Brugada Syndrome: Practice Essentials, Background, Pathophysiology (original) (raw)
Practice Essentials
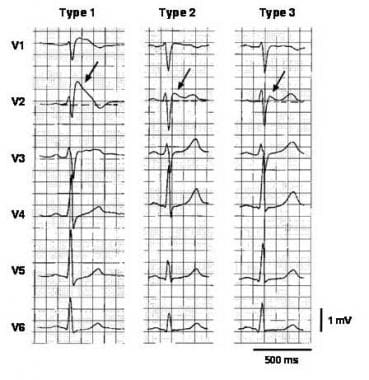
Brugada syndrome is a disorder characterized by sudden death associated with one of several ECG patterns characterized by incomplete right bundle-branch block and ST-segment elevations in the anterior precordial leads. See the image below.
Three types of ST-segment elevation in Brugada syndrome, as shown in the precordial leads on ECG in the same patient at different times. Left panel shows a type 1 ECG pattern with pronounced elevation of the J point (arrow), a coved-type ST segment, and an inverted T wave in V1 and V2. The middle panel illustrates a type 2 pattern with a saddleback ST-segment elevated by >1 mm. The right panel shows a type 3 pattern in which the ST segment is elevated < 1 mm. According to a consensus report (Antzelevitch, 2005), the type 1 ECG pattern is diagnostic of Brugada syndrome. Modified from Wilde, 2002. Image courtesy of Richard Nunez, MD, and EMedHome.com (https://www.emedhome.com/).
Signs and symptoms
Signs and symptoms in patients with Brugada syndrome may include the following:
- Syncope and cardiac arrest: Most common clinical manifestations; in many cases, cardiac arrest occurs during sleep or rest
- Nightmares or thrashing at night
- Asymptomatic, but routine ECG shows ST-segment elevation in leads V1-V3
- Associated atrial fibrillation (20%) [1]
- Fever: Often reported to trigger or exacerbate clinical manifestations
The lack of a prodrome has been reported to be more common in patients with ventricular fibrillation documented as the cause of syncope in patients with Brugada syndrome. [2]
See Presentation for more detail.
Diagnosis
Most patients with Brugada syndrome have a normal physical examination. However, such an examination is necessary to exclude other potential cardiac causes of syncope or cardiac arrest in an otherwise healthy patient (eg, heart murmurs from hypertrophic cardiomyopathy or from a valvular or septal defect).
Testing
In patients with suspected Brugada syndrome, consider the following studies:
- 12-lead ECG in all patients with syncope
- Drug challenge with a sodium channel blocker in patients with syncope without an obvious cause
- Electrophysiologic study to determine the inducibility of arrhythmias for risk stratification
Laboratory tests that may aid in the diagnosis of Brugada syndrome include the following:
- Serum potassium and calcium levels: In patients presenting with ST-segment elevation in the right precordial leads
- Potassium and calcium levels: ECG patterns in patients with hypercalcemia and hyperkalemia similar to that of Brugada syndrome
- CK-MB and troponin levels: In patients with symptoms compatible with an acute coronary syndrome
- Genetic testing for a mutation in SCN5A
Further testing may be indicated to exclude other diagnostic possibilities.
Imaging studies
Perform echocardiography and/or MRI, primarily to exclude arrhythmogenic right ventricular cardiomyopathy, as well as to assess for other potential causes of arrhythmias.
See Workup for more detail.
Management
To date, the only treatment that has proven effective in treating ventricular tachycardia and fibrillation and preventing sudden death in patients with Brugada syndrome is implantation of an automatic implantable cardiac defibrillator (ICD). Radiofrequency catheter ablation has been recently reported as an effective new treatment. [3, 4, 5, 6, 7]
No pharmacologic therapy has been proven to reduce the occurrence of ventricular arrhythmias or sudden death; however, theoretically, drugs that counteract the ionic current imbalance in Brugada syndrome could be used to treat it. For example, quinidine, which blocks the calcium-independent transient outward potassium current (Ito), has been shown to normalize the ECG pattern in patients with Brugada syndrome. [8] However, quinidine also blocks sodium (Na) currents, which could have contrary effects.
