From the Triumvirate to the Ominous Octet: A New Paradigm for the Treatment of Type 2 Diabetes Mellitus (original) (raw)
Insulin resistance in muscle and liver and β-cell failure represent the core pathophysiologic defects in type 2 diabetes. It now is recognized that the β-cell failure occurs much earlier and is more severe than previously thought. Subjects in the upper tertile of impaired glucose tolerance (IGT) are maximally/near-maximally insulin resistant and have lost over 80% of their β-cell function. In addition to the muscle, liver, and β-cell (triumvirate), the fat cell (accelerated lipolysis), gastrointestinal tract (incretin deficiency/resistance), α-cell (hyperglucagonemia), kidney (increased glucose reabsorption), and brain (insulin resistance) all play important roles in the development of glucose intolerance in type 2 diabetic individuals. Collectively, these eight players comprise the ominous octet and dictate that: 1) multiple drugs used in combination will be required to correct the multiple pathophysiological defects, 2) treatment should be based upon reversal of known pathogenic abnormalities and not simply on reducing the A1C, and 3) therapy must be started early to prevent/slow the progressive β-cell failure that already is well established in IGT subjects. A treatment paradigm shift is recommended in which combination therapy is initiated with diet/exercise, metformin (which improves insulin sensitivity and has antiatherogenic effects), a thiazolidinedione (TZD) (which improves insulin sensitivity, preserves β-cell function, and exerts antiatherogenic effects), and exenatide (which preserves β-cell function and promotes weight loss). Sulfonylureas are not recommended because, after an initial improvement in glycemic control, they are associated with a progressive rise in A1C and progressive loss of β-cell function.
NATURAL HISTORY OF TYPE 2 DIABETES
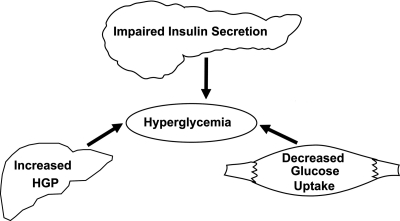
The natural history of type 2 diabetes has been well described in multiple populations (1–16) (rev. in (17,18). Individuals destined to develop type 2 diabetes inherit a set of genes from their parents that make their tissues resistant to insulin (1,16,19–24). In liver, the insulin resistance is manifested by an overproduction of glucose during the basal state despite the presence of fasting hyperinsulinemia (25) and an impaired suppression of hepatic glucose production (HGP) in response to insulin (26), as occurs following a meal (27). In muscle (19,26,28,29), the insulin resistance is manifest by impaired glucose uptake following ingestion of a carbohydrate meal and results in postprandial hyperglycemia (27). Although the origins of the insulin resistance can be traced to their genetic background (17,20), the epidemic of diabetes that has enveloped westernized countries is related to the epidemic of obesity and physical inactivity (30). Both obesity (31) and decreased physical activity (32) are insulin-resistant states and, when added to the genetic burden of the insulin resistance, place a major stress on the pancreatic β-cells to augment their secretion of insulin to offset the defect in insulin action (1,17). As long as the β-cells are able to augment their secretion of insulin sufficiently to offset the insulin resistance, glucose tolerance remains normal (33). However, with time the β-cells begin to fail and initially the postprandial plasma glucose levels and subsequently the fasting plasma glucose concentration begin to rise, leading to the onset of overt diabetes (1–4,12,17,18,34). Collectively, the insulin resistance in muscle and liver and β-cell failure have been referred to as the triumvirate (1) (Fig. 1). The resultant hyperglycemia and poor metabolic control may cause a further decline in insulin sensitivity, but it is the progressive β-cell failure that determines the rate of disease progression.
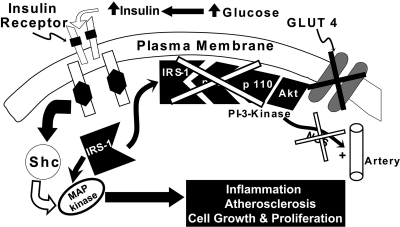
FIG. 1.
Pathogenesis of type 2 diabetes: the triumvirate. Insulin resistance in muscle and liver and impaired insulin secretion represent the core defects in type 2 diabetes (1). See text for a more detailed explanation.
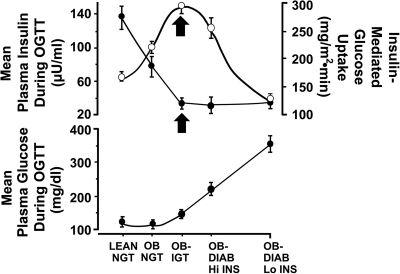
The natural history of type 2 diabetes described above (1) is depicted by a prospective study carried out by Felber and colleagues in Lausanne, Switzerland (35) (Fig. 2). Although the study was originally cross-sectional in nature, subjects were followed up for 6 years and shown to progress from one category of glucose intolerance to the next. All subjects had a euglycemic insulin clamp to measure tissue sensitivity to insulin and an oral glucose tolerance test (OGTT) to provide an overall measure of glucose homeostasis and β-cell function. In lean subjects with normal glucose tolerance (NGT), the mean plasma glucose and insulin concentrations during the OGTT were 115 mg/dl and 62 μU/ml, while the mean rate of insulin-stimulated glucose disposal (measured with a 40 mU/m2 per min euglycemic insulin clamp) was 265 mg/m2 per min. Obesity was associated with a 29% decline in insulin sensitivity, but glucose tolerance remained perfectly normal because of the compensatory increase in insulin secretion. With time the obese NGT individuals progressed to IGT in association with a further 28% reduction in insulin sensitivity (total decrease = 57% from NGT to IGT). However, the rise in plasma glucose concentration was quite modest because of a further compensatory increase in insulin secretion. However, people with IGT are in a very precarious position. They are maximally or near-maximally insulin resistant, and their β-cells are functioning at less than maximum capacity. With time the β-cells cannot continue to produce these very large amounts of insulin and the obese IGT individual progresses to overt diabetes. The decline in glucose tolerance is associated with a marked decrease in insulin secretion without further change in insulin sensitivity (Fig. 2). This characteristic rise in insulin response to insulin resistance and hyperglycemia, followed by a subsequent decline, has been referred to as Starling's curve of the pancreas (1). This natural history of type 2 diabetes has been demonstrated in many prospective studies carried out in many diverse ethnic populations (1–18,36,37). Although the relative contributions of insulin resistance and β-cell failure to the development of type 2 diabetes may differ in different ethnic groups (38), the onset and pace of β-cell failure determines the rate of progression of hyperglycemia.
FIG. 2.
Natural history of type 2 diabetes. The plasma insulin response (○) depicts the classic Starling's curve of the pancreas (1). See text for a more detailed explanation. ●, insulin-mediated glucose uptake (top panel).
β-CELL FUNCTION
Although the plasma insulin response to the development of insulin resistance typically is increased during the natural history of type 2 diabetes (Fig. 2), this does not mean that the β-cell is functioning normally. To the contrary, recent studies from our group have demonstrated that the onset of β-cell failure occurs much earlier and is more severe than previously appreciated. In the San Antonio Metabolism (SAM) study and the Veterans Administration Genetic Epidemiology Study (VAGES), we examined a large number of subjects with NGT (n = 318), IGT (n = 259), and type 2 diabetes (n = 201) (39–42). All subjects had an OGTT with plasma glucose and insulin concentrations measured every 15 min to evaluate overall glucose tolerance and β-cell function and a euglycemic insulin clamp to measure insulin sensitivity. It now is recognized that simply measuring the plasma insulin response to a glucose challenge does not provide a valid index of β-cell function (43). The β-cell responds to an increment in glucose (ΔG) with an increment in insulin (ΔI) (43). Thus, a better measure of β-cell function is ΔI/ΔG. However, the β-cell also is keenly aware of the body's sensitivity to insulin and adjusts its secretion of insulin to maintain normoglycemia (33,43–45). Thus, the gold standard for measuring β-cell function is the insulin secretion/insulin resistance (ΔI/ΔG ÷ IR), or so called disposition, index. Note that insulin resistance is the inverse of insulin sensitivity. Supplemental Fig. A1 (available in an online appendix at http://diabetes.diabetesjournals.org/cgi/content/full/db09-9028/DC1) displays the glucose area under the curve (AUC) and insulin AUC in NGT, IGT, and type 2 diabetic subjects who participated in VAGES and SAM. In the right panel, the typical inverted U-shaped or Starling's curve of the pancreas for the plasma insulin response is evident. Although subjects with IGT have an increase in the absolute plasma insulin concentration, this should not be interpreted to mean that the β-cells in these individuals are functioning normally.
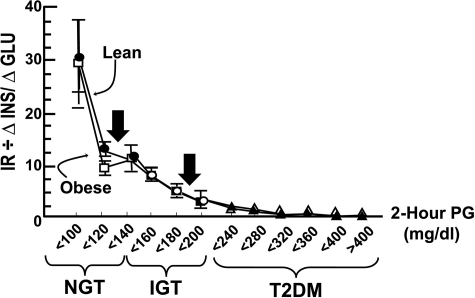
Figure 3 depicts the insulin secretion/insulin resistance index (ΔI/ΔG ÷ IR) in NGT, IGT, and type 2 diabetic subjects as a function of the 2-h plasma glucose concentration during the OGTT. If a 2-h plasma glucose <140 mg/dl is considered to represent “normal” glucose tolerance, subjects in the upper tertile (2-h PG = 120–139 mg/dl) have lost two-thirds of their β-cell function (see arrow in Fig. 3). Most disturbingly, subjects in the upper tertile of IGT (2-h PG = 180–199 mg/dl) have lost 80–85% of their β-cell function (see second arrow in Fig. 3). Although not commented upon, similar conclusions can be reached from data in previous publications (2,3,7,15). The therapeutic implications of these findings are readily evident. By the time that the diagnosis of diabetes is made, the patient has lost over 80% of his/her β-cell function, and it is essential that the physician intervene aggressively with therapies known to correct known pathophysiological disturbances in β-cell function.
FIG. 3.
Insulin secretion/insulin resistance (disposition) index (ΔI/ΔG ÷ IR) in individuals with NGT, IGT, and type 2 diabetes (T2DM) as a function of the 2-h plasma glucose (PG) concentration in lean and obese subjects (39–42).
In biomedical phenomena, most reactions take place as a log function. Figure 4 depicts the natural log of the 2-h plasma glucose concentration during the OGTT as a function of the natural log of the insulin secretion/insulin resistance (β-cell function) index. These two variables are strongly and linearly related with an r value of 0.91 (P < 0.00001). There are no cut points that distinguish NGT from IGT from type 2 diabetes. Rather, glucose intolerance is a continuum, and subjects simply move up and down this curve as a function of the insulin secretion/insulin resistance index. Therefore, the current diagnostic criteria (46) for IGT and type 2 diabetes are quite arbitrary and, like plasma cholesterol, glucose tolerance should be viewed as a continuum of risk. The higher the 2-h plasma glucose concentration, even within the range of IGT, the greater is the risk for microvascular complications (see subsequent discussion).
FIG. 4.
Natural log of the 2-h plasma glucose (PG) concentration versus natural log of the insulin secretion/insulin resistance index (measure of β-cell function) (39–42). T2DM, type 2 diabetes.
Even more ominous are the observations of Butler et al. (47). In a postmortem analysis, these investigators quantitated relative β-cell volume and related it to the fasting plasma glucose concentration. As individuals progressed from NGT to impaired fasting glucose (IFG), there was a 50% decline in β-cell volume, suggesting a significant loss of β-cell mass long before the onset of type 2 diabetes. With the progression to overt diabetes, there was a further and significant loss of β-cell volume. Although β-cell volume should not be viewed to be synonymous with β-cell mass, these results suggest that significant loss of β-cell mass occurs long before the onset of type 2 diabetes, according to current diagnostic criteria (46).
In summary, our findings (40–42) demonstrate that, at the stage of IGT, individuals have lost over 80% of their β-cell function, while the results of Butler et al. (47) suggest that subjects with “pre-diabetes” have lost approximately half of their β-cell volume.
“PRE-DIABETES”
The recently published results of the Diabetes Prevention Program (DPP) (48) have raised further concern about the clinical implications of the term “pre-diabetes.” In the DPP, individuals who entered with a diagnosis of IGT and still had IGT 3 years later had a 7.9% incidence of background diabetic retinopathy at the time of study end. Individuals who entered the DPP with IGT but who progressed to diabetes after 3 years had a 12.6% incidence of diabetic retinopathy at the time of study end. Moreover, these IGT individuals developed diabetic retinopathy with an A1C of 5.9 and 6.1%, respectively, values much less than the current American Diabetes Association (ADA) treatment goal of 7% (49). Peripheral neuropathy also is a common finding in IGT, occurring in as many as 5–10% individuals (50,51).
In summary, individuals with IGT are maximally or near- maximally insulin resistant, they have lost 80% of their β-cell function, and they have an approximate 10% incidence of diabetic retinopathy. By both pathophysiological and clinical standpoints, these pre-diabetic individuals with IGT should be considered to have type 2 diabetes.
The clinical implications of these findings for the treatment of type 2 diabetes are that the physician must intervene early, at the stage of IGT or IFG, with interventions that target pathogenic mechanisms known to promote β-cell failure.
PATHOGENESIS OF β-CELL FAILURE (supplemental Fig. A2)
Age.
Advancing age plays an important role in the progressive β-cell failure that characterizes type 2 diabetes. Numerous studies (52–54) have demonstrated a progressive age-related decline in β-cell function. This is consistent with the well-established observation that the incidence of diabetes increases progressively with advancing age.
Genes.
β-Cell failure also clusters in families, and studies in first-degree relatives of type 2 diabetic parents and in twins have provided strong evidence for the genetic basis of the β-cell dysfunction (55–58). Impaired insulin secretion has been shown to be an inherited trait in Finnish families with type 2 diabetes with evidence for a susceptibility locus on chromosome 12 (59). Most recently, a number of genes associated with β-cell dysfunction in type 2 diabetic individuals have been described (20,60–62). Of these genes, the transcription factor TCF7L2 is best established (60,61). Studies by Groop and colleagues (63) have shown that the T-allele of single nucleotide polymorphism rs7903146 of the TCF7L2 gene is associated with impaired insulin secretion in vivo and reduced responsiveness to glucagon-like peptide 1 (GLP-1). Both the CT and TT genotypes predict type 2 diabetes in multiple ethnic groups (64). In both the Malmo and Botnia studies, presence of either the CT or TT genotype was associated with a significant reduction in the diabetes-free survival time, with odds ratios of 1.58 and 1.61, respectively (63). TCF7L2 encodes for a transcription factor involved in Wnt signaling, which plays a central role in the regulation of β-cell proliferation and insulin secretion (65).
Unfortunately, at present there are no known therapeutic interventions that can reverse either the age-related decline or genetic-related factors responsible for impaired insulin secretion. However, there are a number of causes of β-cell failure that can be reversed or ameliorated.
Insulin resistance.
Insulin resistance, by placing an increased demand on the β-cell to hypersecrete insulin, also plays an important role in the progressive β-cell failure of type 2 diabetes. Therefore, interventions aimed at enhancing insulin sensitivity are of paramount importance. The precise mechanism(s) via which insulin resistance leads to β-cell failure remain(s) unknown. It commonly is stated that the β-cell, by being forced to continuously hypersecrete insulin, eventually wears out. Although simplistic in nature, this explanation lacks a mechanistic cause. An alternate hypothesis, for which considerable evidence exists, is that the cause of the insulin resistance is also directly responsible for the β-cell failure. Thus, just as excess deposition of fat (LC-fatty acyl CoAs, diacylglycerol, and ceramide) in liver and muscle has been shown to cause insulin resistance in these organs, i.e., lipotoxicity, deposition of fat in the β-cell leads to impaired insulin secretion and β-cell failure (see subsequent discussion). Similarly, hypersecretion of islet amyloid polypeptide (IAPP), which is co-secreted in a one-to-one ratio with insulin, can lead to progressive β-cell failure (see subsequent discussion).
Lipotoxicity.
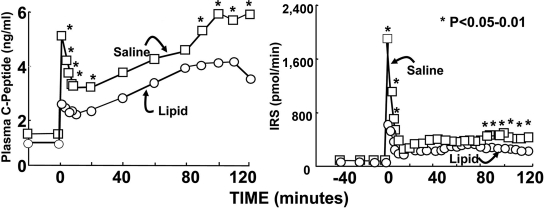
Elevated plasma free fatty acid (FFA) levels impair insulin secretion, and this has been referred to as lipotoxicity (66,67). Studies from our laboratory (24) have shown that a physiological elevation of the plasma FFA concentration for as little as 48 h markedly impairs insulin secretion in genetically predisposed individuals (Fig. 5). In this study, the normal glucose tolerant offspring of two type 2 diabetic parents received a 48-h infusion of saline or Intralipid to approximately double the plasma FFA concentration and then received a 2-h hyperglycemic (125 mg/dl) clamp. Compared with saline infusion, lipid infusion markedly impaired both the first and second phases of C-peptide release and reduced the insulin secretory rate, calculated by deconvolution of the plasma C-peptide curve. Conversely, a sustained reduction in plasma FFA concentration with acipimox in nondiabetic subjects with a strong family history of type 2 diabetes improved insulin secretion (68). In vivo studies in rodents (69–71) and in humans (72), as well as in vitro studies (73), also support an important role for lipotoxicity. Thus, when human pancreatic islets were incubated for 48 h in presence of 2 mmol/l FFA (oleate-to-palmitate ratio 2:1), insulin secretion, especially the acute insulin response, was markedly reduced. Exposure to FFA caused a marked inhibition of insulin mRNA expression, decreased glucose-stimulated insulin release, and reduction of islet insulin content (69). Rosiglitazone, a peroxisome proliferator–activated receptor (PPAR)γ agonist, prevented all of these deleterious effects of FFA (74). Consistent with these in vitro observations, we have shown that both rosiglitazone and pioglitazone markedly improve the insulin secretion/insulin resistance index in vivo in type 2 diabetic humans (75).
FIG. 5.
Effect of physiological elevation (48 h) in the plasma FFA concentration (brought about by lipid infusion) on plasma C-peptide concentration (left) and insulin secretory response (deconvolution of the palsma C-peptide curve) (right) in offspring of two type 2 diabetic parents (24).
In summary, interventions—such as weight loss and TZDs—that mobilize fat out of the β-cell would be expected to reverse lipotoxicity and preserve β-cell function.
Glucotoxicity.
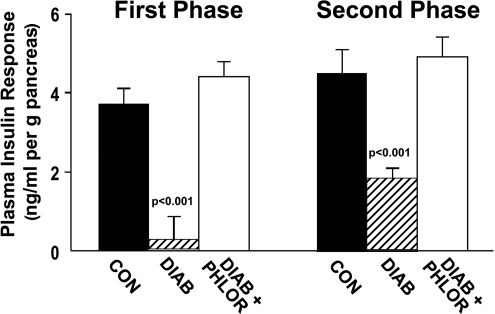
Chronically elevated plasma glucose levels also impair β-cell function, and this has been referred to as glucotoxicity (76). Studies by Rossetti et al. (77) have provided definitive proof of this concept (Fig. 6). Partially pancreatectomized diabetic rats are characterized by severe defects in both first- and second-phase insulin secretion compared with control rats. Following treatment with phlorizin, an inhibitor of renal glucose transport, the plasma glucose profile was normalized without changes in any other circulating metabolites. Normalization of the plasma glucose profile was associated with restoration of both the first and second phases of insulin secretion. In vitro studies with isolated human islets also have demonstrated that chronic exposure to elevated plasma glucose levels impairs insulin secretion (78,79). In rats, Leahy et al. (80) showed that elevation of the mean day-long plasma glucose concentration in vivo by as little as 16 mg/dl leads to a marked inhibition of glucose-stimulated insulin secretion in the isolated perfused pancreas.
FIG. 6.
