The Relative Importance of Physician Communication, Participatory Decision Making, and Patient Understanding in Diabetes Self-management (original) (raw)
Abstract
OBJECTIVE
Patients' self-management practices have substantial consequences on morbidity and mortality in diabetes. While the quality of patient-physician relations has been associated with improved health outcomes and functional status, little is known about the impact of different patient-physician interaction styles on patients' diabetes self-management. This study assessed the influence of patients' evaluation of their physicians' participatory decision-making style, rating of physician communication, and reported understanding of diabetes self-care on their self-reported diabetes management.
DESIGN
We surveyed 2,000 patients receiving diabetes care across 25 Veterans' Affairs facilities. We measured patients' evaluation of provider participatory decision making with a 4-item scale (Provider Participatory Decision-making Style [PDMstyle]; α = 0.96), rating of providers' communication with a 5-item scale (Provider Communication [PCOM]; α = 0.93), understanding of diabetes self-care with an 8-item scale (α = 0.90), and patients' completion of diabetes self-care activities (self-management) in 5 domains (α = 0.68). Using multivariable linear regression, we examined self-management with the independent associations of PDMstyle, PCOM, and Understanding.
RESULTS
Sixty-six percent of the sample completed the surveys (N = 1,314). Higher ratings in PDMstyle and PCOM were each associated with higher self-management assessments (P < .01 in all models). When modeled together, PCOM remained a significant independent predictor of self-management (standardized β: 0.18; P < .001), but PDMstyle became nonsignificant. Adding Understanding to the model diminished the unique effect of PCOM in predicting self-management (standardized β: 0.10; P = .004). Understanding was strongly and independently associated with self-management (standardized β: 0.25; P < .001).
CONCLUSION
For these patients, ratings of providers' communication effectiveness were more important than a participatory decision-making style in predicting diabetes self-management. Reported understanding of self-care behaviors was highly predictive of and attenuated the effect of both PDMstyle and PCOM on self-management, raising the possibility that both provider styles enhance self-management through increased patient understanding or self-confidence.
Keywords: physician-patient relations, disease management, self-care, ambulatory care, chronic disease
Almost 100 million Americans have 1 or more chronic conditions, a number projected to increase by 35 million in the next 25 years.1 Primary care providers face a significant challenge in helping patients manage their chronic conditions to improve their health and quality of life.2,3 And among chronic diseases, diabetes mellitus presents patients with an especially daunting array of behavioral challenges, because optimal control requires a high degree of self-management.* Despite solid evidence for improved clinical outcomes with effective treatment,4–8 many people with diabetes continue to have suboptimal glycemic and blood pressure control and elevated low-density lipoprotein levels.9 Moreover, although more than 95% of treatment for diabetes is carried out by patients or their family members, physicians vary widely in their provision of recommendations for self-management,10 and many patients have received no assistance with self-management.11,12 At the same time, many patients face considerable difficulty in carrying out recommended treatment behaviors.10,13,14 One third to three fourths of patients with diabetes report not following physician recommendations for treatment.15–17
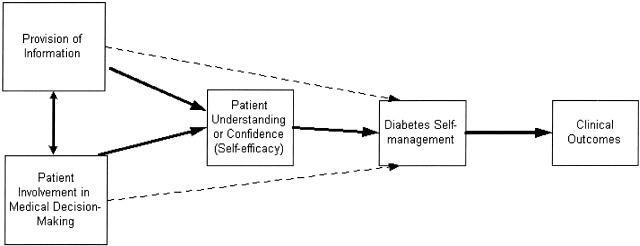
To facilitate patients' self-management, chronic disease experts have called for a “paradigm shift” in provider-patient relations from directive to more collaborative patient-provider interaction styles, with joint definition of problems, treatment goals, and management strategies.18–25 Enhancing patient-provider communication and shared decision making have been shown to result in greater patient satisfaction, adherence to treatment plans,26–28 and improved health outcomes, such as higher self-reported health status, emotional health, symptom relief, and physiological measures of disease control.1,22,29–36 Several recent randomized clinical trials of programs explicitly promoting patient involvement in defining treatment goals and therapeutic strategies for type 1 and type 2 diabetes have also found improved clinical outcomes.37,38 The consistency of these studies' findings of improved physiological outcomes and reported health status is impressive. Yet, the causal mechanism for their results remains unclear. Inherent in a shared decision-making style is: 1) a substantial increase in provider communication and provision of information; and 2) an increase in patient involvement in medical decision making. Much additional research needs to be done to tease out which aspects of these patient-provider interaction styles (or provider styles) are most effective in promoting improved self-management among different groups of patients.39–42 Moreover, we need to better understand the mechanisms by which these styles affect patient self-management. One hypothesis is that they improve self-management by increasing patients' understanding of their conditions and treatments as well as self-confidence in their own self-care abilities (self-efficacy), both of which have been shown to be positively related to treatment adherence.40,43 It is also possible that their effect is explained through other mechanisms, such as increased patient motivation and fit between treatment and patient goals and lifestyles,44 or that they exert a direct effect on patients' self-management. Clarifying these questions will help physicians and health care systems best target time and resources to improve communication, patient self-care behaviors, and ultimately health status.
