Type 1 diabetes (original) (raw)
. Author manuscript; available in PMC: 2015 Mar 31.
Abstract
Over the past decade, knowledge of the pathogenesis and natural history of type 1 diabetes has grown substantially, particularly with regard to disease prediction and heterogeneity, pancreatic pathology, and epidemiology. Technological improvements in insulin pumps and continuous glucose monitors help patients with type 1 diabetes manage the challenge of lifelong insulin administration. Agents that show promise for averting debilitating disease-associated complications have also been identified. However, despite broad organisational, intellectual, and fiscal investments, no means for preventing or curing type 1 diabetes exists, and, globally, the quality of diabetes management remains uneven. This Seminar discusses current progress in epidemiology, pathology, diagnosis, and treatment of type 1 diabetes, and prospects for an improved future for individuals with this disease.
Introduction
Type 1 diabetes is generally thought to be precipitated by an immune-associated, if not directly immune-mediated, destruction of insulin-producing pancreatic β cells.1,2 Historically, type 1 diabetes was largely considered a disorder in children and adolescents, but this opinion has changed over the past decade, so that age at symptomatic onset is no longer a restricting factor.3 Polydipsia, polyphagia, and polyuria (the classic trio of symptoms associated with disease onset) along with overt hyperglycaemia remain diagnostic hallmarks in children and adolescents, and to a lesser extent in adults. An immediate need for exogenous insulin replacement is also a hallmark of type 1 diabetes, for which lifetime treatment is needed. Key questions remain regarding the epidemiology of type 1 diabetes, effectiveness of current therapies, understanding how the disorder develops, and preventing or curing the disease.
Epidemiology
Although type 1 diabetes can be diagnosed at any age, it is one of the most common chronic diseases of childhood.4 Peaks in presentation occur between 5–7 years of age and at or near puberty.5 Whereas most autoimmune disorders disproportionately affect women, type 1 diabetes is slightly more common in boys and men.6 The incidence of type 1 diabetes varies with seasonal changes and birth month. More cases are diagnosed in autumn and winter,7 and being born in the spring is associated with a higher chance of having type 1 diabetes.8 Development of type 1 diabetes-associated autoimmunity (ie, formation of islet autoantibodies) in the months or years before onset of symptomatic type 1 diabetes also shows some seasonal synchronisation.9 These concepts support a theoretical role for an environ mental agent initiating or driving the pathogenic processes in type 1 diabetes.
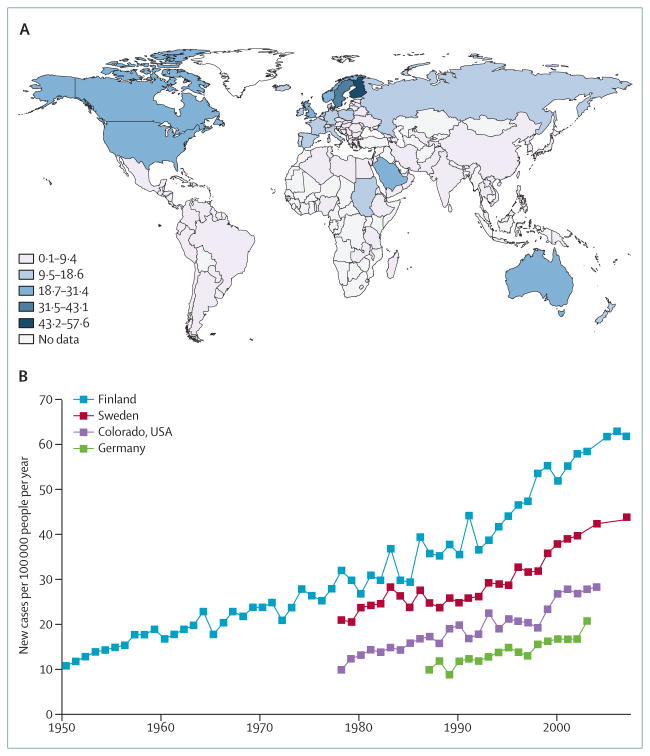
Globally, the incidence and prevalence of type 1 diabetes vary substantially (figure 1).10 Type 1 diabetes is most common in Finland (>60 cases per 100 000 people each year) and Sardinia (around 40 cases per 100 000 people each year).16 By contrast, the disorder is uncommon in China, India, and Venezuela (around 0·1 cases per 100 000 people each year). The global incidence of type 1 diabetes represents an epidemiological conundrum; wide variations in disease incidence are noted between neighbouring areas in Europe and in North America. For example, incidence in Estonia is less than one-third of the incidence in Finland, although the two countries are separated by less than 120 km.17 The incidence of type 1 diabetes has been increasing worldwide for several decades.18 In Finland, Germany, and Norway, annual increases in incidence of 2·4%, 2·6%, and 3·3%, respectively, have been reported.16,19,20 In many countries, the rise in incidence of type 1 diabetes has fluctuated, although Sweden has recently seen incidence rates plateau.12 If incidence rates continue to increase on their existing path, global incidence could double over the next decade.16 Increases in incidence have not occurred equally across all age groups; in Europe, the most substantial increases have been noted in children younger than 5 years of age.5,21 The mechanisms underlying these enigmas in geographical incidence and increased incidence rates of type 1 diabetes are unknown, but have largely been attributed to environmental influences. Genetic changes or more children being born from mothers with type 1 diabetes cannot solely explain such rapid rates of increased incidence.22 Finally, genetic predisposition seems to be less of a factor now than it was in the past as a prerequisite for developing type 1 diabetes.23,24
Figure 1. Incidence of type 1 diabetes in children aged 0–14 years, by geographical region and over time.
(A) Estimated global incidence of type 1 diabetes, by region, in 2011.11 (B) Time-based trends for the incidence of type 1 diabetes in children ages 0–14 years in areas with high or high-intermediate rates of disease.12–15
A plethora of environmental influences have been purported to affect the epidemiology of type 1 diabetes,25 with infant and adolescent diets,26 vitamin D and vitamin D pathway constituents,27–29 and viruses receiving the most focus.30,31 Interest is growing in models to describe the influence of environment on type 1 diabetes, including the hygiene hypothesis32 and gut microbiome;33 however, no specific agents with an unequivocal influence on pathogenesis have been identified.
Diagnosis
Diagnosis of diabetes has historically included fasting blood glucose higher than 7 mmol/L (126 mg/dL), any blood glucose of 11·1 mmol/L (200 mg/dL) or higher with symptoms of hyperglycaemia, or an abnormal 2 horal glucose-tolerance test.34 In 2009, the American Diabetes Association modified their guidelines for diabetes diagnosis to include glycated haemoglobin (HbA1C; a test that averages blood glucose concentrations over 3 months) of 6·5% or higher.35 Despite efforts to standardise diagnosis of type 1 diagnosis, the causes and typology remain unclear. Particularly among adults, diagnosis of type 1 versus type 2 diabetes can be challenging. Around 5–15% of adults diagnosed with type 2 diabetes might actually have type 1 disease with islet autoantibodies present;36 if this is the case, perhaps as many as 50% of actual type 1 diabetes cases are misdiagnosed as type 2, meaning that the number of cases of type 1 disease is vastly underestimated. Accurate diagnosis of this disorder is crucial for optimum care and avoiding complications, and correctly noting diabetic ketoacidosis at diagnosis of type 1 disease represents a key window for survival.37
Attempts to distinguish adult cases of type 1 diabetes from those with type 2 disease have resulted in the proposal of new disease classifications, including latent autoimmune disease of adults (LADA) and ketosis-prone diabetes.38,39 The lack of firm diagnostic criteria for LADA, including retrospective criteria and similarities between patients with type 1 diabetes and LADA, have stunted enthusiasm for adopting it as a novel category for diabetes.40
Disease heterogeneity
Most cases of type 1 diabetes represent an immune, if not autoimmune-mediated disorder, meaning patients often show features of an immunological contribution to disease pathogenesis (eg, autoantibodies or genetic associations with genes controlling immune responses). However, not all patients with type 1 diabetes have these characteristics, leading to proposed classifications of type 1A (autoimmune) diabetes,41 for the 70–90% of patients with type 1 disease that have immunological, self-reactive autoantibodies, and type 1B (idiopathic) diabetes, representing the remainder whose specific pathogenesis remains unclear.42 A subset of individuals within this latter group have monogenic forms of diabetes, such as maturity onset diabetes of the young (MODY).43 Despite knowledge gains that could allow for adopting this new set of terminologies for subgrouping cases of type 1 diabetes, the terms type 1A and type 1B diabetes are not commonly used; similarly, subtypes of type 2 diabetes in children are poorly characterised, particularly in minority populations in the USA.44
Other factors that complicate diagnosis of type 1 diabetes include the growing problem of obesity (both childhood and adult), difficulties in health-care provider recognition of disease, and increasingly diverse genetic admixtures due to migration and social changes.45–47 For example, a third to half of Hispanic and African American children seem to have a form of type 1 diabetes without islet autoantibodies, and with pancreatic histology showing a lack of islets and complete loss of β cells—ie, pseudoatrophic islets.42 A 2011 study of adult-onset type 1 diabetes suggested that autoimmune type 1 diabetes in children and adults differs by just a few age-dependent genetic effects;48 however, overall, type 1 diabetes seems to represent a heterogeneous disease whose pathogenic processes, genetics, and phenotypic characteristics show marked variation.
