Histone Deacetylase 6 and Heat Shock Protein 90 Control the Functions of Foxp3+ T-Regulatory Cells (original) (raw)
Abstract
Foxp3+ T-regulatory cells (Tregs) are key to immune homeostasis such that their diminished numbers or function can cause autoimmunity and allograft rejection. Foxp3+ Tregs express multiple histone/protein deacetylases (HDACs) that regulate chromatin remodeling, gene expression, and protein function. Pan-HDAC inhibitors developed for oncologic applications enhance Treg production and Treg suppression function but have limited nononcologic utility given their broad actions and various side effects. We show, using HDAC6-deficient mice and wild-type (WT) mice treated with HDAC6-specific inhibitors, that HDAC6 inhibition promotes Treg suppressive activity in models of inflammation and autoimmunity, including multiple forms of experimental colitis and fully major histocompatibility complex (MHC)-incompatible cardiac allograft rejection. Many of the beneficial effects of HDAC6 targeting are also achieved by inhibition of the HDAC6-regulated protein heat shock protein 90 (HSP90). Hence, selective targeting of a single HDAC isoform, HDAC6, or its downstream target, HSP90, can promote Treg-dependent suppression of autoimmunity and transplant rejection.
INTRODUCTION
The 18 known mammalian histone/protein deacetylases (HDACs) are divided into class I (HDAC1, HDAC2, HDAC3, and HDAC8), class IIa (HDAC4, HDAC5, HDAC7, and HDAC9), class IIb (HDAC6 and HDAC10), class III (SIRT1 to SIRT7), and class IV (HDAC11) groups (21b). Though at first defined by their ability to deacetylate histones and thereby dampen histone-DNA and histone-protein interactions, HDACs were quickly recognized as also affecting the functions of many nonhistone proteins (21). Indeed, like protein phosphorylation, protein acetylation is now considered to be a major posttranslational modification regulating cellular functions (13).
In ongoing studies, broadly active pharmacologic HDAC inhibitors (HDACi) are being evaluated in clinical trials as anticancer agents due to their abilities to promote tumor cell cycle arrest, differentiation, and apoptosis (34, 41). There is also interest in the potential use of HDACi therapy for autoimmunity and transplantation, but there are concerns that the pan-HDACi may be too broadly acting and/or toxic for wide clinical use beyond oncology (55). We have shown that the exposure of a distinct subpopulation of suppressive T cells, so-called Foxp3+ T-regulatory cells (Tregs) (18, 32, 57), to pan-HDACi but not class I-specific HDACi promoted Foxp3 acetylation and increased Treg suppressive functions, with therapeutic efficacy in autoimmune and transplant models (16, 52). The various pan-HDACi are thought to primarily block the functions of classical, Zn2+-dependent class I and class IIb HDACs, since class IIa HDACs appear to lack significant deacetylase activity, at least against canonical substrates (19, 21b). Our pharmacologic and other data thereby suggested the potential relevance of HDAC6, the main class IIb HDAC, as a useful target for therapeutic manipulation in inflammation and autoimmunity.
Primarily cytoplasmic, HDAC6 regulates acetylation of multiple proteins, including α-tubulin and heat shock protein 90 (HSP90), but also has deacetylase-independent functions (3, 21a, 24, 27, 54). Unique in the field of HDACi, HDAC6 isoform-selective inhibitors (HDAC6i) are reported (8, 12, 22, 28, 46, 48, 50). We now show, using HDAC6-deficient mice and HDAC6i, that HDAC6 targeting promotes the suppressive functions of Foxp3+ Tregs and that an important downstream mediator of these actions, HSP90, can be targeted with comparable effects. We conclude that specific targeting of a single HDAC, or one of its key downstream targets, may be an important new approach for the therapy of autoimmunity and transplant rejection.
MATERIALS AND METHODS
Mice.
BALB/c (H-2 d), C57BL/6 (B6, H-2 b), B6/Thy1.1 (H-2 b), and B6/Rag1−/− (H-2 b) mice (The Jackson Laboratory), plus B6/HDAC6−/− (62) (H-2 b) mice, were housed under specific-pathogen-free conditions. Studies were approved by the Institutional Animal Care and Use Committee of the Children's Hospital of Philadelphia.
Reagents.
We purchased geldanamycin, rapamycin (RPM), suberoylanilide hydroxamic acid (SAHA), and trichostatin A (TsA) (Alexis); monoclonal antibodies (MAbs) to acetyl-α-tubulin (6-11B-1; Sigma), Foxp3 (FJK-16S; eBioscience), and indicated cell markers (BD Pharmingen); rabbit antibodies (Abs) to acetyl-HSP90 (K294; Rockland Immunochemicals), acetyllysine (Cell Signaling), and HSC70 (Santa Cruz); and magnetically activated cell separation (MACS) columns for isolation of CD4+ CD25+ Tregs and CD4+ CD25− conventional T cells (Miltenyi). Rabbit anti-acetyl-HSP90 Ab (K69) (60) was kindly provided by Kapil Bhalla (MCG Cancer Center, Augusta, GA), and 17-demethoxygeldanamycin (17-AAG) was kindly provided by Infinity Pharmaceuticals (Cambridge, MA). Production and characterization of the selective HDAC6i compounds tubacin (22) and tubastatin A (8) were described previously. Pan-HDACi (SAHA and TsA), HDAC6i (tubacin and tubastatin A), and HSP90 inhibitors (HSP90i; geldanamycin and 17-AAG) were each dissolved in dimethyl sulfoxide (DMSO) and delivered by intraperitoneal (i.p.) injection or diluted in culture medium prior to use in vitro.
Homeostatic proliferation.
Congenic Thy1.1+ CD4+ CD25− wild-type (WT) conventional T cells and Thy1.2+ CD+ CD25+ Tregs from WT or HDAC6−/− mice were purified on MACS columns and adoptively transferred (1:1 ratio) to B6/Rag1−/− mice (8 to 10 mice/group). Specified groups received daily i.p. injections of DMSO or 17-AAG dissolved in DMSO. Recipient spleen and lymph nodes (LN) were harvested after 7 days, and absolute numbers of Thy1.1+ CD4+ T cells were determined by flow cytometry (52).
Colitis models.
We evaluated the effects of HDAC6 targeting in dextran sodium sulfate (DSS) and adoptive transfer models of colitis (58), using 10 mice per group. Freshly prepared 4% (wt/vol) DSS (MP Biomedicals) was added daily for 5 days to the pH-balanced tap water of WT B6 mice (35). Mice were treated daily for 7 days with tubacin or niltubacin (0.5 mg/kg of body weight/day, i.p.), and colitis was assessed by daily monitoring of body weight, stool consistency, and fecal blood. Stool consistency was scored as 0 (hard), 2 (soft), or 4 (diarrhea), and fecal blood (Hemoccult) was scored as 0 (absent), 2 (occult), or 4 (gross). To assess prevention of colitis in a T cell-dependent model (37), CD4+ CD45RBhi T cells (1 × 106) isolated from WT mice using magnetic beads (>95% cell purity, flow cytometry) were injected i.p. into B6/Rag1−/− mice plus CD4+ CD25+ Tregs (1.25 × 105) isolated using magnetic beads from HDAC6−/− or WT mice (>90% Treg purity, flow cytometry) and mice were monitored biweekly for clinical evidence of colitis. To assess therapy of established T cell-dependent colitis, B6/Rag1−/− mice were injected i.p. with CD4+ CD45RBhi cells (1 × 106). Once colitis had developed, mice also received CD4+ CD25+ Tregs (5 × 105 cells) isolated as described above from HDAC6−/− or WT mice or treatment with HDAC6i (tubastatin A) or HSP90i (17-AAG). Mice were monitored for continued weight loss and stool consistency. At the cessation of the study, paraffin sections of colons stained with Alcian Blue or hematoxylin and eosin were graded histologically or evaluated by immunoperoxidase staining for Foxp3+ Treg infiltration (52).
CD25+ cell depletion.
Mice were thymectomized and treated with depleting CD25 MAb (PC61, 250 μg, i.p.) at 7, 6, and 5 days before induction of colitis; efficacy of depletion was monitored by flow cytometry using a second CD25 MAb (7D4), as described previously (29).
Transplantation.
Survival of heterotopic vascularized cardiac allografts (H2 d_→_H2 b) was monitored by palpation and confirmed by histology (52). Therapies begun at transplantation included 14 days of i.p. injection of tubacin (1.2 mg/kg), tubastatin A (40 mg/kg), 17-AAG (40 mg/kg), RPM, or DMSO carrier. We used low doses of RPM (0.1 mg/kg) that, alone, resulted in only a few days of prolongation of cardiac allograft survival (52).
Treg assays.
