Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I (original) (raw)
Abstract
Most patients with autoimmune polyendocrine syndrome type I (APS-I) display chronic mucocutaneous candidiasis (CMC). We hypothesized that this CMC might result from autoimmunity to interleukin (IL)-17 cytokines. We found high titers of autoantibodies (auto-Abs) against IL-17A, IL-17F, and/or IL-22 in the sera of all 33 patients tested, as detected by multiplex particle-based flow cytometry. The auto-Abs against IL-17A, IL-17F, and IL-22 were specific in the five patients tested, as shown by Western blotting. The auto-Abs against IL-17A were neutralizing in the only patient tested, as shown by bioassays of IL-17A activity. None of the 37 healthy controls and none of the 103 patients with other autoimmune disorders tested had such auto-Abs. None of the patients with APS-I had auto-Abs against cytokines previously shown to cause other well-defined clinical syndromes in other patients (IL-6, interferon [IFN]-γ, or granulocyte/macrophage colony-stimulating factor) or against other cytokines (IL-1β, IL-10, IL-12, IL-18, IL-21, IL-23, IL-26, IFN-β, tumor necrosis factor [α], or transforming growth factor β). These findings suggest that auto-Abs against IL-17A, IL-17F, and IL-22 may cause CMC in patients with APS-I.
Autoimmune polyendocrine syndrome type I (APS-I), also known as autoimmune polyendocrinopathy with candidiasis and ectodermal dystrophy (Online Mendelian Inheritance in Man no. 240300), is a rare, autosomal recessive primary immunodeficiency first described clinically in 1929 (Notarangelo et al., 2006; Husebye et al., 2009). APS-I is characterized principally by multiple autoimmune endocrinopathies, hypoparathyroidism, and adrenal insufficiency in particular, with some of these symptoms being caused by pathogenic autoantibodies (auto-Abs). A genome-wide mapping approach led to the identification of APS-I–causing mutations in the AIRE gene in 1997 (Finnish-German APECED Consortium, 1997; Nagamine et al., 1997). Autoimmunity in patients with APS-I may be accounted for by the key role of AIRE in tolerance. AIRE is expressed in the thymus, where it contributes to the expression of peripheral antigens (Anderson et al., 2002; Mathis and Benoist, 2009). This gene has also been shown to be expressed in secondary lymphoid organs, where it also contributes to tolerance (Gardner et al., 2008). Surprisingly, most patients with APS-I suffer from chronic mucocutaneous candidiasis (CMC) without displaying any marked susceptibility to any other pathogen. The product of the AIRE gene is not involved in any known cellular pathway governing host defense. The pathogenesis of CMC in patients with APS-I has thus remained both intriguing and elusive.
High titers of auto-Abs against some type I IFNs, including IFN-α and -ω in particular, are found in all patients (Meager et al., 2006; Meloni et al., 2008). These auto-Abs are a hallmark of APS-I and are therefore useful for diagnostic purposes (Husebye et al., 2009). However, they confer no particular overt predisposition to viral diseases, perhaps because of the large number of redundant type I IFN species, resulting in incomplete neutralization of the overall antiviral activity of IFNs by the auto-Abs. It has been suggested that these auto-Abs contribute to CMC in APS-I patients (Meager et al., 2006). However, this is now thought unlikely because of the absence of CMC in patients with various forms of STAT1 and TYK2 deficiency and impaired responses to type I IFNs, and in patients with various forms of NEMO, UNC-93B, and TLR3 deficiencies and impaired production of type I IFNs (Minegishi et al., 2006; Zhang et al., 2008; Chapgier et al., 2009). Nevertheless, based on this observation, we hypothesized that CMC in patients with APS-I might result from autoimmunity to cytokines other than type I IFNs potentially involved in protective immunity to Candida albicans in the skin and mucosae.
Recent studies in the mouse have suggested that IL-17 cytokines, such as IL-17A, IL-17F, and IL-22 (Korn et al., 2009), may be important in host defense against Candida (Conti et al., 2009; van de Veerdonk et al., 2009). However, it is difficult to assess mucocutaneous immunity to Candida in mice (Netea et al., 2008), in which IL-17 cytokines seem to be important for the control of various other pathogens, particularly in the lungs and gastrointestinal tract (Dubin and Kolls, 2008; Khader et al., 2009). Stimulation with Candida in vitro leads to the preferential generation of IL-17A– and IL-22–producing human T cells (Acosta-Rodriguez et al., 2007; Liu et al., 2009). Furthermore, patients with STAT3 deficiency display a predisposition to CMC (and staphylococcal disease) and lack IL-17–producing T cells (de Beaucoudrey et al., 2008; Ma et al., 2008; Milner et al., 2008; Minegishi et al., 2009). Similarly, some patients with IL-12p40 or IL-12Rβ1 deficiency present CMC (together with mycobacteriosis and salmonellosis) and have lower than normal proportions of IL-17–producing T cells (de Beaucoudrey et al., 2008). Finally, patients with rare defects of CARD9, which normally controls the production of IL-17 in response to dectin-1 and -2 stimulation by Candida, suffer from candidiasis (LeibundGut-Landmann et al., 2007; Glocker et al., 2009; Robinson et al., 2009). We therefore hypothesized that autoimmunity to IL-17 cytokines might account for CMC in patients with APS-I.
