Early establishment of a pool of latently infected, resting CD4+ T cells during primary HIV-1 infection (original) (raw)
Abstract
The presence of latently infected, resting CD4+ T cells carrying replication-competent HIV-1 has been demonstrated in chronically infected individuals who are antiretroviral therapy naive as well as in those who are receiving highly active antiretroviral therapy (HAART). It is not clear, however, whether the establishment of a pool of latently infected CD4+ T cells can be blocked by early initiation of HAART after primary infection. The present study demonstrates that initiation of HAART in infected individuals as early as 10 days after the onset of symptoms of primary HIV-1 infection did not prevent generation of latently infected, resting CD4+ T cells carrying integrated HIV-1 DNA as well as infectious HIV-1 despite the successful control of plasma viremia shortly after institution of HAART. Furthermore, there was no correlation between either the duration of HAART at the time of study (range: 0.2–17 months) or the time of initiation of HAART after the onset of symptoms of primary HIV-1 infection (range: 0.3–4 months) and the frequencies of resting CD4+ T cells carrying either integrated HIV-1 DNA or infectious virus. These results underscore the rapidity with which latent reservoirs are established in primary HIV-1 infection and indicate that it is unlikely that early treatment during primary infection can prevent establishment of a pool of latently infected, resting CD4+ T cells as long as treatment is initiated after plasma viremia becomes evident.
Keywords: latency/primary infection/HAART therapy
During primary infection with HIV type 1 (HIV-1), there is intense replication and widespread dissemination of virus and precipitous decline of the level of CD4+ T cells with manifestations of clinical symptoms including fever, lymphadenopathy, pharyngitis, rash, and other clinical findings, often lasting 1–2 weeks (1–7). Despite the fact that there is active viral replication in lymphoid organs of infected individuals in the absence of antiretroviral therapy regardless of the stage of disease (8–10), the peak of plasma viremia during primary infection typically resolves spontaneously with a decrease in levels of circulating virus of up to 2–3 orders of magnitude over a few weeks (3, 11, 12). During primary infection, levels of plasma HIV-1 are generally high (104-108 copies of HIV RNA/ml plasma) (3, 4), and the level of plasma viremia at 4 to 12 months after primary HIV-1 infection is correlated with the risk for more rapid disease progression (7, 13–15). In this regard, early identification and treatment during this stage of infection is believed to be critical to prevent further the spread of virus and deterioration of the immune system.
There is also growing interest in the concept of early treatment during primary HIV-1 infection to block establishment of a pool of latently infected, resting CD4+ T cells. In this regard, Chun et al. (16, 17) have described a stable form of latency in CD4+ T cells that have undergone integration of proviral HIV DNA both in lymph nodes and peripheral blood of infected individuals (16, 17). Furthermore, a small, but detectable, reservoir of latently infected, resting CD4+ T cells recently has been shown to persist in patients receiving highly active antiretroviral therapy (HAART) in whom plasma viremia had fallen to below the level of detectability of commonly used assays (18–20). Despite the fact that HAART successfully can control viral replication and plasma viremia in most chronically infected individuals (21, 22), the presence of residual latently infected, resting CD4+ T cells is of serious concern because these cells serve as a potential source of reactivation of viral replication and remain a major obstacle for eradication of HIV-1 in infected individuals receiving HAART (18–20). Because HIV-1 latency in resting CD4+ T cells is likely established very early in the course of infection when there are high levels of viremia and activated CD4+ T cells, it is critical to assess the possibility of blocking establishment of latency in resting CD4+ T cells by early treatment. The present study addresses this question.
MATERIALS AND METHODS
Patient Population.
Ten subjects were enrolled in the primary HIV-1 infection study at the University of Washington in accordance with an Institutional Review Board-approved protocol. All subjects had a compatible exposure history and detectable plasma HIV-1 viremia. Nine subjects presented with symptoms and one with asymptomatic seroconversion. All subjects were seen within 90 days after onset of symptoms or seroconversion. After informed consent was obtained, patients were treated immediately upon diagnosis with a regimen of HAART consisting of zidovudine (AZT), lamivudine (3TC), and indinavir. These 10 individuals were subjected to apheresis to obtain peripheral blood mononuclear cells (Table 1).