Carboxyfluorescein succinimidyl ester (CFSE)-labeled CD4+ CD25− cells (5 × 104/well) were stimulated with CD3 MAb in the presence of irradiated syngeneic antigen-presenting cells (APC) and various ratios of purified CD4+ CD25+ WT or HDAC6−/− Tregs; suppression of proliferation was determined by flow cytometric analysis of CFSE dilution at 72 h (52) using a Cyan flow cytometer (Dako), and data were analyzed using FlowJo software (TreeStar).
Flow cytometry.
Spleen, lymph node, and lamina propria cells were incubated with labeled MAbs to CD4, CD8, CD25, CD44, CD62L, or CD103 for 20 min at 4°C; washed; and analyzed by flow cytometry (45). For intracellular Foxp3 staining (52), cells were treated with GolgiStop (BD Pharmingen), stimulated for 4 h with phorbol myristate acetate (PMA)-ionomycin, stained with cell surface markers, fixed in 0.1% paraformaldehyde, permeabilized, and labeled with allophycocyanin-conjugated anti-Foxp3 MAb.
qPCR.
We performed quantitative reverse transcription-PCR (qPCR) as described previously (52) with correction of differences in cDNA input by normalizing signals obtained with specific primers to 18S rRNA; we excluded nonspecific amplification by performing reverse transcription-PCRs (RT-PCRs) without target cDNA.
Immunoprecipitation and Western blotting.
CD4+ CD25+ Tregs isolated using magnetic beads from WT B6 mice were lysed using radioimmunoprecipitation assay (RIPA) buffer. HSP90 was immunoprecipitated by using rabbit anti-HSP90 Ab (Santa Cruz Biotechnology) and an immunoprecipitation kit (Millipore; Catch and Release v.2.0), and the eluate was evaluated by Western blot analysis using goat anti-rabbit acetylated lysine MAb (Santa Cruz Biotechnology).
T cell migration studies.
Naïve CD45RBhi CD4+ CD25− cells (1 × 106) from WT or HDAC6−/− mice were injected i.p. into B6/Rag1−/− mice. Mice were treated daily for 7 days with tubacin or niltubacin (0.5 mg/kg/day, i.p.). At weekly intervals, mice were euthanized and spleen, peripheral lymph nodes (PLN), and mesenteric lymph nodes (MLN) were analyzed by flow cytometry for the percentages of CD4+ T cells and CD4+ Foxp3+ cells, and colons were assessed for evaluation by histology and immunohistology (52).
Microarray data.
RNA integrity and quantity were analyzed using a DU640 spectrophotometer (Beckman-Coulter). Microarray experiments were performed using whole-mouse-genome oligoarrays (Mouse430a; Affymetrix). Array data were analyzed using Mayday (version 2.10) (5). Array data were subjected to robust multiarray average (RMA) normalization. Normalized data were used for calculating fold changes of up- and downregulated genes using Student's t test. Only data with a false discovery rate (FDR)-adjusted P value of <0.05 and at least 2× differential expression were included in the analysis. Data underwent z-score transformation for display.
Statistics.
Comparisons of in vitro data from three or more groups were analyzed by analysis of variance (ANOVA) for statistical significance, and colitis and allograft survival data were analyzed by log-rank/Mantel-Cox testing; a P value of <0.05 was considered significant.
Microarray data accession number.
We deposited our data in the NCBI Gene Expression Omnibus (GEO) database (www.ncbi.nlm.nih.gov/geo) under accession number GSE27896.
RESULTS
Gene targeting of HDAC6 enhances Foxp3+ Treg suppression.
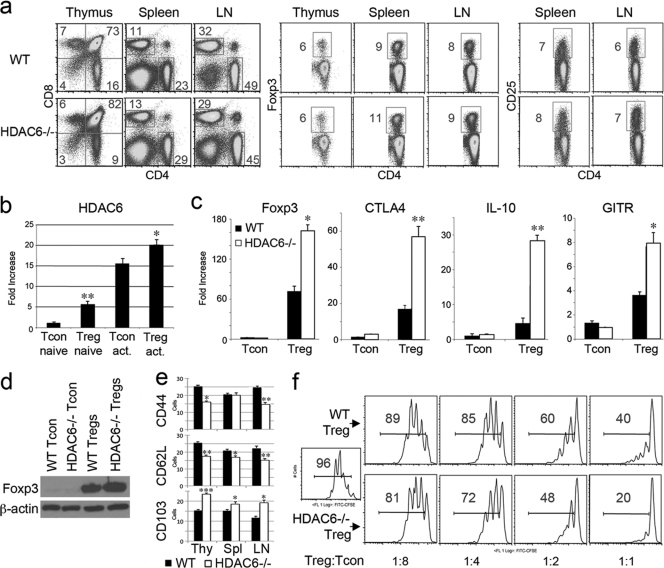
We have shown that in vivo administration of a pan-HDACi, such as SAHA or TsA, can increase the number and suppressive function of Foxp3+ Tregs (52), whereas no effect was seen using a relatively class I-selective HDACi, MS275 (16), leading us to focus on the best-established and best-known catalytically active class IIb HDAC, HDAC6. Both HDAC6-selective inhibitors (HDAC6i) (8, 12, 22, 28, 46, 48, 50) and HDAC6−/− mice (20, 62) have been developed. We began by studying HDAC6−/− mice that have hyperacetylated α-tubulin in various tissues but are otherwise unremarkable, displaying normal lymphocyte development and only a minor reduction in T cell-dependent antibody production (62). Using flow cytometry, we noted that HDAC6−/− mice have slightly more CD4+ CD8+ double-positive thymocytes, and correspondingly fewer single-positive CD4+ and CD8+ cells, than do WT mice, but there were negligible differences in the proportions of CD4+ and CD8+ T cells in secondary lymphoid tissues, and the proportions of CD4+ Foxp3+ and CD4+ CD25+ Tregs were also normal (Fig. 1a). We used qPCR to evaluate HDAC6 expression in resting and T cell-receptor (TCR)-activated CD4+ CD25+ Foxp3+ Tregs and CD4+ CD25− conventional T cells (Tcon cells) isolated from WT C57BL/6 mice and noted a 5-fold-higher expression of HDAC6 in freshly isolated Tregs than in Tcon cells (Fig. 1b, P < 0.01). Compared to WT Tregs, HDAC6−/− Tregs also contained higher levels of Foxp3 (P < 0.05), CTLA-4 (P < 0.01), interleukin-10 (IL-10) (P < 0.01), and GITR (P < 0.05) mRNA expression (Fig. 1c), though levels of Foxp3 protein were only marginally increased (Fig. 1d). Given increased expression of CTLA-4, IL-10, and GITR by effector/memory cells compared with that by naïve Tregs, we assessed additional Treg phenotypic characteristics by flow cytometry. Compared to WT Tregs, HDAC6−/− Tregs had decreased expression of CD44 and CD62L and increased expression of CD103 (Fig. 1e) consistent with a Treg effector/memory phenotype. HDAC6−/− Tregs were also more effective than WT Tregs in suppressing the in vitro proliferation of CFSE-labeled WT Tcon cells (Fig. 1f), whereas HDAC6−/− and WT Tcon cells were equally responsive to suppression by WT Tregs (data not shown). These data show that genetic targeting of HDAC6 does not affect Treg numbers or markedly alter Foxp3 expression but does affect the phenotype of Tregs and, at least in vitro, led to increased Treg suppressive function.
Fig. 1.
HDAC6 deletion enhances Treg suppression. (a) No major differences were seen in proportions of CD4, CD8, or CD4+ Foxp3+ cells in thymi, spleens, or pooled lymph nodes of HDAC6−/− versus WT mice; flow cytometry data representative of 4 mice/group. (b) qPCR analysis of HDAC6 expression in naïve or activated CD4+ CD25− T cells (Tcon) and CD4+ CD25+ (Treg) cells isolated from WT mice; cells were activated with CD3/CD28 MAbs (1 μg/ml). Data (means ± standard deviations, n = 6/group) are expressed as fold increases over levels in naïve Tcon cells (normalized to 18S rRNA); significant differences between corresponding naïve and activated cells are shown (*, P < 0.05; **, P < 0.01). (c) qPCR analysis of Treg genes in naïve WT versus HDAC6−/− Tregs versus Tcon cells; data (means ± standard deviations, n = 6/group) are expressed as fold increases over levels in naïve CD4+ CD25− cells (normalized to 18S rRNA); significant differences between Tregs are shown (*, P < 0.05; **, P < 0.01). (d) HDAC6−/− Tregs cells express ∼1.5-fold more Foxp3 as determined by Western blot analysis of Tregs and Tcon cells (5 × 106) isolated from the spleen and lymph nodes using magnetic beads. (e) Flow cytometric analysis (means ± standard deviations, n = 3/group) of phenotypic markers characteristic of effector/memory Tregs in thymi (Thy), spleens (Spl), or lymph nodes (LN); *, P < 0.05; **, P < 0.01. (f) HDAC6−/− Tregs have increased suppressive capability compared to WT Tregs as shown using in vitro assays. Tregs from each group were added to CFSE-labeled Tcon cells that were activated for 72 h with CD3 MAb and irradiated APC; the percentage of proliferating T cells is shown in each plot; data are representative of 6 experiments. FITC, fluorescein isothiocyanate.
