Long COVID: major findings, mechanisms and recommendations (original) (raw)
Introduction
Long COVID (sometimes referred to as ‘post-acute sequelae of COVID-19’) is a multisystemic condition comprising often severe symptoms that follow a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. At least 65 million individuals around the world have long COVID, based on a conservative estimated incidence of 10% of infected people and more than 651 million documented COVID-19 cases worldwide1; the number is likely much higher due to many undocumented cases. The incidence is estimated at 10–30% of non-hospitalized cases, 50–70% of hospitalized cases2,3 and 10–12% of vaccinated cases[4](/articles/s41579-022-00846-2#ref-CR4 "Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. https://doi.org/10.1038/s41591-022-01840-0
(2022)."),[5](/articles/s41579-022-00846-2#ref-CR5 "Ayoubkhani, D. et al. Risk of Long Covid in people infected with SARS-CoV-2 after two doses of a COVID-19 vaccine: community-based, matched cohort study. Preprint at medRxiv
https://doi.org/10.1101/2022.02.23.22271388
(2022)."). Long COVID is associated with all ages and acute phase disease severities, with the highest percentage of diagnoses between the ages of 36 and 50 years, and most long COVID cases are in non-hospitalized patients with a mild acute illness[6](/articles/s41579-022-00846-2#ref-CR6 "FAIR Health. Patients Diagnosed with Post-COVID Conditions: An Analysis of Private Healthcare Claims Using the Official ICD-10 Diagnostic Code (FAIR Health, 2022)."), as this population represents the majority of overall COVID-19 cases. There are many research challenges, as outlined in this Review, and many open questions, particularly relating to pathophysiology, effective treatments and risk factors.Hundreds of biomedical findings have been documented, with many patients experiencing dozens of symptoms across multiple organ systems7 (Fig. 1). Long COVID encompasses multiple adverse outcomes, with common new-onset conditions including cardiovascular, thrombotic and cerebrovascular disease8, type 2 diabetes9, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)10,11 and dysautonomia, especially postural orthostatic tachycardia syndrome (POTS)12 (Fig. 2). Symptoms can last for years[13](/articles/s41579-022-00846-2#ref-CR13 "Demko, Z. O. et al. Post-acute sequelae of SARS-CoV-2 (PASC) impact quality of life at 6, 12 and 18 months post-infection. Preprint at medRxiv https://doi.org/10.1101/2022.08.08.22278543
(2022)."), and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong[14](/articles/s41579-022-00846-2#ref-CR14 "Cairns, R. & Hotopf, M. A systematic review describing the prognosis of chronic fatigue syndrome. Occup. Med. Oxf. Engl. 55, 20–31 (2005)."). With significant proportions of individuals with long COVID unable to return to work[7](/articles/s41579-022-00846-2#ref-CR7 "Davis, H. E. et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 38, 101019 (2021)."), the scale of newly disabled individuals is contributing to labour shortages[15](/articles/s41579-022-00846-2#ref-CR15 "Bach, K. Is ‘long Covid’ worsening the labor shortage? Brookings
https://www.brookings.edu/research/is-long-covid-worsening-the-labor-shortage/
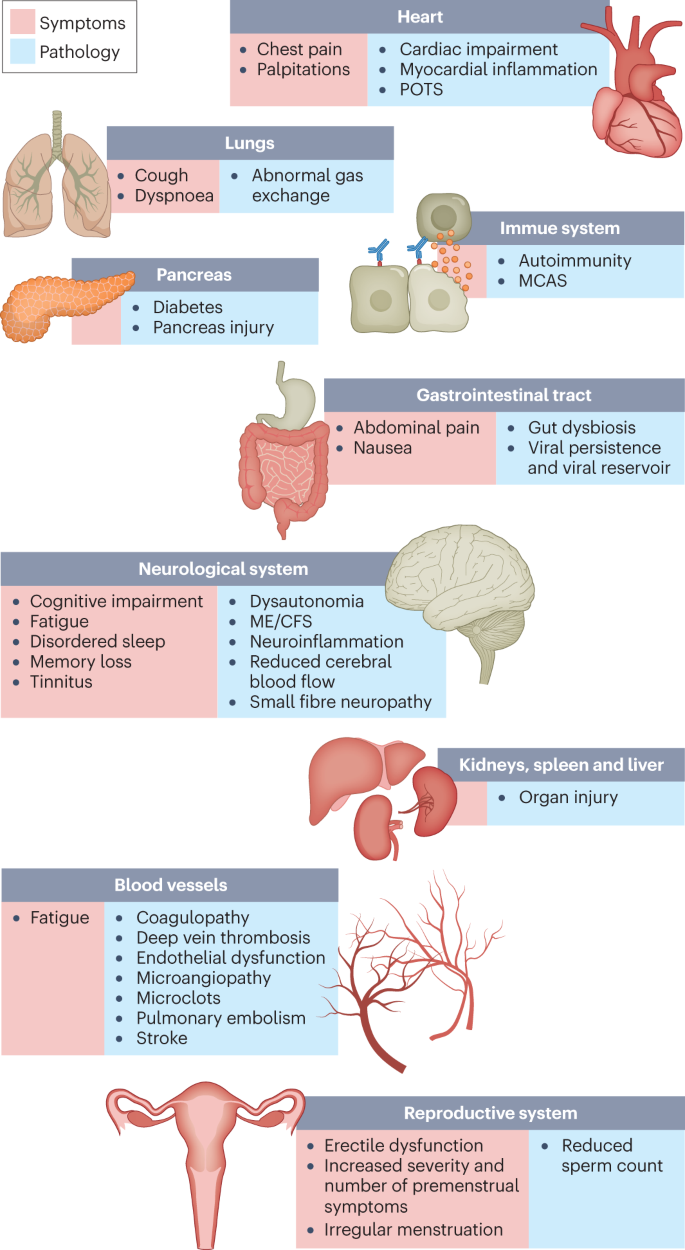
(2022)."). There are currently no validated effective treatments.Fig. 1: Long COVID symptoms and the impacts on numerous organs with differing pathology.
The impacts of long COVID on numerous organs with a wide variety of pathology are shown. The presentation of pathologies is often overlapping, which can exacerbate management challenges. MCAS, mast cell activation syndrome; ME/CFS, myalgic encephalomyelitis/chronic fatigue syndrome; POTS, postural orthostatic tachycardia syndrome.
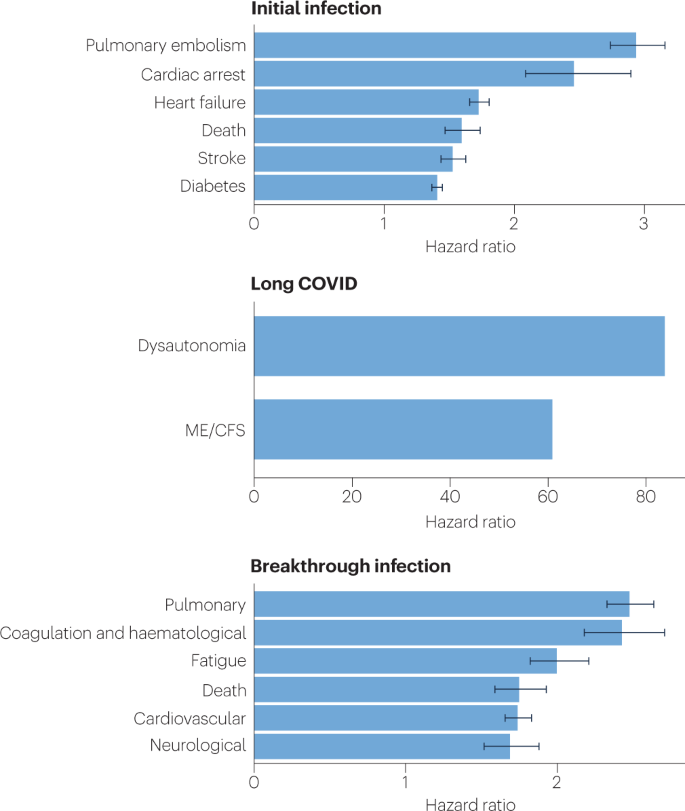
Fig. 2: SARS-CoV-2 infection, COVID-19 and long COVID increases the risk of several medical conditions.
Because diagnosis-specific data on large populations with long COVID are sparse, outcomes from general infections are included and a large proportion of medical conditions are expected to result from long COVID, although the precise proportion cannot be determined. One year after the initial infection, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections increased the risk of cardiac arrest, death, diabetes, heart failure, pulmonary embolism and stroke, as studied with use of US Department of Veterans Affairs databases. Additionally, there is clear increased risk of developing myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia. Six months after breakthrough infection, increased risks were observed for cardiovascular conditions, coagulation and haematological conditions, death, fatigue, neurological conditions and pulmonary conditions in the same cohort. The hazard ratio is the ratio of how often an event occurs in one group relative to another; in this case people who have had COVID-19 compared with those who have not. Data sources are as follows: diabetes9, cardiovascular outcomes8, dysautonomia12,[201](/articles/s41579-022-00846-2#ref-CR201 "Dysautonomia International. What is dysautonomia? Dysautonomia International http://www.dysautonomiainternational.org/page.php?ID=34
(2022)."), ME/CFS[10](/articles/s41579-022-00846-2#ref-CR10 "Mancini, D. M. et al. Use of cardiopulmonary stress testing for patients with unexplained dyspnea post–coronavirus disease. JACC Heart Fail. 9, 927–937 (2021)."),[202](/articles/s41579-022-00846-2#ref-CR202 "CDC. Epidemiology | Presentation and clinical course | Healthcare providers | Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). CDC
https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/epidemiology.html
(2021).") and breakthrough infections[4](/articles/s41579-022-00846-2#ref-CR4 "Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med.
https://doi.org/10.1038/s41591-022-01840-0
(2022).").There are likely multiple, potentially overlapping, causes of long COVID. Several hypotheses for its pathogenesis have been suggested, including persisting reservoirs of SARS-CoV-2 in tissues[16](/articles/s41579-022-00846-2#ref-CR16 "Swank, Z. et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciac722
(2022)."),[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."); immune dysregulation[17](#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[18](#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv
https://doi.org/10.1101/2022.08.09.22278592
(2022)."),[19](#ref-CR19 "Glynne, P., Tahmasebi, N., Gant, V. & Gupta, R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J. Investig. Med. 70, 61–67 (2022)."),[20](/articles/s41579-022-00846-2#ref-CR20 "Phetsouphanh, C. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 23, 210–216 (2022).") with or without reactivation of underlying pathogens, including herpesviruses such as Epstein–Barr virus (EBV) and human herpesvirus 6 (HHV-6) among others[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv
https://doi.org/10.1101/2022.08.09.22278592
(2022)."),[21](/articles/s41579-022-00846-2#ref-CR21 "Zubchenko, S., Kril, I., Nadizhko, O., Matsyura, O. & Chopyak, V. Herpesvirus infections and post-COVID-19 manifestations: a pilot observational study. Rheumatol. Int.
https://doi.org/10.1007/s00296-022-05146-9
(2022)."),[22](/articles/s41579-022-00846-2#ref-CR22 "Peluso, M. J. et al. Evidence of recent Epstein-Barr virus reactivation in individuals experiencing Long COVID. Preprint at medRxiv
https://doi.org/10.1101/2022.06.21.22276660
(2022)."); impacts of SARS-CoV-2 on the microbiota, including the virome[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[23](#ref-CR23 "Yeoh, Y. K. et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 70, 698–706 (2021)."),[24](#ref-CR24 "Liu, Q. et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut 71, 544–552 (2022)."),[25](/articles/s41579-022-00846-2#ref-CR25 "Mendes de Almeida, V. Gut microbiota from patients with mild COVID-19 cause alterations in mice that resemble post-COVID syndrome. Res. Sq.
https://doi.org/10.21203/rs.3.rs-1756189/v1
(2022)."); autoimmunity[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[26](#ref-CR26 "Wallukat, G. et al. Functional autoantibodies against G-protein coupled receptors in patients with persistent long-COVID-19 symptoms. J. Transl Autoimmun. 4, 100100 (2021)."),[27](#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022)."),[28](/articles/s41579-022-00846-2#ref-CR28 "Arthur, J. M. et al. Development of ACE2 autoantibodies after SARS-CoV-2 infection. PLoS ONE 16, e0257016 (2021).") and priming of the immune system from molecular mimicry[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."); microvascular blood clotting with endothelial dysfunction[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[29](#ref-CR29 "Haffke, M. et al. Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS). J. Transl Med. 20, 138 (2022)."),[30](#ref-CR30 "Charfeddine, S. Long COVID 19 syndrome: is it related to microcirculation and endothelial dysfunction? Insights from TUN-EndCOV study. Front. Cardiovasc. Med.
https://doi.org/10.3389/fcvm.2021.745758
(2021)."),[31](/articles/s41579-022-00846-2#ref-CR31 "Pretorius, E. et al. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/post-acute sequelae of COVID-19 (PASC). Cardiovasc. Diabetol. 21, 148 (2022)."); and dysfunctional signalling in the brainstem and/or vagus nerve[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[32](/articles/s41579-022-00846-2#ref-CR32 "Spudich, S. & Nath, A. Nervous system consequences of COVID-19. Science 375, 267–269 (2022).") (Fig. [3](/articles/s41579-022-00846-2#Fig3)). Mechanistic studies are generally at an early stage, and although work that builds on existing research from postviral illnesses such as ME/CFS has advanced some theories, many questions remain and are a priority to address. Risk factors potentially include female sex, type 2 diabetes, EBV reactivation, the presence of specific autoantibodies[27](/articles/s41579-022-00846-2#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022)."), connective tissue disorders[33](/articles/s41579-022-00846-2#ref-CR33 "Renz-Polster, H., Tremblay, M.-E., Bienzle, D. & Fischer, J. E. The pathobiology of myalgic encephalomyelitis/chronic fatigue syndrome: the case for neuroglial failure. Front. Cell. Neurosci. 16, 888232 (2022)."), attention deficit hyperactivity disorder, chronic urticaria and allergic rhinitis[34](/articles/s41579-022-00846-2#ref-CR34 "Merzon, E. et al. Clinical and socio-demographic variables associated with the diagnosis of long COVID syndrome in youth: a population-based study. Int. J. Environ. Res. Public Health 19, 5993 (2022)."), although a third of people with long COVID have no identified pre-existing conditions[6](/articles/s41579-022-00846-2#ref-CR6 "FAIR Health. Patients Diagnosed with Post-COVID Conditions: An Analysis of Private Healthcare Claims Using the Official ICD-10 Diagnostic Code (FAIR Health, 2022)."). A higher prevalence of long Covid has been reported in certain ethnicities, including people with Hispanic or Latino heritage[35](/articles/s41579-022-00846-2#ref-CR35 "CDC. Long COVID - household pulse survey - COVID-19. CDC
https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm
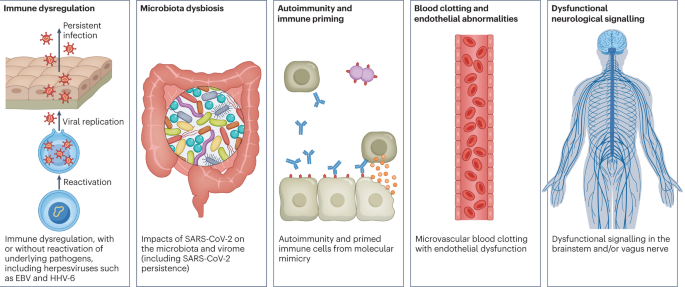
(2022)."). Socio-economic risk factors include lower income and an inability to adequately rest in the early weeks after developing COVID-19 (refs. [36](/articles/s41579-022-00846-2#ref-CR36 "Williamson, A. E., Tydeman, F., Miners, A., Pyper, K. & Martineau, A. R. Short-term and long-term impacts of COVID-19 on economic vulnerability: a population-based longitudinal study (COVIDENCE UK). BMJ Open 12, e065083 (2022)."),[37](/articles/s41579-022-00846-2#ref-CR37 "Ziauddeen, N. et al. Characteristics and impact of Long Covid: findings from an online survey. PLoS ONE 17, e0264331 (2022).")). Before the emergence of SARS-CoV-2, multiple viral and bacterial infections were known to cause postinfectious illnesses such as ME/CFS[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[38](/articles/s41579-022-00846-2#ref-CR38 "Choutka, J., Jansari, V., Hornig, M. & Iwasaki, A. Unexplained post-acute infection syndromes. Nat. Med. 28, 911–923 (2022)."), and there are indications that long COVID shares their mechanistic and phenotypic characteristics[17](/articles/s41579-022-00846-2#ref-CR17 "Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021)."),[39](/articles/s41579-022-00846-2#ref-CR39 "Komaroff, A. L. & Lipkin, W. I. Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends Mol. Med. 27, 895–906 (2021)."). Further, dysautonomia has been observed in other postviral illnesses and is frequently observed in long COVID[7](/articles/s41579-022-00846-2#ref-CR7 "Davis, H. E. et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 38, 101019 (2021).").Fig. 3: Hypothesized mechanisms of long COVID pathogenesis.
