1.02 (0.93–1.12) | 0.79 (0.70–0.88) | 1.14 (0.92–1.40) |
| Anxiety disorder | 0.96 (0.93–1.00) | 1.10 (1.01–1.19) | 0.96 (0.91–1.01) | 0.93 (0.88–1.00) | 1.02 (0.89–1.16) |
| Rheumatoid arthritis | 0.99 (0.94–1.05) | 1.09 (0.94–1.26) | 0.99 (0.91–1.08) | 1.04 (0.94–1.14) | 0.99 (0.79–1.24) |
| Migraine | 0.98 (0.92–0.95) | 1.05 (0.87–1.25) | 1.03 (0.93–1.13) | 0.98 (0.87–1.11) | 0.84 (0.63–1.11) |
| Asthma | 0.98 (0.96–1.00) | 0.98 (0.90–1.05) | 0.99 (0.95–1.03) | 1.00 (0.95–1.04) | 1.02 (0.93–1.12) |
| Thyroid disorders | 0.87 (0.71–1.07) | 1.03 (0.56–1.89) | 1.31 (1.05–1.62) | 0.72 (0.44–1.17) | 0.32 (0.07–1.40) |
The robustness of the associations between CVH and stroke events was examined by several sensitivity analyses. First, in partition model, additional adjustment for sleep duration and different intensity of physical activity was not essentially changed the association between sedentary time and individual NCDs (Supplemental Table S5), which indicated these associations were statistically independent of physical activity and sleeping. Second, we repeated the main analysis among participants with at least 2 years of follow-up, and the HRs of individual NCDs comparing > 6 h/day to ≤ 2 h/day sedentary time were similar (Supplemental Table S6). Third, the associations between sedentary time and individual NCDs with multiple imputed data showed that the HRs remained essentially unchanged (Supplemental Table S7). Finally, the results of non-smoking participants were generally consistent with the main analyses that sedentary time was associated with high risks of the NCDs, except for IHD (Supplemental Table S8).
Discussion
Our comprehensive analysis of a large UK-based prospective study showed linear dose-response associations of sedentary time with 14 types of NCDs. Sedentary time of > 6 h/day was found to be associated with increased risk of 12 of the 45 NCDs, statistically independent of physical activity and sleeping. Replacing sedentary time with equivalent VPA than LPA and MPA could be associated with risk reduction of more types of NCDs.
For cardiometabolic diseases, our study was consistent with a previous study of older US women showing that high sedentary time was associated with increased risks of CVD and coronary heart disease in a dose-response manner.10 A meta-analysis that included 9 prospective cohort studies also summarized a link between the highest sedentary time category and an increased risk of CVD, but presented a non-linear association.24 A previous study that included 71,018 US women reported a weak association between prolong sitting time (≥10 h/day) and risk of stroke.25 Similarly, a previous study that included 82,695 US men showed sedentary time of ≥ 5 h/day was associated with high risk of heart failure. In the current study, no significant associations of high sedentary time defined over 6 h/day with stroke, heart failure or atrial fibrillation, the reason may be different definition of sedentary time or heterogeneity of study population. There was a consensus that high sedentary time increased the risk of diabetes, with a linear association.11,26 Sedentary behaviour reduces voluntary energy expenditure, inhibits the activation of the body's largest skeletal muscles, and further leading to reducing venous and arterial blood flow, all of which might contribute to impaired glucose metabolism.10
For neoplasms, we only found suggestive evidence about the associations of sedentary time with lung, breast and endometrium cancer before multiple correction, which were generally similar to a recent review that sedentary time, independent of physical activity, has been shown to increase the risk of colon, endometrial, and lung cancers.27 Previous studies also demonstrated no significant associations with multiple site-specific cancer, such as ovary,28 prostate,29 oesophago gastric,30 colorectal cancer.13 Moreover, a meta-analysis including 43 observational studies almost presented consistent associations between sedentary time and site-specific cancers.31 While sedentary time may be linked to cancer biomarkers of low energy expenditure, postural effects could also be involved. The physiological mechanisms activated by standing might lead to improved glucose regulation, mitochondrial function, and endothelial function.32
The range of health conditions in our study expanded upon previous studies focusing on sedentary time and NCDs. The association between sedentary time and dementia was controversial. Our findings were in accordance with a previous study using five population cohort that revealed no significant association between sedentary time and cognition.33 However, a system review and meta-analysis reported an association between high sedentary time and increased risk of dementia, although subgroup analyses showed no statistically significant differences.12 A recent meta-analysis of 12 prospective studies identified an increased risk of depression due to mentally passive sedentary time, especially watching television.34 Additional studies also reported a significant link between sedentary time and depression/anxiety symptoms.35,36 Moreover, several previous studies reported an increased sedentary time in schizophrenia patients, but no studies examined this prospective association.37,38 Our study found that sedentary time was inversely associated with the risk of schizophrenia, which may be explained by unmeasured confounding or reverse causality. Future studies should focus on the physiological and psychological mechanisms. Although previous studies involved the relationship between sedentary time and respiratory diseases,39 there was limited evidence about prospective associations with COPD and asthma in large-scale population-based studies. Importantly, our studies provided comprehensive prospective associations of sedentary time with some NCDs that were rarely studied, such as migraine, rheumatoid arthritis, gout, CKD, CLD, thyroid disorder and diverticular disease.