Pharmacologic inhibition of HDAC6 enhances Foxp3+ Treg suppression.
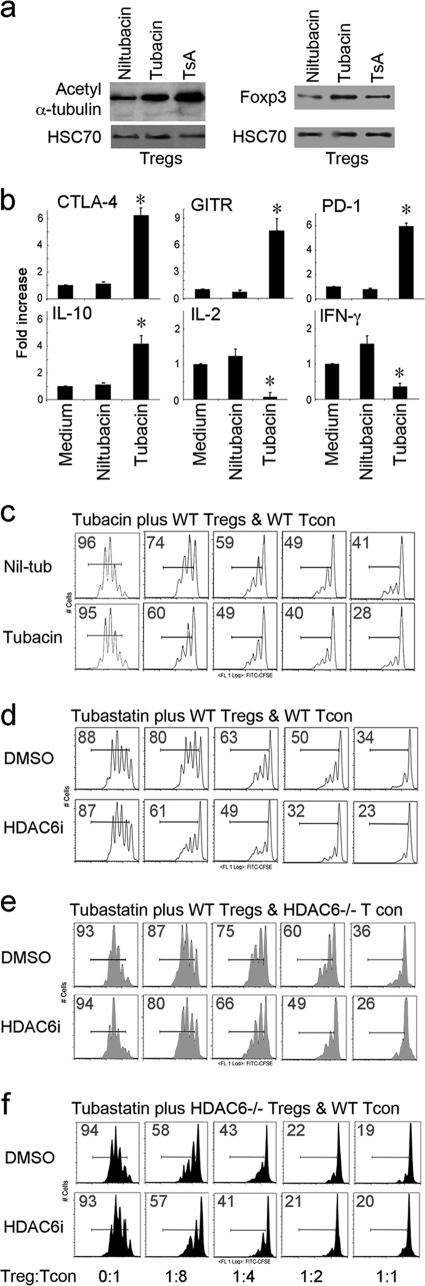
Though examples of Zn2+-dependent HDAC class-selective (14) and subclass-selective (38) compounds are known, HDAC6-selective inhibitors (HDAC6i) were the first, and remain the best-established, HDAC isoform-selective inhibitors to date (9, 50). We have tested 2 of these compounds, including tubacin (22), the first known HDAC6i (and its inactive control, niltubacin), and a recently developed HDAC6i, tubastatin A (8), for their effects on Tregs, with comparable results. Using the example of tubacin (0.1 μM), treatment with HDAC6i or use of the pan-HDACi TsA (20 nM) increased acetylation of α-tubulin in WT Tregs and increased Foxp3 expression by 1.5- to 2-fold (Fig. 2a). Activation of Tregs in the presence of tubacin, but not niltubacin, upregulated the expression of multiple Treg-associated genes (P < 0.05), including CTLA-4, IL-10, PD-1, and GITR, and downregulated expression of IL-2 and gamma interferon (IFN-γ) (_P_ < 0.05) (Fig. 2b). Consistent with these effects, use of tubacin, but not niltubacin, increased the ability of Tregs to suppress the _in vitro_ proliferation of CFSE-labeled Tcon cells but had no effect on Tcon cell proliferation in the absence of Tregs (Fig. 2c and data not shown). Since tubacin is not commercially available and is a large, waxy, complex molecule (>700 Da) with limited bioavailability, we also show results using a recently developed and commercially available HDAC6i, tubastatin A. Tubastatin A is >1,000-fold selective for HDAC6 over other HDACs, except for an ∼57-fold selectivity for HDAC6 versus HDAC8 (8). As with tubacin, tubastatin A use increased Treg suppression of T cell proliferation in vitro (Fig. 2d), and use of cells from WT versus HDAC6−/− mice showed that this effect was independent of HDAC6 expression in Tcon cells (Fig. 2e) but was dependent upon HDAC6 expression in Tregs (Fig. 2f). Hence, use of HDAC6i in vitro had negligible effects on Tcon cell proliferation but promoted Foxp3 and Foxp3-associated gene expression and increased the suppressive capabilities of Tregs in an HDAC6-specific manner.
Fig. 2.
HDAC6i therapy enhances Treg suppression. (a) Increased acetylation of α-tubulin and increased expression of Foxp3 in Western blots of CD4+ CD25+ Tregs treated overnight with tubacin (0.1 μM) or TsA (1 ng/ml) versus control cells treated with niltubacin (0.1 μM). (b) qPCR analysis of gene expression in Tregs isolated from WT mice and treated overnight with tubacin or niltubacin (0.1 μM) or medium alone, plus activating CD3/CD28 MAbs (1 μg/ml); data (means ± standard deviations) are expressed as fold increases over levels in untreated WT Tregs (normalized to 18S rRNA); *, P < 0.01 for tubacin-treated Tregs versus niltubacin or medium alone. (c) Tubacin (0.1 μM) promotes the function of WT Tregs as shown by addition to standard in vitro Treg suppression assays (detailed in Fig. 1f). (d) Experiment similar to that shown in panel c except for use of tubastatin A (100 ng/ml). (e and f) Same conditions as those in panel d but with use of HDAC6−/− CFSE+ Tcon cells (e) or HDAC6−/− Tregs (f) so as to further limit the potential cellular target of added HDAC6i. Data for Treg suppression assays (c to f) are representative of at least 4 experiments.
Migration-independent effects of HDAC6 targeting involve a Treg-associated HSP90 pathway.
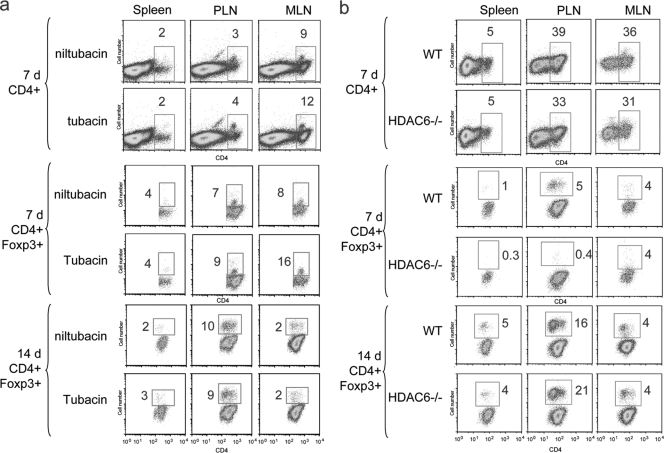
HDAC6 is implicated in the deacetylation of cortactin (61), α-tubulin (24), HSP90 (3, 27), and other proteins, including some, such as tubulin and cortactin, that affect cell migration (54). We therefore tested the effects of HDAC6 targeting on cell migration in vivo, using HDAC6i therapy and also HDAC6−/− versus WT cells. In the case of HDAC6i therapy, we injected CD4+ CD45RBhi naïve WT T cells (1 × 106 cells, <1% Foxp3+) into B6/Rag1−/− mice that lack T and B cells and waited 2 to 3 weeks to allow for their homeostatic proliferation (59). Groups of mice were injected daily with tubacin or niltubacin for 7 days and euthanized at 7 or 14 days, and peripheral lymphoid tissues were evaluated by flow cytometry. There were no significant differences in the numbers of CD4+ or Foxp3+ cells present within lymphoid tissues of mice receiving HDAC6i or control, suggesting equal rates of migration (Fig. 3a). Adoptive transfer of HDAC6−/− CD45RBhi cells to B6/Rag1−/− mice gave comparable data, again with similar numbers of CD4+ cells and as many or more Foxp3+ T cells by day 14 post-transfer of HDAC6−/− versus WT cells (Fig. 3b). These data indicate that HDAC6 targeting in vivo does not impair overall CD4+ T cell migration, proliferation, or the conversion of transferred cells into Foxp3+ Treg cells.
Fig. 3.
