Infection of Dendritic Cells (DCs), Not DC-SIGN-Mediated Internalization of Human Immunodeficiency Virus, Is Required for Long-Term Transfer of Virus to T Cells (original) (raw)
Abstract
The C-type lectin DC-SIGN expressed on immature dendritic cells (DCs) captures human immunodeficiency virus (HIV) particles and enhances the infection of CD4+ T cells. This process, known as _trans_-enhancement of T-cell infection, has been related to HIV endocytosis. It has been proposed that DC-SIGN targets HIV to a nondegradative compartment within DCs and DC-SIGN-expressing cells, allowing incoming virus to persist for several days before infecting target cells. In this study, we provide several lines of evidence suggesting that intracellular storage of intact virions does not contribute to HIV transmission. We show that endocytosis-defective DC-SIGN molecules enhance T-cell infection as efficiently as their wild-type counterparts, indicating that DC-SIGN-mediated HIV internalization is dispensable for _trans_-enhancement. Furthermore, using immature DCs that are genetically resistant to infection, we demonstrate that several days after viral uptake, HIV transfer from DCs to T cells requires viral fusion and occurs exclusively through DC infection and transmission of newly synthesized viral particles. Importantly, our results suggest that DC-SIGN participates in this process by cooperating with the HIV entry receptors to facilitate _cis_-infection of immature DCs and subsequent viral transfer to T cells. We suggest that such a mechanism, rather than intracellular storage of incoming virus, accounts for the long-term transfer of HIV to CD4+ T cells and may contribute to the spread of infection by DCs.
Immature dendritic cells (DCs) residing in the genital tract are considered to play an important role during the early steps of human immunodeficiency virus (HIV) dissemination after sexual transmission (10, 30). The normal function of DCs is to scavenge and internalize pathogens before migrating to the lymph nodes, where they present processed antigens to resting T cells, initiating an adaptive immune response (21). HIV is believed to hijack the physiological functions of immature DCs to gain access to the CD4+ T-cell compartment in the lymphoid tissues (7, 35). Contact between DCs and CD4+ T cells promotes highly efficient viral transfer, which results in boosted HIV replication and extensive spread of infection (24, 27).
The C-type (calcium-dependent) lectin DC-SIGN (CD209), expressed on certain DC subsets located in mucosal tissues, plays a central role in HIV transmission from DCs to T cells (7, 35). DC-SIGN binds the HIV glycoprotein gp120 with a high affinity and transmits virions to T cells in trans (3, 7, 35). Immature DCs and DC-SIGN-expressing cell lines exposed to small amounts of HIV particles promote more efficient infection of activated T cells than that by free virus (7, 35). This process, known as _trans_-enhancement of T-cell infection, relies on the capacity of DC-SIGN to capture and transfer input virus to T cells without the need for viral replication within DCs or DC-SIGN transfectants (7, 35). In addition, it has been reported that HIV particles captured by DC-SIGN-expressing cells are remarkably stable and remain infectious for several days (7, 35). Indeed, it has been shown that DC-SIGN-expressing cells pulsed with HIV particles and cultured for 4 days are still able to efficiently infect target cells, whereas cell-free virus rapidly loses its infectivity (7, 35).
The molecular mechanisms by which DC-SIGN and DCs transmit HIV infection to T cells are poorly understood. The abilities of DC-SIGN to enhance T-cell infection and to preserve viral infectivity for prolonged periods have been related to the internalization of virus (13). It has been suggested that the internalization signals in the DC-SIGN cytoplasmic tail target intact HIV particles to low-pH nonlysosomal compartments within immature DCs and DC-SIGN-expressing cells (13). Indeed, DC-SIGN mutants carrying a large deletion of the cytoplasmic tail which eliminates the two putative internalization motifs (a dileucine [LL] and a tyrosine-based motif, YXXL) and a triacidic cluster (EEE) are deficient in endocytosis and cannot enhance T-cell infection or retain viral infectivity (13). Furthermore, neutralization of the intracellular pH by concanamycin A has been shown to abrogate _trans_-enhancement of T-cell infection (13). Together, these observations resulted in the proposal of DCs as a “Trojan horse” that facilitates HIV dissemination. In this model, HIV uses DC-SIGN to gain access to a nondegradative intracellular endosome, allowing the virus to persist for a sufficiently long time to be transported from mucosal surfaces to the T-cell compartment in lymphoid tissues (13).
Upon interaction with CD4+ T lymphocytes, internalized virus is thought to recycle back to the DC-T-cell interface and efficiently infect target cells (13). However, the concept of prolonged intracellular storage of incoming virus within DCs is at odds with certain observations. Firstly, several studies indicate that HIV is rapidly degraded following uptake into DCs and DC-SIGN-expressing cell lines (22). Secondly, it has been shown that virus transfer from DC-SIGN-expressing cells to T cells occurs efficiently in the presence of drugs such as bafilomycin A1 or concanamycin, which raise the intracellular pH (23). Finally, recent studies indicate that productive infection of DCs contributes to long-term transfer of virus from DCs to T cells (16). Indeed, HIV transmission is inhibited when DCs are treated with the reverse transcriptase inhibitor zidovudine and cultured for several days prior to adding T cells (16, 34). Thus, the molecular mechanisms by which DCs mediate the transmission of HIV infection to T cells and the contribution of DC-SIGN-mediated internalization to this process are not yet fully understood.
In this study, we provide several lines of evidence that exclude any significant role of stored incoming viral particles in HIV transmission to T cells. We show that DC-SIGN-mediated HIV internalization is dispensable for both _trans_-enhancement of T-cell infection and retention of viral infectivity. Moreover, we formally demonstrate that long-term transfer of HIV to T cells occurs exclusively through DC infection and transmission of viral progeny. We show that DC-SIGN mediates _cis_-infection of DCs and suggest that such a mechanism accounts for the long-term transfer of HIV to T cells and may contribute to the spread of infection by DCs.
MATERIALS AND METHODS
Cell culture.
All products used for cell culture were obtained from Invitrogen. Raji cells and 293T cells were maintained in RPMI and Dulbecco's modified Eagle's medium, respectively, supplemented with 10% fetal calf serum, 2 mM l-glutamine, and antibiotics (100 μg/ml streptomycin and 100 U/ml penicillin). Human peripheral blood mononuclear cells (PBMC) were isolated from healthy donors by using Ficoll Paque Plus (Amersham Biosciences) gradients. Activated T cells were generated by stimulation of PBMC with phytohemagglutinin A (3 μg/ml; Murex) and interleukin-2 (IL-2) (10 U/ml; Chiron) for 3 days. Monocyte-derived immature DCs were generated as previously described (17). Briefly, human PBMC were isolated from healthy donors. Monocytes were negatively selected with biotin-antibody cocktail microbeads (Miltenyi Biotec) and seeded at 106 cells/ml in RPMI supplemented with 10% fetal calf serum, penicillin-streptomycin, 50 ng/ml of recombinant human IL-4 (PeproTech), and 800 U/ml of recombinant human granulocyte-macrophage colony-stimulating factor (GM-CSF; Gentaur) for 6 days. The purity of DCs was confirmed by flow cytometry. Immature DCs were CD3 and CD14 negative and expressed high levels of DC-SIGN and CD1a. In some experiments, monocytes from individuals carrying a homozygous 32-bp deletion in the ccr5 gene (Δ32/Δ32) (28) were isolated and differentiated into immature DCs as described above.
