Atrial fibrillation and the risk of myocardial infarction: a nation-wide propensity-matched study (original) (raw)
Introduction
The significance of atrial fibrillation (AF) as a major public health problem comes from its increasing prevalence and strong association with morbidity and mortality1,2. Patients with AF have 5 times the risk of stroke and double the risk of mortality compared with those without AF3,4. AF has known to complicate acute myocardial infarction (MI)5. In addition to being an established complicating factor for MI, recent studies have revealed that AF increased the risk of MI6,7. In the Atherosclerosis Risk in Communities (ARIC) study, AF was associated with an increased risk of non-ST segment elevation MI (NSTEMI)6. In a recent study performed by Soliman et al.7, AF was associated with a 70% increased risk of incident MI. However, these results are yet to be validated in a nationwide population based cohort and the mechanisms explaining these associations are not fully understood.
Thus, we examined the association between AF and MI by analyzing a recently developed Korean National Health Insurance Service–national sample cohort (NHIS-NSC) database, which includes over five hundred thousand individuals. In addition, the beneficial effects of the commonly prescribed medications for AF patients on the occurrence of MI have not been elucidated. Herein, we also analyzed the association of medications with incident MI in AF patients.
Methods
Source of study data
The national health insurance service (NHIS) in Korea is a single-payer program and is mandatory for all residents in South Korea. This retrospective study used the NHIS-NSC 2002–2013 dataset, comprising a random sample of 1,025,340 subjects, which amounted to 2.2% of the entire Korean population in the NHIS in 2002 (46,605,433). Data were produced by the NHIS using a systematic sampling method for the purpose of research. Random sampling was used based on 1,476 strata8. As all individuals in South Korea are enrolled in the NHIS, this database represents the entire Korean population9. This is a semi-dynamic cohort database; the cohort has been followed up to either the time of the participant’s disqualification of health services due to death or emigration or the end of the study period. The database contains eligibility and demographic information regarding health insurance and medical aid beneficiaries, medical bill details, diagnostic codes, medical treatment, disease histories, prescription drug used, and personal information for inpatients and outpatient visits.
In this cohort, the subjects’ disease information was classified according to the 10th revision of the International Classification of Diseases (ICD-10) codes obtained from the Korean National Statistical Office (Supplementary Table S1). This study was approved by the Institutional Review Board (IRB) of Yonsei University College of Medicine in Seoul, Korea. The IRB waived the requirement to obtain informed consent, and this study was conducted in accordance with the tenets of the Declaration of Helsinki.
Study population
A total of 506,805 patients, who had a health check-up between 2009 and 2013, were enrolled and follow-up data were reviewed until December 2013. AF cases were identified by ICD-10 codes (ICD-10: I48)10. To ensure accuracy of diagnosis, we defined patients as AF only when it was a discharge diagnosis or was confirmed more than twice in the outpatient department. To further evaluate the accuracy of the definition of AF, a validation study was performed in 628 randomly selected patients with ICD-10 code of I48 in 2 separate hospitals. Their electrocardiograms (ECGs) were reviewed by two physicians. Patients were determined to have AF if documented by ECG. The positive predictive value was 94.1%. The clinical end point was the first occurrence of MI during follow up. MI cases were identified by ICD-10 codes of I21or I22, and were ascertained when the diagnosis was confirmed by hospitalization or death from MI. To evaluate the accuracy of our definition of MI, we conducted a validation study with medical records of two independent tertiary hospitals from 2006–2013. A total of 4,688 patients were found to have ICD codes of I21 or I22. Data of clinical history, cardiac biomarkers, ECGs and the results of coronary angiography were reviewed by two cardiologists. The positive predictive value was 86.5%.
Medical records of all patients were reviewed from 2002 till 2013 in order to clarify the newly diagnosed AF and MI during the study period. The laboratory and survey questionnaire data of general and life-transition health examinations for all cohort members were merged.