Negligible effects of HDAC6i targeting on CD45RBhi T cell migration and proliferation post-adoptive transfer. Rag1−/− mice received naïve WT CD45RBhi CD4+ CD25− cells (1 × 106) by i.p. injection and were treated daily with tubacin or niltubacin (0.5 mg/kg/day, i.p.) for 7 days (a) or WT or HDAC6−/− CD45RBhi CD4+ CD25− cells (1 × 106) (b). Spleens, peripheral lymph nodes (PLN), and mesenteric lymph nodes (MLN) were analyzed by flow cytometry at 7 and 14 days for CD4+ cells and CD4+ Foxp3+ cells; the percentage of indicated cells is shown in each plot; data are representative of 4 experiments.
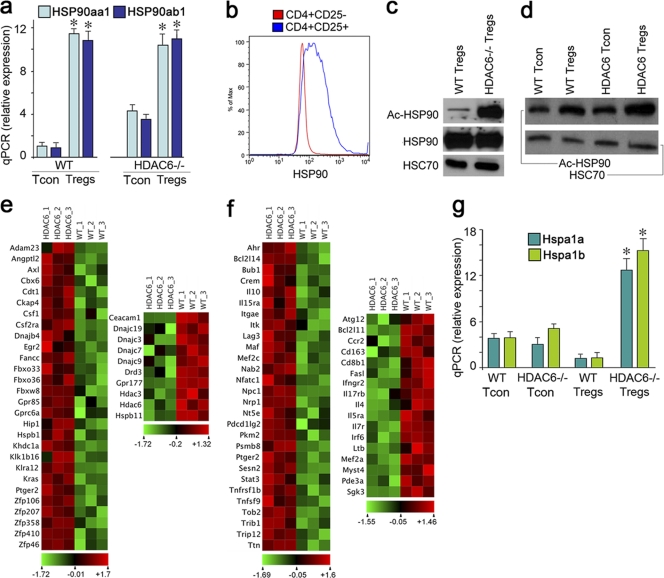
HDAC6 and HSP90 are present in a cytoplasmic complex, and HDAC6 inhibition leads to HSP90 acetylation and disruption of its key chaperone functions (3, 27). We therefore explored aspects of HSP90 expression and acetylation in the context of HDAC6 targeting. HDAC6 depletion led to significantly increased mRNA levels of both HSP90 isoforms in HDAC6−/− cells versus WT controls (Fig. 4a), and Tregs expressed considerably more HSP90 protein than did conventional T cells (Fig. 4b). Moreover, while Western blot analysis showed comparable levels of HSP90 in HDAC6−/− and WT Tregs, HDAC6−/− Tregs had a marked increase in levels of acetylated HSP90 over those in WT controls, as assessed using antibodies directed against acetylated K69 (Fig. 4c) or, to a lesser extent, acetylated K294 (Fig. 4d) of HSP90. Acetylation at K69 (60) or K294 (47) reduces ATP binding to HSP90 and decreases HSP90 binding to its cochaperones and client proteins (60). Many client proteins released upon HSP90 acetylation are degraded through the proteasome, but at least one important client protein, heat shock factor 1 (HSF1), migrates to the nucleus and induces expression of hundreds of genes expressing heat shock elements within their regulatory regions, including HSP90 itself (51, 53). Microarray analysis showed that a large number of known HSF1-regulated genes were upregulated in HDAC6−/− versus WT Tregs and showed reduced expression of a small number of HSF1-regulated genes (Fig. 4e). This analysis also showed that HDAC6 deletion increased the expression of a number of functionally important Treg genes, including Ahr, IL-10, Lag3, Nrp1, Nt5e, and Stat3 genes, and decreased expression of multiple additional cytokines, cytokine receptors, and other genes characteristic of non-Tregs (43) (Fig. 4f). Upregulation of both HSP70 isoforms in HDAC6−/− Tregs versus WT Tregs was confirmed by qPCR (Fig. 4g). This is important since HSP70 is known to form a biochemical complex with Foxp3, and its upregulation can significantly enhance Treg survival and suppressive function in vitro and in vivo (16).
Fig. 4.
HDAC6 targeting increases Treg expression of HSF1-regulated genes. (a) qPCR analysis of HSP90aa1 and HSP90ab1 expression in naïve Tcon cells and Tregs of WT and HDAC6−/− B6 mice; data (means ± standard deviations, n = 6/group) are expressed as fold increases over levels in naïve Tcon cells (normalized to 18S rRNA); *, P < 0.01 for HDAC6−/− versus respective WT cells. (b) Flow cytometry showed increased expression of HSP90 in Tregs versus Tcon cells. (c and d) Western blot analyses showed a marked increase in acetylation of HSP90 in HDAC6−/− Tregs versus WT controls. Lysates of cells isolated using magnetic beads were separated by 10% SDS-PAGE, and blots were probed using Abs to HSP90 and acetylated K69-HSP90 (c) and acetylated K294-HSP90 (d); HSC70 was used as a loading control, and results are representative of 3 experiments. (e and f) Microarray analysis of Tregs isolated from HDAC6−/− and WT mice using the Affymetrix Mouse430a chip. Array data were subjected to robust multiarray average (RMA) normalization and z-score transformation for display and analyzed using Mayday (version 2.10) (5). (e) Genes known to be upregulated by transactivated HSF1 after its release from acetylated HSP90 are shown at left, and additional genes downregulated by HSF1 are shown at right. (f) Genes known to be important to Treg function and upregulated HDAC6−/− Tregs are shown at left, and genes downregulated in HDAC6−/− Tregs are shown at right. (g) qPCR analysis of both inducible HSP70 genes, HSPA1a and HSPA1b, that require HSF1 binding for expression; data (means ± standard deviations, n = 6/group) are expressed as fold increases over levels in naïve Tcon cells (normalized to 18S rRNA) (*, P < 0.01 for CD4+ CD25+ HDAC6−/− Tregs versus all other groups).
Given the increased expression of HSP90 and HSF1-regulated genes in HDAC6−/− Tregs, we assessed the effects on Treg function of HSP90i exposure, using either of two of the most potent HSP90i available, geldanamycin and its derivative 17-AAG. In vitro studies showed that HSP90i use had negligible direct effects on T cell proliferation, as seen with no Tregs added, whereas WT Tregs treated with either HSP90i showed increased suppressive function (Fig. 5a). We next compared the effects of HDAC6 and HSP90 targeting in vivo in a 7-day homeostatic proliferation model (16). Using a 4:1 ratio of conventional T cells to Tregs, injection of WT Tregs did not significantly inhibit T cell expansion, whereas use of HDAC6−/− Tregs significantly decreased proliferation within spleens and lymph nodes (Fig. 5b). Daily injection of 17-AAG likewise significantly decreased homeostatic proliferation in both sites when used in conjunction with WT Tregs but had no additional significant benefit when used in conjunction with HDAC6−/− Tregs. Taken together, these data (Fig. 4 and 5) indicate that HDAC6 targeting can induce HSP90 acetylation, which is known to cause client protein release and the upregulation of multiple HSF1-regulated genes, and we propose that this mechanism may thereby contribute to the significantly increased Treg suppressive functions that we observed both in vitro and in vivo.
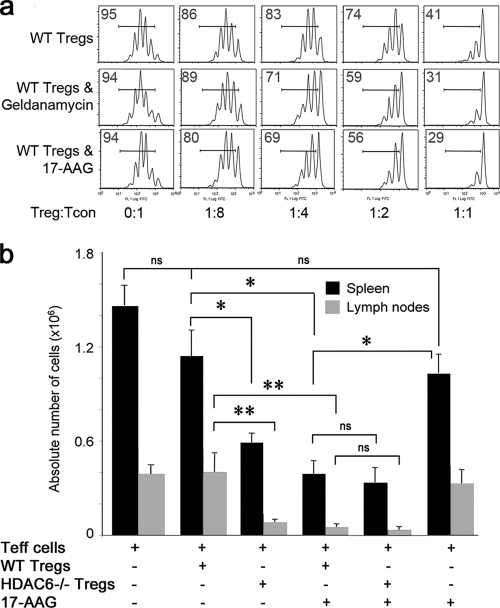
Fig. 5.
Nonadditive effects of joint targeting of HDAC6 and HSP90. (a) In vitro suppression assays comparing effects of treatment of WT Tregs with the HSP90i geldanamycin (3.6 nM) or 17-AAG (0.1 μM); the percentage of dividing CFSE+ Tcon cells in each well is shown at top left, and data are representative of 3 separate experiments. FITC, fluorescein isothiocyanate. (b) Comparable efficacies of HDAC6−/− Tregs and HSP90i therapy in inhibiting homeostatic T cell proliferation. Rag−/− C57BL/6 mice (3/group) were injected intravenously with 1 × 106 Thy1.1+ Tcon cells and 2.5 × 105 cells of either WT or HDAC6−/− Thy1.2+ Tregs. The indicated groups of mice were treated daily with 17-AAG (40 mg/kg) or control DMSO for 7 days. Thereafter, spleens and lymph nodes were collected, single-cell suspensions were prepared, and live Thy1.1+ cells were determined by flow cytometry; total numbers of homeostatic proliferating cells were expressed as absolute numbers of cells × 106. Data are representative of 3 experiments. *, P < 0.05; **, P < 0.01; ns, not significant.