First-phase (0–10 min) and second-phase (10–120 min) plasma insulin response during hyperglycemic clamp in partially pancreatectomized diabetic (DIAB) and control (CON) rats (77). PHLOR, phlorizin.
Thus, strict glycemic control is essential not only to prevent the microvascular complications of diabetes but also to reverse the glucotoxic effect of chronic hyperglycemia on the β-cells (80–84), as well as on hepatic and muscle insulin resistance.
IAPP.
Hypersecretion of IAPP and amyloid deposition within the pancreas have also been implicated in the progressive β-cell failure of type 2 diabetes (85,86). Although convincing evidence for a pathogenic role of IAPP exists in rodents (87,88), the natural history of pancreatic amylin deposition in humans has yet to be defined (89).
To address this issue, Chavez and colleagues (90,91) examined the relationship between pancreatic amylin deposition and β-cell function in 150 baboons spanning a wide range of glucose tolerance. Since the baboon genome shares more than 98% homology with the human genome, results in baboons are likely to be pertinent to those in humans (92). As the relative amyloid area of the pancreatic islets increased from <5.5% to >51%, there was a progressive decline in the log of HOMA-β. The decline in β-cell function was strongly correlated with the increase in fasting plasma glucose concentration. Studies by Butler and colleagues (93,94) have also provided additional evidence for a β-cell toxic effect for the soluble IAPP fibrils.
Because amylin is secreted in a one-to-one ratio with insulin (95,96) and IAPP oligomers are toxic (89,93,94), interventions that improve insulin sensitivity, i.e., TZDs/metformin/weight loss, by leading to a reduction in insulin secretion, would be expected to preserve β-cell function on a long-term basis. Of note, rosiglitazone has been shown to protect human islets against human IAPP toxicity by a phosphatidylinositol (PI) 3-kinase–dependent pathway (97).
Incretins.
Abnormalities in the incretin axis have been shown to play an important role in the progressive β-cell failure of type 2 diabetes. GLP-1 and glucose-dependent insulinotrophic polypeptide (also called gastric inhibitory polypeptide [GIP]) account for ∼90% of the incretin effect (98–100). In type 2 diabetes, there is a deficiency of GLP-1 (98–100) and resistance to the action of GIP (102–105). The deficiency of GLP-1 can be observed in individuals with IGT and worsens progressively with progression to type 2 diabetes (101). In addition to deficiency of GLP-1, there is resistance to the stimulatory effect of GLP-1 on insulin secretion (106,107). In contrast to GLP-1, plasma levels of GIP are elevated in type 2 diabetes, yet circulating plasma insulin levels are reduced (108). This suggests that there is β-cell resistance to the stimulatory effect of GIP on insulin secretion, and this, in fact, has been demonstrated (105). Of note, recent studies have shown that tight glycemic control can restore the β-cells' insulin secretory response to GIP (109). Thus, β-cell resistance to GIP is another manifestation of glucotoxicity.
Because GLP-1 deficiency occurs early in the natural history of type 2 diabetes, it follows that GLP-1 replacement therapy is a logical choice to restore the deficient insulin response that is characteristic of the diabetic condition.
Summary: β-cell dysfunction and development of type 2 diabetes.
In summary, although insulin resistance in liver and muscle are well established early in the natural history of the disease, type 2 diabetes does not occur in the absence of progressive β-cell failure.
INSULIN RESISTANCE
Both the liver and muscle are severely resistant to insulin in individuals with type 2 diabetes (rev. in (1,17,18). However, when discussing insulin resistance, it is important to distinguish what is responsible for the insulin resistance in the basal or fasting state and what is responsible for the insulin resistance in the insulin-stimulated state.
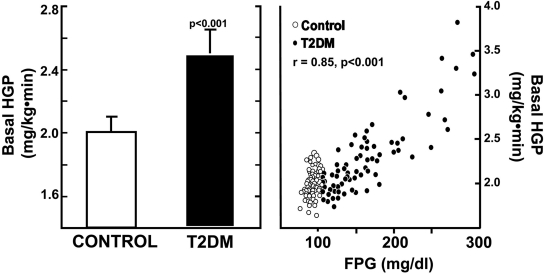
Liver.
The brain has an obligate need for glucose and is responsible for ∼50% of glucose utilization under basal or fasting conditions (110). This glucose demand is met primarily by glucose production by the liver and to a smaller extent the kidneys (110). Following an overnight fast, the liver of nondiabetic individuals produces glucose at the rate of ∼2 mg/kg per min (1,25) (Fig. 7). In type 2 diabetic individuals, the rate of basal HGP is increased, averaging ∼2.5 mg/kg per min (1,25) (Fig. 7). In an average 80-kg person, this amounts to the addition of an extra 25–30 g of glucose to the systemic circulation every night. As shown in Fig. 7, control subjects cluster with a fasting plasma glucose concentration of ∼85–90 mg/dl, and their rate of HGP averages ∼2 mg/kg per min. In type 2 diabetic subjects, as the rate of basal HGP rises, so also does the fasting plasma glucose concentration, and these two variables are strongly correlated with an R value of 0.847 (P < 0.001). This overproduction of glucose by the liver occurs in the presence of fasting plasma insulin levels that are increased 2.5- to 3-fold, indicating severe resistance to the suppressive effect of insulin on HGP. Similar observations have been made by others (27,110–116). The increase in basal HGP is explained entirely by an increase in hepatic gluconeogenesis (117–119). In addition to hepatic insulin resistance, multiple other factors contribute to accelerated rate of HGP including: 1) increased circulating glucagon levels and enhanced hepatic sensitivity to glucagon (120–122); 2) lipotoxicity leading to increased expression and activity of phosphoenolpyruvate carboxykinase and pyruvate carboxylase (123), the rate-limiting enzymes for gluconeogenesis; and 3) glucotoxicity, leading to increased expression and activity of glucose-6-phosphatase, the rate-limiting enzyme for glucose escape from the liver (124).
FIG. 7.
Basal HGP (left) in control and type 2 diabetic (T2DM) subjects. The relationship between basal HGP and fasting plasma glucose (FPG) concentration is shown on the right (1,25).
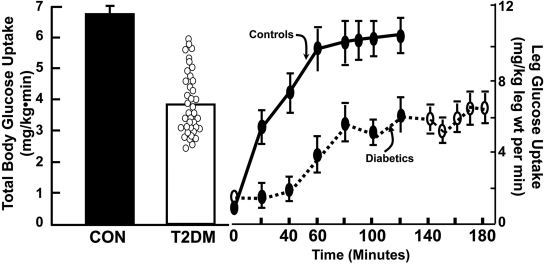
Muscle.
Using the euglycemic insulin clamp technique (125) in combination with tritiated glucose to measure total body glucose disposal, we (1,18,19,26,28,29,40,111,126) and others (12,16,44,45,116,127–130) conclusively have demonstrated that lean type 2 diabetic individuals are severely resistant to insulin compared with age-, weight-, and sex-matched control subjects (Fig. 8). Employing femoral arterial and venous catheterization in combination with the insulin clamp, we further demonstrated that muscle insulin resistance could account for over 85–90% of the impairment in total body glucose disposal in type 2 diabetic subjects (19,28) (Fig. 8). Even though the insulin clamp was extended for an additional hour in diabetic subjects to account for the delay in onset of insulin action, the rate of insulin-stimulated glucose disposal remained 50% less than in control subjects. A similar defect in insulin-stimulated muscle glucose uptake in type 2 diabetic subjects has been demonstrated by others (131–133).
FIG. 8.
Insulin-stimulated total body glucose uptake (left) and insulin-stimulated leg glucose uptake (right) in control (CON) and type 2 diabetic (T2DM) subjects (28,29).
In type 2 diabetic subjects we, as well as others, have documented the presence of multiple intramyocellular defects in insulin action (rev. in (17,18,126), including impaired glucose transport and phosphorylation (19,133–137), reduced glycogen synthesis (111,138,139), and decreased glucose oxidation (26,140–142). However, more proximal defects in the insulin signal transduction system play a paramount role in the muscle insulin resistance (126,143).
Insulin signal transduction.
For insulin to work, it must first bind to and then activate the insulin receptor by phosphorylating key tyrosine residues on the β chain (126,144–146) (supplemental Fig. A3). This results in the translocation of insulin receptor substrate (IRS)-1 to the plasma membrane, where it interacts with the insulin receptor and also undergoes tyrosine phosphorylation. This leads to the activation of PI 3-kinase and Akt, resulting in glucose transport into the cell, activation of nitric oxide synthase with arterial vasodilation (147–149), and stimulation of multiple intracellular metabolic processes.
Studies from our laboratory were the first to demonstrate in humans that the ability of insulin to tyrosine phosphorylate IRS-1 was severely impaired in lean type 2 diabetic individuals (126,143,150), in obese normal glucose tolerant individuals (143), and in the insulin-resistant, normal glucose tolerant offspring of two type 2 diabetic parents (151,152) (Fig. 9). Similar defects have been demonstrated by others in human muscle (21,23,153–156). This defect in insulin signaling leads to decreased glucose transport, impaired release of nitric oxide with endothelial dysfunction, and multiple defects in intramyocellular glucose metabolism.
FIG. 9.
Relationship between impaired insulin signal transduction and accelerated atherogenesis in insulin-resistant subjects, i.e., type 2 diabetes and obesity (126,143).
In contrast to the severe defect in IRS-1 activation, we have shown that the mitogen-activated protein (MAP) kinase pathway, which can be activated by Shc, is normally responsive to insulin (143) (Fig. 9). The MAP kinase pathway, when stimulated, leads to the activation of a number of intracellular pathways involved in inflammation, cellular proliferation, and atherosclerosis (157–159). Thus, the block at the level of IRS-1 impairs glucose transport into the cell and the resultant hyperglycemia stimulates insulin secretion. Because the MAP kinase pathway retains its sensitivity to insulin (143,159,160), this causes excessive stimulation of this pathway and activation of multiple intracellular pathways involved in inflammation and atherogenesis. This, in part, explains the strong association between insulin resistance and atherosclerotic cardiovascular disease in nondiabetic, as well as in type 2 diabetic, individuals (161–166).
As shown by Miyazaki et al. (150) in our laboratory, there is only one class of oral antidiabetic drugs—the TZDs—that simultaneously augment insulin signaling through IRS-1 and inhibit the MAP kinase pathways. These molecular observations help to explain the recent results from the CHICAGO (Carotid Intima-Media Thickness in Atherosclerosis Using Pioglitazone) (167) and PERISCOPE (Pioglitazone Effect on Regression of Intravascular Sonographic Coronary Obstruction Prospective Evaluation) (168) studies, in which pioglitazone was shown to halt the progression of carotid intima-media thickness and coronary atherosclerosis, respectively, in type 2 diabetic patients. Consistent with these anatomical studies, pioglitazone in the PROactive study (169) was shown to decrease (P = 0.027) the second principal end point of death, myocardial infarction, and stroke by 16%. The primary composite end point was reduced by 10% but did not reach statistical significance because of an increase in leg revascularization, which is not an end point in most cardiovascular studies. This is not surprising since gravity, not lipids or blood pressure, is the most important risk for peripheral vascular disease.
Route of glucose administration: oral vs. intravenous.
The euglycemic insulin clamp, by maintaining plasma glucose and insulin levels constant, has become the gold standard for quantitating insulin sensitivity. However, the normal route of glucose administration in every day life is via the gastrointestinal tract. Using a double tracer technique (1-14C-glucose orally and 3-3H-glucose intravenously) in combination with hepatic vein catheterization, we set out to examine the disposal of oral versus intravenous glucose in healthy, normal glucose tolerant and type 2 diabetic subjects (170–174).
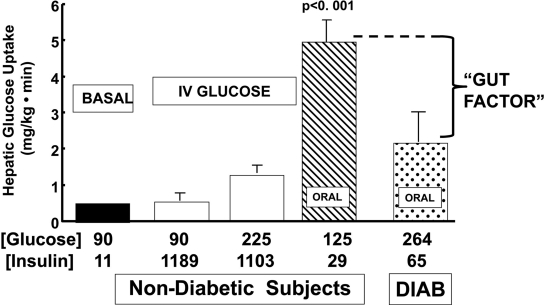
Under basal conditions, with fasting plasma glucose and insulin concentrations of 90 mg/dl and 11 mU/ml, respectively, the splanchnic tissues, which primarily reflect the liver, take up glucose at the rate of 0.5 mg/kg per min (Fig. 10). When insulin was administered intravenously to raise the plasma insulin concentration to 1,189 μU/ml, while maintaining euglycemia, in subjects with NGT, no stimulation of hepatic glucose uptake was observed. When insulin was infused with glucose to elevate both glucose and insulin levels, hepatic glucose uptake increased, but only in proportion to the increase in plasma glucose concentration, despite plasma insulin concentrations in excess of 1,000 μU/ml. In contrast, when glucose was administered orally, hepatic glucose uptake increased 4.5-fold, despite plasma insulin and glucose concentrations that were much lower than with intravenous glucose plus insulin administration (Fig. 10). When the same oral glucose load was administered to type 2 diabetic individuals, despite higher plasma glucose and insulin concentrations than in nondiabetic subjects, hepatic glucose uptake was reduced by >50%. Thus, individuals with type 2 diabetes lack the gut factor that is responsible for augmenting hepatic glucose uptake following glucose ingestion.
FIG. 10.
Hepatic glucose uptake in nondiabetic and diabetic (DIAB) subjects as a function of plasma glucose and insulin concentrations and route of glucose administration (170–174).
Summary: pathogenesis.
In summary, impaired insulin secretion, decreased muscle glucose uptake, increased HGP, and decreased hepatic glucose uptake all contribute to the glucose intolerance in type 2 diabetic individuals.
DYSHARMONIOUS QUARTET (SUPPLEMENTAL FIG. A4)
The last decade has taught us that the fat cell also plays a pivotal role in the pathogenesis of type 2 diabetes. Collectively, the fat cell and his three friends—the muscle, liver, and β-cell—comprise the harmonious quartet, or perhaps more appropriately, the dysharmonious quartet, since together they sing a very bad tune for the diabetic patient. Considerable evidence implicates deranged adipocyte metabolism and altered fat topography in the pathogenesis of glucose intolerance in type 2 diabetes (17,26,68,127,175–178): 1) Fat cells are resistant to insulin's antilipolytic effect, leading to day-long elevation in the plasma FFA concentration (26,140,175–179). 2) Chronically increased plasma FFA levels stimulate gluconeogenesis (180–182), induce hepatic/muscle insulin resistance (142,183–185), and impair insulin secretion (24,186). These FFA-induced disturbances are referred to as lipotoxicity. 3) Dysfunctional fat cells produce excessive amounts of insulin resistance–inducing, inflammatory, and atherosclerotic-provoking adipocytokines and fail to secrete normal amounts of insulin-sensitizing adipocytokines such as adiponectin (175,176). 4) Enlarged fat cells are insulin resistant and have diminished capacity to store fat (187,188). When adipocyte storage capacity is exceeded, lipid “overflows” into muscle, liver, and β-cells, causing muscle/hepatic insulin resistance and impaired insulin secretion (rev. in (175,176). Lipid can also overflow into arterial vascular smooth cells, leading to the acceleration of atherosclerosis.
Using 14C-palmitate in combination with the insulin clamp technique, Groop et al. (26) demonstrated that the antilipolytic effect of insulin was markedly impaired in lean type 2 diabetic subjects, as well as in obese nondiabetic subjects (140). In both type 2 diabetic (supplemental Fig. A5) and obese nondiabetic subjects, the ability of insulin to suppress the plasma FFA concentration and inhibit FFA turnover is significantly impaired compared with lean normal glucose tolerant control subjects at all plasma insulin concentrations spanning the physiological and pharmacological range.
Many investigators, including Boden, Shulman, and ourselves (181,182,185,189), have shown that a physiological elevation in the plasma FFA concentration stimulates HGP and impairs insulin-stimulated glucose uptake in liver (190) and muscle (151,182–185,189–194). As discussed earlier, we and others (24,186) have also shown that elevated plasma FFA levels inhibit insulin secretion.
Many years ago, Professor Philip Randle (195) described his now famous cycle of substrate competition, whereby elevated FFA oxidation in muscle reciprocally impaired glucose oxidation. Although there clearly is substrate competition between FFA and glucose with respect to oxidative metabolism (196,197), FFAs have been shown to have independent effects to inhibit glycogen synthase (198,199) and both glucose transport and glucose phosphorylation (192,200).
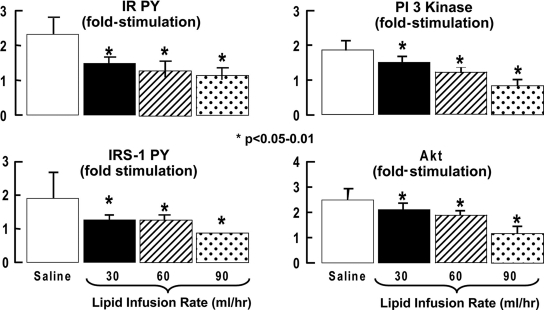
More recently, we have examined the effect of a 4-h lipid versus saline infusion on the insulin signal transduction system in healthy lean normal glucose tolerant subjects (201). Lipid was infused at three rates (30, 60, and 90 ml/h) to cause a physiological and pharmacological elevation in the plasma FFA concentration. During the saline control study, insulin increased whole-body glucose metabolism from 2.7 to 10.8 mg · kg−1 · min−1. Lipid infusion caused a dose-response decline in insulin-stimulated whole-body glucose disposal (by 22, 30, and 34%, respectively), which primarily reflects muscle. Compared with the saline control study, lipid infusion caused a dose-response inhibition of muscle insulin receptor tyrosine phosphorylation, IRS-1 tyrosine phosphorylation, PI 3-kinase activity, and Akt serine phosphorylation (Fig. 11).
FIG. 11.
Effect of lipid infusion to cause a physiological-pharmacological elevation in plasma FFA concentration on insulin signal transduction in healthy nondiabetic subjects (201). PY, phosphorylation.
After fatty acids enter the cell, they can be converted to triglycerides, which are inert, or to toxic lipid metabolites such as fatty acyl CoAs, diacylglycerol, and ceramide. Using magnetic resonance spectroscopy, we quantitated intramyocellular triglyceride content in healthy normal glucose tolerant and type 2 diabetic subjects and demonstrated that muscle lipid content was significantly increased in the diabetic group (R.A.D., unpublished data). Similar results have been reported by Petersen et al. (202). Fatty acyl CoAs, which are known to inhibit insulin signaling (203,204), were also significantly increased in muscle in diabetic subjects (205,206). Diabetic subjects were treated with pioglitazone, which increases the expression of peroxisome proliferator–activated γ coactivator 1 (PGC-1) (207). PGC-1 is the master regulator of mitochondrial biogenesis and augments the expression of multiple genes involved in mitochondrial oxidative phosphorylation (208–210). Pioglitazone reduced the intramyocellular lipid and fatty acyl CoA concentrations, and the decrement in muscle fatty acyl CoA content was closely related to the improvement in insulin-stimulated muscle glucose disposal (205). When we reduced the intramyocellular fatty acyl CoA content with acipimox, a potent inhibitor of lipolysis, a similar improvement in insulin-mediated glucose disposal was noted (206). Increased intramyocellular levels of diacylglycerol (194,211) and ceramides (212,213) have also been demonstrated in type 2 diabetic and obese nondiabetic subjects and shown to be related to the insulin resistance and impaired insulin signaling in muscle. Most recently, we demonstrated that a 48-h lipid infusion, designed to increase the plasma FFA concentration ∼1.5- to 2.0-fold, inhibited the expression of PGC1α, PGC1β, PDHA1, and multiple mitochondrial genes involved in oxidative phosphorylation in muscle (214), thus mimicking the pattern of gene expression observed in type 2 diabetic subjects and in the normal glucose tolerant, insulin-resistant offspring of two type 2 diabetic parents (215,216). Most recently, we examined the effect of palmitoyl carnitine on ATP synthesis in mitochondria isolated from muscle of normal glucose tolerant subjects (217). Low concentrations of palmitoyl carnitine (1–4 μmol/l) augmented ATP synthesis. However, palmitoyl carnitine concentrations >4 μmol/l were associated with marked inhibition of ATP synthesis and a decrease in the inner mitochondrial membrane potential, which provides the electromotive driving force for electron transport. Collectively, these findings provide strong support for lipotoxicity and adipocyte insulin resistance in the pathogenesis of type 2 diabetes.