Antibodies and reagents.
The anti-DC-SIGN monoclonal antibody (MAb) clones 1B10 (immunoglobulin G2a [IgG2a]) and 8A5 (IgG2a) have been described previously (9, 17, 25). Phycoerythrin (PE)-conjugated mouse anti-DC-SIGN FAB161P was purchased from R&D Systems. Anti-CXCR4-PE and anti-CCR5-PE MAbs were purchased from Pharmingen. T20 was obtained from the NIH AIDS Research and Reference Reagent Program.
DC-SIGN constructs.
The DC-SIGN wild-type (WT) pcDNA3 vector (Invitrogen) was described previously (9). All DC-SIGN mutants were constructed by site-directed mutagenesis (QuikChange kit; Stratagene) and inserted into the pCDNA vector (17). TRIP ΔU3-CMV vectors (38) (a gift from P. Charneau, Institut Pasteur, Paris, France) encoding DC-SIGN cDNAs were generated by replacing the BamHI-XhoI fragment encoding enhanced green fluorescent protein with a PCR-generated BamHI-SalI fragment encoding either WT DC-SIGN, DC-SIGN LL, DC-SIGN EEE, DC-SIGN Y, DC-SIGN LL/EEE/Y, or DC-SIGN ΔN. All constructs were verified by sequencing.
Flow cytometry assays.
Cells were stained with PE-conjugated anti-DC-SIGN (FAB161P), anti-CXCR4, anti-CCR5, or a PE-isotype control MAb for 30 min at 4°C. Cells were washed and fixed with paraformaldehyde (3.2%) prior to fluorescence-activated cell sorting (FACS) analysis and data processing with CellQuest software (BD Biosciences).
Lentiviral transduction.
Raji cells expressing DC-SIGN or its mutants were generated by transduction with the retroviral TRIP ΔU3 vector expressing DC-SIGN as previously described (17). Transduced cells were stained with PE-conjugated anti-DC-SIGN MAb and sorted for high DC-SIGN expression.
Expression of 35S-radiolabeled gp120 and DC-SIGN binding assays.
The pSFV140BX08 plasmid was used as a template to generate a recombinant Semliki Forest virus (SFV) carrying HIV gp120 (31). The sequence coding for gp120 was amplified by PCR, using the sense primer 5′-ATATTGCGCGCATGAAAGTGAAGGAGACC-3′ and the antisense primer 5′-ATATTGGGCCCTCAGGCGGGGGCCACCTGGGAGGTCTCGGTGCCGGTGGGTGCTATTCCTAATGG-3′, which contains the 1D4 tag peptide sequence. The amplified sequence coding for gp120 was digested with BssHII and ApaI and introduced into corresponding sites in the pSFV vector. Soluble HIV gp120 was produced in SFV vector-infected baby hamster kidney (BHK) cells as described previously (17, 18, 31). At 6 h postinfection, the medium was replaced with methionine-cysteine- and serum-free Dulbecco's modified Eagle's medium (ICN Biomedicals) for 1 h. Synthesis of soluble proteins was continued for up to 24 h postinfection in the presence of 200 μCi/ml [35S]cysteine-methionine (Pro-Mix35S; Amersham Biosciences). Supernatants were clarified and concentrated in a 30-kDa concentration column (Biomax; Millipore). For DC-SIGN binding assays, Raji and DC-SIGN-expressing Raji cells (5 × 105 cells) were incubated for 2 h at 4°C with [35S]gp120 (25 nM) in binding buffer (RPMI with 1 mM CaCl2 and 2 mM MgCl2). After being washed, the cells were shifted to 37°C for 30 min. To quantify gp120 endocytosis, cells were treated with 200 μl RPMI containing 20 mM EDTA in order to remove gp120 bound to DC-SIGN at the cell surface (17). Cells were washed and resuspended in binding buffer prior to the addition of Optiphase Supermix solution (Wallac). 35S activity was counted in a 1450 Microbeta Trilux counter (Wallac).
HIV strains.
JR-CSF Luc (a gift from V. Planelles, Rochester, New York) is an HIV type 1 (HIV-1) provirus that carries the firefly luciferase reporter gene (luc) in place of HIV-1 nef. Replication-competent HIV strains were generated by calcium phosphate-mediated transfection of 293T cells as previously described (1). Virus concentrations were determined by a p24 Gag-specific enzyme-linked immunosorbent assay (ELISA; Perkin-Elmer). Viruses were titrated by infecting GHOST CD4/CXCR4/CCR5 cells (a gift from D. R. Littman, Skirball Institute, New York). Single-cycle pseudotyped HIV particles were generated as described above by cotransfection of HIV-1 NL ΔEnv Luc (a gift from D. R. Littman, Skirball Institute, New York) and a cDNA plasmid encoding the X4 isolate HXB2 envelope or the R5 BaL envelope (a gift from D. R. Littman, Skirball Institute, New York) (4). For real-time PCR experiments, HIV NL43 (X4 strain) was produced in MT4 cells and titrated as described above. NLAD8 (R5 HIV strain) was a gift from O. Schwartz (Pasteur Institute, Paris, France).
HIV-1 transmission assays.
Raji-DC-SIGN cells or immature DCs (1 × 105 cells) were incubated with HIV particles for 2 h at 37°C. For capture assays, cells were washed extensively with phosphate-buffered saline (PBS) and cocultured with an equal number of 293T cells expressing CD4 and CCR5. For enhancement experiments, virus-pulsed cells were directly added to activated PBMC (1 × 105 cells). HIV transmission was evaluated by measuring luciferase activity in the coculture at 3 days postinfection, using a luciferase reporter assay kit (Promega) and a Victor luminometer (Perkin-Elmer). For transmission experiments performed with wild-type virus, aliquots of coculture supernatant were taken at the indicated time points and quantified for p24 Gag content by ELISA. For retention experiments, activated T cells were added 3 days after pulsing of DCs or Raji-DC-SIGN cells with virus. When indicated, immature DCs were preincubated with anti-DC-SIGN MAb 1B10, an isotype control MAb (25 μg/ml), or T20 (1 μM).
Immunofluorescence microscopy.
Raji or Raji-DC-SIGN cells (3 × 105 cells) were incubated for 1 h at 4°C with the anti-DC-SIGN MAb 8A5 (20 μg/ml in RPMI containing 0.2% bovine serum albumin). Cells were washed twice and either incubated at 37°C for 30 min or maintained at 4°C before being fixed with 4% paraformaldehyde for 20 min at room temperature. Fixed cells were adhered to polylysine-coated coverslips (50 μg/ml) overnight at 4°C. Coverslips were washed once with PBS, treated with 0.2 M glycine in PBS for 10 min, and permeabilized with 0.05% saponin in PBS containing 0.2% bovine serum albumin. To visualize DC-SIGN-bound 8A5, cells were incubated with fluorescein isothiocyanate-coupled goat anti-mouse IgG (1/150; Vector Laboratories). Cells were washed and mounted in Vectashield medium containing 4′,6′-diamidino-2-phenylindole (Vector Laboratories) and imaged with a TCS4D confocal microscope (Leica).