There are several hypothesized mechanisms for long COVID pathogenesis, including immune dysregulation, microbiota disruption, autoimmunity, clotting and endothelial abnormality, and dysfunctional neurological signalling. EBV, Epstein–Barr virus; HHV-6, human herpesvirus 6; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
In this Review, we explore the current knowledge base of long COVID as well as misconceptions surrounding long COVID and areas where additional research is needed. Because most patients with long COVID were not hospitalized for their initial SARS-CoV-2 infection6, we focus on research that includes patients with mild acute COVID-19 (meaning not hospitalized and without evidence of respiratory disease). Most of the studies we discuss refer to adults, except for those in Box 1.
Major findings
Immunology and virology
Studies looking at immune dysregulation in individuals with long COVID who had mild acute COVID-19 have found T cell alterations, including exhausted T cells[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv https://doi.org/10.1101/2022.08.09.22278592
(2022)."), reduced CD4+ and CD8+ effector memory cell numbers[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv
https://doi.org/10.1101/2022.08.09.22278592
(2022)."),[19](/articles/s41579-022-00846-2#ref-CR19 "Glynne, P., Tahmasebi, N., Gant, V. & Gupta, R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J. Investig. Med. 70, 61–67 (2022).") and elevated PD1 expression on central memory cells, persisting for at least 13 months[19](/articles/s41579-022-00846-2#ref-CR19 "Glynne, P., Tahmasebi, N., Gant, V. & Gupta, R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J. Investig. Med. 70, 61–67 (2022)."). Studies have also reported highly activated innate immune cells, a lack of naive T and B cells and elevated expression of type I and type III interferons (interferon-β (IFNβ) and IFNλ1), persisting for at least 8 months[20](/articles/s41579-022-00846-2#ref-CR20 "Phetsouphanh, C. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 23, 210–216 (2022)."). A comprehensive study comparing patients with long COVID with uninfected individuals and infected individuals without long COVID found increases in the numbers of non-classical monocytes, activated B cells, double-negative B cells, and IL-4- and IL-6-secreting CD4+ T cells and decreases in the numbers of conventional dendritic cells and exhausted T cells and low cortisol levels in individuals with long COVID at a median of 14 months after infection[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv
https://doi.org/10.1101/2022.08.09.22278592
(2022)."). The expansion of cytotoxic T cells has been found to be associated with the gastrointestinal presentation of long COVID[27](/articles/s41579-022-00846-2#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022)."). Additional studies have found elevated levels of cytokines, particularly IL-1β, IL-6, TNF and IP10 (refs. [40](/articles/s41579-022-00846-2#ref-CR40 "Schultheiß, C. et al. From online data collection to identification of disease mechanisms: the IL-1ß, IL-6 and TNF-α cytokine triad is associated with post-acute sequelae of COVID-19 in a digital research cohort. SSRN
https://doi.org/10.2139/ssrn.3963839
(2021)."),[41](/articles/s41579-022-00846-2#ref-CR41 "Peluso, M. J. et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J. Infect. Dis. 224, 1839–1848 (2021).")), and a recent preprint has reported persistent elevation of the level of CCL11, which is associated with cognitive dysfunction[42](/articles/s41579-022-00846-2#ref-CR42 "Fernández-Castañeda, A. et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Preprint at bioRxiv
https://doi.org/10.1101/2022.01.07.475453
(2022)."). It remains to be seen whether the pattern of cytokines in ME/CFS, where the levels of certain cytokines are elevated in the first 2–3 years of illness but decrease over time without a corresponding decrease in symptoms[43](/articles/s41579-022-00846-2#ref-CR43 "Hornig, M. et al. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci. Adv. 1, e1400121 (2015)."), is similar in long COVID.Multiple studies have found elevated levels of autoantibodies in long COVID27, including autoantibodies to ACE2 (ref. 28) (the receptor for SARS-CoV-2 entry), β2-adrenoceptor, muscarinic M2 receptor, angiotensin II AT1 receptor and the angiotensin 1–7 MAS receptor26. High levels of other autoantibodies have been found in some patients with COVID-19 more generally, including autoantibodies that target the tissue (such as connective tissue, extracellular matrix components, vascular endothelium, coagulation factors and platelets), organ systems (including the lung, central nervous system, skin and gastrointestinal tract), immunomodulatory proteins (cytokines, chemokines, complement components and cell-surface proteins)44. A major comprehensive study, however, did not find autoantibodies to be a major component of long COVID[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv https://doi.org/10.1101/2022.08.09.22278592
(2022).").Reactivated viruses, including EBV and HHV-6, have been found in patients with long COVID[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv https://doi.org/10.1101/2022.08.09.22278592
(2022)."),[21](/articles/s41579-022-00846-2#ref-CR21 "Zubchenko, S., Kril, I., Nadizhko, O., Matsyura, O. & Chopyak, V. Herpesvirus infections and post-COVID-19 manifestations: a pilot observational study. Rheumatol. Int.
https://doi.org/10.1007/s00296-022-05146-9
(2022)."),[22](/articles/s41579-022-00846-2#ref-CR22 "Peluso, M. J. et al. Evidence of recent Epstein-Barr virus reactivation in individuals experiencing Long COVID. Preprint at medRxiv
https://doi.org/10.1101/2022.06.21.22276660
(2022)."),[27](/articles/s41579-022-00846-2#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022).") (and have been identified in ME/CFS[45](/articles/s41579-022-00846-2#ref-CR45 "Shikova, E. et al. Cytomegalovirus, Epstein-Barr virus, and human herpesvirus-6 infections in patients with myalgic еncephalomyelitis/chronic fatigue syndrome. J. Med. Virol. 92, 3682–3688 (2020).")), and lead to mitochondrial fragmentation and severely affect energy metabolism[46](/articles/s41579-022-00846-2#ref-CR46 "Schreiner, P. et al. Human herpesvirus-6 reactivation, mitochondrial fragmentation, and the coordination of antiviral and metabolic phenotypes in myalgic encephalomyelitis/chronic fatigue syndrome. Immunohorizons 4, 201–215 (2020)."). A recent preprint has reported that EBV reactivation is associated with fatigue and neurocognitive dysfunction in patients with long COVID[22](/articles/s41579-022-00846-2#ref-CR22 "Peluso, M. J. et al. Evidence of recent Epstein-Barr virus reactivation in individuals experiencing Long COVID. Preprint at medRxiv
https://doi.org/10.1101/2022.06.21.22276660
(2022).").Several studies have shown low or no SARS-CoV-2 antibody production and other insufficient immune responses in the acute stage of COVID-19 to be predictive of long COVID at 6–7 months, in both hospitalized patients and non-hospitalized patients47,48. These insufficient immune responses include a low baseline level of IgG48, low levels of receptor-binding domain and spike-specific memory B cells, low levels of nucleocapsid IgG[49](/articles/s41579-022-00846-2#ref-CR49 "Talla, A. et al. Longitudinal immune dynamics of mild COVID-19 define signatures of recovery and persistence. Preprint at bioRxiv https://doi.org/10.1101/2021.05.26.442666
(2021).") and low peaks of spike-specific IgG[47](/articles/s41579-022-00846-2#ref-CR47 "García-Abellán, J. et al. Antibody response to SARS-CoV-2 is associated with long-term clinical outcome in patients with COVID-19: a longitudinal study. J. Clin. Immunol. 41, 1490–1501 (2021)."). In a recent preprint, low or absent CD4+ T cell and CD8+ T cell responses were noted in patients with severe long COVID[49](/articles/s41579-022-00846-2#ref-CR49 "Talla, A. et al. Longitudinal immune dynamics of mild COVID-19 define signatures of recovery and persistence. Preprint at bioRxiv
https://doi.org/10.1101/2021.05.26.442666
(2021)."), and a separate study found lower levels of CD8+ T cells expressing CD107a and a decline in nucleocapsid-specific interferon-γ-producing CD8+ T cells in patients with long COVID compared with infected controls without long COVID[50](/articles/s41579-022-00846-2#ref-CR50 "Peluso, M. J. et al. Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms. Cell Rep. 36, 109518 (2021)."). High levels of autoantibodies in long COVID have been found to be inversely correlated with protective COVID-19 antibodies, suggesting that patients with high autoantibody levels may be more likely to have breakthrough infections[27](/articles/s41579-022-00846-2#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022)."). SARS-CoV-2 viral rebound in the gut, possibly resulting from viral persistence, has also been associated with lower levels and slower production of receptor-binding domain IgA and IgG antibodies[51](/articles/s41579-022-00846-2#ref-CR51 "Hu, F. et al. A compromised specific humoral immune response against the SARS-CoV-2 receptor-binding domain is related to viral persistence and periodic shedding in the gastrointestinal tract. Cell. Mol. Immunol. 17, 1119–1125 (2020)."). There are major differences in antibody creation, seroreversion and antibody titre levels across the sexes, with women being less likely to seroconvert, being more likely to serorevert and having lower antibody levels overall[52](/articles/s41579-022-00846-2#ref-CR52 "Korte, W. et al. SARS-CoV-2 IgG and IgA antibody response is gender dependent; and IgG antibodies rapidly decline early on. J. Infect. 82, e11–e14 (2021)."),[53](/articles/s41579-022-00846-2#ref-CR53 "Jo, W. et al. A two-phase, single cohort study of COVID-19 antibody sera-surveillance. Ann. Epidemiol. Public Health 4, 1055 (2021)."), even affecting antibody waning after vaccination[54](/articles/s41579-022-00846-2#ref-CR54 "Nomura, Y. et al. Attenuation of antibody titers from 3 to 6 months after the second dose of the BNT162b2 vaccine depends on sex, with age and smoking risk factors for lower antibody titers at 6 months. Vaccines 9, 1500 (2021).").Several reports have pointed towards possible viral persistence as a driver of long COVID symptoms; viral proteins and/or RNA has been found in the reproductive system, cardiovascular system, brain, muscles, eyes, lymph nodes, appendix, breast tissue, hepatic tissue, lung tissue, plasma, stool and urine55,[56](#ref-CR56 "Goh, D. et al. Persistence of residual SARS-CoV-2 viral antigen and RNA in tissues of patients with long COVID-19. Preprint at https://www.researchsquare.com/article/rs-1379777/v1
(2022)."),[57](#ref-CR57 "Ceulemans, L. J. et al. Persistence of SARS-CoV-2 RNA in lung tissue after mild COVID-19. Lancet Respir. Med. 9, e78–e79 (2021)."),[58](#ref-CR58 "Gaebler, C. et al. Evolution of antibody immunity to SARS-CoV-2. Nature 591, 639–644 (2021)."),[59](#ref-CR59 "Menuchin-Lasowski, Y. et al. SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids. Stem Cell Rep 17, 789–803 (2022)."),[60](/articles/s41579-022-00846-2#ref-CR60 "Cheung, C. C. L. et al. Residual SARS-CoV-2 viral antigens detected in GI and hepatic tissues from five recovered patients with COVID-19. Gut 71, 226–229 (2022)."). In one study, circulating SARS-CoV-2 spike antigen was found in 60% of a cohort of 37 patients with long COVID up to 12 months after diagnosis compared with 0% of 26 SARS-CoV-2-infected individuals, likely implying a reservoir of active virus or components of the virus[16](/articles/s41579-022-00846-2#ref-CR16 "Swank, Z. et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin. Infect. Dis.
https://doi.org/10.1093/cid/ciac722
(2022)."). Indeed, multiple reports following gastrointestinal biopsies have indicated the presence of virus, suggestive of a persistent reservoir in some patients[58](/articles/s41579-022-00846-2#ref-CR58 "Gaebler, C. et al. Evolution of antibody immunity to SARS-CoV-2. Nature 591, 639–644 (2021)."),[61](/articles/s41579-022-00846-2#ref-CR61 "Natarajan, A. et al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med 3, 371–387.e9 (2022).").Vascular issues and organ damage
Although COVID-19 was initially recognized as a respiratory illness, SARS-CoV-2 has capability to damage many organ systems. The damage that has been demonstrated across diverse tissues has predominantly been attributed to immune-mediated response and inflammation, rather than direct infection of cells by the virus. Circulatory system disruption includes endothelial dysfunction and subsequent downstream effects, and increased risks of deep vein thrombosis, pulmonary embolism and bleeding events29,[30](/articles/s41579-022-00846-2#ref-CR30 "Charfeddine, S. Long COVID 19 syndrome: is it related to microcirculation and endothelial dysfunction? Insights from TUN-EndCOV study. Front. Cardiovasc. Med. https://doi.org/10.3389/fcvm.2021.745758
(2021)."),[62](/articles/s41579-022-00846-2#ref-CR62 "Katsoularis, I. et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ 377, e069590 (2022)."). Microclots detected in both acute COVID-19 and long COVID contribute to thrombosis[63](/articles/s41579-022-00846-2#ref-CR63 "Pretorius, E. et al. Persistent clotting protein pathology in Long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 20, 172 (2021).") and are an attractive diagnostic and therapeutic target. Long-term changes to the size and stiffness of blood cells have also been found in long COVID, with the potential to affect oxygen delivery[64](/articles/s41579-022-00846-2#ref-CR64 "Kubánková, M. et al. Physical phenotype of blood cells is altered in COVID-19. Biophys. J. 120, 2838–2847 (2021)."). A long-lasting reduction in vascular density, specifically affecting small capillaries, was found in patients with long COVID compared with controls, 18 months after infection[65](/articles/s41579-022-00846-2#ref-CR65 "Osiaevi, I. et al. Persistent capillary rarefication in long COVID syndrome. Angiogenesis
https://doi.org/10.1007/s10456-022-09850-9
(2022)."). A study finding elevated levels of vascular transformation blood biomarkers in long COVID also found that the angiogenesis markers ANG1 and P-selectin both had high sensitivity and specificity for predicting long COVID status[66](/articles/s41579-022-00846-2#ref-CR66 "Patel, M. A. et al. Elevated vascular transformation blood biomarkers in long-COVID indicate angiogenesis as a key pathophysiological mechanism. Mol. Med. 28, 122 (2022).").An analysis of the US Department of Veterans Affairs databases (VA data) including more than 150,000 individuals 1 year after SARS-CoV-2 infection indicated a significantly increased risk of a variety of cardiovascular diseases, including heart failure, dysrhythmias and stroke, independent of the severity of initial COVID-19 presentation8 (Fig. 2). Cardiac MRI studies revealed cardiac impairment in 78% of 100 individuals who had a prior COVID-19 episode (investigated an average of 71 days after infection67) and in 58% of participants with long COVID (studied 12 months after infection68), reinforcing the durability of cardiac abnormalities.