Therefore, we sought to assess the influence of patients' evaluation of their providers' participatory decision-making style, rating of physician communication, and understanding of diabetes self-care on their diabetes management. The conceptual model we tested is depicted in Figure 1. Using data from a survey of 2,000 diabetic patients receiving care in 25 VA medical centers, we asked: 1) Do patients' assessments of their physicians' provision of information and participatory decision-making style correlate with variations in self-reported diabetes management? 2) What is the relative importance of patients' assessments of these 2 provider styles in predicting their diabetes self-management? 3) Is there evidence that these provider styles improve patient self-management through greater reported understanding of diabetes self-care?
FIGURE 1.
Conceptual model tested: how provider styles influence patients' diabetes self-management.
METHODS
Study Population
The initial sample was composed of 2,000 veterans receiving diabetes care at 1 of 25 VA medical centers located in 4 Veterans' Integrated Service Networks, representing 3 of the 4 census regions. Patients were identified using electronic pharmacy and laboratory information for fiscal years 1998 and 1999 from each participating VA facility and a national utilization database.45,46 Patients were eligible if they satisfied 1 of the following criteria within the past 12 months: 1) one hospitalization with a diabetes-related ICD-9 code (250.x, 357.2, 362.0, or 366.41); 2) two outpatient visits with a diabetes-related ICD-9 code; or 3) at least 1 prescription for a glucose control medication or monitoring supplies. A final eligibility criterion was 2 outpatient visits of any kind in fiscal year 1999. From among those eligible, we randomly sampled 80 patients in each of the 25 facilities for inclusion in the study.
Approval for the study was obtained from the VA Ann Arbor Institutional Review Board. The survey was administered in collaboration with the VA Office of Quality and Performance, as part of a broad effort to improve the quality of diabetes care in the VA. Survey administration consisted of an introductory initial letter followed by the survey itself (1 week later), a reminder post card (at 2 weeks), and a second mailing of surveys (at 4 weeks) sent to nonresponders.
Study Variables
The survey questions were part of a questionnaire created for the Diabetes Quality Improvement Project.47 The survey contained approximately 150 items. These included measures of general health and functioning, diabetes severity, satisfaction with diabetes care, understanding of diabetes care, self-management behaviors, utilization of medical services, and demographics. For the current analyses, we focused on measures of overall self-management and self-management in 5 separate domains (medication, diet, exercise, blood glucose monitoring, and foot care), level of overall understanding of diabetes care and understanding of each of the above 5 domains, evaluation of level of patient involvement in medical decision making (Provider Participatory Decision-making Style [PDMstyle]), and satisfaction with patient- provider communication (Provider Communication [PCOM]). (See Table 1 for description of the scales for each of these variables.) Survey data were supplemented with information extracted from VA national databases. This study included supplemental information on number of outpatient clinic visits to primary care and diabetes-related providers and verification of demographic information (e.g., gender).
Table 1.
Summary Descriptions of Principal Scales Used in Analyses
| Variable* | Scale Domains | Scale Range | Meaning of High Score | Mean | Standard Deviation | Alpha Cronbach |
|---|---|---|---|---|---|---|
| Patient self-management | 1) Taking medications | 0–100 | Greater adherence to treatment recommendations in 5 domains of self-care | 71.32 | 17.11 | 0.68 |
| 2) Exercising regularly | ||||||
| 3) Following eating plan | ||||||
| 4) Checking blood sugar | ||||||
| 5) Checking feet for wounds or sores | ||||||
| Provider participatory decision-making (PDMstyle) | 1) Offer choices in medical care | 0–100 | More participatory | 43.90 | 37.89 | 0.96 |
| 2) Discuss pros and cons of each choice with you | ||||||
| 3) Get you to state which choice or option you prefer | ||||||
| 4) Take your preferences into account when making treatment decisions | ||||||
| Provider Communication (PCOM) | 1) Tell you everything | 0–100 | Better communication | 59.32 | 28.86 | 0.93 |
| 2) Let you know test results when promised | ||||||
| 3) Explain treatment alternatives | ||||||
| 4) Explain side-effects of medications | ||||||
| 5) Tell you what to expect from your disease or treatment | ||||||
| Patient understanding (Understanding) | 1) How to care for feet | 0–100 | Greater understanding of diabetes self-care | 76.29 | 22.52 | 0.90 |
| 2) How to take medications | ||||||
| 3) What to do for symptoms of low blood sugar | ||||||
| 4) How to make food choices | ||||||
| 5) How and when to test blood sugar | ||||||
| 6) Diabetes complications | ||||||
| 7) How to exercise | ||||||
| 8) Target blood glucose values |
The principal outcome measure assessed was the overall self-management scale, as described above and in Table 1. Respondents were asked, “Over the past year, how difficult has it been for you to do each of the following exactly as the doctor who takes care of your diabetes suggested?” The 4 valid response categories ranged from “So difficult that I couldn't do it at all” to “Not difficult, I got it exactly right.” The self-management scale was designed to reflect how well patients feel able to manage aspects of their diabetes care and has been found to be a valid reflection of patients' own involvement with their care. In light of the evidence that adherence to treatment recommendations in 1 domain of diabetes care does not correlate strongly with adherence in other domains,48,49 we also looked at each separate domain as dichotomous dependent variables divided into “Poor” (response categories of did not do at all, hardly ever do, and do some of the time) and “Good” (do most of the time, and got it exactly right).
