Case Report: Severe Melorheostosis Involving the Ipsilateral Extremities (original) (raw)
Abstract
Melorheostosis is a rare, noninheritable bone dysplasia characterized by its classic radiographic feature of flowing hyperostosis resembling dripping candle wax, generally on one side of the long bone. The condition originally was described by Leri and Joanny in 1922. Its etiology remains speculative, and treatment in most instances has been symptomatic. Melorheostosis usually affects one limb, more often the lower extremity, and rarely the axial skeleton. We report a rare case of severe melorheostosis in the ipsilateral upper and lower extremities with normal contralateral extremities. The plain radiographs revealed almost all the bones in the affected extremities, from clavicle and scapula to distal phalanges of the fingers and from femur to distal phalanges of the toes, presented extensive, dense hyperostosis and heterotopic ossification in the periarticular soft tissue. Physical examination showed considerable swelling and deformities of the left limbs, stiffness and distortion of the joints, and anesthesia in the left ulnar regions of the forearm and hand. The examination of the right side was normal. Computed tomography scans showed multiple areas of classic candle wax-like hyperostosis and narrowing or disappearance of the medullary cavity. Histologic analysis confirmed the clinical and imaging diagnosis and revealed extremely dense sclerotic bone of cortical pattern.
Introduction
Melorheostosis is a rare benign sclerosing bone dysplasia. The name is derived from the Greek terms melos (limbs), rheos (flow), and osteon (bone). This disorder tends to be segmental [6, 8, 11]. It may result in pain, limb-length inequality, joint stiffness, progressive deformity, ossification in adjacent soft tissues, and others [4, 10, 11].
One possible etiology of melorheostosis is a loss of function mutation in the LEMD3 gene (12q12–12q14.3), a protein of the inner nuclear membrane involved in bone morphogenic protein and tumor growth factor-β signaling [5]. However, another study did not find mutation in three patients with sporadic melorheostosis [12]. The exact causes remain unclear.
We report the case of a 44-year-old Asian woman who experienced limb pain, swelling, deformity, and limitation of motion for more than 30 years, and extensive disease.
Case Report
A 44-year-old Asian woman presented with a history of left upper and lower extremity pain and swelling for 38 years and limitation of articular motion for 30 years. Her limb pain initially appeared at the age of 6 years, most prominently in her left knee. After middle school, the swelling and restriction of joint motion gradually progressed. During the previous 10 years, she often felt anesthesia in the ulnar areas of the left forearm and hand. There was no relevant family history or trauma, and her son had no similar problems.
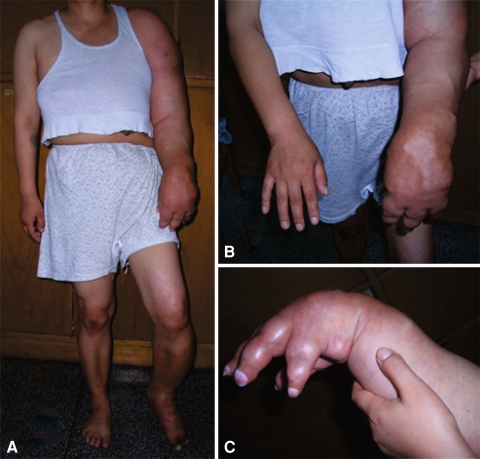
On physical examination, the patient had overgrowth of the left limbs: 9 cm in the upper extremity and 5 cm in the lower extremity. The circumferences of the left upper arm, wrist, and leg were 14, 9, and 6 cm larger, respectively, than those of the right side (Fig. 1A). The swelling was bony hard and nontender. High skin temperature and hyperpigmentation also were present. The joints below the left shoulder and knee were completely or near-completely stiff, including 0° flexion of the shoulder, 60° flexion of the elbow, 80° flexion of the wrist (Fig. 1B), 0° to 5° flexion of the proximal and distal interphalangeal joints (Fig. 1C), 20° flexion of the knee, 25° flexion of the ankle (Fig. 1A), 0° to 10° flexion of the metatarsophalangeal and interphalangeal joints, and 45° to 50° flexion of the metacarpophalangeal joints. Range of motion in the hip was restricted to 25° to 50° flexion. She had decreased sensation in the ulnar half of the forearm and hand. Tinel’s sign was positive around the territory of the sulcus for the ulnar nerve. No abnormality was detected in the right limbs.
Fig. 1A–C.
(A) A clinical photograph shows the extent of the swelling and malformation. Contrasting with the normal right extremities, the length and circumference of the left upper and lower extremities obviously are increased. (B) A clinical photograph shows the left forearm and wrist are swollen compared with the right forearm and wrist. (C) A clinical photograph shows the left fingers are excessively overgrown, resembling dilated balloons; the wrist was 80° flexed and stiff.