Quantification of HIV-1 DNA by real-time PCR.
Quantification of HIV DNA formed after the second template switch (referred to as late viral DNA) was performed as described previously (19). DNA was extracted using a DNeasy kit (QIAGEN), and equal amounts of DNA (40 ng) were analyzed by R-Gag PCR with the following primers: the sense primer M667 (5′-CTAACTAGGGAACCCACTG) and the antisense primer M661B (5′-TCCTGCGTCGAGAGATCTC). The results were normalized to β-globin copy numbers.
RESULTS
Enhancement of T-cell infection and retention of viral infectivity do not require DC-SIGN-mediated HIV internalization.
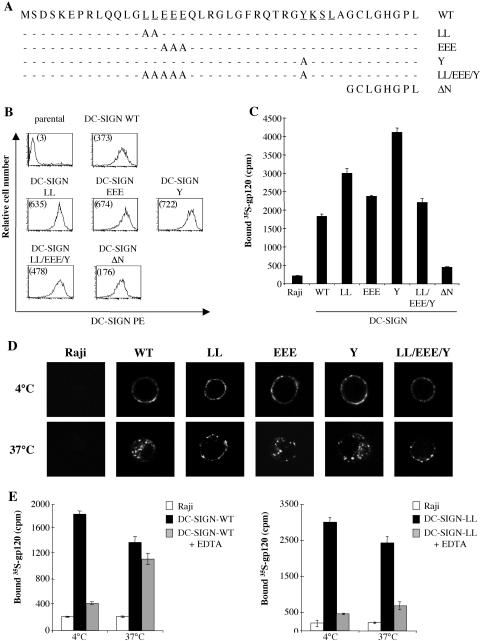
To investigate the specific role of each DC-SIGN internalization motif in HIV transmission, we generated DC-SIGN molecules in which the LL, YSKL, and EEE sequences were replaced by alanine, individually or together (Fig. 1A). Raji cells were transduced with lentiviral vectors encoding these mutated DC-SIGN molecules, and cells were sorted to obtain populations expressing DC-SIGN at levels higher than that of Raji DC-SIGN WT (Fig. 1B). As a control, we also generated a DC-SIGN ΔN mutant lacking the first 35 amino acids of the cytoplasmic domain (Fig. 1A). Cell surface expression levels of DC-SIGN ΔN were found to be significantly lower than that of DC-SIGN WT even after several rounds of transduction and cell sorting (Fig. 1B). All the alanine substitution DC-SIGN mutants (LL, EEE, Y, and LL/EEE/Y) were able to bind 35S-labeled gp120 at least as efficiently as WT DC-SIGN, in correlation with DC-SIGN expression levels (Fig. 1C). Similar results were obtained for binding of whole virus particles (data not shown). In contrast, we observed that the deletion mutant DC-SIGN ΔN poorly captures soluble gp120 (Fig. 1C). This is likely due to the reduced cell surface expression levels of DC-SIGN ΔN since we observed that the Kd of this truncated receptor for HIV gp120 was comparable to that of DC-SIGN WT and the alanine substitution mutants (data not shown). Consistent with this, Raji DC-SIGN WT cells sorted to give the same expression level as DC-SIGN ΔN captured similarly low levels of gp120 and whole HIV particles to those of DC-SIGN ΔN (data not shown).
FIG. 1.
Characterization of WT and mutant DC-SIGN proteins. (A) Schematic representation of mutations introduced into the DC-SIGN cytoplasmic tail. The dileucine (LL) motif, tyrosine-based (YSKL) motif, and triacidic cluster (EEE) are underlined. (B) FACS analysis of Raji cells expressing either WT or mutated forms of DC-SIGN. The mean fluorescence intensities are indicated in parentheses. (C) HIV gp120 binding. [35S]gp120 (25 nM) was incubated for 1 h at 4°C with Raji and Raji-DC-SIGN cells. Cells were washed four times before measurements of cell-associated radioactivity. (D) Subcellular localization of WT and mutant DC-SIGN. Anti-DC-SIGN MAb 8A5 was incubated with Raji or Raji-DC-SIGN WT cells or LL, Y, or EEE mutant cells for 1 h at 4°C. Cells were washed to eliminate unbound antibody and incubated for 30 min at either 4°C or 37°C. DC-SIGN-bound 8A5 was detected with a fluorescein isothiocyanate-conjugated secondary Ab. (E) DC-SIGN-mediated gp120 internalization. 35S-labeled gp120 was bound to Raji, Raji-DC-SIGN WT (left panel), or Raji-DC-SIGN LL mutant (right panel) cells for 1 h at 4°C. Cells were extensively washed and incubated for 30 min at either 4°C or 37°C. Cells were treated with EDTA or mock treated to distinguish internalized from cell surface-bound gp120. Cells were then washed three times before measurements of cell-associated radioactivity.
To characterize the internalization and subcellular localization of WT and mutant DC-SIGN, Raji cells were pulsed with the anti-DC-SIGN MAb 8A5 at 4°C, washed, and then either shifted to 37°C for 30 min to allow endocytosis or kept on ice. Cells were fixed and stained with a fluorescently labeled secondary antibody. Confocal microscopy showed that WT DC-SIGN and the EEE and Y mutants were efficiently internalized upon antibody-induced DC-SIGN endocytosis, while the DC-SIGN LL and LL/EEE/Y mutants remained predominantly at the cell surface (Fig. 1D). These data confirm our observations and those of others indicating that the LL motif is required for efficient DC-SIGN endocytosis and intracellular trafficking (5, 17, 29). To compare the abilities of WT DC-SIGN and the LL mutant to promote HIV gp120 endocytosis, Raji-DC-SIGN cells were incubated on ice with 35S-labeled gp120, washed to remove unbound material, and maintained on ice or shifted to 37°C for 30 min. Cells were then treated with PBS containing EDTA for 10 min to distinguish internalized protein from glycoprotein bound to DC-SIGN at the cell surface, as we have previously described (17). For Raji-DC-SIGN WT cells, we found that >90% of the gp120 bound to DC-SIGN was eliminated by EDTA washing when cells were maintained at 4°C. After incubation for 30 min at 37°C, we observed that a large fraction of gp120 protein was resistant to EDTA treatment, indicating that it had been internalized (Fig. 1E, left panel). In contrast, we observed that EDTA treatment of Raji-DC-SIGN LL cells removed gp120 after binding at both 4°C and 37°C, suggesting that DC-SIGN molecules mutated in the LL motif are unable to promote gp120 internalization (Fig. 1E, right panel). Similar results were obtained with the DC-SIGN LL/EEE/Y mutant (data not shown).