RESULTS AND DISCUSSION
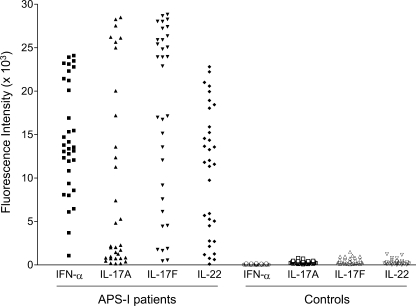
We searched for auto-Abs against IL-17 cytokines (IL-17A, IL-17F, IL-22, and IL-26, which is absent from mice) or against IL-17–inducing cytokines (IL-1β, IL-6, IL-21, IL-23, and TGF-β) in 33 patients diagnosed with APS-I on the basis of autoimmune polyendocrinopathy, circulating auto-Abs against IFN-α and –ω, and the presence of two mutant AIRE alleles (Table I). CMC was observed in 29 out of the 33 patients (Table I). Multiplex particle-based flow cytometry revealed a high fluorescence intensity (FI; >1,000, arbitrary definition) of IgG auto-Abs against IL-17A in the plasma of 22 patients, with a high FI of auto-Abs against IL-17F in 31 patients and of auto-Abs against IL-22 in 30 patients (Fig. 1 and Table I). All 33 patients had significant (P = 6.4 × 10−9, 4.6 × 10−12, and 2.16 × 10−11, respectively) levels of auto-Abs against at least one of these three cytokines. 5 patients had a significant reaction against a single cytokine, 6 had a reaction against two cytokines, and 22 had a reaction against all three cytokines. No auto-Abs against IL-17A, IL-17F, and IL-22 were found in plasma samples from the 37 healthy individuals tested. Similarly, no auto-Abs against any of these three cytokines were found in plasma samples from another 103 patients with various autoimmune conditions (Fig. S4, A and B). No auto-Abs against IL-1β, IL-6, IL-23, or IL-26 (whether as a monomer or a dimer) were found in the APS-I patients (Fig. S3, A–D). There were no auto-Abs against IL-12, IFN-γ, or GM-CSF (Fig. S3, E–G), consistent with the lack of mycobacterial disease and alveolar proteinosis in patients with APS-I. No auto-Abs were found against any of the other cytokines tested, including IL-10, IL-18, IFN-β, and TNF (Fig. S3, H–K). As expected, all APS-I patients had auto-Abs against IFN-α (Fig. 1 and Table I) and IFN-ω (not depicted). In addition, no IgA antibodies, a key element of mucosal immunity, directed against IL-17A, IL-17F, or IL-22 were detected in the plasma of 21 APS-I patients by classical ELISA (not depicted).
Table I.
APS-I patients tested
| Patients | Gender | Age | Origin | AIRE genotype | Auto-Abs against | Mucocutaneous candidiasis phenotype | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Luminex | ELISA | Age of onset | Clinical features | ||||||||||
| IFN-α | IL-17A | IL-17F | IL-22 | IL-17A | IL-17F | IL-22 | |||||||
| APS-I 1 | M | 12 yr | Saudi Arabia | 845insc/845insc | 8,584 | 7,406 | 1,874 | 11,810 | 0.11 | 0.21 | 2.41 | 18 mo | Mouth, nails, esophagus |
| APS-I 2 | M | 9 yr | Africa | c958del/c958del | 1,070 | 1,264 | 23,963 | 13,661 | 0.03 | 2.16 | 2.41 | 6 yr | Nails, scalp, eyes |
| APS-I 3 | M | 13 yr | Africa | c958del/c958del | 6,467 | 4,824 | 28,271 | 13,265 | 0.03 | 2.61 | 2.51 | – | Nails |
| APS-I 4 | F | 26 yr | North Africa | ex6_8del/ex6_8del | 10,836 | 828 | 1,765 | 761 | 0.02 | 0.11 | 0.26 | 16 yr | Nails, scalp |
| APS-I 5 | M | 25 yr | North Africa | ex6_8del/ex6_8del | 12,785 | 1,448 | 16,980 | 2,758 | 0.04 | 1.33 | 0.26 | 7 yr | Nails, scalp, digestive tract |
| APS-I 6 | F | 10 yr | North Africa | ex6_8del/ex6_8del | 3,705 | 1,998 | 16,742 | 5,691 | – | 1 | 1.09 | 1 mo | Mouth, eyes, vulva |
| APS-I 7 | M | 10 yr | France | R257X/P539L | 20,109 | 27,523 | 25,409 | 18,446 | 2.29 | 1.95 | 2.83 | 2 mo | Mouth, esophagus, respiratory tract |
| APS-I 8 | F | 21 yr | Ireland | 964del13/964del13 | 14,169 | 192 | 1,645 | 5,914 | 0.02 | 0.13 | 0.21 | 3 yr | Mouth, scalp, skin |
| APS-I 9 | M | 20 yr | Ireland | 964del13/964del13 | 12,325 | 455 | 6,135 | 11,345 | 0.03 | 0.31 | 2.06 | 3 yr | Mouth, nails, perineum |
| APS-I 10 | F | 29 yr | UK | 964del13/964del13 | 9,371 | 734 | 15,140 | 615 | 0 | 0.11 | 0.03 | 4 yr | Mouth, esophagus, nails |
| APS-I 11 | F | 36 yr | UK | 964del13/964del13 | 12,078 | 148 | 4,439 | 102 | 0.01 | 0.15 | 0.16 | Childhood | Mouth, esophagus, vagina |
| APS-I 12 | F | 41 yr | UK | 964del13/964del13 | 6,098 | 17,201 | 24,837 | 9,749 | 0.16 | 0.47 | 0.64 | 4 yr | Mouth, nails, vagina, anus |
| APS-I 13 | F | 18 yr | Ireland | 964del13/964del13 | 13,379 | 367 | 548 | 2,708 | 0.02 | 0.1 | 0.18 | Childhood | Skin, scalp |