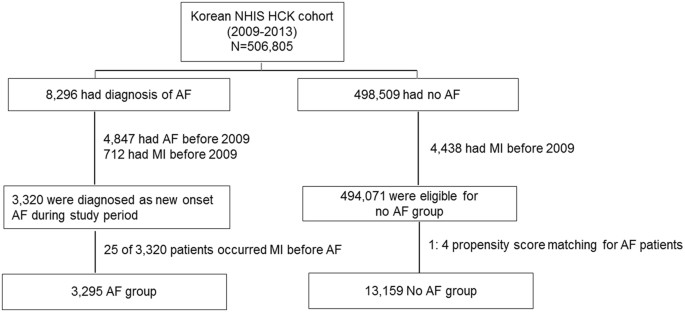
Of the 8,296 patients with AF, patients who had AF or MI before 2009 (n = 4,976) and who suffered an MI before AF (n = 25) were excluded. Finally 3,295 patients were enrolled in the AF group. Among those without AF (n = 498,509), 494,071 patients were enrolled in the no-AF group after excluding the patients who suffered an MI before 2009 (n = 4,438). Given the differences in the baseline characteristics and the risk of cardiovascular diseases between the AF and control groups, we used 1:4 propensity score matching and calculated the propensity score, with predicted probability of AF occurrence conditional on baseline covariates, by multivariable logistic regression (Table 1)11. We attempted to match each patient in the AF cohort with a patient in the control cohort with a similar propensity score, based on nearest-neighbor matching without replacement, using a caliper width equal to 0.05 of the standard deviation of the logit of the propensity score. Pre- and post-match absolute standardized differences were presented as Love Plots12.
Table 1 Baseline characteristics by AF status before and after propensity score matching
The following variables were entered: age, sex, and a history of congestive heart failure, hypertension, diabetes mellitus, chronic kidney disease (CKD) or end-stage renal disease (ESRD), dyslipidemia, ischemic stroke, peripheral artery occlusive disease (PAOD), chronic obstructive pulmonary disease (COPD), history of malignancy, anemia, smoking history, blood pressure, body mass index, waist circumference, body surface area, cholesterol level, serum creatinine, and estimated –glomerular filtration rate (eGFR). Covariates included in propensity matching were the data from baseline examination at the time of health check-up, and the definitions of comorbidities were based on ICD codes. The matching procedure was performed using R packages (R Foundation for Statistical Computing, Vienna, Austria), including Matchit, RItools, and CEM13. Finally, a total of 3,295 AF patients and 13,159 no-AF patients were evaluated in this study (Fig. 1).
Figure 1
Study population. NHIS HCK, National Health Insurance Service-health check-up; AF, atrial fibrillation; MI, myocardial infarction.
Statistical analysis
Data were presented as mean ± SD for normally distributed continuous variables and as proportions for categorical variables. Age-adjusted incidence rate of MI per 1000 person-years in patients with and without AF was calculated in the propensity matched population and in the sex subgroup. Person-time for the incidence rate in the AF group was calculated from AF diagnosis to the occurrence of MI or censoring. In the no-AF group, person-time was calculated from baseline to MI occurrence or censoring. Cumulative incidence of MI was plotted using a Kaplan-Meier method, with statistical significance examined using log-rank test by AF status. The risk of MI was assessed using Cox regression analysis. Statistical analysis was performed using SPSS 21.0 statistical software (SPSS Inc., Chicago, IL, USA). All p-values were two tailed, and values less than 0.05 were considered statistically significant.
Results
Baseline characteristics
The mean age of matched patients was 63 years (range, 19–98 years) and 58% of the patients were male. Table 1 shows the baseline characteristics of the study population stratified by AF status. In the full pre-match cohort, patients with AF were older, had a higher body mass index, a higher prevalence of heart failure (HF), hypertension, diabetes, CKD or ESRD, dyslipidemia, ischemic stroke, PAOD, and COPD (all P < 0.001). Mean CHA2DS2-VASc score was 2.6 ± 1.9 in the AF group and 1.2 ± 1.3 in the no-AF group (P < 0.001). Covariates with significant imbalances in the pre-matched cohort which were well balanced after propensity matching are displayed in Table 1. Absolute standardized differences in all measured covariates were less than 5%, suggesting substantial covariate balance across the groups (Supplementary Fig. S1).
Aspirin, anticoagulants, statin, digoxin, beta blocking agent (BB), and calcium channel blocker (CCB) were more frequently prescribed in the AF group than in the no-AF group; aspirin (50.3% vs. 27.5%, P < 0.001), anticoagulant (20.9% vs. 0.3%, P < 0.001), statin (38.2% vs. 28.5%, P < 0.001), digoxin (13.4% vs. 0.9%, P < 0.001), BB (43.1% vs.16.1%, P < 0.001), and CCB (11.4% vs. 2.5%, P < 0.001).