QUINTESSENTIAL QUINTET
Although the fat cell is a worthy member of the dysharmonious quartet, the time has arrived to expand the playing field to include the gastrointestinal tissues as the fifth member of the quintessential quintet.
Glucose ingestion elicits a much greater insulin response than an intravenous glucose infusion that mimics the plasma glucose concentration profile observed with oral glucose (98–100). The great majority (>99%) of this incretin effect can be explained by two hormones: GLP-1 and GIP (98–100). As discussed earlier, GLP-1 secretion by the L-cells of the distal small intestine is deficient (98–100), while GIP secretion by the K-cells of the more proximal small intestine is increased, but there is resistance to the stimulatory effect of GIP on insulin secretion (102–105). GLP-1 also is a potent inhibitor of glucagon secretion (98–100), and the deficient GLP-1 response contributes to the paradoxical rise in plasma glucagon secretion and impaired suppression of HGP that occurs after ingestion of a mixed meal (218). Clearly, the gut is a major endocrine organ and contributes to the pathogenesis of type 2 diabetes.
Studies from our laboratory have demonstrated that in healthy normal glucose tolerant subjects, approximately one-half of the suppression of HGP following a mixed meal is secondary to inhibition of glucagon secretion, the other one-half is secondary to the increase in insulin secretion, and the insulin-to-glucagon ratio correlated strongly with the suppression of HGP during the meal (218). These studies also demonstrated that a large amount of the ingested glucose load did not appear in the systemic circulation, consistent with previous studies from our laboratory (28,170–172). This could have been the result of delayed gastric emptying, a known effect of exenatide, or an increase in splanchnic (primarily reflects liver) glucose uptake. To examine this question more directly, type 2 diabetic subjects received a 6-h meal tolerance test with the double tracer technique (1-14C-glucose orally and 3-3H-glucose intravenously) before and after 2 weeks of exenatide treatment (219). Exenatide was not given on the day of the study. The ingested glucose load was labeled with acetaminophen to follow gastric empting. Exenatide significantly reduced both the fasting and postprandial plasma glucose levels following ingestion of the meal compared with the baseline study performed prior to exenatide. The increment in insulin secretory rate divided by the increment in plasma glucose concentration increased more than twofold, demonstrating a potent stimulatory effect of exenatide on β-cell function. The increase in insulin secretion, in concert with a decline in glucagon release, led to a significant reduction in HGP following ingestion of the mixed meal. Gastric emptying was unaltered by exenatide, since the last dose of exenatide was administered more than ∼16 h prior to the meal. Neither splanchnic nor peripheral tissue glucose uptake was significantly altered. Thus, the primary effect of exenatide to improve glucose tolerance is related to the incretin's suppressive effect on HGP. Most recently, Cherrington (220) and Bergman (221) and colleagues have presented evidence in support of an effect of GLP-1 to enhance hepatic glucose uptake of ingested glucose in dogs.
SETACEOUS SEXTET
The sixth member, who establishes the setaceous sextet, is the pancreatic α-cell. Many groups, dating back to the 1970s, have demonstrated that the basal plasma glucagon concentration is elevated in type 2 diabetic individuals (119–121,222–224). The important contribution of elevated fasting plasma glucagon levels to the increased basal rate of HGP in type 2 diabetic individuals was provided by Baron et al. (122). Compared with control subjects, diabetic individuals had a markedly elevated rate of basal HGP, which correlated closely with the increase in fasting plasma glucagon concentration. Following somatostatin infusion, plasma glucagon levels declined by 44% in association with a 58% decrease in basal HGP. These results conclusively demonstrate the pivotal role of hyperglucagonemia in the pathogenesis of fasting hyperglycemia in type 2 diabetes. There also is evidence that the liver may be hypersensitive to the stimulatory effect of glucagon in hepatic gluconeogenesis (120).
In summary, drugs that inhibit glucagon secretion or block the glucagon receptor are likely to be effective in treating patients with type 2 diabetes. One such example is exenatide (225), but glucagon receptor antagonists also have been shown to be effective (226).
SEPTICIDAL SEPTET
The next, and most recent member, implicated in the pathogenesis of type 2 diabetes is the kidney who along with the muscle, liver, α-cell, β-cell, adipocyte, and gut, forms the septicidal septet.
The kidney filters ∼162 g ([glomerular filtration rate = 180 l/day] × [fasting plasma glucose = 900 mg/l]) of glucose every day. Ninty percent of the filtered glucose is reabsorbed by the high capacity SGLT2 transporter in the convoluted segment of the proximal tubule, and the remaining 10% of the filtered glucose is reabsorbed by the SGLT1 transporter in the straight segment of the descending proximal tubule (227). The result is that no glucose appears in the urine.
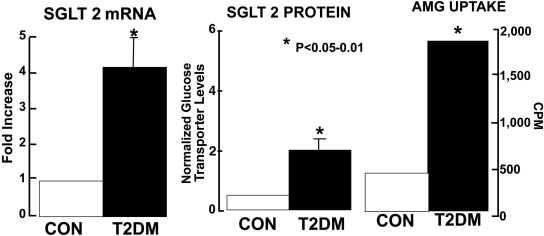
In animal models of both type 1 and type 2 diabetes, the maximal renal tubular reabsorptive capacity, or Tm, for glucose is increased (228–230). In humans with type 1 diabetes, Mogensen et al. (231) have shown that the Tm for glucose is increased. In human type 2 diabetes, the Tm for glucose has not been systematically examined. No studies in either type 1 or type 2 diabetic individuals have examined the splay in the glucose titration curve in humans. However, cultured human proximal renal tubular cells from type 2 diabetic patients demonstrate markedly increased levels of SGLT2 mRNA and protein and a fourfold increase in the uptake of α-methyl-d-glucopyranoside (AMG), a nonmetabolizeable glucose analog (232) (Fig. 12).
FIG. 12.
SGLT 2 transporter mRNA (left) and protein (middle) and glucose transport (α-methyl-d-glucopyranoside) (right) are increased in cultured renal proximal tubular epithelial cells of individuals with type 2 diabetes (T2DM) versus nondiabetic subjects (CON) (232).
These observations have important clinical implications. Thus, an adaptive response by the kidney to conserve glucose, which is essential to meet the energy demands of the body, especially the brain and other neural tissues, which have an obligate need for glucose, becomes maladaptive in the diabetic patient. Instead of dumping glucose in the urine to correct the hyperglycemia, the kidney chooses to hold on to the glucose. Even worse, the ability of the diabetic kidney to reabsorb glucose appears to be augmented by an absolute increase in the renal reabsorptive capacity for glucose.
In summary, the development of medications that inhibit renal proximal tubular glucose reabsorption provides a rational approach to the treatment of type 2 diabetes (227).
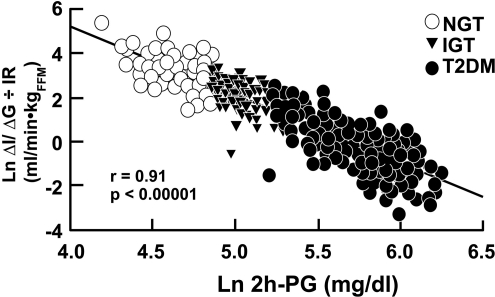
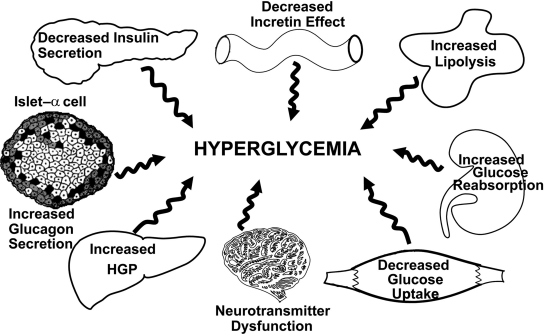
OMINOUS OCTET (FIG. 13)
FIG. 13.
The ominous octet. See text for a more detailed explanation.
The last, and perhaps most important, player to be implicated in the pathogenesis of type 2 diabetes is the brain, which, along with his seven companions, forms the ominous octet. It is abundantly clear that the current epidemic of diabetes is being driven by the epidemic of obesity (207,233). Porte and colleagues (234–237) were among the first to demonstrate that, in rodents, insulin was a powerful appetite suppressant. Obese individuals, both diabetic and nondiabetic, are characterized by insulin resistance and compensatory hyperinsulinemia. Nonetheless, food intake is increased in obese subjects despite the presence of hyperinsulinemia, and one could postulate that the insulin resistance in peripheral tissues also extends to the brain.
Our laboratory has attempted to address the issue of impaired appetite regulation by insulin in obese subjects using functional magnetic resonance imaging (MRI) to examine the cerebral response to an ingested glucose load (238). After glucose ingestion, two hypothalamic areas with consistent inhibition were noted: the lower posterior hypothalamus, which contains the ventromedial nuclei, and the upper posterior hypothalamus, which contains the paraventricular nuclei. In both of these hypothalamic areas, which are key centers for appetite regulation, the magnitude of the inhibitory response following glucose ingestion was reduced in obese, insulin-resistant, normal glucose tolerant subjects, and there was a delay in the time taken to reach the maximum inhibitory response, even though the plasma insulin response was markedly increased in the obese group. Whether the impaired functional MRI response in obese subjects contributes to or is a consequence of the insulin resistance and weight gain remains to be determined. Nonetheless, these results suggest that the brain, like other organs (liver, muscle, and fat) in the body, may be resistant to insulin. Studies by Obici et al. (239,240) in rodents have also provided evidence for cerebral insulin resistance leading to increased HGP and reduced muscle glucose uptake.
IMPLICATIONS FOR THERAPY
The preceding review of the pathophysiology of type 2 diabetes has important therapeutic implications (Table 1). First, effective treatment of type 2 diabetes will require multiple drugs used in combination to correct the multiple pathophysiological defects. Second, the treatment should be based upon known pathogenic abnormalities and NOT simply on the reduction in A1C. Third, therapy must be started early in the natural history of type 2 diabetes, if progressive β-cell failure is to be prevented.
TABLE 1.
Pathogenesis of type 2 diabetes: implications for therapy
- 1) Effective treatment of type 2 diabetes requires multiple drugs used in combination to correct multiple pathophysiological defects.
- 2) Treatment should be based on known pathogenic abnormalities and not simply on reduction of A1C.
- 3) Therapy must be started early in the natural history of type 2 diabetes to prevent progressive β-cell failure.
Let us now examine the current therapeutic options as they relate to four of the key pathophysiological derangements present in type 2 diabetes (Fig. 14). At the level of the liver, we have shown that both metformin (241–243) and the TZDs (175,244–252) are potent insulin sensitizers and inhibit the increased rate of hepatic gluconeogenesis (220,221) that is characteristic of type 2 diabetic patients. In muscle, TZDs are potent insulin sensitizers (244–252), whereas metformin is a very weak insulin sensitizer (241,243,253). Since the TZDs work through the classic insulin signaling pathway (150,254), whereas metformin works through the AMP kinase pathway (255,256), combination therapy with a TZD plus metformin gives a completely additive effect to reduce the A1C (257–265), and hypoglycemia is not encountered because these drugs are insulin sensitizers and do not augment insulin secretion. In adipose tissue, the TZDs are also excellent insulin sensitizers and are potent inhibitors of lipolysis (263). TZDs also effectively mobilize fat out of muscle, liver, and β-cell, thereby ameliorating lipotoxicity (175,176,205,264–267).
FIG. 14.
Treatment of type 2 diabetes: a therapeutic approach based upon pathophysiology. See text for a more detailed explanation.
At the level of the β-cell, only the TZDs conclusively have been shown to improve and preserve β-cell function (75,268) and demonstrate durability of control (167,168,260, 268–272). There is also evidence that the GLP-1 analogs can preserve β-cell function on a long-term basis (273–275). Nonetheless, the two most commonly prescribed drugs in the U.S. and throughout the world are the sulfonylureas and metformin, and neither of these drugs exerts any significant protective effect on the β-cell. This is a major concern, since progressive β-cell failure is the primary pathogenic abnormality responsible for the development of overt diabetes and the progressive rise in A1C (Fig. 2 and supplemental Fig. A1).
Sulfonylureas and metformin.
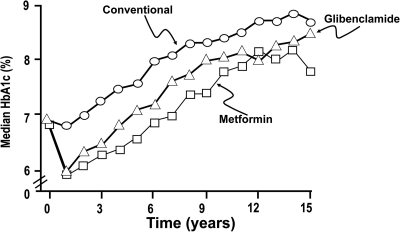
Professor Robert Turner, in the UK Prospective Diabetes Study (UKPDS), was the first to conclusively show that sulfonylureas had no protective effect on the β-cell in newly diagnosed type 2 diabetic patients over the 15-year study duration (36). After an initial drop in the A1C, sulfonylurea-treated patients experienced a progressive deterioration in glycemic control that paralleled the rise in A1C in the conventionally treated group (Fig. 15). Moreover, in the UKPDS sulfonylureas were shown not to have a significant protective effect against atherosclerotic cardiovascular complications (34), and some studies even have suggested that sulfonylureas may accelerate the atherogenic process (276,277). Similarly, metformin-treated patients in the UKPDS, after an initial decline in A1C, secondary to the biguanide's inhibitory effect on HGP, also experienced a progressive deterioration in glycemic control (Fig. 15) (278). Using HOMA-β, Professors Holman and Turner showed that the relentless rise in A1C observed with both sulfonylureas and metformin resulted from a progressive decline in β-cell function and that by 3 years ∼50% of diabetic patients required an additional pharmacological agent to maintain the A1C <7.0% (279–284). Although there is some in vitro evidence that metformin may improve β-cell function and prevent β-cell apoptosis (285,286), the in vivo data from the UKPDS fail to support any role for metformin in the preservation of β-cell function. However, metformin was shown to reduce macrovascular events in UKPDS (278), although by today's standards the number of diabetic subjects in the metformin arm (n = 342) would be considered inadequate to justify any conclusions about cardiovascular protection.
FIG. 15.
The effect of sulfonylurea (glibenclamide = glyburide) and metformin therapy on the plasma A1C concentration in newly diagnosed type 2 diabetic subjects. Conventionally treated diabetic subjects received diet plus exercise therapy (36,279).
It is especially noteworthy that UKPDS was originally designed as a monotherapy study. However, after 3 years it became evident that neither monotherapy with metformin nor sulfonylureas was capable of preventing progressive β-cell failure and stabilizing the A1C at its starting level (279–283). Therefore, the investigators altered the study protocol to allow metformin to be added to the sulfonylurea arm, sulfonylureas to be added to the metformin arm, and/or insulin to be added to the sulfonylurea arm (279–283). Although the addition of a second oral antidiabetic agent improved glycemic control, after the initial decline in A1C progressive β-cell failure continued and the A1C rose progressively.
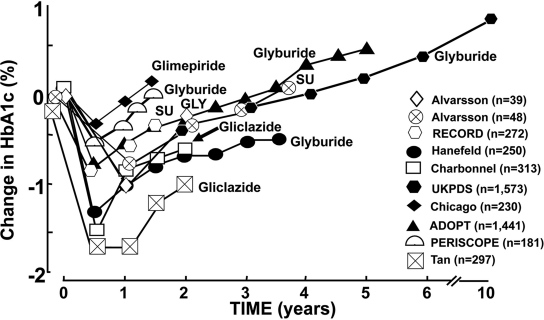
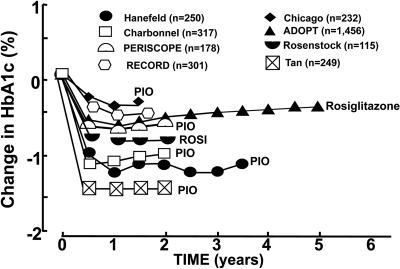
ADOPT (A Diabetes Outcome Progression Trial) (268) has provided results similar to those obtained in the UKPDS. In newly diagnosed type 2 diabetic patients treated with glyburide, after an initial decline, the A1C rose continuously due to the progressive loss of β-cell function (Fig. 16). In contrast, rosiglitazone caused an initial reduction in A1C that was largely sustained over the 5-year study duration because of a durable effect to preserve β-cell function (Fig. 17). The rate of decline in β-cell function was 3.5-fold greater in glyburide-treated patients versus rosiglitazone-treated patients. Although metformin produced a more sustained effect to lower the A1C than the sulfonylureas in ADOPT, it also was associated with a progressive rise in A1C and progressive decline in β-cell function after the first year (268).
FIG. 16.
Summary of studies examining the effect of sulfonylurea (SU) treatment versus placebo or versus active-comparator on A1C in type 2 diabetic subjects (36,166,167,260,269–273,279–285). See text for a more detailed discussion. GLY, glyburide.
FIG. 17.
Summary of studies examining the effect of TZDs versus placebo or versus active-comparator on A1C in type 2 diabetic subjects (167,168,260,268–273). See text for a more detailed discussion. PIO, pioglitazone; ROSI, rosiglitazone.
A number of long-term (>1.5 years), active-comparator, or placebo-controlled studies have examined the ability of sulfonylureas to produce a durable reduction in A1C in type 2 diabetic patients. All of these studies (36,166,167, 260,268–272) showed that, after an initial decline in A1C, a variety of sulfonylureas, including glyburide, glimepiride, and gliclazide, were associated with a progressive decline in β-cell function with an accompanying loss of glycemic control (Fig. 16). There are no exceptions to this consistent loss of glycemic control with the sulfonylureas after the initial 18 months of therapy. Thus, evidence-based medicine conclusively demonstrates that the glucose-lowering effect of the sulfonylureas is not durable and that the loss of glycemic control is associated with progressive β-cell failure (36,37,166,167,268–272,279–283).
TZDs.
In contrast to the sulfonylureas, eight long-term (>1.5 years) active-comparator or double-blind placebo-controlled studies with the TZDs present a very different picture (Fig. 17) (167,168,268–272). Thus, after an initial decline in A1C, durability of glycemic control is maintained because of the preservation of β-cell function in type 2 diabetic patients. In addition to these studies performed in type 2 diabetic patients, there are five studies in subjects with IGT demonstrating that TZDs prevent the progression of IGT to type 2 diabetes (286–290). The DREAM (Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication) study showed a 62% decrease in the development of type 2 diabetes with rosiglitazone (287), while the ACT NOW (Actos Now for Prevention of Diabetes) study (290) showed a 81% reduction in the conversion of IGT to type 2 diabetes with pioglitazone. All five of these studies showed that, in addition to their insulin sensitizing effect, the TZDs had a major action to preserve β-cell function. In ACT NOW, the improvement in the insulin secretion/insulin resistance (disposition) index (measure of β-cell function) was shown both with the OGTT and the frequently sampled intravenous glucose tolerance test. Similar results have been demonstrated in the TRIPOD (Troglitazone In Prevention Of Diabetes) and PIPOD (Pioglitazone In Prevention Of Diabetes) studies (286,289) in which the development of diabetes in Hispanic women with a history of gestational diabetes was decreased by 52 and 62%, respectively. Many in vivo and in vitro studies with human and rodent islets have shown that TZDs exert a protective effect on β-cell function (291–295).
GLP-1 analogs.