| APS-I 14 | M | 12 yr | Ireland | 964del13/964del13 | 13,555 | 24,983 | 17,131 | 22,225 | 0.36 | 0.35 | 1.06 | Few weeks | Mouth, nails, scalp |
| APS-I 15 | M | 18 yr | UK | 964del13/964del13 | 16,906 | 28,484 | 25,907 | 20,585 | 2.34 | 0.5 | 1.07 | 3 yr | Mouth, nails |
| APS-I 16 | M | 18 yr | UK | 964del13/964del13 | 15,473 | 28,262 | 23,926 | 12,034 | 1.89 | 0.52 | 0.3 | 3 yr | Mouth, nails |
| APS-I 17 | M | 13 yr | Ireland | 964del13/964del13 | 8,086 | 805 | 23,917 | 14,558 | 0.02 | 0.64 | 0.91 | 5 yr | Mouth, nails |
| APS-I 18 | F | 10 yr | UK | 964del13/964del13 | 13,053 | 5,282 | 27,409 | 15,236 | 0.03 | 1.52 | 0.61 | Few weeks | Mouth |
| APS-I 19 | M | 6 yr | UK | 964del13/964del13 | 13,797 | 13,588 | 28,025 | 13,575 | 0.25 | 1.84 | 1.83 | Birth | Mouth, perineum |
| APS-I 20 | M | 17 yr | UK | 964del13/964del13 | 11,946 | 11,272 | 25,904 | 2,129 | 0.08 | 0.39 | 0.12 | 7 yr | Penis, perineum |
| APS-I 21 | M | 9 yr | UK | 964del13/964del13 | 13,127 | 752 | 12,048 | 18,039 | 0.08 | 0.44 | 1.11 | 2 yr | Esophagus, nails |
| APS-I 22 | F | 52 yr | UK | 964del13/c.769C>T | 8,012 | 955 | 22,886 | 4,502 | ND | ND | ND | Childhood | Mouth |
| APS-I 23 | M | 16 mo | Hungary | R257X/R257X | 23,216 | 20,035 | 4,531 | 21,012 | 0.55 | 0.08 | 2.31 | – | None |
| APS-I 24 | M | 18 yr | Hungary | R257X/C449fsX479 | 23,486 | 1,708 | 28,012 | 18,937 | 0.05 | 1.97 | 0.45 | – | None |
| APS-I 25 | M | 14 yr | Hungary | R257X/L323fsX373 | 23,923 | 2,025 | 9,169 | 5,259 | 0.06 | 0.15 | 0.18 | – | None |
| APS-I 26 | F | 21 yr | Hungary | R257X/R257X | 23,120 | 12,359 | 28,834 | 11,583 | 0.43 | 2.86 | 0.16 | – | None |
| APS-I 27 | M | 28 yr | Canada | 964del13/964del13 | 21,225 | 737 | 7,576 | 5,047 | 0.02 | 0.09 | 0.04 | 3 yr | Mucosa, skin, nails, eyes, scalp |
| APS-I 28 | F | 31 yr | Canada | 964del13/964del13 | 22,324 | 26,214 | 25,064 | 1,178 | 0.91 | 0.78 | 0.03 | Birth | Mucosa, skin, nails, eyes, scalp |
| APS-I 29 | F | 16 yr | Canada | delT253/R257X | 24,099 | 2,268 | 13,563 | 15,899 | 0.08 | 0.79 | 0.14 | 2 yr | Nails |
| APS-I 30 | M | 19 yr | Canada | delT253/R257X | 21,442 | 153 | 448 | 1,264 | 0.03 | 0.04 | 0.24 | 3 yr | Mucosa, skin, nails |
| APS-I 31 | F | 5 yr | Canada | 964del13/964del13 | 22,798 | 26,120 | 28,667 | 19,954 | 1.99 | >3 | 1.83 | 6 mo | Mucosa |
| APS-I 32 | F | 31 yr | UK | 964del13/964del13 | 14,718 | 2,155 | 27,222 | 14,358 | ND | ND | ND | 15 yr | Mouth, nails |
| APS-I 33 | F | 7 yr | UK | 964del13/964del13 | 15,332 | 25,648 | 26,358 | 22,808 | ND | ND | ND | 4 yr | Mouth, nails, scalp |
Figure 1.
High titers of auto-Abs against IFN-α, IL-17A, IL-17F, and IL-22 in the plasma from patients with APS-I. Anti–IFN-α, –IL-17A, –IL-17F, and –IL-22 circulating IgG titers were measured by multiplex particle-based flow cytometry in 33 samples from patients with APS-I and in 37 samples from healthy controls. FI is plotted on the y axis. Representative data for two experiments are shown.
We also ran classical ELISA, with plasma samples diluted by a factor of five more than in the multiplex assays. 4 out of the 30 patients tested had high titers of IgG (OD > 1) auto-Abs against IL-17A (P = 0.056), 10 patients had high titers of auto-Abs against IL-17F (P = 1.4 × 10−7), and 12 patients had high titers of auto-Abs against IL-22 (P = 1.23 × 10−7; Fig. S1 and Table I). 17 patients had auto-Abs against at least one of these three cytokines, including 10 patients with auto-Abs against a single cytokine, 5 patients with auto-Abs against two cytokines, and 2 patients with auto-Abs against all three cytokines. No such auto-Abs were detected in the 37 healthy controls tested. This assay was not used to test patients with various autoimmune diseases. There were no detectable auto-Abs against TGF-β1, IL-6, IL-21, IL-23, or IL-26, or against IL-12 or IFN-γ in any of the APS-I patients (Fig. S2, A–G). Thus, in both ELISA and multiplex particle-based flow cytometry, the only auto-Abs detected in the 33 patients with APS-I tested were directed against IFN-α, IFN-ω, IL-17A, IL-17F, and IL-22 (Fig. 1, Fig. S1, and Table I). Moreover, all 33 patients with APS-I had auto-Abs against at least one out of three IL-17 cytokines (IL-17A, IL-17F, and IL-22). High titers of auto-Abs against all three of these cytokines were found in 22 patients.