In secondary analyses the scale for overall understanding of diabetes care was also used as a dependent variable (see Table 1). Respondents were asked to indicate how well they understood how to care for feet, how to take medications, how to make appropriate food choices, how and when to test blood sugar, how to exercise appropriately, what to do for symptoms of low blood sugar, and what target blood glucose values should be.
To understand the influence of provider styles and patient understanding on self-management, we examined 3 principal independent measures: physician decision-making style, provider communication, and overall patient understanding. Provider Participatory Decision-making Style a 4-item scale, measured assessment of physician decision-making style. This measure was originally described in 1995 by Kaplan et al.50 and is defined as the propensity of physicians to involve patients in treatment decisions. Respondents were asked how often the doctors or health care professionals who take care of their diabetes: 1) offered them choices in their medical care; 2) discussed the pros and cons of each choice with them; 3) got them to state which choice or option they would prefer; 4) took their preferences into account when making treatment decisions. These questions were rated on a 5-point scale from 0 (none of the time) to 4 (all of the time).
A 5-item scale taken from the American Board of Internal Medicine patient survey measured satisfaction with provider communication about their illness and treatment. Respondents were asked how the doctors or health care professionals who take care of their diabetes were at: 1) telling them everything; 2) letting them know test results when promised; 3) explaining treatment alternatives; 4) explaining side effects of medications; 5) telling them what to expect from their disease or treatment. Response categories ranged from “Poor” (0) to “Excellent” (4). The third primary dependent variable, patients' understanding of their diabetes self-care, was assessed as described above.
Covariate adjustors included demographic information gathered from the survey, such as age, ethnicity, gender, education level, household income, treatment regimen, and how long they had had diabetes. Two measures of health status were included: diabetes-related severity and co-morbidities, and general health perceptions. The number and severity of diabetes co-morbidities were measured using the components of the Total Illness Burden Index that are directly related to diabetes, a validated scale that ranges from 0 to 100.41,51 General health perceptions were measured by a single item (“In general, would you say your health is…” with responses ranging from “Excellent” to “Poor”).
Analyses
Because study participants were clustered by medical facility, we conducted preliminary analyses using multilevel models that computed the intraclass correlation coefficients for our principal dependent variables (SAS MIXED, version 6.12; SAS Institute, Inc., Cary, NC). The intraclass coefficients were very close to zero and did not approach significance, indicating that self-management and evaluation of provider styles did not vary significantly by facility. We therefore conducted our primary analyses using ordinary least squares multiple regression. These analyses were conducted using STATA 6 (Stata Corp., College Station, Tex) on data sets stripped of all personal and facility-level identifiers.
We used linear regression to examine separately the bivariate and multivariate association of PDMstyle, PCOM, and respondents' understanding of diabetes care as predictors of overall self-management. To assess the relative predictive power of each of our 3 principal independent variables, we compared their standardized β coefficients in models combining the 2 provider variables and then added Understanding to this combined model. All regression models also adjusted for age, ethnicity (coded as white, black, Latino, and other), gender, education level, household income (coded as ≤$10,000, 10–15,000,10–15,000, 10–15,000,15–25,000, and >$25,000), treatment regimen (coded as on insulin, on oral medications only, and no medications), duration of diabetes, general health status, and diabetes co-morbidities. Logistic regression analyses were used to evaluate factors associated with each of the 5 components of self-management (see above).
We then sought to determine the magnitude of the associations between respondents' evaluation of their providers' participatory decision-making style and of their provider communication with both respondents' self-management and understanding of diabetes care. Accordingly, we used the relevant regression models to calculate predicted mean self-management scores and overall understanding scores with PDMstyle scores for the 30th percentile (mean score = 0) and 90th percentile (mean score = 74.8), and PCOM scores for the 30th percentile (mean score = 21.7) and 90th percentile (mean score = 79.9). We represented the scales at these levels to compare the extremes of the response categories: the 30th percentile was the lowest possible percentile for the PDMstyle scale because some respondents ranked their providers 0 on the scale. For these calculations, we held all covariate values constant at their means.
Regression diagnostic procedures yielded no evidence of substantive multi-collinearity, heteroscedasticity, or overly influential outliers in any of the models. There was no evidence of significant interactions among our 3 principal explanatory variables, PDMstyle, PCOM, and Understanding, or for second-order curvilinear relationships between these 3 explanatory scales and the scale of self-reported self-management. Finally, we conducted a confirmatory factor analysis using maximum likelihood estimation (SAS CALIS in LINEQS mode, version 6.12) to assess whether PDMstyle and PCOM were in fact measuring 2 distinct constructs.52 This analysis found that a single-factor model produced a very poor fit of the data (Bentler's Comparative Fit Index [CFI] = 0.72; root mean square of approximation [RMSEA] = 0.34; χ2 = 3,356.01; 25 df; P < .01; n = 1,170). In contrast, a model in which the 4 PDMstyle items were constrained to load on one factor and the 5 PCOM items on a second factor fit the data well (CFI = 0.99; RMSEA = 0.07; χ2 = 172.48; 24 df; P < .01; n = 1,170). In this second model, the 2 factors were allowed to covary. The observed correlation was r = 0.53, suggesting that the two factors are correlated, but not redundant. Therefore, on the basis of our prior hypothesis, content validity, and factor analysis, we concluded that the 2 measures indeed were measuring different although possibly related psychological constructs in our sample.