Multiple studies have revealed multi-organ damage associated with COVID-19. One prospective study of low-risk individuals, looking at the heart, lungs, liver, kidneys, pancreas and spleen, noted that 70% of 201 patients had damage to at least one organ and 29% had multi-organ damage69. In a 1-year follow-up study, conducted by the same research group with 536 participants, the study authors found that 59% had single-organ damage and 27% multi-organ damage[70](/articles/s41579-022-00846-2#ref-CR70 "Dennis, A. et al. Multi-organ impairment and Long COVID: a 1-year prospective, longitudinal cohort study. Preprint at medRxiv https://doi.org/10.1101/2022.03.18.22272607
(2022)."). A dedicated kidney study of VA data including more than 89,000 individuals who had COVID-19 noted an increased risk of numerous adverse kidney outcomes[71](/articles/s41579-022-00846-2#ref-CR71 "Bowe, B., Xie, Y., Xu, E. & Al-Aly, Z. Kidney outcomes in Long COVID. J. Am. Soc. Nephrol. 32, 2851–2862 (2021)."). Another VA data analysis, including more than 181,000 individuals who had COVID-19, found that infection also increases the risk of type 2 diabetes[9](/articles/s41579-022-00846-2#ref-CR9 "Xie, Y. & Al-Aly, Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 10, 311–321 (2022).") (Fig. [2](/articles/s41579-022-00846-2#Fig2)). The organ damage experienced by patients with long COVID appears durable, and long-term effects remain unknown.Neurological and cognitive systems
Neurological and cognitive symptoms are a major feature of long COVID, including sensorimotor symptoms, memory loss, cognitive impairment, paresthesia, dizziness and balance issues, sensitivity to light and noise, loss of (or phantom) smell or taste, and autonomic dysfunction, often impacting activities of daily living7,32. Audiovestibular manifestations of long COVID include tinnitus, hearing loss and vertigo7,72.
In a meta-analysis, fatigue was found in 32% and cognitive impairment was found in 22% of patients with COVID-19 at 12 weeks after infection3. Cognitive impairments in long COVID are debilitating, at the same magnitude as intoxication at the UK drink driving limit or 10 years of cognitive ageing73, and may increase over time, with one study finding occurrence in 16% of patients at 2 months after infection and 26% of patients at 12 months after infection[74](/articles/s41579-022-00846-2#ref-CR74 "Cysique, L. A. et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. Preprint at medRxiv https://doi.org/10.1101/2022.06.07.22276020
(2022)."). Activation of the kynurenine pathway, particularly the presence of the metabolites quinolinic acid, 3-hydroxyanthranilic acid and kynurenine, has been identified in long COVID, and is associated with cognitive impairment[74](/articles/s41579-022-00846-2#ref-CR74 "Cysique, L. A. et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. Preprint at medRxiv
https://doi.org/10.1101/2022.06.07.22276020
(2022)."). Cognitive impairment has also been found in individuals who recovered from COVID-19 (ref. [75](/articles/s41579-022-00846-2#ref-CR75 "Crivelli, L. et al. Changes in cognitive functioning after COVID-19: a systematic review and meta-analysis. Alzheimers Dement. 18, 1047–1066 (2022).")), and at higher rates when objective versus subjective measures were used[3](/articles/s41579-022-00846-2#ref-CR3 "Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 101, 93–135 (2022)."), suggesting that a subset of those with cognitive impairment may not recognize and/or report their impairment. Cognitive impairment is a feature that manifests itself independently of mental health conditions such as anxiety and depression[74](/articles/s41579-022-00846-2#ref-CR74 "Cysique, L. A. et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. Preprint at medRxiv
https://doi.org/10.1101/2022.06.07.22276020
(2022)."),[76](/articles/s41579-022-00846-2#ref-CR76 "Woo, M. S. et al. Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2, fcaa205 (2020)."), and occurs at similar rates in hospitalized and non-hospitalized patients[74](/articles/s41579-022-00846-2#ref-CR74 "Cysique, L. A. et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. Preprint at medRxiv
https://doi.org/10.1101/2022.06.07.22276020
(2022)."),[76](/articles/s41579-022-00846-2#ref-CR76 "Woo, M. S. et al. Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2, fcaa205 (2020)."). A report of more than 1.3 million people who had COVID-19 showed mental health conditions such as anxiety and depression returned to normal over time, but increased risks of cognitive impairment (brain fog), seizures, dementia, psychosis and other neurocognitive conditions persisted for at least 2 years[77](/articles/s41579-022-00846-2#ref-CR77 "Taquet, M. et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry 9, 815–827 (2022).").Possible mechanisms for these neuropathologies include neuroinflammation, damage to blood vessels by coagulopathy and endothelial dysfunction, and injury to neurons32. Studies have found Alzheimer disease-like signalling in patients with long COVID78, peptides that self-assemble into amyloid clumps which are toxic to neurons79, widespread neuroinflammation[80](/articles/s41579-022-00846-2#ref-CR80 "Visser, D. et al. Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET. Preprint at medRxiv https://doi.org/10.1101/2022.06.02.22275916
(2022)."), brain and brainstem hypometabolism correlated with specific symptoms[81](/articles/s41579-022-00846-2#ref-CR81 "Guedj, E. et al. 18F-FDG brain PET hypometabolism in patients with long COVID. Eur. J. Nucl. Med. Mol. Imaging 48, 2823–2833 (2021)."),[82](/articles/s41579-022-00846-2#ref-CR82 "Hugon, J. et al. Cognitive decline and brainstem hypometabolism in long COVID: a case series. Brain Behav. 12, e2513 (2022).") and abnormal cerebrospinal fluid findings in non-hospitalized individuals with long COVID along with an association between younger age and a delayed onset of neurological symptoms[83](/articles/s41579-022-00846-2#ref-CR83 "Apple, A. C. et al. Risk factors and abnormal cerebrospinal fluid associate with cognitive symptoms after mild COVID-19. Ann. Clin. Transl Neurol. 9, 221–226 (2022)."). Multilineage cellular dysregulation and myelin loss were reported in a recent preprint in patients with long COVID who had mild infections, with microglial reactivity similar to that seen in chemotherapy, known as ‘chemo-brain’[42](/articles/s41579-022-00846-2#ref-CR42 "Fernández-Castañeda, A. et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Preprint at bioRxiv
https://doi.org/10.1101/2022.01.07.475453
(2022)."). A study from the UK Biobank, including brain imaging in the same patients before and after COVID-19 as well as control individuals, showed a reduction in grey matter thickness in the orbitofrontal cortex and parahippocampal gyrus (markers of tissue damage in areas connected to the primary olfactory cortex), an overall reduction in brain size and greater cognitive decline in patients after COVID-19 compared with controls, even in non-hospitalized patients. Although that study looked at individuals with COVID-19 compared with controls, not specifically long COVID, it may have an implication for the cognitive component of long COVID[84](/articles/s41579-022-00846-2#ref-CR84 "Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604, 697–707 (2022)."). Abnormal levels of mitochondrial proteins as well as SARS-CoV-2 spike and nucleocapsid proteins have been found in the central nervous system[85](/articles/s41579-022-00846-2#ref-CR85 "Peluso, M. J. et al. SARS-CoV-2 and mitochondrial proteins in neural-derived exosomes of COVID-19. Ann. Neurol. 91, 772–781 (2022)."). Tetrahydrobiopterin deficiencies and oxidative stress are found in long COVID as well[86](/articles/s41579-022-00846-2#ref-CR86 "Villaume, W. A. Marginal BH4 deficiencies, iNOS, and self-perpetuating oxidative stress in post-acute sequelae of Covid-19. Med. Hypotheses 163, 110842 (2022).").In the eyes, corneal small nerve fibre loss and increased dendritic cell density have been found in long COVID[87](/articles/s41579-022-00846-2#ref-CR87 "Bitirgen, G. et al. Corneal confocal microscopy identifies corneal nerve fibre loss and increased dendritic cells in patients with long COVID. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319450
(2021)."),[88](/articles/s41579-022-00846-2#ref-CR88 "Barros, A. et al. Small fiber neuropathy in the cornea of Covid-19 patients associated with the generation of ocular surface disease. Ocul. Surf. 23, 40–48 (2022)."), as well as significantly altered pupillary light responses[89](/articles/s41579-022-00846-2#ref-CR89 "Bitirgen, G. et al. Abnormal quantitative pupillary light responses following COVID-19. Int. Ophthalmol.
https://doi.org/10.1007/s10792-022-02275-9
(2022).") and impaired retinal microcirculation[90](/articles/s41579-022-00846-2#ref-CR90 "Mardin, C. Y. et al. Possible impact of functional active GPCR-autoantibodies on retinal microcirculation in long-COVID. Invest. Ophthalmol. Vis. Sci. 63, 3315–F0124 (2022)."). SARS-CoV-2 can infect and replicate in retinal[59](/articles/s41579-022-00846-2#ref-CR59 "Menuchin-Lasowski, Y. et al. SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids. Stem Cell Rep 17, 789–803 (2022).") and brain[91](/articles/s41579-022-00846-2#ref-CR91 "Zhang, B.-Z. et al. SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res. 30, 928–931 (2020).") organoids. Other manifestations of long COVID include retinal haemorrhages, cotton wool spots and retinal vein occlusion[92](/articles/s41579-022-00846-2#ref-CR92 "Sen, S. et al. Retinal manifestations in patients with SARS-CoV-2 infection and pathogenetic implications: a systematic review. Int. Ophthalmol. 42, 323–336 (2022).").Mouse models of mild SARS-CoV-2 infection demonstrated microglial reactivity and elevated levels of CCL11, which is associated with cognitive dysfunction and impaired neurogenesis[42](/articles/s41579-022-00846-2#ref-CR42 "Fernández-Castañeda, A. et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Preprint at bioRxiv https://doi.org/10.1101/2022.01.07.475453
(2022)."). Hamster models exhibited an ongoing inflammatory state, involving T cell and myeloid activation, production of pro-inflammatory cytokines and an interferon response that was correlated with anxiety and depression-like behaviours in the hamsters, with similar transcriptional signatures found in the tissue of humans who had recovered from COVID-19 (ref. [93](/articles/s41579-022-00846-2#ref-CR93 "Frere, J. J. et al. SARS-CoV-2 infection in hamsters and humans results in lasting and unique systemic perturbations post recovery. Sci. Transl Med. 14, eabq3059 (2022).")). Infected non-human primates with mild illness showed neuroinflammation, neuronal injury and apoptosis, brain microhaemorrhages, and chronic hypoxaemia and brain hypoxia[94](/articles/s41579-022-00846-2#ref-CR94 "Rutkai, I. et al. Neuropathology and virus in brain of SARS-CoV-2 infected non-human primates. Nat. Commun. 13, 1745 (2022).").Recent reports indicate low blood cortisol levels in patients with long COVID as compared with control individuals, more than 1 year into symptom duration[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv https://doi.org/10.1101/2022.08.09.22278592
(2022)."),[27](/articles/s41579-022-00846-2#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022)."). Low cortisol production by the adrenal gland should be compensated by an increase in adrenocorticotropic hormone (ACTH) production by the pituitary gland, but this was not the case, supporting hypothalamus–pituitary–adrenal axis dysfunction[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv
https://doi.org/10.1101/2022.08.09.22278592
(2022)."). This may also reflect an underlying neuroinflammatory process. Low cortisol levels have previously been documented in individuals with ME/CFS.ME/CFS, dysautonomia and related conditions
ME/CFS is a multisystem neuroimmune illness with onset often following a viral or bacterial infection. Criteria include a “substantial reduction or impairment in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities” for at least 6 months, accompanied by a profound fatigue that is not alleviated by rest, along with postexertional malaise, unrefreshing sleep and cognitive impairment or orthostatic intolerance (or both)95. Up to 75% of people with ME/CFS cannot work full-time and 25% have severe ME/CFS, which often means they are bed-bound, have extreme sensitivity to sensory input and are dependent on others for care96. There is a vast collection of biomedical findings in ME/CFS[97](/articles/s41579-022-00846-2#ref-CR97 "The ME Association. Index of ME/CFS published research - Nov 2022. 224 Index of ME/CFS Published Research. The ME Association https://meassociation.org.uk/
(2022)."),[98](/articles/s41579-022-00846-2#ref-CR98 "Seltzer, J. & Thomas, J. ME Research Summary 2019 (The ME Association, 2019)."), although these are not well known to researchers and clinicians in other fields.Many researchers have commented on the similarity between ME/CFS and long COVID99; around half of individuals with long COVID are estimated to meet the criteria for ME/CFS10,11,29,100, and in studies where the cardinal ME/CFS symptom of postexertional malaise is measured, a majority of individuals with long COVID report experiencing postexertional malaise7,100. A study of orthostatic stress in individuals with long COVID and individuals with ME/CFS found similar haemodynamic, symptomatic and cognitive abnormalities in both groups compared with healthy individuals101. Importantly, it is not surprising that ME/CFS should stem from SARS-CoV-2 infection as 27.1% of SARS-CoV infection survivors in one study met the criteria for ME/CFS diagnosis 4 years after onset102. A wide range of pathogens cause ME/CFS onset, including EBV, Coxiella burnetii (which causes Q fever), Ross River virus and West Nile virus38.
Consistent abnormal findings in ME/CFS include diminished natural killer cell function, T cell exhaustion and other T cell abnormalities, mitochondrial dysfunction, and vascular and endothelial abnormalities, including deformed red blood cells and reduced blood volume. Other abnormalities include exercise intolerance, impaired oxygen consumption and a reduced anaerobic threshold, and abnormal metabolic profiles, including altered usage of fatty acids and amino acids. Altered neurological functions have also been observed, including neuroinflammation, reduced cerebral blood flow, brainstem abnormalities and elevated ventricular lactate level, as well as abnormal eye and vision findings. Reactivated herpesviruses (including EBV, HHV-6, HHV-7 and human cytomegalovirus) are also associated with ME/CFS[97](/articles/s41579-022-00846-2#ref-CR97 "The ME Association. Index of ME/CFS published research - Nov 2022. 224 Index of ME/CFS Published Research. The ME Association https://meassociation.org.uk/
(2022)."),[98](/articles/s41579-022-00846-2#ref-CR98 "Seltzer, J. & Thomas, J. ME Research Summary 2019 (The ME Association, 2019)."),[103](/articles/s41579-022-00846-2#ref-CR103 "Keller, B. A., Pryor, J. L. & Giloteaux, L. Inability of myalgic encephalomyelitis/chronic fatigue syndrome patients to reproduce VO2peak indicates functional impairment. J. Transl Med. 12, 104 (2014)."),[104](/articles/s41579-022-00846-2#ref-CR104 "Saha, A. K. et al. Erythrocyte deformability as a potential biomarker for chronic fatigue syndrome. Blood 132, 4874 (2018).").Many of these findings have been observed in long COVID studies in both adults and children (Box 1). Long COVID research has found mitochondrial dysfunction including loss of mitochondrial membrane potential105 and possible dysfunctional mitochondrial metabolism106, altered fatty acid metabolism and dysfunctional mitochondrion-dependent lipid catabolism consistent with mitochondrial dysfunction in exercise intolerance107, redox imbalance108, and exercise intolerance and impaired oxygen extraction100,109,110. Studies have also found endothelial dysfunction29, cerebral blood flow abnormalities and metabolic changes81,111,112,113 (even in individuals with long COVID whose POTS symptoms abate114), extensive neuroinflammation[42](/articles/s41579-022-00846-2#ref-CR42 "Fernández-Castañeda, A. et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Preprint at bioRxiv https://doi.org/10.1101/2022.01.07.475453
(2022)."),[80](/articles/s41579-022-00846-2#ref-CR80 "Visser, D. et al. Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET. Preprint at medRxiv
https://doi.org/10.1101/2022.06.02.22275916
(2022)."), reactivated herpesviruses[18](/articles/s41579-022-00846-2#ref-CR18 "Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv
https://doi.org/10.1101/2022.08.09.22278592
(2022)."),[21](/articles/s41579-022-00846-2#ref-CR21 "Zubchenko, S., Kril, I., Nadizhko, O., Matsyura, O. & Chopyak, V. Herpesvirus infections and post-COVID-19 manifestations: a pilot observational study. Rheumatol. Int.
https://doi.org/10.1007/s00296-022-05146-9
(2022)."),[27](/articles/s41579-022-00846-2#ref-CR27 "Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022)."), deformed red blood cells[64](/articles/s41579-022-00846-2#ref-CR64 "Kubánková, M. et al. Physical phenotype of blood cells is altered in COVID-19. Biophys. J. 120, 2838–2847 (2021).") and many findings discussed elsewhere. Microclots and hyperactivated platelets are found not only in individuals with long COVID but also in individuals with ME/CFS[115](/articles/s41579-022-00846-2#ref-CR115 "Nunes, J. M., Kruger, A., Proal, A., Kell, D. B. & Pretorius, E. The occurrence of hyperactivated platelets and fibrinaloid microclots in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Pharmaceuticals 15, 931 (2022).").Dysautonomia, particularly POTS, is commonly comorbid with ME/CFS116 and also often has a viral onset117. POTS is associated with G protein-coupled adrenergic receptor and muscarinic acetylcholine receptor autoantibodies, platelet storage pool deficiency, small fibre neuropathy and other neuropathologies118. Both POTS and small fibre neuropathy are commonly found in long COVID111,119, with one study finding POTS in 67% of a cohort with long COVID120.