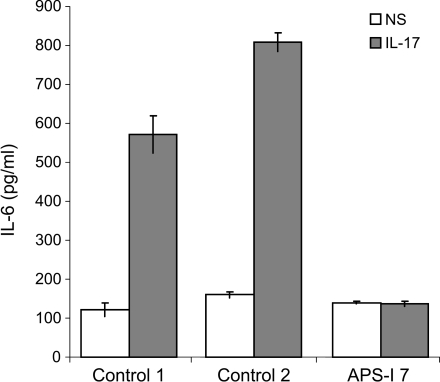
We performed Western blotting to assess the specificity of these auto-Abs. Plasma samples from five patients with APS-I and auto-Abs against IL-17A, IL-17F, and/or IL-22, as detected by ELISA and multiplex particle-based flow cytometry, and from a healthy individual were tested for their ability to recognize rIL-17A, rIL-17F, and rIL-22 on Western blots. The three cytokines were clearly recognized by plasma samples from patients but not by the control plasma (Fig. 2). The plasma samples from patients did not recognize IL-23 in a control assay. Finally, we investigated whether the auto-Abs against IL-17A neutralized this cytokine in a simple biological assay. We incubated fibroblasts from a healthy control with up to 50 ng/ml rIL-17A in the presence of plasma from healthy individuals, or from a patient with APS-I and auto-Abs against IL-17, as detected by ELISA and Western blotting. We then measured the induction of IL-6 by ELISA on the supernatant. Strikingly, even strong dilutions of plasma samples from patients (up to 0.1%; not depicted) completely abolished fibroblastic cell responses to such high concentrations of rIL-17 (Fig. 3), whereas control plasma had no effect. Lower concentrations of IL-17A failed to induce IL-6, even in the presence of control plasma (unpublished data). The lack of robust bioassays precluded assessments of the possible neutralizing effects of auto-Abs against IL-17F and IL-22. Thus, all patients with APS-I tested had high titers of auto-Abs against IL-17A, IL-17F, and IL-22 in their plasma, and these auto-Abs were specific and neutralizing, at least in the patients tested. These data suggest that most patients with APS-I carry neutralizing auto-Abs against IL-17A, IL-17F, and IL-22.
Figure 2.
Specific auto-Abs against IL-17A, IL-17F, and/or IL-22 in the plasma from patients with APS-I. Western blot against rIL-17A, rIL-17F, rIL-22, and rIL-23 were performed using plasma from a healthy individual or from five patients with APS-I, diluted 1:500. Representative data for three experiments are shown. Dashed lines indicate that intervening lanes have been spliced out.
Figure 3.
Neutralizing auto-Abs against IL-17A in the plasma from a patient with APS-I. IL-6 production, after 48 h of stimulation with 50 ng/ml IL-17A, by control SV-40–transformed fibroblasts incubated with 10% plasma from two controls or from one patient (APS-I patient 7; means and errors bars from duplicates are shown). The data shown are representative of two experiments.
APS-I patients may display auto-Abs against IL-17 cytokines as a result of impaired AIRE-dependent tolerance induction if the expression of the corresponding cytokine genes is normally controlled by AIRE in the thymus or in secondary lymphoid organs. Whatever the mechanism, these data suggest that impaired IL-17 immunity may account for CMC in patients with APS-I. In particular, these data are consistent with the impaired IL-17 immunity reported in other patients with known inborn errors of immunity predisposing to CMC (and other infectious diseases). Indeed, patients with low proportions (IL12B, IL12RB1) or a lack of (STAT3) IL-17–producing circulating T cells suffer from mild (IL12B, IL12RB1) or severe (STAT3) CMC, respectively. Patients with APS-I and auto-Abs against IL-17 cytokines do not suffer from severe staphylococcal disease, unlike STAT3-deficient patients (Freeman and Holland, 2009). Impaired IL-17 immunity probably contributes to staphylococcal disease in STAT3-deficient patients, as epithelial cells in the skin and lungs, the organs most frequently affected by staphylococcal infection in these patients, specifically rely on IL-17 stimulation for the induction of known antistaphylococcal target genes (Minegishi et al., 2009). The lack of overt staphylococcal disease in most APS-I patients may result from residual IL-17 immunity, as observed to an even greater extent in patients with IL-12p40 and IL-12Rβ1 deficiencies who also control staphylococcal infections normally (Filipe-Santos et al., 2006). In any case, proof that human IL-17 cytokines play an essential role in immunity to Candida will require the identification of mutations specifically impairing IL-17 immunity in other patients with inherited, isolated CMC without APS-I (Ryan et al., 2008; Hong et al., 2009). The recent observation that some patients with isolated CMC have smaller than normal proportions of IL-17–producing T cells and produce low levels of IL-17 suggests that this may be plausible (unpublished data; Eyerich et al., 2008).