Pathophysiology
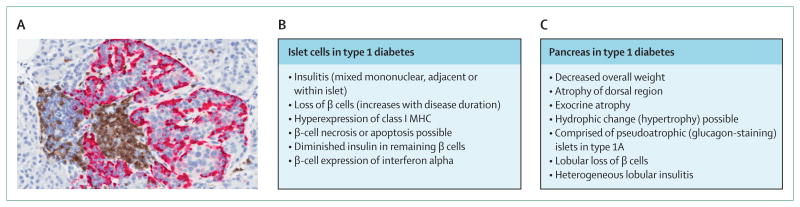
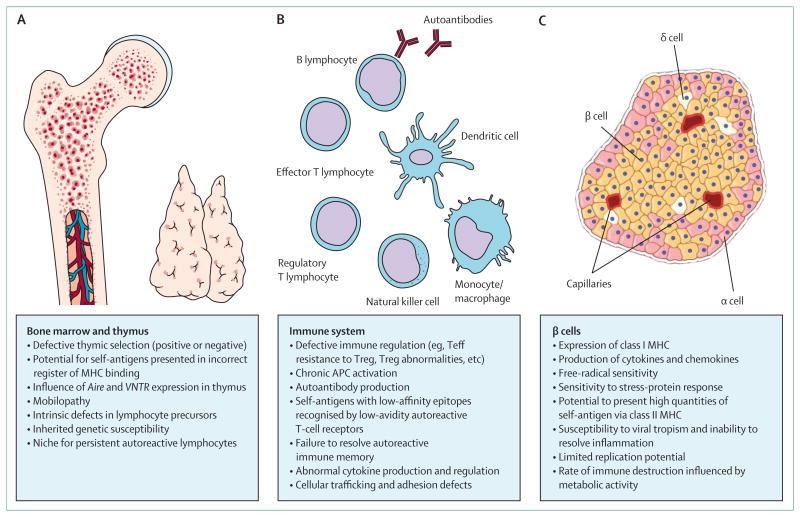
Most research articles on the pathogenesis of type 1 diabetes begin by noting that the disorder results from an autoimmune destruction of insulin-secreting pancreatic β cells. The presence of a chronic inflammatory infiltrate that affects pancreatic islets at symptomatic onset of type 1 diabetes is the basis of this observation (figure 2).49 Another dogma is that in patients with longstanding disease, the pancreas is devoid of insulin-producing cells and the remaining β cells are incapable of regeneration. Both of these concepts of pathogenesis of type 1 diabetes have been debated.50,51 Recent data suggest that although most patients with longstanding type 1 diabetes have few β cells, if any, there is evidence for β-cell regeneration in infants and very young children (but not in adolescents or adults).51,52 Much of what we understand about the pathogenesis of type 1 diabetes derives from analysis of pancreatic specimens, serum, and peripheral-blood lymphocytes obtained from patients with the disorder.53,54 Studies of these constituents suggest that a series of functional defects in the bone marrow and thymus, immune system, and β cells collectively contribute to the pathophysiology of type 1 diabetes (figure 3).
Figure 2. Pathological characteristics of the pancreas in type 1 diabetes.
(A) Islet infiltrate (ie, insulitis) seen in a patient with recent-onset type 1 diabetes. Immunohistochemistry shows the intra-islet presence of CD3-positive cells (brown) and glucagon-producing alpha cells (pink). Image courtesy of M Campbell Thompson, University of Florida, Gainsville, FL, USA. (B) Histological features of islets and (C) gross pathological characteristics of the pancreas associated with the natural history of type 1 diabetes (ie, preonset, onset, postonset).
Figure 3. Physiological contributions to the pathogenic processes that underlie type 1 diabetes.
A series of defects emanating from (A) the bone marrow and thymus, (B) immune system, and (C) β cells collectively lead to loss of insulin production by autoimmune mechanisms. These actions are continuous throughout the natural history of type 1 diabetes. 2,54–56 Teff=effector T cell. Treg=regulatory T cell APC=anaphase-promoting complex.
Pancreatic pathology
Most studies of pancreatic pathology of type 1 diabetes involve retrospective, sample-based analysis of pancreata obtained at autopsy from individuals who died at or near the time of diagnosis, revealing a range of islet cell and whole organ features (figure 2). To overcome limitations with investigations of autopsy tissue, and to extend studies of pancreatic pathology throughout the natural history of type 1 diabetes, efforts are being made in Belgium, Finland, and the USA (Network for Pancreatic Organ Donors with Diabetes [nPOD]57) to collect tissues from cadaveric donors with serological evidence of anti-islet autoimmunity (ie, type 1 diabetes-associated autoantibodies)—a subset of whom would presumably have developed type 1 diabetes if they had survived. Additionally, the nPOD effort attempts to extend investigations to the entire pancreas, rather than be limited by use of a biopsy sample. Through these and other studies, analyses of pancreata from individuals with recent-onset type 1 diabetes suggest that around 70% of islets display complete insulin absence;51,52 nearly 20% of insulin-containing islets, as opposed to only 1% of insulin-deficient islets, are inflamed (ie, insulitis), and many pancreata have non-inflamed insulin-containing islets that seem to be normal.58,59 In patients with type 1 diabetes with surviving β cells, insulitic lesions are usually lobular, analogous to the lobular loss of melanocytes in vitiligo.60 Although it is often stated that symptoms occur when 90–95% of β cells are lost, diagnosis of type 1 diabetes can occur when roughly two-thirds of the islets are devoid of insulin-producing cells.61,62 Among individuals who have had type 1 diabetes for more than 5 years, most of the remaining islets are insulin deficient, containing a normal complement of other hormone secreting cells (ie, α cells that secrete glucagon, δ cells that secrete somatostatin, and PP cells that secrete pancreatic polypeptide).62 Thus, type 1 diabetes involves a selective loss of β cells. In terms of potential pathogenic mechanisms, CD8+ T cells are the most predominant population within the insulitis lesion, followed by (in declining order) macrophages (CD68+), CD4+ T cells, B lymphocytes (CD20+), and plasma cells (CD138+).62 Surprisingly, FOXP3+ cells (ie, regulatory T cells; a population of intense research interest2) and natural killer cells are rare in this lesion. Although much focus has been directed at inflammatory-cell com position, other pancreatic features in type 1 diabetes could have pathogenic significance (figure 3). One of the most underappreciated asps of disease might be pancreatic size. Recent efforts suggest that at the time of diagnosis of type 1 diabetes, and in the period before disease onset (ie, autoantibodies are present), affected individuals have a smaller pancreas compared with age-matched, BMI-matched, and age-plus-BMI-matched individuals.63,64 This feature, combined with the absence of insulitis, suggests that multiple mechanisms lead to the loss of β cells in the pathogenesis of type 1 diabetes.
Serological
A key distinguishing feature between type 1 and type 2 diabetes is the presence of autoantibodies against β-cell autoantigens. More than 90% of individuals with newly diagnosed type 1 diabetes have one or more of the following autoantibodies at disease onset:53 those reactive to insulin (IAA), glutamic acid decarboxylase (GADA), insulinoma-associated autoantigen 2 (IA2A), and zinc transporter 8 (ZnT8A).65 These autoantibodies can appear as early as 6 months of age, with a peak incidence before 2 years of age in genetically susceptible individuals;66 thus, they are present months to years before symptomatic onset. In addition to having diagnostic value in type 1 diabetes, autoantibodies can help identify people with an increased risk for developing the disease, through detection in first-degree relatives or in the general population. IAA concentration correlates with the rate of progression to overt type 1 diabetes in children followed from birth.67,68 This finding, combined with an extensive series of independent investigations in humans and in rodent models of type 1 diabetes, support the growing notion that proinsulin is a key autoantigen in the disease;69 a concept that might partly explain the selective β-cell loss in type 1 diabetes.
Lipid and metabolite profiles can also serve as markers for impending type 1 diabetes; these markers include decreased phosphatidylcholine at birth, and reduced triglycerides and antioxidant ether phospholipids followed by increased proinflammatory lysophosphatidylcholine several months before seroconversion to auto antibody positivity.70 Another study found higher concentrations of odd-chain triglycerides and poly-unsaturated fatty acid-containing phospholipids, and lower concentrations of methionine, in those who developed type 1 diabetes-associated autoantibodies.71
Genetics
Type 1 diabetes is clearly a polygenic disorder, with nearly 40 loci (so far) known to affect disease susceptibility.72 The HLA region on chromosome 6 (ie, the IDDM1 locus) provides perhaps one-half of the genetic susceptibility that leads to risk of type 1 diabetes.73 Of the many HLA types, HLA class II show the strongest association with type 1 diabetes, where haplotypes DRB1*0401-DQB1*0302 and DRB1*0301-DQB1*0201 confer the greatest susceptibility, and DRB1*1501 and DQA1*0102-DQB1*0602 provide disease resistance.74 Class I MHCs also seem to influence risk for type 1 diabetes, independent of class II molecules.73 Of the remaining loci, only those for the insulin VNTR, PTPN22, CTLA4, and IL2RA are associated with odds ratios greater than 1·1.75 Most of the loci associated with risk of type 1 diabetes are thought to involve immune responses,72 supporting the notion that the genetic influences involve mechanisms that collectively contribute to aberrant immune responsive ness, including the development and maintenance of tolerance. This mechanism might help explain the differing rates of progression to type 1 diabetes in adults versus children, where only minor variations in genetic susceptibility have been noted.48 Genetic susceptibility might also influence responses to environmental stimuli or physiological pathways (eg, vitamin D and interferon induced helicase).29,76
Natural history
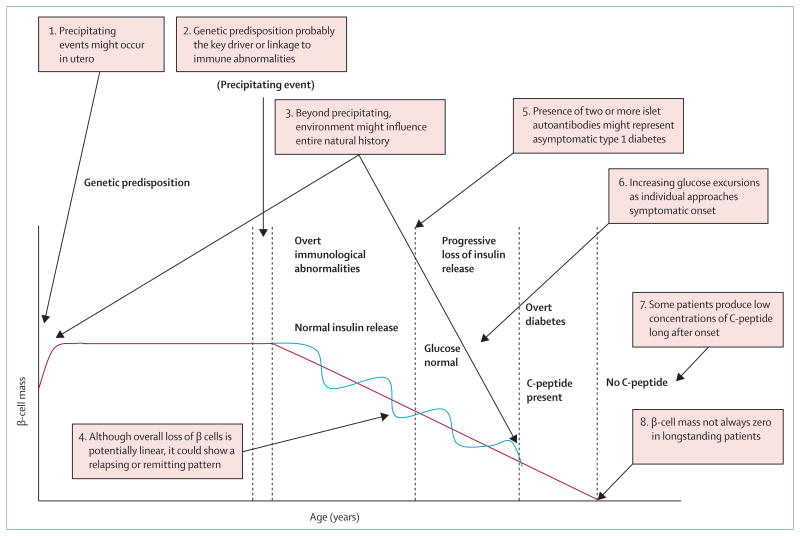
A model originally posed in 1986,77 updated in our 2001 article,78 and modified subsequently, poses that individuals are born with various degrees of genetic susceptibility for type 1 diabetes. Although this model has stood the test of time, some modifications should be considered due to knowledge gains (figure 4). For example, environmental influences might occur as early as in utero and probably continue during the first months to years of life, thereby affecting the onset and continuance of β-cell autoimmunity. Physiological events, including immune-system development and normal turnover of β cells, might also contribute to these pathogenic processes.55 Inherent immune dysregulation, probably facilitated by genetic susceptibility, results in early serological evidence of β-cell destruction—ie, altered aminoacids and autoantibodies associated with type 1 diabetes. In most individuals, changes in insulin secretion and glucose tolerance occur months to decades after multiple islet autoantibodies are detected.79 Not all individuals with anti-β-cell autoimmunity progress to overt disease (less than 5% who express a single type 1 diabetes-associated autoantibody progress41), for reasons unknown. Metabolic changes in the natural history of type 1 diabetes are marked by decreased early C-peptide response at least 2 years before onset,80 increased glucose fluctuations as an individual approaches onset,81 and an overall linear rise, with a last-minute surge, in plasma glucose in the months before onset.82 Once a critical mass (not well defined) of β cells is destroyed, symptomatic onset occurs, and the need for exogenous insulin replacement begins. This symptomatic onset happens after a silent phase that lasts for months to many years, that could, in genetically susceptible individuals with multiple autoantibodies, be considered asymptomatic type 1 diabetes. This classification seems appropriate in view of the ongoing disease processes and the near certainty that such individuals will eventually become symptomatic (insulin dependent). The loss of β-cell mass probably affects the performance of remaining β cells and other islet cell types, as shown by functional (and structural) studies. This disease feature will probably have implications for detecting and defining the stage of decline and the effect of therapeutic interventions.83 After diagnosis, the ability to retain residual β-cell function (assessed by production of C-peptide) is heterogeneous, in terms of the time it takes to reach an undetectable stage and the number of patients who, despite decades with type 1 diabetes, retain the ability to produce C-peptide.84 Thus, disease hetero geneity is an important asp of type 1 diabetes, and suggests a role for genetics, age at disease onset, and intensity of disease management on the ability to retain β-cell function.