RESULTS
The cooperation rate was 72%, with 1,431 eligible patients filling out the survey. Of these, 117 (8%) were determined to be ineligible for the study, either because they indicated that they did not have diabetes (n = 53), they left too much of the survey blank to confirm their eligibility (n = 31), or they were deceased at the time of the study (n = 33). Thus, our final survey sample size was 1,314, 66% of the original sample. Administrative data showed that the respondents (n = 1,431) were older (68 vs 65; P < .001) and had more outpatient visits in the study period (4.8 vs 4.1; P < .001) than nonrespondents.
Table 2 summarizes some of the principal demographic and health characteristics of the survey sample.
Table 2.
Characteristics of Eligible Survey Responders (N = 1,314)
| Mean age, y (SD) | 67 (11) |
|---|---|
| Mean years with diabetes (SD) | 12 (9) |
| Male gender, % | 98 |
| Ethnicity, % | |
| White | 81 |
| African American | 12 |
| Latino | 4 |
| Other | 3 |
| Education, y, % | |
| 0–8 | 13 |
| 9–12 | 52 |
| 13–16 | 27 |
| ≥17 | 8 |
| Income, % | |
| $≤10,000 | 20 |
| $10,000–15,000 | 26 |
| $15,000–25,000 | 29 |
| >$25,000 | 25 |
| Hypoglycemic regimen, % | |
| Oral medications only | 58 |
| On insulin | 35 |
| No medications | 7 |
| Health status, % | |
| Excellent/very good | 7 |
| Good | 34 |
| Fair | 44 |
| Poor | 15 |
| Mean outpatient visits in last year, n (SD) | 5 (4) |
| Mean diabetes co-morbidity (TIBI) scale (SD) | 40 (19)* |
| Mean general health perception score (SD) | 38 (25)† |
Relationship of Provider Style Variables and Understanding to Patient Self-management
PDMstyle was a highly significant positive predictor of overall self-management in multiple linear regression models that did not include PCOM or Understanding (Table 3, Model 1, β = 0.04, P = .007, model _R_2 = .18). In the logistic regression models predicting the separate domains of diabetes self-management (analyses not shown), PDMstyle was a significant predictor only of observing a good diabetes diet (P = .003). It was not significantly associated with medications taking, exercise, blood glucose monitoring, or foot care.
Table 3.
Associations Between Evaluations of Provider Participatory Decision-making Style (PDMstyle), Provider Communication (PCOM), and Patients' Understanding of Diabetes Care with Patients' Reported Diabetes Self-management*
| Overall Self-management | ||||||
|---|---|---|---|---|---|---|
| Predictors | Model 1† (Model _R_2 = .18) | Model 2‡ (Model _R_2 = .21) | Model 3§ (Model _R_2 = .25) | |||
| Beta | P Value | Beta | P Value | Beta | P Value | |
| PDMstyle | 0.04 | .007 | — | — | — | — |
| PCOM | — | — | 0.10 | <.001 | — | — |
| Overall Understanding of diabetes care | — | — | — | — | 0.21 | <.001 |
Provider communication was significantly associated with overall self-management (β = 0.10, P < .001, model _R_2 = .21; (see Table 3, Model 2). It was also associated with medications taking (P < .001), diet (P < .001), blood glucose monitoring (P = .008), and foot care (P = .002), but not with exercise. Overall understanding was highly predictive of overall self-management (Table 3, Model 3, β = 0.21, P < .001) and of self-management in each of all 5 domains of diabetes care (P < .001 in all logistic regression models).
Relative Predictive Power of PDMstyle, PCOM, and Understanding for Self-management in Combined Multivariate Models
As Table 4 shows, when we combined PDMstyle and PCOM in the same model, provider communication remained highly significant (standardized β = 0.175, P < .001), but PDMstyle was no longer significantly associated with self-management (standardized β = −0.003, _P_ > .20). When Understanding was added to this model, the unique effect of PCOM in predicting self-management dropped substantially but remained significant (standardized β = 0.10, P = .004).Understanding was strongly and independently associated with self-management (standardized β = 0.25, P < .001) in this model. This suggests that at least some of the influence of provider communication and participatory decision-making style may be mediated by patients' understanding of their diabetes care or confidence in their self-care abilities.
Table 4.
Associations Between Provider Participatory Decision-making Style (PDMstyle), Provider Communication (PCOM), and Patient Understanding with Patients' Reported Self-management, after Adjustment*
| Overall Self-management | ||||
|---|---|---|---|---|
| Model A† (Model _R_2 = .21) | Model B‡ (Model _R_2 = .25) | |||
| Predictors | Standardized beta coefficient | P Value (SE) | Standardized beta coefficient | P Value (SE) |
| PDMstyle | −0.003 | >.20 (0.015) | −0.041 | >.20 (0.015) |
| PCOM | 0.175 | <.001 (0.020) | 0.100 | .004 (0.020) |
| Overall Understanding of diabetes care | — | — | 0.246 | <.001 (0.025) |
Similarly, in the separate logistic regressions including both PCOM and Understanding as independent variables with self-management in each of the 5 domains of diabetes care as the dependent variables, PCOM remained statistically significant for medications taking (P = .009), diet adherence (P < .001), and foot care (P = .015), but lost statistical significance for blood glucose monitoring (P = .140) and continued to be nonsignificant for exercise (P = .38). Understanding was a highly significant predictor of self-management in all domains (P = .009) in all logistic regression models.