In particular, television watching and using computer were often used as proxy for total leisure sedentary behaviours in observational studies,13,30,40,41 because the behaviours are modifiable by intervention and showed higher validity than total sedentary behaviours as it is easier to recall.42 Leisure television and computer time were associated with less and shorter breaks, lower total energy expenditure and different snacking behaviours, possibly increasing adverse effects of prolonged sitting.43 Besides, current public health physical activity recommendations are primarily based on epidemiological evidence of non-substitution models. Our study showed that the ISM provided richer and more specific information than previous “static” methods. It would capture greater benefits when replacing sedentary time with different intensity of physical activity.21,44,45
Assuming that our findings represented causal effects, substituting sedentary time with other intensity of physical activity may have considerable public health and clinical care implications, e.g. replacing 0.5 h/day sedentary time with VPA may be associated with 8% lower risk of incident diabetes. A recent US study consistently showed that substituting 0.5 h/day sedentary time with moderate-to-vigorous physical activity could decrease 15% risk of diabetes.11 More physical activity would be likely to maximize weight loss, skeletal muscle mass gain, and strength gain and can improve insulin resistance.11 A study from UK Biobank also found that reallocating 20 min/day to MVPA from all other behaviours proportionally was associated with 9% lower risk of cardiovascular disease.46 Similarly, a recent UK Biobank study showed that replacing sedentary time with moderate-to-vigorous activity may reduce risks of depression and anxiety symptoms.47 However, previous study also found inconsistent results that replacing 1 h/day sedentary time with moderate-to-vigorous physical activity was not associated with differences in anxiety symptoms,48 which were accordance with our results about anxiety disorder. Substituting sedentary time with physical activity might be associated with neuropsychiatric symptoms through various mechanisms, such as modulating neuroplasticity, reducing inflammation, and promoting self-esteem.49 Our findings complement the physical activity recommendations that substituting effect of sedentary time with physical activity on the risks of comprehensive NCDs, rather only focusing on separate effects of sedentary time and physical activity. In real life, it is very difficult to achieve 1 h/day VPA for general population. However, our study highlighted that replacing sedentary time with any equivalent amounts of VPA than LPA and MPA was associated with risk reduction of more types of NCDs.
Several limitations of our study need to be considered. First, given the observational study design, the exact conclusions of causality should be made with caution as residual confounding cannot be fully ruled out. Second, sedentary time and physical activity information was subjectively measured, which are known to cause possible measurement bias. Recently, the UK Biobank has objectively measured activity levels using 7-day accelerometers in partly selected participants.50 However, the follow-up time since these accelerometer measurements were collected is too short to evaluate multiple NCDs, and the whole sample was not large enough. Third, sedentary behaviour defined in our study only included television watching, time spent using computers and driving, which were done in leisure time. We did not capture other activities, such as occupational sedentary behaviour, which can be the majority of daily sedentary time for desk-based workers. Therefore, the conclusions cannot be generalized to total sedentary behaviour. Future research efforts should be directed at expanding the current set of analyses to total sedentary time, including accelerometer data. Fourth, we did not include a comprehensive diet behaviour as covariable, which may influence some NCDs incidence. Fifth, the observed interconnectedness between NCDs may not be fully considered, the temporal order of NCDs incidence could yield residual bias. To reduce type I errors, however, all analyses were corrected for multiple testing using Bonferroni's method. Finally, sedentary habits at baseline may have changed during the follow-up, but our results do not account for these changes. Extrapolation of the current findings to a younger population should be subjected to further research.