HDAC6 targeting affects the development and progression of murine colitis.
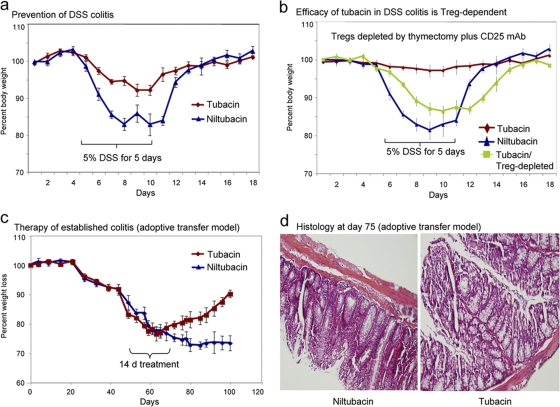
Colitis is a common presentation of children with FOXP3 mutations and associated IPEX (immunodysregulation polyendocrinopathy enteropathy X-linked) syndrome, and murine colitis is widely used for in vivo studies of Treg suppression (33, 36). To evaluate the effects of HDAC6 targeting in vivo, we used 2 different murine models and either of the HDAC6i, which gave comparable results. We began with the dextran sodium sulfate (DSS) model of colitis (16, 52), which, while only partly T cell dependent, allows for a quick assessment of a given agent's anti-inflammatory effects compared to the more lengthy adoptive transfer models used subsequently. We evaluated the effects of administration of the original HDAC6i, tubacin, or its inactive control, niltubacin, from the day of introduction of DSS (5%) to the drinking water, with cessation of DSS after 5 days and of tubacin and niltubacin after 7 days. Mice were monitored for weight loss, diarrhea, and bleeding throughout the experiment. Tubacin-treated mice were protected against development of weight loss and diarrhea (Fig. 6a), and this effect was Treg dependent (Fig. 6b). We also tested tubacin as therapy for a purely T cell-mediated model of colitis induced by injection of B6/Rag1−/− mice with CD4+ CD25− cells. Once mice had lost ∼15% of their initial body weight, they were considered to have developed colitis and were treated with either tubacin or niltubacin. Mice treated with HDAC6i for 14 days began to gain weight ∼10 days into treatment and continued to improve even after discontinuation of tubacin, whereas controls continued to lose weight and required euthanasia due to morbidity (Fig. 6c). Histologic evaluation of colons at 100 days post-cell transfer showed increased mononuclear cell infiltration, goblet cell loss, and areas of mucosal sloughing in niltubacin-treated versus tubacin-treated mice (Fig. 6d).
Fig. 6.
Efficacy of tubacin (HDAC6i) in both prevention and therapy of colitis. (a) Mice receiving DSS plus tubacin or niltubacin (0.5 mg/kg/day) were monitored for weight loss; tubacin-treated mice lost less weight than did niltubacin-treated mice (P < 0.025). (b) Beneficial effects of tubacin therapy in preventing DSS colitis were abrogated by Treg depletion (thymectomy and CD25 MAb) (_P_ > 0.05 versus niltubacin). (c) Rag1−/− mice adoptively transferred with 1 × 106 C57BL/6 CD4+ CD45RBhi cells developed clinical evidence of colitis and >20% weight loss by ∼55 days posttransfer; in contrast to the use of niltubacin, mice treated with tubacin (0.5 mg/kg/day) showed clinical improvement (P < 0.005). (d) Hematoxylin and eosin-stained colonic sections (original magnifications, ×125) from mice shown in panel c at 28 days after initiation of HDAC6i therapy. All studies involved 8 to 10 mice/group, and data are representative of 3 experiments.
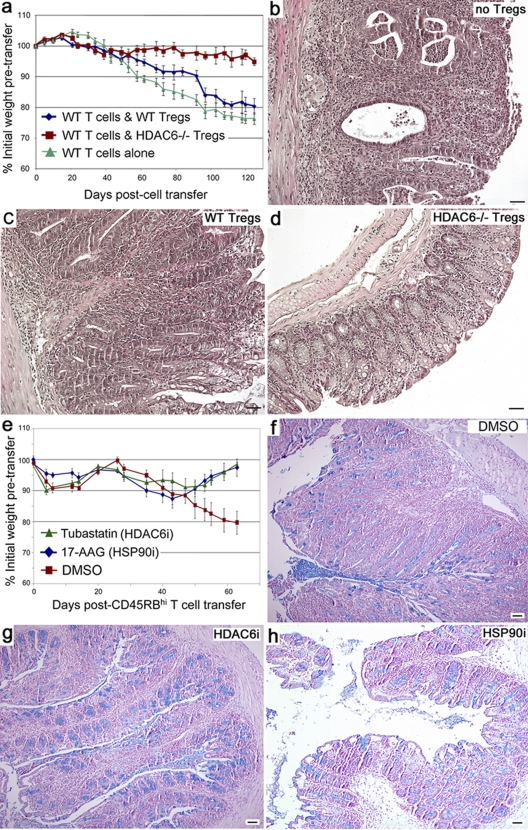
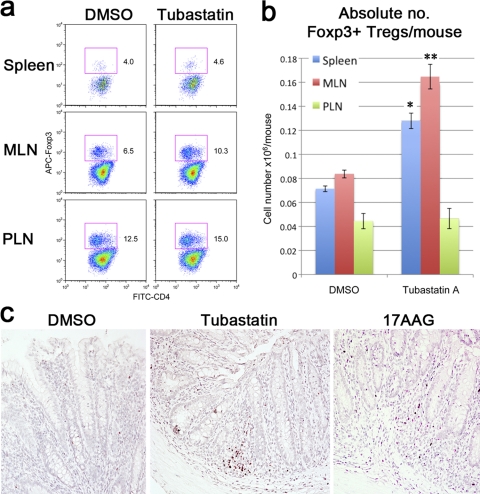
We next analyzed the effects of HDAC6 and HSP90 targeting in the CD45RBhi adoptive transfer model of colitis. A key role for HDAC6 within Tregs was shown by transfer to B6/Rag−/− mice of 1 × 106 CD45RBhi WT T cells plus limiting numbers of purified WT or HDAC6−/− Tregs (0.125 × 106) (Fig. 7a). Mice receiving CD45RBhi T cells alone progressively lost weight and developed diarrhea and by sacrifice at 100 days showed histologic evidence of severe colitis (Fig. 7b), as did mice given WT Tregs (Fig. 7c). However, mice receiving HDAC6−/− Tregs maintained weight and at 100 days showed only minor evidence of colitis, with markedly less mononuclear cell infiltration and mucosal thickening, and preservation of mucosal architecture (Fig. 7d). Pharmacologic targeting of HDAC6 or HSP90 was also efficacious in the CD45RBhi adoptive transfer model of colitis, as shown by studies in which adoptively transferred B6/Rag−/− mice were treated with HDAC6i (tubastatin A) or HSP90i (17-AAG) once colitis was established (Fig. 7e). By 60 days post-CD45RBhi cell transfer, untreated mice had developed diarrhea, lost ∼20% of their starting weight, and showed histologic evidence of severe colitis, with mucosal thickening, mononuclear cell infiltration, goblet cell loss, and areas of mucosal sloughing (Fig. 7f). In contrast, mice treated with HDAC6i or HSP90i recovered body weights (Fig. 7e) and normal stool formation and upon histologic examination showed reduced mononuclear cell infiltration, preservation of goblet cells, and intact mucosal surfaces (Fig. 7g and h). Flow cytometric analysis of lymphoid tissues of treated mice showed increased proportions (Fig. 8a) and absolute numbers (Fig. 8b) of Foxp3+ Tregs in mucosal lymph nodes and spleens compared to DMSO-treated controls, and immunohistology showed markedly increased numbers of intramucosal Foxp3+ Tregs in tubastatin-treated or HSP90i-treated versus DMSO-treated mice (Fig. 8c). Hence, these studies show that targeting of HDAC6, including solely within the Treg compartment, can limit development of colitis and that treatment using HDAC6i or HSP90i can rescue mice once colitis has developed.
Fig. 7.