Predicted Mean Self-management and Understanding Scores Based on PDMstyle and PCOM Ratings
Predicted mean self-management scores based on the level of Understanding, PDMstyle, and PCOM scores are presented in Table 5. Whereas predicted self-management scores at the 0–30th and 90th–100th percentiles of PCOM ratings differed by 6.8 points, or 0.40 SD, there was little difference between the 30th and 90th percentile of PDMstyle ratings, and in fact a slight decrease from 72.3 to 70.2. Predicted self-management scores at the 30th and 90th percentiles of patient understanding, however, differed by 10 points (0.58 SD).
Table 5.
Predicted Self-management Score Based on Patients' Evaluation of Provider Participatory Decision-making Style (PDMstyle), Communication (PCOM), and Their Own Understanding of Diabetes Care*
| Patients' Evaluation Variable† | Predicted Mean Self-management Score Adjusted Mean (95% CI) |
|---|---|
| PDMstyle | |
| 0–30th percentile (0) | 72.3 (±17.1) |
| 90th–100th percentile (74.8) | 70.2 (±17.1) |
| PCOM | |
| 0–30th percentile (21.7) | 68.8 (±15.1) |
| 90th–100th percentile (79.9) | 75.6 (±15.1) |
| Understanding | |
| 0–30th percentile (46.7) | 67.8 (±13.8) |
| 90th–100th percentile (92.0) | 77.8 (±12.6) |
Because the influence of communication and PDMstyle on self-management seemed to be at least in part mediated by Understanding, we also examined the predicted mean Understanding scores from the adjusted model simultaneously containing both PDMstyle and PCOM as independent variables. Predicted mean understanding scores increased considerably from the 30th to the 90th percentile of both PCOM and PDMstyle ratings, increasing 17.7 points (or 0.79 SD) with higher PCOM ratings and 10 points (or 0.44 SD) with higher PDMstyle ratings.
DISCUSSION
The tasks patients with diabetes need to undertake to manage their illness are complicated and can be difficult to sustain. Physicians may feel frustrated about their ability to improve patients' self-management and constrained by the limited time available in office visits. Whereas the results of multifaceted disease management programs that incorporate a focus on patient self-management are promising,38,53 most primary care physicians work in practice settings without such programs. Our study findings build on prior research affirming the importance of physician communication and participatory decision-making style for improving patients' health outcomes. Specifically, we found that patients' evaluations of their physicians' communication and participatory decision-making style were both strongly associated with their reported diabetes management, even after controlling for sociodemographic and health variables such as patient age and health status that have been found to influence patients' self-management.16 This finding suggests that improved patient self-management is one mechanism by which these patient-provider interaction styles may lead to the improved health outcomes found in prior studies.
Comparing patients' perceptions of these two provider styles, we found that patients' evaluations of how well their physicians provided information on their illness and treatment were more strongly associated with diabetes self-management than a participatory decision-making style. This was true both for overall self-management and for patients' management of the 5 separate domains of diabetes self-care. This finding does not imply that a participatory decision-making style is unimportant, but it does suggest that perhaps the most critical pathway may be its impact of facilitating information exchange and overall communication. Several recent studies have focused on patients' ratings of their providers' participatory decision-making styles (using the same scale as that used in this study: PDMstyle) as a marker of differential treatment of different sociodemographic groups in medical care.42,50 For example, Cooper-Patrick et al. found that African-American patients rated their physicians' decision-making style as less participatory than did white patients.42 However, this study did not simultaneously assess ratings of providers' provision of information. Our findings suggest that patients' perceptions of information provision may be an equally or even more important dimension of patient-provider relations than participatory decision-making style for patients' disease management and health outcomes. Future studies should assess whether the relative importance of these two provider styles may vary for different populations, as well as explore other features of patient-provider relations that may contribute to disparities in care processes and outcomes.