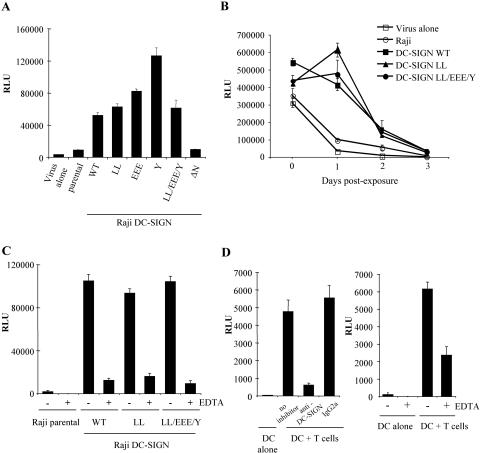
We then investigated the capacity of each DC-SIGN mutant to enhance T-cell infection. To rule out the possibility that transfer of infectivity is dependent on infection of DC-SIGN-expressing Raji cells, all subsequent experiments were carried out using the R5 JR-CSF Luc reporter virus that does not replicate in these cells. Parental Raji or Raji-DC-SIGN cells were incubated at a low multiplicity of infection (MOI) with JR-CSF Luc for 2 h and cocultured with activated T cells. As a control, T cells were also directly infected with the same quantity of virus in the absence of Raji cells. We observed that the endocytosis-defective DC-SIGN LL and DC-SIGN LL/EEE/Y mutants enhanced T-cell infection as efficiently as WT DC-SIGN and the EEE and Y mutants (Fig. 2A). In contrast, the DC-SIGN ΔN mutant poorly enhanced infection in comparison to virus alone or to parental Raji cells (Fig. 2A). Similar results were obtained when Raji and Raji-DC-SIGN cells were pulsed with R5 BaL Luc pseudotyped viruses (data not shown).
FIG. 2.
DC-SIGN-mediated enhancement of T-cell infection does not require DC-SIGN internalization. (A) Enhancement of T-cell infection. Raji or Raji-DC-SIGN cells were incubated with JR-CSF Luc at a low MOI (0.1) for 2 h at 37°C and cocultured with activated T cells. Viral replication was assessed by measuring luciferase activities in cell lysates at 3 days postinfection. As a control, activated T cells were incubated with virus alone. RLU, relative light units. (B) Retention of viral infectivity. Raji and DC-SIGN-expressing cells were pulsed with JR-CSF (MOI, 0.1) at 37°C, and aliquots of cells were added daily to 293T cells expressing CD4 and CCR5. Luciferase activities were determined 3 days later. (C) Raji and Raji-DC-SIGN cells were incubated with JR-CSF Luc (MOI, 0.1) for 3 h at 37°C. Cells were treated for 10 min with 20 mM EDTA to remove virus bound to DC-SIGN at the cell surface or were mock treated with PBS. After being washed extensively, cells were cocultured with 293T cells expressing CD4 and CCR5, and luciferase activities were determined 3 days later. (D) (Left panel) Immature DCs were pulsed with HIV Luc pseudotyped with the HXB2 envelope (10 ng of p24) for 2 hours at 37°C. Cells were treated with 20 mM EDTA for 10 min or mock treated with PBS, washed extensively, and cocultured with activated T cells for 3 days before determining the luciferase activity. (Right panel) DCs were pretreated with anti-DC-SIGN MAb (20 μg/ml) or an isotype control (20 μg/ml) for 20 min, washed extensively, and pulsed with HIV Luc pseudotyped with the HXB2 envelope (10 ng of p24) for 2 hours at 37°C. Cells were washed and cocultured with activated T cells for 3 days before determining the luciferase activity. Data are representative of three independent experiments, and values are given as means of triplicates ± standard deviations.
We then investigated whether DC-SIGN endocytosis is required to retain HIV particles in an infectious form for several days. Raji and Raji-DC-SIGN cells were pulsed with JR-CSF at 37°C, and aliquots of cells were added daily to 293T cells expressing CD4 and CCR5. After 1 day of culture, virus bound to WT DC-SIGN and the LL and LL/EEE/Y mutants all retained infectivity, in contrast to virus alone or pulsed with parental Raji cells (Fig. 2B). However, we observed that the ability of both WT and mutated DC-SIGN molecules to preserve viral infectivity dramatically decreased after 2 days of culture and was completely lost by day 3 (Fig. 2B).
To determine whether _trans_-enhancement of T-cell infection relies on HIV particles presented by DC-SIGN at the cell surface, parental, Raji DC-SIGN WT, and LL and LL/EEE/Y mutant cells were pulsed with JR-CSF virus for 2 hours at 37°C to allow endocytosis. Cells were treated with PBS containing EDTA for 10 min to remove cell surface-bound virus, washed extensively, and cocultured with activated T cells (Fig. 2C). Control experiments were also performed in which Raji-DC-SIGN cells were treated with EDTA for 10 min prior to adding virus. Under these conditions, the capacity of DC-SIGN to enhance T-cell infection was not affected, indicating that there are no adverse effects of EDTA treatment on cellular processes or cell-cell contact (data not shown). We found that EDTA treatment abrogates HIV transfer mediated by WT or mutated DC-SIGN molecules, suggesting that in Raji cells expressing DC-SIGN, cell surface-bound viruses, rather than internalized particles, are transmitted to target cells (Fig. 2C).
We next extended our studies to investigate the role of cell surface-bound virus in transfer from primary immature DCs to T cells. We first verified that pretreatment of DCs with a neutralizing anti-DC-SIGN MAb significantly blocks transfer of HXB2 Luc pseudotyped viruses to T cells, indicating that DC-SIGN is the major cell surface protein involved in viral transmission (Fig. 2D, left panel). We observed that when DCs were pulsed with X4 HXB2 Luc pseudotyped viruses and then treated with EDTA, luciferase activities in DC-T-cell cocultures were reduced but not completely abrogated (Fig. 2D, right panel). This suggests that in contrast to Raji-DC-SIGN cells, in immature DCs both DC-SIGN-bound virus at the cell surface and internalized particles are transferred to target cells shortly after viral exposure.
Prolonged transfer of HIV from immature DCs to T cells occurs exclusively through a coreceptor-mediated DC infection pathway.
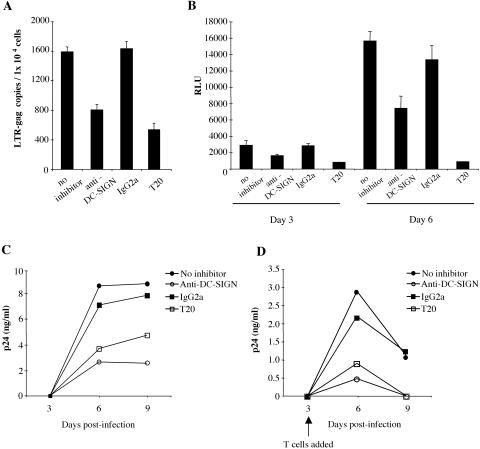
We next investigated the mechanisms by which immature DCs transmit infectious particles to T cells several days after viral exposure. Coexpression of DC-SIGN with the HIV entry receptors has been shown to enhance the efficiency of HIV infection of cell lines, particularly when the cell surface levels of CD4 and the chemokine coreceptors are limiting (15). Since immature DCs express low levels of CCR5 and CXCR4 and allow replication of both HIV X4 and R5 strains (2, 8, 23), we investigated whether DC-SIGN could facilitate HIV entry and infection of immature DCs and also studied the contribution of this mechanism to long-term transfer of HIV to T cells. For this experiment, monocyte-derived DCs were preincubated with the anti-DC-SIGN MAb 1B10 and, as a control, with the viral fusion inhibitor T20 before infection for 4 hours with the X4 HIV strain NL43. We observed that the neutralizing anti-DC-SIGN MAb 1B10 inhibited the formation of late viral DNA products with a similar efficiency to that of the fusion inhibitor T20 (Fig. 3A). Furthermore, at a low MOI, anti-DC-SIGN MAb reduced DC infection by single-cycle pseudotyped HXB2 HIV particles, while an isotype control had no effect (Fig. 3B). Similar results were also observed with R5 HIV strains (data not shown). We then extended our investigations to the role of DC-SIGN in DC infection and long-term transfer of HIV to T cells. We found that pretreatment of cells with neutralizing anti-DC-SIGN MAb strongly diminished both infection of DCs by the R5 strain NLAD8 (Fig. 3C) and transmission of virus to T cells following prolonged culture of DCs (Fig. 3D). The inhibitory effect of the anti-DC-SIGN MAb on DC infection was observed at low but not high virus concentrations of both R5 and X4 virus strains (data not shown). We also found that viral transmission was inhibited when DCs were pretreated with T20 and cultured for 3 days prior to the addition of T cells, indicating that viral fusion is required for long-term HIV transfer from DCs to T cells (Fig. 3D). Taken together, these results suggest that DC-SIGN-mediated _cis_-infection of immature DCs contributes to HIV transfer to T cells several days after viral exposure.