Incretins also have been shown to improve β-cell function and maintain durability of glycemic control. Bunck et al. (273) studied 69 metformin-treated type 2 diabetic patients with a mean age of 58 years and BMI of 30.5 kg/m2. Subjects received glargine insulin or exenatide to similarly reduce the A1C to 6.8%. Before and after 1 year, C-peptide secretion was evaluated with an 80-min hyperglycemic clamp. During the repeat hyperglycemic clamp performed after 1 year, both the first (0–10 min) and second (10–80 min) phases of insulin secretion were increased 1.5- and 2.9-fold, respectively, in the group treated with exenatide versus the group treated with glargine. Glargine increased by 31% the ratio of the C-peptide response during the hyperglycemic clamp performed after 1 year compared with the hyperglycemic clamp performed at baseline. In contrast, exenatide increased the ratio more than threefold, demonstrating a potent effect of this GLP-1 analog to augment β-cell function.
In a 32-week double-blind, placebo-controlled study, exenatide (10 μg b.i.d.) reduced A1C by ∼1.0–1.2% and markedly decreased the postprandial rise in plasma glucose concentration while maintaining the plasma insulin response at pre-exenatide treatment levels (274). Consequently, the ΔI/ΔG ratio increased dramatically, indicating a robust effect on β-cell function. A subset of these subjects were followed-up for 3.5 years, and the decline in A1C was shown to persist (275). However, it is not known whether the subjects who did not continue in this long-term extension study had the same characteristics, i.e., level of glycemic control, etc., as those who continued to be followed for 3.5 years. In vivo studies in rodents (296,297) and in vitro studies with cultured human islets (298) have shown that exenatide can expand β-cell mass and prevent apoptosis of islets, respectively. Whether these effects to augment β-cell mass will be observed in diabetic humans remains to be determined. Irrespective of changes in β-cell mass, the studies of Bunck et al. (273) clearly document a major effect of exenatide to augment β-cell function.
In addition to their effect on the β-cell, exenatide and other GLP-1 beneficially impact four other members of the ominous octet: liver (reduced HGP), α-cell (reduced glucagon secretion), gut (replacement of deficient GLP-1 response), and brain (reduced appetite with weight loss). Importantly, the stimulatory effect of exenatide on insulin secretion dissipates when normoglycemia is achieved, thereby minimizing the adverse effect of hypoglycemia.
Dipeptidyl peptidase-IV inhibitors.
There are no long-term studies examining the effect of the dipeptidyl peptidase-IV (DPP-IV) inhibitors on β-cell function. However, in short-term studies, from several months to 1 year, both sitagliptin and vildagliptin (98,99,299,300) reduce the postprandial plasma glucose concentration while maintaining the plasma insulin response, indicating a positive effect on β-cell function. Whether this enhancement in insulin secretion will be translated into preservation of β-cell function on a long-term basis remains to be determined. The DPP-IV inhibitors also decrease glucagon secretion, and in concert with the rise in plasma insulin, this leads to a reduction in basal HGP (301). Hypoglycemia does not occur with the DPP-IV inhibitors, but they do not suppress appetite or cause weight loss.
Summary.
The introduction of the TZDs and GLP-1 analogs into the diabetes market place and their potential to preserve β-cell function offer a new therapeutic approach to the treatment of type 2 diabetes.
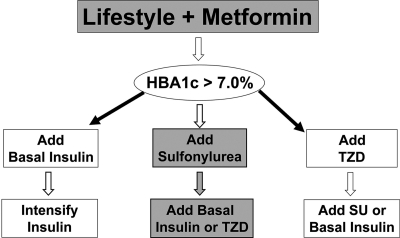
ADA ALGORITHM FOR TREATMENT OF TYPE 2 DIABETES
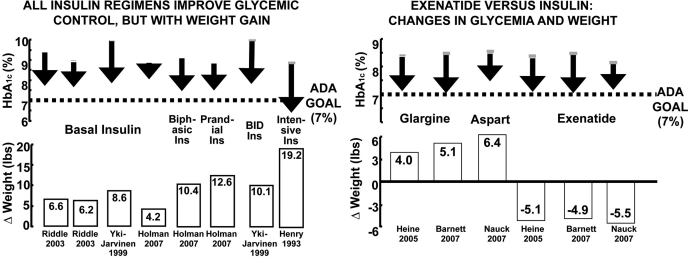
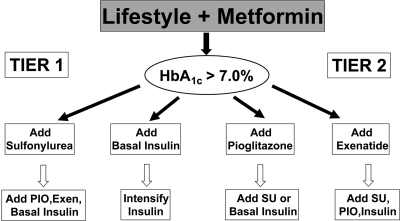
The ADA algorithm for the treatment of type 2 diabetes advocates a stepwise therapeutic approach that is based upon reduction in the plasma glucose concentration and NOT upon known pathophysiological disturbances (49). It dictates the initiation of therapy with lifestyle modification plus metformin to achieve an A1C < 7.0% (Fig. 18). If the goal is not reached or if secondary failure occurs, the ADA algorithm suggests one of three options: 1) First is the addition of basal insulin, an option unlikely to be chosen by primary care physicians or most endocrinologists in the U.S. and unlikely to achieve the desired level of glycemic control based upon well-designed studies by experts in the field of insulin therapy (302–308). Moreover, all of these insulin-based add-on studies have been associated with a high incidence of hypoglycemia and major weight gain (range 4.2–19.2 lbs, mean 8.5 lbs within 6–12 months or less) (Fig. 19). 2) Second is the addition of a TZD, but this option is unlikely to be chosen because of the concerns raised in the ADA algorithm about this class of drugs. Thus, the ADA algorithm basically guides the physician to select a sulfonylurea as the choice for a second antidiabetic agent. Moreover, third party reimbursers like this option because sulfonylureas are inexpensive. Neither the GLP-1 analogs nor the DPP-4 inhibitors are included as an option in the ADA algorithm (49). Since neither the sulfonylureas nor metformin exerts any effect to preserve β-cell function (see previous discussion and Fig. 16), the 20% of β-cell function that was present at the time of diagnosis of diabetes (40–42) will largely have been lost by the time that combined sulfonylurea/metformin therapy has failed, and the majority of these patients will require insulin treatment. Insulin therapy is difficult for most primary care physicians, and even in the hands of experienced endocrinologists it is not easy to achieve and maintain an A1C <7%—let alone <6.5%—without significant hypoglycemia and weight gain (302–308). Moreover, it is unclear why one would initiate insulin before exenatide, since insulin rarely decreases the A1C to <7.0% and is associated with significant weight gain and hypoglycemia (302–308) (Fig. 19). Most recently, an ADA Consensus Statement has significantly revised the ADA therapeutic algorithm (309). A two-tier approach is advocated, and sulfonylureas have been elevated into the first tier and are to be used if diet/exercise plus metformin fail to reduce the A1C to <7.0% (Fig. 20). From the pathophysiological standpoint, this represents a major step backward, since an overwhelming body of evidence-based medicine (Fig. 16) conclusively demonstrates that sulfonylureas do not preserve β-cell function and do not achieve durability of glycemic control. Although this algorithm is not the official policy statement of ADA, it is likely to be interpreted as such by most third-party payers.
FIG. 18.
ADA algorithm for the treatment of type 2 diabetes (49). See text for a more detailed explanation. SU, sulfonylurea.
FIG. 19.
Effect of insulin (Ins) and exenatide on A1C and body weight in type 2 diabetic subjects (302–308).
FIG. 20.
ADA consensus statement algorithm on the treatment of type 2 diabetes. As indicated, this does not represent the official statement of ADA (49). See text for a detailed discussion (309). Exen, exenatide; PIO, pioglitazone; SU, sulfonylurea.
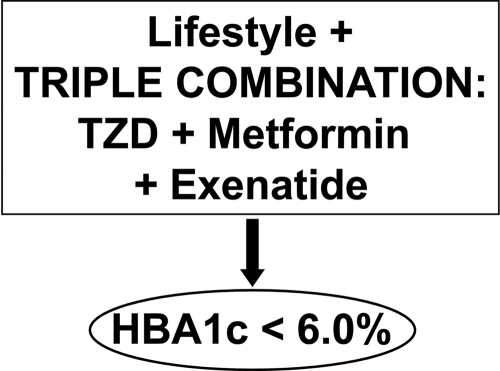
PATHOPHYSIOLOGICAL-BASED ALGORITHM
An alternate therapeutic algorithm is based upon known pathophysiological disturbances in type 2 diabetes (Fig. 21). This algorithm provides a more rational approach and is more likely to produce a durable long-term effect. This algorithm initiates treatment with lifestyle modification plus triple combination therapy with drugs known to improve insulin sensitivity (TZDs and metformin) and, most importantly, with drugs that have been shown to preserve β-cell function (TZDs and exenatide) (Fig. 21). Further, a more rational goal of therapy should be an A1C <6.0%, since the DPP has taught us that as many as 12% of individuals with IGT and an A1C of 6.0% already have background diabetic retinopathy.
FIG. 21.
Pathophysiological-based algorithm: treatment of type 2 diabetes based upon pathophysiology. See text for a detailed discussion.
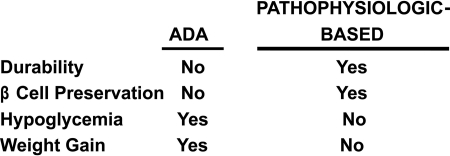
Comparison of the stepwise ADA algorithm with the combination pathophysiological-based algorithm is shown in Fig. 22. Many studies, including the UKPDS, have shown that stepped metformin/sulfonylurea therapy does not achieve durable glycemic control. Conversely, the TZDs and the GLP-1 analogs, when used as monotherapy, each have been shown to have a more durable effect. When used in combination, if anything, one would hypothesize an even more durable effect on β-cell function and reduction in A1C, although this remains to be proven. Neither the sulfonylureas nor metformin has been shown to preserve β-cell function. In contrast, both the TZDs and exenatide have been shown to preserve β-cell function. Hypoglycemia is common with the sulfonylureas and insulin, and this prohibits the achievement of the optimal A1C goal of 6.0%, let alone an A1C <7.0% (the ADA-recommended goal). In contrast, hypoglycemia is uncommon with the insulin sensitizers and GLP-1 analogs, allowing the physician to titrate these drugs to maximum doses to reduce the A1C <6.0%. Lastly, weight gain is common with sulfonylurea and insulin therapy, whereas weight loss is the norm with exenatide, and exenatide blocks the weight gain that is associated with the TZDs.
FIG. 22.
Comparison of the ADA and pathophysiological-based algorithms. See text for a detailed discussion.
Summary: Treatment.
Although this paradigm shift, which is based upon pathophysiology, represents a novel approach to the treatment of type 2 diabetes, it is substantiated by a vast body of basic scientific and clinical investigational studies. Because this algorithm is based upon the reversal of known pathophysiological defects, it has a high probability of achieving durable glycemic control. If the plasma glucose concentration can be maintained within the normal nondiabetic range, the microvascular complications of the disease, which are costly to treat and associated with major morbidity and mortality, can be prevented. Most importantly, this will enhance the quality of life for all diabetic patients.
Supplementary Material
Online-Only Appendix
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
REFERENCES
- 1.DeFronzo RA. Lilly Lecture: The triumvirate: β-cell, muscle, liver: a collusion responsible for NIDDM. Diabetes 1988; 37: 667– 687 [DOI] [PubMed] [Google Scholar]
- 2.Zimmet P, Whitehouse S, Alford F, Chisholm D. The relationship of insulin response to a glucose stimulus over a wide range of glucose tolerance. Diabetologia 1978; 15: 23– 27 [DOI] [PubMed] [Google Scholar]
- 3.Saad MF, Knowler WC, Pettitt DJ, Nelson RG, Mott DM, Bennett PH. Sequential changes in serum insulin concentration during development of non-insulin-dependent diabetes. Lancet 1989; i: 1356– 1359 [DOI] [PubMed] [Google Scholar]
- 4.Lillioja S, Mott DM, Howard BV, Bennett PH, Yki-Jarvinen H, Freymond D, Nyomba BL, Zurlo F, Swinburn B, Bogardus C. Impaired glucose tolerance as a disorder of insulin action: longitudinal and cross-sectional studies in Pima Indians. N Engl J Med 1988; 318: 1217– 1225 [DOI] [PubMed] [Google Scholar]
- 5.Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR. Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann Intern Med 1990; 113: 909– 915 [DOI] [PubMed] [Google Scholar]
- 6.Martin BC, Warren JH, Krolewski AS, Bergman RN, Soeldner JS, Kahn CR. Role of glucose and insulin resistance in development of type 2 diabetes mellitus: results of a 25-year follow-up study. Lancet 1992; 340: 925– 929 [DOI] [PubMed] [Google Scholar]
- 7.Saad MF, Knowler WC, Pettitt DJ, Nelson RG, Mott DM, Bennett PH. The natural history of impaired glucose tolerance in the Pima Indians. N Engl J Med 1988; 319: 1500– 1505 [DOI] [PubMed] [Google Scholar]
- 8.Jallut D, Golay A, Munger R, Frascarolo P, Schutz Y, Jequier E, Felber JP. Impaired glucose tolerance and diabetes in obesity: a 6 year follow-up study of glucose metabolism. Metabolism 1990; 39: 1068– 1075 [DOI] [PubMed] [Google Scholar]
- 9.Gulli G, Ferrannini E, Stern M, Haffner S, DeFronzo RA. The metabolic profile of NIDDM is fully established in glucose-tolerant offspring of two Mexican-American NIDDM parents. Diabetes 1992; 41: 1575– 1586 [DOI] [PubMed] [Google Scholar]
- 10.Haffner SM, Miettinen H, Gaskill SP, Stern MP. Decreased insulin secretion and increased insulin resistance are independently related to the 7-year risk of NIDDM in Mexican-Americans. Diabetes 1995; 44: 1386– 1391 [DOI] [PubMed] [Google Scholar]
- 11.Haffner SM, Miettinen H, Stern MP. Insulin secretion and resistance in nondiabetic Mexican Americans and non-Hispanic whites with a parental history of diabetes. J Clin Endocrinol Metab 1996; 81: 1846– 1851 [DOI] [PubMed] [Google Scholar]
- 12.Lillioja S, Mott DM, Spraul M, Ferraro R, Foley JE, Ravussin E, Knowler WC, Bennett PH, Bogardus C. Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus. N Engl J Med 1993; 329: 1988– 1992 [DOI] [PubMed] [Google Scholar]
- 13.Dowse GK, Zimmet PZ, Collins VR. Insulin levels and the natural history of glucose intolerance in Nauruans. Diabetes 1996; 45: 1367– 1372 [DOI] [PubMed] [Google Scholar]
- 14.Lyssenko V, Almgren P, Anevski D, Perfekt R, Lahti K, Nissen M, Isomaa B, Forsen B, Homstrom N, Saloranta C, Taskinen MR, Groop L, Tuomi T, Botnia study group Predictors of and longitudinal changes in insulin sensitivity and secretion preceding onset of type 2 diabetes. Diabetes 2005; 54: 166– 174 [DOI] [PubMed] [Google Scholar]
- 15.Weyer C, Tataranni PA, Bogardus C, Pratley RE. Insulin resistance and insulin secretory dysfunction are independent predictors of worsening of glucose tolerance during each stage of type 2 diabetes development. Diabetes Care 2001; 24: 89– 94 [DOI] [PubMed] [Google Scholar]
- 16.Eriksson J, Franssila-Kallunki A, Ekstrand A, Saloranta C, Widen E, Schalin C, Groop L. Early metabolic defects in persons at increased risk for non-insulin-dependent diabetes mellitus. N Engl J Med 1989; 321: 337– 343 [DOI] [PubMed] [Google Scholar]
- 17.DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Rev 1997; 5: 177– 269 [Google Scholar]
- 18.DeFronzo RA. Pathogenesis of type 2 diabetes mellitus. Med Clin North Am 2004; 88: 787– 835 [DOI] [PubMed] [Google Scholar]
- 19.Pendergrass M, Bertoldo A, Bonadonna R, Nucci G, Mandarino L, Cobelli C, DeFronzo RA. Muscle glucose transport and phosphorylation in type 2 diabetic, obese non-diabetic, and genetically predisposed individuals. Am J Physiol Endocrinol Metab 2007; 292: E92– E100 [DOI] [PubMed] [Google Scholar]
- 20.Groop L, Lyssenko V. Genes and type 2 diabetes mellitus. Current Diab Reports 2008; 8: 192– 197 [DOI] [PubMed] [Google Scholar]
- 21.Rothman DL, Magnusson I, Cline G, Gerard D, Kahn CR, Shulman RG, Shulman GI. Decreased muscle glucose transport/phosphorylation is an early defect in the pathogenesis of non-insulin-dependent diabetes mellitus. Proc Natl Acad Sci U S A 1995; 92: 983– 987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pratipanawatr W, Pratipanawatr T, Cusi K, Berria R, Jenkinson CP, Maezono K, DeFronzo RA, Mandarino L. Skeletal muscle insulin resistance in normoglycemic subjects with a strong family history of type 2 diabetes is associated with decreased insulin-stimulated IRS-1 tyrosine phosphorylation. Diabetes 2001; 50: 2572– 2578 [DOI] [PubMed] [Google Scholar]
- 23.Morino K, Petersen KF, Dufour S, Befroy D, Frattini J, Shatzkes N, Neschen S, White MF, Bilz S, Sono S, Pypaert M, Shulman GI. Reduced mitochondrial density and increased IRS-1 serine phosphorylation in muscle of insulin-resistant offspring of type 2 diabetic parents. J Clin Invest 2005; 115: 3587– 3593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kashyap S, Belfort R, Gastaldelli A, Pratipanawatr T, Berria R, Pratipanawatr W, Bajaj M, Mandarino L, DeFronzo RA, Cusi K. A sustained increase in plasma free fatty acids impairs insulin secretion in nondiabetic subjects genetically predisposed to develop type 2 diabetes. Diabetes 2003; 52: 2461– 2474 [DOI] [PubMed] [Google Scholar]
- 25.DeFronzo RA, Ferrannini E, Simonson DC. Fasting hyperglycemia in non-insulin dependent diabetes mellitus: contributions of excessive hepatic glucose production and impaired tissue glucose uptake. Metabolism 1989; 38: 387– 395 [DOI] [PubMed] [Google Scholar]
- 26.Groop LC, Bonadonna RC, Del Prato S, Ratheiser K, Zyck K, DeFronzo RA. Glucose and free fatty acid metabolism in non-insulin-dependent diabetes mellitus: evidence for multiple sites of insulin resistance. J Clin Invest 1989; 84: 205– 213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferrannini E, Simonson DC, Katz LD, Reichard G, Bevilacqua S, Barrett EJ, Olsson M, DeFronzo RA. The disposal of an oral glucose load in patients with non-insulin dependent diabetes. Metabolism 1988; 37: 79– 85 [DOI] [PubMed] [Google Scholar]
- 28.DeFronzo RA, Gunnarsson R, Bjorkman O, Olsson M, Wahren J. Effects of insulin on peripheral and splanchnic glucose metabolism in non-insulin-dependent (type II) diabetes mellitus. J Clin Invest 1985; 76: 149– 155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeFronzo RA, Diebert D, Hendler R, Felig P. Insulin sensitivity and insulin binding in maturity onset diabetes. J Clin Invest 1979; 63: 939– 946 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 30.James WP. The fundamental drivers of the obesity epidemic. Obesity Rev 2008; 9( Suppl. 1): 6– 13 [DOI] [PubMed] [Google Scholar]