Figure 4. The natural history of type 1 diabetes—a 25-year-old concept revisited.
A re-creation of the model of type 1 diabetes, originally proposed in 1986, is shown in black.77 Additions and conjures based on recent knowledge gains are shown in purple.
Management of type 1 diabetes
The discovery of insulin in 1921–22 was clearly the most significant therapeutic event in the history of type 1 diabetes; however, exogenous insulin replacement does not always provide the metabolic regulation necessary to avoid one or more disease associated-complications (eg, retinopathy, neuropathy, cardio vascular disease, and hypoglycaemia). As a result, diabetes management in modern countries often includes use of insulin analogues and mechanical technologies (eg, insulin pumps and continuous glucose monitors) for improved treatment of type 1 disease.85 In the future, therapies that closer emulate the physiological role of the endocrine pancreas will, hopefully, improve lifestyles in addition to preventing complications. As a fi rst step, global disparities in insulin access and diabetes management must be addressed.
Present care
After initial diagnosis and metabolic stabilisation, some patients with type 1 diabetes retain the ability to produce endogenous insulin. Although this endogenous secretion is typically low, maintenance is important since it is associated with less retinopathy and less severe hypoglycaemia at later stages of the disease.86 Therefore, preserving insulin secretion after disease onset is increasingly a therapeutic goal, and can involve intensive insulin therapy, mechanical technologies, or, as in several trials, immune intervention to disrupt β-cell destruction. C-peptide is secreted from β cells at a one-to-one ratio with insulin, and analysis of C-peptide concentration after disease onset shows that loss is more rapid in the fi rst year after diagnosis than in the second year.83 Furthermore, children and adolescents lose endogenous insulin production at a greater rate than do adults with type 1 diabetes.
Several methods exist for metabolic optimisation via insulin therapy. With multiple daily injions, a long-acting insulin analogue provides basal insulin and a rapid-acting insulin is administered before meals, based on grams of carbohydrate consumed (ie, basal-bolus therapy). Over the past decade, use of continuous sub cutaneous insulin infusions (CSII; insulin pumps) has increased substantially.87 A randomised controlled trial in adults with type 1 diabetes reported lower HbA1C concentrations with sensor-augmented pump therapy than with injection therapy, and a greater proportion of patients reaching the targeted levels of HbA1C.88 A meta-analysis has also shown that insulin pumps lower HbA1C concentrations more than multiple daily injections in adults with type 1 diabetes, with similar rates of hypoglycaemia.89 However, whether CSII is better, overall, than multiple daily injection for management of type 1 diabetes is debated, since outcomes reported in studies have varied substantially.90
In addition to improved insulin preparations and delivery systems, advancements to enhance glycaemic control and lessened hypoglycaemia include point-of-care HbA1C measurements, self-monitoring blood-glucose reports, and real-time continuous glucose monitors. Tamborlane and colleagues91 reported that a real-time continuous glucose monitoring system decreased the amount of time spent in hypoglycaemia (<4 mmol/L [70 mg/dL]) and lowered HbA1C when used by patients an average of 6 days a week. In this study, the degree of HbA1C reduction directly correlated with higher HbA1C concentrations before beginning continuous glucose monitoring. In a second study, continuous glucose monitoring lowered nocturnal hypoglycaemia in children (<18 years) with type 1 diabetes, compared with self-monitored blood glucose.92 Therefore, continuous glucose monitoring is most appropriate for highly motivated patients with type 1 diabetes who are willing to wear the monitoring device, and those with continuous poor control during intensive insulin therapy.93
With insulin pumps and continuous glucose monitor ing improving diabetes care, these two technologies are now being used together as sensor-augmented pump therapy. A trial comparing a sensor-augmented pump with multiple daily injection therapy showed significant improvement in HbA1C reduction with less hypoglycaemia in the sensor-augmented pump cohort.88,94 Although current sensor-augmented pump therapy uses each device independently, integration of both systems is being investigated. A key element for such efforts involves low-glucose suspend systems that monitor blood glucose with a continuous glucose monitor and suspend insulin delivery when glucose falls below a preset threshold for up to 2 h, to prevent hypoglycaemic episodes.95 Low-glucose suspend systems are currently available for clinical use in Europe, but remain in clinic trial testing in the USA.
Future care
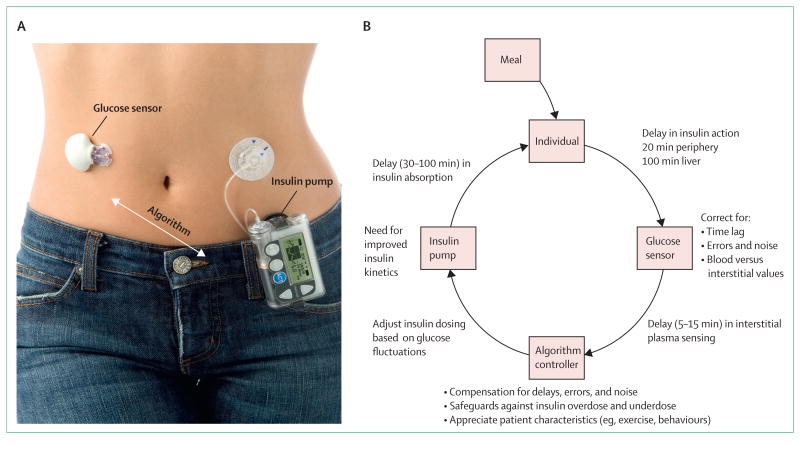
Insulin pumps and continuous glucose monitors are making substantial progress in diabetes care, with additional improvements on the horizon. Efforts are underway to combine insulin pumps and continuous glucose monitors with a computer algorithm—ie, an integrated closed-loop system, or artificial pancreas (figure 5). The integrated closed-loop systems tested so far have reported favourable results;97 when comparing the safety and efficacy of overnight closed-loop delivery of insulin with conventional insulin-pump therapy in adults with type 1 diabetes, closed-loop delivery improved overnight control of glycaemia and reduced the risk of nocturnal hypoglycaemia.98,99 It is hoped that newer generations of continuous glucose monitors will have improved signal transmission and accuracy, and avoid the need for finger-stick glucose calibration.
Figure 5. Closed-loop system for type 1 diabetes therapy (artificial pancreas).
(A) Prototype of a closed-loop system.96 (B) Components of a closed-loop system. Three potential delays in the system include glucose sensing in interstitial fluid, insulin absorption (depends on use of rapid vs regular insulin), and insulin action in peripheral tissues and liver.
New insulin analogues, incretins, and other hormones are being investigated for their ability to improve management of type 1 diabetes. Examples include insulin degludec (recently approved for use in the EU, although approval declined by the US Food and Drug Administration), an analogue that might improve basal insulin administration in patients with type 1 diabetes, since it provides effective glycaemic control and reduces the risk of nocturnal hypoglycaemia.100 GLP-1 might also prove beneficial, with studies noting that this incretin decreased peak postprandial glucose by 45% regardless of residual β-cell function.101 The hormone pramlintide has been shown to reduce postprandial hyperglycaemia, bodyweight, insulin dosage, and HbA1C concentrations, and to reduce postprandial glucagon and glucose excursions and slow gastric emptying.102 Leptin, the adipocyte hormone, might also benefit type 1 diabetes therapy via its ability to reverse a catabolic state through suppression of hypergluca-gonaemia.103 Amidst the optimism surrounding potential benefits with these new therapies, the need for long-term studies validating their safety in large populations remains.
Burden of type 1 diabetes: complications, excess mortality, and insulin access
The physical, social, and economic costs of type 1 diabetes are difficult to calculate, and attempts to quantify these variables typically do not distinguish between type 1 and type 2 disease. However, two studies have provided cost estimates specifically for type 1 diabetes, proposing an annual figure of $14·4–14·9 billion in the USA.104,105 Regardless of the financial costs, achieving normoglycaemia is an important therapeutic goal for patients with type 1 diabetes, especially for avoiding complications.
Complications associated with type 1 diabetes
Complications in type 1 (and type 2) diabetes are classified as macrovascular or microvascular. Cardiovascular disease is becoming a more common macrovasular complication as individuals with in type 1 diabetes live longer.106 Individuals with type 1 diabetes have a ten-times higher risk for cardiovascular events (eg, myocardial infarction, stroke, angina, and the need for coronary-artery revascularisation) than age-matched non-diabetic populations.107 The Pittsburgh Epidemiology of Diabetes Complications study108 of type 1 diabetes reported cardiovascular events in adult patients younger than 40 years of age to be 1% per year, and three times higher in individuals older than 55 years. The Epidemiology of Diabetes Interventions and Complications (EDIC) study,109 which followed participants with type 1 diabetes for long-term complications, found intensive diabetes treatment reduced the risk of cardiovascular events by 42% compared with conventional treatment. Patients with type 1 diabetes have less favourable outcomes than non-diabetic patients after an acute coronary event,110 a finding that might be explained by a recent report that, after myocardial infarction, patients with type 1 diabetes express antibodies to cardiac proteins, whereas patients with type 2 diabetes do not.111 The risk for microvascular complications, including retinopathy, nephropathy, and neuropathy, decreases with intensive insulin therapy. Over the past 5 years, several large clinical trials have advanced the prediction and prevention of microvascular complications (table 1).