FIG. 3.
DC-SIGN-mediated _cis_-infection of DCs contributes to long-term transfer of HIV to CD4+ T cells. (A) HIV DNA synthesis. DCs (1 × 106) were preincubated with either anti-DC-SIGN MAb (25 μg/ml), an isotype control (25 μg/ml), or T20 (1 μM) or were mock treated. Cells were then infected with the HIV X4 strain NL43 (100 ng of p24) for 4 hours at 37°C, washed extensively, and maintained in culture for 2 days. Cells were harvested, and late viral DNA products were quantified by real-time PCR. (B) DC infection by X4 HIV Luc. Immature DCs were pretreated with inhibitors as described for panel A. Cells were then infected with single-cycle HIV Luc pseudotyped with the HXB2 envelope (10 ng of p24) for 3 h at 37°C. DCs were washed extensively and maintained in RPMI supplemented with GM-CSF and IL-4 for either 3 or 6 days before determining the luciferase activity. (C) DCs were pretreated with inhibitors as described for panel A before the addition of NLAD8 (0.4 ng of p24 for 1 × 105 cells) for 3 h at 37°C. Cells were washed extensively and maintained in culture. p24 Gag accumulation in cell supernatants was determined on days 3, 6, and 9. (D) DCs were infected as described for panel C. Three days after infection, DCs were cocultured with 1 × 105 activated primary T cells. Aliquots of culture supernatants were taken at the indicated time points and assayed for p24. The experiments presented here were carried out using DCs generated from different donors. Data are representative of three independent experiments, and values are given as means of triplicates ± standard deviations.
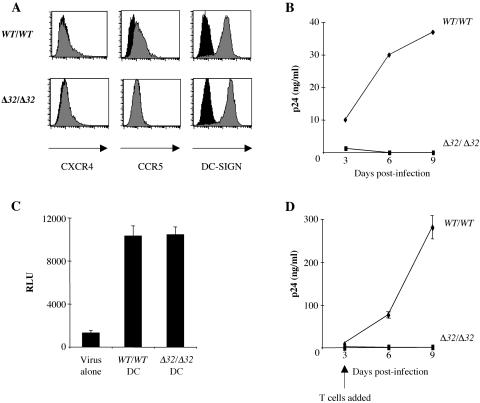
We further investigated the requirement for DC infection in long-term viral transfer by using immature DCs that are genetically resistant to HIV infection. We generated immature DCs from healthy donors (WT/WT) and from individuals carrying a homozygous 32-bp deletion in the ccr5 gene (Δ32/Δ32) which confers resistance to infection by R5 HIV strains (28). This cellular model allowed us to evaluate the relative contributions of incoming virus versus newly synthesized virions in DC-mediated HIV transmission. As shown in Fig. 4A, DC-SIGN and CXCR4 expression levels were similar in WT/WT and Δ32/Δ32 DCs. As expected, Δ32/Δ32 DCs did not express CCR5 at the cell surface (Fig. 4A) and were resistant to infection by the R5 HIV strain NLAD8 (Fig. 4B). To investigate the capacity of WT/WT and Δ32/Δ32 DCs to boost T-cell infection shortly after virus exposure, cells were pulsed with R5 BaL Luc pseudotyped viruses for 2 hours before being cocultured with activated T cells. Compared to direct infection of T cells, we found that both WT/WT and Δ32/Δ32 DCs captured HIV and enhanced viral infection, with equal efficiencies (Fig. 4C). Similar results were obtained with the NLAD8 wild-type strain and with JR-CSF Luc (data not shown). To test whether immature DCs retain incoming virions in an infectious form, WT/WT and Δ32/Δ32 DCs were pulsed with NLAD8 for 3 h, washed extensively, and cultured for 3 days before adding activated T cells. As observed by others (32), WT/WT DCs transmitted HIV infection several days after virus exposure (Fig. 4D). In contrast, we found that Δ32/Δ32 DCs, which cannot be infected by the R5 NLAD8 strain, were totally unable to transfer infectious particles to T cells (Fig. 4D), indicating that DC infection is crucial for long-term transfer of HIV to T cells.
FIG. 4.
DC infection is essential for delayed transfer of HIV to T cells. (A) FACS analysis of cell surface expression of CXCR4, CCR5, and DC-SIGN on WT/WT and Δ32/Δ32 immature DCs. Black histograms show data for an isotype control Ab. (B) DC infection. WT/WT and Δ32/Δ32 DCs (4 × 105) were infected with the R5 strain NLAD8 (10 ng of p24) for 3 h at 37°C. Cells were washed and cultured in medium containing GM-CSF and IL-4. Viral p24 Gag in the culture supernatants was measured on days 3, 6, and 9 postinfection. (C) Short-term transfer. WT/WT and Δ32/Δ32 immature DCs were infected at a low MOI (0.1) with R5 BaL Luc pseudotyped viruses for 2 hours and cocultured with activated T cells. Luciferase activities in cell lysates were evaluated at 3 days postinfection. As a control, HIV Luc viruses were incubated with medium alone (virus alone) and, 2 hours later, transferred to T cells. (D) Long-term transfer. WT/WT and Δ32/Δ32 DCs (4 × 105) were infected with the R5 HIV strain NLAD8 (10 ng of p24) for 3 h at 37°C. Cells were washed and cultured in RPMI-GM-CSF-IL-4 for 3 days before the addition of an equal number of activated T cells. Aliquots of culture supernatants were taken at the indicated time points and assayed for p24 antigen by enzyme-linked immunosorbent assay. Data are representative of two independent experiments using two different Δ32/Δ32 donors.