Mast cell activation syndrome is also commonly comorbid with ME/CFS. The number and severity of mast cell activation syndrome symptoms substantially increased in patients with long COVID compared with pre-COVID and control individuals121, with histamine receptor antagonists resulting in improvements in the majority of patients19.
Other conditions that are commonly comorbid with ME/CFS include connective tissue disorders including Ehlers–Danlos syndrome and hypermobility, neuro-orthopaedic spinal and skull conditions, and endometriosis33,122,123. Evidence is indicating these conditions may be comorbid with long COVID as well. The overlap of postviral conditions with these conditions should be explored further.
Reproductive system
Impacts on the reproductive system are often reported in long COVID, although little research has been done to document the extent of the impact and sex-specific pathophysiology. Menstrual alterations are more likely to occur in women and people who menstruate with long COVID than in women and people who menstruate with no history of COVID and those who had COVID-19 but not long COVID124. Menstruation and the week before menstruation have been identified by patients as triggers for relapses of long COVID symptoms7. Declined ovarian reserve and reproductive endocrine disorder have been observed in people with COVID-19 (ref. 125), and initial theories suggest that SARS-CoV-2 infection affects ovary hormone production and/or the endometrial response due to the abundance of ACE2 receptors on ovarian and endometrial tissue[126](/articles/s41579-022-00846-2#ref-CR126 "Sharp, G. C. et al. The COVID-19 pandemic and the menstrual cycle: research gaps and opportunities. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyab239
(2021)."). Individuals with both COVID-19 and menstrual changes were more likely to experience fatigue, headache, body ache and pain, and shortness of breath than those who did not have menstrual changes, and the most common menstrual changes were irregular menstruation, increased premenstrual symptoms and infrequent menstruation[127](/articles/s41579-022-00846-2#ref-CR127 "Khan, S. M. et al. SARS-CoV-2 infection and subsequent changes in the menstrual cycle among participants in the Arizona CoVHORT study. Am. J. Obstet. Gynecol. 226, 270–273 (2022).").Research on ME/CFS shows associations between ME/CFS and premenstrual dysphoric disorder, polycystic ovarian syndrome, menstrual cycle abnormalities, ovarian cysts, early menopause and endometriosis128,129,130. Pregnancy, postpartum changes, perimenopause and menstrual cycle fluctuations affect ME/CFS and influence metabolic and immune system changes129. Long COVID research should focus on these relationships to better understand the pathophysiology.
Viral persistence in the penile tissue has been documented, as has an increased risk of erectile dysfunction, likely resulting from endothelial dysfunction131. In one study, impairments to sperm count, semen volume, motility, sperm morphology and sperm concentration were reported in individuals with long COVID compared with control individuals, and were correlated with elevated levels of cytokines and the presence of caspase 8, caspase 9 and caspase 3 in seminal fluid132.
Respiratory system
Respiratory conditions are a common phenotype in long COVID, and in one study occurred twice as often in COVID-19 survivors as in the general population2. Shortness of breath and cough are the most common respiratory symptoms, and persisted for at least 7 months in 40% and 20% of patients with long COVID, respectively7. Several imaging studies that included non-hospitalized individuals with long COVID demonstrated pulmonary abnormalities including in air trapping and lung perfusion133,134. An immunological and proteomic study of patients 3–6 months after infection indicated apoptosis and epithelial damage in the airway but not in blood samples135. Further immunological characterization comparing individuals with long COVID with individuals who had recovered from COVID-19 noted a correlation between decreased lung function, systemic inflammation and SARS-CoV-2-specific T cells136.
Gastrointestinal system
Long COVID gastrointestinal symptoms include nausea, abdominal pain, loss of appetite, heartburn and constipation137. The gut microbiota composition is significantly altered in patients with COVID-19 (ref. 23), and gut microbiota dysbiosis is also a key component of ME/CFS138. Higher levels of Ruminococcus gnavus and Bacteroides vulgatus and lower levels of Faecalibacterium prausnitzii have been found in people with long COVID compared with non-COVID-19 controls (from before the pandemic), with gut dysbiosis lasting at least 14 months; low levels of butyrate-producing bacteria are strongly correlated with long COVID at 6 months24. Persisting respiratory and neurological symptoms are each associated with specific gut pathogens24. Additionally, SARS-CoV-2 RNA is present in stool samples of patients with COVID-19 (ref. 139), with one study indicating persistence in the faeces of 12.7% of participants 4 months after diagnosis of COVID-19 and in 3.8% of participants at 7 months after diagnosis61. Most patients with long COVID symptoms and inflammatory bowel disease 7 months after infection had antigen persistence in the gut mucosa140. Higher levels of fungal translocation, from the gut and/or lung epithelium, have been found in the plasma of patients with long COVID compared with those without long COVID or SARS-CoV-2-negative controls, possibly inducing cytokine production[141](/articles/s41579-022-00846-2#ref-CR141 "Giron, L. B. et al. Markers of fungal translocation are elevated during post-acute sequelae of SARS-CoV-2 and induce NF-κB signaling. JCI Insight https://doi.org/10.1172/jci.insight.160989
(2022)."). Transferring gut bacteria from patients with long COVID to healthy mice resulted in lost cognitive functioning and impaired lung defences in the mice, who were partially treated with the commensal probiotic bacterium _Bifidobacterium longum_[25](/articles/s41579-022-00846-2#ref-CR25 "Mendes de Almeida, V. Gut microbiota from patients with mild COVID-19 cause alterations in mice that resemble post-COVID syndrome. Res. Sq.
https://doi.org/10.21203/rs.3.rs-1756189/v1
(2022).").Timelines
The onset and time course of symptoms differ across individuals and by symptom type. Neurological symptoms often have a delayed onset of weeks to months: among participants with cognitive symptoms, 43% reported a delayed onset of cognitive symptoms at least 1 month after COVID-19, with the delay associated with younger age83. Several neurocognitive symptoms worsen over time and tend to persist longer, whereas gastrointestinal and respiratory symptoms are more likely to resolve7,[74](/articles/s41579-022-00846-2#ref-CR74 "Cysique, L. A. et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. Preprint at medRxiv https://doi.org/10.1101/2022.06.07.22276020
(2022)."),[142](/articles/s41579-022-00846-2#ref-CR142 "Jason, L. A. et al. COVID-19 symptoms over time: comparing long-haulers to ME/CFS. Fatigue Biomed. Health Behav. 9, 59–68 (2021)."). Additionally, pain in joints, bones, ears, neck and back are more common at 1 year than at 2 months, as is paresthesia, hair loss, blurry vision and swelling of the legs, hands and feet[143](/articles/s41579-022-00846-2#ref-CR143 "Tran, V.-T., Porcher, R., Pane, I. & Ravaud, P. Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nat. Commun. 13, 1812 (2022)."). Parosmia has an average onset of 3 months after the initial infection[144](/articles/s41579-022-00846-2#ref-CR144 "Walker, A., Kelly, C., Pottinger, G. & Hopkins, C. Parosmia — a common consequence of covid-19. BMJ 377, e069860 (2022)."); unlike other neurocognitive symptoms, it often decreases over time[143](/articles/s41579-022-00846-2#ref-CR143 "Tran, V.-T., Porcher, R., Pane, I. & Ravaud, P. Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nat. Commun. 13, 1812 (2022).").Few people with long COVID demonstrate full recovery, with one study finding that 85% of patients who had symptoms 2 months after the initial infection reported symptoms 1 year after symptom onset143. Future prognosis is uncertain, although diagnoses of ME/CFS and dysautonomia are generally lifelong.
Diagnostic tools and treatments
Although diagnostic tools exist for some components of long COVID (for example, tilt table tests for POTS145 and MRI scans to detect cardiovascular impairment68), diagnostic tools for long COVID are mostly in development, including imaging to detect microclots63, corneal microscopy to identify small fibre neuropathy[87](/articles/s41579-022-00846-2#ref-CR87 "Bitirgen, G. et al. Corneal confocal microscopy identifies corneal nerve fibre loss and increased dendritic cells in patients with long COVID. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319450
(2021)."), new fragmentation of QRS complex on electrocardiograms as indicative of cardiac injury[146](/articles/s41579-022-00846-2#ref-CR146 "Stavileci, B., Özdemir, E., Özdemir, B., Ereren, E. & Cengiz, M. De-novo development of fragmented QRS during a six-month follow-up period in patients with COVID-19 disease and its cardiac effects. J. Electrocardiol. 72, 44–48 (2022).") and use of hyperpolarized MRI to detect pulmonary gas exchange abnormalities[147](/articles/s41579-022-00846-2#ref-CR147 "Grist, J. T. et al. Lung abnormalities depicted with hyperpolarized 129Xe MRI in patients with long COVID. Radiology 305, 709–717 (2022)."). On the basis of the tests that are offered as standard care, the results for patients with long COVID are often normal; many providers are unaware of the symptom-specific testing and diagnostic recommendations from the ME/CFS community[148](/articles/s41579-022-00846-2#ref-CR148 "US ME/CFS Clinician Coalition. Testing Recommendations for Suspected ME/CFS (US ME/CFS Clinician Coalition, 2021)."). Early research into biomarkers suggests that levels of extracellular vesicles[85](/articles/s41579-022-00846-2#ref-CR85 "Peluso, M. J. et al. SARS-CoV-2 and mitochondrial proteins in neural-derived exosomes of COVID-19. Ann. Neurol. 91, 772–781 (2022).") and/or immune markers indicating high cytotoxicity[149](/articles/s41579-022-00846-2#ref-CR149 "Galán, M. et al. Persistent overactive cytotoxic immune response in a Spanish cohort of individuals with long-COVID: identification of diagnostic biomarkers. Front. Immunol. 13, 848886 (2022).") could be indicative of long COVID. Intriguingly, dogs can identify individuals with long COVID on the basis of sweat samples[150](/articles/s41579-022-00846-2#ref-CR150 "Grandjean, D. et al. Screening for SARS-CoV-2 persistence in Long COVID patients using sniffer dogs and scents from axillary sweats samples. Clin. Trials 12, 2 (2022)."). Biomarker research in ME/CFS may also be applicable to long COVID, including electrical impedance blood tests, saliva tests, erythrocyte deformation, sex-specific plasma lipid profiles and variables related to isocapnic buffering[151](#ref-CR151 "Pifarré, F. et al. The use of oxygen as a possible screening biomarker for the diagnosis of chronic fatigue. Apunt. Sports Med 57, 100379 (2022)."),[152](#ref-CR152 "Jason, L. A., Kalns, J., Richarte, A., Katz, B. Z. & Torres, C. Saliva fatigue biomarker index as a marker for severe myalgic encephalomyelitis/chronic fatigue syndrome in a community based sample. Fatigue Biomed. Health Behav. 9, 189–195 (2021)."),[153](#ref-CR153 "Esfandyarpour, R., Kashi, A., Nemat-Gorgani, M., Wilhelmy, J. & Davis, R. W. A nanoelectronics-blood-based diagnostic biomarker for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Proc. Natl Acad. Sci. USA 116, 10250–10257 (2019)."),[154](/articles/s41579-022-00846-2#ref-CR154 "Nkiliza, A. et al. Sex-specific plasma lipid profiles of ME/CFS patients and their association with pain, fatigue, and cognitive symptoms. J. Transl Med. 19, 370 (2021)."). The importance of developing and validating biomarkers that can be used for the diagnosis of long COVID cannot be adequately emphasized — they will not only be helpful in establishing the diagnosis but will also be helpful for objectively defining treatment responses.Although there are currently no broadly effective treatments for long COVID, treatments for certain components have been effective for subsets of populations (Table 1). Many strategies for ME/CFS are effective for individuals with long COVID, including pacing7,37 and symptom-specific pharmacological options (for example, β-blockers for POTS, low-dose naltrexone for neuroinflammation155 and intravenous immunoglobulin for immune dysfunction) and non-pharmacological options (including increasing salt intake for POTS, cognitive pacing for cognitive dysfunction and elimination diets for gastrointestinal symptoms)96. Low-dose naltrexone has been used in many diseases, including ME/CFS155, and has also shown promise in treating long COVID[156](/articles/s41579-022-00846-2#ref-CR156 "Pitt, B., Tate, A. M., Gluck, D., Rosenson, R. S. & Goonewardena, S. N. Repurposing low-dose naltrexone (LDN) for the prevention and treatment of immunothrombosis in COVID-19. Eur. Heart J. Cardiovasc. Pharmacother. https://doi.org/10.1093/ehjcvp/pvac014
(2022)."). H1 and H2 antihistamines, often following protocols for mast cell activation syndrome and particularly involving famotidine, are used to alleviate a wide range of symptoms[19](/articles/s41579-022-00846-2#ref-CR19 "Glynne, P., Tahmasebi, N., Gant, V. & Gupta, R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J. Investig. Med. 70, 61–67 (2022)."),[157](/articles/s41579-022-00846-2#ref-CR157 "Alper, K. Case report: famotidine for neuropsychiatric symptoms in COVID-19. Front. Med. 7, 614393 (2020)."), although they are not a cure. Another drug, BC007, potentially addresses autoimmunity by neutralizing G protein-coupled receptor autoantibody levels[158](/articles/s41579-022-00846-2#ref-CR158 "Hohberger, B. et al. Case report: neutralization of autoantibodies targeting G-protein-coupled receptors improves capillary impairment and fatigue symptoms after COVID-19 infection. Front. Med. 8, 754667 (2021)."). Anticoagulant regimens are a promising way to address abnormal clotting[159](/articles/s41579-022-00846-2#ref-CR159 "Wang, C. et al. Long COVID: the nature of thrombotic sequelae determines the necessity of early anticoagulation. Front. Cell. Infect. Microbiol. 12, 861703 (2022)."); in one study, resolution of symptoms was seen in all 24 patients receiving triple anticoagulant therapy[31](/articles/s41579-022-00846-2#ref-CR31 "Pretorius, E. et al. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/post-acute sequelae of COVID-19 (PASC). Cardiovasc. Diabetol. 21, 148 (2022)."). Apheresis has also shown promise to alleviate long COVID symptoms; it has been theorized to help remove microclots[160](/articles/s41579-022-00846-2#ref-CR160 "The ME Association. A new treatment for Long Covid? The ME Association
https://meassociation.org.uk/2021/10/a-new-treatment-for-long-covid/
(2021).") and has been shown to reduce autoantibodies in ME/CFS[161](/articles/s41579-022-00846-2#ref-CR161 "Tölle, M. et al. Myalgic encephalomyelitis/chronic fatigue syndrome: efficacy of repeat immunoadsorption. J. Clin. Med. 9, E2443 (2020)."). However, it is quite expensive, and its benefits are uncertain. Some supplements have shown promise in treating both long COVID and ME/CFS, including coenzyme Q10 and d\-ribose[162](/articles/s41579-022-00846-2#ref-CR162 "Wood, E., Hall, K. H. & Tate, W. Role of mitochondria, oxidative stress and the response to antioxidants in myalgic encephalomyelitis/chronic fatigue syndrome: a possible approach to SARS-CoV-2 ‘long-haulers’? Chronic Dis. Transl Med. 7, 14–26 (2020)."), and may deserve further study.Table 1 Summary of candidate treatments and supporting evidence
Of note, exercise is harmful for patients with long COVID who have ME/CFS or postexertional malaise110,[163](/articles/s41579-022-00846-2#ref-CR163 "NICE. Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management. NICE https://www.nice.org.uk/guidance/NG206
(2021).") and should not be used as a treatment[164](#ref-CR164 "World Health Organization. Support for Rehabilitation Self-Management After COVID-19 Related Illness (WHO, 2021)."),[165](#ref-CR165 "CDC. Treatment of ME/CFS | Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). CDC
https://www.cdc.gov/me-cfs/treatment/index.html
(2021)."),[166](/articles/s41579-022-00846-2#ref-CR166 "Long COVID Physio. Exercise. Long COVID Physio
https://longcovid.physio/exercise
(2022)."); one study of people with long COVID noted that physical activity worsened the condition of 75% of patients, and less than 1% saw improvement[109](/articles/s41579-022-00846-2#ref-CR109 "Wright, J., Astill, S. L. & Sivan, M. The relationship between physical activity and Long COVID: a cross-sectional study. Int. J. Environ. Res. Public Health 19, 5093 (2022).").Pilot studies and case reports have revealed additional treatment options worth exploring. A case report noted resolution of long COVID following treatment with the antiviral Paxlovid[167](/articles/s41579-022-00846-2#ref-CR167 "Geng, L. N., Bonilla, H. F., Shafer, R. W., Miglis, M. G. & Yang, P. C. Case report of breakthrough long COVID and the use of nirmatrelvir-ritonavir. Preprint at https://www.researchsquare.com/article/rs-1443341/v1
(2022)."), and a study investigating the treatment of acute COVID-19 with Paxlovid showed a 25% reduction in the incidence of long COVID[168](/articles/s41579-022-00846-2#ref-CR168 "Xie, Y., Choi, T. & Al-Aly, Z. Nirmatrelvir and the risk of post-acute sequelae of COVID-19. Preprint at medRxiv
https://doi.org/10.1101/2022.11.03.22281783
(2022)."); Paxlovid should be investigated further for prevention and treatment of long COVID. A small trial of sulodexide in individuals with endothelial dysfunction saw a reduction in symptom severity[169](/articles/s41579-022-00846-2#ref-CR169 "Charfeddine, S. et al. Sulodexide in the treatment of patients with long COVID 19 symptoms and endothelial dysfunction: the results of TUN-EndCOV study. Arch. Cardiovasc. Dis. Suppl. 14, 127 (2022)."). Pilot studies of probiotics indicated potential in alleviating gastrointestinal and non-gastrointestinal symptoms[170](/articles/s41579-022-00846-2#ref-CR170 "Thomas, R. et al. A randomised, double-blind, placebo-controlled trial evaluating concentrated phytochemical-rich nutritional capsule in addition to a probiotic capsule on clinical outcomes among individuals with COVID-19 — the UK Phyto-V study. COVID 2, 433–449 (2022)."),[171](/articles/s41579-022-00846-2#ref-CR171 "Zhang, L. et al. Gut microbiota-derived synbiotic formula (SIM01) as a novel adjuvant therapy for COVID-19: an open-label pilot study. J. Gastroenterol. Hepatol. 37, 823–831 (2022)."). Two patients with long COVID experienced substantial alleviation of dysautonomia symptoms following stellate ganglion block[172](/articles/s41579-022-00846-2#ref-CR172 "Liu, L. D. & Duricka, D. L. Stellate ganglion block reduces symptoms of Long COVID: a case series. J. Neuroimmunol. 362, 577784 (2022)."). An early study noted that Pycnogenol statistically significantly improved physiological measurements (for example, reduction in oxidative stress) and quality of life (indicated by higher Karnofsky Performance Scale Index scores)[173](/articles/s41579-022-00846-2#ref-CR173 "Belcaro, G. et al. Preventive effects of Pycnogenol® on cardiovascular risk factors (including endothelial function) and microcirculation in subjects recovering from coronavirus disease 2019 (COVID-19). Minerva Med. 113, 300–308 (2022)."),[174](/articles/s41579-022-00846-2#ref-CR174 "Crooks, V., Waller, S., Smith, T. & Hahn, T. J. The use of the Karnofsky Performance Scale in determining outcomes and risk in geriatric outpatients. J. Gerontol. 46, M139–M144 (1991)."), as hypothesized on the basis of success in other clinical studies.Taken together, the current treatment options are based on small-scale pilot studies in long COVID or what has been effective in other diseases; several additional trials are in progress175. There is a wide range of possible treatment options from ME/CFS covering various mechanisms, including improving natural killer cell function, removing autoantibodies, immunosuppressants, antivirals for reactivated herpesviruses, antioxidants, mitochondrial support and mitochondrial energy generation176,177; most need to be clinically trialled, which should happen urgently. Many newer treatment options remain underexplored, including anticoagulants and SARS-CoV-2-specific antivirals, and a lack of funding is a significant limitation to robust trials.