Effects of HDAC6 and HSP90 targeting on T cell-dependent colitis. (a) B6/Rag1−/− mice (n = 8/group) were adoptively transferred with 1 × 106 WT CD4+ CD45RBhi cells and 1.25 × 105 CD4+ CD25+ cells from naïve WT mice (blue diamonds), HDAC6−/− mice (red squares), or control naïve Tcon cells (green triangles); for data from 60 days onwards, P was <0.05 for WT Tregs versus Tcon cells and P was <0.007 for HDAC6−/− versus WT Tregs. (b to d) Hematoxylin and eosin-stained sections of colons (original magnifications, ×125) harvested at 60 days post-cell transfer of 1 × 106 WT B6 CD4+ CD45RBhi cells and no Tregs (b), WT Tregs (c), or HDAC6−/− Tregs (d). (e) B6/Rag1−/− mice (n = 8/group) adoptively transferred with 1 × 106 WT CD4+ CD45RBhi cells and after 30 days treated daily for 14 days with tubastatin A (25 mg/kg), 17-AAG (40 mg/kg), or DMSO alone; data are presented as weight loss (mean ± standard deviation), and P is <0.01 from 50 days onwards for HDAC6i or HSP90i versus DMSO. (f to h) Alcian Blue-stained sections of colonic samples from groups of mice shown in panel e, including those receiving DMSO alone (f), tubastatin A (g), or 17-AAG (h); note the loss of blue goblet cells and the significant mononuclear infiltrate in the DMSO-treated colon (representative of 3 mice/group).
Fig. 8.
HDAC6i treatment increased Treg numbers in colitic mice. (a) Flow cytometric evaluation of CD4+ Foxp3+ cells in Rag1−/− mice (n = 4/group) adoptively transferred with WT CD4+ CD45RBhi cells (1 × 106) and 30 days later injected daily i.p. with either tubastatin A (25 mg/kg) or DMSO control for 14 days. Mice were then euthanized, and tissues were harvested for flow cytometry. (b) Absolute numbers of Foxp3+ cells isolated from the mice shown in panel a; compared to use of DMSO alone, tubastatin A increased Treg numbers in the spleen (*, P < 0.01) and mesenteric lymph nodes (MLN) (**, _P_ < 0.005), whereas the numbers of Tregs in peripheral lymph nodes (PLN) were unchanged (_P_ > 0.05). (c) Immunoperoxidase staining of representative samples of n = 4/group showing, compared to DMSO-treated mice, increased Foxp3+ Treg infiltration of colons from mice receiving CD45RBhi cells and therapy for 14 days with either HDAC6i (tubastatin A) or HSP90i (17-AAG) once colitis had developed. (Paraffin sections, blue hematoxylin counterstain; diaminobenzidine-positive cells in brown; original magnifications, ×300.)
HDAC6 targeting prevents allograft rejection.
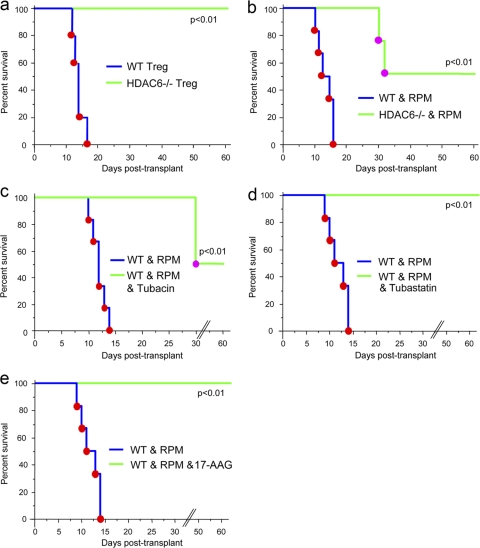
While helpful in the evaluation of Treg function, the available murine colitis models, even the adoptive transfer models, may provide data that may not necessarily have broad implications beyond the specific assay conditions. We therefore also explored the effects of HDAC targeting in fully major histocompatibility complex (MHC)-mismatched transplant models, using BALB/c donors and C57BL/6 recipients, since allografts elicit a powerful immune response without any additional stimulus and involve T cell-dependent effector mechanisms that are shared between all vertebrate species, including humans (23). We began with use of a cardiac allograft model in which acute rejection in B6/Rag−/− mice is mediated by adoptively transferred B6 T cells but can be suppressed by cotransfer of B6 Tregs (52). Using a 4:1 ratio of conventional T cells to Tregs, we found that the acute rejection or long-term engraftment of cardiac allografts could be solely determined by the presence or absence of HDAC6 within the adoptively transferred Treg population (Fig. 9a). In fully immunocompetent hosts, long-term allograft survival (>60 days) was also seen in HDAC6−/− but not WT mice (Fig. 9b) when recipients were treated for 14 days with a subtherapeutic dose of rapamycin (RPM; 0.1 mg/kg/day, i.p.). Likewise, long-term allograft survival was achieved in WT recipients receiving a 14-day course of low-dose RPM plus treatment with HDAC6i, including tubacin (Fig. 9c) and tubastatin A (Fig. 9d), or HSP90i (17-AAG) (Fig. 9e). Hence, targeting HDAC6, including just within the Treg population, can result in long-term allograft survival in fully MHC-disparate combinations.
Fig. 9.
Effects of HDAC6 and HSP90 targeting on T cell-dependent allograft rejection. Kaplan-Meier plots of fully MHC-disparate cardiac allograft survival in B6/Rag1−/− mice adoptively transferred with WT T cells (1 × 106) and 0.25 ×106 WT or HDAC6−/− Tregs (a); WT or HDAC6−/− mice treated for 14 days with low-dose RPM (0.1 mg/kg/day, 14 days) (b); or WT mice treated daily for 14 days with low-dose RPM plus tubacin (1.2 mg/kg) (c), tubastatin A (40 mg/kg) (d), or 17-AAG (40 mg/kg) (e). Data in each panel are from 4 or 5 allografts/group and are representative of 2 separate sets of experiments in each case.
DISCUSSION
While Foxp3 is well defined as a lineage specification factor for the development and function of CD4+ CD25+ Treg cells, practical details as to how to control Foxp3 expression and promote Treg development remain poorly understood. Likewise, proposals to restore immune homeostasis in patients with autoimmunity or transplant rejection have not advanced much beyond the planning stage, given initial data suggesting the potential instability of Treg suppressive functions after ex vivo expansion (42, 53a) and the possible conversion of induced Tregs to other effector cell lineages posttransfer (17, 26). An alternative to adoptive transfer of ex vivo expanded Tregs involves pharmacologic modulation of Treg numbers and/or function, as can be achieved with murine (52) and human (1) Tregs exposed to HDACi. The current study arose from two broad considerations relevant to how HDACi compounds might be employed for the management of inflammatory and autoimmune diseases.
First, not all HDACi promote Treg functions (55). Thus, various pan-HDACi, including TsA, SAHA, and other similar hydroxamate compounds, boost Treg suppression in vitro even at nanomolar concentrations, whereas use of HDAC class I selective compounds, such as the benzamide compounds MS275 and MS1293, had no effect on Treg function when assayed at micromolar levels (56). Moreover, studies in murine colitis models confirmed the efficacy of pan-HDACi in boosting Treg function and reversing established colitis in a Treg-dependent manner, whereas use of HDAC class I-selective inhibitors again had no beneficial effects (16). Since HDAC class IIa enzymes are thought to largely lack potent catalytic activity (19, 21b), the pharmacologic evidence thereby pointed to the importance of HDAC class IIb enzyme targeting in control of Treg functions. There are 2 known HDAC class IIa enzymes, HDAC6 and HDAC10. While little is known of the biology or functions of HDAC10, HDAC6 is known to regulate the acetylation of multiple proteins, such as α-tubulin and HSP90, and also has deacetylase-independent functions (3, 21a, 24, 27, 54). HDAC6 therefore arose as a prime candidate for consideration as a therapeutic target in efforts to promote Treg functions.
Second, there are reasons to seek more selective agents than the various existing pan-HDACi compounds. Use of pan-HDACi agents in clinical trials was linked with serious adverse reactions, including electrocardiographic abnormalities (49) and dose-limiting nausea, vomiting, thrombocytopenia, and profound fatigue (25). Pan-HDACi and class I-selective agents may also promote reactivation of latent viruses, such as HIV (2), and may have adverse effects in patients with chronic obstructive airway disease (4). In addition to evidence that many HDACi compounds induce DNA damage (30), the available data have led to a risk/benefit assessment that existing HDACi are probably best suited to oncologic applications, including therapy of hematologic malignancies (34).