DISCUSSION
Mucosal DCs are likely to be the first cells targeted by HIV after sexual transmission, and due to their anatomical distribution and their motility, they are believed to play a crucial role in virus dissemination within the host (10, 30). DCs express the HIV entry receptors (CD4, CCR5, and CXCR4) and also C-type lectins that may facilitate virus capture and transmission to CD4+ T cells (33, 37). DC-SIGN is the only C-type lectin receptor identified so far that mediates _trans_-enhancement of T-cell infection, an infection-independent mechanism through which DCs can amplify T-cell infection (7, 13). In contrast to previous observations (13), our data indicate that _trans_-enhancement of T-cell infection occurs efficiently in the absence of DC-SIGN endocytosis. We found that alanine substitutions in each DC-SIGN internalization signal have no impact on the capacity of DC-SIGN to boost viral replication in T cells soon after viral exposure. The internalization-defective DC-SIGN mutants (LL and LL/EEE/Y) were still able to capture HIV and enhance T-cell infection, with equal efficiencies to those of their WT counterparts. We suggest that our observations and those of others (13) that DC-SIGN ΔN mutants are unable to mediate _trans_-enhancement are a result of poor surface expression and virus capture rather than a requirement for HIV internalization in the transfer process. Consistent with this, it has been shown that the efficiency of DC-SIGN-mediated HIV transmission depends on the amount of virus bound to DC-SIGN and closely correlates with DC-SIGN expression levels (26). DC-SIGN captures HIV particles through high-affinity calcium-dependent interactions between its carbohydrate recognition domain and the highly glycosylated gp120 envelope protein (35). Our data indicate that removal of DC-SIGN-bound HIV at the cell surface by the calcium chelator EDTA inhibits viral transmission mediated by DC-SIGN-expressing cells. Our study argues in favor of a model in which the _trans_-enhancement process occurs mainly through DC-SIGN-bound virus at the cell surface and is independent of DC-SIGN internalization signals. It is likely that the high-affinity binding of gp120 to DC-SIGN (Kd, 1.5 nM) (3) allows the concentration of HIV particles at the cell surface, resulting in optimal interactions with the HIV entry receptors expressed on target cells and enhanced infection relative to that by cell-free virus. Our data indicate that in immature DCs, both cell surface-bound and internalized HIV particles are transmitted to T cells soon after viral uptake. Indeed, we observed that HIV transmission was significantly reduced, but not completely abrogated, when DC-bound HIV was removed by EDTA. This is consistent with fluorescence microscopy observations of HIV internalization in DCs and transfer to sites of cell-cell contact (6, 20). However, based on our findings using endocytosis-deficient DC-SIGN mutants, it is unlikely that DC-SIGN is directly responsible for HIV internalization in DCs. It is conceivable that HIV particles bound to DC-SIGN at the cell surface are subsequently internalized into DCs independently of the DC-SIGN endocytosis motifs by an alternative mechanism such as phagocytosis.
Immature DCs are able to efficiently transmit HIV to CD4+ T cells, even several days after virus exposure (11, 32). DC-SIGN has been proposed to play an important role in this process by targeting HIV to a low-pH compartment, where incoming virus escapes lysosomal degradation and persists for several days without a loss of infectivity (13). We provide several lines of evidence that argue against this model. Firstly, we show that in Raji cells, DC-SIGN does not maintain HIV virions in an infectious form for a prolonged period. Secondly, we show that long-term HIV transmission depends on viral fusion, as it is blocked when immature DCs are preincubated with the fusion inhibitor T20. These data are consistent with recent studies indicating that DC infection contributes to prolonged HIV transmission to T cells (16, 34). Finally, we demonstrate that DCs genetically resistant to HIV infection (Δ32/Δ32 DCs) are unable to promote the long-term transfer of virions to T cells, despite their ability to efficiently capture and transmit virus shortly after viral uptake. These results exclude any significant role of stored incoming viral particles in the long-term transfer of virus to T cells and formally demonstrate that in immature DCs, this process occurs exclusively through DC infection and transmission of newly synthesized virions. Interestingly, a similar requirement for viral replication has been observed for Langerhans cells (LCs), an epidermal DC subset that lacks DC-SIGN and is suspected to be an initial target of HIV after sexual transmission (11). Using an ex vivo explant model of LC infection, it has been shown that LC-mediated viral transmission to T cells is blocked by preincubating LCs with neutralizing anti-CD4 antibodies or the CCR5 agonist PSC-RANTES (11). Topical application of PSC-RANTES or inhibitors of HIV attachment to CCR5 or of viral fusion is also able to block vaginal transmission of simian-human immunodeficiency virus (SHIV) in macaques, demonstrating the importance of infection of mucosal cells, possibly including DCs, in HIV transmission in vivo (14, 36).
Our data indicate that DC-SIGN is required for efficient HIV entry into immature DCs, since an anti-DC-SIGN MAb inhibits the formation of late viral DNA products. With a low virus input, neutralizing anti-DC-SIGN MAb also inhibits both DC infection by X4 and R5 HIV strains and subsequent long-term transfer of viral infection to T cells. Together, these results suggest that DC-SIGN acts as a _cis_-receptor that facilitates HIV infection of immature DCs. DC-SIGN has been shown to enhance the efficiency of HIV entry into cell lines that express low levels of coreceptors (15). This is supported by the finding that mannan, a ligand of DC-SIGN, blocks HIV infection of monocyte-derived immature DCs (33). DC-SIGN has also been described to promote _cis_-infection of DCs by other enveloped viruses such as dengue virus and cytomegalovirus (9, 17). This function probably relies on the capacity of DC-SIGN to concentrate viral particles at the cell surface, allowing optimal interactions with their cognate receptors and enhanced viral entry (17).
Recent studies have led to the proposal that HIV transfer from immature DCs to T cells occurs in two phases: a short-term phase (up to 24 h after viral exposure) transfers input virions, while long-term transfer (from 24 h to 72 h) is proposed to involve DC infection (34). Our study supports this model and further characterizes the role played by DC-SIGN in both short- and long-term transfer. In conclusion, we propose that in both cases, DC-SIGN acts as an attachment factor that concentrates HIV particles at the DC surface. Shortly after viral exposure, DC-SIGN acts essentially as a _trans_-receptor that permits the transfer of input virus to CD4+ T cells independent of DC-SIGN internalization signals. DC-SIGN-bound virus may also be transferred in cis to the canonical HIV entry receptors, resulting in efficient DC infection, which is essential for the long-term transfer of virus. The relative contribution of each phase to HIV transmission in vivo remains to be established. Immature DCs may transfer HIV to T lymphocytes residing in the mucosa or after trafficking to CD4+ T cells in lymphoid tissues. It has been observed that immature DCs can migrate to lymph nodes within 24 h (12). Such a timescale suggests that both DC-SIGN-mediated _cis_-infection of DCs and _trans_-enhancement of T-cell infection may occur in vivo, either in mucosal surfaces or in lymph nodes. However, it is likely that DC infection, which provides a continuous source of virus for T cells, may represent the major mechanism that contributes to HIV dissemination and persistence of viral infection in vivo.
Acknowledgments
We thank A. Saïb, O. Schwartz, and A. Moris for helpful discussions. We are very grateful to M. Parmentier and J. L. Pablos for providing ccr5 Δ32/Δ32 blood samples. We thank Emmanuelle Perret and Julie Harriague for assistance with confocal microscopy and all members of the cell sorting facility of the Pasteur Institute. We thank the NIH AIDS Research and Reference Reagent Program for reagents.