In conclusion, our findings provide evidence on the detrimental effect of longer sedentary time. We found that more than 6 h/day of sedentary time was associated with increased risk of 12 of the 45 NCDs, statistically independent of physical activity and sleeping. Replacing sedentary time with any equivalent amounts of VPA than LPA and MPA could be associated with risk reduction of more types of NCDs. Recommendations for sedentary time could indicate that any reduction in sedentary behaviour coincides with increasing time spent in healthier alternatives to ensure positive replacement effects. Further studies are needed to investigate causality by an experimental intervention.
Funding
This work was supported by the National Natural Science Foundation of China (91746205, 71910107004).
Data sharing statement
The data that support the findings of this study are available from UK Biobank project site, subject to registration and application process. Further details can be found at https://www.ukbiobank.ac.uk.
Contributors
YGW and ZC conceived the study. ZC and CJX wrote the first and successive drafts of the manuscript. ZC, CJX and PJZ analyzed the data. YGW had full access to the data and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors reviewed the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of interests
The authors declare that they have no competing interests.
Acknowledgements
We thank the participants of the UK Biobank. This research has been conducted using the UK Biobank Resource under the project number of 45676.
Footnotes
Appendix. Supplementary materials
References
- 1.British Heart Foundation . British Heart Foundation; 2021. BHF Cardiovascular Disease Statistics-UK. physical-inactivity-report—mymarathon-final.pdf. Factsheet. https://www.bhf.org.uk/-/media/files/research/heart-statistics/Accessed 26 Jan. [Google Scholar]
- 2.Heron L., O'Neill C., McAneney H., et al. Direct healthcare costs of sedentary behaviour in the UK. J Epidemiol Community Health. 2019;73:625–629. doi: 10.1136/jech-2018-211758. [DOI] [PubMed] [Google Scholar]
- 3.Matthews C.E., Chen K.Y., Freedson P.S., et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ross R., Chaput J.P., Giangregorio L.M., et al. Canadian 24-hour movement guidelines for adults aged 18-64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45:S57–S102. doi: 10.1139/apnm-2020-0467. [DOI] [PubMed] [Google Scholar]
- 5.Saunders T.J., McIsaac T., Douillette K., et al. Sedentary behaviour and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45:S197–S217. doi: 10.1139/apnm-2020-0272. [DOI] [PubMed] [Google Scholar]
- 6.Bull F.C., Al-Ansari S.S., Biddle S., et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekelund U., Brown W.J., Steene-Johannessen J., et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53:886–894. doi: 10.1136/bjsports-2017-098963. [DOI] [PubMed] [Google Scholar]
- 8.Ekelund U., Tarp J., Fagerland M.W., et al. Joint associations of accelero-meter measured physical activity and sedentary time with all-cause mortality: a harmonised meta-analysis in more than 44 000 middle-aged and older individuals. Br J Sports Med. 2020;54:1499–1506. doi: 10.1136/bjsports-2020-103270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilchrist S.C., Howard V.J., Akinyemiju T., et al. Association of sedentary behavior with cancer mortality in middle-aged and older US adults. JAMA Oncol. 2020;6:1210–1217. doi: 10.1001/jamaoncol.2020.2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bellettiere J., LaMonte M.J., Evenson K.R., et al. Sedentary behavior and cardiovascular disease in older women: the Objective Physical Activity and Cardiovascular Health (OPACH) study. Circulation. 2019;139:1036–1046. doi: 10.1161/CIRCULATIONAHA.118.035312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bellettiere J., LaMonte M.J., Healy G.N., et al. Sedentary behavior and diabetes risk among women over the age of 65 years: the OPACH study. Diabetes Care. 2021;44:563–570. doi: 10.2337/dc20-0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yan S., Fu W., Wang C., et al. Association between sedentary behavior and the risk of dementia: a systematic review and meta-analysis. Transl Psychiatry. 2020;10:112. doi: 10.1038/s41398-020-0799-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris J.S., Bradbury K.E., Cross A.J., et al. Physical activity, sedentary behaviour and colorectal cancer risk in the UK Biobank. Br J Cancer. 2018;118:920–929. doi: 10.1038/bjc.2017.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dumuid D., Pedišić Ž., Stanford T.E., et al. The compositional isotemporal substitution model: a method for estimating changes in a health outcome for reallocation of time between sleep, physical activity and sedentary behaviour. Stat Methods Med Res. 2019;28:846–857. doi: 10.1177/0962280217737805. [DOI] [PubMed] [Google Scholar]