- 31.DeFronzo RA, Soman V, Sherwin RS, Hendler R, Felig P. Insulin binding to monocytes and insulin action in human obesity, starvation, and refeeding. J Clin Invest 1978; 62: 204– 213 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Koivisto VA, Yki-Järvinen M, DeFronzo RA. Physical training and insulin sensitivity. Diabetes Metab Rev 1986; 1: 445– 481 [DOI] [PubMed] [Google Scholar]
- 33.Diamond MP, Thornton K, Connolly-Diamond M, Sherwin RS, DeFronzo RA. Reciprocal variation in insulin-stimulated glucose uptake and pancreatic insulin secretion in women with normal glucose tolerance. J Soc Gynecol Invest 1995; 2: 708– 715 [DOI] [PubMed] [Google Scholar]
- 34.Bergman RN, Finegood DT, Kahn SE. The evolution of beta-cell dysfunction and insulin resistance in type 2 diabetes. Eur J Clin Invest 2002; 32: 35– 45 [DOI] [PubMed] [Google Scholar]
- 35.Jallut D, Golay A, Munger R, Frascarolo P, Schutz Y, Jequier E, Felber JP. Impaired glucose tolerance and diabetes in obesity: a 6-year follow-up study of glucose metabolism. Metabolism 1990; 39: 1068– 1075 [DOI] [PubMed] [Google Scholar]
- 36.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837– 853 [PubMed] [Google Scholar]
- 37.Levy J, Atkinson AB, Bell PM, McCance DR, Hadden DR. Beta-cell deterioration determines the onset and rate of progression of secondary dietary failure in type 2 diabetes mellitus: the 10-year follow-up of the Belfast Diet Study. Diabet Med 1998; 15: 290– 296 [DOI] [PubMed] [Google Scholar]
- 38.Abdul-Ghani MA, Matsuda M, Sabbah M, Jenkinson C, Richardson DK, DeFronzo RA. The relative contribution of insulin resistance and beta cell failure to the transition from normal to impaired glucose tolerance varies in different ethnic groups. Diabete Metab Synd 2007; 1: 105– 112 [Google Scholar]
- 39.Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, DeFronzo RA. Beta cell dysfunction and glucose intolerance: results from the San Antonio Metabolism (SAM) study. Diabetologia 2004; 47: 31– 39 [DOI] [PubMed] [Google Scholar]
- 40.Ferrannini E, Gastaldelli A, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA. Beta cell function in subjects spanning the range from normal glucose tolerance to overt diabetes mellitus: a new analysis. J Clin Endocrinol Metab 2005; 90: 493– 500 [DOI] [PubMed] [Google Scholar]
- 41.Abdul-Ghani M, Jenkinson C, Richardson D, Tripathy D, DeFronzo RA. Insulin secretion and insulin action in subjects with impaired fasting glucose and impaired glucose tolerance: results from the Veterans Administration Genetic Epidemiology Study (VAGES). Diabetes 2006; 55: 1430– 1435 [DOI] [PubMed] [Google Scholar]
- 42.Abdul-Ghani M, Tripathy D, DeFronzo RA. Contributions of β-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care 2006; 29: 1130– 1139 [DOI] [PubMed] [Google Scholar]
- 43.Ahren B, Taborsky GJ. Beta-cell function and insulin secretion. In_Ellenberg Rifkin's Diabetes Mellitus_Porte D, Sherin RS, Baron A. Eds. New York, McGraw Hill, 2003, p. 43– 65 [Google Scholar]
- 44.Reaven GM, Hollenbeck CB, Chen YD. Relationship between glucose tolerance, insulin secretion, and insulin action in non-obese individuals with varying degrees of glucose tolerance. Diabetologia 1989; 32: 52– 55 [DOI] [PubMed] [Google Scholar]
- 45.Bergman RN. Lilly Lecture: Toward physiological understanding of glucose tolerance: minimal-model approach. Diabetes 1989; 38: 1512– 1527 [DOI] [PubMed] [Google Scholar]
- 46.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2008; 31( Suppl. 1): S55– S60 [DOI] [PubMed] [Google Scholar]
- 47.Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. β-Cell deficit and increased β-cell apoptosis in humans with type 2 diabetes. Diabetes 2003; 52: 102– 110 [DOI] [PubMed] [Google Scholar]
- 48.Diabetes Prevention Program Research Group The prevalence of retinopathy in impaired glucose tolerance and recent-onset diabetes in the Diabetes Prevention Program. Diabet Med 2007; 24: 137– 144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. Diabetes Care 2006; 29: 1963– 1972 [DOI] [PubMed] [Google Scholar]
- 50.Ziegler D, Rathmann W, Dickhaus T, Meisinger C, Mielck A. KORA Study Group Prevalence of polyneuropathy in pre-diabetes and diabetes is associated with abdominal obesity and macroangiopathy: the MONICA/KORA Augsburg Surveys S2 and S3. Diabetes Care 2008; 31: 464– 469 [DOI] [PubMed] [Google Scholar]
- 51.Smith AG, Russell J, Feldman EL, Goldstein J, Peltier A, Smith S, Hamwi J, Pollari D, Bixby B, Howard J, Singleton JR. Lifestyle intervention for pre-diabetic neuropathy. Diabetes Care 2006; 6: 415– 416 [DOI] [PubMed] [Google Scholar]
- 52.Muller DC, Elahi D, Tobin JD, Andres R. Insulin response during the oral glucose tolerance test: the role of age, sex, body fat and the pattern of fat distribution. Aging 1996; 8: 13– 21 [DOI] [PubMed] [Google Scholar]
- 53.Rosenthal M, Doberne L, Greenfield M, Widstrom A, Reaven GM, Rosenthal M, Doberne L, Greenfield M, Widstrom A, Reaven GM. Effect of age on glucose tolerance, insulin secretion, and in vivo insulin action. J Am Geriatrics Soc 1982; 30: 562– 567 [DOI] [PubMed] [Google Scholar]
- 54.Chang AM, Halter JB. Aging and insulin secretion. Am J Physiol Endocrinol Metab 2003; 284: E7– E12 [DOI] [PubMed] [Google Scholar]
- 55.Gautier JF, Wilson C, Weyer c, Mott D, Knowler WC, Cavaghan M, Polonsky KS, Bogardus C, Pratley RE. Low acute insulin secretory responses in adult offspring of people with early onset type 2 diabetes. Diabetes 2001; 50: 1828– 1833 [DOI] [PubMed] [Google Scholar]
- 56.Vauhkonen N, Niskanane L, Vanninen E, Kainulainen S, Uusitupa M, Laakso M. Defects in insulin secretion and insulin action in non-insulin-dependent diabetes mellitus are inherited. Metabolic studies on offspring of diabetic probands. J Clin Invest 1997; 100: 86– 96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vaag A, Henriksen JE, Madsbad S, Holm N, Beck-Nielsen H. Insulin secretion, insulin action, and hepatic glucose production in identical twins discordant for non-insulin-dependent diabetes mellitus. J Clin Invest 1995; 95: 690– 698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barnett AH, Spilipoulos AJ, Pyke DA, Stubbs WA, Burrin J, Alberti KGMM. Metabolic studies in unaffected co-twins of non-insulin-dependent diabetics. BMJ 1981; 282: 1656– 1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Watanabe RM, Valle T, Hauser ER, Ghosh S, Eriksson J, Kohtamaki K, Enholm C, Tuomilehto J, Collins FS, Bergman RN, Boehnke M. Familiarity of quantitative metabolic traits in Finnish families with non-insulin-dependent diabetes mellitus: Finland-United States Investigation of NIDDM Genes (FUSION) Study Investigators. Hum Hered 1999; 39: 159– 168 [DOI] [PubMed] [Google Scholar]
- 60.Grant SF, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J, Helgason A, Stefansson H, Emilsson V, Helgadottir A, Styrkarsdottir U, Magnusson KP, Walters GB, Palsdottir E, Jonsdottir T, Gudmundsdottir T, Gylfason A, Saemundsdottir J, Wilensky RL, Reilly MP, Rader DJ, Bagger Y, Christiansen C, Gudnason V, Sigurdsson G, Thorsteinsdottir U, Gulcher JR, Kong A, Stefansson K. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet 2006; 38: 320– 323 [DOI] [PubMed] [Google Scholar]
- 61.Helgason A, Palsson S, Thorleifsson G, Grant SF, Emilsson V, Gunnarsdottir S, Adeyemo A, Chen Y, Chen G, Reynisdottir I, Benediktsson R, Hinney A, Hansen T, Andersen G, Borch-Johnsen K, Jorgensen T, Schafer H, Faruque M, Doumatey A, Zhou J, Wilensky RL, Reilly MP, Rader DJ, Bagger Y, Christiansen C, Sigurdsson G, Hebebrand J, Pedersen O, Thorsteinsdottir U, Gulcher JR, Kong A, Rotimi C, Stefansson K. Refining the impact of TCF7L2 gene variants on type 2 diabetes and adaptive evolution. Nat Genet 2007; 39: 218– 225 [DOI] [PubMed] [Google Scholar]
- 62.Steinthorsdottir V, Thorleifsson G, Reynisdottir I, Benediktsson R, Jonsdottir T, Walters GB, Styrkarsdottir U, Gretarsdottir S, Emilsson V, Ghosh S, Baker A, Snorradottir S, Bjarnason H, Ng MC, Hansen T, Bagger Y, Wilensky RL, Reilly MP, Adeyemo A, Chen Y, Zhou J, Gudnason V, Chen G, Huang H, Lashley K, Doumatey A, So WY, Ma RC, Andersen G, Borch-Johnsen K, Jorgensen T, van Vliet-Ostaptchouk JV, Hofker MH, Wijmenga C, Christiansen C, Rader DJ, Rotimi C, Gurney M, Chan JC, Pedersen O, Sigurdsson G, Gulcher JR, Thorsteinsdottir U, Kong A, Stefansson K. A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat Genet 2007; 39: 770– 775 [DOI] [PubMed] [Google Scholar]
- 63.Lyssenko V, Lupi R, Marchetti P, Del Guerra S, Orho-Melander M, Almgren P, Sjogren M, Ling C, Eriksson KF, Lethagen AL, Mancarella R, Berglund G, Tuomi T, Nilsson P, Del Prato S, Groop L. Mechanisms by which common variants in the TCF7L2 gene increase risk of type 2 diabetes. J Clin Invest 2007; 117: 2155– 2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cauchi S, Meyre D, Dina C, Choquet H, Samson C, Gallina S, Balkau B, Charpentier G, Pattou F, Stetsyuk V, Scharfmann R, Staels B, Fruhbeck G, Froguel P. Transcription factor TCF7L2 genetic study in the French population: expression in human β-cells and adipose tissue and strong association with type 2 diabetes. Diabetes 2006; 55: 2903– 2908 [DOI] [PubMed] [Google Scholar]
- 65.Welters HJ, Kulkarni RN. Wnt signaling: relevance to β-cell biology and diabetes. Trends Endocrinol Metab 2008; 19: 349– 355 [DOI] [PubMed] [Google Scholar]
- 66.Unger RH. Lipotoxicity in the pathogenesis of obesity-dependent NIDDM: genetic and clinical implications. Diabetes 1995; 44: 863– 870 [DOI] [PubMed] [Google Scholar]
- 67.Prentki M, Nolan CJ. Islet beta cell failure in type 2 diabetes. J Clin Invest 2006; 116: 1802– 1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kashyap S, Belfort R, Gastaldelli A, Pratipanawatr T, Berria R, Pratipanawatr W, Bajaj M, Mandarino L, DeFronzo RA, Cusi K. A sustained increase in plasma free fatty acids impairs insulin secretion in non-diabetic subjects genetically predisposed to develop type 2 diabetes. Diabetes 2003; 52: 2461– 2474 [DOI] [PubMed] [Google Scholar]
- 69.Higa M, Zhou YT, Ravazzola M, Baetens D, Orci L, Unger RH. Troglitazone prevents mitochondrial alterations, beta cell destruction, and diabetes in obese prediabetic rats. Proc Natl Acad Sci U S A 1999; 96: 11513– 11518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Matsui J, Terauchi Y, Kubota N, Takamoto I, Eto K, Yamashita T, Komeda K, Yamauchi T, Kamon J, Kita S, Noda M, Kadowaki T. Pioglitazone reduces islet triglyceride content and restores impaired glucose-stimulated insulin secretion in heterozygous peroxisome proliferator-activated receptor-γ–deficient mice on a high-fat diet. Diabetes 2004; 53: 2844– 2854 [DOI] [PubMed] [Google Scholar]
- 71.Shimabukuro M, Zhou YT, Lee Y, Unger RH. Troglitazone lowers islet fat and restores beta cell function of Zucker diabetic fatty rats. J Biol Chem 1998; 273: 3547– 3550 [DOI] [PubMed] [Google Scholar]
- 72.Paolisso G, Tagliamonte MR, Rizzo MR, Gualdiero P, Saccomanno F, Gambardella A, Giugliano D, D'Onofrio F, Howard BV. Lowering fatty acids potentiates acute insulin response in first degree relatives of people with type II diabetes. Diabetologia 1998; 41: 1127– 1132 [DOI] [PubMed] [Google Scholar]
- 73.Lupi R, Dotta F, Marselli L, Del Guerra S, Masini M., Santangelo C, Patane G, Boggi U, Piro S, Anello M, Bergamini E, Mosca F, Di Mario U, Del Prato S, Marchetti P. Prolonged exposure to free fatty acids has cytostatic and pro-apoptotic effects on human pancreatic islets: evidence that β-cell death is caspase mediated, partially dependent on ceramide pathway, and Bcl-2 regulated. Diabetes 2002; 51: 1437– 1442 [DOI] [PubMed] [Google Scholar]
- 74.Lupi R, Del Guerra S, Marselli L, Bugliani M, Boggi U, Mosca F, Marchetti P, Del Prato S. Rosiglitazone prevents the impairment of human islet function induced by fatty acids: evidence for a role of PPARgamma2 in the modulation of insulin secretion. Am J Physiol Endocrinol Metab 2004; 286: E560– E567 [DOI] [PubMed] [Google Scholar]
- 75.Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA. Thiazolidinediones improve beta-cell function in type 2 diabetic patients. Am J Physiol Endocrinol Metab 2007; 292: E871– E883 [DOI] [PubMed] [Google Scholar]
- 76.Rossetti L, Giaccari A, DeFronzo RA. Glucose toxicity (Review). Diabetes Care 1990; 13: 610– 630 [DOI] [PubMed] [Google Scholar]
- 77.Rossetti L, Shulman GI, Zawalich W, DeFronzo RA. Effect of chronic hyperglycemia on in vivo insulin secretion in partially pancreatectomized rats. J Clin Invest 1987; 80: 1037– 1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Patane G, Anello M, Piro S, Vigneri R, Purrello F, Rabuazzo AM. Role of ATP production and uncoupling protein-2 in the insulin secretory defect induced by chronic exposure to high glucose or free fatty acids and effects of peroxisome proliferator–activated receptor-γ inhibition. Diabetes 2002; 51: 2749– 2756 [DOI] [PubMed] [Google Scholar]
- 79.Andreozzi F, D'Alessandris C, Federici M, Laratta E, Del Guerra S, Del Prato S, Marchetti P, Lauro R, Perticone F, Sesti G. Activation of the hexosamine pathway leads to phosphorylation of insulin receptor substrate-1 on Ser307 and Ser612 and impairs the phosphatidylinositol 3-kinase/Akt/mammalian target of rapamycin insulin biosynthetic pathway in RIN pancreatic beta-cells. Endocrinology 2004; 145: 2845– 2857 [DOI] [PubMed] [Google Scholar]
- 80.Leahy JL, Cooper HE, Deal DA, Weir GC. Chronic hyperglycemia is associated with impaired glucose influence on insulin secretion: a study in normal rats using chronic in vivo glucose infusions. J Clin Invest 1986; 77: 908– 915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Leahy JL, Cooper HE, Weir GC. Impaired insulin secretion associated with near normoglycemia: study in normal rats with 96-h in vivo glucose infusions. Diabetes 1987; 36: 459– 464 [DOI] [PubMed] [Google Scholar]
- 82.Garvey WT, Olefsky JM, Griffin J, Hamman RF, Kolterman OG. The effect of insulin treatment on insulin secretion and insulin action in type II diabetes mellitus. Diabetes 1985; 34: 222– 234 [DOI] [PubMed] [Google Scholar]
- 83.Kosaka K, Kuzuya T, Akanuma Y, Hagura R. Increase in insulin response after treatment of overt maturity-onset diabetes is independent of the mode of treatment. Diabetologia 1980; 18: 23– 28 [DOI] [PubMed] [Google Scholar]
- 84.Andrews WJ, Vasquez B, Nagulesparan M, Klimes I, Foley J, Unger R, Reaven GM. Insulin therapy in obese, non-insulin-dependent diabetes induces improvements in insulin action and secretion that are maintained for two weeks after insulin withdrawal. Diabetes 1984; 33: 634– 642 [DOI] [PubMed] [Google Scholar]
- 85.Eriksson J, Nakazato M, Miyazato M, Shiomi K, Matsukura S, Groop L. Islet amyloid polypeptide plasma concentrations in individuals at increased risk of developing type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1992; 35: 291– 293 [DOI] [PubMed] [Google Scholar]
- 86.Johnson KH, O'Brien TD, Betsholtz C, Westermark P. Islet amyloid, islet-amyloid polypeptide, and diabetes mellitus. N Engl J Med 1989; 321: 513– 518 [DOI] [PubMed] [Google Scholar]
- 87.Ohsawa H, Kanatsuka A, Yamaguchi T, Makino H, Yoshida S. Islet amyloid polypeptide inhibits glucose-stimulated insulin secretion from isolated rat pancreatic islets. Biochem Biophy Res Com 1989; 160: 961– 967 [DOI] [PubMed] [Google Scholar]
- 88.Bretherton-Watt D, Ghatei MA, Bloom SR, Jamal H, Ferrier GJ, Girgis SI, Legon S. Altered islet amyloid polypeptide (amylin) gene expression in rat models of diabetes. Diabetologia 1989; 32: 881– 883 [DOI] [PubMed] [Google Scholar]
- 89.Haataja L, Gurlo T, Huang CJ, Butler PC. Islet amyloid in type 2 diabetes and the toxic oligomer hypothesis. Endocr Rev 2008; 29: 303– 316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chavez AO, Lopez-Alvarenga JC, Triplitt C, Bastarrachea RA, Musi N, Comuzzie AG, DeFronzo RA, Folli F. Physiological and molecular determinants of insulin action in the baboon. Diabetes 2008; 57: 899– 908 [DOI] [PubMed] [Google Scholar]
- 91.Mendoza RG, Davalli A, Chavez-Velazquez AO, Comuzzie A, Tejero E, Alvarenga JC, Bastarrachea R, Zuo P, Chang Z, Dick E, Hubbard G, Cruz AM, Perez CT, Malff G, DeFronzo RA, Folli F. Fasting plasma glucose (FPG) and HbA1c predict quantitatively baboon pancreatic islet amyloidosis (PIA): a novel non-human primate model of β-cell failure in type 2 diabetes mellitus (T2DM) (Abstract). Diabetes 2008; 57( Suppl. 1): A439 [Google Scholar]
- 92.Cox LA, Mahaney MC, Vandeberg JL, Rogers J. A second-generation genetic linkage map of the baboon (Papio hamadryas) genome. Genomics 2006; 88: 274– 281 [DOI] [PubMed] [Google Scholar]
- 93.Huang CJ, Lin CY, Haataja L, Gurlo T, Butler AE, Rizza RA, Butler PC. High expression rates of human islet amyloid polypeptide induce endoplasmic reticulum stress mediated β-cell apoptosis, a characteristic of humans with type 2 but not type 1 diabetes. Diabetes 2007; 56: 2016– 2027 [DOI] [PubMed] [Google Scholar]
- 94.Ritzel RA, Meier JJ, Lin CY, Veldhuis JD, Butler PC. Human islet amyloid polypeptide oligomers disrupt cell coupling, induce apoptosis, and impair insulin secretion in isolated human islets. Diabetes 2007; 56: 65– 71 [DOI] [PubMed] [Google Scholar]