See Treatment and Medication for more detail.

Background
Brugada syndrome is a disorder characterized by sudden death associated with one of several electrocardiographic (ECG) patterns characterized by incomplete right bundle-branch block and ST elevations in the anterior precordial leads. See the image below.
Three types of ST-segment elevation in Brugada syndrome, as shown in the precordial leads on ECG in the same patient at different times. Left panel shows a type 1 ECG pattern with pronounced elevation of the J point (arrow), a coved-type ST segment, and an inverted T wave in V1 and V2. The middle panel illustrates a type 2 pattern with a saddleback ST-segment elevated by >1 mm. The right panel shows a type 3 pattern in which the ST segment is elevated < 1 mm. According to a consensus report (Antzelevitch, 2005), the type 1 ECG pattern is diagnostic of Brugada syndrome. Modified from Wilde, 2002. Image courtesy of Richard Nunez, MD, and EMedHome.com (https://www.emedhome.com/).
In the initial description of Brugada syndrome, the heart was reported to be structurally normal, but this concept has been challenged. [9] Subtle structural abnormalities in the right ventricular outflow tract have been reported.
Brugada syndrome is genetically determined and has an autosomal dominant pattern of transmission in about 50% of familial cases (see Etiology). The typical patient with Brugada syndrome is young, male, and otherwise healthy, with normal general medical and cardiovascular physical examinations.
Patients with Brugada syndrome are prone to develop ventricular tachyarrhythmias that may lead to syncope, cardiac arrest, or sudden cardiac death. [10, 11, 12] Infrahisian conduction delay and atrial fibrillation may also be manifestations of the syndrome. [13, 14]
About 5% of survivors of cardiac arrest have no clinically identified cardiac abnormality. About half of these cases are thought to be due to Brugada syndrome. [15]
At present, implantation of an automatic implantable cardiac defibrillator (ICD) is the only treatment proven effective in treating ventricular tachycardia and fibrillation and preventing sudden death in patients with Brugada syndrome (see Treatment).

Pathophysiology
Brugada syndrome is an example of a channelopathy, a disease caused by an alteration in the transmembrane ion currents that together constitute the cardiac action potential. Specifically, in 10-30% of cases, mutations in the SCN5A gene, which encodes the cardiac voltage-gated sodium channel Nav 1.5, have been found. These loss-of-function mutations reduce the sodium current (INa) available during the phases 0 (upstroke) and 1 (early repolarization) of the cardiac action potential.
This decrease in INa is thought to affect the right ventricular endocardium differently from the epicardium. Thus, it underlies both the Brugada ECG pattern and the clinical manifestations of the Brugada syndrome.
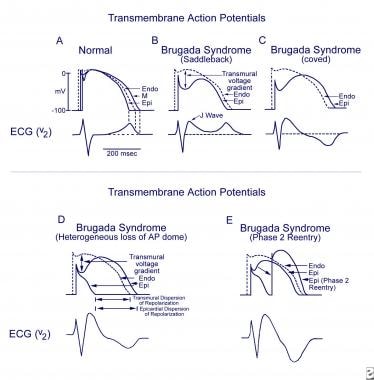
The exact mechanisms underlying the ECG alterations and arrhythmogenesis in Brugada syndrome are disputed. [16] The repolarization-defect theory is based on the fact that right ventricular epicardial cells display a more prominent notch in the action potential than endocardial cells. This is thought to be due to an increased contribution of the transient outward current (Ito) to the action potential waveform in that tissue.
A decrease in INa accentuates this difference, causing a voltage gradient during repolarization and the characteristic ST elevations on ECG. Research has provided human evidence for a repolarization gradient in patients with Brugada syndrome using simultaneous endocardial and epicardial unipolar recordings. [17] See the image below.