Impact of vaccines, variants and reinfections
The impact of vaccination on the incidence of long COVID differs across studies, in part because of differing study methods, time since vaccination and definitions of long COVID. One study indicated no significant difference in the development of long COVID between vaccinated individuals and unvaccinated individuals178; other studies indicate that vaccines provide partial protection, with a reduced risk of long COVID between 15% and 41%[4](/articles/s41579-022-00846-2#ref-CR4 "Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. https://doi.org/10.1038/s41591-022-01840-0
(2022)."),[5](/articles/s41579-022-00846-2#ref-CR5 "Ayoubkhani, D. et al. Risk of Long Covid in people infected with SARS-CoV-2 after two doses of a COVID-19 vaccine: community-based, matched cohort study. Preprint at medRxiv
https://doi.org/10.1101/2022.02.23.22271388
(2022)."), with long COVID continuing to impact 9% of people with COVID-19.The different SARS-CoV-2 variants and level of (and time since) vaccination may impact the development of long COVID. The UK’s Office for National Statistics found that long COVID was 50% less common in double-vaccinated participants with Omicron BA.1 than in double-vaccinated participants Delta, but that there was no significant difference between triple-vaccinated participants; it also found long COVID was more common after Omicron BA.2 infection than after BA.1 infection in triple-vaccinated participants, with 9.3% developing long COVID from infection with the BA.2 variant[179](/articles/s41579-022-00846-2#ref-CR179 "Office for National Statistics. Self-reported long COVID after infection with the Omicron variant in the UK: 6 May 2022. Office for National Statistics https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidafterinfectionwiththeomicronvariant/6may2022
(2022).").The impact of vaccination on long COVID symptoms in people who had already developed long COVID differs among patients, with 16.7% of patients experiencing a relief of symptoms, 21.4% experiencing a worsening of symptoms and the remainder experiencing unchanged symptoms180.
Reinfections are increasingly common[181](/articles/s41579-022-00846-2#ref-CR181 "VA COVID-19 Observational Research Collaboratory. Burden of PCR-confirmed SARS-CoV-2 reinfection in the U.S. Veterans Administration, March 2020 – January 2022. Preprint at medRxiv https://doi.org/10.1101/2022.03.20.22272571
(2022)."). The impact of multiple instances of COVID-19, including the rate of long COVID in those who recovered from a first infection but developed long COVID following reinfection, and the impact of reinfection on those with pre-existing long COVID is crucial to understand to inform future policy decisions. Early research shows an increasing risk of long COVID sequelae after the second and third infection, even in double-vaccinated and triple-vaccinated people[182](/articles/s41579-022-00846-2#ref-CR182 "Bowe, B., Xie, Y. & Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med.
https://doi.org/10.1038/s41591-022-02051-3
(2022)."). Existing literature suggests multiple infections may cause additional harm or susceptibility to the ME/CFS-type presentation[33](/articles/s41579-022-00846-2#ref-CR33 "Renz-Polster, H., Tremblay, M.-E., Bienzle, D. & Fischer, J. E. The pathobiology of myalgic encephalomyelitis/chronic fatigue syndrome: the case for neuroglial failure. Front. Cell. Neurosci. 16, 888232 (2022)."),[183](/articles/s41579-022-00846-2#ref-CR183 "Blomberg, J., Gottfries, C.-G., Elfaitouri, A., Rizwan, M. & Rosén, A. Infection elicited autoimmunity and myalgic encephalomyelitis/chronic fatigue syndrome: an explanatory model. Front. Immunol. 9, 229 (2018).").There is also early evidence that certain immune responses in people with long COVID, including low levels of protective antibodies and elevated levels of autoantibodies, may suggest an increased susceptibility to reinfection27.
Challenges and recommendations
Issues with PCR and antibody testing throughout the pandemic, inaccurate pandemic narratives and widespread lack of postviral knowledge have caused downstream issues and biases in long COVID research and care.
Testing issues
Most patients with COVID-19 from the first waves did not have laboratory-confirmed infection, with PCR tests being difficult to access unless individuals were hospitalized. Only 1–3% of cases to March 2020 were likely detected184, and the CDC estimates that only 25% of cases in the USA were reported from February 2020 to September 2021 (ref. [185](/articles/s41579-022-00846-2#ref-CR185 "CDC. Estimated COVID-19 burden. Centers for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html
(2020).")); that percentage has likely decreased with the rise in use of at-home rapid tests.Although PCR tests are our best tool for detecting SARS-CoV-2 infections, their false negative rates are still high186. Further bias is caused by false negative rates being higher in women and adults younger than 40 years187, those with a low viral load188 and children (Box 1), with several studies showing 52–90% of cases in children missed by PCR tests189,190. The high false negative PCR rate results in symptomatic patients with COVID-19, who seek a COVID-19 test but receive a false negative result, being included as a control in many studies. Those who have a positive PCR test result (who are more likely to be included in research) are more likely to be male or have a higher viral load. Additionally, the lack of test accessibility as well as the false negative rates has created a significant barrier to care, as many long COVID clinics require PCR tests for admission.
Similarly, there is a broad misconception that everyone makes and retains SARS-CoV-2 antibodies, and many clinicians and researchers are unaware of the limited utility of antibody tests to determine prior infection. Between 22% and 36% of people infected with SARS-CoV-2 do not seroconvert, and many others lose their antibodies over the first few months, with both non-seroconversion and seroreversion being more likely in women, children and individuals with mild infections52,53,191,192,193. At 4 and 8 months after infection, 19% and 61% of patients, respectively, who had mild infections and developed antibodies were found to have seroreverted, compared with 2% and 29% of patients, respectively who had severe infections191. Still, many clinicians and researchers use antibody tests to include or exclude patients with COVID-19 from control groups.
Furthermore, during periods of test inaccessibility, tests were given on the basis of patients having COVID-19-specific symptoms such as loss of smell and taste, fever, and respiratory symptoms, resulting in a bias towards people with those symptoms.
Misinformation on PCR and antibody tests has resulted in the categorization of patients with long COVID into non-COVID-19 control groups, biasing the research output. Because low or no antibody levels and viral load may be related to long COVID pathophysiology, including a clinically diagnosed cohort will strengthen the research.
Important miscues
The narrative that COVID-19 had only respiratory sequelae led to a delayed realization of the neurological, cardiovascular and other multisystem impacts of COVID-19. Many long COVID clinics and providers still disproportionately focus on respiratory rehabilitation, which results in skewed electronic health record data. Electronic health record data are also more comprehensive for those who were hospitalized with COVID-19 than for those who were in community care, leading to a bias towards the more traditional severe respiratory presentation and less focus on non-hospitalized patients, who tend to have neurological and/or ME/CFS-type presentations.
The narrative that initially mild COVID-19 cases, generally defined as not requiring hospitalization in the acute phase, would not have long-term consequences has also had downstream effects on research. These so-called mild cases that result in long COVID often have an underlying biology different from acute severe cases, but the same types of tests are being used to evaluate patients. This is despite basic tests such as D-dimer, C-reactive protein (CRP) and antinuclear antibody tests and complete blood count being known to often return normal results in patients with long COVID. Tests that return abnormal results in patients with ME/CFS and dysautonomia, such as total immunoglobulin tests, natural killer cell function tests, the tilt table or NASA lean test, the four-point salivary cortisol test, reactivated herpesvirus panels, small fibre neuropathy biopsy, and tests looking for abnormal brain perfusion96, should instead be prioritized. Other recurring issues include studies failing to include the full range of symptoms, particularly neurological and reproductive system symptoms, and not asking patients about symptom frequency, severity and disability. Cardinal symptoms such as postexertional malaise are not widely known, and therefore are rarely included in study designs.
Widespread lack of postviral knowledge and misinformation
The widespread lack of knowledge of viral-onset illnesses, especially ME/CFS and dysautonomia, as well as often imperfect coding, prevents these conditions from being identified and documented by clinicians; this means that they are frequently absent from electronic health record data. Further, because ME/CFS and dysautonomia research is not widely known or comprehensively taught in medical schools194, long COVID research is often not built on past findings, and tends to repeat old hypotheses. Additionally, long COVID research studies and medical histories tend to document only the risk factors for severe acute COVID-19, which are different from the risk factors for conditions that overlap with long COVID such as ME/CFS and dysautonomia (for example, connective tissue disorders such as Ehlers–Danlos syndrome, prior illnesses such as infectious mononucleosis and mast cell involvement)33,195,196.
Clinicians who are not familiar with ME/CFS and dysautonomia often misdiagnose mental health disorders in patients; four in five patients with POTS receive a diagnosis with a psychiatric or psychological condition before receiving a POTS diagnosis, with only 37% continuing to have the psychiatric or psychological diagnosis once they have received their POTS diagnosis117. Researchers who are unfamiliar with ME/CFS and dysautonomia often do not know to use specific validated tools when conducting mental health testing, as anxiety scales often include autonomic symptoms such as tachycardia, and depression scales often include symptoms such as fatigue, both of which overestimate mental health disorder prevalence in these conditions197,198.
Recommendations
Although research into long COVID has been expansive and has accelerated, the existing research is not enough to improve outcomes for people with long COVID. To ensure an adequate response to the long COVID crisis, we need research that builds on existing knowledge and is inclusive of the patient experience, training and education for the health-care and research workforce, a public communication campaign, and robust policies and funding to support research and care in long COVID.
Research
We need a comprehensive long COVID research agenda that builds on the existing knowledge from ME/CFS, dysautonomia and other viral-onset conditions, including but not limited to brain and brainstem inflammation, appropriate neuroimaging techniques, neuroimmunology, metabolic profiling, impaired endothelial function, mitochondrial fragmentation, antiviral and metabolic phenotypes, hypoperfusion/cerebral blood flow, nanoneedle diagnostic testing, overlaps with connective tissue disorders, autoimmunity and autoantibodies, viral/microbial persistence, intracranial hypertension, hypermobility, craniocervical obstructions, altered T and B cells, metabolomics and proteomics, elevated blood lactate level, herpesvirus reactivations, immune changes in the early versus late postviral years, and changes to the gut microbiota. The mechanisms of and overlaps between long COVID and connective tissue involvement, mast cells and inflammatory conditions such as endometriosis are particularly understudied and should be focused on. Because of the high prevalence of ME/CFS, POTS and other postinfectious illnesses in patients with long COVID, long COVID research should include people who developed ME/CFS and other postinfectious illnesses from a trigger other than SARS-CoV-2 in comparator groups to improve understanding of the onset and pathophysiology of these illnesses113. Additionally, there is a known immune exhaustion process that occurs between the second and third year of illness in ME/CFS, with test results for cytokines being different between patients who have been sick for shorter durations (less than 2 years) than for those who have been sick for longer durations43. Because of this, studies should implement subanalyses based on the length of time participants have been ill. Because ME/CFS and dysautonomia research is not widely known across the biomedical field, long COVID research should be led by experts from these areas to build on existing research and create new diagnostic and imaging tools.
Robust clinical trials must be a priority moving forward as patients currently have few treatment options. In the absence of validated treatment options, patients and physicians conduct individual experiments, which result in the duplication of efforts without generalizable knowledge and pose undue risks to patients. Robust study design and knowledge sharing must be prioritized by both funding institutions and clinician-researchers.
It is critical that research on long COVID be representative of (or oversample) the populations who had COVID-19 and are developing long COVID at high rates, which is disproportionately people of colour[35](/articles/s41579-022-00846-2#ref-CR35 "CDC. Long COVID - household pulse survey - COVID-19. CDC https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm
(2022)."). Medical research has historically under-represented these populations, and over-representation of white and socio-economically privileged patients has been common in long COVID research. Researchers must work within communities of colour, LGBTQ+ communities and low-income communities to build trust and conduct culturally competent studies that will provide insights and treatments for long COVID for marginalized populations.As a subset of patients will improve over time, and others will have episodic symptoms, care should be taken to incorporate the possibility of alleviation of symptoms into the study design, and care should be taken not to ascribe improvement to a particular cause without proper modelling.
Finally, it is critical that communities of patients with long COVID and associated conditions are meaningfully engaged in long COVID research and clinical trials. The knowledge of those who experience an illness is crucial in identifying proper study design and key research questions and solutions, improving the speed and direction of research.