Table 1.
Clinical features of subjects with primary HIV-1 infection treated with zidovudine, lamivudine, and indinavir
| Subject | Initial CD4 count, cells/μl | CD4 count at time of study, cells/μl | Initial plasma HIV RNA, copies/ml* | Plasma HIV RNA at time of study, copies/ml* |
|---|---|---|---|---|
| 1 | 381 | 1,172 | 3,250,000 | 1,034 |
| 2 | 777 | 1,034 | 22,200 | 267 |
| 3 | 641 | 790 | 96,900 | 343 |
| 4 | 680 | 838 | 12,500 | <50 |
| 5 | 257 | 364 | 38,400 | <50 |
| 6 | 927 | 731 | 6,000,000 | 73 |
| 7 | 378 | 743 | 49,100 | <50 |
| 8 | 397 | 567 | 94,300 | <50 |
| 9 | 601 | 590 | 1,017 | 169 |
| 10 | 559 | 842 | 336,689 | <50 |
Isolation of Resting CD4+ T Cells.
Resting CD4+ T cells were isolated from peripheral blood mononuclear cells of HIV-1-infected individuals by using a column-based purification technique (Stem Cell Technologies, Paisley, Scotland). In brief, peripheral blood mononuclear cells from infected individuals were incubated with anti-CD8, CD14, CD16, CD19, CD41, and glycoporin antibodies to enrich for CD4+ T cells and anti-CD25 and anti-HLA-DR antibodies to deplete further activated CD4+ T cells. After 30 min of incubation on ice, magnetic colloids were added to cell–antibody complexes to deplete cells stained with the above antibodies by using a column and a magnet. The purity of cells after column depletion was determined by flow cytometric analysis of purified cells by using fluorescein isothiocyanate-conjugated anti-CD4 and phycoerythrin-conjugated HLA-DR antibodies (Beckton Dickinson).
Assays for Total and Integrated HIV-1 DNA.
To determine the frequency of latently infected, resting CD4+ T cells from infected individuals carrying total and stably integrated HIV-1 provirus, PCR-based assays were carried out as described (18).
Micro-Coculture Assay.
To determine the frequency of latently infected, resting CD4+ T cells from infected individuals carrying replication-competent HIV-1, micro-coculture assays were carried out as described (17).
Statistical Analysis.
Spearman rank correlations were used as a measure of correlation between duration of therapy or time of initiation of HAART after the onset of symptoms of primary HIV-1 infection and the frequencies of cells carrying total and integrated HIV-1 DNA or infectious HIV-1. The Bonferroni method was used to adjust P values for multiple testing.
RESULTS
Effect of HAART on Plasma Viremia in Primary HIV-1 Infection.