Schematics show the 3 types of action potentials in the right ventricle: endocardial (End), mid myocardial (M), and epicardial (Epi). A, Normal situation on V2 ECG generated by transmural voltage gradients during the depolarization and repolarization phases of the action potential. B-E, Different alterations of the epicardial action potential that produce the ECG changes observed in patients with Brugada syndrome. Adapted from Antzelevitch, 2005.
When the usual relative durations of repolarization are not altered, the T wave remains upright, causing a saddleback ECG pattern (type 2 or 3). When the alteration in repolarization is sufficient to cause a reversal of the normal gradient of repolarization, the T wave inverts, and the coved (type 1) ECG pattern is seen. In a similar way, a heterogeneous alteration in cardiac repolarization may predispose to the development of reentrant arrhythmias, termed phase 2 reentry, that can clinically cause ventricular tachycardia and ventricular fibrillation. [18]
An alternative hypothesis, the depolarization/conduction disorder model, proposes that the typical Brugada ECG findings can be explained by slow conduction and activation delays in the right ventricle (in particular in the right ventricular outflow tract). [16]
One study used ajmaline provocation to elicit a type 1 Brugada ECG pattern in 91 patients, and found that the repolarization abnormalities were concordant with the depolarization abnormalities and appeared to be secondary to the depolarization changes. [19] Using vectorcardiograms and body surface potential maps, investigators were able to show that depolarization abnormalities and conduction delay mapped to the right ventricle.

Etiology
The prototypical case of Brugada syndrome has been associated with alterations in the SCN5A gene, of which nearly 300 mutations have been described. [20] Mutations in other genes have been proposed to cause a variant of Brugada syndrome, including the genes coding for alpha1- and beta2b-subunits of the L-type calcium channel (CACNA1C and CACNB2), which are thought to cause a syndrome of precordial ST elevation, sudden death, and short QT interval. [21]
Mutations in the genes GPD1-L [22] and SCN1B [23] have been identified in a few familial cases. Cases in which a mutation in the SCN5A gene cannot be demonstrated may be due to mutations of these genes, due to other unidentified genes, or located in regions of the coding sequence or promoter region of SCN5A that are not routinely sequenced in lab tests.
Many clinical situations have been reported to unmask or exacerbate the ECG pattern of Brugada syndrome. Examples are a febrile state, hyperkalemia, hypokalemia, hypercalcemia, alcohol or cocaine intoxication, and the use of certain medications, including sodium channel blockers, vagotonic agents, alpha-adrenergic agonists, beta-adrenergic blockers, heterocyclic antidepressants, and a combination of glucose and insulin. [18]

Epidemiology
United States statistics
Because of its recent identification, the prevalence of Brugada syndrome is not well established. In a large university hospital on the West Coast of the United States, the prevalence of a Brugada ECG pattern among unselected, mainly white and Hispanic adults was 2 of 1348 patients (0.14%); in both cases, the ECG patterns were type 2. [24] The prevalence in Asian and other ethnic populations may be higher.
International statistics
The highest prevalence of Brugada syndrome is in Southeast Asia; the lowest is in North Africa. [25] In parts of Asia (eg, the Philippines, Thailand, Japan), Brugada syndrome seems to be the most common cause of natural death in men younger than 50 years. It is known as Lai Tai (Thailand), Bangungot (Philippines), and Pokkuri (Japan). In Northeast Thailand, the mortality rate from Lai Tai is approximately 30 cases per 100,000 population per year. [26]
Race-, sex-, and age-related demographics
Brugada syndrome is most common in people from Asia. The reason for this observation is not yet fully understood but may be due to an Asian-specific sequence in the promoter region of SCN5A. [27]
Brugada syndrome is 8-10 times more prevalent in men than in women, although the probability of having a mutated gene does not differ by sex. The penetrance of the mutation therefore appears to be much higher in men than in women.