- 95.Hartter E, Svoboda T, Ludvik B, Schuller M, Lell B, Kuenburg E, Brunnbauer M, Woloszczuk W, Prager R. Basal and stimulated plasma levels of pancreatic amylin indicate its co-secretion with insulin in humans. Diabetologia 1991; 34: 52– 54 [DOI] [PubMed] [Google Scholar]
- 96.Lukinius A, Wilander E, Westermark GT, Engstrom U, Westermark P. Co-localization of islet amyloid polypeptide and insulin in the beta cell secretory granules of the human pancreatic islets. Diabetologia 1989; 32: 240– 244 [DOI] [PubMed] [Google Scholar]
- 97.Lin CY, Gurlo T, Haataja L, Hsueh WA, Butler PC. Activation of peroxisome proliferator-activated receptor-gamma by rosiglitazone protects human islet cells against human islet amyloid polypeptide toxicity by a phosphatidylinositol 3′-kinase-dependent pathway. J Clin Endocrinol Metab 2005; 90: 6678– 6686 [DOI] [PubMed] [Google Scholar]
- 98.Drucker DJ. The biology of incretin hormones. Cell Metab 2006; 3: 153– 165 [DOI] [PubMed] [Google Scholar]
- 99.Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 2006; 368: 1696– 1705 [DOI] [PubMed] [Google Scholar]
- 100.Meier JJ, Nauck MA. Incretins and the development of type 2 diabetes. Curren Diab Reports 2006; 6: 194– 201 [DOI] [PubMed] [Google Scholar]
- 101.Toft-Nielsen MB, Damholt MB, Madsbad S, Hilsted LM, Hughes TE, Michelsen BK, Holst JJ. Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 2001; 86: 3717– 3723 [DOI] [PubMed] [Google Scholar]
- 102.Nauck M, Stockmann F, Ebert R, Creutzfeldt W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 1986; 29: 46– 52 [DOI] [PubMed] [Google Scholar]
- 103.Holst JJ. Glucagon-like peptide-1: from extract to agent. The Claude Bernard Lecture, 2005. Diabetologia 2006; 49: 253– 260 [DOI] [PubMed] [Google Scholar]
- 104.Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7–36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest 1993; 91: 301– 307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Meier JJ, Hucking K, Holst JJ, Deacon CF, Schmiegel WH, Nauck MA. Reduced insulinotropic effect of gastric inhibitory polypeptide in first-degree relatives of patients with type 2 diabetes. Diabetes 2001; 50: 2497– 2504 [DOI] [PubMed] [Google Scholar]
- 106.Kjems LL, Holst JJ, Volund A, Madsbad S. The influence of GLP-1 on glucose-stimulated insulin secretion: effects on β-cell sensitivity in type 2 and nondiabetic subjects. Diabetes 2003; 52: 380– 386 [DOI] [PubMed] [Google Scholar]
- 107.Holst JJ, Gromada J. Role of incretin hormones in the regulation of insulin secretion in diabetic and nondiabetic humans. Am J Physiol Endocrinol Metab 2004; 287: E199– E206 [DOI] [PubMed] [Google Scholar]
- 108.Jones IR, Owens DR, Luzio S, Williams S, Hayes TM. The glucose dependent insulinotropic polypeptide response to oral glucose and mixed meals is increased in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1989; 32: 668– 677 [DOI] [PubMed] [Google Scholar]
- 109.Hojberg PV, Vilsboll T, Rabol R, Knop FK, Bache M, Krarup T, Holst JJ, Madsbad S. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia 2009; 52: 199– 207 [DOI] [PubMed] [Google Scholar]
- 110.DeFronzo RA, Ferrannini E. Regulation of intermediatory metabolism during fasting and refeeding. Chapter 52. In_Endocrinology_DeGroot LJ, Jameson JL. Eds. Elsevier, Philadelphia, PA, 2006, p. 1015– 1043 [Google Scholar]
- 111.Shulman GI, Rothman DL, Smith D, Johnson CM, Blair JB, Shulman RG, DeFronzo RA. Mechanism of liver glycogen repletion in vivo by nuclear magnetic resonance spectroscopy. J Clin Invest 1985; 76: 1229– 1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Firth R, Bell P, Rizza R. Insulin action in non-insulin-dependent diabetes mellitus: the relationship between hepatic and extrahepatic insulin resistance and obesity. Metabolism 1987; 36: 1091– 1095 [DOI] [PubMed] [Google Scholar]
- 113.Campbell PJ, Mandarino LJ, Gerich JE. Quantification of the relative impairment in actions of insulin on hepatic glucose production and peripheral glucose uptake in non-insulin-dependent diabetes mellitus. Metabolism 1988; 37: 15– 21 [DOI] [PubMed] [Google Scholar]
- 114.Chen YD, Jeng CY, Hollenbeck CB, Wu MS, Reaven GM. Relationship between plasma glucose and insulin concentration, glucose production, and glucose disposal in normal subjects and patients with non-insulin-dependent diabetes. J Clin Invest 1988; 82: 21– 25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Jeng CY, Sheu WH, Fuh MM, Chen YD, Reaven GM. Relationship between hepatic glucose production and fasting plasma glucose concentration in patients with NIDDM. Diabetes 1994; 43: 1440– 1444 [DOI] [PubMed] [Google Scholar]
- 116.Henry RR, Wallace P, Olefsky JM. Effects of weight loss on mechanisms of hyperglycemia in obese non-insulin-dependent diabetes mellitus. Diabetes 1986; 35: 990– 998 [DOI] [PubMed] [Google Scholar]
- 117.DeFronzo RA, Ferrannini E. Regulation of hepatic glucose metabolism in humans. Diabetes Metab Rev 1987; 3: 415– 460 [DOI] [PubMed] [Google Scholar]
- 118.Magnusson I, Rothman DL, Katz LD, Shulman RG, Shulman GI. Increased rate of gluconeogenesis in type II diabetes mellitus: a 13C nuclear magnetic resonance study. J Clin Invest 1992; 90: 1323– 1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Consoli A, Nurjhan N, Reilly JJ, Jr, Bier DM, Gerich JE. Mechanism of increased gluconeogenesis in noninsulin-dependent diabetes mellitus: role of alterations in systemic, hepatic, and muscle lactate and alanine metabolism. J Clin Invest 1990; 86: 2038– 2045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Matsuda M, DeFronzo RA, Glass L, Consoli A, Giordano M, Bressler P, DelPrato S. Glucagon dose response curve for hepatic glucose production and glucose disposal in type 2 diabetic patients and normal individuals. Metabolism 2002; 51: 1111– 1119 [DOI] [PubMed] [Google Scholar]
- 121.Unger RH, Aguilar-Parada E, Muller WA, Eisentraut AM. Studies of pancreatic α-cell function in normal and diabetic subjects. J Clin Invest 1970; 49: 837– 848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Baron AD, Schaeffer L, Shragg P, Kolterman OG. Role of hyperglucagonemia in maintenance of increased rates of hepatic glucose output in type II diabetics. Diabetes 1987; 36: 274– 283 [DOI] [PubMed] [Google Scholar]
- 123.Gastaldelli A, Baldi S, Pettiti M, Toschi E, Camastra S, Natali A, Landau BR, Ferrannini E. Influence of obesity and type 2 diabetes on gluconeogenesis and glucose output in humans: a quantitative study. Diabetes 2000; 49: 1367– 1373 [DOI] [PubMed] [Google Scholar]
- 124.Clore JN, Stillman J, Sugerman H. Glucose-6-phosphatase flux in vitro is increased in type 2 diabetes. Diabetes 2000; 49: 969– 974 [DOI] [PubMed] [Google Scholar]
- 125.DeFronzo RA, Tobin JD, Andres R. The glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 1979; 237: E214– E223 [DOI] [PubMed] [Google Scholar]
- 126.Bajaj M, DeFronzo RA. Metabolic and molecular basis of insulin resistance. J Nuclear Cardiol 2003; 10: 311– 323 [DOI] [PubMed] [Google Scholar]
- 127.Reaven GM. Banting Lecture: Role of insulin resistance in human disease. Diabetes 1988; 37: 595– 607 [DOI] [PubMed] [Google Scholar]
- 128.Kolterman OG, Gray RS, Griffin J, Burstein P, Insel J, Scarlett JA, Olefsky JM. Receptor and postreceptor defects contribute to the insulin resistance in noninsulin-dependent diabetes mellitus. J Clin Invest 1981; 68: 957– 969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Campbell PJ, Mandarino LJ, Gerich JE. Quantification of the relative impairment in actions of insulin on hepatic glucose production and peripheral glucose uptake in non-insulin-dependent diabetes mellitus. Metabolism 1988; 37: 15– 21 [DOI] [PubMed] [Google Scholar]
- 130.Bogardus C, Lillioja S, Howard BV, Reaven G, Mott D. Relationships between insulin secretion, insulin action, and fasting plasma glucose concentration in nondiabetic and noninsulin-dependent diabetic subjects. J Clin Invest 1984; 74: 1238– 1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Butterfield WJ, Whichelow MJ. Peripheral glucose metabolism in control subjects and diabetic patients during glucose, glucose-insulin, and insulin sensitivity tests. Diabetologia 1965; 1: 43– 53 [Google Scholar]
- 132.Zierler KL, Rabinowitz D. Roles of insulin and growth hormone, based on studies of forearm metabolism in man. Medicine 1963; 42: 385– 402 [DOI] [PubMed] [Google Scholar]
- 133.Bonadonna RC, Del Prato S, Bonora E, Saccomani MP, Gulli G, Natali A, Frascerra S, Pecori N, Ferrannini E, Bier D, Cobelli C, DeFronzo RA. Roles of glucose transport and glucose phosphorylation in muscle insulin resistance of NIDDM. Diabetes 1996; 45: 915– 925 [DOI] [PubMed] [Google Scholar]
- 134.Rothman DL, Shulman RG, Shulman GI. 31P nuclear magnetic resonance measurements of muscle glucose-6-phosphate: evidence for reduced insulin-dependent muscle glucose transport or phosphorylation activity in non-insulin-dependent diabetes mellitus. J Clin Invest 1992; 89: 1069– 1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cline GW, Petersen KF, Krssak M, Shen J, Hundal RS, Trajanoski Z, Inzucchi S, Dresner A, Rothman DL, Shulman GI. Impaired glucose transport as a cause of decreased insulin-stimulated muscle glycogen synthesis in type 2 diabetes. N Engl J Med 1999; 341: 240– 246 [DOI] [PubMed] [Google Scholar]
- 136.Mandarino LJ, Printz RL, Cusi KA, Kinchington P, O'Doherty RM, Osawa H, Sewel C, Consoli A, Granner DK, DeFronzo RA. Regulation of hexokinase II and glycogen synthase mRNA, protein, and activity in human muscle. Am J Physiol 1995; 269: E701– E708 [DOI] [PubMed] [Google Scholar]
- 137.Vogt C, Yki-Jarvinen H, Iozzo P, Pipek R, Pendergrass M, Koval J, Ardehali H, Printz R, Granner D, DeFronzo RA, Mandarino L. Effects of insulin on subcellular localization of hexokinase II in human skeletal muscle in vivo. J Clin Endocrinol Metab 1998; 83: 230– 234 [DOI] [PubMed] [Google Scholar]
- 138.Mandarino LJ, Wright KS, Verity LS, Nichols J, Bell JM, Kolterman OG, Beck-Nielsen H. Effects of insulin infusion on human skeletal muscle pyruvate dehydrogenase, phosphofructokinase, and glycogen synthase: evidence for their role in oxidative and nonoxidative glucose metabolism. J Clin Invest 1987; 80: 655– 663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Shulman GI, Rothman DL, Jue T, Stein P, DeFronzo RA, Shulman RG. Quantitation of muscle glycogen synthesis in normal subjects and subjects with non-insulin-dependent diabetes by 13C nuclear magnetic resonance spectroscopy. N Engl J Med 1990; 322: 223– 228 [DOI] [PubMed] [Google Scholar]
- 140.Groop L, Saloranta C, Shank M, Bonadonna RC, Ferrannini E, DeFronzo RA. The role of free fatty acid metabolism in the pathogensis of insulin resistance in obesity and non-insulin dependent diabetes mellitus. J Clin Endocrinol Metab 1991; 72: 96– 107 [DOI] [PubMed] [Google Scholar]
- 141.Felber JP, Ferrannini E, Golay A, Meyer HV, Thiebaud D, Curchod B, Maeder E, Jequier E, DeFronzo RA. Role of lipid oxidation in the pathogenesis of insulin resistance of obesity and type II diabetes. Diabetes 1987; 36: 1341– 1350 [DOI] [PubMed] [Google Scholar]
- 142.Golay A, Felber JP, Jequier E, DeFronzo RA, Ferrannini E. Metabolic basis of obesity and non-insulin dependent diabetes mellitus. Diabetes/Metab Rev 1988; 4: 727– 747 [DOI] [PubMed] [Google Scholar]
- 143.Cusi K, Maezono K, Osman A, Pendergrass M, Patti ME, Pratipanawatr T, DeFronzo RA, Kahn CR, Mandarino LJ. Insulin resistance differentially affects the PI 3-kinase and MAP kinase-mediated signaling in human muscle. J Clin Invest 2000; 105: 311– 320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid metabolism. Nature 2001; 414: 799– 806 [DOI] [PubMed] [Google Scholar]
- 145.Tanijuchi CM, Emanuelli B, Kahn CR. Critical nodes in signaling pathways: insight into insulin action. Nat Rev Mol Cell Biol 2006; 7: 85– 96 [DOI] [PubMed] [Google Scholar]
- 146.Musi N, Goodyear LJ. Insulin resistance and improvements in signal transduction. Endocrine 2006; 29: 73– 80 [DOI] [PubMed] [Google Scholar]
- 147.Kashyap SR, DeFronzo RA. The insulin resistance syndrome: physiological considerations. Diabetes Vasc Dis Res 2007; 4: 13– 19 [DOI] [PubMed] [Google Scholar]
- 148.Kashyap SR, Roman LJ, McLain J, Masters BS, Bajaj M, Suraamornkul S, Belfort R, Berria R, Kellogg DL, Jr, Liu Y, DeFronzo R. Insulin resistance is associated with impaired nitric oxide synthase (NOS) activity in skeletal muscle of type 2 diabetic subjects. J Clin Endocrinol Metab 2005; 90: 1100– 1105 [DOI] [PubMed] [Google Scholar]
- 149.Montagnani M, Chen H, Barr VA, Quon MJ. Insulin-stimulated activation of eNOS is independent of Ca2+ but requires phosphorylation by Akt at Ser(1179). J Biol Chem 2001; 276: 30392– 30398 [DOI] [PubMed] [Google Scholar]
- 150.Miyazaki Y, He H, Mandarino LJ, DeFronzo RA. Rosiglitazone improves downstream insulin-receptor signaling in type 2 diabetic patients. Diabetes 2003; 52: 1943– 1950 [DOI] [PubMed] [Google Scholar]
- 151.Kashyap S, Belfort R, Berria R, Surammornkul S, Pratipanawatr T, Finalyson J, Barrentine A, Mandarino L, DeFronzo RA, Cusi K. Discordant effects of a chronic physiological increase in plasma FFA on insulin signaling in healthy subjects with or without a family history of type 2 diabetes. Am J Physiol Endocrinol Metab 2004; 287: E537– E546 [DOI] [PubMed] [Google Scholar]
- 152.Pratipanawatr W, Pratipanawatr T, Cusi K, Berria R, Jenkinson CP, Maezono K, DeFronzo RA, Mandarino L. Skeletal muscle insulin resistance in normoglycemic subjects with a strong family history of type 2 diabetes is associated with decreased insulin-stimulated IRS-1 tyrosine phosphorylation. Diabetes 2001; 50: 2572– 2578 [DOI] [PubMed] [Google Scholar]
- 153.Krook A, Bjornholm M, Galuska D, Jiang XJ, Fahlman R, Myers MG, Jr, Wallberg-Henriksson H, Zierath JR. Characterization of signal transduction and glucose transport in skeletal muscle from type 2 diabetic patients. Diabetes 2000; 49: 284– 292 [DOI] [PubMed] [Google Scholar]
- 154.Kim YB, Ciaraldi TP, Kong A, Kim D, Chu N, Mohideen P, Mudaliar S, Henry RR, Kahn BB. Troglitazone but not metformin restores insulin-stimulated phosphoinositide 3-kinase activity and increases p110beta protein levels in skeletal muscle of type 2 diabetic subjects. Diabetes 2002; 51: 443– 448 [DOI] [PubMed] [Google Scholar]
- 155.Hundal RS, Petersen KF, Mayerson AB, Randhawa PS, Inzucchi S, Shoelson SE, Shulman GI. Mechanism by which high-dose aspirin improves glucose metabolism in type 2 diabetes. J Clin Invest 2002; 109: 1321– 1326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bouzakri K, Roques M, Gual P, Espinosa S, Guebre-Egziabher F, Riou JP, Laville M, Le Marchand-Brustel Y, Tanti JF, Vidal H. Reduced activation of phosphatidylinositol-3 kinase and increased serine 636 phosphorylation of insulin receptor substrate-1 in primary culture of skeletal muscle cells from patients with type 2 diabetes. Diabetes 2003; 52: 1319– 1325 [DOI] [PubMed] [Google Scholar]
- 157.Wang CC, Goalstone ML, Draznin B. Molecular mechanisms of insulin resistance that impact cardiovascular biology. Diabetes 2004; 53: 2735– 2740 [DOI] [PubMed] [Google Scholar]
- 158.Draznin B. Molecular mechanisms of insulin resistance: serine phosphorylation of insulin receptor substrate-1 and increased expression of p85α: the two sides of a coin. Diabetes 2006; 55: 2392– 2397 [DOI] [PubMed] [Google Scholar]
- 159.Hsueh WA, Law RE. Insulin signaling in the arterial wall. Am J Cardiol 1999; 84: 21J– 24J [DOI] [PubMed] [Google Scholar]
- 160.Krook A, Bjornholm M, Galuska D, Jiang XJ, Fahlman R, Myers MG, Jr, Wallberg-Henriksson H, Zierath JR. Characterization of signal transduction and glucose transport in skeletal muscle from type 2 diabetic patients. Diabetes 2000; 49: 284– 292 [DOI] [PubMed] [Google Scholar]
- 161.Hanley AJ, Williams K, Stern MP, Haffner SM. Homeostasis model assessment of insulin resistance in relation to the incidence of cardiovascular disease: the San Antonio Heart Study. Diabetes Care 2002; 25: 1177– 1184 [DOI] [PubMed] [Google Scholar]
- 162.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683– 689 [DOI] [PubMed] [Google Scholar]
- 163.Rutter MK, Meigs JB, Sullivan LM, D'Agostino RB, Sr, Wilson PW. Insulin resistance, the metabolic syndrome, and incident cardiovascular events in the Framingham Offspring Study. Diabetes 2005; 54: 3252– 3257 [DOI] [PubMed] [Google Scholar]
- 164.Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Meigs JB, Bonadonna RC, Muggeo M. Insulin resistance as estimated by homeostasis model assessment predicts incident symptomatic cardiovascular disease in Caucasian subjects from the general population: the Bruneck study. Diabetes Care 2007; 30: 318– 324 [DOI] [PubMed] [Google Scholar]
- 165.Howard G, Bergman R, Wagenknecht LE, Haffner SM, Savage PJ, Saad MF, Laws A, D'Agostino RB., Jr Ability of alternative indices of insulin sensitivity to predict cardiovascular risk: comparison with the “minimal model”: Insulin Resistance Atherosclerosis Study (IRAS) Investigators. Ann Epidemiol 1998; 8: 358– 369 [DOI] [PubMed] [Google Scholar]
- 166.Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, Saggiani F, Poli M, Perbellini S, Raffaelli A, Cacciatori V, Santi L, Targher G, Bonadonna R, Muggeo M. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care 2002; 25: 1135– 1141 [DOI] [PubMed] [Google Scholar]
- 167.Mazzone T, Meyer PM, Feinstein SB, Davidson MH, Kondos GT, D'Agostino RB, Sr, Perez A, Provost JC, Haffner SM. Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: a randomized trial. JAMA 2006; 296: 2572– 2581 [DOI] [PubMed] [Google Scholar]