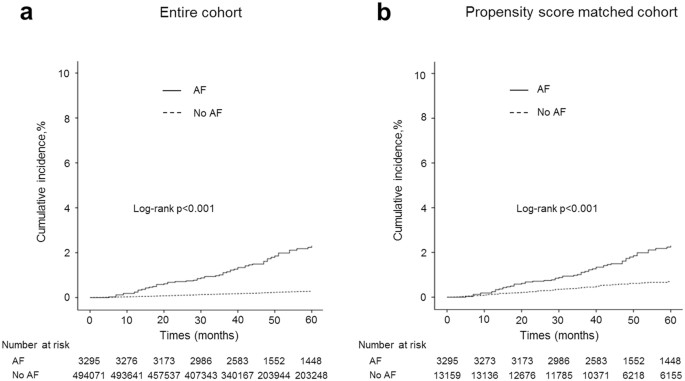
AF and the risk of MI
Over 4.2 years of follow up, 137 incident MI events occurred. Figure 2 shows the unadjusted cumulative incidence of MI stratified by baseline AF status in the entire cohort (Fig. 2a) and the matched cohort (Fig. 2b). Patients with AF had a higher incidence of MI than those without AF in both the entire cohort and the matched cohort (log rank p < 0.001 for both cohorts).
Figure 2
Unadjusted cumulative incidence of myocardial infarction by baseline atrial fibrillation status in the entire cohort (a) and in the propensity scored matched cohort (b). Cumulative incidence was calculated using Kaplan-Meier estimates and compared using the log-rank test.
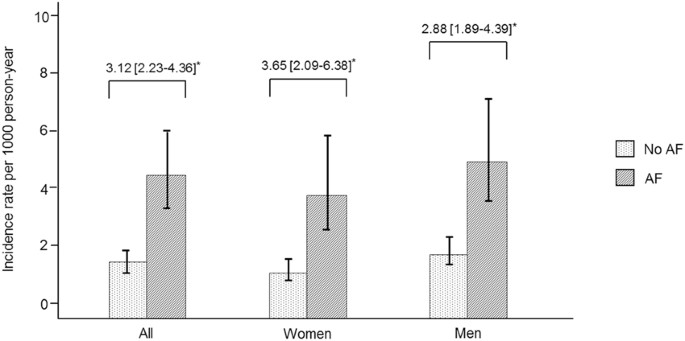
The age-adjusted incidence rate of MI among participants was higher in those with AF than in those without AF (4.42 vs 1.42 per 1000 person-years), with an incidence rate ratio (IRR) of 3.12 [95% CI, 2.23–4.36]. In a sex stratified analysis, the higher age-adjusted MI IRRs by AF status was observed in women (IRR, 3.65; 95% CI, 2.09–6.38) compared with men (IRR, 2.88; 95% CI, 1.89–4.39) (Fig. 3).
Figure 3
Age-adjusted incidence rate and incidence rate ratios of myocardial infarction by atrial fibrillation status. Incidence rate per 1,000 person-years. *Age adjusted incidence rate and incidence rate ratios were based on the average of the cohort.
In a Cox proportional hazards model of the matched cohort, AF [Hazard ratio (HR), 3.12; 95% CI, 2.23–4.37, p < 0.001] was an independent risk factor for MI. Other risk factors were hypertension (HR, 1.87; 95% CI, 1.30–2.69, p < 0.001), diabetes (HR, 1.79; 95% CI, 1.28–2.51, p < 0.001), HF (HR, 2.04; 95% CI, 1.32–3.14, p = 0.003), CKD or ESRD (HR, 2.70; 95% CI, 1.90–3.85, p < 0.001) and dyslipidemia (HR, 1.45; 95% CI, 1.04–2.03, p = 0.031) (Table 2).
Table 2 The independent clinical predictors of myocardial infarction in propensity score matched cohort.