Another important practical implication of this finding stems from the recognition of the need for physicians to balance multiple, often competing priorities in the limited time available in office visits. Kaplan et al.50 found that a major predictor of PDMstyle was length of office visit, with higher PDMstyle ratings for visits of 21 to 30 minutes, concluding that visits of at least 20 minutes may be required to involve patients effectively in treatment decisions. Although our findings should be considered preliminary, they suggest that, in the face of time limitations, providing certain populations of patients with as complete information as possible on their illness and treatment alternatives may enhance their management of their illnesses more than increased sharing of the medical decisions per se. Numerous studies have documented patients' unmet desires for more information from their physicians, and patients have been shown to be less effective in information seeking during visits of less than 18 minutes.43,54–56 As many as 50% of patients leave an office visit not knowing what they are supposed to do to take care of themselves.43 Some research suggests that less than 1 minute of a twenty-minute physician visit is spent giving patients any information at all.57
Of note, this study population was composed predominantly of male, elderly patients. Our findings on the relative importance of provision of information may reflect a better match between many of these patients' preferences for participation and provider style. While this study did not elicit respondents' preferences for participation, in other studies age has been the only characteristic consistently associated with desire for participation in medical decision making, with older patients expressing less desire to participate.28,39,58 We are not aware of any studies exploring the extent to which the match between patients' desire for participation and their evaluation of their physicians' participatory decision making may influence their health behaviors or outcomes. Such an association would further argue for physicians explicitly assessing patients' desires to participate in medical decision making as a routine part of establishing a therapeutic relationship. In randomized controlled trials of interventions to increase patient participation, patients in the experimental group were more effective in obtaining information from their physicians after intervention than were controls.29 In our study sample, it may be that those patients who rated their physicians higher on providing information were more effective in eliciting information, regardless of whether they felt that their physicians were actively involving them in treatment decisions. By providing more information, physicians provide an essential base on which their patients can make their own decisions about their treatment priorities.
Our third key finding was that patients who rated their physicians as providing more information and involving them more in decision making had significantly better self-reported understanding of their diabetes care, and it was patient understanding that had the strongest independent effect on self-management. This suggests that PCOM and PDMstyle enhance self-management through increased patient understanding, perhaps by increasing self-confidence in self-care abilities and knowledge (self-efficacy). Some researchers also postulate that involving patients in decision making should lead to better self-management by increasing patient motivation and engagement in treatment.44 We were not able to test this hypothesis directly. However, if PDMstyle did act principally by increasing motivation in this sample, we would expect PDMstyle to have had a strong independent effect on self-management in the combined model, which it did not.
There are limitations to this study. Most important, it is a cross-sectional study. Longitudinal studies are necessary to establish the causal relations among the associations seen in this study. A longitudinal analysis would be important to understand better the relationship between provider communication and participatory decision-making style. For example, it is possible that participatory decision making could lead to changes in understanding and self-management over time, whereas communication carries more variance in these outcomes in the cross section. Second, all measures were based on self-report. Accordingly, we cannot be certain whether physicians' differences in style led to better reported self-management or those with better self-management perceived their physicians differently. Of note, however, at least 1 study showed that physicians' independently rated communication style during office visits corresponded with questionnaire-based patient reports of PDMstyle.59 Similarly, respondents' understanding of diabetes care was based on their own assessment, rather than on an evaluation of their actual knowledge. On this point, it is equally significant if patients' self-reported understanding served as a marker for confidence in their understanding, or “self-efficacy,” since this has also been associated with patients' self-management of a wide range of chronic conditions.20,36 Third, as noted above, the results of this study may not be generalizable to younger or predominantly female populations. Fourth, we examined reported self-management as the outcome measure, rather than a medical outcome such as glucose control or quality-of-life measure. Most studies of the effects of increased patient participation have used physiological measures of disease control and self-reported functional and health status as outcome measures. Prior research suggests that supporting patient involvement in treatment decisions may promote quality of life to a greater extent than self-management.40 Future longitudinal studies should further examine the link between reported self-management and disease-specific intermediate or downstream outcomes.35 Finally, this study evaluated the effects of provider styles in office visits, rather than in comprehensive disease management programs in which both information provision and patient involvement in setting treatment goals and strategies are likely of a much higher magnitude and intensity than can occur in standard practice.3,37,38 Exploring the relationships among the variables we studied in the context of such programs would be a fruitful area for future research.
This study, taken together with previous research on self-management, has implications both for individual physicians and for the organization of medical care. On an individual level, the ability to provide clear information to patients on their disease and treatment options and to determine their desire to participate in medical decisions should be considered a necessary clinical skill.43 As important, care should be structured to maximize the exchange of information to facilitate patients' self-management.31,53,60,61 At a minimum, such care necessitates adequate time for office visits for those with chronic illnesses to allow for effective communication and discussion,43 as well as mechanisms to ensure appropriate follow-up for patients and intervals between visits.62 Measures to promote better physician communication and patient understanding of diabetes care should improve patients' self-management and, thereby, health outcomes.
Acknowledgments
The authors thank Joel Howell for his thoughtful suggestions on an earlier version of this manuscript. We also thank Mary Hogan for expert project management and Jill Baker for carefully coding survey responses.
This work was supported by The Department of Veterans Affairs Office of Quality and Performance, the VA Health Services Research and Development Program (Grant DIS-99221-1), and The Robert Wood Johnson Foundation. Dr. Kerr is a VA HSR&D Career Development Awardee.
The views expressed herein do not necessarily represent those of The Robert Wood Johnson Foundation or The Department of Veterans Affairs.
Footnotes
*
As per Clark et al, self-management or self-care in the context of chronic diseases refers to a set of skilled behaviors to manage one's illness. These include: “1) engaging in activities that promote health, build physiologic reserve, and prevent adverse sequelae; 2) interacting with health care providers and adhering to recommended treatment protocols; 3) monitoring physical and emotional states and making appropriate management decisions on the basis of the results of self-monitoring; and 4) managing the effects of illness on the patient's ability to function in important roles and on emotions, self-esteem, and relationships with others.”20 This study focuses on the first two of these skilled behaviors.