- 168.Nissen SE, Nicholls SJ, Wolski K, Nesto R, Kupfer S, Perez A, Jure H, De Larochelliere R, Staniloae CS, Mavromatis K, Saw J, Hu B, Lincoff AM, Tuzcu EMPERISCOPE Investigators Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA 2008; 299: 1561– 1573 [DOI] [PubMed] [Google Scholar]
- 169.Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefebvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Koranyi L, Laakso M, Mokan M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton JPROactive investigators Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005; 366: 1279– 1289 [DOI] [PubMed] [Google Scholar]
- 170.DeFronzo RA, Ferrannini E, Hendler R, Wahren J, Felig P. Influence of hyperinsulinemia, hyperglycemia, and the route of glucose administration on splanchnic glucose exchange. Proc Natl Acad Sci U S A 1978; 75: 5173– 5177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.DeFronzo RA, Ferrannini E, Wahren J, Felig P. Lack of gastrointestinal mediator of insulin action in maturity onset diabetes. Lancet 1978; 2: 1077– 1079 [DOI] [PubMed] [Google Scholar]
- 172.DeFronzo RA, Ferrannini E, Hendler R, Felig P, Wahren J. Regulation of splanchnic and peripheral glucose uptake by insulin and hyperglycemia. Diabetes 1983; 32: 35– 45 [DOI] [PubMed] [Google Scholar]
- 173.DeFronzo RA, Gunnarsson R, Bjorkman O, Olsson M, Wahren J. Effects of insulin on peripheral and splanchnic glucose metabolism in non-insulin-dependent (type II) diabetes mellitus. J Clin Invest 1985; 76: 149– 155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ferrannini E, Simonson DC, Katz LD, Reichard G, Bevilacqua S, Barrett EJ, Olsson M, DeFronzo RA. The disposal of an oral glucose load in patients with non-insulin dependent diabetes. Metabolism 1988; 37: 79– 85 [DOI] [PubMed] [Google Scholar]
- 175.Bays H, Mandarino L, DeFronzo RA. Role of the adipocytes, FFA, and ectopic fat in the pathogenesis of type 2 diabetes mellitus: PPAR agonists provide a rational therapeutic approach. J Clin Endocrinol Metab 2004; 89: 463– 478 [DOI] [PubMed] [Google Scholar]
- 176.Bays HE, Gonzalez-Campoy JM, Bray GA, Kitabchi AE, Bergman DA, Schorr AB, Rodbard HW, Henry RR. Pathogenic potential of adipose tissue and metabolic consequences of adipocyte hypertrophy and increased visceral adiposity. Expert Rev Cardio Ther 2008; 6: 343– 368 [DOI] [PubMed] [Google Scholar]
- 177.Bonadonna RC, DeFronzo RA. Glucose metabolism in obesity and type 2 diabetes. Diabete Metab 1991; 17: 112– 135 [PubMed] [Google Scholar]
- 178.DeFronzo RA. Dysfunctional fat cells, lipotoxicity, and type 2 diabetes. Int J Clin Pract Suppl 2004; 143: 9– 21 [DOI] [PubMed] [Google Scholar]
- 179.Fraze E, Donner CC, Swislocki AL, Chiou YA, Chen YD, Reaven GM. Ambient plasma free fatty acid concentrations in noninsulin-dependent diabetes mellitus: evidence for insulin resistance. J Clin Endocrinol Metab 1985; 61: 807– 811 [DOI] [PubMed] [Google Scholar]
- 180.Williamson JR, Kreisberg RA, Felts PW. Mechanism for the stimulation of gluconeogenesis by fatty acids in perfused rat liver. Proc Natl Acad Sci U S A 1966; 56: 247– 254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Bevilacqua S, Bonadonna R, Buzzigoli G, Boni C, Ciociaro D, Maccari F, Giorico MA, Ferrannini E. Acute elevation of free fatty acid levels leads to hepatic insulin resistance in obese subjects. Metabolism 1987; 36: 502– 506 [DOI] [PubMed] [Google Scholar]
- 182.Ferrannini E, Barrett EJ, Bevilacqua S, DeFronzo RA. Effect of fatty acids on glucose production and utilization in man. J Clin Invest 1983; 72: 1737– 1747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Thiebaud D, DeFronzo RA, Jacot E, Golay A, Acheson K, Maeder E, Jequier E, Felber JP. Effect of long chain triglyceride infusion on glucose metabolism in man. Metabolism 1982; 31: 1128– 1136 [DOI] [PubMed] [Google Scholar]
- 184.Felber JP, Vannotti A. Effects of fat infusion on glucose tolerance and insulin plasma levels. Int J Exp Med 1964; 10: 153– 156 [DOI] [PubMed] [Google Scholar]
- 185.Roden M, Price TB, Perseghin G, Petersen KF, Rothman DL, Cline GW, Shulman GI. Mechanism of free fatty acid-induced insulin resistance in humans. J Clin Invest 1996; 97: 2859– 2865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Carpentier A, Mittelman SD, Bergman RN, Giacca A, Lewis GF. Prolonged elevation of plasma free fatty acids impairs pancreatic beta-cell function in obese nondiabetic humans but not in individuals with type 2 diabetes. Diabetes 2000; 49: 399– 408 [DOI] [PubMed] [Google Scholar]
- 187.Salans LB, Bray GA, Cushman SW, Danforth E, Jr, Glennon JA, Horton ES, Sims EA. Glucose metabolism and the response to insulin by human adipose tissue in spontaneous and experimental obesity: effects of dietary composition and adipose cell size. J Clin Invest 1974; 53: 848– 856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Bray GA, Glennon JA, Salans LB, Horton ES, Danforth E, Jr, Sims EA. Spontaneous and experimental human obesity: effects of diet and adipose cell size on lipolysis and lipogenesis. Metabolism 1977; 26: 739– 747 [DOI] [PubMed] [Google Scholar]
- 189.Boden G, Shulman GI. Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and beta-cell dysfunction. Eur J Clin Invest 2002; 32( Suppl. 3): 14– 23 [DOI] [PubMed] [Google Scholar]
- 190.Bajaj M, Pratipanawatr T, Berria R, Pratipanawatr W, Kashyap S, Cusi K, Mandarino L, DeFronzo RA. Free fatty acids reduce splanchnic and peripheral glucose uptake in patients with type 2 diabetes. Diabetes 2002; 51: 3043– 3048 [DOI] [PubMed] [Google Scholar]
- 191.Richardson DK, Kashyap S, Bajaj M, Cusi K, DeFronzo RA, Jenkinson CP, Mandarino LJ. Lipid infusion induces an inflammatory/fibrotic response and decreases expression of nuclear encoded mitochondrial genes in human skeletal muscle. J Biol Chem 2005; 280: 10290– 10297 [DOI] [PubMed] [Google Scholar]
- 192.Dresner A, Laurent D, Marcucci M, Griffin ME, Dufour S, Cline GW, Slezak LA, Andersen DK, Hundal RS, Rothman DL, Petersen KF, Shulman GI. Effects of free fatty acids on glucose transport and IRS-1-associated phosphatidylinositol 3-kinase activity. J Clin Invest 1999; 103: 253– 259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Griffin ME, Marcucci MJ, Cline GW, Bell K, Barucci N, Lee D, Goodyear LJ, Kraegen EW, White MF, Shulman GI. Free fatty acid-induced insulin resistance is associated with activation of protein kinase C theta and alterations in the insulin signaling cascade. Diabetes 1999; 48: 1270– 1274 [DOI] [PubMed] [Google Scholar]
- 194.Itani SI, Ruderman NB, Schmieder F, Boden G. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IκB-α. Diabetes 2002; 51: 2005– 2011 [DOI] [PubMed] [Google Scholar]
- 195.Randle PJ, Garland PB, Hales CN, Newsholme EA. The glucose fatty-acid cycle: its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1963; 1: 785– 789 [DOI] [PubMed] [Google Scholar]
- 196.Mandarino LJ, Consoli A, Jain A, Kelley DE. Interaction of carbohydrate and fat fuels in human skeletal muscle: impact of obesity and NIDDM. Am J Physiol 1996; 270: E463– E470 [DOI] [PubMed] [Google Scholar]
- 197.Kelley D, Mandarino L. Fuel selection in human skeletal muscle in insulin resistance: a reexamination. Diabetes 2000; 49: 677– 683 [DOI] [PubMed] [Google Scholar]
- 198.Wititsuwannakul D, Kim KH. Mechanism of palmityl coenzyme A inhibition of liver glycogen synthase. J Biol Chem 1977; 252: 7812– 7817 [PubMed] [Google Scholar]
- 199.Johnson AB, Argyraki M, Thow JC, Cooper BG, Fulcher G, Taylor R. Effect of increased free fatty acid supply on glucose metabolism and skeletal muscle glycogen synthase activity in normal man. Clin Science 1992; 82: 219– 226 [DOI] [PubMed] [Google Scholar]
- 200.Pendergrass M, Nucci G, DeFronzo R. In vivo glucose transport (GT) and phosphorylation (GP) in skeletal muscle are impaired by elevation of plasma FFA (Abstract). Diabetes 1998; 47:( Suppl. 1): A65 [Google Scholar]
- 201.Belfort R, Mandarino L, Kashyap S, Wirfel K, Pratipanawatr T, Berria R, Cusi K, DeFronzo RA. Dose response effect of elevated plasma FFA on insulin signaling. Diabetes 2005; 54: 1640– 1648 [DOI] [PubMed] [Google Scholar]
- 202.Petersen KF, Dufour S, Shulman GI. Decreased insulin-stimulated ATP synthesis and phosphate transport in muscle of insulin-resistant offspring of type 2 diabetic parents. Plos Med 2005; 2: 879– 884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Yu C, Chen Y, Cline GW, Zhang D, Zong H, Wang Y, Bergeron R, Kim JK, Cushman SW, Cooney GJ, Atcheson B, White MF, Kraegen EW, Shulman GI. Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem 2002; 277: 50230– 50236 [DOI] [PubMed] [Google Scholar]
- 204.Ellis BA, Poynten A, Lowy AJ, Furler SM, Chisholm DJ, Kraegen EW, Cooney GJ. Long-chain acyl-CoA esters as indicators of lipid metabolism and insulin sensitivity in rat and human muscle. Am J Physiol Endocrinol Metab 2000; 279: E554– E560 [DOI] [PubMed] [Google Scholar]
- 205.Coletta DK, Sriwijitkamol A, Wajcberg E, Tantiwong P, Li M, Prentki M, Madiraju M, Jenkinson CP, Cersosimo E, Musi N, DeFronzo RA. Pioglitazone stimulates AMPK signalling and increases the expression of genes involved in adiponectin signalling, mitochondrial function and fat oxidation in human skeletal muscle in vivo. Diabetologia In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Bajaj M, Suraamornkul S, Romanelli A, Cline GW, Mandarino LJ, Shulman GI, DeFronzo RA. Effect of sustained reduction in plasma free fatty acid concentration on intramuscular long chain-fatty acyl-CoAs and insulin action in patients with type 2 diabetes. Diabetes 2005; 54: 3148– 3153 [DOI] [PubMed] [Google Scholar]
- 207.Attie AD, Kendziorski CM. PGC-1alpha at the crossroads of type 2 diabetes. Nat Genet 2003; 34: 244– 245 [DOI] [PubMed] [Google Scholar]
- 208.Puigserver P, Spiegelman BM. Peroxisome proliferator-activated receptor-gamma coactivator 1 alpha (PGC-1 alpha): transcriptional coactivator and metabolic regulator. Endocrine Rev 2003; 24: 78– 90 [DOI] [PubMed] [Google Scholar]
- 209.Mootha VK, Handschin C, Arlow D, Xie X, St Pierre J, Sihag S, Yang W, Altshuler D, Puigserver P, Patterson N, Willy PJ, Schulman IG, Heyman RA, Lander ES, Spiegelman BM. Erralpha and Gabpa/b specify PGC-1alpha-dependent oxidative phosphorylation gene expression that is altered in diabetic muscle. Proc Natl Acad Sci U S A 2004; 101: 6570– 6575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell 1999; 98: 115– 124 [DOI] [PubMed] [Google Scholar]
- 211.Montell E, Turini M, Marotta M, Roberts M, Noe V, Ciudad CJ, Mace K, Gomez-Foix AM. DAG accumulation from saturated fatty acids desensitizes insulin stimulation of glucose uptake in muscle cells. Am J Physiol Endocrinol Metab 2001; 280: E229– E237 [DOI] [PubMed] [Google Scholar]
- 212.Adams JM, Pratipanawatr T, Berria R, Wang E, DeFronzo RA, Sullards MC, Mandarino LJ. Ceramide content is increased in skeletal muscle from obese insulin resistant humans. Diabetes 2004; 53: 25– 31 [DOI] [PubMed] [Google Scholar]
- 213.Haus JM, Kashyap SR, Kasumov T, Zhang R, Kelly KR, DeFronzo RA, Kirwan JP. Plasma ceramides are elevated in obese subjects with type 2 diabetes and are associated with the level of insulin resistance. Diabetes 2009; 58: 337– 343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Richardson DK, Kashyap S, Bajaj M, Cusi K, DeFronzo RA, Jenkinson CP, Mandarino LJ. Lipid infusion induces an inflammatory/fibrotic response and decreases expression of nuclear encoded mitochondrial genes in human skeletal muscle. J Biol Chem 2005; 280: 10290– 10297 [DOI] [PubMed] [Google Scholar]
- 215.Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, Miyazaki Y, Kohane I, Costello M, Saccone R, Landaker EJ, Goldfine AB, Mun E, DeFronzo R, Finlayson J, Kahn CR, Mandarino LJ. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: Potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A 2003; 100: 8466– 8471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstrale M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 2003; 34: 267– 273 [DOI] [PubMed] [Google Scholar]
- 217.Abdul-Ghani MA, Mueller FL, Liu Y, Chavez A, Balas B, Tripathy D, Jani R, Monroy A, Folli F, van Remmen H, DeFronzo RA. Deleterious action of fatty acids on mitochondrial ATP synthsis: the link between lipotoxicity, mitochondrial dysfunction, and insulin resistance. Am J Physiol 2008; 295: E678– E685 [DOI] [PubMed] [Google Scholar]
- 218.Cervera A, Wajcberg E, Sriwijitkamol A, Fernandez M, Zuo P, Triplitt C, Musi N, DeFronzo RA, Cersosimo E. Mechanisms of action of exenatide to reduce postprandial hyperglycemia in type 2 diabetes. Am J Physiol Endocrinol Metab 2008; 294: E846– E852 [DOI] [PubMed] [Google Scholar]
- 219.Cervera A, Wajcberg E, Triplitt C, Fernandez M, Zuo P, DeFronzo RA, Cersosimo E. Improved splanchnic glucose metabolism is responsible for glycemic control in T2DM subjects treated with exenatide (Abstract). Diabetes 2007; 56( Suppl. 1): A404 [Google Scholar]
- 220.Edgerton DS, Johnson KMS, Neal DW, Scott M, Hobbs CH, Zhang X, Duttaroy A, Cherrington AD. Inhibition of dipeptidyl peptidase-4 by vildagliptin during glucagon-like peptide-1 infusion increases liver glucose uptake in the conscious dog. Diabetes 2009; 58: 243– 249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Ionut V, Zheng D, Stefanovski D, Bergman RN. Exenatide can reduce glucose independent of islet hormones or gastric emptying. Am J Physiol Endocrinol Metab 2008; 295: E269– E277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Reaven GM, Chen YD, Golay A, Swislocki AL, Jaspan JB. Documentation of hyperglucagonemia throughout the day in nonobese and obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1987; 64: 106– 110 [DOI] [PubMed] [Google Scholar]
- 223.Unger RH, Aguilar-Parada E, Muller WA, Eisentraut AM. Studies of pancreatic α-cell function in normal and diabetic subjects. J Clin Invest 1970; 49: 837– 848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Boden G, Soriano M, Hoeldtke RD, Owen OE. Counterregulatory hormone release and glucose recovery after hypoglycemia in non-insulin-dependent diabetic patients. Diabetes 1983; 32: 1055– 1059 [DOI] [PubMed] [Google Scholar]
- 225.Triplitt C, DeFronzo RA. Exenatide: first in class incretin mimetic for the treatment of type 2 diabetes mellitus. Expert Rev Endocrinol Metab 2006; 1: 329– 341 [DOI] [PubMed] [Google Scholar]
- 226.Petersen KF, Sullivan JT. Effects of a novel glucagon receptor antagonist (Bay 27–9955) on glucagon-stimulated glucose production in humans. Diabetologia 2001; 44: 2018– 2024 [DOI] [PubMed] [Google Scholar]
- 227.DeFronzo RA, Abdul-Ghani M. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocrine Practice In press [DOI] [PubMed] [Google Scholar]
- 228.Noonan WT, Shaprio VM, Banks RO. Renal glucose reabsorption during hypertonic glucose infusion in female streptozotocin-induced diabetic rats. Life Sci 2001; 68: 2967– 2977 [DOI] [PubMed] [Google Scholar]
- 229.Dominguez JH, Camp K, Maianu L, Feister H, Garvey WT. Molecular adaptations of GLUT1 and GLUT2 in renal proximal tubules of diabetic rats. Am J Physiol 1994; 266: F283– F290 [DOI] [PubMed] [Google Scholar]
- 230.Kamran M, Peterson RG, Dominguez JH. Overexpression of GLUT2 gene in renal proximal tubules of diabetic Zucker rats. J Am Soc Nephol 1997; 8: 943– 948 [DOI] [PubMed] [Google Scholar]
- 231.Mogensen CE. Maximum tubular reabsorpiton capacity for glucose and renal hemodynamics during rapid hypertonic glucose infusion in normal and diabetic subjects. Scan J Clin Lab Invest 1971; 28: 101– 109 [DOI] [PubMed] [Google Scholar]
- 232.Rahmoune H, Thompson PW, Ward JM, Smith CD, Hong G, Brown J. Glucose transporters in human renal proximal tubular cells isolated from the urine of patients with non–insulin-dependent diabetes. Diabetes 2005; 54: 3427– 3434 [DOI] [PubMed] [Google Scholar]
- 233.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 2004; 291: 2847– 2850 [DOI] [PubMed] [Google Scholar]
- 234.Porte D. Central regulation of energy homeostasis. Diabetes 2006; 55( Suppl. 2): S155– S160 [Google Scholar]
- 235.Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DC. Central nervous system control of food intake. Nature 2000; 404: 661– 671 [DOI] [PubMed] [Google Scholar]
- 236.Bruning JC, Gautam D, Burks DJ, Gillette J, Schubert M, Orban PC, Klein R, Krone W, Muller-Wieland D, Kahn CR. Role of brain insulin receptor in control of body weight and reproduction. Science 2000; 289: 2122– 2125 [DOI] [PubMed] [Google Scholar]
- 237.Plum L, Belgardt BF, Bruning JC. Central insulin action in energy and glucose homeostasis. J Clin Invest 2006; 116: 1761– 1766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Matsuda M, Liu Y, Mahankali S, Pu Y, Mahankali A, Wang J, DeFronzo RA, Fox PT, Gao JH. Altered hypothalamic function in response to glucose ingestion in obese humans. Diabetes 1999; 48: 1801– 1806 [DOI] [PubMed] [Google Scholar]
- 239.Obici S, Feng Z, Karkanias G, Baskin DG, Rossetti L. Decreasing hypothalamic insulin receptors causes hyperphagia and insulin resistance in rats. Nat Neurosci 2002; 5: 566– 572 [DOI] [PubMed] [Google Scholar]
- 240.Obici S, Feng Z, Tan J, Liu L, Karkanias G, Rossetti L. Central melanocortin receptors regulate insulin action. J Clin Invest 2001; 108: 1079– 1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Cusi K, Consoli A, DeFronzo RA. Metabolic effects of metformin on glucose and lactate metabolism in NIDDM. J Clin Endocrinol Metab 1996; 81: 4059– 4067 [DOI] [PubMed] [Google Scholar]