These considerations led us to explore the effects of HDAC6 targeting on Tregs and, by extension, whether isoform-selective HDAC6i might have important advantages as anti-inflammatory agents. HDAC6 was expressed at severalfold-higher levels in Tregs than in Tcon cells, and HDAC6-knockout mice thereby provided a gold standard as to how effective pharmacologic inhibitors of HDAC6 might be expected to be in modulating immune events. HDAC6−/− mice are immunocompetent and not prone to tumorigenesis or chronic infections. However, their Tregs were more suppressive in vitro and in vivo than were WT Tregs. While HDAC6−/− Tregs express more Foxp3, CTLA-4, and IL-10 than do their WT counterparts, the basis for this increased suppressive capability is clearly complex. HDAC6 gene targeting would be expected to disrupt both the deacetylase-dependent and -independent functions of normal HDAC6. The latter encompass multifaceted roles for HDAC6 in regulation of proteasomal degradation (39a) and cell migration (31, 54) and have not been explored with regard to Tregs. Moreover, in the specific context of the accumulation of ubiquitinated proteins following proteasomal inhibition, HDAC6 is critically required in order to induce an HSF1-regulated response (7). However, evidence of the effects of genetic or pharmacologic HDAC6 targeting on deacetylase-dependent functions was readily apparent in our studies, with hyperacetylation of HSP90 and the upregulation of many HSF1-regulated genes in HDAC6−/− Tregs, including multiple HSP family members. While many additional genes of importance to Treg biology, but without known regulation via HSF1, were also differentially expressed in HDAC6−/− Tregs, these actions of the HSF1/HSP pathway are likely of major importance both mechanistically and, as noted below, therapeutically. We have recently shown that HSP70 forms a complex with Foxp3 in Tregs, that upregulation of HSP70 promotes Treg survival and suppressive functions under conditions of cell stress, and that inhibition of HSP70 impairs Treg survival and suppressive functions (16). The current data point to a major role for intracellular heat shock responses in control of Treg functions that warrants further dissection.
In the current study, analysis of the effects of tubacin and tubastatin A on WT versus HDAC6−/− cells supported previous assessments, based on in vitro screening with recombinant proteins, that these small molecules are selective inhibitors of the HDAC6 isoform. Use of these HDAC6i provided data comparable to those seen with HDAC6−/− cells; as a result, these compounds are powerful tools to analyze the effects of HDAC6 targeting on immune responses in normal individuals. Clearly, their administration in vivo can potentially target HDAC6 in many cell types. However, our findings in colitis and transplant models that the presence or absence of HDAC6, just within Tregs, is a powerful determinant of Treg-dependent resolution of colitis, and resistance to allograft rejection, underscore the importance of HDAC6 as a therapeutic target for modulation of Treg responses. Analysis of the effects of HSP90i in vitro and in vivo in our studies indicated that at least for the models under consideration, targeting of HDAC6 and that of HSP90 had broadly comparable effects and the two did not show obvious additional benefits when used together, though different outcomes may well be found in other models. Moreover, such a combination might allow for lower doses of each inhibitor to be used, but the broad message from our work so far is that the benefits of targeting the HSF1/HSP pathway appear to be achieved by pharmacologic modulation of HDAC6 or HSP90. Some 14 HSP90i compounds, including 17-AAG, are currently being evaluated in phase 1 and phase 2 clinical trials; while data are preliminary, toxicity has rarely been observed (39, 40). Clinical development of HDAC6i is less advanced, but HDAC6 targeting is being considered as a therapy for neurodegenerative conditions (8).
Our finding that selective targeting of an individual HDAC isoform can provide effects on Tregs, and associated suppression of T cell-dependent immune responses, comparable with those seen using broadly acting pan-HDACi provides a powerful rationale for the ongoing evaluation of HDACi in the regulation of inflammation. Ultimately, HDAC6 isoform-selective inhibitors may provide an alternate, pharmacologic approach to therapies dependent upon Treg expansion and adoptive transfer for the management of autoimmunity and transplant rejection.
ACKNOWLEDGMENTS
This work was supported by research grants from the National Institutes of Health (K08DK080189 to E.F.D. and P01AI073489 to W.W.H.) and CDHNF/CCFA (2712) grants to E.F.D.
We thank Kapil Bhalla for the gift of anti-acetylated HSP90 Ab.
Footnotes
▿
Published ahead of print on 28 March 2011.
REFERENCES
- 1.Akimova T., et al. 2010. Histone/protein deacetylase inhibitors increase suppressive functions of human FOXP3+ Tregs. Clin. Immunol. 136:348–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Archin N. M., et al. 2009. Expression of latent HIV induced by the potent HDAC inhibitor suberoylanilide hydroxamic acid. AIDS Res. Hum. Retroviruses 25:207–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bali P., et al. 2005. Inhibition of histone deacetylase 6 acetylates and disrupts the chaperone function of heat shock protein 90: a novel basis for antileukemia activity of histone deacetylase inhibitors. J. Biol. Chem. 280:26729–26734 [DOI] [PubMed] [Google Scholar]
- 4.Barnes P. J. 2009. Role of HDAC2 in the pathophysiology of COPD. Annu. Rev. Physiol. 71:451–464 [DOI] [PubMed] [Google Scholar]
- 5.Battke F., Symons S., Nieselt K. 2010. Mayday—integrative analytics for expression data. BMC Bioinformatics 11:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reference deleted.
- 7.Boyault C., et al. 2007. HDAC6 controls major cell response pathways to cytotoxic accumulation of protein aggregates. Genes Dev. 21:2172–2181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butler K. V., et al. 2010. Rational design and simple chemistry yield a superior, neuroprotective HDAC6 inhibitor, tubastatin A. J. Am. Chem. Soc. 132:10842–10846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butler K. V., Kozikowski A. P. 2008. Chemical origins of isoform selectivity in histone deacetylase inhibitors. Curr. Pharm. Des. 14:505–528 [DOI] [PubMed] [Google Scholar]
- 10.Reference deleted.
- 11.Reference deleted.
- 12.Chen Y., et al. 2008. A series of potent and selective, triazolylphenyl-based histone deacetylases inhibitors with activity against pancreatic cancer cells and Plasmodium falciparum. J. Med. Chem. 51:3437–3448 [DOI] [PubMed] [Google Scholar]
- 13.Choudhary C., et al. 2009. Lysine acetylation targets protein complexes and co-regulates major cellular functions. Science 325:834–840 [DOI] [PubMed] [Google Scholar]
- 14.Dejligbjerg M., et al. 2008. Differential effects of class I isoform histone deacetylase depletion and enzymatic inhibition by belinostat or valproic acid in HeLa cells. Mol. Cancer 7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reference deleted.