Various human diseases seem to be caused by the production of auto-Abs against cytokines. Patients with pulmonary alveolar proteinosis were shown to display auto-Abs against GM-CSF in 1999 (Kitamura et al., 1999). Mutations in the GM-CSF receptor were subsequently found in other patients, establishing a causal relationship between impaired GM-CSF immunity and alveolar proteinosis (Martinez-Moczygemba et al., 2008; Suzuki et al., 2008). Patients with mycobacterial diseases and inherited IFN-γR1 deficiency were first reported in 1996 (Filipe-Santos et al., 2006). Autoimmune phenocopies, with auto-Abs against IFN-γ, were subsequently found in other patients (Döffinger et al., 2004; Kampmann et al., 2005; Patel et al., 2005). We recently reported a patient with auto-Abs against IL-6 and staphylococcal disease (Puel et al., 2008). There may be a causal relationship between auto-Abs against IL-6 and staphylococcal disease, as STAT3- and Tyk2-deficient patients suffer from staphylococcal disease and have a poor cellular response to IL-6 (Minegishi et al., 2006, 2007, 2009). However, no germline mutation in the gene encoding IL-6 or its receptor has yet been reported in similar patients. This description of patients with auto-Abs against IL-17 cytokines is the fourth reported example of pathogenic auto-Abs against human cytokines. Other auto-Abs against cytokines not tested in this study, including some that would impair the development of IL-17–producing T cells, may also contribute to the development of CMC in APS-I patients.
MATERIALS AND METHODS
Patients.
33 patients with APS-I (18 male and 15 female patients; Table I and Table S1), 103 patients with endocrine/autoimmune disorders, and 37 healthy controls (15 male and 22 female subjects) were enrolled in this study, with informed consent and approval obtained by the Necker Hospital and Medical School Institutional Review Board (IRB) and the Rockefeller University IRB.
Plasma and serum samples.
Plasma and serum samples from the patients and controls were frozen at −20°C immediately after collection.
ELISA.
ELISA was performed as previously described (Puel et al., 2008). In brief, 96-well ELISA plates (MaxiSorp; Thermo Fisher Scientific) were coated by incubation overnight at 4°C with 2 µg/ml rIL-6, rIL-12p70, rIL-17A, rIL-17F, rIL-21, rIL-22, rIL-23, rIL-26 monomer, rIL-26 dimer, rTGF-β, and rIFN-γ (R&D Systems). Plates were then washed (PBS/Tween 0.005%), blocked by incubation with the same buffer supplemented with 5% nonfat milk powder, washed, and incubated with 1:500 dilutions of plasma samples from the patients or controls for 2 h at room temperature (or with specific mAbs as positive controls). Plates were thoroughly washed. Horseradish peroxidase (HRP)–conjugated Fc-specific IgG fractions from polyclonal goat antiserum against human IgG or IgA (Nordic Immunological Laboratories) were added to a final concentration of 2 µg/ml. Plates were incubated for 1 h at room temperature and washed. Substrate was added and OD was measured.
Multiplex particle-based flow cytometry.
Recombinant human cytokines (rIL-1β, rIL-6, rIL-10, rIL-12p40, rIL-12p70, rIL-17A, rIL-17F, rIL-18, rIL-22, rIL-23, rIL-26 monomer, rIL-26 dimer, rIFN-α, rIFN-β, rIFN-γ, rTNF, and rGM-CSF; R&D Systems) were covalently coupled to carboxylated beads (Bio-Plex; Bio-Rad Laboratories). Beads were first activated with 1-ethyl-3-[3-dimethylaminopropyl]carbodiimide hydrochloride (Thermo Fisher Scientific) in the presence of _N_-hydroxysuccinimide (Thermo Fisher Scientific), according to the manufacturer’s instructions, to form amine-reactive intermediates. The activated beads were incubated with the corresponding cytokines at a concentration of 20 µg/ml in the reaction mixture for 3 h at room temperature on a rotator. Beads were washed and stored in blocking buffer (10 mM PBS, 1% BSA, 0.05% NaN3). Cytokine-coupled beads were incubated with plasma or serum from patients for 1 h in 96-well filter plates (MultiScreenHTS; Millipore) at room temperature in the dark on a horizontal shaker. Fluids were aspirated with a vacuum manifold and beads were washed three times with 10 mM PBS/0.05% Tween 20. Beads were incubated for 30 min with a PE-labeled anti–human IgG-Fc antibody (Leinco/Biotrend), washed as described, and resuspended in 100 µl PBS/Tween. They were then analyzed on an analyzer (Bio-Plex) using Bio-Plex Manager 3.0 software (both from Bio-Rad Laboratories). Successful coupling of the cytokines to their respective bead sets was verified with specific mAbs.
Western blotting.
We subjected 500 ng rIL-17A, rIL-17, rIL-22, rIL-23 (R&D Systems), or BSA to SDS-PAGE (10% acrylamide) under reducing conditions. The protein bands were electroblotted onto nitrocellulose membranes (iBlot Gel Transfer Stacks; Invitrogen). Membranes were blocked by incubation for 1 h at room temperature with PBS supplemented with 5% BSA and 0.05% Tween 20, and were washed and incubated overnight at 4°C with plasma samples from a patient or a control diluted 1:500 in PBS, 5% BSA, 0.01% Tween 20. The membranes were washed three times and incubated for 1 h at room temperature with HRP-coupled anti–human IgG and used at a final concentration of 0.67 µg/ml. The membranes were washed three times and developed for ECL (GE Healthcare).
Neutralization assay.