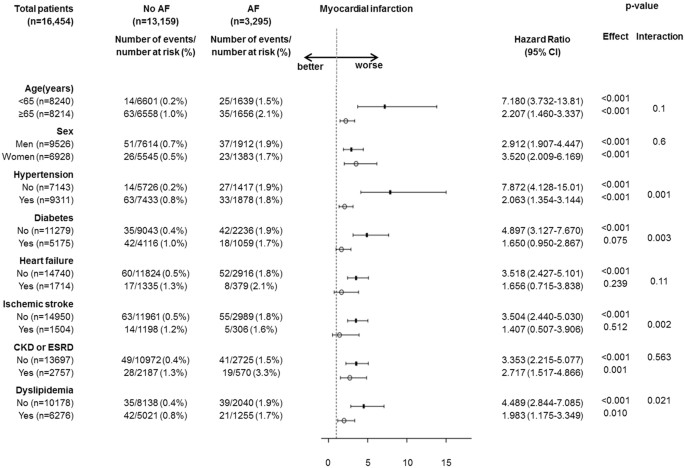
Association of AF with MI in subgroups
The associations of AF with MI among various subgroups of patients are displayed in Fig. 4. The risk of hospitalization or death due to MI was significantly higher in the AF group than in the no-AF group, regardless of age (p for interaction = 0.1), sex (p for interaction = 0.6), comorbidities with HF (p for interaction = 0.11), and CKD or ESRD (p for interaction = 0.56) at baseline. On the other hand, we found that the risk of AF associated incident MI was higher in patients free of hypertension [HR, 7.87 (95% CI, 4.13–15.0) vs. 2.06 (95% CI, 1.35–3.14), p for interaction = 0.001], diabetes [HR, 4.89 (95% CI, 3.13–7.67) vs. 1.66 (95% CI, 0.72–3.84), p for interaction = 0.003], ischemic stroke [HR, 3.50 (95% CI, 2.44–5.03) vs. 1.407 (95% CI, 0.51–3.91), p for interaction = 0.002], and dyslipidemia [HR, 4.49 (95% CI, 2.84–7.09) vs. 1.98 (95% CI, 1.18–3.35), p for interaction = 0.021] at baseline.
Figure 4
Effects of atrial fibrillation on the risk of myocardial infarction in different groups of patients. CI, confidence interval. Hazard ratios were calculated based on Cox regression after propensity matching. The P for interaction was calculated using the interaction term for AF and each subgroup based on Cox regression.
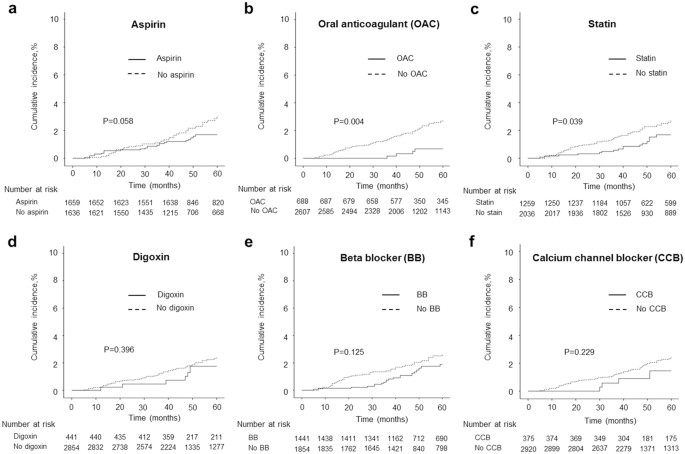
Risk of MI in association with medications in AF patients
Medications analyzed in this study were aspirin, anticoagulants, statin, digoxin, BB and CCB. Anticoagulants included in the analysis were warfarin, direct thrombin inhibitor and factor Xa inhibitors. Pharmacological treatment was ascertained when there were at least 90 days or more prescriptions were prescribed after the incident diagnosis of AF.