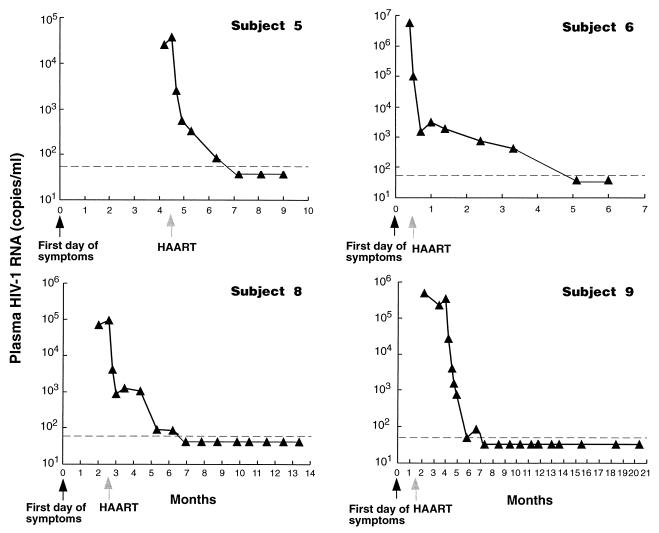
To investigate whether early initiation of HAART during primary HIV-1 infection can prevent establishment of the latent viral reservoir in infected individuals, we examined the size and inducibility of latently infected, resting CD4+ T cells from infected individuals in whom HAART was administered at various times after the onset of symptoms and in whom therapy had been administered for various durations of time. The plasma viral loads of all infected individuals who participated in our study rapidly declined regardless of time elapsed between the first day of symptoms and the initiation of HAART. All 10 patients had excellent virologic responses to HAART. At the time of study, the level of plasma viremia (copies of HIV-1 RNA/ml plasma) in 5 of 10 patients was <50 copies/ml (limit of detectability); in 4 patients, the level of plasma viremia was between 50 and 400 copies/ml; in 1 patient, the level of plasma viremia was ≈1,000 copies/ml. However, in the latter patient, the level of pre-treatment plasma viremia had decreased by more than 3 logs from the initial level (Table 1). Representative time courses for changes in plasma viremia for four of these patients is shown in Fig. 1.
Figure 1.
Time course of changes in plasma HIV-1 RNA after time of infection and initiation of HAART. The zero time point is taken as the day on which infected individuals experienced initial symptoms of HIV-1 infection (black arrows). The time of the initiation of HAART is indicated by gray arrows. The dashed line indicates the limit of detection of the assay (50 copies of HIV-1 RNA/ml plasma).
Detection of Total and Integrated HIV-1 DNA in Resting CD4+ T Cells.
Subjects underwent leukopheresis at varying time points after initiation of HAART. This varied from 0.2 to 17 months (median: 6.8 months). Upon obtaining peripheral blood mononuclear cells of infected individuals, we first isolated resting CD4+ T cells by using a column-based magnetic bead depletion. The purity of resting CD4+ T cells was generally >95%. To determine what fraction of resting CD4+ T cells carry the stable form of HIV-1 DNA, we used a previously described Alu-LTR PCR method. The Alu-LTR PCR was applied to serially diluted genomic DNA from purified resting CD4+ T cells from infected individuals. The integrated form of HIV-1 DNA was detected in all 10 HAART-treated patients. The frequency of resting CD4+ T cells carrying integrated HIV-1 DNA together with the duration of therapy at the time of study and the time of initiation of HAART after the onset of symptoms is shown in Table 2.
Table 2.
Relationship between duration of therapy or time of initiation of HAART and frequency of resting CD4+ T cells carrying integrated HIV-1 DNA after primary HIV-1 infection
| Subject | Duration of therapy at time of study, months | Time of initiation of HAART after onset of symptoms, months | Frequency of resting CD4+ T cells carrying integrated HIV-1 DNA, copies/106 cells* |
|---|---|---|---|
| 1 | 0.2 | 0.3 | 81.7 |
| 2 | 1.6 | 2.8 | 40.5 |
| 3 | 1.7 | 3.4 | 142.8 |
| 4 | 2.6 | 0.7 | 1.6 |
| 5 | 4.7 | 4.4 | 142.8 |
| 6 | 5.2 | 0.5 | 205.8 |
| 7 | 9.3 | 4.4 | 28.3 |
| 8 | 11.0 | 2.6 | 205.8 |
| 9 | 14.6 | 1.4 | 40.5 |
| 10 | 17.0 | 4.0 | 1.6 |
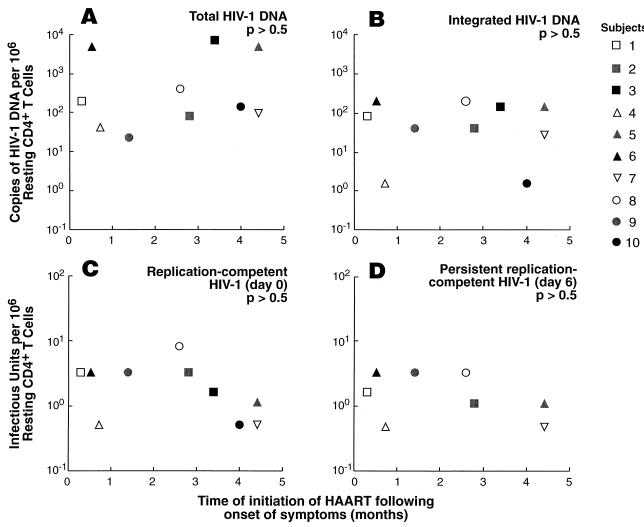
