Allergies: MedlinePlus Medical Encyclopedia (original) (raw)
An allergy is an immune response or reaction to substances that are usually not harmful.
Allergies are very common. Both genes and environment play a role. If both your parents have allergies, there is a good chance that you could also have allergies.
The immune system normally protects the body against harmful substances, such as bacteria and viruses. The immune system can also react to foreign substances called allergens. These allergens are usually harmless, and in most people do not cause a problem.
In a person with allergies, the immune response is oversensitive. When it recognizes an allergen, the immune system launches a response. Chemicals such as histamines are released. These chemicals cause allergy symptoms.
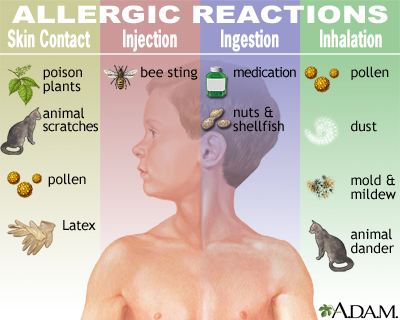
Common allergens include:
- Drugs
- Dust
- Food
- Insect venom
- Mold
- Pet and other animal dander
- Pollen
Some people have allergy-like reactions to hot or cold temperatures, sunlight, or other environmental triggers. Sometimes, friction (rubbing or roughly stroking the skin) will cause symptoms.
Allergies may make certain medical conditions, such as sinus problems, eczema, and asthma, worse.
Mostly, the part of the body the allergen touches determines what symptoms you develop. For example:
- Allergens that you breathe in often cause a stuffy nose, itchy nose and throat, mucus, cough, and wheezing.
- Allergens that touch the eyes may cause itchy, watery, red, swollen eyes.
- Allergens that touch the skin can cause a skin rash, hives, itching, blisters, or skin peeling.
- Medicine allergies and food allergies may involve the whole body and can lead to a variety of symptoms.
At times, an allergy can trigger a response that involves the entire body.

The health care provider will perform a physical exam and ask questions, such as when the allergy symptoms occur.
Allergy testing may be needed to find out whether the symptoms are an actual allergy or are caused by other problems. For example, eating contaminated food (food poisoning) may cause symptoms similar to food allergies. Some medicines (such as aspirin and ampicillin) can produce non-allergic reactions, including rashes. A runny nose or cough may actually be due to an infection.
Skin testing is the most common method of allergy testing:
- The prick test involves placing a small amount of the suspected allergy-causing substances on the skin, and then slightly pricking the area so the substance goes under the skin. The skin is closely watched for signs of a reaction, which include swelling and redness.
- The intradermal test involves injecting a tiny amount of allergen under your skin, then watching the skin for a reaction.
- Both the prick and intradermal tests are read 15 minutes after application of the test.
- The patch test involves placing a patch with the suspected allergen on your skin. The skin is then closely watched for signs of a reaction. This test is used to determine contact allergy. It is usually read 48 to 72 hours after application of the test.
The provider may also check your reaction to physical triggers by applying heat, cold, or other stimulation to your body and watching for an allergic response.
Blood tests that may be done include:
- Immunoglobulin E (IgE), which measures levels of allergy-related substances
- Complete blood count (CBC) during which an eosinophil white blood cell count is done
In some cases, the provider may tell you to avoid certain items to see if you get better, or to use suspected items to see if you feel worse. This is called "use or elimination testing." This is often used to check for food or medicine allergies.
Severe allergic reactions (anaphylaxis) need to be treated with a medicine called epinephrine. It can be life-saving when given right away. If you use epinephrine, call 911 or the local emergency number and go straight to the hospital.
The best way to reduce symptoms is to avoid what causes your allergies. This is especially important for food and medicine allergies.
There are several types of medicines to prevent and treat allergies. Which medicine your provider recommends depends on the type and severity of your symptoms, your age, and overall health.
Illnesses that are caused by allergies (such as asthma, hay fever, and eczema) may need other treatments.
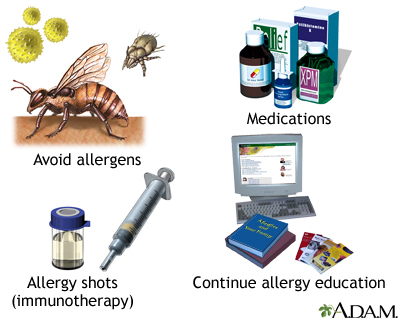
Medicines that can be used to treat allergies include:
ANTIHISTAMINES
Antihistamines are available over-the-counter and by prescription. They are available in many forms, including:
- Capsules and pills
- Eye drops
- Injection
- Liquid
- Nasal spray
CORTICOSTEROIDS
These are anti-inflammatory medicines. They are available in many forms, including:
- Creams, lotions, and ointment for the skin
- Eye drops
- Nasal spray
- Lung inhaler
- Pills
- Injection
People with severe allergic symptoms may be prescribed corticosteroid pills or injections for short periods.