Figure 5 shows the effect of each medication on the occurrence of MI in AF patients. Anticoagulants were prescribed in 688 of the 3,295 AF patients without gender difference in prescription rate (men, 21.1% vs. women, 20.6%, p = 0.76). AF associated incident MI occurred less in patients on anticoagulant (0.6% vs. 2.1%, p = 0.004). Statins were prescribed in 1,259 of the 3,295 AF patients and prescription rate was higher in women than in men (men, 34.1% vs. women, 43.9%, p < 0.001). AF associated incident MI was less in patients on statin therapy (1.3% vs. 2.2%, p = 0.05). Cumulative incidence of MI was lower in patients who were taking an anticoagulant (Fig. 5b, p = 0.004) and statin (Fig. 5c, p = 0.039). Aspirin users showed a similar trend, which did not reach statistical significance (Fig. 5a, p = 0.058). The most commonly prescribed rate control agent was BB, followed by digoxin and CCB. AF-associated MI events did not differ between patients who were taking digoxin (Fig. 5d), BB (Fig. 5e), and CCB (Fig. 5f) and those who were not taking these medications. Overall death, regardless of the mode of death, occurred more often in patients with MI than in those without MI during the follow up period (35.8% vs 4.6%, p < 0.001).
Figure 5
Risk of incident myocardial infarction associated with medication in patients with atrial fibrillation. The cumulative incidences of myocardial infarction were calculated using Kaplan-Meier estimates and compared using the log-rank test.
Discussion
In this study from NHIS, our principal findings are as follows: (1) AF was significantly associated with increased risk of incident MI. (2) Association between AF and the risk of MI did not differ by sex. (3) The risk of AF associated incident MI was higher in patients free of hypertension, diabetes, ischemic stroke, and dyslipidemia. (4) The incidence of AF associated incident MI was lower in patients on anticoagulant and statin therapies.
In this study, AF was associated with 3-fold increased risk of MI, even after the risk factors and potential confounders for MI were included in the matching. These findings were in accordance with the recently reported several studies which showed AF as an independent risk factor for MI6,7,14,15.
Contrary to recent studies which showed gender difference in the association between AF and MI6,7,15, it were not observed in this study. Previously, it was reported that women were less likely to receive warfarin than men16,17 and this may be the possible explanation for gender difference of MI14. However, in our study, use of anticoagulant did not differ between sex and this, in part, may contribute to the similar risk of MI between men and women.
Notably, we confirmed that the risk of MI was significantly higher in patients with AF free of overt cardiovascular disease than in subjects without AF. Previous study from Olmsted County revealed that lone AF had a comparable risk of embolic events and mortality to the general population18,19. In contrast, recent studies showed that patients with AF without cardiovascular co-morbidities had an increased risk of cardiovascular events and mortality15,20. These interactions suggest that shared underlying risk factors are not the only mechanisms explaining the association between AF and MI. There are plausible explanations for why AF patients with less co-morbidity were predisposed to MI. In patients with established risk factors for MI, AF may contribute less to the occurrence to MI, compared with those who were previously healthy. In our study, anticoagulants showed beneficial effect against AF associated incident MI. Accordingly, embolic events to coronary arteries are another possible explanation. Statin use, and also, is higher in patients with cardiovascular diseases, which may decrease the incident MI. Further study is needed in this regard.
In this analysis stratified by medications after AF diagnosis, the risk of incident MI was less in anticoagulant users. Previously, it was reported that warfarin might have a protective effect against MI21. Prevention of thrombus formation with anticoagulation, in part, might be an explanation. In our study, the anticoagulants analyzed were direct thrombin inhibitor, factor Xa inhibitors, as well as warfarin, and whether the new oral anticoagulants could have a role in preventing MI in the setting of AF needs to be further investigated.
Clinical trials have already demonstrated a clear beneficial effect of statin for prevention of ischemic heart disease22,23. In accordance with these studies, this study revealed that the risk of AF associated incident MI was less in statin users than in non-users. In a study, association between AF and inflammation has been reported24. The role of inflammation in MI has already been established25. Anti-inflammatory and anti-thrombotic activities of statin may reduce the risk of AF associated incident MI.
Type 2 MI can occur due to poorly controlled ventricular response in AF patients26. The rate control strategy in AF patients is expected to reduce the occurrence of type 2 MI, by reducing the oxygen demand and by increasing the diastolic filling time of coronary arteries. However, the result of this study was not in accordance with this common belief, suggesting that type 2 MI is less likely to be the main mechanism by which AF leads to MI.
Considering MI as a known risk factor for AF27, this result suggests a bidirectional relationship between AF and MI. However, the pathophysiology of AF associated incident MI is complex and incompletely understood. Further research to determine the underlying mechanism with the association of AF and MI is warranted. The prevalence of AF doubles with each additional decade of life28. With an increasing older population, the occurrence of AF itself and AF-associated morbidity and mortality is expected to increase as well. From a preventive perspective, the notion should suggest that AF potentiates the risk of MI.