By using Spearman rank correlations, we determined that there was no significant correlation between the number of copies of total HIV-1 DNA per 106 resting CD4+ T cells (P > 0.5) or the number of integrated copies of HIV-1 DNA per 106 resting CD4+ T cells (P > 0.5) and the duration of HAART at the time of study (Fig. 2 A and B). Likewise, there was no significant correlation between these two parameters (P > 0.5 for each) and the time of initiation of HAART after the onset of symptoms of primary HIV-1 infection (Fig. 3 A and B). Of note, measurements of total copy numbers of HIV-1 DNA indicated that levels of unintegrated HIV-1 DNA were higher than integrated HIV-1 DNA in resting CD4+ T cells in 9 of 10 infected individuals (Fig. 2 A and B).
Figure 2.
Frequencies of resting CD4+ T cells carrying various forms of HIV-1 DNA as well as infectious virus in infected individuals who received HAART for varying durations of times after primary infection. Frequencies of resting CD4+ T cells carrying total (A) and integrated (B) HIV-1 DNA are shown. The copy numbers of HIV-1 DNA including both unintegrated and integrated HIV-1 DNA in purified resting CD4+ T cells in infected individuals were calculated as described above. The frequencies of resting CD4+ T cells with integrated HIV-1 DNA were determined by Alu-LTR PCR by using serially diluted genomic DNA from resting CD4+ T cells. Frequencies of resting CD4+ T cells carrying replication-competent HIV-1 DNA were determined by activating purified resting CD4+ T cells on day 0 (C). Frequencies of resting CD4+ T cells carrying persistent, replication-competent HIV-1 DNA were determined by activating 6-day preincubated cells in the absence of activating stimuli (D). For each assay, the statistical method of Myers et al. was used to calculate copy numbers or infectious units per million resting CD4+ T cells (27).
Figure 3.
Frequencies of resting CD4+ T cells carrying various forms of HIV-1 DNA as well as infectious virus in infected individuals in whom HAART was initiated at various times after the onset of symptoms of primary HIV-1 infection. Frequencies of resting CD4+ T cells carrying total (A) and integrated (B) HIV-1 DNA are shown. The copy numbers of HIV-1 DNA including both unintegrated and integrated HIV-1 DNA in purified resting CD4+ T cells in infected individuals were calculated as described above. The frequencies of resting CD4+ T cells with integrated HIV-1 DNA were determined by Alu-LTR PCR by using serially diluted genomic DNA from resting CD4+ T cells. Frequencies of resting CD4+ T cells carrying replication-competent HIV-1 DNA were determined by activating purified resting CD4+ T cells on day 0 (C). Frequencies of resting CD4+ T cells carrying persistent-replication competent HIV-1 DNA were determined by activating 6-day preincubated cells in the absence of activating stimuli (D). For each assay, the statistical method of Myers et al. was used to calculate copy numbers or infectious units per million resting CD4+ T cells (27).
These results demonstrate that early initiation of HAART during primary infection failed to prevent the establishment of a latently infected pool of resting CD4+ T cells carrying integrated HIV-1 DNA. Moreover, the fact that there is a higher frequency of resting CD4+ T cells that carry the unintegrated form than the integrated form of HIV-1 DNA agrees with previous findings (18), suggesting that there is ongoing viral replication despite the fact that plasma viremia is not detected in some infected individuals.