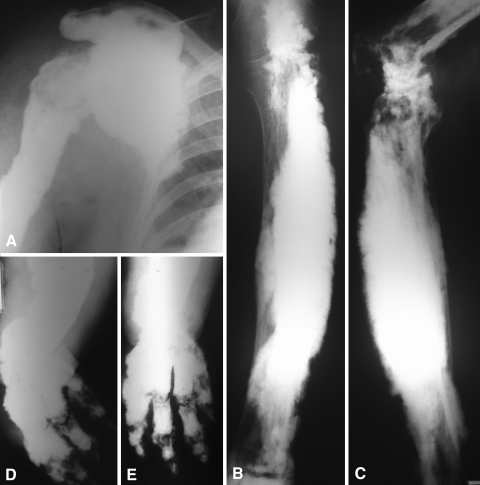
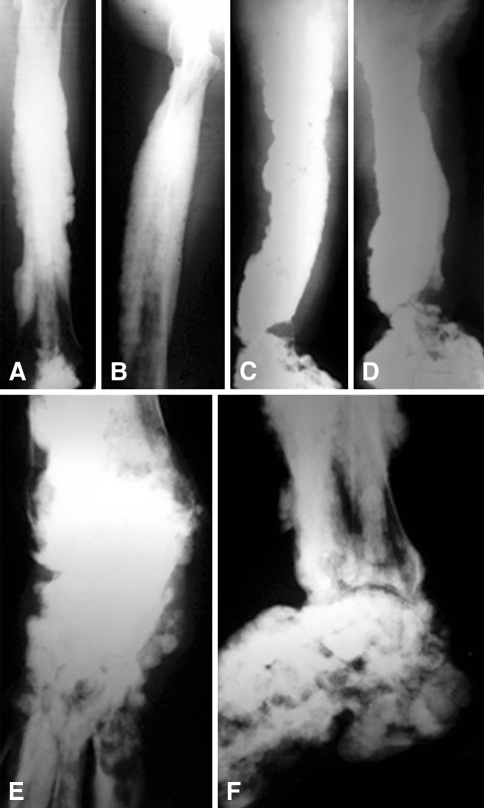
Plain radiographs showed extensive, dense, undulating or irregular cortical hyperostosis, resembling candle wax, extending along the length of both sides of the long bones, resulting in deformity of the bones and narrowing or disappearance of the medullary cavities. There was no distinct demarcation between the affected and normal bones. The bones involved were the clavicle, scapula, humerus (Fig. 2A), radius, ulna (Fig. 2B–C), carpal bones, metacarpal bones, phalanges of the fingers (Fig. 2D–E), femur (Fig. 3A–B), tibia, fibula (Fig. 3C–D), tarsal bones (Fig. 3E–F), metatarsal bones, and phalanges of the toes. Fusion could be detected between the radius and ulna, between the tibia and fibula, and in the shoulder, elbow, wrist, knee, ankle, and the small joints of the hand and foot. We also observed soft tissue ossifications about the joints. Plain radiographs of bones on the right side were normal.
Fig. 2A–E.
(A) A radiograph of the left shoulder reveals serious bone sclerosis and hyperostosis of the scapula and humerus. The joint space of the shoulder has disappeared. (B) Lateral and (C) anteroposterior radiographs of the left forearm reveal extensive, dense, cortical hyperostosis and fusion of the radius and ulna. (D) Lateral and (E) anteroposterior radiographs of the left hand show the carpal bones are deformed and fused.
Fig. 3A–F.
(A) Lateral and (B) anteroposterior radiographs of the left femur show the flowing hyperostosis resembling dripping candle wax, extending along the length of both sides of the femur. (C) Lateral and (D) anteroposterior radiographs of the left leg show the tibia and fibula are fused together. (E) Lateral and (F) anteroposterior radiographs of the left ankle reveal a rough articular surface and narrowed joint space. The boundary between the tarsal bones is obscure.
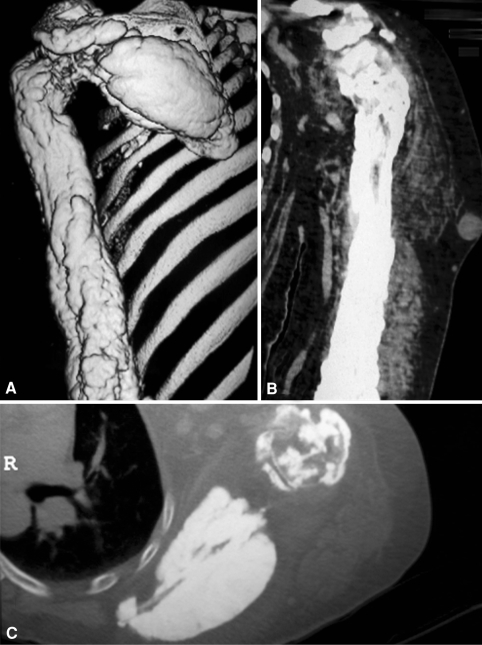
Computed tomography (CT) scans and three-dimensional reconstruction of the scapula, humerus, and shoulder showed candle wax-like or massive, rough hyperostosis around cortical and cancellous bones, accompanied by deformity of the bones (Fig. 4A), narrowing of the medullary cavity (Fig. 4B–C), fusion of the joints, and soft tissue swelling.