SV-40–transformed control fibroblasts were plated in 24-well plates (60,000 fibroblasts/well) in 0.5 ml DMEM/10% FCS (Invitrogen). On the following day, cells were washed in 1× PBS (Invitrogen) and incubated with 10% plasma (from a control or a patient) in DMEM. They were left unstimulated or were stimulated with 50 ng/ml rIL-17A (R&D Systems). The supernatants were collected 24 and 48 h after stimulation, and IL-6 production was assessed by ELISA (Sanquin Mast Diagnostic) according to the manufacturer’s instructions.
Online supplemental material.
Fig. S1 shows anti–IL-17A, –IL-17F, and –IL-22 IgG auto-Abs measured by ELISA in plasma from APS-I patients and controls. Fig. S2 shows anti–TGF-β1, –IL-6, –IL-21, –IL-23, –IL-12, –IFN-γ, and –IL-26 IgG auto-Abs measured by ELISA in plasma from controls and APS-I patients. Fig. S3 shows anti–IL-1β, –IL-6, –IL-23, –IL-26, –IL-12, –IFN-γ, –GM-CSF, –IFN-β, –IL-10, –IL-18, and -TNF IgG auto-Abs measured by multiplex particle-based flow cytometry in plasma from healthy controls and APS-I patients. Fig. S4 shows anti–IFN-α, –IL-17A, –IL-17F, and –IL-22 IgG auto-Abs in 100 patients suffering from autoimmune and/or endocrine disorders. Table S1 shows the autoimmune/endocrine phenotypes and treatments of each APS-I patient tested. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20091983/DC1.
Acknowledgments
We would like to thank all members of the Paris and New York branches of the laboratory for helpful discussions; T. Leclerc for technical assistance; M. Courat, M. N'Guyen, B. Delaney, and Y. Nemirovskaya for secretarial assistance; and Frédéric Rieux-Laucat and B. Grimbacher for discussions. We would also like to thank the clinicians who provided us with samples and the patients who agreed to participate in our study.
The Laboratory of Human Genetics of Infectious Diseases is supported by the Rockefeller University Center for Clinical and Translational Science (grant 5UL1RR024143-03) and the Rockefeller University. We would like to thank the Rockefeller University, the Institut National de la Santé et de la Recherche Médicale, the University Paris Descartes, the Agence Nationale de la Recherche, the European Union, the March of Dimes, the Dana Foundation, the Addenbrooke's Charitable Trust, the National Institute for Health Research Cambridge Biomedical Research Center, and the Howard Hughes Medical Institute for their support. L. Marodi was supported by the Hungarian Scientific Research Fund.
The authors have no conflicting financial interests.
Footnotes
Abbreviations used:
APS-I
autoimmune polyendocrine syndrome type I
auto-Abs
autoantibodies
CMC
chronic mucocutaneous candidiasis
FI
fluorescence intensity
References
- Acosta-Rodriguez E.V., Rivino L., Geginat J., Jarrossay D., Gattorno M., Lanzavecchia A., Sallusto F., Napolitani G. 2007. Surface phenotype and antigenic specificity of human interleukin 17-producing T helper memory cells. Nat. Immunol. 8:639–646 10.1038/ni1467 [DOI] [PubMed] [Google Scholar]
- Anderson M.S., Venanzi E.S., Klein L., Chen Z., Berzins S.P., Turley S.J., von Boehmer H., Bronson R., Dierich A., Benoist C., Mathis D. 2002. Projection of an immunological self shadow within the thymus by the aire protein. Science. 298:1395–1401 10.1126/science.1075958 [DOI] [PubMed] [Google Scholar]
- Chapgier A., Kong X.F., Boisson-Dupuis S., Jouanguy E., Averbuch D., Feinberg J., Zhang S.Y., Bustamante J., Vogt G., Lejeune J., et al. 2009. A partial form of recessive STAT1 deficiency in humans. J. Clin. Invest. 119:1502–1514 10.1172/JCI37083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti H.R., Shen F., Nayyar N., Stocum E., Sun J.N., Lindemann M.J., Ho A.W., Hai J.H., Yu J.J., Jung J.W., et al. 2009. Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. J. Exp. Med. 206:299–311 10.1084/jem.20081463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beaucoudrey L., Puel A., Filipe-Santos O., Cobat A., Ghandil P., Chrabieh M., Feinberg J., von Bernuth H., Samarina A., Jannière L., et al. 2008. Mutations in STAT3 and IL12RB1 impair the development of human IL-17–producing T cells. J. Exp. Med. 205:1543–1550 10.1084/jem.20080321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Döffinger R., Helbert M.R., Barcenas-Morales G., Yang K., Dupuis S., Ceron-Gutierrez L., Espitia-Pinzon C., Barnes N., Bothamley G., Casanova J.L., et al. 2004. Autoantibodies to interferon-gamma in a patient with selective susceptibility to mycobacterial infection and organ-specific autoimmunity. Clin. Infect. Dis. 38:e10–e14 10.1086/380453 [DOI] [PubMed] [Google Scholar]
- Dubin P.J., Kolls J.K. 2008. Th17 cytokines and mucosal immunity. Immunol. Rev. 226:160–171 10.1111/j.1600-065X.2008.00703.x [DOI] [PubMed] [Google Scholar]