Table 1. Large-scale studies on prediction and prevention of complications associated with type 1 diabetes.
| Complications assessed | Main findings | |
|---|---|---|
| Diabetes Control and Complications Trial (DCCT)/Pittsburgh Epidemiology of Diabetes Complications study (2009)112 | Cardiovascular disease, nephropathy, retinopathy | The frequencies of serious complications in patients with type 1 diabetes, especially when treated intensively, are lower than those reported historically |
| Finnish Diabetic Nephropathy (FinnDiane)Study (2009)113 | Cardiovascular disease, nephropathy | In patients with type 1 diabetes, variations in glycated haemoglobin concentration predicted the incidence of microalbuminuria and progression to renal disease, and incidence of cardiovascular disease |
| DCCT/Epidemiology of Diabetes Interventions and Complications (EDIC)study (2011)114 | Nephropathy | In patients with type 1 diabetes and persistent microalbuminuria, intensive glycaemic control, blood pressure control, and favourable lipid panels lead to fewer long-term renal complications |
| FinnDiane (2009)115 | Nephropathy | An independent and graded association exists between the presence and severity of kidney disease and premature mortality in type 1 diabetes |
| Genetics of Diabetes in Kidney Collection(2009)116 | Nephropathy | Identified genes associated with susceptibility to diabetic nephropathy, near the FRMD3 and CARS loci |
| Swedish Renal Registry (2010)117 | Nephropathy | Substantial differences in risk for nephropathy in male versus female patients with type 1 diabetes, with age at diagnosis an important factor (early diagnosis lowers risk) |
| DCCT/EDIC (2009)118 | Autonomic neuropathy | Patients given intensive insulin therapy had less cardiac autonomic neuropathy than those who received conventional treatment |
| Acetyl-L-carnitine Clinical Trials (2009)119 | Neuropathy | Raised triglycerides correlate with progression of diabetic neuropathy |
| DCCT/EDIC (2008)120 | Retinopathy | Intensive insulin therapy (vs conventional therapy) reduces development and progression of diabetic retinopathy, with a treatment-related difference (metabolic memory) continuing for at least 10 years |
| DIabetic REtinopathy Candesartan Trials(DIRECT; 2008)121 | Retinopathy | The angiotensin receptor blocker, candesartan, reduces retinopathy development but does not stop retinopathy progression |
Access to insulin
Despite the progress made for treatment of type 1 diabetes, individuals in many parts of the world die because of lack of access to insulin.122 For example, in Mozambique, the life expectancy for a newly diagnosed child with type 1 diabetes is 7 months.123 Inequalities in the availability of technologies to reduce complications, improve quality of life, and improve diabetes manage ment (eg, HbA1C testing and blood-glucose monitoring) also raise ethical concerns. Much public debate has centred on why the global community accepts this treatment disparity.124 Fortunately, organisations such as the International Diabetes Federation, Life for a Child, Insulin for Life, and others are developing means to alleviate this disparity.
Prevention and cure
Nearly three decades have passed since the first immune-based therapies, using ciclosporin, were attempted to reverse type 1 diabetes.125 Many practical and intellectual advances have been made since then, including improved metabolic testing, better understanding of disease pathogenesis, and availability of immune markers.126 Efforts to prevent or cure type 1 diabetes are now done via large collaborative networks (eg, NIH TrialNet, Immune Tolerance Network, and Islet Cell Transplantation Consortium), with rigorous mechanistic assays and uniform protocols. Finally, although controversial, therapeutic interventions have clearly benefited from studies in animal models of type 1 diabetes, particularly the NOD mouse.127
Primary and secondary prevention
Since type 1 diabetes is now a predictable disease, several large trials are investigating methods to prevent or delay the onset of disease. Primary prevention studies, in individuals with a genetic risk for type 1 diabetes but without islet autoantibodies, have largely focused on dietary modifications early in infancy. A study in Finland128 identified 230 infants with a first-degree relative with type 1 diabetes, and randomly assigned infants to receive a hydrolysed infant formula or conventional formula whenever breast milk was not available during the first 6–8 months of life. Children who received the hydrolysed formula were less likely to develop two or more islet autoantibodies compared with those who received the conventional formula, with an unadjusted hazard ratio of 0·52.128 Another trial removed bovine insulin from infant formula and reported less progression (compared with infants who received normal cow's milk formula) to the development of one islet autoantibody after 3 years of follow-up.129
Studies of secondary prevention, to delay onset of type 1 diabetes, are done in individuals with multiple islet autoantibodies but without overt hyperglycaemia. In one trial, individuals with at least two islet autoantibodies (one being an antibody against insulin) who had a first degree relative with type 1 diabetes, received oral insulin.130 Overall, administration of oral insulin did not delay progression to overt diabetes, but a post-hoc analysis suggested that individuals with high titre insulin autoantibodies benefited from treatment—it was estimated that diabetes onset was delayed as much as 5 years.131 Other agents used for secondary prevention, nicotinamide and intranasal insulin, have not been shown to delay or prevent diabetes onset.132,133
Reversal
Currently, there are no approved agents to stop the autoimmune destruction of β cells after diagnosis of type 1 diabetes. In the past 5 years, interest in reversal of type 1 diabetes has grown.134 In addition to preserving production of C-peptide, a key goal is to induce immune tolerance against β cells and thereby halt autoimmune destruction. Most approaches involve provision of self-antigen (eg, vaccination with specific islet-cell proteins, such as insulin or GAD) or immune suppression (table 2). Disappointingly, after promising phase 1–2 trials in patients with recent-onset type 1 diabetes and detectable endogenous insulin production, phase 3 trials of anti-CD3 antibodies (otelixizumab and teplizumab), and the Diamyd vaccine (GAD-alum immunotherapy) did not meet primary endpoints.135–141 Administration of DiaPep277, a synthetic immunomodulator, at 3-month intervals resulted in less of a decline in stimulated C-peptide concentrations at 1 year in adults with type 1 diabetes than in the cohort that received placebo.142,143 Other phase 2 studies of immune modulators showed evidence of therapeutic efficacy in settings of recent-onset type 1 diabetes; however, even with continued use, most did not show durable effects. For example, the fusion protein CTLA4-Ig (abatacept) preserved stimulated C-peptide concentration for only 9 months despite continuous intravenous administration for 2 years.138 These results imply that single-agent immunosuppression alone might be insufficient to completely control the autoimmune destruction of β cells, or that more specific and targeted therapies are needed. Combination therapies that target several pathogenic pathways and improve β-cell viability might be needed to preserve endogenous insulin production in patients with type 1 diabetes. A 2007 trial of autologous haematopoietic stem-cell transplantation combined with high-dose immunosuppression (ie, cytoxan and thymoglobulin) reported increased C-peptide production and insulin independence in most patients who received treatment at disease onset.144 However, the effects of this invasive treat ment waned over time, with loss of insulin independence in most patients after 5 years.145 It is crucial to re-examine the design and metabolic and immunological outcomes of these phase 2–3 trials, and to consider disease hetero geneity, to better understand how to approach reversal of type 1 diabetes.146,147 Additionally, testing agents that target inflammation (eg, anakinra [interleukin-1 receptor antagonist] and canakinumab [anti-interleukin-1b com pound]), alone or in combination could prove beneficial.148
Table 2. Agents assessed as immunomodulatory therapy to reverse type 1 diabetes.
| Study phase and year | Main findings | |
|---|---|---|
| Insulin APL (NBI-6042) | Phase 2; 2009 | No change in metabolic response (ie, C-peptide preservation)135 |
| Anti-CD20 (rituximab) | Phase 2; 2011 | Preservation of C-peptide concentrations at 1 year, but no difference from placebo at2 years136 |
| Anti-CD3 (teplizumab) | Phase 3; 2011 | Although phase 2 studies showed preservation of C-peptide concentrations, phase I trials (Protégé study)137 showed no change in metabolic respons and the study stopped early |
| CTLA4—immunoglobulin fusion protein (abatacept) | Phase 2; 2011 | T-cell co-stimulatory modulation slowed reduction in β-cell function over 2 years, although preservation of C-peptide was seen for 9·6 months138 |
| Anti-CD3 (otelixizumab) | Phase 3; 2011 | Although phase 2 studies showed preservation of C-peptide concentrations, a phase 3 trial showed no change in metabolic response139 |
| GAD65 protein (Diamyd) | Phase 3; 2012 | Phase 2 studies reported preserved C-peptide concentration, with no improvements in insulin needs. Two phase 3 trials did not meet endpoints140,141 |
| HSP60 (DiaPep277) | Phase 3; 2012 | Phase 2 trials suggested increased C-peptide concentrations; a phase 3 trial noted C-peptide preservation at 1 year, but only in adults (age 16-45 years) with type 1 diabetes142 |
Islet-cell transplantation
In 2000, a breakthrough protocol was developed for islet transplantation without the use of glucocorticoids for immune suppression;149 the initially promising results deteriorated so that at 5 years, only 10% of patients remained independent of exogenous insulin.150 Therefore, islet transplantation remains an experimental procedure, with ongoing research focusing on new methods using biomaterials (eg, encapsulation), immune modulation, site of delivery, improved vascularisation, and more.151 Many of the limitations for islet transplantation hold true for another promising area, the use of stem cells as insulin-producing surrogates for β cells. It remains hopeful that an insulin-producing cell (stem cell, cadaveric islet, xenogeneic islet, etc), combined with an immunoprotive barrier (ie, encapsulation) will provide a therapeutically meaningful advance.
Unanswered questions
This is a season of change with respect to understanding of the epidemiology, pathogenesis, treatment, and prospects for curing type 1 diabetes. In hindsight, many long-held goals once thought readily achievable have been difficult to realise, and concepts regarded as dogmas have proven to be flawed.