This work was supported by grants from SIDACTION and ANRS (Agence Nationale de Recherches sur le SIDA). L.B. and P.-Y.L. were funded by fellowships from SIDACTION and the Pediatric Dengue Vaccine Initiative, respectively.
REFERENCES
- 1.Amara, A., A. Vidy, G. Boulla, K. Mollier, J. Garcia-Perez, J. Alcami, C. Blanpain, M. Parmentier, J. L. Virelizier, P. Charneau, and F. Arenzana-Seisdedos. 2003. G protein-dependent CCR5 signaling is not required for efficient infection of primary T lymphocytes and macrophages by R5 human immunodeficiency virus type 1 isolates. J. Virol. 77**:**2550-2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canque, B., Y. Bakri, S. Camus, M. Yagello, A. Benjouad, and J. C. Gluckman. 1999. The susceptibility to X4 and R5 human immunodeficiency virus-1 strains of dendritic cells derived in vitro from CD34(+) hematopoietic progenitor cells is primarily determined by their maturation stage. Blood 93**:**3866-3875. [PubMed] [Google Scholar]
- 3.Curtis, B. M., S. Scharnowske, and A. J. Watson. 1992. Sequence and expression of a membrane-associated C-type lectin that exhibits CD4-independent binding of human immunodeficiency virus envelope glycoprotein gp120. Proc. Natl. Acad. Sci. USA 89**:**8356-8360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deng, H. K., D. Unutmaz, V. N. KewalRamani, and D. R. Littman. 1997. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature 388**:**296-300. [DOI] [PubMed] [Google Scholar]
- 5.Engering, A., T. B. Geijtenbeek, S. J. van Vliet, M. Wijers, E. van Liempt, N. Demaurex, A. Lanzavecchia, J. Fransen, C. G. Figdor, V. Piguet, and Y. van Kooyk. 2002. The dendritic cell-specific adhesion receptor DC-SIGN internalizes antigen for presentation to T cells. J. Immunol. 168**:**2118-2126. [DOI] [PubMed] [Google Scholar]
- 6.Garcia, E., M. Pion, A. Pelchen-Matthews, L. Collinson, J. F. Arrighi, G. Blot, F. Leuba, J. M. Escola, N. Demaurex, M. Marsh, and V. Piguet. 2005. HIV-1 trafficking to the dendritic cell-T-cell infectious synapse uses a pathway of tetraspanin sorting to the immunological synapse. Traffic 6**:**488-501. [DOI] [PubMed] [Google Scholar]
- 7.Geijtenbeek, T. B., D. S. Kwon, R. Torensma, S. J. van Vliet, G. C. van Duijnhoven, J. Middel, I. L. Cornelissen, H. S. Nottet, V. N. KewalRamani, D. R. Littman, C. G. Figdor, and Y. van Kooyk. 2000. DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances trans-infection of T cells. Cell 100**:**587-597. [DOI] [PubMed] [Google Scholar]
- 8.Granelli-Piperno, A., E. Delgado, V. Finkel, W. Paxton, and R. M. Steinman. 1998. Immature dendritic cells selectively replicate macrophage-tropic (M-tropic) human immunodeficiency virus type 1, while mature cells efficiently transmit both M- and T-tropic virus to T cells. J. Virol. 72**:**2733-2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halary, F., A. Amara, H. Lortat-Jacob, M. Messerle, T. Delaunay, C. Houles, F. Fieschi, F. Arenzana-Seisdedos, J. F. Moreau, and J. Dechanet-Merville. 2002. Human cytomegalovirus binding to DC-SIGN is required for dendritic cell infection and target cell trans-infection. Immunity 17**:**653-664. [DOI] [PubMed] [Google Scholar]
- 10.Hu, J., M. B. Gardner, and C. J. Miller. 2000. Simian immunodeficiency virus rapidly penetrates the cervicovaginal mucosa after intravaginal inoculation and infects intraepithelial dendritic cells. J. Virol. 74**:**6087-6095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawamura, T., F. O. Gulden, M. Sugaya, D. T. McNamara, D. L. Borris, M. M. Lederman, J. M. Orenstein, P. A. Zimmerman, and A. Blauvelt. 2003. R5 HIV productively infects Langerhans cells, and infection levels are regulated by compound CCR5 polymorphisms. Proc. Natl. Acad. Sci. USA 100**:**8401-8406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kissenpfennig, A., S. Henri, B. Dubois, C. Laplace-Builhe, P. Perrin, N. Romani, C. H. Tripp, P. Douillard, L. Leserman, D. Kaiserlian, S. Saeland, J. Davoust, and B. Malissen. 2005. Dynamics and function of Langerhans cells in vivo: dermal dendritic cells colonize lymph node areas distinct from slower migrating Langerhans cells. Immunity 22**:**643-654. [DOI] [PubMed] [Google Scholar]
- 13.Kwon, D. S., G. Gregorio, N. Bitton, W. A. Hendrickson, and D. R. Littman. 2002. DC-SIGN-mediated internalization of HIV is required for trans-enhancement of T cell infection. Immunity 16**:**135-144. [DOI] [PubMed] [Google Scholar]
- 14.Lederman, M. M., R. S. Veazey, R. Offord, D. E. Mosier, J. Dufour, M. Mefford, M. Piatak, Jr., J. D. Lifson, J. R. Salkowitz, B. Rodriguez, A. Blauvelt, and O. Hartley. 2004. Prevention of vaginal SHIV transmission in rhesus macaques through inhibition of CCR5. Science 306**:**485-487. [DOI] [PubMed] [Google Scholar]
- 15.Lee, B., G. Leslie, E. Soilleux, U. O'Doherty, S. Baik, E. Levroney, K. Flummerfelt, W. Swiggard, N. Coleman, M. Malim, and R. W. Doms. 2001. cis expression of DC-SIGN allows for more efficient entry of human and simian immunodeficiency viruses via CD4 and a coreceptor. J. Virol. 75**:**12028-12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lore, K., A. Smed-Sorensen, J. Vasudevan, J. R. Mascola, and R. A. Koup. 2005. Myeloid and plasmacytoid dendritic cells transfer HIV-1 preferentially to antigen-specific CD4+ T cells. J. Exp. Med. 201**:**2023-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lozach, P. Y., L. Burleigh, I. Staropoli, E. Navarro-Sanchez, J. Harriague, J. L. Virelizier, F. A. Rey, P. Despres, F. Arenzana-Seisdedos, and A. Amara. 2005. Dendritic cell-specific intercellular adhesion molecule 3-grabbing non-integrin (DC-SIGN)-mediated enhancement of dengue virus infection is independent of DC-SIGN internalization signals. J. Biol. Chem. 280**:**23698-23708. [DOI] [PubMed] [Google Scholar]