- Eyerich K., Foerster S., Rombold S., Seidl H.P., Behrendt H., Hofmann H., Ring J., Traidl-Hoffmann C. 2008. Patients with chronic mucocutaneous candidiasis exhibit reduced production of Th17-associated cytokines IL-17 and IL-22. J. Invest. Dermatol. 128:2640–2645 10.1038/jid.2008.139 [DOI] [PubMed] [Google Scholar]
- Filipe-Santos O., Bustamante J., Chapgier A., Vogt G., de Beaucoudrey L., Feinberg J., Jouanguy E., Boisson-Dupuis S., Fieschi C., Picard C., Casanova J.L. 2006. Inborn errors of IL-12/23- and IFN-gamma-mediated immunity: molecular, cellular, and clinical features. Semin. Immunol. 18:347–361 10.1016/j.smim.2006.07.010 [DOI] [PubMed] [Google Scholar]
- Finnish-German APECED Consortium 1997. An autoimmune disease, APECED, caused by mutations in a novel gene featuring two PHD-type zinc-finger domains. Nat. Genet. 17:399–403 [DOI] [PubMed] [Google Scholar]
- Freeman A.F., Holland S.M. 2009. Clinical manifestations, etiology, and pathogenesis of the hyper-IgE syndromes. Pediatr. Res. 65:32R–37R [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner J.M., Devoss J.J., Friedman R.S., Wong D.J., Tan Y.X., Zhou X., Johannes K.P., Su M.A., Chang H.Y., Krummel M.F., Anderson M.S. 2008. Deletional tolerance mediated by extrathymic Aire-expressing cells. Science. 321:843–847 10.1126/science.1159407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glocker E.O., Hennigs A., Nabavi M., Schäffer A.A., Woellner C., Salzer U., Pfeifer D., Veelken H., Warnatz K., Tahami F., et al. 2009. A homozygous CARD9 mutation in a family with susceptibility to fungal infections. N. Engl. J. Med. 361:1727–1735 10.1056/NEJMoa0810719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong M., Ryan K.R., Arkwright P.D., Gennery A.R., Costigan C., Dominguez M., Denning D.W., McConnell V., Cant A.J., Abinun M., et al. 2009. Pattern recognition receptor expression is not impaired in patients with chronic mucocutanous candidiasis with or without autoimmune polyendocrinopathy candidiasis ectodermal dystrophy. Clin. Exp. Immunol. 156:40–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husebye E.S., Perheentupa J., Rautemaa R., Kämpe O. 2009. Clinical manifestations and management of patients with autoimmune polyendocrine syndrome type I. J. Intern. Med. 265:514–529 10.1111/j.1365-2796.2009.02090.x [DOI] [PubMed] [Google Scholar]
- Kampmann B., Hemingway C., Stephens A., Davidson R., Goodsall A., Anderson S., Nicol M., Schölvinck E., Relman D., Waddell S., et al. 2005. Acquired predisposition to mycobacterial disease due to autoantibodies to IFN-gamma. J. Clin. Invest. 115:2480–2488 10.1172/JCI19316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khader S.A., Gaffen S.L., Kolls J.K. 2009. Th17 cells at the crossroads of innate and adaptive immunity against infectious diseases at the mucosa. Mucosal Immunol. 2:403–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitamura T., Tanaka N., Watanabe J., Uchida S., Kanegasaki S., Yamada Y., Nakata K. 1999. Idiopathic pulmonary alveolar proteinosis as an autoimmune disease with neutralizing antibody against granulocyte/macrophage colony-stimulating factor. J. Exp. Med. 190:875–880 10.1084/jem.190.6.875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn T., Bettelli E., Oukka M., Kuchroo V.K. 2009. IL-17 and Th17 cells. Annu. Rev. Immunol. 27:485–517 10.1146/annurev.immunol.021908.132710 [DOI] [PubMed] [Google Scholar]
- LeibundGut-Landmann S., Gross O., Robinson M.J., Osorio F., Slack E.C., Tsoni S.V., Schweighoffer E., Tybulewicz V., Brown G.D., Ruland J., Reis e Sousa C. 2007. Syk- and CARD9-dependent coupling of innate immunity to the induction of T helper cells that produce interleukin 17. Nat. Immunol. 8:630–638 10.1038/ni1460 [DOI] [PubMed] [Google Scholar]
- Liu Y., Yang B., Zhou M., Li L., Zhou H., Zhang J., Chen H., Wu C. 2009. Memory IL-22-producing CD4+ T cells specific for Candida albicans are present in humans. Eur. J. Immunol. 39:1472–1479 10.1002/eji.200838811 [DOI] [PubMed] [Google Scholar]
- Ma C.S., Chew G.Y., Simpson N., Priyadarshi A., Wong M., Grimbacher B., Fulcher D.A., Tangye S.G., Cook M.C. 2008. Deficiency of Th17 cells in hyper IgE syndrome due to mutations in STAT3. J. Exp. Med. 205:1551–1557 10.1084/jem.20080218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Moczygemba M., Doan M.L., Elidemir O., Fan L.L., Cheung S.W., Lei J.T., Moore J.P., Tavana G., Lewis L.R., Zhu Y., et al. 2008. Pulmonary alveolar proteinosis caused by deletion of the GM-CSFRα gene in the X chromosome pseudoautosomal region 1. J. Exp. Med. 205:2711–2716 10.1084/jem.20080759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathis D., Benoist C. 2009. Aire. Annu. Rev. Immunol. 27:287–312 10.1146/annurev.immunol.25.022106.141532 [DOI] [PubMed] [Google Scholar]