DECONGESTANTS
Decongestants help relieve a stuffy nose. Do not use decongestant nasal spray for more than several days because they can cause a rebound effect and make the congestion worse. Decongestants in pill form do not cause this problem. People with high blood pressure, heart problems, or prostate enlargement should use decongestants with caution.
OTHER MEDICINES
Leukotriene inhibitors are medicines that block the substances that trigger allergies. People with asthma and indoor and outdoor allergies may be prescribed these medicines.
ALLERGY SHOTS
Allergy shots (immunotherapy) are sometimes recommended if you cannot avoid the allergen and your symptoms are hard to control. Allergy shots keep your body from over-reacting to the allergen. You will get regular injections of the allergen. Each dose is slightly larger than the last dose until a maximum dose is reached. Allergy shots are only used for environmental allergies (pollens, pet dander, dust) or venom allergies. These shots do not work for everybody and you will have to visit the provider often.
SUBLINGUAL IMMUNOTHERAPY TREATMENT (SLIT)
Instead of shots, medicine put under the tongue may help for grass, ragweed, and dust mite allergies.
ORAL IMMUNOTHERAPY (OIT)
For people with peanut allergy, oral immunotherapy may be an option. This treatment involves eating tiny amounts of peanut powder and slowly increasing the dose over time until they are eating the equivalent of about 1 peanut every day. OIT is a treatment rather than a cure of food allergy and there is a risk of allergic reaction with the dosing of the peanut powder. This requires a significant commitment of time for visits to the provider and dosing at home.
XOLAIR:
Xolair (omalizumab) is a medication that was recently approved for the treatment of food allergies. Xolair does not cure food allergies but can decrease a person’s likelihood of reacting to a tiny amount of their food allergen. Xolair is an injection that is given either once a month or every 2 weeks, depending on the results of a blood test. People can be allergic to Xolair and there may be an increased risk of certain cancers or heart issues in people taking Xolair. Talk to your provider about Xolair if you have food allergies.
Most allergies can be easily treated with medicine.
Some children may outgrow an allergy, especially food allergies. But once a substance has triggered an allergic reaction, it usually continues to affect the person.
Allergy shots are most effective when used to treat hay fever and insect sting allergies. They are not used to treat food allergies because of the danger of a severe reaction.
Allergy shots may need years of treatment, but they work in most cases. However, they may cause uncomfortable side effects (such as hives and rash) and dangerous outcomes (such as anaphylaxis). Talk with your provider whether allergy drops (SLIT) are right for you.
Treatments for food allergies are evolving quickly. Speak with your provider about different food allergy treatments available.
Complications that may result from allergies or their treatment include:
- Anaphylaxis (life-threatening allergic reaction)
- Breathing problems and discomfort during the allergic reaction
- Drowsiness and other side effects of medicines
Contact your provider for an appointment if:
- Severe symptoms of allergy occur
- Treatment for allergies no longer works
Breastfeeding may help prevent certain food allergies when you feed babies this way only for 4 to 6 months. However, changing a mother's diet during pregnancy or while breastfeeding does not seem to help prevent allergies.
For most children, changing the diet or using special formulas does not seem to prevent allergies. If a parent, brother, sister, or other family member has a history of eczema and allergies, discuss feeding with your child's doctor. Infants with eczema or food allergy often benefit from early introduction (before 12 months of life) of peanuts and/or eggs. Discuss with your child’s provider if this is something that you should do.
There is also evidence that being exposed to certain allergens (such as dust mites and cat dander) in the first year of life may prevent some allergies. This is called the "hygiene hypothesis." It came from the observation that infants on farms tend to have fewer allergies than those who grow up in more sterile environments. However, older children do not seem to benefit.
Once allergies have developed, treating the allergies and carefully avoiding allergy triggers can prevent reactions in the future.
Allergy - allergies; Allergy - allergens
Chiriac AM, Bousquet J, Demoly P. In vivo methods for the study and diagnosis of allergy. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 67.
Custovic A, Tovey E. Allergen control for prevention and management of allergic diseases. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 84.
Nadeau KC. Approach to the patient with allergic or immunologic disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 230.
Wallace DV, Dykewicz MS, Oppenheimer J, Portnoy JM, Lang DM. Pharmacologic treatment of seasonal allergic rhinitis: synopsis of guidance from the 2017 Joint Task Force on Practice Parameters. Ann Intern Med. 2017;167(12):876-881. PMID: 29181536 pubmed.ncbi.nlm.nih.gov/29181536/.
Wise SK, Damask C, Greenhawt M, et al. A synopsis of guidance for allergic rhinitis diagnosis and management from ICAR 2023. J Allerg Clin Immun Pactice. 2023;11(3):773-796.PMID: 36894277. pubmed.ncbi.nlm.nih.gov/36894277/.
Updated by: Deborah Pedersen, MD, MS, Allergy & Asthma Care, PC, Taunton, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.