Brugada syndrome most commonly affects otherwise healthy men aged 30-50 years, but affected patients aged 0-84 years have been reported. The mean age of patients who die suddenly is 41 years. [18]

Prognosis
Brugada syndrome is a cause of polymorphic ventricular tachycardia, which may degenerate into ventricular fibrillation and cause cardiac arrest. Prolonged hypoxia during cardiac arrest may leave patients with neurologic sequelae. Implantable cardioverters-defibrillators (ICDs) are often used to treat patients with Brugada syndrome, exposing them to complications related to device implantation and the potential for inappropriate shocks.
During a mean follow-up of 24 months, sudden cardiac death or ventricular fibrillation occurred in 8.2% of patients with Brugada syndrome. A history of syncope, a spontaneously abnormal ECG, and inducibility during programmed electrical stimulation (by one study) significantly increased this risk. [11]
Brugada syndrome may be a significant cause of death, aside from accidents, in men under 40. The true incidence is not known due to reporting biases. Although there is a strong population dependence, an estimated 4% of all sudden deaths and at least 20% of sudden deaths in patients with structurally normal hearts are due to the syndrome. Those with the syndrome have a mean age of sudden death of 41 ±15 years. [28]

Patient Education
Educating the patient and his or her family members and coworkers about basic cardiopulmonary resuscitation (CPR) is important. Genetic counseling is reasonable if desired by the patient and family.

- Bordachar P, Reuter S, Garrigue S, et al. Incidence, clinical implications and prognosis of atrial arrhythmias in Brugada syndrome. Eur Heart J. 2004 May. 25(10):879-84. [QxMD MEDLINE Link].
- Take Y, Morita H, Toh N, et al. Identification of high-risk syncope related to ventricular fibrillation in patients with Brugada syndrome. Heart Rhythm. 2012 May. 9(5):752-9. [QxMD MEDLINE Link].
- Brugada J, Campuzano O, Arbelo E, Sarquella-Brugada G, Brugada R. Present status of Brugada syndrome: JACC state-of-the-art review. J Am Coll Cardiol. 2018 Aug 28. 72(9):1046-59. [QxMD MEDLINE Link]. [Full Text].
- Nademanee K, Veerakul G, Chandanamattha P, et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011 Mar 29. 123(12):1270-9. [QxMD MEDLINE Link]. [Full Text].
- Brugada J, Pappone C, Berruezo A, et al. Brugada syndrome phenotype elimination by epicardial substrate ablation. Circ Arrhythm Electrophysiol. 2015 Dec. 8(6):1373-81. [QxMD MEDLINE Link]. [Full Text].
- Zhang P, Tung R, Zhang Z, et al. Characterization of the epicardial substrate for catheter ablation of Brugada syndrome. Heart Rhythm. 2016 Nov. 13(11):2151-8. [QxMD MEDLINE Link].
- Talib AK, Nogami A. Catheter ablation for Brugada syndrome. Korean Circ J. 2020 Apr. 50(4):289-301. [QxMD MEDLINE Link]. [Full Text].
- Antzelevitch C, Brugada P, Brugada J, Brugada R, Nademanee K, Towbin J. The Brugada syndrome. Clinical Approaches to Tachyarrhythmias. Armonk NY: Futura Publishing Company; 1999.
- Frustaci A, Priori SG, Pieroni M, et al. Cardiac histological substrate in patients with clinical phenotype of Brugada syndrome. Circulation. 2005 Dec 13. 112(24):3680-7. [QxMD MEDLINE Link]. [Full Text].
- Martini B, Nava A, Thiene G, et al. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J. 1989 Dec. 118(6):1203-9. [QxMD MEDLINE Link].
- Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003 Dec 23. 108(25):3092-6. [QxMD MEDLINE Link]. [Full Text].
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992 Nov 15. 20(6):1391-6. [QxMD MEDLINE Link].