REFERENCES
- 1.Glasgow RE, Wagner EH, Kaplan RM, Vinicor F, Smith L, Norman J. If diabetes is a public health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;21:159–70. doi: 10.1007/BF02908297. [DOI] [PubMed] [Google Scholar]
- 2.Etzwiler DD. Chronic care: a need in search of a system. Diabetes Educ. 1997;23:569–73. doi: 10.1177/014572179702300509. [DOI] [PubMed] [Google Scholar]
- 3.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [PubMed] [Google Scholar]
- 4.The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342:381–9. doi: 10.1056/NEJM200002103420603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–65. [PubMed] [Google Scholar]
- 7.United Kingdom Prospective Diabetes Study (UKPDS) Relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years. BMJ. 1995;310:83–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Pyorala K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) Diabetes Care. 1997;20:614–20. doi: 10.2337/diacare.20.4.614. [DOI] [PubMed] [Google Scholar]
- 9.Harris MI. Health care and health status and outcomes for patients with type 2 diabetes. Diabetes Care. 2000;23:754–8. doi: 10.2337/diacare.23.6.754. [DOI] [PubMed] [Google Scholar]
- 10.Glasgow RE, Hampson SE, Strycker LA, Ruggiero L. Personal-model beliefs and social-environmental barriers related to diabetes self-management. Diabetes Care. 1997;20:556–61. doi: 10.2337/diacare.20.4.556. [DOI] [PubMed] [Google Scholar]
- 11.Lorenz RA, Bubb J, Davis D, et al. Changing behavior. Practical lessons from the diabetes control and complications trial. Diabetes Care. 1996;19:648–52. doi: 10.2337/diacare.19.6.648. [DOI] [PubMed] [Google Scholar]
- 12.Glasgow RE, Strycker LA. Preventive care practices for diabetes management in two primary care samples. Am J Prev Med. 2000;19:9–14. doi: 10.1016/s0749-3797(00)00157-4. [DOI] [PubMed] [Google Scholar]
- 13.Hunt LM, Pugh J, Valenzuela M. How patients adapt diabetes self-care recommendations in everyday life. J Fam Pract. 1998;46:207–15. [PubMed] [Google Scholar]
- 14.McNabb WL. Adherence in diabetes: can we define it and can we measure it? Diabetes Care. 1997;20:215–8. doi: 10.2337/diacare.20.2.215. [DOI] [PubMed] [Google Scholar]
- 15.Lutfey KE, Wishner WJ. Beyond “compliance” is “adherence”. Improving the prospect of diabetes care. Diabetes Care. 1999;22:635–9. doi: 10.2337/diacare.22.4.635. [DOI] [PubMed] [Google Scholar]
- 16.Kravitz RL, Hays RD, Sherbourne CD, et al. Recall of recommendations and adherence to advice among patients with chronic medical conditions. Arch Intern Med. 1993;153:1869–78. [PubMed] [Google Scholar]
- 17.Rosenstock IM. Enhancing patient compliance with health recommendations. J Pediatr Health Care. 1988;2:67–72. doi: 10.1016/0891-5245(88)90169-1. [DOI] [PubMed] [Google Scholar]
- 18.Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26:597–604. doi: 10.1177/014572170002600405. [DOI] [PubMed] [Google Scholar]
- 19.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 20.Clark NM, Gong M. Management of chronic disease by practitioners and patients: are we teaching the wrong things? BMJ. 2000;320:572–5. doi: 10.1136/bmj.320.7234.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holman H, Lorig K. Patients as partners in managing chronic disease. Partnership is a prerequisite for effective and efficient health care. BMJ. 2000;320:526–7. doi: 10.1136/bmj.320.7234.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA. 1996;275:152–6. [PubMed] [Google Scholar]
- 24.Glasgow RE, Anderson RM. In diabetes care, moving from compliance to adherence is not enough. Something entirely different is needed. Diabetes Care. 1999;22:2090–2. doi: 10.2337/diacare.22.12.2090. [DOI] [PubMed] [Google Scholar]
- 25.Laine C, Caro JF. Preventing complications in diabetes mellitus: the role of the primary care physician. Med Clin North Am. 1996;80:457–74. doi: 10.1016/s0025-7125(05)70448-x. [DOI] [PubMed] [Google Scholar]
- 26.DiMatteo MR. The physician-patient relationship: effects on the quality of health care. Clin Obstet Gynecol. 1994;37:149–61. doi: 10.1097/00003081-199403000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102:520–8. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 28.Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz RL. Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med. 1992;15:447–68. doi: 10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- 29.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):110S–127S. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 30.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–51. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 32.Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment. Results of a randomized controlled trial. Diabetes Care. 1995;18:943–9. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 33.Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 34.Clark NM, Janz NK, Dodge JA, et al. Changes in functional health status of older women with heart disease: evaluation of a program based on self-regulation. J Gerontol B Psychol Sci Soc Sci. 2000;55:117S–26S. doi: 10.1093/geronb/55.2.s117. [DOI] [PubMed] [Google Scholar]