Lessons learned
Despite the advances in type 1 diabetes research and therapy, some researchers and clinicians are disappointed by a perceived lack of progress. Large investments in terms of time, finances (foundation, government, and industry-based), and patient resources have been directed to several promising areas—ie, islet-cell transplantation, stem cells, genetics, primary and secondary disease prevention, and reversal of type 1 diabetes—with results that are often deemed to have limited benefit.134
Type 1 diabetes has proven to be much more resistant than initially expected to therapeutic interventions with conventional or experimental agents, whether the goal is disease prevention or reversal.152 Inability to overcome the autoimmune nature of this disease, perhaps the result of robust immunological memory combined with failure to attenuate deleterious immune responses that are not subject to normal regulation, is a hurdle that needs to be addressed with intense research. Similarly, islet-cell transplantation depends on overcoming recurrent autoimmunity and averting alloimmunity.153 Additional hurdles for islet-cell transplantation include a limited donor pool and the need for chronic immunosuppression (or a method to induce long-term immunological tolerance) to allow for functional engraftment. To achieve progress with islet-cell transplantation, investigators are focusing on xenotransplantation, encapsulation, novel sites for cell delivery (eg, eye), and development of surrogate insulin-producing cells.151
Investigations into the genetic basis of type 1 diabetes have been criticised for making little headway into understanding the pathogenesis of this disease. The polygenic nature of type 1 diabetes (more than 40 loci have been associated with disease susceptibility or resistance72) combined with environmental associations mean that disease pathogenesis can be unpredictable. An additional complication arises from the fact that although many genotypic associations with the disease exist, the specific phenotypes resulting from these genetic influences are largely unknown. Efforts are underway to assign specific phenotypes to genotypes, and to improve understanding of the genetic risk for type 1 diabetes by genotyping at multiple susceptibility loci.154
Difficulty understanding the genetic complexity of type 1 diabetes is compounded by a lack of knowledge regarding the immune response in this disorder. Despite decades of investigation, the mechanisms by which β cells are eliminated or selectively destroyed (apart from antigen-specific immune responses) remain unclear.55 Over the past decade, investigators have devoted much effort to describing the putative role for adaptive, rather than innate immune responses, in terms of their pathogenic contributions to type 1 diabetes. Understanding the innate and adaptive immune response, and the role of β cells in the pathogenesis of type 1 diabetes, will be crucial for development of improved therapies. Fortunately, well organised trial networks (eg, NIH TrialNet and Immune Tolerance Network) and registries (eg, T1D Exchange) can test agents capable of providing therapeutic benefit, improve patient recruitment, and increase the precision of disease prediction.155 Additional modifications that could improve the applicability of type 1 diabetes research include changes in clinical trial design (eg, adaptive trial design),156 identifying more practical therapies (in terms of finance and delivery of public health care), better defining disease heterogeneity,147 utilising animal models of type 1 diabetes more effectively,127 and applying the concept that type 1 diabetes begins long before symptomatic onset. Redefining type 1 diabetes as having a silent or asymptomatic state (eg, multiple autoantibodies, genetic risk, with varying degrees of dysglycaemia) could allow therapeutic interventions to be given earlier in the natural history of disease when they might be more effective. This concept is based on studies in animal models of type 1 diabetes, where earlier interventions seem to be more efficacious, and the belief that intervention before a critical threshold of remnant β-cell mass is lost would avoid several sequelae that are often present at symptomatic onset (eg, glucose toxicity, stress response, etc).
Where do we go from here?
Knowledge voids that have long existed for type 1 diabetes, unfortunately, remain today. The most pressing questions are: what environmental constituents un equivocally contribute to the formation of type 1 diabetes? In what way does genetic susceptibility contribute to disease development? Can a safe and effective closed-loop therapy system be developed? What drugs should be used in attempts to prevent or reverse type 1 diabetes? Are agents capable of instilling long-term immunological tolerance available? Can improved markers for predicting disease development be obtained? Can β-cell replication and neogenesis be safely induced in humans? Finally, why are pancreatic β cells specifically targeted for destruction, and do inherent processes contribute to their demise? These questions form a roadmap for the next generation of investigations, and if properly addressed, should result in substantial improvements in the lives of individuals burdened with type 1 diabetes.
Acknowledgments
This work was partly supported by grants from the National Institutes of Health, the Juvenile Diabetes Research Foundation, the American Diabetes Association, the Brehm Coalition for Type 1 Diabetes research, the Children's Diabetes Foundation, the Helmsley Trust, and the Jeffrey Keene Family Professorship.
Footnotes
Contributors: All authors planned the outline, contributed to figures and tables, and wrote and approved the manuscript. MAA and AWM did the literature search.
Conflicts of interest: MAA serves, or has served, as an adviser to Genzyme, Diamyd, GlaxoSmithKline, Takeda, Tolerx, Coronado Biosciences, Sanofi, Exsulin, Grifols, and Amylin. GSE served as an adviser to Sanofi. GSE and AWM received research support from Novartis.
Search strategy and selection criteria: We searched Medline from Jan 1, 2008, to Feb 1, 2013, with the terms “type 1 diabetes”, with restrictions for studies in humans and articles published in English. Earlier articles were derived from our longstanding reference collections.
Contributor Information
Mark A Atkinson, Department of Pathology and Department of Pediatrics, University of Florida, Gainesville, FL, USA.
George S Eisenbarth, Barbara Davis Center for Childhood Diabetes, Aurora, CO, USA.
Aaron W Michels, Barbara Davis Center for Childhood Diabetes, Aurora, CO, USA.
References
- 1.Todd JA. Etiology of type 1 diabetes. Immunity. 2010;32:457–67. doi: 10.1016/j.immuni.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Bluestone JA, Herold K, Eisenbarth G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature. 2010;464:1293–300. doi: 10.1038/nature08933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leslie RD. Predicting adult-onset autoimmune diabetes: clarity from complexity. Diabetes. 2010;59:330–31. doi: 10.2337/db09-1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gale EA. Type 1 diabetes in the young: the harvest of sorrow goes on. Diabetologia. 2005;48:1435–38. doi: 10.1007/s00125-005-1833-0. [DOI] [PubMed] [Google Scholar]
- 5.Harjutsalo V, Sjoberg L, Tuomilehto J. Time trends in the incidence of type 1 diabetes in Finnish children: a cohort study. Lancet. 2008;371:1777–82. doi: 10.1016/S0140-6736(08)60765-5. [DOI] [PubMed] [Google Scholar]
- 6.Ostman J, Lonnberg G, Arnqvist HJ, et al. Gender differences and temporal variation in the incidence of type 1 diabetes: results of 8012 cases in the nationwide Diabetes Incidence Study in Sweden 1983–2002. J Intern Med. 2008;263:386–94. doi: 10.1111/j.1365-2796.2007.01896.x. [DOI] [PubMed] [Google Scholar]
- 7.Moltchanova EV, Schreier N, Lammi N, Karvonen M. Seasonal variation of diagnosis of type 1 diabetes mellitus in children worldwide. Diabet Med. 2009;26:673–78. doi: 10.1111/j.1464-5491.2009.02743.x. [DOI] [PubMed] [Google Scholar]
- 8.Kahn HS, Morgan TM, Case LD, et al. Association of type 1 diabetes with month of birth among US youth: the SEARCH for Diabetes in Youth study. Diabete. Care. 2009;32:2010–15. doi: 10.2337/dc09-0891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kukko M, Kimpimaki T, Korhonen S, et al. Dynamics of diabetes-associated autoantibodies in young children with human leukocyte antigen-conferred risk of type 1 diabetes recruited from the general population. J Clin Endocrinol Metab. 2005;90:2712–17. doi: 10.1210/jc.2004-1371. [DOI] [PubMed] [Google Scholar]
- 10.Maahs DM, West NA, Lawrence JM, Mayer-Davis EJ. Epidemiology of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39:481–97. doi: 10.1016/j.ecl.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 12.Berhan Y, Waernbaum I, Lind T, Mollsten A, Dahlquist G. Thirty years of prospective nationwide incidence of childhood type 1 diabetes: the accelerating increase by time tends to level off in Sweden. Diabetes. 2011;60:577–81. doi: 10.2337/db10-0813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ehehalt S, Dietz K, Willasch AM, Neu A. Epidemiological perspectives on type 1 diabetes in childhood and adolescence in Germany: 20 years of the Baden-Wurttemberg Diabetes Incidence Registry (DIARY) Diabetes Care. 2010;33:338–40. doi: 10.2337/dc09-1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knip M. Pathogenesis of type 1 diabetes: implications for incidence trends. Horm Res Paediatr. 2011;76(suppl 1):57–64. doi: 10.1159/000329169. [DOI] [PubMed] [Google Scholar]
- 15.TEDDY Study Group. The Environmental Determinants of Diabetes in the Young (TEDDY) Study. Ann NY Acad Sci. 2008;1150:1–13. doi: 10.1196/annals.1447.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G, EURODIAB Study Group Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet. 2009;373:2027–33. doi: 10.1016/S0140-6736(09)60568-7. [DOI] [PubMed] [Google Scholar]
- 17.Podar T, Solntsev A, Karvonen M, et al. Increasing incidence of childhood-onset type I diabetes in 3 Baltic countries and Finland 1983–1998. Diabetologia. 2001;44(suppl 3):17–20. doi: 10.1007/pl00002947. [DOI] [PubMed] [Google Scholar]
- 18.Dabelea D. The accelerating epidemic of childhood diabetes. Lancet. 2009;373:1999–2000. doi: 10.1016/S0140-6736(09)60874-6. [DOI] [PubMed] [Google Scholar]