- Vorobiof G, Kroening D, Hall B, Brugada R, Huang D. Brugada syndrome with marked conduction disease: dual implications of a SCN5A mutation. Pacing Clin Electrophysiol. 2008 May. 31(5):630-4. [QxMD MEDLINE Link].
- Kusano KF, Taniyama M, Nakamura K, et al. Atrial fibrillation in patients with Brugada syndrome relationships of gene mutation, electrophysiology, and clinical backgrounds. J Am Coll Cardiol. 2008 Mar 25. 51(12):1169-75. [QxMD MEDLINE Link]. [Full Text].
- Alings M, Wilde A. "Brugada" syndrome: clinical data and suggested pathophysiological mechanism. Circulation. 1999 Feb 9. 99(5):666-73. [QxMD MEDLINE Link].
- Meregalli PG, Wilde AA, Tan HL. Pathophysiological mechanisms of Brugada syndrome: depolarization disorder, repolarization disorder, or more?. Cardiovasc Res. 2005 Aug 15. 67(3):367-78. [QxMD MEDLINE Link].
- Nagase S, Kusano KF, Morita H, et al. Longer repolarization in the epicardium at the right ventricular outflow tract causes type 1 electrocardiogram in patients with Brugada syndrome. J Am Coll Cardiol. 2008 Mar 25. 51(12):1154-61. [QxMD MEDLINE Link]. [Full Text].
- Antzelevitch C, Brugada P, Brugada J, Brugada R. Brugada syndrome: from cell to bedside. Curr Probl Cardiol. 2005 Jan. 30(1):9-54. [QxMD MEDLINE Link]. [Full Text].
- Postema PG, van Dessel PF, Kors JA, et al. Local depolarization abnormalities are the dominant pathophysiologic mechanism for type 1 electrocardiogram in brugada syndrome a study of electrocardiograms, vectorcardiograms, and body surface potential maps during ajmaline provocation. J Am Coll Cardiol. 2010 Feb 23. 55(8):789-97. [QxMD MEDLINE Link]. [Full Text].
- Kapplinger JD, Tester DJ, Alders M, et al. An international compendium of mutations in the SCN5A-encoded cardiac sodium channel in patients referred for Brugada syndrome genetic testing. Heart Rhythm. 2010 Jan. 7(1):33-46. [QxMD MEDLINE Link]. [Full Text].
- Antzelevitch C, Pollevick GD, Cordeiro JM, et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death. Circulation. 2007 Jan 30. 115(4):442-9. [QxMD MEDLINE Link]. [Full Text].
- London B, Michalec M, Mehdi H, et al. Mutation in glycerol-3-phosphate dehydrogenase 1 like gene (GPD1-L) decreases cardiac Na+ current and causes inherited arrhythmias. Circulation. 2007 Nov 13. 116(20):2260-8. [QxMD MEDLINE Link]. [Full Text].
- Watanabe H, Koopmann TT, Le Scouarnec S, et al. Sodium channel beta1 subunit mutations associated with Brugada syndrome and cardiac conduction disease in humans. J Clin Invest. 2008 Jun. 118(6):2260-8. [QxMD MEDLINE Link]. [Full Text].
- Donohue D, Tehrani F, Jamehdor R, Lam C, Movahed MR. The prevalence of Brugada ECG in adult patients in a large university hospital in the western United States. Am Heart Hosp J. 2008 Winter. 6(1):48-50. [QxMD MEDLINE Link].
- Vutthikraivit W, Rattanawong P, Putthapiban P, et al. Worldwide prevalence of Brugada syndrome: a systematic review and meta-analysis. Acta Cardiol Sin. 2018 May. 34(3):267-77. [QxMD MEDLINE Link]. [Full Text].
- Nademanee K, Veerakul G, Nimmannit S, et al. Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation. 1997 Oct 21. 96(8):2595-600. [QxMD MEDLINE Link]. [Full Text].