Detection of Replication Competent HIV-1 in Resting CD4+ T Cells.
Because a high proportion of HIV-1 DNA in cells of infected individuals exists as a defective form (17, 23, 24) and only replication-competent HIV-1 provirus can give rise to infectious virus, we carried out a quantitative micro-coculture assay by using purified resting CD4+ T cells to measure directly the frequency of resting CD4+ T cells that are capable of producing infectious virus upon cellular activation. To differentiate between replication-competent unintegrated and integrated HIV-1, purified resting CD4+ T cells were preincubated in the absence of activating stimuli for 6 days to allow for the decay of unintegrated HIV-1 DNA. Serially diluted fresh (day 0) as well as preincubated (day 6) resting CD4+ T cells were activated in vitro in duplicate as described (17), and supernatant from each culture was collected on day 14 for determination of HIV-1 p24 by ELISA. Infectious virus was isolated from stimulated resting CD4+ T cells from 10 of 10 infected individuals regardless of the duration of HAART at the time of study (Fig. 2 C and D) and the time between the onset of symptoms and the initiation of HAART (Fig. 3 C and D).
By using Spearman rank correlations, we determined that there was no significant correlation between the frequency of resting CD4+ T cells carrying HIV-1 on day 0 (P > 0.5) or day 6 (P > 0.5) of culture and the duration of HAART at the time of study (Fig. 2 C and D). Likewise, there was no significant correlation between these two parameters (P > 0.5 for each) and the time of initiation of HAART after the onset of symptoms of primary HIV-1 infection (Fig. 3 C and D).
These data suggest that HAART administered during the early stage of primary infection failed to block the establishment of a pool of latently infected, resting CD4+ T cells carrying replication competent HIV-1. Furthermore, latently infected resting CD4+ T cells carrying replication-competent HIV-1 persist even after a prolonged period of therapy after primary infection as previously suggested (18–20).
DISCUSSION
In the present study, we have examined whether early initiation of HAART during primary HIV-1 infection can prevent the establishment of viral latency in resting CD4+ T cells. Despite recently reported therapeutic successes in suppressing plasma viremia to below detectable levels with HAART (21, 22), it has been shown that replication-competent HIV-1 persists in latently infected, resting CD4+ T cells even after a prolonged period of treatment, and this population of cells represent a major obstacle in attempts to completely eradicate HIV-1 in infected individuals. It is unclear how early in the course of primary HIV-1 infection this pool of latently infected cells is established. Given the fact that high levels of plasma viremia (3, 4, 11, 14) and elevated degrees of CD4+ T cell activation (25) are commonly observed during primary infection, it has been speculated that this is the critical period for the establishment of chronic infection and the pool of latently infected, resting CD4+ T cells, and this is the period that is most amenable to therapeutic intervention for the purposes of preventing the establishment of this pool of latently infected cells. Our findings indicate that initiation of HAART as early as 10 days after the onset of symptoms of primary HIV-1 infection could not prevent formation of a latent reservoir of virus. The initial peak of plasma viremia during primary HIV-1 infection generally resolves spontaneously in most infected individuals within several weeks (3, 11, 12), and most chronically infected individuals carry replication-competent HIV-1 in their resting CD4+ T cells (17, 18). Therefore, the failure of HAART initiated during the chronic phase of infection to block establishment of latently infected, resting CD4+ T cells carrying replication-competent HIV-1 is not surprising. The data from this study indicate that once plasma viremia is present and virus is disseminated to lymphoid organs (26), the pool of latently infected CD4+ T cells is already established. Although initiation of HAART during primary infection may hasten the decrease in virus replication and plasma viremia and may have some long term beneficial effect, if it is initiated after the appearance of high levels of plasma viremia, it apparently does not abort the establishment of the latently infected reservoir. In this regard, although the present study shows no significant correlation between either the duration of HAART at the time of study or the time of initiation of HAART after the onset of symptoms of primary HIV-1 infection and the frequencies of resting CD4+ T cells carrying either integrated HIV-1 DNA or infectious virus, it should be pointed out that the longest duration of therapy among our 10 patients was only 17 months. It is certainly possible that the combination of early initiation of therapy during primary HIV-1 infection and a prolonged period on therapy will result over time in marked decreases and perhaps eradication of the pool of latently infected cells.