- 19.Thunander M, Petersson C, Jonzon K, et al. Incidence of type 1 and type 2 diabetes in adults and children in Kronoberg, Sweden. Diabetes Res Clin Pract. 2008;82:247–55. doi: 10.1016/j.diabres.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Ehehalt S, Dietz K, Willasch AM, Neu A. Prediction model for the incidence and prevalence of type 1 diabetes in childhood and adolescence: evidence for a cohort-dependent increase within the next two decades in Germany. Pediatr Diabetes. 2012;13:15–20. doi: 10.1111/j.1399-5448.2011.00799.x. [DOI] [PubMed] [Google Scholar]
- 21.DIAMOND Project Group. Incidence and trends of childhood type 1 diabetes worldwide 1990–1999. Diabet Med. 2006;23:857–66. doi: 10.1111/j.1464-5491.2006.01925.x. [DOI] [PubMed] [Google Scholar]
- 22.Soltesz G, Patterson CC, Dahlquist G. Worldwide childhood type 1 diabetes incidence—what can we learn from epidemiology? Pediatr Diabetes. 2007;8(suppl 6):6–14. doi: 10.1111/j.1399-5448.2007.00280.x. [DOI] [PubMed] [Google Scholar]
- 23.Gillespie KM, Bain SC, Barnett AH, et al. The rising incidence of childhood type 1 diabetes and reduced contribution of high-risk HLA haplotypes. Lancet. 2004;364:1699–700. doi: 10.1016/S0140-6736(04)17357-1. [DOI] [PubMed] [Google Scholar]
- 24.Steck AK, Armstrong TK, Babu SR, Eisenbarth GS. Stepwise or linear decrease in penetrance of type 1 diabetes with lower-risk HLA genotypes over the past 40 years. Diabetes. 2011;60:1045–49. doi: 10.2337/db10-1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maclaren N, Atkinson M. Is insulin-dependent diabetes mellitus environmentally induced? N Engl J Med. 1992;327:348–49. doi: 10.1056/NEJM199207303270509. [DOI] [PubMed] [Google Scholar]
- 26.Knip M, Virtanen SM, Akerblom HK. Infant feeding and the risk of type 1 diabetes. Am J Clin Nutr. 2010;91:1506–13. doi: 10.3945/ajcn.2010.28701C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Svoren BM, Volkening LK, Wood JR, Laffel LM. Significant vitamin D deficiency in youth with type 1 diabetes mellitus. J Pediatr. 2009;154:132–34. doi: 10.1016/j.jpeds.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blanton D, Han Z, Bierschenk L, et al. Reduced serum vitamin D-binding protein levels are associated with type 1 diabetes. Diabetes. 2011;60:2566–70. doi: 10.2337/db11-0576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cooper JD, Smyth DJ, Walker NM, et al. Inherited variation in vitamin D genes is associated with predisposition to autoimmune disease type 1 diabetes. Diabetes. 2011;60:1624–31. doi: 10.2337/db10-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yeung WC, Rawlinson WD, Craig ME. Enterovirus infection and type 1 diabetes mellitus: systematic review and meta-analysis of observational molecular studies. BMJ. 2011;342:35. doi: 10.1136/bmj.d35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stene LC, Rewers M. Immunology in the clinic review series; focus on type 1 diabetes and viruses: the enterovirus link to type 1 diabetes: critical review of human studies. Clin Exp Immunol. 2012;168:12–23. doi: 10.1111/j.1365-2249.2011.04555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bach JF, Chatenoud L. The hygiene hypothesis: an explanation for the increased frequency of insulin-dependent diabetes. Cold Spring Harb Perspect Med. 2012;2:a007799. doi: 10.1101/cshperspect.a007799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boerner BP, Sarvetnick NE. Type 1 diabetes: role of intestinal microbiome in humans and mice. Ann NY Acad Sci. 2011;1243:103–18. doi: 10.1111/j.1749-6632.2011.06340.x. [DOI] [PubMed] [Google Scholar]
- 34.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(suppl 1):64–71. doi: 10.2337/dc12-s064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–34. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tuomi T. Type 1 and type 2 diabetes: what do they have in common? Diabetes. 2005;54(suppl 2):40–45. doi: 10.2337/diabetes.54.suppl_2.s40. [DOI] [PubMed] [Google Scholar]
- 37.Usher-Smith JA, Thompson MJ, Sharp SJ, Walter FM. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ. 2011;343:4092. doi: 10.1136/bmj.d4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leslie RD, Kolb H, Schloot NC, et al. Diabetes classification: grey zones, sound and smoke: Action LADA 1. Diabetes Metab Res Rev. 2008;24:511–19. doi: 10.1002/dmrr.877. [DOI] [PubMed] [Google Scholar]
- 39.Naik RG, Brooks-Worrell BM, Palmer JP. Latent autoimmune diabetes in adults. J Clin Endocrinol Metab. 2009;94:4635–44. doi: 10.1210/jc.2009-1120. [DOI] [PubMed] [Google Scholar]
- 40.Gale EA. Latent autoimmune diabetes in adults: a guide for the perplexed. Diabetologia. 2005;48:2195–99. doi: 10.1007/s00125-005-1954-5. [DOI] [PubMed] [Google Scholar]
- 41.Eisenbarth GS. Update in type 1 diabetes. J Clin Endocrinol Metab. 2007;92:2403–7. doi: 10.1210/jc.2007-0339. [DOI] [PubMed] [Google Scholar]
- 42.Gianani R, Campbell-Thompson M, Sarkar SA, et al. Dimorphic histopathology of long-standing childhood-onset diabetes. Diabetologia. 2010;53:690–98. doi: 10.1007/s00125-009-1642-y. [DOI] [PubMed] [Google Scholar]
- 43.Hattersley A, Bruining J, Shield J, Njolstad P, Donaghue KC. The diagnosis and management of monogenic diabetes in children and adolescents. Pediatr Diabetes. 2009;10(suppl 12):33–42. doi: 10.1111/j.1399-5448.2009.00571.x. [DOI] [PubMed] [Google Scholar]
- 44.Dabelea D, Bell RA, D'Agostino RB, Jr, et al. Incidence of diabetes in youth in the United States. JAMA. 2007;297:2716–24. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- 45.Wilkin TJ. The accelerator hypothesis: a review of the evidence for insulin resistance as the basis for type I as well as type II diabetes. Int J Obes (Lond) 2009;33:716–26. doi: 10.1038/ijo.2009.97. [DOI] [PubMed] [Google Scholar]
- 46.Soderstrom U, Aman J, Hjern A. Being born in Sweden increases the risk for type 1 diabetes—a study of migration of children to Sweden as a natural experiment. Acta Paediatr. 2012;101:73–77. doi: 10.1111/j.1651-2227.2011.02410.x. [DOI] [PubMed] [Google Scholar]
- 47.Puett RC, Lamichhane AP, Nichols MD, et al. Neighborhood context and incidence of type 1 diabetes: the SEARCH for Diabetes in Youth study. Health Place. 2012;18:911–16. doi: 10.1016/j.healthplace.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Howson JM, Rosinger S, Smyth DJ, Boehm BO, Todd JA. Genetic analysis of adult-onset autoimmune diabetes. Diabetes. 2011;60:2645–53. doi: 10.2337/db11-0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.In't Veld P. Insulitis in human type 1 diabetes: the quest for an elusive lesion. Islets. 2011;3:131–38. doi: 10.4161/isl.3.4.15728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Butler PC, Meier JJ, Butler AE, Bhushan A. The replication of beta cells in normal physiology, in disease and for therapy. Nat Clin Pract Endocrinol Metab. 2007;3:758–68. doi: 10.1038/ncpendmet0647. [DOI] [PubMed] [Google Scholar]
- 51.Gregg BE, Moore PC, Demozay D, et al. Formation of a human beta-cell population within pancreatic islets is set early in life. J Clin Endocrinol Metab. 2012;97:3197–206. doi: 10.1210/jc.2012-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keenan HA, Sun JK, Levine J, et al. Residual insulin production and pancreatic ß-cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes. 2010;59:2846–53. doi: 10.2337/db10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bingley PJ. Clinical applications of diabetes antibody testing. J Clin Endocrinol Metab. 2010;95:25–33. doi: 10.1210/jc.2009-1365. [DOI] [PubMed] [Google Scholar]
- 54.Roep BO, Peakman M. Diabetogenic T lymphocytes in human type 1 diabetes. Curr Opin Immunol. 2011;23:746–53. doi: 10.1016/j.coi.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 55.Atkinson MA, Bluestone JA, Eisenbarth GS, et al. How does type 1 diabetes develop?: the notion of homicide or beta-cell suicide revisited. Diabetes. 2011;60:1370–79. doi: 10.2337/db10-1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lehuen A, Diana J, Zaccone P, Cooke A. Immune cell crosstalk in type 1 diabetes. Nat Rev Immunol. 2010;10:501–13. doi: 10.1038/nri2787. [DOI] [PubMed] [Google Scholar]
- 57.Campbell-Thompson M, Wasserfall C, Kaddis J, et al. Network for Pancreatic Organ Donors with Diabetes (nPOD): developing a tissue biobank for type 1 diabetes. Diabetes Metab Res Rev. 2012;28:608–17. doi: 10.1002/dmrr.2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gepts W. Pathologic anatomy of the pancreas in juvenile diabetes mellitus. Diabetes. 1965;14:619–33. doi: 10.2337/diab.14.10.619. [DOI] [PubMed] [Google Scholar]
- 59.Foulis AK, Liddle CN, Farquharson MA, Richmond JA, Weir RS. The histopathology of the pancreas in type 1 (insulin-dependent) diabetes mellitus: a 25-year review of deaths in patients under 20 years of age in the United Kingdom. Diabetologia. 1986;29:267–74. doi: 10.1007/BF00452061. [DOI] [PubMed] [Google Scholar]
- 60.Michels AW, Eisenbarth GS. Immune intervention in type 1 diabetes. Semin Immunol. 2011;23:214–19. doi: 10.1016/j.smim.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Foulis AK, Stewart JA. The pancreas in recent-onset type 1 (insulin-dependent) diabetes mellitus: insulin content of islets, insulitis and associated changes in the exocrine acinar tissue. Diabetologia. 1984;26:456–61. doi: 10.1007/BF00262221. [DOI] [PubMed] [Google Scholar]
- 62.Willcox A, Richardson SJ, Bone AJ, Foulis AK, Morgan NG. Analysis of islet inflammation in human type 1 diabetes. Clin Exp Immunol. 2009;155:173–81. doi: 10.1111/j.1365-2249.2008.03860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gaglia JL, Guimaraes AR, Harisinghani M, et al. Noninvasive imaging of pancreatic islet inflammation in type 1A diabetes patients. J Clin Invest. 2011;121:442–45. doi: 10.1172/JCI44339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Campbell-Thompson M, Wasserfall C, Montgomery EL, Atkinson MA, Kaddis JS. Pancreas organ weight in individuals with disease-associated autoantibodies at risk for type 1 diabetes. JAMA. 2012;308:2337–39. doi: 10.1001/jama.2012.15008. [DOI] [PubMed] [Google Scholar]
- 65.Ziegler AG, Nepom GT. Prediction and pathogenesis in type 1 diabetes. Immunity. 2010;32:468–78. doi: 10.1016/j.immuni.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ziegler AG, Bonifacio E. Age-related islet autoantibody incidence in off spring of patients with type 1 diabetes. Diabetologia. 2012;55:1937–43. doi: 10.1007/s00125-012-2472-x. [DOI] [PubMed] [Google Scholar]