- Bezzina CR, Shimizu W, Yang P, et al. Common sodium channel promoter haplotype in asian subjects underlies variability in cardiac conduction. Circulation. 2006 Jan 24. 113(3):338-44. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005 Feb 8. 111(5):659-70. [QxMD MEDLINE Link]. [Full Text].
- Wilde AA, Antzelevitch C, Borggrefe M, et al. Proposed diagnostic criteria for the Brugada syndrome: consensus report. Circulation. 2002 Nov 5. 106(19):2514-9. [QxMD MEDLINE Link]. [Full Text].
- Sangwatanaroj S, Prechawat S, Sunsaneewitayakul B, Sitthisook S, Tosukhowong P, Tungsanga K. New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives. Eur Heart J. 2001 Dec. 22(24):2290-6. [QxMD MEDLINE Link].
- Takagi M, Yokoyama Y, Aonuma K, Aihara N, Hiraoka M. Clinical characteristics and risk stratification in symptomatic and asymptomatic patients with brugada syndrome: multicenter study in Japan. J Cardiovasc Electrophysiol. 2007 Dec. 18(12):1244-51. [QxMD MEDLINE Link].
- Junttila MJ, Brugada P, Hong K, et al. Differences in 12-lead electrocardiogram between symptomatic and asymptomatic Brugada syndrome patients. J Cardiovasc Electrophysiol. 2008 Apr. 19(4):380-3. [QxMD MEDLINE Link].
- Sarkozy A, Chierchia GB, Paparella G, et al. Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome. Circ Arrhythm Electrophysiol. 2009 Apr. 2(2):154-61. [QxMD MEDLINE Link]. [Full Text].
- Kamakura S, Ohe T, Nakazawa K, et al. Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1-V3. Circ Arrhythm Electrophysiol. 2009 Oct. 2(5):495-503. [QxMD MEDLINE Link]. [Full Text].
- Zorzi A, Migliore F, Marras E, et al. Should all individuals with a nondiagnostic Brugada-electrocardiogram undergo sodium-channel blocker test?. Heart Rhythm. 2012 Jun. 9(6):909-16. [QxMD MEDLINE Link].
- Brugada P, Geelen P, Brugada R, Mont L, Brugada J. Prognostic value of electrophysiologic investigations in Brugada syndrome. J Cardiovasc Electrophysiol. 2001 Sep. 12(9):1004-7. [QxMD MEDLINE Link].
- Priori SG, Napolitano C, Gasparini M, et al. Natural history of Brugada syndrome: insights for risk stratification and management. Circulation. 2002 Mar 19. 105(11):1342-7. [QxMD MEDLINE Link]. [Full Text].
- Gehi AK, Duong TD, Metz LD, Gomes JA, Mehta D. Risk stratification of individuals with the Brugada electrocardiogram: a meta-analysis. J Cardiovasc Electrophysiol. 2006 Jun. 17(6):577-83. [QxMD MEDLINE Link].
- Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010 Feb 9. 121(5):635-43. [QxMD MEDLINE Link]. [Full Text].
- Priori SG, Gasparini M, Napolitano C, et al. Risk stratification in Brugada syndrome: results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. J Am Coll Cardiol. 2012 Jan 3. 59(1):37-45. [QxMD MEDLINE Link]. [Full Text].
- Raju H, Papadakis M, Govindan M, et al. Low prevalence of risk markers in cases of sudden death due to Brugada syndrome relevance to risk stratification in Brugada syndrome. J Am Coll Cardiol. 2011 Jun 7. 57(23):2340-5. [QxMD MEDLINE Link].
- Pelliccia A, Fagard R, Bjornstad HH, et al. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005 Jul. 26(14):1422-45. [QxMD MEDLINE Link].
- [Guideline] Ackerman MJ, Zipes DP, Kovacs RJ, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 10: The cardiac channelopathies: a scientific statement from the American Heart Association and American College of Cardiology. Circulation. 2015 Dec 1. 132(22):e326-9. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013 Dec. 10(12):1932-63. [QxMD MEDLINE Link].