Limitations
There are several limitations to this study. Although we ascertained AF cases with ECGs as well as ICD codes, it is possible that paroxysmal or asymptomatic AF cases were not detected. Also, we could not analyze paroxysmal, persistent and permanent AF separately. Second, because MI cases were identified by ICD-10 code, data for cardiac markers, ECGs, and coronary angiography were not available, which could have provided further information about the type of MI26. We could not analyze the association of AF with different types of MI. Third, even though the NHIS recommends biennial health check-up to all health insurance subscribers, it is not compulsory and there is a possibility that healthier and more educated subjects could have participated in this study. Fourth, potentially uncontrolled covariates may exist because comorbidities included in propensity matching are the data from baseline examination. They may be absent at baseline, but may have developed during the follow-up. Fifth, similar to other studies, considerable confounders may remain although propensity-score matching was well balanced. Despite the limitations, this study is the nation-wide population based observational studies providing the further evidence for a link between AF and MI, and the effects of medications on the occurrence of AF related incident MI.
Conclusions
AF is associated with an increased risk of MI in the nationwide cohort study of Korean population. The association between AF and MI did not differ by sex and higher in patients free of cardiovascular diseases at baseline. Anticoagulants and statin showed beneficial effects against MI in AF patients. Our finding suggests that AF complications beyond stroke should extend to total mortality to include MI.
References
- Miyasaka, Y. et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 114, 119–125 (2006).
Article PubMed Google Scholar - Go, A. S. et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 285, 2370–2375 (2001).
Article CAS PubMed Google Scholar - Conen, D. et al. Risk of death and cardiovascular events in initially healthy women with new-onset atrial fibrillation. JAMA. 305, 2080–2087 (2011).
Article CAS PubMed PubMed Central Google Scholar - Miyasaka, Y. et al. Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-based study. J Am Coll Cardiol. 49, 986–992 (2007).
Article PubMed Google Scholar - Hod, H. et al. Early atrial fibrillation during evolving myocardial infarction: a consequence of impaired left atrial perfusion. Circulation. 75, 146–150 (1987).
Article CAS PubMed Google Scholar - Soliman, E. Z. et al. Atrial Fibrillation and Risk of ST-Segment-Elevation Versus Non-ST-Segment-Elevation Myocardial Infarction: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 131, 1843–1850 (2015).
Article PubMed PubMed Central Google Scholar - Soliman, E. Z. et al. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med. 174, 107–114 (2014).
Article PubMed PubMed Central Google Scholar - Lee, J., Lee, J. S., Park, S. H., Shin, S. A. & Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol (2016).
- Song, S. O. et al. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab J. 38, 395–403 (2014).
Article PubMed PubMed Central Google Scholar - Chao, T. F. et al. Age Threshold for Increased Stroke Risk Among Patients With Atrial Fibrillation: A Nationwide Cohort Study From Taiwan. J Am Coll Cardiol. 66, 1339–1347 (2015).
Article PubMed Google Scholar - Rubin, D. B. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 127, 757–763 (1997).
Article CAS PubMed Google Scholar - Ahmed, A. et al. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 27, 1431–1439 (2006).
Article PubMed PubMed Central Google Scholar - Ho, D. E., Imai, K., King, G. & Stuart, E. A. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political analysis. 15, 199–236 (2007).
Article Google Scholar - Guo, X. Y. et al. Atrial fibrillation is associated with an increased risk of myocardial infarction: Insights from a meta-analysis. Atherosclerosis. 254, 1–7 (2016).
Article CAS PubMed Google Scholar - Chao, T. F. et al. Acute myocardial infarction in patients with atrial fibrillation with a CHA2DS2-VASc score of 0 or 1: a nationwide cohort study. Heart Rhythm. 11, 1941–1947 (2014).
Article PubMed Google Scholar - Niska, R. & Han, B. Anticoagulation for patients with atrial fibrillation in ambulatory care settings. J Am Board Fam Med. 22, 299–306 (2009).