- 67.Steck AK, Johnson K, Barriga KJ, et al. Age of islet autoantibody appearance and mean levels of insulin, but not GAD or IA-2 autoantibodies, predict age of diagnosis of type 1 diabetes: diabetes autoimmunity study in the young. Diabetes Care. 2011;34:1397–99. doi: 10.2337/dc10-2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Parikka V, Nanto-Salonen K, Saarinen M, et al. Early seroconversion and rapidly increasing autoantibody concentrations predict prepubertal manifestation of type 1 diabetes in children at genetic risk. Diabetologia. 2012;55:1926–36. doi: 10.1007/s00125-012-2523-3. [DOI] [PubMed] [Google Scholar]
- 69.Kent SC, Chen Y, Bregoli L, et al. Expanded T cells from pancreatic lymph nodes of type 1 diabetic subjects recognize an insulin epitope. Nature. 2005;435:224–28. doi: 10.1038/nature03625. [DOI] [PubMed] [Google Scholar]
- 70.Oresic M, Simell S, Sysi-Aho M, et al. Dysregulation of lipid and amino acid metabolism precedes islet autoimmunity in children who later progress to type 1 diabetes. J Exp Med. 2008;205:2975–84. doi: 10.1084/jem.20081800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pflueger M, Seppanen-Laakso T, Suortti T, et al. Age- and islet autoimmunity-associated differences in amino acid and lipid metabolites in children at risk for type 1 diabetes. Diabetes. 2011;60:2740–47. doi: 10.2337/db10-1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Concannon P, Rich SS, Nepom GT. Genetics of type 1A diabetes. N Engl J Med. 2009;360:1646–54. doi: 10.1056/NEJMra0808284. [DOI] [PubMed] [Google Scholar]
- 73.Noble JA, Valdes AM, Varney MD, et al. HLA class I and genetic susceptibility to type 1 diabetes: results from the type 1 Diabetes Genetics Consortium. Diabetes. 2010;59:2972–79. doi: 10.2337/db10-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Erlich H, Valdes AM, Noble J, et al. HLA DR-DQ haplotypes and genotypes and type 1 diabetes risk: analysis of the type 1 diabetes genetics consortium families. Diabetes. 2008;57:1084–92. doi: 10.2337/db07-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Polychronakos C, Li Q. Understanding type 1 diabetes through genetics: advances and prospects. Nat Rev Genet. 2011;12:781–92. doi: 10.1038/nrg3069. [DOI] [PubMed] [Google Scholar]
- 76.Winkler C, Lauber C, Adler K, et al. An interferon-induced helicase (IFIH1) gene polymorphism associates with different rates of progression from autoimmunity to type 1 diabetes. Diabetes. 2011;60:685–90. doi: 10.2337/db10-1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eisenbarth GS. Type I diabetes mellitus. A chronic autoimmune disease. N Engl J Med. 1986;314:1360–68. doi: 10.1056/NEJM198605223142106. [DOI] [PubMed] [Google Scholar]
- 78.Atkinson MA, Eisenbarth GS. Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet. 2001;358:221–29. doi: 10.1016/S0140-6736(01)05415-0. [DOI] [PubMed] [Google Scholar]
- 79.Bonifacio E, Ziegler AG. Advances in the prediction and natural history of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39:513–25. doi: 10.1016/j.ecl.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 80.Sosenko JM, Palmer JP, Rafkin LE, et al. Trends of earlier and later responses of C-peptide to oral glucose challenges with progression to type 1 diabetes in diabetes prevention trial-type 1 participants. Diabetes Care. 2010;33:620–25. doi: 10.2337/dc09-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sosenko JM, Skyler JS, Krischer JP, et al. Glucose excursions between states of glycemia with progression to type 1 diabetes in the diabetes prevention trial-type 1 (DPT-1) Diabetes. 2010;59:2386–89. doi: 10.2337/db10-0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ferrannini E, Mari A, Nofrate V, Sosenko JM, Skyler JS. Progression to diabetes in relatives of type 1 diabetic patients: mechanisms and mode of onset. Diabetes. 2010;59:679–85. doi: 10.2337/db09-1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Greenbaum CJ, Beam CA, Boulware D, et al. Fall in C-peptide during first 2 years from diagnosis: evidence of at least two distinct phases from composite type 1 diabetes TrialNet data. Diabetes. 2012;61:2066–73. doi: 10.2337/db11-1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Keenan HA, Sun JK, Levine J, et al. Residual insulin production and pancreatic ss-cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes. 2010;59:2846–53. doi: 10.2337/db10-0676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hirsch IB. Clinical review: realistic expectations and practical use of continuous glucose monitoring for the endocrinologist. J Clin Endocrinol Metab. 2009;94:2232–38. doi: 10.1210/jc.2008-2625. [DOI] [PubMed] [Google Scholar]
- 86.Steffes MW, Sibley S, Jackson M, Thomas W. Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Diabetes Care. 2003;26:832–36. doi: 10.2337/diacare.26.3.832. [DOI] [PubMed] [Google Scholar]
- 87.Pickup JC. Insulin-pump therapy for type 1 diabetes mellitus. N Engl J Med. 2012;366:1616–24. doi: 10.1056/NEJMct1113948. [DOI] [PubMed] [Google Scholar]
- 88.Bergenstal RM, Tamborlane WV, Ahmann A, et al. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. 2010;363:311–20. doi: 10.1056/NEJMoa1002853. [DOI] [PubMed] [Google Scholar]
- 89.Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. 2012;157:336–47. doi: 10.7326/0003-4819-157-5-201209040-00508. [DOI] [PubMed] [Google Scholar]
- 90.Pickup JC, Freeman SC, Sutton AJ. Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: meta-analysis of randomised controlled trials using individual patient data. BMJ. 2011;343:3805. doi: 10.1136/bmj.d3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Tamborlane WV, Beck RW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359:1464–76. doi: 10.1056/NEJMoa0805017. [DOI] [PubMed] [Google Scholar]
- 92.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Prolonged nocturnal hypoglycemia is common during 12 months of continuous glucose monitoring in children and adults with type 1 diabetes. Diabetes Care. 2010;33:1004–8. doi: 10.2337/dc09-2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ahmet A, Dagenais S, Barrowman NJ, Collins CJ, Lawson ML. Prevalence of nocturnal hypoglycemia in pediatric type 1 diabetes: a pilot study using continuous glucose monitoring. J Pediatr. 2011;159:297–302. doi: 10.1016/j.jpeds.2011.01.064. [DOI] [PubMed] [Google Scholar]
- 94.STAR 3 Study Group. Sensor-augmented pump therapy for A1C reduction (STAR 3) study: results from the 6-month continuation phase. Diabetes Care. 2011;34:2403–5. doi: 10.2337/dc11-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hirsch IB. Low glucose suspend: ready for prime time? Diabetes Technol Ther. 2012;14:201–2. doi: 10.1089/dia.2012.0036. [DOI] [PubMed] [Google Scholar]
- 96.Cobelli C, Renard E, Kovatchev B. Artificial pancreas: past, present, future. Diabetes. 2011;60:2672–82. doi: 10.2337/db11-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Breton M, Farret A, Bruttomesso D, et al. Fully integrated artificial pancreas in type 1 diabetes: modular closed-loop glucose control maintains near normoglycemia. Diabetes. 2012;61:2230–37. doi: 10.2337/db11-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Garg S, Brazg RL, Bailey TS, et al. Reduction in duration of hypoglycemia by automatic suspension of insulin delivery: the in-clinic ASPIRE study. Diabetes Technol Ther. 2012;14:205–9. doi: 10.1089/dia.2011.0292. [DOI] [PubMed] [Google Scholar]
- 99.Buckingham B, Chase HP, Dassau E, et al. Prevention of nocturnal hypoglycemia using predictive alarm algorithms and insulin pump suspension. Diabetes Care. 2010;33:1013–17. doi: 10.2337/dc09-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Heller S, Buse J, Fisher M, et al. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes (BEGIN Basal-Bolus Type 1): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379:1489–97. doi: 10.1016/S0140-6736(12)60204-9. [DOI] [PubMed] [Google Scholar]
- 101.Kielgast U, Holst JJ, Madsbad S. Antidiabetic actions of endogenous and exogenous GLP-1 in type 1 diabetic patients with and without residual beta-cell function. Diabetes. 2011;60:1599–607. doi: 10.2337/db10-1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ryan G, Briscoe TA, Jobe L. Review of pramlintide as adjunctive therapy in treatment of type 1 and type 2 diabetes. Drug Des Devel Ther. 2009;2:203–14. doi: 10.2147/dddt.s3225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Oral EA. Leptin for type 1 diabetes: coming onto stage to be (or not?) Pediatr Diabetes. 2012;13:68–73. doi: 10.1111/j.1399-5448.2011.00797.x. [DOI] [PubMed] [Google Scholar]
- 104.Dall TM, Mann SE, Zhang Y, et al. Distinguishing the economic costs associated with type 1 and type 2 diabetes. Popul Health Manag. 2009;12:103–10. doi: 10.1089/pop.2009.12203. [DOI] [PubMed] [Google Scholar]
- 105.Tao B, Pietropaolo M, Atkinson M, Schatz D, Taylor D. Estimating the cost of type 1 diabetes in the US: a propensity score matching method. PLoS One. 2010;5:11501. doi: 10.1371/journal.pone.0011501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Melendez-Ramirez LY, Richards RJ, Cefalu WT. Complications of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39:625–40. doi: 10.1016/j.ecl.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 107.Orchard TJ, Costacou T, Kretowski A, Nesto RW. Type 1 diabetes and coronary artery disease. Diabetes Care. 2006;29:2528–38. doi: 10.2337/dc06-1161. [DOI] [PubMed] [Google Scholar]
- 108.Maser RE, Wolfson SK, Jr, Ellis D, et al. Cardiovascular disease and arterial calcification in insulin-dependent diabetes mellitus: interrelations and risk factor profiles. Pittsburgh Epidemiology of Diabetes Complications Study-V. Arterioscler Thromb. 1991;11:958–65. doi: 10.1161/01.atv.11.4.958. [DOI] [PubMed] [Google Scholar]
- 109.Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–53. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Eckel RH, Eisenbarth GS. Autoimmune diabetes inflames the heart. Sci Transl Med. 2012;4:138fs18. doi: 10.1126/scitranslmed.3004219. [DOI] [PubMed] [Google Scholar]