- Meager A., Visvalingam K., Peterson P., Möll K., Murumägi A., Krohn K., Eskelin P., Perheentupa J., Husebye E., Kadota Y., Willcox N. 2006. Anti-interferon autoantibodies in autoimmune polyendocrinopathy syndrome type 1. PLoS Med. 3:e289 10.1371/journal.pmed.0030289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meloni A., Furcas M., Cetani F., Marcocci C., Falorni A., Perniola R., Pura M., Bøe Wolff A.S., Husebye E.S., Lilic D., et al. 2008. Autoantibodies against type I interferons as an additional diagnostic criterion for autoimmune polyendocrine syndrome type I. J. Clin. Endocrinol. Metab. 93:4389–4397 10.1210/jc.2008-0935 [DOI] [PubMed] [Google Scholar]
- Milner J.D., Brenchley J.M., Laurence A., Freeman A.F., Hill B.J., Elias K.M., Kanno Y., Spalding C., Elloumi H.Z., Paulson M.L., et al. 2008. Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature. 452:773–776 10.1038/nature06764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minegishi Y., Saito M., Morio T., Watanabe K., Agematsu K., Tsuchiya S., Takada H., Hara T., Kawamura N., Ariga T., et al. 2006. Human tyrosine kinase 2 deficiency reveals its requisite roles in multiple cytokine signals involved in innate and acquired immunity. Immunity. 25:745–755 10.1016/j.immuni.2006.09.009 [DOI] [PubMed] [Google Scholar]
- Minegishi Y., Saito M., Tsuchiya S., Tsuge I., Takada H., Hara T., Kawamura N., Ariga T., Pasic S., Stojkovic O., et al. 2007. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 448:1058–1062 10.1038/nature06096 [DOI] [PubMed] [Google Scholar]
- Minegishi Y., Saito M., Nagasawa M., Takada H., Hara T., Tsuchiya S., Agematsu K., Yamada M., Kawamura N., Ariga T., et al. 2009. Molecular explanation for the contradiction between systemic Th17 defect and localized bacterial infection in hyper-IgE syndrome. J. Exp. Med. 206:1291–1301 10.1084/jem.20082767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagamine K., Peterson P., Scott H.S., Kudoh J., Minoshima S., Heino M., Krohn K.J., Lalioti M.D., Mullis P.E., Antonarakis S.E., et al. 1997. Positional cloning of the APECED gene. Nat. Genet. 17:393–398 10.1038/ng1297-393 [DOI] [PubMed] [Google Scholar]
- Netea M.G., Brown G.D., Kullberg B.J., Gow N.A. 2008. An integrated model of the recognition of Candida albicans by the innate immune system. Nat. Rev. Microbiol. 6:67–78 10.1038/nrmicro1815 [DOI] [PubMed] [Google Scholar]
- Notarangelo L.D., Gambineri E., Badolato R. 2006. Immunodeficiencies with autoimmune consequences. Adv. Immunol. 89:321–370 10.1016/S0065-2776(05)89008-X [DOI] [PubMed] [Google Scholar]
- Patel S.Y., Ding L., Brown M.R., Lantz L., Gay T., Cohen S., Martyak L.A., Kubak B., Holland S.M. 2005. Anti-IFN-gamma autoantibodies in disseminated nontuberculous mycobacterial infections. J. Immunol. 175:4769–4776 [DOI] [PubMed] [Google Scholar]
- Puel A., Picard C., Lorrot M., Pons C., Chrabieh M., Lorenzo L., Mamani-Matsuda M., Jouanguy E., Gendrel D., Casanova J.L. 2008. Recurrent staphylococcal cellulitis and subcutaneous abscesses in a child with autoantibodies against IL-6. J. Immunol. 180:647–654 [DOI] [PubMed] [Google Scholar]
- Robinson M.J., Osorio F., Rosas M., Freitas R.P., Schweighoffer E., Gross O., Verbeek J.S., Ruland J., Tybulewicz V., Brown G.D., et al. 2009. Dectin-2 is a Syk-coupled pattern recognition receptor crucial for Th17 responses to fungal infection. J. Exp. Med. 206:2037–2051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan K.R., Hong M., Arkwright P.D., Gennery A.R., Costigan C., Dominguez M., Denning D., McConnell V., Cant A.J., Abinun M., et al. 2008. Impaired dendritic cell maturation and cytokine production in patients with chronic mucocutanous candidiasis with or without APECED. Clin. Exp. Immunol. 154:406–414 10.1111/j.1365-2249.2008.03778.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki T., Sakagami T., Rubin B.K., Nogee L.M., Wood R.E., Zimmerman S.L., Smolarek T., Dishop M.K., Wert S.E., Whitsett J.A., et al. 2008. Familial pulmonary alveolar proteinosis caused by mutations in CSF2RA. J. Exp. Med. 205:2703–2710 10.1084/jem.20080990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Veerdonk F.L., Marijnissen R.J., Kullberg B.J., Koenen H.J., Cheng S.C., Joosten I., van den Berg W.B., Williams D.L., van der Meer J.W., Joosten L.A., Netea M.G. 2009. The macrophage mannose receptor induces IL-17 in response to Candida albicans. Cell Host Microbe. 5:329–340 10.1016/j.chom.2009.02.006 [DOI] [PubMed] [Google Scholar]
- Zhang S.Y., Boisson-Dupuis S., Chapgier A., Yang K., Bustamante J., Puel A., Picard C., Abel L., Jouanguy E., Casanova J.L. 2008. Inborn errors of interferon (IFN)-mediated immunity in humans: insights into the respective roles of IFN-alpha/beta, IFN-gamma, and IFN-lambda in host defense. Immunol. Rev. 226:29–40 10.1111/j.1600-065X.2008.00698.x [DOI] [PubMed] [Google Scholar]