- 242.DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin dependent diabetes mellitus. N Engl J Med 1995; 333: 541– 549 [DOI] [PubMed] [Google Scholar]
- 243.Cusi K, DeFronzo RA. Metformin: a review of its metabolic effects. Diabetes Reviews 1998; 6: 89– 131 [Google Scholar]
- 244.Miyazaki Y, Mahankali A, Matsuda M, Glass L, Mahankali S, Ferranini E, Cusi K, Mandarino L, DeFronzo RA. Improved glycemic control and enhanced insulin sensitivity in liver and muscle in type 2 diabetic subjects treated with pioglitazone. Diabetes Care 2001; 24: 710– 719 [DOI] [PubMed] [Google Scholar]
- 245.Miyazaki Y, Glass L, Triplitt C, Matsuda M, Cusi K, Mandarino L, DeFronzo RA. Effect of rosiglitazone on glucose and free fatty acid metabolism in type 2 diabetic patients. Diabetologia 2001; 44: 2210– 2219 [DOI] [PubMed] [Google Scholar]
- 246.Miyazaki Y, Mahankali A, Matsuda M, Mahankali S, Hardies J, Cusi K, Mandarino LJ, DeFronzo RA. Effect of pioglitazone on abdominal fat distribution and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab 2002; 87: 2784– 2791 [DOI] [PubMed] [Google Scholar]
- 247.Bajaj M, Suraamornkul S, Hardies LJ, Pratipanawatr T, DeFronzo RA. Plasma resistin concentration, hepatic fat content, and hepatic and peripheral insulin resistance in pioglitazone-treated type 2 diabetic patients. Internatl J Obesity 2004; 28: 783– 789 [DOI] [PubMed] [Google Scholar]
- 248.Bajaj M, Soraamornkul S, Glass L, Musi N, DeFronzo RA. Effects of PPARα and PPARγ agonists on glucose and lipid metabolism in patients with type 2 diabetes mellitus. Diabetes 2005; 54: 3148– 3153 [DOI] [PubMed] [Google Scholar]
- 249.Gastaldelli Am, Miyazaki Y, Mahankali A, Berria R, Pettiti M, Buzzigoli E, Ferrannini E, DeFronzo RA. The effect of pioglitazone on the liver. Diabetes Care 2006; 29: 2275– 2281 [DOI] [PubMed] [Google Scholar]
- 250.Gastaldelli A, Miyazaki Y, Matsuda M, Pettiti M, Santini E, Ferrannini E, DeFronzo R. The effect of rosiglitazone on the liver: decreased gluconeogenesis in patients with type 2 diabetes. J Clin Endocrinol Metab 2006; 91: 806– 812 [DOI] [PubMed] [Google Scholar]
- 251.Bajaj M, Suraamornkul S, Hardies LJ, Glass L, Musi N, DeFronzo RA. Effects of peroxisome proliferator-activated receptor (PPAR)-alpha and PPAR-gamma agonists on glucose and lipid metabolism in patients with type 2 diabetes mellitus. Diabetologia 2007; 50: 1723– 1731 [DOI] [PubMed] [Google Scholar]
- 252.Miyazaki Y, DeFronzo RA. Rosiglitazone and pioglitazone similarly improve insulin sensitivity and secretion, glucose tolerance and adipocytokines in type 2 diabetic patients. Diabetes Obes Metab 2008; 10: 1204– 1211 [DOI] [PubMed] [Google Scholar]
- 253.Natali A, Ferrannini E. Effects of metformin and thiazolidinediones on suppression of hepatic glucose production and stimulation of glucose uptake in type 2 diabetes: a systematic review. Diabetologia 2006; 49: 434– 441 [DOI] [PubMed] [Google Scholar]
- 254.Kim YB, Ciaraldi TP, Kong A, Kim D, Chu N, Mohideen P, Mudaliar S, Henry RR, Kahn BB. Troglitazone but not metformin restores insulin-stimulated phosphoinositide 3-kinase activity and increases p110-β protein levels in skeletal muscle of type 2 diabetic subjects. Diabetes 2002; 51: 443– 448 [DOI] [PubMed] [Google Scholar]
- 255.Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 2001; 108: 1167– 1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Musi N, Hirshman MF, Nygren J, Svanfeldt M, Bavenholm P, Rooyackers O, Zhou G, Williamson JM, Ljunqvist O, Efendic S, Moller DE, Thorell A, Goodyear LJ. Metformin increases AMP-activated protein kinase activity in skeletal muscle of subjects with type 2 diabetes. Diabetes 2002; 51: 2074– 2081 [DOI] [PubMed] [Google Scholar]
- 257.Einhorn D, Rendell M, Rosenzweig J, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride in combination with metformin in the treatment of type 2 diabetes mellitus: a randomized, placebo-controlled study. The Pioglitazone 027 Study Group. Clin Ther 2000; 22: 1395– 1409 [DOI] [PubMed] [Google Scholar]
- 258.Fonseca V, Rosenstock J, Patwardhan R, Salzman A. Effect of metformin and rosiglitazone combination therapy in patients with type 2 diabetes mellitus: a randomized controlled trial. JAMA 2000; 283: 1695– 1702 [DOI] [PubMed] [Google Scholar]
- 259.Matthews DR, Charbonnel BH, Hanefeld M, Brunetti P, Schernthaner G. Long-term therapy with addition of pioglitazone to metformin compared with the addition of gliclazide to metformin in patients with type 2 diabetes: a randomized, comparative study. Diab/Metab Res Rev 2005; 21: 167– 174 [DOI] [PubMed] [Google Scholar]
- 260.Charbonnel B, Schernthaner G, Brunetti P, Matthews DR, Urquhart R, Tan MH, Hanefeld M. Long-term efficacy and tolerability of add-on pioglitazone therapy to failing monotherapy compared with addition of gliclazide or metformin in patients with type 2 diabetes. Diabetologia 2005; 48: 1093– 1104 [DOI] [PubMed] [Google Scholar]
- 261.Inzucchi SE, Maggs DG, Spollett GR, Page SL, Rife FS, Walton V, Shulman GI. Efficacy and metabolic effects of metformin and troglitazone in type II diabetes mellitus. N Engl J Med 1998; 338: 867– 872 [DOI] [PubMed] [Google Scholar]
- 262.Bajaj M, DeFronzo RA. Combination therapy in type 2 diabetes. In_International Textbook of Diabetes Mellitus_3rd ed DeFronzo RA, Ferrannini E, Keen H, Zimmet P. Eds. New York, Wiley, 2004, p. 915– 950 [Google Scholar]
- 263.Miyazaki Y, Glass L, Triplitt C, Matsuda M, Cusi K, Mandarino L, DeFronzo RA. Effect of rosiglitazone on glucose and free fatty acid metabolism in type 2 diabetic patients. Diabetologia 2001; 44: 2210– 2219 [DOI] [PubMed] [Google Scholar]
- 264.Miyazaki Y, Mahankali A, Matsuda M, Mahankali S, Hardies J, Cusi K, Mandarino LJ, DeFronzo RA. Effect of pioglitazone on abdominal fat distribution and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab 2002; 87: 2784– 2791 [DOI] [PubMed] [Google Scholar]
- 265.Bajaj M, Suraamornkul S, Pratipanawatr T, Hardies LJ, Pratipanawatr W, Glass L, Miyazaki Y, DeFronzo RA. Pioglitazone reduces hepatic fat content and augments splanchnic glucose uptake in patients with type 2 diabetes. Diabetes 2003; 52: 1364– 1370 [DOI] [PubMed] [Google Scholar]
- 266.Belfort R, Harrison SA, Brown K, Darfland C, Finch J, Hardies J, Balas B, Gastaldelli A, Tio F, Puicini J, Berria R, Mia JZ, Dwivedi S, Havranek R, Fincke C, DeFronzo RA, Bannayan GA, Schenker S, Cusi K. A placebo controlled trial of pioglitazone in patients with non-alcoholic steatohepatitis. N Engl J Med 2006; 355: 2297– 2307 [DOI] [PubMed] [Google Scholar]
- 267.Yki-Jarvinen H. Thiazolidinediones. N Engl J Med 2004; 351: 1106– 1118 [DOI] [PubMed] [Google Scholar]
- 268.Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, Kravitz BG, Lachin JM, O'Neill MC, Zinman B, Viberti GADOPT Study Group Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006; 355: 2427– 2443 [DOI] [PubMed] [Google Scholar]
- 269.Hanefeld M, Pfutzner A, Forst T, Lubben G. Glycemic control and treatment failure with pioglitazone versus glibenclamide in type 2 diabetes mellitus: a 42-month, open-label, observational, primary care study. Cur Med Res Opinion 2006; 22: 1211– 1215 [DOI] [PubMed] [Google Scholar]
- 270.Tan MH, Baksi A, Krahulec B, Kubalski P, Stankiewicz A, Urquhart R, Edwards G, Johns DGLAL Study Group Comparison of pioglitazone and gliclazide in sustaining glycemic control over 2 years in patients with type 2 diabetes. Diabetes Care 2005; 28: 544– 550 [DOI] [PubMed] [Google Scholar]
- 271.Rosenstock J, Goldstein BJ, Vinik AI, O'neill MC, Porter LE, Heise MA, Kravitz B, Dirani RG, Freed MIRESULT Study Group Effect of early addition of rosiglitazone to sulphonylurea therapy in older type 2 diabetes patients (>60 years): the Rosiglitazone Early vs. SULphonylurea Titration (RESULT) study. Diab Obes Metab 2006; 8: 49– 57 [DOI] [PubMed] [Google Scholar]
- 272.Home PD, Jones NP, Pocock SJ, Beck-Nielsen H, Gomis R, Hanefeld M, Komajda M, Curtis P; RECORD Study Group Rosiglitazone RECORD study: glucose control outcomes at 18 months. Diabet Med 2007; 24: 626– 634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Bunck MC, Diamant M, Cornér A, Eliasson B, Malloy JL, Shaginian RM, Deng W, Kendall DM, Taskinen MR, Smith U, Yki-Järvinen H, Heine RJ. One-year treatment with exenatide improves β-cell function, compared with insulin glargine, in metformin-treated type 2 diabetic patients: a randomized, controlled trial. Diabetes Care In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.DeFronzo RA, Ratner RE, Han J, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care 2005; 28: 1092– 1100 [DOI] [PubMed] [Google Scholar]
- 275.Klonoff DC, Buse JB, Nielsen LL, Guan X, Bowlus CL, Holcombe JH, Wintle ME, Maggs DG. Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr Med Res Opin 2008; 24: 275– 286 [DOI] [PubMed] [Google Scholar]
- 276.Johnson JA, Majumdar SR, Simpson SH, Toth EL. Decreased mortality associated with the use of metformin compared with sulfonylurea monotherapy in type 2 diabetes. Diabetes Care 2002; 25: 2244– 2248 [DOI] [PubMed] [Google Scholar]
- 277.Evans JM, Ogston SA, Emslie-Smith A, Morris AD. Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia 2006; 49: 930– 936 [DOI] [PubMed] [Google Scholar]
- 278.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UPKDS 34). Lancet 1998; 352: 854– 865 [PubMed] [Google Scholar]
- 279.Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA 1999; 281: 2005– 2012 [DOI] [PubMed] [Google Scholar]
- 280.U.K. Prospective Diabetes Diabetes Study Group UKPDS 28: a randomized trial of efficacy of early addition of metformin in sulfonylurea-treated type 2 diabetes. Diabetes Care 1998; 21: 87– 92 [DOI] [PubMed] [Google Scholar]
- 281.Wright A, Burden AC, Paisey RB, Cull CA, Holman RRU.K. Prospective Diabetes Study Group Sulfonylurea inadequacy: efficacy of addition of insulin over 6 years in patients with type 2 diabetes in the U.K. Prospective Diabetes Study (UKPDS 57). Diabetes Care 2002; 25: 330– 336 [DOI] [PubMed] [Google Scholar]
- 282.Matthews DR, Cull CA, Stratton IM, Holman RR, Turner RC. UKPDS 26: Sulphonylurea failure in non-insulin-dependent diabetic patients over six years. UK Prospective Diabetes Study (UKPDS) Group. Diabet Med 1998; 15: 297– 303 [DOI] [PubMed] [Google Scholar]
- 283.U.K. prospective diabetes study 16 Overview of 6 years' therapy of type II diabetes: a progressive disease. U.K. Prospective Diabetes Study Group. Diabetes 1995; 44: 1249– 1258 [PubMed] [Google Scholar]
- 284.Lupi R, Del Guerra S, Tellini C, Giannarelli R, Coppelli A, Lorenzetti M, Carmellini M, Mosca F, Navalesi R, Marchetti P. The biguanide compound metformin prevents desensitization of human pancreatic islets induced by high glucose. Eur J Pharmacol 1999; 364: 205– 209 [DOI] [PubMed] [Google Scholar]
- 285.Lupi R, Del Guerra S, Fierabracci V, Marselli L, Novelli M, Patane G, Boggi U, Mosca F, Piro S, Del Prato S, Marchetti P. Lipotoxicity in human pancreatic islets and the protective effect of metformin. Diabetes 2002; 51( Suppl. 1): S134– S137 [DOI] [PubMed] [Google Scholar]
- 286.Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, Ochoa C, Kawakubo M, Buchanan TA. Effect of pioglitazone on pancreatic β-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes 2006; 55: 517– 522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.The Dream (Diabetes Reduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomized controlled trial. Lancet 2006; 368: 1096– 1105 [DOI] [PubMed] [Google Scholar]
- 288.Knowler WC, Hamman RF, Edelstein SL, Barrett-Connor E, Ehrmann DA, Walker EA, Fowler SE, Nathan DM, Kahn SEthe Diabetes Prevention Program Research Group Prevention of type 2 diabetes with troglitazone in the Diabetes Prevention Program. Diabetes 2005; 54: 1150– 1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Buchanan TA, Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, Ochoa C, Tan S, Berkowitz K, Hodis HN, Azen SP. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk hispanic women. Diabetes 2002; 51: 2796– 2803 [DOI] [PubMed] [Google Scholar]
- 290.DeFronzo RA, Banerji MA, Bray G, Buchanan T, Clement S, Henry R, Kitabchi A, Mudaliar S, Musi N, Ratner R, Reaven P, Schwenke D, Stenz F, Tripathy D. ACTos NOW for the prevention of diabetes (ACT NOW) study Late-breaking abstract presented at the 68th Annual Meeting of the American Diabetes Association, 6–10 June 2008, San Francisco, California [Google Scholar]
- 291.Lupi R, Del Guerra S, Marselli L, Bugliani M, Boggi U, Mosca F, Marchetti P, Del Prato S. Rosiglitazone prevents the impairment of human islet function induced by fatty acids: evidence for a role of PPARgamma2 in the modulation of insulin secretion. Am J Physiol Endocrinol Metab 2004; 286: E560– E567 [DOI] [PubMed] [Google Scholar]
- 292.Finegood DT, McArthur MD, Kojwang D, Thomas MJ, Topp BG, Leonard T, Buckingham RE. β-Cell mass dynamics in Zucker diabetic fatty rats: rosiglitazone prevents the rise in net cell death. Diabetes 2001; 50: 1021– 1029 [DOI] [PubMed] [Google Scholar]
- 293.Kim HI, Cha JY, Kim SY, Kim JW, Roh KJ, Seong JK, Lee NT, Choi KY, Kim KS, Ahn YH. Peroxisomal proliferator–activated receptor-γ upregulates glucokinase gene expression in β-cells. Diabetes 2002; 51: 676– 685 [DOI] [PubMed] [Google Scholar]
- 294.Santini E, Fallahi P, Ferrari SM, Masoni A, Antonelli A, Ferrannini E. Effect of PPAR-gamma activation and inhibition on glucose-stimulated insulin release in INS-1e cells. Diabetes 2004; 53( Suppl. 3): S79– S83 [DOI] [PubMed] [Google Scholar]
- 295.Masuda K, Okamoto Y, Tsuura Y, Kato S, Miura T, Tsuda K, Horikoshi H, Ishida H, Seino Y. Effects of Troglitazone (CS-045) on insulin secretion in isolated rat pancreatic islets and HIT cells: an insulinotropic mechanism distinct from glibenclamide. Diabetologia 1995; 38: 24– 30 [DOI] [PubMed] [Google Scholar]
- 296.Tourrel C, Bailbe D, Meile MJ, Kergoat M, Portha B. Glucagon-like peptide-1 and exendin-4 stimulate beta-cell neogenesis in streptozotocin-treated newborn rats resulting in persistently improved glucose homeostasis at adult age. Diabetes 2001; 50: 1562– 1570 [DOI] [PubMed] [Google Scholar]
- 297.Kim JG, Baggio LL, Bridon DP, Castaigne JP, Robitaille MF, Jette L, Benquet C, Drucker DJ. Development and characterization of a glucagon-like peptide 1-albumin conjugate: the ability to activate the glucagon-like peptide 1 receptor in vivo. Diabetes 2003; 52: 751– 759 [DOI] [PubMed] [Google Scholar]
- 298.Farilla L, Bulotta A, Hirshberg B, Li Calzi S, Khoury N, Noushmehr H, Bertolotto C, Di Mario U, Harlan DM, Perfetti R. Glucagon-like peptide 1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology 2003; 144: 5149– 5158 [DOI] [PubMed] [Google Scholar]
- 299.Ahren B, Pacini G, Foley JE, Schweizer A. Improved meal-related beta-cell function and insulin sensitivity by the dipeptidyl peptidase-IV inhibitor vildagliptin in metformin-treated patients with type 2 diabetes over 1 year. Diabetes Care 2005; 28: 1936– 1940 [DOI] [PubMed] [Google Scholar]
- 300.Deacon CF. Dipeptidyl peptidase 4 inhibition with sitagliptin: a new therapy for type 2 diabetes. Expert Opin Invest Drugs 2007; 16: 533– 545 [DOI] [PubMed] [Google Scholar]
- 301.Balas B, Baig MR, Watson C, Dunning BE, Ligueros-Saylan M, Wang Y, He YL, Darland C, Holst JJ, Deacon CF, Cusi K, Mari A, Foley JE, DeFronzo RA. The dipeptidyl peptidase IV inhibitor vildagliptin suppresses endogenous glucose production and enhances islet function after single-dose administration in type 2 diabetic patients. J Clin Endocrinol Metab 2007; 92: 1249– 1255 [DOI] [PubMed] [Google Scholar]
- 302.Riddle MC, Rosenstock J, Gerich JInsulin Glargine 4002 Study Investigators The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003; 26: 3080– 3086 [DOI] [PubMed] [Google Scholar]
- 303.Yki-Jarvinen H, Ryysy L, Nikkila K, Tulokas T, Vanamo R, Heikkila M. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med 1999; 130: 389– 396 [DOI] [PubMed] [Google Scholar]
- 304.Holman RR, Thorne KI, Farmer AJ, Davies MJ, Keenan JF, Paul S, Levy JCfor the 4-T study group Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med 2007; 357: 1716– 1730 [DOI] [PubMed] [Google Scholar]
- 305.Henry RR, Gumbiner B, Ditzler T, Wallace P, Lyon R, Glauber HS. Intensive conventional insulin therapy for type II diabetes. Metabolic effects during a 6-mo outpatient trial. Diabetes Care 1993; 16: 21– 31 [DOI] [PubMed] [Google Scholar]
- 306.Heine RJ, Van Gaal LF, Johns D, Mihm MJ, Widel MH, Brodows RGGWAA Study Group Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med 2005; 143: 559– 569 [DOI] [PubMed] [Google Scholar]
- 307.Barnett AH, Burger J, Johns D, Brodows R, Kendall DM, Roberts A, Trautmann ME. Tolerability and efficacy of exenatide and titrated insulin glargine in adult patients with type 2 diabetes previously uncontrolled with metformin or a sulfonylurea: a multinational, randomized, open-label, two-period, crossover noninferiority trial. Clin Thera 2007; 29: 2333– 2348 [DOI] [PubMed] [Google Scholar]
- 308.Nauck MA, Duran S, Kim D, Johns D, Northrup J, Festa A, Brodows R, Trautmann M. A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study. Diabetologia 2007; 50: 259– 267 [DOI] [PubMed] [Google Scholar]
- 309.Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009; 32: 193– 203 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online-Only Appendix