Training and education of the health-care and research workforce
To prepare the next generation of health-care providers and researchers, medical schools must improve their education on pandemics, viruses and infection-initiated illnesses such as long COVID and ME/CFS, and competency evaluations should include these illnesses. As of 2013, only 6% of medical schools fully cover ME/CFS across the domains of treatment, research and curricula, which has created obstacles to care, accurate diagnosis, research and treatment194. To ensure people with long COVID and associated conditions can receive adequate care now, professional societies and government agencies must educate the health-care and research workforce on these illnesses, including the history of and current best practices for ME/CFS to not repeat mistakes of the past, which have worsened patients’ prognoses. The research community has made a misstep in its efforts to treat ME/CFS199, and some physicians, poorly educated in the aetiology and pathophysiology of the disorder, still advise patients to pursue harmful interventions such as graded exercise therapy and cognitive behavioural therapy, despite the injury that these interventions cause200 and the fact that they are explicitly not advised as treatments[163](/articles/s41579-022-00846-2#ref-CR163 "NICE. Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management. NICE https://www.nice.org.uk/guidance/NG206
(2021)."),[164](/articles/s41579-022-00846-2#ref-CR164 "World Health Organization. Support for Rehabilitation Self-Management After COVID-19 Related Illness (WHO, 2021)."),[166](/articles/s41579-022-00846-2#ref-CR166 "Long COVID Physio. Exercise. Long COVID Physio
https://longcovid.physio/exercise
(2022).").Public communications campaign
In addition to providing education on long COVID to the biomedical community, we need a public communications campaign that informs the public about the risks and outcomes of long COVID.
Policies and funding
Finally, we need policies and funding that will sustain long COVID research and enable people with long COVID to receive adequate care and support. For instance, in the USA, the creation of a national institute for complex chronic conditions within the NIH would go a long way in providing a durable funding mechanism and a robust research agenda. Further, we need to create and fund centres of excellence, which would provide inclusive, historically informed and culturally competent care, as well as conduct research and provide medical education to primary care providers. Additionally, research and clinical care do not exist in silos. It is critical to push forward policies that address both the social determinants of health and the social support that is needed for disabled people.
Conclusions
Long COVID is a multisystemic illness encompassing ME/CFS, dysautonomia, impacts on multiple organ systems, and vascular and clotting abnormalities. It has already debilitated millions of individuals worldwide, and that number is continuing to grow. On the basis of more than 2 years of research on long COVID and decades of research on conditions such as ME/CFS, a significant proportion of individuals with long COVID may have lifelong disabilities if no action is taken. Diagnostic and treatment options are currently insufficient, and many clinical trials are urgently needed to rigorously test treatments that address hypothesized underlying biological mechanisms, including viral persistence, neuroinflammation, excessive blood clotting and autoimmunity.
Change history
17 April 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41579-023-00896-0
References
- Ballering, A. V., van Zon, S. K. R., Hartman, T. C. O. & Rosmalen, J. G. M. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet 400, 452–461 (2022).
Article CAS PubMed PubMed Central Google Scholar - Bull-Otterson, L. Post–COVID conditions among adult COVID-19 survivors aged 18–64 and ≥65 years — United States, March 2020–November 2021. MMWR Morb. Mortal. Wkly Rep. 71, 713 (2022).
Article CAS PubMed Central Google Scholar - Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 101, 93–135 (2022).
Article CAS PubMed Google Scholar - Al-Aly, Z., Bowe, B. & Xie, Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat. Med. https://doi.org/10.1038/s41591-022-01840-0 (2022).
Article PubMed PubMed Central Google Scholar - Ayoubkhani, D. et al. Risk of Long Covid in people infected with SARS-CoV-2 after two doses of a COVID-19 vaccine: community-based, matched cohort study. Preprint at medRxiv https://doi.org/10.1101/2022.02.23.22271388 (2022).
- FAIR Health. Patients Diagnosed with Post-COVID Conditions: An Analysis of Private Healthcare Claims Using the Official ICD-10 Diagnostic Code (FAIR Health, 2022).
- Davis, H. E. et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 38, 101019 (2021).
Article PubMed PubMed Central Google Scholar - Xie, Y., Xu, E., Bowe, B. & Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 28, 583–590 (2022).
Article CAS PubMed PubMed Central Google Scholar - Xie, Y. & Al-Aly, Z. Risks and burdens of incident diabetes in long COVID: a cohort study. Lancet Diabetes Endocrinol. 10, 311–321 (2022).
Article CAS PubMed PubMed Central Google Scholar - Mancini, D. M. et al. Use of cardiopulmonary stress testing for patients with unexplained dyspnea post–coronavirus disease. JACC Heart Fail. 9, 927–937 (2021).
Article PubMed PubMed Central Google Scholar - Kedor, C. et al. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat. Commun. 13, 5104 (2022).
Article CAS PubMed PubMed Central Google Scholar - Larsen, N. W. et al. Characterization of autonomic symptom burden in long COVID: a global survey of 2314 adults. Front. Neurol. 13, 1012668 (2022).
Article PubMed PubMed Central Google Scholar - Demko, Z. O. et al. Post-acute sequelae of SARS-CoV-2 (PASC) impact quality of life at 6, 12 and 18 months post-infection. Preprint at medRxiv https://doi.org/10.1101/2022.08.08.22278543 (2022).
- Cairns, R. & Hotopf, M. A systematic review describing the prognosis of chronic fatigue syndrome. Occup. Med. Oxf. Engl. 55, 20–31 (2005).
Article CAS Google Scholar - Bach, K. Is ‘long Covid’ worsening the labor shortage? Brookings https://www.brookings.edu/research/is-long-covid-worsening-the-labor-shortage/ (2022).
- Swank, Z. et al. Persistent circulating severe acute respiratory syndrome coronavirus 2 spike is associated with post-acute coronavirus disease 2019 sequelae. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciac722 (2022).
Article Google Scholar - Proal, A. D. & VanElzakker, M. B. Long COVID or post-acute sequelae of COVID-19 (PASC): an overview of biological factors that may contribute to persistent symptoms. Front. Microbiol. 12, 698169 (2021).
Article PubMed PubMed Central Google Scholar - Klein, J. et al. Distinguishing features of Long COVID identified through immune profiling. Preprint at medRxiv https://doi.org/10.1101/2022.08.09.22278592 (2022).
- Glynne, P., Tahmasebi, N., Gant, V. & Gupta, R. Long COVID following mild SARS-CoV-2 infection: characteristic T cell alterations and response to antihistamines. J. Investig. Med. 70, 61–67 (2022).
Article PubMed Google Scholar - Phetsouphanh, C. et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 23, 210–216 (2022).
Article CAS PubMed Google Scholar - Zubchenko, S., Kril, I., Nadizhko, O., Matsyura, O. & Chopyak, V. Herpesvirus infections and post-COVID-19 manifestations: a pilot observational study. Rheumatol. Int. https://doi.org/10.1007/s00296-022-05146-9 (2022).
Article PubMed PubMed Central Google Scholar - Peluso, M. J. et al. Evidence of recent Epstein-Barr virus reactivation in individuals experiencing Long COVID. Preprint at medRxiv https://doi.org/10.1101/2022.06.21.22276660 (2022).
Article PubMed Google Scholar - Yeoh, Y. K. et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 70, 698–706 (2021).
Article CAS PubMed Google Scholar - Liu, Q. et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut 71, 544–552 (2022).
Article CAS PubMed Google Scholar - Mendes de Almeida, V. Gut microbiota from patients with mild COVID-19 cause alterations in mice that resemble post-COVID syndrome. Res. Sq. https://doi.org/10.21203/rs.3.rs-1756189/v1 (2022).
Article Google Scholar - Wallukat, G. et al. Functional autoantibodies against G-protein coupled receptors in patients with persistent long-COVID-19 symptoms. J. Transl Autoimmun. 4, 100100 (2021).
Article CAS PubMed PubMed Central Google Scholar - Su, Y. et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell 185, 881–895.e20 (2022).
Article CAS PubMed PubMed Central Google Scholar - Arthur, J. M. et al. Development of ACE2 autoantibodies after SARS-CoV-2 infection. PLoS ONE 16, e0257016 (2021).
Article CAS PubMed PubMed Central Google Scholar - Haffke, M. et al. Endothelial dysfunction and altered endothelial biomarkers in patients with post-COVID-19 syndrome and chronic fatigue syndrome (ME/CFS). J. Transl Med. 20, 138 (2022).
Article CAS PubMed PubMed Central Google Scholar - Charfeddine, S. Long COVID 19 syndrome: is it related to microcirculation and endothelial dysfunction? Insights from TUN-EndCOV study. Front. Cardiovasc. Med. https://doi.org/10.3389/fcvm.2021.745758 (2021).
Article PubMed PubMed Central Google Scholar - Pretorius, E. et al. Prevalence of symptoms, comorbidities, fibrin amyloid microclots and platelet pathology in individuals with Long COVID/post-acute sequelae of COVID-19 (PASC). Cardiovasc. Diabetol. 21, 148 (2022).
Article CAS PubMed PubMed Central Google Scholar - Spudich, S. & Nath, A. Nervous system consequences of COVID-19. Science 375, 267–269 (2022).
Article CAS PubMed Google Scholar - Renz-Polster, H., Tremblay, M.-E., Bienzle, D. & Fischer, J. E. The pathobiology of myalgic encephalomyelitis/chronic fatigue syndrome: the case for neuroglial failure. Front. Cell. Neurosci. 16, 888232 (2022).
Article CAS PubMed PubMed Central Google Scholar - Merzon, E. et al. Clinical and socio-demographic variables associated with the diagnosis of long COVID syndrome in youth: a population-based study. Int. J. Environ. Res. Public Health 19, 5993 (2022).
Article CAS PubMed PubMed Central Google Scholar - CDC. Long COVID - household pulse survey - COVID-19. CDC https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm (2022).
- Williamson, A. E., Tydeman, F., Miners, A., Pyper, K. & Martineau, A. R. Short-term and long-term impacts of COVID-19 on economic vulnerability: a population-based longitudinal study (COVIDENCE UK). BMJ Open 12, e065083 (2022).
Article PubMed Google Scholar - Ziauddeen, N. et al. Characteristics and impact of Long Covid: findings from an online survey. PLoS ONE 17, e0264331 (2022).
Article CAS PubMed PubMed Central Google Scholar - Choutka, J., Jansari, V., Hornig, M. & Iwasaki, A. Unexplained post-acute infection syndromes. Nat. Med. 28, 911–923 (2022).
Article CAS PubMed Google Scholar - Komaroff, A. L. & Lipkin, W. I. Insights from myalgic encephalomyelitis/chronic fatigue syndrome may help unravel the pathogenesis of postacute COVID-19 syndrome. Trends Mol. Med. 27, 895–906 (2021).
Article CAS PubMed PubMed Central Google Scholar - Schultheiß, C. et al. From online data collection to identification of disease mechanisms: the IL-1ß, IL-6 and TNF-α cytokine triad is associated with post-acute sequelae of COVID-19 in a digital research cohort. SSRN https://doi.org/10.2139/ssrn.3963839 (2021).
Article Google Scholar - Peluso, M. J. et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J. Infect. Dis. 224, 1839–1848 (2021).
Article CAS PubMed PubMed Central Google Scholar - Fernández-Castañeda, A. et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Preprint at bioRxiv https://doi.org/10.1101/2022.01.07.475453 (2022).
Article PubMed PubMed Central Google Scholar - Hornig, M. et al. Distinct plasma immune signatures in ME/CFS are present early in the course of illness. Sci. Adv. 1, e1400121 (2015).
Article PubMed PubMed Central Google Scholar - Wang, E. Y. et al. Diverse functional autoantibodies in patients with COVID-19. Nature 595, 283–288 (2021).
Article CAS PubMed Google Scholar - Shikova, E. et al. Cytomegalovirus, Epstein-Barr virus, and human herpesvirus-6 infections in patients with myalgic еncephalomyelitis/chronic fatigue syndrome. J. Med. Virol. 92, 3682–3688 (2020).
Article CAS PubMed PubMed Central Google Scholar - Schreiner, P. et al. Human herpesvirus-6 reactivation, mitochondrial fragmentation, and the coordination of antiviral and metabolic phenotypes in myalgic encephalomyelitis/chronic fatigue syndrome. Immunohorizons 4, 201–215 (2020).
Article CAS PubMed Google Scholar - García-Abellán, J. et al. Antibody response to SARS-CoV-2 is associated with long-term clinical outcome in patients with COVID-19: a longitudinal study. J. Clin. Immunol. 41, 1490–1501 (2021).
Article PubMed PubMed Central Google Scholar - Augustin, M. et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Reg. Health Eur. 6, 100122 (2021).
Article PubMed PubMed Central Google Scholar - Talla, A. et al. Longitudinal immune dynamics of mild COVID-19 define signatures of recovery and persistence. Preprint at bioRxiv https://doi.org/10.1101/2021.05.26.442666 (2021).
Article Google Scholar - Peluso, M. J. et al. Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms. Cell Rep. 36, 109518 (2021).
Article CAS PubMed PubMed Central Google Scholar - Hu, F. et al. A compromised specific humoral immune response against the SARS-CoV-2 receptor-binding domain is related to viral persistence and periodic shedding in the gastrointestinal tract. Cell. Mol. Immunol. 17, 1119–1125 (2020).
Article CAS PubMed Google Scholar - Korte, W. et al. SARS-CoV-2 IgG and IgA antibody response is gender dependent; and IgG antibodies rapidly decline early on. J. Infect. 82, e11–e14 (2021).
Article CAS PubMed Google Scholar - Jo, W. et al. A two-phase, single cohort study of COVID-19 antibody sera-surveillance. Ann. Epidemiol. Public Health 4, 1055 (2021).
Article Google Scholar - Nomura, Y. et al. Attenuation of antibody titers from 3 to 6 months after the second dose of the BNT162b2 vaccine depends on sex, with age and smoking risk factors for lower antibody titers at 6 months. Vaccines 9, 1500 (2021).
Article CAS PubMed PubMed Central Google Scholar - Tejerina, F. et al. Post-COVID-19 syndrome. SARS-CoV-2 RNA detection in plasma, stool, and urine in patients with persistent symptoms after COVID-19. BMC Infect. Dis. 22, 211 (2022).
Article CAS PubMed PubMed Central Google Scholar - Goh, D. et al. Persistence of residual SARS-CoV-2 viral antigen and RNA in tissues of patients with long COVID-19. Preprint at https://www.researchsquare.com/article/rs-1379777/v1 (2022).
- Ceulemans, L. J. et al. Persistence of SARS-CoV-2 RNA in lung tissue after mild COVID-19. Lancet Respir. Med. 9, e78–e79 (2021).
Article CAS PubMed PubMed Central Google Scholar - Gaebler, C. et al. Evolution of antibody immunity to SARS-CoV-2. Nature 591, 639–644 (2021).
Article CAS PubMed PubMed Central Google Scholar - Menuchin-Lasowski, Y. et al. SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids. Stem Cell Rep 17, 789–803 (2022).
Article CAS Google Scholar - Cheung, C. C. L. et al. Residual SARS-CoV-2 viral antigens detected in GI and hepatic tissues from five recovered patients with COVID-19. Gut 71, 226–229 (2022).
Article CAS PubMed Google Scholar - Natarajan, A. et al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med 3, 371–387.e9 (2022).
Article CAS PubMed Google Scholar - Katsoularis, I. et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ 377, e069590 (2022).
Article PubMed Google Scholar - Pretorius, E. et al. Persistent clotting protein pathology in Long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 20, 172 (2021).
Article CAS PubMed PubMed Central Google Scholar - Kubánková, M. et al. Physical phenotype of blood cells is altered in COVID-19. Biophys. J. 120, 2838–2847 (2021).
Article PubMed PubMed Central Google Scholar - Osiaevi, I. et al. Persistent capillary rarefication in long COVID syndrome. Angiogenesis https://doi.org/10.1007/s10456-022-09850-9 (2022).
Article PubMed PubMed Central Google Scholar - Patel, M. A. et al. Elevated vascular transformation blood biomarkers in long-COVID indicate angiogenesis as a key pathophysiological mechanism. Mol. Med. 28, 122 (2022).
Article CAS PubMed PubMed Central Google Scholar - Puntmann, V. O. et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 5, 1265–1273 (2020).