Fig. 4A–C.
(A) A three-dimensional CT reconstruction shows candle wax-like or massive hyperostosis around the scapula and humerus, resulting in serious deformity. (B) A CT scan of the humeral coronal plane shows the candle wax-like hyperostotic change. The medullary cavity has almost disappeared. (C) A CT scan of the scapular horizontal plane shows the scapula is thickened. Hyperostotic bone almost totally occupies the humeral medullary cavity.
Laboratory findings for serum calcium, phosphorus, alkaline phosphatase, C-reactive protein, erythrocyte sedimentation rate, α-fetoprotein, carcinoembryonic antigen, and carbohydrate antigen were within normal limits.
The pathology report described nonspecific, dense cortical bone. The hyperostotic bone consisted of mature and immature bone elements.
Pamidronate (30 mg/day for 3 days) infusion and meloxicam (7.5 mg/day for 28 days) for oral use were given to the patient. At followup 6 months later, the patient reported slight alleviation of the pain.
Discussion
Melorheostosis is a rare chronic bone disorder first described in 1922 by Leri and Joanny [9]. Men and women are equally affected, and no hereditary features have been discovered. The onset is insidious, and the first symptom of neuralgia or arthralgia usually occurs in childhood or early adolescence. Range-of-motion limitation and joint deformities develop gradually [1]. Our patient had initial onset of pain in the knee at the age of 6 years.
Melorheostosis may present in a monostotic, polyostotic, or monomelic form. The monomelic variant is the most common presentation of the disease [16]. In our patient, the entire left upper and lower extremities were involved simultaneously and the right extremities were completely normal, which is rare.
Several hypotheses have been suggested concerning its etiology, such as an embryonal mesodermal disorder that affects osseous and soft tissue, a loss-of-function mutation in LEMD3 gene (sometimes referred to as MAN1), a vascular disturbance, and an inflammatory process [5, 15]. In 1979, Murray and McCredie [13] suggested an infection associated with nerve roots may be responsible for melorheostosis, because they detected a good correlation between hyperostotic lesions and the sclerotomes. This may in part explain the monomelic and linear track involvement and distribution of melorheostosis. However, according to the hypothesis of Murray and McCredie, when infection encroaches on nerve roots, the involved nerve roots should adjoin each other. We believe it is unreasonable to presume ipsilateral distant lower limb nerve roots are involved and the adjacent contralateral upper limb nerve roots are intact, as in our patient. Another possible explanation is involvement of the corticospinal tract or spinothalamic tract, but then the symptoms in the axial skeleton or nervous system also should be apparent. We also might speculate the pathologic changes reside in the fasciculus proprius of the spinal cord, but the hypothesis needs further study. The etiology of melorheostosis remains obscure.
Radiographic findings have been the cornerstone of the diagnosis, consisting of candle wax-like hyperostotic changes of the cortex, generally on one side of the bone. There is usually a distinct demarcation between the affected and normal bone. Dense linear areas are seen mainly in the cortex but also extending into the cancellous bone. Melorheostosis affects mainly the long bones of the upper and lower limbs, and also the short bones of the hand and foot, but rarely the axial skeleton [4]. In our patient, plain radiographs showed the classic radiographic features of melorheostosis, but the severity was unusual, including severe thickening and deformity of the bones. Almost all the bones and joints in the left limbs were affected, every bone was extensively affected, and there was no distinct demarcation between the affected and normal bone. The radius and ulna, tibia and fibula, and small bones in the hand and foot were almost completely fused.
Routine laboratory findings usually are normal. Histologic findings are usually nonspecific and often show dense bone formation, a mixture of mature and immature bone elements, and thickened and enlarged bony trabeculae constituting largely primary Haversian systems [3]. Osteoclastic activity is not a prominent feature; however, osteoblastic activity along the margins of osteons is common [2].
The differential diagnosis for melorheostosis, especially for the forme fruste, includes osteopoikilosis, osteopathic striata, myositis ossificans, parosteal osteosarcoma, and osteoma [7, 14, 16]. In our patient, according to the clinical presentation, characteristic appearance of plain radiographs, CT scans, and histologic features, the diagnosis was easily made.