Finally, clinical trials aimed at early identification and treatment of individuals recently exposed to HIV and before the appearance of high levels of plasma viremia will be necessary to address whether prevention of the early establishment of the pool of latently infected, resting CD4+ T cells is possible with currently available antiretroviral agents.
Acknowledgments
We thank Denny Lee and Eric Peterson for providing patient laboratory data and Claire Hallahan for her help with statistical analysis. We also thank Drs. Oren Cohen, Mark Dybul, Audrey Kinter, and Mario Ostrowski for helpful discussions and review of the manuscript. This study was partially supported by National Institutes of Health Grants AI-41535 and T32AI-07140, and by a grant from Merck Research Laboratories.
ABBREVIATION
HAART
highly active antiretroviral therapy
References
- 1.Tindall B, Cooper D A. AIDS. 1991;5:1–14. [PubMed] [Google Scholar]
- 2.Busch M P, Eble B E, Khayam-Bashi H, Heilbron D, Murphy E L, Kwok S, Sninsky J, Perkins H A, Vyas G N. N Engl J Med. 1991;325:1–5. doi: 10.1056/NEJM199107043250101. [DOI] [PubMed] [Google Scholar]
- 3.Clark S J, Saag M S, Decker W D, Campbell-Hill S, Roberson J L, Veldkamp P J, Kappes J C, Hahn B H, Shaw G M. N Engl J Med. 1991;324:954–960. doi: 10.1056/NEJM199104043241404. [DOI] [PubMed] [Google Scholar]
- 4.Daar E S, Moudgil T, Meyer R D, Ho D D. N Engl J Med. 1991;324:961–964. doi: 10.1056/NEJM199104043241405. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen C, Lindhardt B O, Jensen B L, Lauritzen E, Gerstoft J, Dickmeiss E, Gaub J, Scheibel E, Karlsmark T. Br Med J. 1989;299:154–157. doi: 10.1136/bmj.299.6692.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinicco A, Fora R, Sciandra M, Lucchini A, Caramello P, Gioannini P. J Acquir Immune Defic Syndr. 1993;6:575–581. [PubMed] [Google Scholar]
- 7.Schacker T W, Hughes J P, Shea T, Coombs R W, Corey L. Ann Intern Med. 1998;128:613–620. doi: 10.7326/0003-4819-128-8-199804150-00001. [DOI] [PubMed] [Google Scholar]
- 8.Pantaleo G, Graziosi C, Butini L, Pizzo P A, Schnittman S M, Kotler D P, Fauci A S. Proc Natl Acad Sci USA. 1991;88:9838–9842. doi: 10.1073/pnas.88.21.9838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pantaleo G, Graziosi C, Demardest J F, Butini L, Montroni M, Fox C H, Orenstein J M, Kotler D P, Fauci A S. Nature (London) 1993;362:355–358. doi: 10.1038/362355a0. [DOI] [PubMed] [Google Scholar]
- 10.Embretson J, Zupancic M, Ribas J L, Burke A, Racz P, Tenner-Racz K, Haase A T. Nature (London) 1993;362:359–362. doi: 10.1038/362359a0. [DOI] [PubMed] [Google Scholar]
- 11.Piatak M, Jr, Saag M S, Yang L C, Clark S J, Kappes J C, Luk K C, Hahn B H, Shaw G M, Lifson J D. Science. 1993;259:1749–1754. doi: 10.1126/science.8096089. [DOI] [PubMed] [Google Scholar]