- 18.Lozach, P. Y., H. Lortat-Jacob, A. de Lacroix de Lavalette, I. Staropoli, S. Foung, A. Amara, C. Houles, F. Fieschi, O. Schwartz, J. L. Virelizier, F. Arenzana-Seisdedos, and R. Altmeyer. 2003. DC-SIGN and L-SIGN are high affinity binding receptors for hepatitis C virus glycoprotein E2. J. Biol. Chem. 278**:**20358-20366. [DOI] [PubMed] [Google Scholar]
- 19.Mannioui, A., E. Nelson, C. Schiffer, N. Felix, E. Le Rouzic, S. Benichou, J. C. Gluckman, and B. Canque. 2005. Human immunodeficiency virus type 1 KK(26-27) matrix mutants display impaired infectivity, circularization and integration but not nuclear import. Virology 339**:**21-30. [DOI] [PubMed] [Google Scholar]
- 20.McDonald, D., L. Wu, S. M. Bohks, V. N. KewalRamani, D. Unutmaz, and T. J. Hope. 2003. Recruitment of HIV and its receptors to dendritic cell-T cell junctions. Science 300**:**1295-1297. [DOI] [PubMed] [Google Scholar]
- 21.Mellman, I., and R. M. Steinman. 2001. Dendritic cells: specialized and regulated antigen processing machines. Cell 106**:**255-258. [DOI] [PubMed] [Google Scholar]
- 22.Moris, A., C. Nobile, F. Buseyne, F. Porrot, J. P. Abastado, and O. Schwartz. 2004. DC-SIGN promotes exogenous MHC-I-restricted HIV-1 antigen presentation. Blood 103**:**2648-2654. [DOI] [PubMed] [Google Scholar]
- 23.Nobile, C., C. Petit, A. Moris, K. Skrabal, J. P. Abastado, F. Mammano, and O. Schwartz. 2005. Covert human immunodeficiency virus replication in dendritic cells and in DC-SIGN-expressing cells promotes long-term transmission to lymphocytes. J. Virol. 79**:**5386-5399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petit, C., F. Buseyne, C. Boccaccio, J. P. Abastado, J. M. Heard, and O. Schwartz. 2001. Nef is required for efficient HIV-1 replication in cocultures of dendritic cells and lymphocytes. Virology 286**:**225-236. [DOI] [PubMed] [Google Scholar]
- 25.Ploquin, M. J., O. M. Diop, N. Sol-Foulon, L. Mortara, A. Faye, M. A. Soares, E. Nerrienet, R. Le Grand, Y. Van Kooyk, A. Amara, O. Schwartz, F. Barre-Sinoussi, and M. C. Muller-Trutwin. 2004. DC-SIGN from African green monkeys is expressed in lymph nodes and mediates infection in trans of simian immunodeficiency virus SIVagm. J. Virol. 78**:**798-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pohlmann, S., F. Baribaud, B. Lee, G. J. Leslie, M. D. Sanchez, K. Hiebenthal-Millow, J. Munch, F. Kirchhoff, and R. W. Doms. 2001. DC-SIGN interactions with human immunodeficiency virus type 1 and 2 and simian immunodeficiency virus. J. Virol. 75**:**4664-4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pope, M., M. G. Betjes, N. Romani, H. Hirmand, P. U. Cameron, L. Hoffman, S. Gezelter, G. Schuler, and R. M. Steinman. 1994. Conjugates of dendritic cells and memory T lymphocytes from skin facilitate productive infection with HIV-1. Cell 78**:**389-398. [DOI] [PubMed] [Google Scholar]
- 28.Samson, M., F. Libert, B. J. Doranz, J. Rucker, C. Liesnard, C. M. Farber, S. Saragosti, C. Lapoumeroulie, J. Cognaux, C. Forceille, G. Muyldermans, C. Verhofstede, G. Burtonboy, M. Georges, T. Imai, S. Rana, Y. Yi, R. J. Smyth, R. G. Collman, R. W. Doms, G. Vassart, and M. Parmentier. 1996. Resistance to HIV-1 infection in Caucasian individuals bearing mutant alleles of the CCR-5 chemokine receptor gene. Nature 382**:**722-725. [DOI] [PubMed] [Google Scholar]
- 29.Sol-Foulon, N., A. Moris, C. Nobile, C. Boccaccio, A. Engering, J. P. Abastado, J. M. Heard, Y. van Kooyk, and O. Schwartz. 2002. HIV-1 Nef-induced upregulation of DC-SIGN in dendritic cells promotes lymphocyte clustering and viral spread. Immunity 16**:**145-155. [DOI] [PubMed] [Google Scholar]
- 30.Spira, A. I., P. A. Marx, B. K. Patterson, J. Mahoney, R. A. Koup, S. M. Wolinsky, and D. D. Ho. 1996. Cellular targets of infection and route of viral dissemination after an intravaginal inoculation of simian immunodeficiency virus into rhesus macaques. J. Exp. Med. 183**:**215-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Staropoli, I., C. Chanel, M. Girard, and R. Altmeyer. 2000. Processing, stability, and receptor binding properties of oligomeric envelope glycoprotein from a primary HIV-1 isolate. J. Biol. Chem. 275**:**35137-35145. [DOI] [PubMed] [Google Scholar]
- 32.Trumpfheller, C., C. G. Park, J. Finke, R. M. Steinman, and A. Granelli-Piperno. 2003. Cell type-dependent retention and transmission of HIV-1 by DC-SIGN. Int. Immunol. 15**:**289-298. [DOI] [PubMed] [Google Scholar]
- 33.Turville, S. G., P. U. Cameron, A. Handley, G. Lin, S. Pohlmann, R. W. Doms, and A. L. Cunningham. 2002. Diversity of receptors binding HIV on dendritic cell subsets. Nat. Immunol. 3**:**975-983. [DOI] [PubMed] [Google Scholar]
- 34.Turville, S. G., J. J. Santos, I. Frank, P. U. Cameron, J. Wilkinson, M. Miranda-Saksena, J. Dable, H. Stossel, N. Romani, M. Piatak, Jr., J. D. Lifson, M. Pope, and A. L. Cunningham. 2004. Immunodeficiency virus uptake, turnover, and 2-phase transfer in human dendritic cells. Blood 103**:**2170-2179. [DOI] [PubMed] [Google Scholar]
- 35.van Kooyk, Y., and T. B. Geijtenbeek. 2003. DC-SIGN: escape mechanism for pathogens. Nat. Rev. Immunol. 3**:**697-709. [DOI] [PubMed] [Google Scholar]
- 36.Veazey, R. S., P. J. Klasse, S. M. Schader, Q. Hu, T. J. Ketas, M. Lu, P. A. Marx, J. Dufour, R. J. Colonno, R. J. Shattock, M. S. Springer, and J. P. Moore. 2005. Protection of macaques from vaginal SHIV challenge by vaginally delivered inhibitors of virus-cell fusion. Nature 438**:**99-102. [DOI] [PubMed] [Google Scholar]
- 37.Zaitseva, M., A. Blauvelt, S. Lee, C. K. Lapham, V. Klaus-Kovtun, H. Mostowski, J. Manischewitz, and H. Golding. 1997. Expression and function of CCR5 and CXCR4 on human Langerhans cells and macrophages: implications for HIV primary infection. Nat. Med. 3**:**1369-1375. [DOI] [PubMed] [Google Scholar]
- 38.Zennou, V., C. Petit, D. Guetard, U. Nerhbass, L. Montagnier, and P. Charneau. 2000. HIV-1 genome nuclear import is mediated by a central DNA flap. Cell 101**:**173-185. [DOI] [PubMed] [Google Scholar]