- 15.Janssen I., Clarke A.E., Carson V., et al. A systematic review of compositional data analysis studies examining associations between sleep, sedentary behaviour, and physical activity with health outcomes in adults. Appl Physiol Nutr Metab. 2020;45:S248–S257. doi: 10.1139/apnm-2020-0160. [DOI] [PubMed] [Google Scholar]
- 16.Millard L.A.C., Tilling K., Gaunt T.R., et al. Association of physical activity intensity and bout length with mortality: An observational study of 79,503 UK Biobank participants. PLoS Med. 2021;18(9):e1003757. doi: 10.1371/journal.pmed.1003757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sudlow C., Gallacher J., Allen N., et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office for National Statistics . How We Spend Our Time London. Office for National Statistics; 2006. The time use survey, 2005. [Google Scholar]
- 19.Craig C.L., Marshall A.L., Sjöström M., et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 20.Stamatakis E., Rogers K., Ding D., et al. All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. Int J Behav Nutr Phys Act. 2015;12:121. doi: 10.1186/s12966-015-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stamatakis E., Gale J., Bauman A., et al. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol. 2019;73:2062–2072. doi: 10.1016/j.jacc.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 22.Hallgren M., Nguyen T.T., Owen N., et al. Cross-sectional and prospective relationships of passive and mentally active sedentary behaviours and physical activity with depression - CORRIGENDUM. Br J Psychiatry. 2020;217:459. doi: 10.1192/bjp.2019.87. [DOI] [PubMed] [Google Scholar]
- 23.Knuppel A., Papier K., Fensom G.K., et al. Meat intake and cancer risk: prospective analyses in UK Biobank. Int J Epidemiol. 2020;49:1540–1552. doi: 10.1093/ije/dyaa142. [DOI] [PubMed] [Google Scholar]
- 24.Pandey A., Salahuddin U., Garg S., et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease: a meta-analysis. JAMA Cardiol. 2016;1:575–583. doi: 10.1001/jamacardio.2016.1567. [DOI] [PubMed] [Google Scholar]
- 25.Chomistek A.K., Manson J.E., Stefanick M.L., et al. Relationship of sedentary behavior and physical activity to incident cardiovascular disease: results from the Women's Health Initiative. J Am Coll Cardiol. 2013;61:2346–2354. doi: 10.1016/j.jacc.2013.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patterson R., McNamara E., Tainio M., et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedenreich C.M., Ryder-Burbidge C., McNeil J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biologic mechanisms. Mol Oncol. 2020;15(3):790–800. doi: 10.1002/1878-0261.12772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biller V.S., Leitzmann M.F., Sedlmeier A.M., et al. Sedentary behaviour in relation to ovarian cancer risk: a systematic review and meta-analysis. Eur J Epidemiol. 2021;36(8):769–780. doi: 10.1007/s10654-020-00712-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berger F.F., Leitzmann M.F., Hillreiner A., et al. Sedentary behavior and prostate cancer: a systematic review and meta-analysis of prospective cohort studies. Cancer Prev Res. 2019;12:675–687. doi: 10.1158/1940-6207.CAPR-19-0271. [DOI] [PubMed] [Google Scholar]
- 30.Kunzmann A.T., Mallon K.P., Hunter R.F., et al. Physical activity, sedentary behaviour and risk of oesophago-gastric cancer: a prospective cohort study within UK Biobank. United Eur Gastroenterol J. 2018;6:1144–1154. doi: 10.1177/2050640618783558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmid D., Leitzmann M.F. Television viewing and time spent sedentary in relation to cancer risk: a meta-analysis. JNCI J Natl Cancer Inst. 2014;106(7):dju098. doi: 10.1093/jnci/dju098. [DOI] [PubMed] [Google Scholar]