- 16.de Zoeten E. F., Wang L., Sai H., Dillmann W. H., Hancock W. W. 2010. Inhibition of HDAC9 increases T regulatory cell function and prevents colitis in mice. Gastroenterology 138:583–594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duarte J. H., Zelenay S., Bergman M. L., Martins A. C., Demengeot J. 2009. Natural Treg cells spontaneously differentiate into pathogenic helper cells in lymphopenic conditions. Eur. J. Immunol. 39:948–955 [DOI] [PubMed] [Google Scholar]
- 18.Feuerer M., Hill J. A., Mathis D., Benoist C. 2009. Foxp3+ regulatory T cells: differentiation, specification, subphenotypes. Nat. Immunol. 10:689–695 [DOI] [PubMed] [Google Scholar]
- 19.Fischle W., et al. 2002. Enzymatic activity associated with class II HDACs is dependent on a multiprotein complex containing HDAC3 and SMRT/N-CoR. Mol. Cell 9:45–57 [DOI] [PubMed] [Google Scholar]
- 20.Gao Y. S., et al. 2007. Histone deacetylase 6 regulates growth factor-induced actin remodeling and endocytosis. Mol. Cell. Biol. 27:8637–8647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glozak M. A., Sengupta N., Zhang X., Seto E. 2005. Acetylation and deacetylation of non-histone proteins. Gene 363:15–23 [DOI] [PubMed] [Google Scholar]
- 21a.Grozinger C. M., Hassig C. A., Schreiber S. L. 1999. Three proteins define a class of human histone deacetylases related to yeast Hda1p. Proc. Natl. Acad. Sci. U. S. A. 96:4868–4873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21b.Haberland M., Montgomery R. L., Olson E. N. 2009. The many roles of histone deacetylases in development and physiology: implications for disease and therapy. Nat. Rev. Genet. 10:32–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haggarty S. J., Koeller K. M., Wong J. C., Grozinger C. M., Schreiber S. L. 2003. Domain-selective small-molecule inhibitor of histone deacetylase 6 (HDAC6)-mediated tubulin deacetylation. Proc. Natl. Acad. Sci. U. S. A. 100:4389–4394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hancock W. W., Buelow R., Sayegh M. H., Turka L. A. 1998. Antibody-induced transplant arteriosclerosis is prevented by graft expression of anti-oxidant and anti-apoptotic genes. Nat. Med. 4:1392–1396 [DOI] [PubMed] [Google Scholar]
- 24.Hubbert C., et al. 2002. HDAC6 is a microtubule-associated deacetylase. Nature 417:455–458 [DOI] [PubMed] [Google Scholar]
- 25.Kelly W. K., et al. 2003. Phase I clinical trial of histone deacetylase inhibitor: suberoylanilide hydroxamic acid administered intravenously. Clin. Cancer Res. 9:3578–3588 [PubMed] [Google Scholar]
- 26.Koenen H. J., et al. 2008. Human CD25highFoxp3pos regulatory T cells differentiate into IL-17-producing cells. Blood 112:2340–2352 [DOI] [PubMed] [Google Scholar]
- 27.Kovacs J. J., et al. 2005. HDAC6 regulates Hsp90 acetylation and chaperone-dependent activation of glucocorticoid receptor. Mol. Cell 18:601–607 [DOI] [PubMed] [Google Scholar]
- 28.Kozikowski A. P., Tapadar S., Luchini D. N., Kim K. H., Billadeau D. D. 2008. Use of the nitrile oxide cycloaddition (NOC) reaction for molecular probe generation: a new class of enzyme selective histone deacetylase inhibitors (HDACIs) showing picomolar activity at HDAC6. J. Med. Chem. 51:4370–4373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee I., et al. 2005. Recruitment of Foxp3+ T regulatory cells mediating allograft tolerance depends on the CCR4 chemokine receptor. J. Exp. Med. 201:1037–1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee J. H., Choy M. L., Ngo L., Foster S. S., Marks P. A. 2010. Histone deacetylase inhibitor induces DNA damage, which normal but not transformed cells can repair. Proc. Natl. Acad. Sci. U. S. A. 107:14639–14644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li D., et al. 2011. Microtubule-associated HDAC6 promotes angiogenesis by regulating cell migration in an EB1-dependent manner. Protein Cell 2:150–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu L. F., Rudensky A. 2009. Molecular orchestration of differentiation and function of regulatory T cells. Genes Dev. 23:1270–1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maloy K. J., Powrie F. 2001. Regulatory T cells in the control of immune pathology. Nat. Immunol. 2:816–822 [DOI] [PubMed] [Google Scholar]
- 34.Marks P. A. 2010. The clinical development of histone deacetylase inhibitors as targeted anticancer drugs. Expert Opin. Investig. Drugs 19:1049–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Melgar S., Karlsson A., Michaelsson E. 2005. Acute colitis induced by dextran sulfate sodium progresses to chronicity in C57BL/6 but not in BALB/c mice: correlation between symptoms and inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 288:G1328–G1338 [DOI] [PubMed] [Google Scholar]
- 36.Mottet C., Uhlig H. H., Powrie F. 2003. Cutting edge: cure of colitis by CD4+CD25+ regulatory T cells. J. Immunol. 170:3939–3943 [DOI] [PubMed] [Google Scholar]
- 37.Mudter J., Wirtz S., Galle P. R., Neurath M. F. 2002. A new model of chronic colitis in SCID mice induced by adoptive transfer of CD62L+ CD4+ T cells: insights into the regulatory role of interleukin-6 on apoptosis. Pathobiology 70:170–176 [DOI] [PubMed] [Google Scholar]
- 38.Oyelere A. K., et al. 2009. Non-peptide macrocyclic histone deacetylase inhibitors. J. Med. Chem. 52:456–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pacey S., et al. A phase II trial of 17-allylamino, 17-demethoxygeldanamycin (17-AAG, tanespimycin) in patients with metastatic melanoma. Invest. New Drugs, in press [DOI] [PubMed] [Google Scholar]
- 39a.Pandey U. B., et al. 2007. HDAC6 rescues neurodegeneration and provides an essential link between autophagy and the UPS. Nature 447:859–863 [DOI] [PubMed] [Google Scholar]
- 40.Porter J. R., Fritz C. C., Depew K. M. 2010. Discovery and development of Hsp90 inhibitors: a promising pathway for cancer therapy. Curr. Opin. Chem. Biol. 14:412–420 [DOI] [PubMed] [Google Scholar]
- 41.Rasheed W., Bishton M., Johnstone R. W., Prince H. M. 2008. Histone deacetylase inhibitors in lymphoma and solid malignancies. Expert Rev. Anticancer Ther. 8:413–432 [DOI] [PubMed] [Google Scholar]
- 42.Riley J. L., June C. H., Blazar B. R. 2009. Human T regulatory cell therapy: take a billion or so and call me in the morning. Immunity 30:656–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sadlon T. J., et al. 2010. Genome-wide identification of human FOXP3 target genes in natural regulatory T cells. J. Immunol. 185:1071–1081 [DOI] [PubMed] [Google Scholar]
- 44.Reference deleted.
- 45.Sato T., et al. 2004. Hyperexpression of inducible costimulator and its contribution on lamina propria T cells in inflammatory bowel disease. Gastroenterology 126:829–839 [DOI] [PubMed] [Google Scholar]
- 46.Schafer S., et al. 2008. Phenylalanine-containing hydroxamic acids as selective inhibitors of class IIb histone deacetylases (HDACs). Bioorg. Med. Chem. 16:2011–2033 [DOI] [PubMed] [Google Scholar]
- 47.Scroggins B. T., et al. 2007. An acetylation site in the middle domain of Hsp90 regulates chaperone function. Mol. Cell 25:151–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smil D. V., et al. 2009. Novel HDAC6 isoform selective chiral small molecule histone deacetylase inhibitors. Bioorg. Med. Chem. Lett. 19:688–692 [DOI] [PubMed] [Google Scholar]
- 49.Strevel E. L., Ing D. J., Siu L. L. 2007. Molecularly targeted oncology therapeutics and prolongation of the QT interval. J. Clin. Oncol. 25:3362–3371 [DOI] [PubMed] [Google Scholar]
- 50.Suzuki T., et al. 2006. Highly potent and selective histone deacetylase 6 inhibitors designed based on a small-molecular substrate. J. Med. Chem. 49:4809–4812 [DOI] [PubMed] [Google Scholar]
- 51.Taipale M., Jarosz D. F., Lindquist S. 2010. HSP90 at the hub of protein homeostasis: emerging mechanistic insights. Nat. Rev. Mol. Cell Biol. 11:515–528 [DOI] [PubMed] [Google Scholar]
- 52.Tao R., et al. 2007. Deacetylase inhibition promotes the generation and function of regulatory T cells. Nat. Med. 13:1299–1307 [DOI] [PubMed] [Google Scholar]
- 53.Trinklein N. D., Murray J. I., Hartman S. J., Botstein D., Myers R. M. 2004. The role of heat shock transcription factor 1 in the genome-wide regulation of the mammalian heat shock response. Mol. Biol. Cell 15:1254–1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53a.Trzonkowski P., et al. 2009. First-in-man clinical results of the treatment of patients with graft versus host disease with human ex vivo expanded CD4+ CD25+ CD127− T regulatory cells. Clin. Immunol. 133:22–26 [DOI] [PubMed] [Google Scholar]
- 54.Valenzuela-Fernandez A., Cabrero J. R., Serrador J. M., Sanchez-Madrid F. 2008. HDAC6: a key regulator of cytoskeleton, cell migration and cell-cell interactions. Trends Cell Biol. 18:291–297 [DOI] [PubMed] [Google Scholar]
- 55.Wang L., de Zoeten E. F., Greene M. I., Hancock W. W. 2009. Immunomodulatory effects of deacetylase inhibitors: therapeutic targeting of FOXP3+ regulatory T cells. Nat. Rev. Drug Discov. 8:969–981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang L., Tao R., Hancock W. W. 2009. Using histone deacetylase inhibitors to enhance Foxp3(+) regulatory T-cell function and induce allograft tolerance. Immunol. Cell Biol. 87:195–202 [DOI] [PubMed] [Google Scholar]
- 57.Wing K., Sakaguchi S. 2010. Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat. Immunol. 11:7–13 [DOI] [PubMed] [Google Scholar]
- 58.Wirtz S., Neurath M. F. 2007. Mouse models of inflammatory bowel disease. Adv. Drug Deliv. Rev. 59:1073–1083 [DOI] [PubMed] [Google Scholar]
- 59.Wu Z., et al. 2004. Homeostatic proliferation is a barrier to transplantation tolerance. Nat. Med. 10:87–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yang Y., et al. 2008. Role of acetylation and extracellular location of heat shock protein 90alpha in tumor cell invasion. Cancer Res. 68:4833–4842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang X., et al. 2007. HDAC6 modulates cell motility by altering the acetylation level of cortactin. Mol. Cell 27:197–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang Y., et al. 2008. Mice lacking histone deacetylase 6 have hyperacetylated tubulin but are viable and develop normally. Mol. Cell. Biol. 28:1688–1701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reference deleted.