Article PubMed PubMed Central Google Scholar - Roca-Fernández, A. et al. Cardiac impairment in Long Covid 1-year post-SARS-CoV-2 infection. Eur. Heart J. 43, ehac544.219 (2022).
Article Google Scholar - Dennis, A. et al. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ Open 11, e048391 (2021).
Article PubMed Google Scholar - Dennis, A. et al. Multi-organ impairment and Long COVID: a 1-year prospective, longitudinal cohort study. Preprint at medRxiv https://doi.org/10.1101/2022.03.18.22272607 (2022).
- Bowe, B., Xie, Y., Xu, E. & Al-Aly, Z. Kidney outcomes in Long COVID. J. Am. Soc. Nephrol. 32, 2851–2862 (2021).
Article CAS PubMed PubMed Central Google Scholar - Almufarrij, I. & Munro, K. J. One year on: an updated systematic review of SARS-CoV-2, COVID-19 and audio-vestibular symptoms. Int. J. Audiol. 60, 935–945 (2021).
Article PubMed Google Scholar - Holdsworth, D. A. et al. Comprehensive clinical assessment identifies specific neurocognitive deficits in working-age patients with long-COVID. PLoS ONE 17, e0267392 (2022).
Article CAS PubMed PubMed Central Google Scholar - Cysique, L. A. et al. Post-acute COVID-19 cognitive impairment and decline uniquely associate with kynurenine pathway activation: a longitudinal observational study. Preprint at medRxiv https://doi.org/10.1101/2022.06.07.22276020 (2022).
- Crivelli, L. et al. Changes in cognitive functioning after COVID-19: a systematic review and meta-analysis. Alzheimers Dement. 18, 1047–1066 (2022).
Article CAS PubMed PubMed Central Google Scholar - Woo, M. S. et al. Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2, fcaa205 (2020).
Article PubMed PubMed Central Google Scholar - Taquet, M. et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry 9, 815–827 (2022).
Article PubMed PubMed Central Google Scholar - Reiken, S. et al. Alzheimer’s-like signaling in brains of COVID-19 patients. Alzheimers Dement. 18, 955–965 (2022).
Article CAS PubMed PubMed Central Google Scholar - Charnley, M. et al. Neurotoxic amyloidogenic peptides in the proteome of SARS-COV2: potential implications for neurological symptoms in COVID-19. Nat. Commun. 13, 3387 (2022).
Article CAS PubMed PubMed Central Google Scholar - Visser, D. et al. Long COVID is associated with extensive in-vivo neuroinflammation on [18F]DPA-714 PET. Preprint at medRxiv https://doi.org/10.1101/2022.06.02.22275916 (2022).
- Guedj, E. et al. 18F-FDG brain PET hypometabolism in patients with long COVID. Eur. J. Nucl. Med. Mol. Imaging 48, 2823–2833 (2021).
Article CAS PubMed PubMed Central Google Scholar - Hugon, J. et al. Cognitive decline and brainstem hypometabolism in long COVID: a case series. Brain Behav. 12, e2513 (2022).
Article CAS PubMed PubMed Central Google Scholar - Apple, A. C. et al. Risk factors and abnormal cerebrospinal fluid associate with cognitive symptoms after mild COVID-19. Ann. Clin. Transl Neurol. 9, 221–226 (2022).
Article CAS PubMed PubMed Central Google Scholar - Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604, 697–707 (2022).
Article CAS PubMed PubMed Central Google Scholar - Peluso, M. J. et al. SARS-CoV-2 and mitochondrial proteins in neural-derived exosomes of COVID-19. Ann. Neurol. 91, 772–781 (2022).
Article CAS PubMed PubMed Central Google Scholar - Villaume, W. A. Marginal BH4 deficiencies, iNOS, and self-perpetuating oxidative stress in post-acute sequelae of Covid-19. Med. Hypotheses 163, 110842 (2022).
Article CAS PubMed PubMed Central Google Scholar - Bitirgen, G. et al. Corneal confocal microscopy identifies corneal nerve fibre loss and increased dendritic cells in patients with long COVID. Br. J. Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319450 (2021).
Article PubMed Google Scholar - Barros, A. et al. Small fiber neuropathy in the cornea of Covid-19 patients associated with the generation of ocular surface disease. Ocul. Surf. 23, 40–48 (2022).
Article PubMed Google Scholar - Bitirgen, G. et al. Abnormal quantitative pupillary light responses following COVID-19. Int. Ophthalmol. https://doi.org/10.1007/s10792-022-02275-9 (2022).
Article PubMed PubMed Central Google Scholar - Mardin, C. Y. et al. Possible impact of functional active GPCR-autoantibodies on retinal microcirculation in long-COVID. Invest. Ophthalmol. Vis. Sci. 63, 3315–F0124 (2022).
Google Scholar - Zhang, B.-Z. et al. SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res. 30, 928–931 (2020).
Article CAS PubMed Google Scholar - Sen, S. et al. Retinal manifestations in patients with SARS-CoV-2 infection and pathogenetic implications: a systematic review. Int. Ophthalmol. 42, 323–336 (2022).
Article PubMed Google Scholar - Frere, J. J. et al. SARS-CoV-2 infection in hamsters and humans results in lasting and unique systemic perturbations post recovery. Sci. Transl Med. 14, eabq3059 (2022).
Article CAS PubMed Google Scholar - Rutkai, I. et al. Neuropathology and virus in brain of SARS-CoV-2 infected non-human primates. Nat. Commun. 13, 1745 (2022).
Article CAS PubMed PubMed Central Google Scholar - Committee on the Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, Board on the Health of Select Populations, & Institute of Medicine. Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness (National Academies Press, 2015).
- Bateman, L. et al. Myalgic encephalomyelitis/chronic fatigue syndrome: essentials of diagnosis and management. Mayo Clin. Proc. 96, 2861–2878 (2021).
Article PubMed Google Scholar - The ME Association. Index of ME/CFS published research - Nov 2022. 224 Index of ME/CFS Published Research. The ME Association https://meassociation.org.uk/ (2022).
- Seltzer, J. & Thomas, J. ME Research Summary 2019 (The ME Association, 2019).
- Wong, T. L. & Weitzer, D. J. Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)-a systemic review and comparison of clinical presentation and symptomatology. Med. (Kaunas.) 57, 418 (2021).
Google Scholar - Twomey, R. et al. Chronic fatigue and postexertional malaise in people living with Long COVID: an observational study. Phys. Ther. 102, pzac005 (2022).
Article PubMed Google Scholar - Vernon, S. D. et al. Orthostatic challenge causes distinctive symptomatic, hemodynamic and cognitive responses in Long COVID and myalgic encephalomyelitis/chronic fatigue syndrome. Front. Med. 9, 917019 (2022).
Article Google Scholar - Lam, M. H.-B. et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch. Intern. Med. 169, 2142–2147 (2009).
Article PubMed Google Scholar - Keller, B. A., Pryor, J. L. & Giloteaux, L. Inability of myalgic encephalomyelitis/chronic fatigue syndrome patients to reproduce VO2peak indicates functional impairment. J. Transl Med. 12, 104 (2014).
Article PubMed PubMed Central Google Scholar - Saha, A. K. et al. Erythrocyte deformability as a potential biomarker for chronic fatigue syndrome. Blood 132, 4874 (2018).
Article Google Scholar - Díaz-Resendiz, K. J. G. et al. Loss of mitochondrial membrane potential (ΔΨm) in leucocytes as post-COVID-19 sequelae. J. Leukoc. Biol. 112, 23–29 (2022).
Article PubMed Google Scholar - Pozzi, A. COVID-19 and mitochondrial non-coding RNAs: new insights from published data. Front. Physiol. 12, 805005 (2022).
Article PubMed PubMed Central Google Scholar - Guntur, V. P. et al. Signatures of mitochondrial dysfunction and impaired fatty acid metabolism in plasma of patients with post-acute sequelae of COVID-19 (PASC). Metabolites 12, 1026 (2022).
Article CAS PubMed PubMed Central Google Scholar - Paul, B. D., Lemle, M. D., Komaroff, A. L. & Snyder, S. H. Redox imbalance links COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome. Proc. Natl Acad. Sci. USA 118, e2024358118 (2021).
Article CAS PubMed PubMed Central Google Scholar - Wright, J., Astill, S. L. & Sivan, M. The relationship between physical activity and Long COVID: a cross-sectional study. Int. J. Environ. Res. Public Health 19, 5093 (2022).
Article CAS PubMed PubMed Central Google Scholar - Heerdt, P. M., Shelley, B. & Singh, I. Impaired systemic oxygen extraction long after mild COVID-19: potential perioperative implications. Br. J. Anaesth. 128, e246–e249 (2022).
Article CAS PubMed Google Scholar - Novak, P. et al. Multisystem involvement in post-acute sequelae of coronavirus disease 19. Ann. Neurol. 91, 367–379 (2022).
Article CAS PubMed PubMed Central Google Scholar - Holmes, E. et al. Incomplete systemic recovery and metabolic phenoreversion in post-acute-phase nonhospitalized COVID-19 patients: implications for assessment of post-acute COVID-19 syndrome. J. Proteome Res. 20, 3315–3329 (2021).
Article CAS PubMed Google Scholar - van Campen, C. L. M. C. & Visser, F. C. Orthostatic intolerance in long-haul COVID after SARS-CoV-2: a case-control comparison with post-EBV and insidious-onset myalgic encephalomyelitis/chronic fatigue syndrome patients. Healthcare 10, 2058 (2022).
Article PubMed Google Scholar - van Campen, C. L. M. C. & Visser, F. C. Long-Haul COVID patients: prevalence of POTS are reduced but cerebral blood flow abnormalities remain abnormal with longer disease duration. Healthcare 10, 2105 (2022).
Article PubMed Google Scholar - Nunes, J. M., Kruger, A., Proal, A., Kell, D. B. & Pretorius, E. The occurrence of hyperactivated platelets and fibrinaloid microclots in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Pharmaceuticals 15, 931 (2022).
Article CAS PubMed PubMed Central Google Scholar - Hoad, A., Spickett, G., Elliott, J. & Newton, J. Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome. QJM 101, 961–965 (2008).
Article CAS PubMed Google Scholar - Shaw, B. H. et al. The face of postural tachycardia syndrome – insights from a large cross‐sectional online community‐based survey. J. Intern. Med. 286, 438–448 (2019).
Article CAS PubMed PubMed Central Google Scholar - Raj, S. R. et al. Postural orthostatic tachycardia syndrome (POTS): priorities for POTS care and research from a 2019 National Institutes of Health expert consensus meeting - part 2. Auton. Neurosci. Basic. Clin. 235, 102836 (2021).
Article Google Scholar - Oaklander, A. L. et al. Peripheral neuropathy evaluations of patients with prolonged Long COVID. Neurol. Neuroimmunol. Neuroinflamm. 9, e1146 (2022).
Article PubMed PubMed Central Google Scholar - Larsen, N. W. et al. Characterization of autonomic symptom burden in long COVID: a global survey of 2,314 adults. Front. Neurol. 13, 1012668 (2022).
Article PubMed PubMed Central Google Scholar - Weinstock, L. B. et al. Mast cell activation symptoms are prevalent in Long-COVID. Int. J. Infect. Dis. 112, 217–226 (2021).
Article CAS PubMed PubMed Central Google Scholar - Boneva, R. S. et al. Endometriosis as a comorbid condition in chronic fatigue syndrome (CFS): secondary analysis of data from a CFS case-control study. Front. Pediatr. 7, 195 (2019).
Article PubMed PubMed Central Google Scholar - Bragée, B. et al. Signs of intracranial hypertension, hypermobility, and craniocervical obstructions in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Front. Neurol. 11, (2020).
- Medina-Perucha, L. et al. Self-reported menstrual alterations during the COVID-19 syndemic in Spain: a cross-sectional study. Int. J. Womens Health 14, 529–544 (2022).
Article CAS PubMed PubMed Central Google Scholar - Ding, T. et al. Analysis of ovarian injury associated with COVID-19 disease in reproductive-aged women in Wuhan, China: an observational study. Front. Med. 8, 635255 (2021).
Article Google Scholar - Sharp, G. C. et al. The COVID-19 pandemic and the menstrual cycle: research gaps and opportunities. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyab239 (2021).
Article PubMed PubMed Central Google Scholar - Khan, S. M. et al. SARS-CoV-2 infection and subsequent changes in the menstrual cycle among participants in the Arizona CoVHORT study. Am. J. Obstet. Gynecol. 226, 270–273 (2022).
Article CAS PubMed Google Scholar - Harlow, B. L., Signorello, L. B., Hall, J. E., Dailey, C. & Komaroff, A. L. Reproductive correlates of chronic fatigue syndrome. Am. J. Med. 105, 94S–99S (1998).
Article CAS PubMed Google Scholar - Thomas, N., Gurvich, C., Huang, K., Gooley, P. R. & Armstrong, C. W. The underlying sex differences in neuroendocrine adaptations relevant to myalgic encephalomyelitis chronic fatigue syndrome. Front. Neuroendocrinol. 66, 100995 (2022).
Article CAS PubMed Google Scholar - Boneva, R. S., Lin, J.-M. S. & Unger, E. R. Early menopause and other gynecologic risk indicators for chronic fatigue syndrome in women. Menopause 22, 826–834 (2015).
Article PubMed PubMed Central Google Scholar - Kresch, E. et al. COVID-19 endothelial dysfunction can cause erectile dysfunction: histopathological, immunohistochemical, and ultrastructural study of the human penis. World J. Mens Health 39, 466–469 (2021).
Article PubMed PubMed Central Google Scholar - Maleki, B. H. & Tartibian, B. COVID-19 and male reproductive function: a prospective, longitudinal cohort study. Reproduction 161, 319–331 (2021).
Article CAS Google Scholar - Yu, J. Z. et al. Lung perfusion disturbances in nonhospitalized post-COVID with dyspnea — a magnetic resonance imaging feasibility study. J. Intern. Med. 292, 941–956 (2022).
Article PubMed Google Scholar - Cho, J. L. et al. Quantitative chest CT assessment of small airways disease in post-acute SARS-CoV-2 infection. Radiology 304, 185–192 (2022).
Article PubMed Google Scholar - Vijayakumar, B. et al. Immuno-proteomic profiling reveals aberrant immune cell regulation in the airways of individuals with ongoing post-COVID-19 respiratory disease. Immunity 55, 542–556.e5 (2022).
Article CAS PubMed PubMed Central Google Scholar - Littlefield, K. M. et al. SARS-CoV-2-specific T cells associate with inflammation and reduced lung function in pulmonary post-acute sequalae of SARS-CoV-2. PLOS Pathog. 18, e1010359 (2022).
Article CAS PubMed PubMed Central Google Scholar - Meringer, H. & Mehandru, S. Gastrointestinal post-acute COVID-19 syndrome. Nat. Rev. Gastroenterol. Hepatol. 19, 345–346 (2022).
Article CAS PubMed PubMed Central Google Scholar - König, R. S. et al. The gut microbiome in myalgic encephalomyelitis (ME)/chronic fatigue syndrome (CFS). Front. Immunol. 12, 628741 (2022).
Article PubMed PubMed Central Google Scholar - Zuo, T. et al. Depicting SARS-CoV-2 faecal viral activity in association with gut microbiota composition in patients with COVID-19. Gut 70, 276–284 (2021).
CAS PubMed Google Scholar - Zollner, A. et al. Postacute COVID-19 is characterized by gut viral antigen persistence in inflammatory bowel diseases. Gastroenterology 163, 495–506.e8 (2022).
Google Scholar - Giron, L. B. et al. Markers of fungal translocation are elevated during post-acute sequelae of SARS-CoV-2 and induce NF-κB signaling. JCI Insight https://doi.org/10.1172/jci.insight.160989 (2022).
- Jason, L. A. et al. COVID-19 symptoms over time: comparing long-haulers to ME/CFS. Fatigue Biomed. Health Behav. 9, 59–68 (2021).
Article CAS Google Scholar - Tran, V.-T., Porcher, R., Pane, I. & Ravaud, P. Course of post COVID-19 disease symptoms over time in the ComPaRe long COVID prospective e-cohort. Nat. Commun. 13, 1812 (2022).