- 32.Kerr J., Anderson C., Lippman S.M. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 2017;18:e457–e471. doi: 10.1016/S1470-2045(17)30411-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maasakkers C.M., Claassen J., Gardiner P.A., et al. The association of sedentary behaviour and cognitive function in people without dementia: a coordinated analysis across five cohort studies from COSMIC. Sports Med. 2020;50:403–413. doi: 10.1007/s40279-019-01186-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang Y.C., Li L.Q., Gan Y., et al. Sedentary behaviors and risk of depression: a meta-analysis of prospective studies. Transl Psychiatry. 2020;10(1):26. doi: 10.1038/s41398-020-0715-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hallgren M., Nguyen T.T.D., Owen N., et al. Associations of interruptions to leisure-time sedentary behaviour with symptoms of depression and anxiety. Transl Psychiatry. 2020;10(1):128. doi: 10.1038/s41398-020-0810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hallgren M., Nguyen T.T.D., Owen N., et al. Associations of sedentary behavior in leisure and occupational contexts with symptoms of depression and anxiety. Prev Med. 2020;133:106021. doi: 10.1016/j.ypmed.2020.106021. [DOI] [PubMed] [Google Scholar]
- 37.Vancampfort D., Firth J., Schuch F.B., et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16:308–315. doi: 10.1002/wps.20458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bueno-Antequera J., Angel Oviedo-Caro M., Munguia-Izquierdo D. Relationship between objectively measured sedentary behavior and health outcomes in schizophrenia patients: the PsychiActive project. Schizophr Res. 2018;197:87–92. doi: 10.1016/j.schres.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 39.Cordova-Rivera L., Gibson P.G., Gardiner P.A., et al. A systematic review of associations of physical activity and sedentary time with asthma outcomes. J Allergy Clin Immunol Pract. 2018;6:1968. doi: 10.1016/j.jaip.2018.02.027. -+ [DOI] [PubMed] [Google Scholar]
- 40.van de Vegte Y.J., Said M.A., Rienstra M., et al. Genome-wide association studies and Mendelian randomization analyses for leisure sedentary behaviours. Nat Commun. 2020;11(1):1770. doi: 10.1038/s41467-020-15553-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bakrania K., Edwardson C.L., Khunti K., et al. Associations between sedentary behaviors and cognitive function: cross-sectional and prospective findings from the UK Biobank. Am J Epidemiol. 2018;187:441–454. doi: 10.1093/aje/kwx273. [DOI] [PubMed] [Google Scholar]
- 42.Prince S.A., LeBlanc A.G., Colley R.C., et al. Measurement of sedentary behaviour in population health surveys: a review and recommendations. PeerJ. 2017;5:e4130. doi: 10.7717/peerj.4130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Benatti F.B., Ried-Larsen M. The effects of breaking up prolonged sitting time: a review of experimental studies. Med Sci Sports Exerc. 2015;47:2053–2061. doi: 10.1249/MSS.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 44.Foster H.M.E., Ho F.K., Sattar N., et al. Understanding how much TV is too much: a nonlinear analysis of the association between television viewing time and adverse health outcomes. Mayo Clin Proc. 2020;95:2429–2441. doi: 10.1016/j.mayocp.2020.04.035. [DOI] [PubMed] [Google Scholar]
- 45.Gilchrist S.C., Howard V.J., Akinyemiju T., et al. Association of sedentary behavior with cancer mortality in middle-aged and older US adults. JAMA Oncol. 2020;6:1210–1217. doi: 10.1001/jamaoncol.2020.2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Walmsley R, Chan S, Smith-Byrne K, et al., Reallocation of time between device-measured movement behaviours and risk of incident cardiovascular disease. Br J Sports Med. 2021, bjsports-2021-104050. 10.1136/bjsports-2021-104050. [DOI] [PMC free article] [PubMed]
- 47.Kandola A.A., Del Pozo Cruz B., Osborn D.P.J., et al. Impact of replacing sedentary behaviour with other movement behaviours on depression and anxiety symptoms: a prospective cohort study in the UK Biobank. BMC Med. 2021;19:133. doi: 10.1186/s12916-021-02007-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kandola A, Lewis G, Osborn DPJ, et al. Device-measured sedentary behaviour and anxiety symptoms during adolescence: a 6-year prospective cohort study. Psychol Med. 2020:1–10. doi: 10.1017/S0033291720004948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kandola A., Ashdown-Franks G., Hendrikse J., et al. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. 2019;107:525–539. doi: 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- 50.Doherty A., Jackson D., Hammerla N., et al. Large scale population assessment of physical activity using wrist worn accelerometers: the UK biobank study. PLoS One. 2017;12(2):e0169649. doi: 10.1371/journal.pone.0169649. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.