Treatment in most instances has been symptomatic. Most patients receive nonoperative treatment. Operative treatment consists of tendon lengthening, excision of hyperostotic bone, osteotomies, and amputation [4]. In our patient, pamidronate and meloxicam only slightly relieved pain, and there were no good surgical measures for this severe condition.
Melorheostosis is a rare sclerosing bone dysplasia. We report a case of melorheostosis with a history of 38 years. The severity and the extension of the disease to ipsilateral limbs are exceedingly rare.
Acknowledgments
We express sincere thanks to all those who have offered us help writing this paper. We also express our appreciation to our teachers and classmates in the Department of Orthopaedics of Xiangya Hospital of Central South University, especially to Dr. Wen-Feng Xiao and Dr. Guo-Jun Li, who offered valuable support and help in the course of collecting data and writing the paper.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the reporting of this case, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Biaou O, Avimadje M, Guira O, Adjagba A, Zannou M, Hauzeur JP. Melorheostosis with bilateral involvement in a black African patient. Joint Bone Spine. 2004;71:70–72. [DOI] [PubMed]
- 2.Campbell CJ, Papademetriou T, Bonfiglio M. Melorheostosis: a report of the clinical, roentgenographic, and pathological findings in fourteen cases. J Bone Joint SurgAm. 1968;50:1281–1304. [PubMed]
- 3.Ethunandan M, Khosla N, Tilley E, Webb A. Melorheostosis involving the craniofacial skeleton. J Craniofac Surg. 2004;15:1062–1065. [DOI] [PubMed]
- 4.Greenspan A, Azouz EM. Bone dysplasia series: melorheostosis: review and update. Can Assoc Radiol J. 1999;50:324–330. [PubMed]
- 5.Hellemans J, Preobrazhenska O, Willaert A, Debeer P, Verdonk PC, Costa T, Janssens K, Menten B, Van Roy N, Vermeulen SJ, Savarirayan R, Van Hul W, Vanhoenacker F, Huylebroeck D, De Paepe A, Naeyaert JM, Vandesompele J, Speleman F, Verschueren K, Coucke PJ, Mortier GR. Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet. 2004;36:1213–1218. [DOI] [PubMed]
- 6.Kalbermatten NT, Vock P, Rüfenacht D, Anderson SE. Progressive melorheostosis in the peripheral and axial skeleton with associated vascular malformations: imaging findings over three decades. Skeletal Radiol. 2001;30:48–52. [DOI] [PubMed]
- 7.Kawabata H, Tsuyuguchi Y, Kawai H, Yasui N. Melorheostosis of the upper limb: a report of two cases. J Hand Surg Am. 1984;9:871–876. [DOI] [PubMed]
- 8.Khurana JS, Ehara S, Rosenberg AE, Rosenthal DI. Melorheostosis of ilium, femur, and adjacent soft tissues. Skeletal Radiol. 1988;17:539–541. [DOI] [PubMed]
- 9.Leri A, Joanny J. Une affection non décrite des os hyperostose “en coulée” sur toute la longeur d’un member ou “melorhéostose.” Bull Mem Soc Med Hosp Paris. 1922;46:1141–1145.
- 10.McCarthy M, Mehdian H, Fairbairn KJ, Stevens A. Melorheostosis of the tenth and eleventh thoracic vertebrae crossing the facet joint: a rare cause of back pain. Skeletal Radiol. 2004;33:283–286. [DOI] [PubMed]
- 11.Motimaya AM, Meyers SP. Melorheostosis involving the cervical and upper thoracic spine: radiographic, CT, and MR imaging findings. AJNR Am J Neuroradiol. 2006;27:1198–1200. [PMC free article] [PubMed]
- 12.Mumm S, Wenkert D, Zhang X, McAlister WH, Mier RJ, Whyte MP. Deactivating germline mutations in LEMD3 cause osteopoikilosis and Buschke-Ollendorff syndrome, but not sporadic melorheostosis. J Bone Miner Res. 2007;22:243–250. [DOI] [PubMed]
- 13.Murray RO, McCredie J. Melorheostosis and the sclerotomes: a radiological correlation. Skeletal Radiol. 1979;4:57–71. [DOI] [PubMed]
- 14.Spieth ME, Greenspan A, Forrester DM, Ansari AN, Kimura RL, Siegel ME. Radionuclide imaging in forme fruste of melorheostosis. Clin Nucl Med. 1994;19:512–515. [DOI] [PubMed]
- 15.Yoshikawa H, Myoui A, Araki N, Ueda T. Melorheostosis with heterotopic ossification. Orthopedics. 2001;24:493–494. [DOI] [PubMed]
- 16.Zeiller SC, Vaccaro AR, Wimberley DW, Albert TJ, Harrop JS, Hilibrand AS. Severe myelopathy resulting from melorheostosis of the cervicothoracic spine: a case report. J Bone Joint Surg Am. 2005;87:2759–2762. [DOI] [PubMed]