- 111.Gottumukkala RV, Lv H, Cornivelli L, et al. Myocardial infarction triggers chronic cardiac autoimmunity in type 1 diabetes. Sci Transl Med. 2012;4:138ra80. doi: 10.1126/scitranslmed.3003551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Nathan DM, Zinman B, Cleary PA, et al. Modern-day clinical course of type 1 diabetes mellitus after 30 years' duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983-2005) Arch Intern Med. 2009;169:1307–16. doi: 10.1001/archinternmed.2009.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Waden J, Forsblom C, Thorn LM, Gordin D, Saraheimo M, Groop PH. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes. 2009;58:2649–55. doi: 10.2337/db09-0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.de Boer IH, Rue TC, Cleary PA, et al. Long-term renal outcomes of patients with type 1 diabetes mellitus and microalbuminuria: an analysis of the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications cohort. Arch Intern Med. 2011;171:412–20. doi: 10.1001/archinternmed.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Groop PH, Thomas MC, Moran JL, et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes. 2009;58:1651–58. doi: 10.2337/db08-1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pezzolesi MG, Poznik GD, Mychaleckyj JC, et al. Genome-wide association scan for diabetic nephropathy susceptibility genes in type 1 diabetes. Diabetes. 2009;58:1403–10. doi: 10.2337/db08-1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mollsten A, Svensson M, Waernbaum I, et al. Cumulative risk, age at onset, and sex-specific differences for developing end-stage renal disease in young patients with type 1 diabetes: a nationwide population-based cohort study. Diabetes. 2010;59:1803–8. doi: 10.2337/db09-1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pop-Busui R, Low PA, Waberski BH, et al. Effects of prior intensive insulin therapy on cardiac autonomic nervous system function in type 1 diabetes mellitus: the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study (DCCT/EDIC) Circulation. 2009;119:2886–93. doi: 10.1161/CIRCULATIONAHA.108.837369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wiggin TD, Sullivan KA, Pop-Busui R, Amato A, Sima AA, Feldman EL. Elevated triglycerides correlate with progression of diabetic neuropathy. Diabetes. 2009;58:1634–40. doi: 10.2337/db08-1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.White NH, Sun W, Cleary PA, et al. Prolonged effect of intensive therapy on the risk of retinopathy complications in patients with type 1 diabetes mellitus: 10 years after the Diabetes Control and Complications Trial. Arch Ophthalmol. 2008;126:1707–15. doi: 10.1001/archopht.126.12.1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chaturvedi N, Porta M, Klein R, et al. Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet. 2008;372:1394–402. doi: 10.1016/S0140-6736(08)61412-9. [DOI] [PubMed] [Google Scholar]
- 122.Gale EA. Dying of diabetes. Lancet. 2006;368:1626–28. doi: 10.1016/S0140-6736(06)69672-4. [DOI] [PubMed] [Google Scholar]
- 123.Beran D, Yudkin JS, de Courten M. Access to care for patients with insulin-requiring diabetes in developing countries: case studies of Mozambique and Zambia. Diabetes Care. 2005;28:2136–40. doi: 10.2337/diacare.28.9.2136. [DOI] [PubMed] [Google Scholar]
- 124.Beran D, Basey M, Wirtz V, Kaplan W, Atkinson M, Yudkin JS. On the road to the insulin centenary. Lancet. 2012;380:1648. doi: 10.1016/S0140-6736(12)61950-3. [DOI] [PubMed] [Google Scholar]
- 125.Bach JF, Chatenoud L. A historical view from thirty eventful years of immunotherapy in autoimmune diabetes. Semin Immunol. 2011;23:174–81. doi: 10.1016/j.smim.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 126.van Belle TL, Coppieters KT, von Herrath MG. Type 1 diabetes: etiology, immunology, and therapeutic strategies. Physiol Rev. 2011;91:79–118. doi: 10.1152/physrev.00003.2010. [DOI] [PubMed] [Google Scholar]
- 127.Atkinson MA. Evaluating preclinical efficacy. Sci Transl Med. 2011;3:96cm22. doi: 10.1126/scitranslmed.3002757. [DOI] [PubMed] [Google Scholar]
- 128.Knip M, Virtanen SM, Seppä K, et al. Finnish TRIGR Study Group. Dietary intervention in infancy and later signs of beta-cell autoimmunity. N Engl J Med. 2010;363:1900–8. doi: 10.1056/NEJMoa1004809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Vaarala O, Ilonen J, Ruohtula T, et al. Removal of bovine insulin from cow's milk formula and early initiation of beta-cell autoimmunity in the FINDIA pilot study. Arch Pediatr Adolesc Med. 2012;166:608–14. doi: 10.1001/archpediatrics.2011.1559. [DOI] [PubMed] [Google Scholar]
- 130.Skyler JS, Type 1 Diabetes TrialNet Study Group Update on worldwide efforts to prevent type 1 diabetes. Ann NY Acad Sci. 2008;1150:190–96. doi: 10.1196/annals.1447.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Skyler JS, Krischer JP, Wolfsdorf J, et al. Effects of oral insulin in relatives of patients with type 1 diabetes: the Diabetes Prevention Trial—Type 1. Diabetes Care. 2005;28:1068–76. doi: 10.2337/diacare.28.5.1068. [DOI] [PubMed] [Google Scholar]
- 132.Gale EA, Bingley PJ, Emmett CL, et al. European Nicotinamide Diabetes Intervention Trial (ENDIT): a randomised controlled trial of intervention before the onset of type 1 diabetes. Lancet. 2004;363:925–31. doi: 10.1016/S0140-6736(04)15786-3. [DOI] [PubMed] [Google Scholar]
- 133.Näntö-Salonen K, Kupila A, Simell S, et al. Nasal insulin to prevent type 1 diabetes in children with HLA genotypes and autoantibodies conferring increased risk of disease: a double-blind, randomised controlled trial. Lancet. 2008;372:1746–55. doi: 10.1016/S0140-6736(08)61309-4. [DOI] [PubMed] [Google Scholar]
- 134.Greenbaum C, Atkinson MA. Persistence is the twin sister of excellence: an important lesson for attempts to prevent and reverse type 1 diabetes. Diabetes. 2011;60:693–94. doi: 10.2337/db10-1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Walter M, Philotheou A, Bonnici F, Ziegler AG, Jimenez R. No effect of the altered peptide ligand NBI-6024 on beta-cell residual function and insulin needs in new-onset type 1 diabetes. Diabetes Care. 2009;32:2036–40. doi: 10.2337/dc09-0449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Pescovitz MD, Greenbaum CJ, Krause-Steinrauf H, et al. Rituximab, B-lymphocyte depletion, and preservation of beta-cell function. N Engl J Med. 2009;361:2143–52. doi: 10.1056/NEJMoa0904452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sherry N, Hagopian W, Ludvigsson J, et al. Teplizumab for treatment of type 1 diabetes (Protege study): 1-year results from a randomised, placebo-controlled trial. Lancet. 2011;378:487–97. doi: 10.1016/S0140-6736(11)60931-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Orban T, Bundy B, Becker DJ, et al. Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet. 2011;378:412–19. doi: 10.1016/S0140-6736(11)60886-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bach JF. Anti-CD3 antibodies for type 1 diabetes: beyond expectations. Lancet. 2011;378:459–60. doi: 10.1016/S0140-6736(11)60980-X. [DOI] [PubMed] [Google Scholar]
- 140.Ludvigsson J, Krisky D, Casas R, et al. GAD65 antigen therapy in recently diagnosed type 1 diabetes mellitus. N Engl J Med. 2012;366:433–42. doi: 10.1056/NEJMoa1107096. [DOI] [PubMed] [Google Scholar]
- 141.Wherrett DK, Bundy B, Becker DJ, et al. Antigen-based therapy with glutamic acid decarboxylase (GAD) vaccine in patients with recent-onset type 1 diabetes: a randomised double-blind trial. Lancet. 2011;378:319–27. doi: 10.1016/S0140-6736(11)60895-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Buzzetti R, Cernea S, Petrone A, et al. C-peptide response and HLA genotypes in subjects with recent-onset type 1 diabetes after immunotherapy with DiaPep277: an exploratory study. Diabetes. 2011;60:3067–72. doi: 10.2337/db10-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schloot NC, Meierhoff G, Lengyel C, et al. Effect of heat shock protein peptide DiaPep277 on beta-cell function in paediatric and adult patients with recent-onset diabetes mellitus type 1: two prospective, randomized, double-blind phase II trials. Diabetes Metab Res Rev. 2007;23:276–85. doi: 10.1002/dmrr.707. [DOI] [PubMed] [Google Scholar]
- 144.Voltarelli JC, Couri CE, Stracieri AB, et al. Autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. JAMA. 2007;297:1568–76. doi: 10.1001/jama.297.14.1568. [DOI] [PubMed] [Google Scholar]
- 145.Couri CE, Oliveira MC, Stracieri AB, et al. C-peptide levels and insulin independence following autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. JAMA. 2009;301:1573–79. doi: 10.1001/jama.2009.470. [DOI] [PubMed] [Google Scholar]
- 146.Herold KC, Bluestone JA. Type 1 diabetes immunotherapy: is the glass half empty or half full? Sci Transl Med. 2011;3:95fs1. doi: 10.1126/scitranslmed.3002981. [DOI] [PubMed] [Google Scholar]
- 147.Pozzilli P. Type 1 diabetes mellitus in 2011: heterogeneity of T1DM raises questions for therapy. Nat Rev Endocrinol. 2012;8:78–80. doi: 10.1038/nrendo.2011.228. [DOI] [PubMed] [Google Scholar]
- 148.Moran A, Bundy B, Becker DJ, et al. Interleukin-1 antagonism in type 1 diabetes of recent onset: two multicentre, randomised, double-blind, placebo-controlled trials. Lancet. 2013;381:1905–15. doi: 10.1016/S0140-6736(13)60023-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Shapiro AM, Lakey JR, Ryan EA, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000;343:230–38. doi: 10.1056/NEJM200007273430401. [DOI] [PubMed] [Google Scholar]
- 150.Ryan EA, Paty BW, Senior PA, et al. Five-year follow-up after clinical islet transplantation. Diabetes. 2005;54:2060–69. doi: 10.2337/diabetes.54.7.2060. [DOI] [PubMed] [Google Scholar]
- 151.Gibly RF, Graham JG, Luo X, Lowe WL, Jr, Hering BJ, Shea LD. Advancing islet transplantation: from engraftment to the immune response. Diabetologia. 2011;54:2494–505. doi: 10.1007/s00125-011-2243-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Staeva TP, Chatenoud L, Insel R, Atkinson MA. Recent lessons learned from prevention and recent-onset type 1 diabetes immunotherapy trials. Diabetes. 2013;62:9–17. doi: 10.2337/db12-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Vendrame F, Pileggi A, Laughlin E, et al. Recurrence of type 1 diabetes after simultaneous pancreas-kidney transplantation, despite immunosuppression, is associated with autoantibodies and pathogenic autoreactive CD4 T-cells. Diabetes. 2010;59:947–57. doi: 10.2337/db09-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Winkler C, Krumsiek J, Lempainen J, et al. A strategy for combining minor genetic susceptibility genes to improve prediction of disease in type 1 diabetes. Genes Immun. 2012;13:549–55. doi: 10.1038/gene.2012.36. [DOI] [PubMed] [Google Scholar]
- 155.Sosenko JM, Skyler JS, Mahon J, et al. The application of the diabetes prevention trial-type 1 risk score for identifying a preclinical state of type 1 diabetes. Diabetes Care. 2012;35:1552–55. doi: 10.2337/dc12-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Atkinson MA. It's time to consider changing the rules: the rationale for rethinking control groups in clinical trials aimed at reversing type 1 diabetes. Diabetes. 2011;60:361–63. doi: 10.2337/db10-1506. [DOI] [PMC free article] [PubMed] [Google Scholar]