- 35.Hays RD, Kravitz RL, Mazel RM, et al. The impact of patient adherence on health outcomes for patients with chronic disease in the Medical Outcomes Study. J Behav Med. 1994;17:347–60. doi: 10.1007/BF01858007. [DOI] [PubMed] [Google Scholar]
- 36.Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Educ Behav. 1999;26:72–89. doi: 10.1177/109019819902600107. [DOI] [PubMed] [Google Scholar]
- 37.Berger M, Muhlhause I. Diabetes care and patient-oriented outcomes. JAMA. 1999;281:1676–8. doi: 10.1001/jama.281.18.1676. [DOI] [PubMed] [Google Scholar]
- 38.Olivarius N, Beck-Neilson H, Andreasen AH, Hoder M, Pedersen PA. Randomized controlled trial of structured personal care of type 2 diabetes mellitus. BMJ. 2001;323:1–9. doi: 10.1136/bmj.323.7319.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Golin CE, DiMatteo MR, Gelberg L. The role of patient participation in the doctor visit. Implications for adherence to diabetes care. Diabetes Care. 1996;19:1153–64. doi: 10.2337/diacare.19.10.1153. [DOI] [PubMed] [Google Scholar]
- 40.Senecal C, Nouwen A, White D. Motivation and dietary self-care in adults with diabetes: are self-efficacy and autonomous self-regulation complementary or competing constructs? Health Psychol. 2000;19:452–7. doi: 10.1037//0278-6133.19.5.452. [DOI] [PubMed] [Google Scholar]
- 41.Kaplan SH, Greenfield S, Gandek B, Rogers WH, Ware JE., Jr Characteristics of physicians with participatory decision-making styles. Ann Intern Med. 1996;124:497–504. doi: 10.7326/0003-4819-124-5-199603010-00007. [DOI] [PubMed] [Google Scholar]
- 42.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 43.DiMatteo MR. The role of the physician in the emerging health care environment. West J Med. 1998;168:328–33. [PMC free article] [PubMed] [Google Scholar]
- 44.Wolpert HA, Anderson BJ. Management of diabetes: are doctors framing the benefits from the wrong perspective? BMJ. 2001;323:994–6. doi: 10.1136/bmj.323.7319.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pogach LM, Hawley G, Weinstock R, et al. Diabetes prevalence and hospital and pharmacy use in the Veterans Health Administration (1994). Use of an ambulatory care pharmacy-derived database. Diabetes Care. 1998;21:368–73. doi: 10.2337/diacare.21.3.368. [DOI] [PubMed] [Google Scholar]
- 46.Boyko EJ, Koepsell TD, Gaziano JM, Horner RD, Feussner JR. US Department of Veterans Affairs medical care system as a resource to epidemiologists. Am J Epidemiol. 2000;151:307–14. doi: 10.1093/oxfordjournals.aje.a010207. [DOI] [PubMed] [Google Scholar]
- 47.Krein SL, Hayward RA, Pogach L, BootsMiller BJ. Department of Veterans Affairs' quality enhancement research initiative for diabetes mellitus. Med Care. 2000;38(6)(Suppl 1):I38S–148S. doi: 10.1097/00005650-200006001-00005. [DOI] [PubMed] [Google Scholar]
- 48.Goodall TA, Halford WK. Self-management of diabetes mellitus: a critical review. Health Psychol. 1991;10:1–8. doi: 10.1037//0278-6133.10.1.1. [DOI] [PubMed] [Google Scholar]
- 49.Clement S. Diabetes self-management education. Diabetes Care. 1995;18:1204–14. doi: 10.2337/diacare.18.8.1204. [DOI] [PubMed] [Google Scholar]
- 50.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style. Results from the Medical Outcomes Study. Med Care. 1995;33:1176–87. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 51.Hayward RA, Manning WG, Kaplan SH, Wagner EH, Greenfield S. Starting insulin therapy in patients with type 2 diabetes: effectiveness, complications, and resource utilization. JAMA. 1997;278:1663–9. [PubMed] [Google Scholar]
- 52.Gorsuch RL. Factor Analysis. 2nd Ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. [Google Scholar]
- 53.Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27:63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- 54.Beisecker AE, Beisecker TD. Patient information-seeking behaviors when communicating with doctors. Med Care. 1990;28:19–28. doi: 10.1097/00005650-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 55.Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Arch Intern Med. 1996;156:1414–20. [PubMed] [Google Scholar]
- 56.Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? JAMA. 1984;252:2990–4. [PubMed] [Google Scholar]
- 57.Waitzkin H, Stoeckle JD. The communication of information about illness. Clinical, sociological, and methodological considerations. Adv Psychosom Med. 1972;8:180–215. doi: 10.1159/000393131. [DOI] [PubMed] [Google Scholar]
- 58.Mansell D, Poses RM, Kazis L, Duefield CA. Clinical factors that influence patients' desire for participation in decisions about illness. Arch Intern Med. 2000;160:2991–6. doi: 10.1001/archinte.160.19.2991. [DOI] [PubMed] [Google Scholar]
- 59.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians' characteristics influence patients' adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993;12:93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 60.Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70:115–26. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- 61.Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320:569–72. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Glasgow RE. A practical model of diabetes management and education. Diabetes Care. 1995;18:117–26. doi: 10.2337/diacare.18.1.117. [DOI] [PubMed] [Google Scholar]