Article PubMed Google Scholar - Gorin, L. et al. Prognosis and guideline-adherent antithrombotic treatment in patients with atrial fibrillation and atrial flutter: implications of undertreatment and overtreatment in real-life clinical practice; the Loire Valley Atrial Fibrillation Project. Chest. 140, 911–917 (2011).
Article PubMed Google Scholar - Kopecky, S. L. et al. The natural history of lone atrial fibrillation. A population-based study over three decades. N Engl J Med. 317, 669–674 (1987).
Article CAS PubMed Google Scholar - Jahangir, A. et al. Long-term progression and outcomes with aging in patients with lone atrial fibrillation: a 30-year follow-up study. Circulation. 115, 3050–3056 (2007).
Article PubMed Google Scholar - Brand, F. N., Abbott, R. D., Kannel, W. B. & Wolf, P. A. Characteristics and prognosis of lone atrial fibrillation. 30-year follow-up in the Framingham Study. JAMA. 254, 3449–3453 (1985).
Article CAS PubMed Google Scholar - Lip, G. Y. & Lane, D. A. Does warfarin for stroke thromboprophylaxis protect against MI in atrial fibrillation patients? Am J Med. 123, 785–789 (2010).
Article CAS PubMed Google Scholar - Sacks, F. M. et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 335, 1001–1009 (1996).
Article CAS PubMed Google Scholar - Downs, J. R. et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 279, 1615–1622 (1998).
Article CAS PubMed Google Scholar - Patel, P., Dokainish, H., Tsai, P. & Lakkis, N. Update on the association of inflammation and atrial fibrillation. J Cardiovasc Electrophysiol. 21, 1064–1070 (2010).
Article PubMed Google Scholar - Shah, P. K. Mechanisms of plaque vulnerability and rupture. J Am Coll Cardiol. 41, 15S–22S (2003).
Article CAS PubMed Google Scholar - Thygesen, K., Alpert, J. S. & White, H. D. Universal definition of myocardial infarction. J Am Coll Cardiol. 50, 2173–2195 (2007).
Article PubMed Google Scholar - Benjamin, E. J. et al. Prevention of atrial fibrillation: report from a national heart, lung, and blood institute workshop. Circulation. 119, 606–618 (2009).
Article PubMed PubMed Central Google Scholar - Kannel, W. B. & Benjamin, E. J. Status of the epidemiology of atrial fibrillation. Med Clin North Am. 92(ix), 17–40 (2008).
Article PubMed PubMed Central Google Scholar
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2012R1A2A2A02045367, 2010–0021993) and grants from the Korean Healthcare technology R&D project funded by the Ministry of Health & Welfare (HI12C1552, HI16C0058, HI15C1200).
Author information
Authors and Affiliations
- Division of Cardiology, Yonsei University College of Medicine, Seoul, Korea
Hye Young Lee, Pil-Sung Yang, Tae-Hoon Kim, Jae-Sun Uhm, Hui-Nam Pak, Moon-Hyoung Lee & Boyoung Joung - Division of Cardiology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
Hye Young Lee
Authors
- Hye Young Lee
You can also search for this author inPubMed Google Scholar - Pil-Sung Yang
You can also search for this author inPubMed Google Scholar - Tae-Hoon Kim
You can also search for this author inPubMed Google Scholar - Jae-Sun Uhm
You can also search for this author inPubMed Google Scholar - Hui-Nam Pak
You can also search for this author inPubMed Google Scholar - Moon-Hyoung Lee
You can also search for this author inPubMed Google Scholar - Boyoung Joung
You can also search for this author inPubMed Google Scholar
Contributions
H.Y.L. and B.O.J. designed the current study and wrote the main manuscript; H.Y.L. and P.S.Y. analyzed the data and created the tables and figures; T.H.K., J.S.U., H.N.P., and M.H.L. participated in clinical data collection.
Corresponding author
Correspondence toBoyoung Joung.
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, H.Y., Yang, PS., Kim, TH. et al. Atrial fibrillation and the risk of myocardial infarction: a nation-wide propensity-matched study.Sci Rep 7, 12716 (2017). https://doi.org/10.1038/s41598-017-13061-4
- Received: 04 April 2017
- Accepted: 18 September 2017
- Published: 05 October 2017
- DOI: https://doi.org/10.1038/s41598-017-13061-4