- 12.Piatak M, Jr, Saag M S, Yang L C, Clark S J, Kappes J C, Luk K C, Hahn B H, Shaw G M, Lifson J D. AIDS. 1993;7:S65–S71. doi: 10.1097/00002030-199311002-00014. [DOI] [PubMed] [Google Scholar]
- 13.Mackewicz C E, Yang L C, Lifson J D, Levy J A. Lancet. 1994;344:1671–1673. doi: 10.1016/s0140-6736(94)90459-6. [DOI] [PubMed] [Google Scholar]
- 14.Mellors J W, Rinaldo C R, Jr, Gupta P, White R M, Todd J A, Kingsley L A. Science. 1996;272:1167–1170. doi: 10.1126/science.272.5265.1167. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien T R, Blattner W A, Waters D, Eyster E, Hilgartner M W, Cohen A R, Luban N, Hatzakis A, Aledort L M, Rosenberg P S, et al. JAMA. 1996;276:105–110. [PubMed] [Google Scholar]
- 16.Chun T W, Finzi D, Margolick J, Chadwick K, Schwartz D, Siliciano R F. Nat Med. 1995;1:1284–1290. doi: 10.1038/nm1295-1284. [DOI] [PubMed] [Google Scholar]
- 17.Chun T W, Carruth L, Finzi D, Shen X, DiGiuseppe J A, Taylor H, Hermankova M, Chadwick K, Margolick J, Quinn T C, et al. Nature (London) 1997;387:183–188. doi: 10.1038/387183a0. [DOI] [PubMed] [Google Scholar]
- 18.Chun T W, Stuyver L, Mizell S B, Ehler L A, Mican J A, Baseler M, Lloyd A L, Nowak M A, Fauci A S. Proc Natl Acad Sci USA. 1997;94:13193–13197. doi: 10.1073/pnas.94.24.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finzi D, Hermankova M, Pierson T, Carruth L M, Buck C, Chaisson R E, Quinn T C, Chadwick K, Margolick J, Brookmeyer R, et al. Science. 1997;278:1295–1300. doi: 10.1126/science.278.5341.1295. [DOI] [PubMed] [Google Scholar]
- 20.Wong J K, Hezareh M, Gunthard H F, Havlir D V, Ignacio C C, Spina C A, Richman D D. Science. 1997;278:1291–1295. doi: 10.1126/science.278.5341.1291. [DOI] [PubMed] [Google Scholar]
- 21.Gulick R M, Mellors J W, Havlir D, Eron J J, Gonzalez C, McMahon D, Richman D D, Valentine F T, Jonas L, Meibohm A, et al. N Engl J Med. 1997;337:734–739. doi: 10.1056/NEJM199709113371102. [DOI] [PubMed] [Google Scholar]
- 22.Hammer S M, Squires K E, Hughes M D, Grimes J M, Demeter L M, Currier J S, Eron J J, Jr, Feinberg J E, Balfour H H, Jr, Deyton L R, et al. N Engl J Med. 1997;337:725–733. doi: 10.1056/NEJM199709113371101. [DOI] [PubMed] [Google Scholar]
- 23.Coffin J M. Science. 1995;267:483–489. doi: 10.1126/science.7824947. [DOI] [PubMed] [Google Scholar]
- 24.Sanchez G, Xu X, Chermann J C, Hirsch I. J Virol. 1997;71:2233–2240. doi: 10.1128/jvi.71.3.2233-2240.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cossarizza A, Ortolani C, Mussini C, Borghi V, Guaraldi G, Mongiardo N, Bellesia E, Franceschini M G, De Rienzo B, Franceschi C. J Infect Dis. 1995;172:105–112. doi: 10.1093/infdis/172.1.105. [DOI] [PubMed] [Google Scholar]
- 26.Pantaleo G, Fauci A S. Annu Rev Immunol. 1995;13:487–512. doi: 10.1146/annurev.iy.13.040195.002415. [DOI] [PubMed] [Google Scholar]
- 27.Myers L E, McQuay L J, Hollinger F B. J Clin Microbiol. 1994;32:732–739. doi: 10.1128/jcm.32.3.732-739.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]