Article CAS PubMed PubMed Central Google Scholar - Walker, A., Kelly, C., Pottinger, G. & Hopkins, C. Parosmia — a common consequence of covid-19. BMJ 377, e069860 (2022).
Article PubMed Google Scholar - Jamal, S. M. et al. Prospective evaluation of autonomic dysfunction in post-acute sequela of COVID-19. J. Am. Coll. Cardiol. 79, 2325–2330 (2022).
Article PubMed PubMed Central Google Scholar - Stavileci, B., Özdemir, E., Özdemir, B., Ereren, E. & Cengiz, M. De-novo development of fragmented QRS during a six-month follow-up period in patients with COVID-19 disease and its cardiac effects. J. Electrocardiol. 72, 44–48 (2022).
Article PubMed PubMed Central Google Scholar - Grist, J. T. et al. Lung abnormalities depicted with hyperpolarized 129Xe MRI in patients with long COVID. Radiology 305, 709–717 (2022).
Article PubMed Google Scholar - US ME/CFS Clinician Coalition. Testing Recommendations for Suspected ME/CFS (US ME/CFS Clinician Coalition, 2021).
- Galán, M. et al. Persistent overactive cytotoxic immune response in a Spanish cohort of individuals with long-COVID: identification of diagnostic biomarkers. Front. Immunol. 13, 848886 (2022).
Article PubMed PubMed Central Google Scholar - Grandjean, D. et al. Screening for SARS-CoV-2 persistence in Long COVID patients using sniffer dogs and scents from axillary sweats samples. Clin. Trials 12, 2 (2022).
Google Scholar - Pifarré, F. et al. The use of oxygen as a possible screening biomarker for the diagnosis of chronic fatigue. Apunt. Sports Med 57, 100379 (2022).
Article Google Scholar - Jason, L. A., Kalns, J., Richarte, A., Katz, B. Z. & Torres, C. Saliva fatigue biomarker index as a marker for severe myalgic encephalomyelitis/chronic fatigue syndrome in a community based sample. Fatigue Biomed. Health Behav. 9, 189–195 (2021).
Article Google Scholar - Esfandyarpour, R., Kashi, A., Nemat-Gorgani, M., Wilhelmy, J. & Davis, R. W. A nanoelectronics-blood-based diagnostic biomarker for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Proc. Natl Acad. Sci. USA 116, 10250–10257 (2019).
Article CAS PubMed PubMed Central Google Scholar - Nkiliza, A. et al. Sex-specific plasma lipid profiles of ME/CFS patients and their association with pain, fatigue, and cognitive symptoms. J. Transl Med. 19, 370 (2021).
Article CAS PubMed PubMed Central Google Scholar - Bolton, M. J., Chapman, B. P. & Van Marwijk, H. Low-dose naltrexone as a treatment for chronic fatigue syndrome. BMJ Case Rep. 13, e232502 (2020).
Article PubMed PubMed Central Google Scholar - Pitt, B., Tate, A. M., Gluck, D., Rosenson, R. S. & Goonewardena, S. N. Repurposing low-dose naltrexone (LDN) for the prevention and treatment of immunothrombosis in COVID-19. Eur. Heart J. Cardiovasc. Pharmacother. https://doi.org/10.1093/ehjcvp/pvac014 (2022).
Article PubMed PubMed Central Google Scholar - Alper, K. Case report: famotidine for neuropsychiatric symptoms in COVID-19. Front. Med. 7, 614393 (2020).
Article Google Scholar - Hohberger, B. et al. Case report: neutralization of autoantibodies targeting G-protein-coupled receptors improves capillary impairment and fatigue symptoms after COVID-19 infection. Front. Med. 8, 754667 (2021).
Article Google Scholar - Wang, C. et al. Long COVID: the nature of thrombotic sequelae determines the necessity of early anticoagulation. Front. Cell. Infect. Microbiol. 12, 861703 (2022).
Article CAS PubMed PubMed Central Google Scholar - The ME Association. A new treatment for Long Covid? The ME Association https://meassociation.org.uk/2021/10/a-new-treatment-for-long-covid/ (2021).
- Tölle, M. et al. Myalgic encephalomyelitis/chronic fatigue syndrome: efficacy of repeat immunoadsorption. J. Clin. Med. 9, E2443 (2020).
Article Google Scholar - Wood, E., Hall, K. H. & Tate, W. Role of mitochondria, oxidative stress and the response to antioxidants in myalgic encephalomyelitis/chronic fatigue syndrome: a possible approach to SARS-CoV-2 ‘long-haulers’? Chronic Dis. Transl Med. 7, 14–26 (2020).
PubMed PubMed Central Google Scholar - NICE. Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management. NICE https://www.nice.org.uk/guidance/NG206 (2021).
- World Health Organization. Support for Rehabilitation Self-Management After COVID-19 Related Illness (WHO, 2021).
- CDC. Treatment of ME/CFS | Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). CDC https://www.cdc.gov/me-cfs/treatment/index.html (2021).
- Long COVID Physio. Exercise. Long COVID Physio https://longcovid.physio/exercise (2022).
- Geng, L. N., Bonilla, H. F., Shafer, R. W., Miglis, M. G. & Yang, P. C. Case report of breakthrough long COVID and the use of nirmatrelvir-ritonavir. Preprint at https://www.researchsquare.com/article/rs-1443341/v1 (2022).
- Xie, Y., Choi, T. & Al-Aly, Z. Nirmatrelvir and the risk of post-acute sequelae of COVID-19. Preprint at medRxiv https://doi.org/10.1101/2022.11.03.22281783 (2022).
- Charfeddine, S. et al. Sulodexide in the treatment of patients with long COVID 19 symptoms and endothelial dysfunction: the results of TUN-EndCOV study. Arch. Cardiovasc. Dis. Suppl. 14, 127 (2022).
Google Scholar - Thomas, R. et al. A randomised, double-blind, placebo-controlled trial evaluating concentrated phytochemical-rich nutritional capsule in addition to a probiotic capsule on clinical outcomes among individuals with COVID-19 — the UK Phyto-V study. COVID 2, 433–449 (2022).
Article CAS Google Scholar - Zhang, L. et al. Gut microbiota-derived synbiotic formula (SIM01) as a novel adjuvant therapy for COVID-19: an open-label pilot study. J. Gastroenterol. Hepatol. 37, 823–831 (2022).
Article CAS PubMed PubMed Central Google Scholar - Liu, L. D. & Duricka, D. L. Stellate ganglion block reduces symptoms of Long COVID: a case series. J. Neuroimmunol. 362, 577784 (2022).
Article CAS PubMed Google Scholar - Belcaro, G. et al. Preventive effects of Pycnogenol® on cardiovascular risk factors (including endothelial function) and microcirculation in subjects recovering from coronavirus disease 2019 (COVID-19). Minerva Med. 113, 300–308 (2022).
Article PubMed Google Scholar - Crooks, V., Waller, S., Smith, T. & Hahn, T. J. The use of the Karnofsky Performance Scale in determining outcomes and risk in geriatric outpatients. J. Gerontol. 46, M139–M144 (1991).
Article CAS PubMed Google Scholar - Ledford, H. Long-COVID treatments: why the world is still waiting. Nature 608, 258–260 (2022).
Article CAS PubMed Google Scholar - Toogood, P. L., Clauw, D. J., Phadke, S. & Hoffman, D. Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): where will the drugs come from? Pharmacol. Res. 165, 105465 (2021).
Article CAS PubMed Google Scholar - US ME/CFS Clinician Coalition. ME/CFS Treatment Recommendations (US ME/CFS Clinician Coalition, 2021).
- Taquet, M., Dercon, Q. & Harrison, P. J. Six-month sequelae of post-vaccination SARS-CoV-2 infection: a retrospective cohort study of 10,024 breakthrough infections. Brain Behav. Immun. 103, 154–162 (2022).
Article CAS PubMed PubMed Central Google Scholar - Office for National Statistics. Self-reported long COVID after infection with the Omicron variant in the UK: 6 May 2022. Office for National Statistics https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/selfreportedlongcovidafterinfectionwiththeomicronvariant/6may2022 (2022).
- Tsuchida, T. et al. Relationship between changes in symptoms and antibody titers after a single vaccination in patients with Long COVID. J. Med. Virol. 94, 3416–3420 (2022).
Article CAS PubMed PubMed Central Google Scholar - VA COVID-19 Observational Research Collaboratory. Burden of PCR-confirmed SARS-CoV-2 reinfection in the U.S. Veterans Administration, March 2020 – January 2022. Preprint at medRxiv https://doi.org/10.1101/2022.03.20.22272571 (2022).
- Bowe, B., Xie, Y. & Al-Aly, Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat. Med. https://doi.org/10.1038/s41591-022-02051-3 (2022).
- Blomberg, J., Gottfries, C.-G., Elfaitouri, A., Rizwan, M. & Rosén, A. Infection elicited autoimmunity and myalgic encephalomyelitis/chronic fatigue syndrome: an explanatory model. Front. Immunol. 9, 229 (2018).
Article PubMed PubMed Central Google Scholar - Cauchemez, S. & Bosetti, P. A reconstruction of early cryptic COVID spread. Nature 600, 40–41 (2021).
Article CAS PubMed Google Scholar - CDC. Estimated COVID-19 burden. Centers for Disease Control and Prevention https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html (2020).
- Kucirka, L. M., Lauer, S. A., Laeyendecker, O., Boon, D. & Lessler, J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Ann. Intern. Med. 173, 262–267 (2020).
Article PubMed Google Scholar - Levine-Tiefenbrun, M. et al. SARS-CoV-2 RT-qPCR test detection rates are associated with patient age, sex, and time since diagnosis. J. Mol. Diagn. 24, 112–119 (2022).
Article CAS PubMed Google Scholar - Jarvis, K. F. & Kelley, J. B. Temporal dynamics of viral load and false negative rate influence the levels of testing necessary to combat COVID-19 spread. Sci. Rep. 11, 9221 (2021).
Article CAS PubMed PubMed Central Google Scholar - Dattner, I. et al. The role of children in the spread of COVID-19: using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. PLoS Comput. Biol. 17, e1008559 (2021).
Article CAS PubMed PubMed Central Google Scholar - Langeland, N. & Cox, R. J. Are low SARS-CoV-2 viral loads in infected children missed by RT-PCR testing? Lancet Reg. Health Eur. 5, 100138 (2021).
Article PubMed PubMed Central Google Scholar - Van Elslande, J. et al. Longitudinal follow-up of IgG anti-nucleocapsid antibodies in SARS-CoV-2 infected patients up to eight months after infection. J. Clin. Virol. 136, 104765 (2021).
Article PubMed PubMed Central Google Scholar - Liu, W. et al. Predictors of nonseroconversion after SARS-CoV-2 infection. Emerg. Infect. Dis. 27, 2454–2458 (2021).
Article CAS PubMed PubMed Central Google Scholar - Toh, Z. Q. et al. Comparison of seroconversion in children and adults with mild COVID-19. JAMA Netw. Open 5, e221313 (2022).
Google Scholar - Peterson, T. M., Peterson, T. W., Emerson, S., Meredyth, A. Evans, E. R. & Jason, L. A. Coverage of CFS within U.S. medical schools. Univers. J. Public Health 1, 177–179 (2013).
Article Google Scholar - Rowe, P. C. et al. Orthostatic intolerance and chronic fatigue syndrome associated with Ehlers-Danlos syndrome. J. Pediatr. 135, 494–499 (1999).
Article CAS PubMed Google Scholar - Nguyen, T. et al. Novel characterisation of mast cell phenotypes from peripheral blood mononuclear cells in chronic fatigue syndrome/myalgic encephalomyelitis patients. Asian Pac. J. Allergy Immunol. 35, 75–81 (2017).
CAS PubMed Google Scholar - Wagner, C., Isenmann, S., Ringendahl, H. & Haensch, C.-A. Anxiety in patients with postural tachycardia syndrome (POTS). Fortschr. Neurol. Psychiatr. 80, 458–462 (2012).
CAS PubMed Google Scholar - Grayson, D. A., Mackinnon, A., Jorm, A. F., Creasey, H. & Broe, G. A. Item bias in the center for epidemiologic studies depression scale: effects of physical disorders and disability in an elderly community sample. J. Gerontol. Ser. B 55, P273–P282 (2000).
Article CAS Google Scholar - Twisk, F. N. M. & Maes, M. A review on cognitive behavorial therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME) / chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients with ME/CFS. Neuro Endocrinol. Lett. 30, 284–299 (2009).
PubMed Google Scholar - Vink, M. & Vink-Niese, F. Is it useful to question the recovery behaviour of patients with ME/CFS or Long COVID? Healthcare 10, 392 (2022).
Article PubMed PubMed Central Google Scholar - Dysautonomia International. What is dysautonomia? Dysautonomia International http://www.dysautonomiainternational.org/page.php?ID=34 (2022).
- CDC. Epidemiology | Presentation and clinical course | Healthcare providers | Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). CDC https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/epidemiology.html (2021).
- Sørensen, A. I. V. et al. A nationwide questionnaire study of post-acute symptoms and health problems after SARS-CoV-2 infection in Denmark. Nat. Commun. 13, 4213 (2022).
Article PubMed PubMed Central Google Scholar - Berg, S. K. et al. Long COVID symptoms in SARS-CoV-2-positive children aged 0–14 years and matched controls in Denmark (LongCOVIDKidsDK): a national, cross-sectional study. Lancet Child Adolesc. Health 6, 614–623 (2022).
Article Google Scholar - Morrow, A. K. et al. Long-term COVID 19 sequelae in adolescents: the overlap with orthostatic intolerance and ME/CFS. Curr. Pediatr. Rep. 10, 31–44 (2022).
Article PubMed PubMed Central Google Scholar - Cooper, S. et al. Long COVID-19 liver manifestation in children. J. Pediatr. Gastroenterol. Nutr. https://doi.org/10.1097/MPG.0000000000003521 (2022).
Article PubMed PubMed Central Google Scholar - Kompaniyets, L. Post–COVID-19 symptoms and conditions among children and adolescents — United States, March 1, 2020–January 31, 2022. MMWR Morb. Mortal. Wkly Rep. 71, 993–999 (2022).
Article PubMed PubMed Central Google Scholar - Edlow, A. G., Castro, V. M., Shook, L. L., Kaimal, A. J. & Perlis, R. H. Neurodevelopmental outcomes at 1 year in infants of mothers who tested positive for SARS-CoV-2 during pregnancy. JAMA Netw. Open 5, e2215787 (2022).
Article PubMed PubMed Central Google Scholar - Morand, A. et al. Similar patterns of [18F]-FDG brain PET hypometabolism in paediatric and adult patients with long COVID: a paediatric case series. Eur. J. Nucl. Med. Mol. Imaging 49, 913–920 (2022).
Article CAS PubMed Google Scholar - Heiss, R. et al. Pulmonary dysfunction after pediatric COVID-19. Radiology https://doi.org/10.1148/radiol.221250 (2022).
Article PubMed Google Scholar
Acknowledgements
We would like to thank the long COVID and associated conditions patient and research community and the entire team at Patient-Led Research Collaborative. E.J.T. was supported by National Center for Advancing Translational Sciences (NCATS) grant UL1TR002550.
Author information
Authors and Affiliations
- Patient-Led Research Collaborative, New York, NY, USA
Hannah E. Davis - Patient-Led Research Collaborative, Oakland, CA, USA
Lisa McCorkell - Scripps Research Translational Institute, Scripps Research, La Jolla, CA, USA
Julia Moore Vogel & Eric J. Topol
Authors
- Hannah E. Davis
You can also search for this author inPubMed Google Scholar - Lisa McCorkell
You can also search for this author inPubMed Google Scholar - Julia Moore Vogel
You can also search for this author inPubMed Google Scholar - Eric J. Topol
You can also search for this author inPubMed Google Scholar
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Correspondence toEric J. Topol.
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Akiko Iwasaki, Ziyad Al-Aly and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Davis, H.E., McCorkell, L., Vogel, J.M. et al. Long COVID: major findings, mechanisms and recommendations.Nat Rev Microbiol 21, 133–146 (2023). https://doi.org/10.1038/s41579-022-00846-2
- Accepted: 05 December 2022
- Published: 13 January 2023
- Issue Date: March 2023
- DOI: https://doi.org/10.1038/s41579-022-00846-2