- [Guideline] Priori SG, Blomstrom-Lundqvist C, Mazzanti A, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015 Nov 1. 36(41):2793-867. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Ackerman MJ, Priori SG, Willems S, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Europace. 2011 Aug. 13(8):1077-109. [QxMD MEDLINE Link]. [Full Text].
- Antzelevitch C. The Brugada syndrome: ionic basis and arrhythmia mechanisms. J Cardiovasc Electrophysiol. 2001 Feb. 12(2):268-72. [QxMD MEDLINE Link].
- Marquez MF, Salica G, Hermosillo AG, et al. Ionic basis of pharmacological therapy in Brugada syndrome. J Cardiovasc Electrophysiol. 2007 Feb. 18(2):234-40. [QxMD MEDLINE Link].
- Marquez MF, Salica G, Hermosillo AG, Pastelin G, Cardenas M. Drug therapy in Brugada syndrome. Curr Drug Targets Cardiovasc Haematol Disord. 2005 Oct. 5(5):409-17. [QxMD MEDLINE Link].
- Yang F, Hanon S, Lam P, Schweitzer P. Quinidine revisited. Am J Med. 2009 Apr. 122(4):317-21. [QxMD MEDLINE Link].
- Postema PG, Wolpert C, Amin AS, et al. Drugs and Brugada syndrome patients: review of the literature, recommendations, and an up-to-date website (www.brugadadrugs.org). Heart Rhythm. 2009 Sep. 6(9):1335-41. [QxMD MEDLINE Link]. [Full Text].
Author
Jose M Dizon, MD Professor of Clinical Medicine, Clinical Electrophysiology Laboratory, Division of Cardiology, Columbia University College of Physicians and Surgeons; Attending Physician, Department of Medicine, New York-Presbyterian/Columbia University Medical Center
Jose M Dizon, MD is a member of the following medical societies: American College of Cardiology, Heart Rhythm Society
Disclosure: Nothing to disclose.
Coauthor(s)
Tamim M Nazif, MD Fellow, Division of Cardiology, Columbia University College of Physicians and Surgeons
Tamim M Nazif, MD is a member of the following medical societies: American College of Cardiology
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Ronald J Oudiz, MD, FACP, FACC, FCCP Professor of Medicine, University of California, Los Angeles, David Geffen School of Medicine; Director, Liu Center for Pulmonary Hypertension, Division of Cardiology, LA Biomedical Research Institute at Harbor-UCLA Medical Center
Ronald J Oudiz, MD, FACP, FACC, FCCP is a member of the following medical societies: American College of Cardiology, American College of Chest Physicians, American College of Physicians, American Heart Association, American Thoracic Society
Disclosure: Serve(d) as a speaker or a member of a speakers bureau for: Actelion, Bayer, Gilead, United Therapeutics
Received research grant from: Actelion, Arena, Gilead, GSK, Liquidia, Reata, United Therapeutics
Received income in an amount equal to or greater than $250 from: Actelion, Complexa, Gilead, Medtronic, Reata, United Therapeutics.
Chief Editor
Mikhael F El-Chami, MD Associate Professor, Department of Medicine, Division of Cardiology, Section of Electrophysiology, Emory University School of Medicine
Mikhael F El-Chami, MD is a member of the following medical societies: Alpha Omega Alpha, American College of Cardiology, American Heart Association, Heart Rhythm Society
Disclosure: Serve(d) as a director, officer, partner, employee, advisor, consultant or trustee for: Medtronic; Boston Scientific, Biotronik
Received research grants (as part of Multicenter studies) from Medtronic and Boston Scientific.
Additional Contributors
Justin D Pearlman, MD, ME, PhD, FACC, MA Chief, Division of Cardiology, Director of Cardiology Consultative Service, Director of Cardiology Clinic Service, Director of Cardiology Non-Invasive Laboratory, Chair of Institutional Review Board, University of California, Los Angeles, David Geffen School of Medicine
Justin D Pearlman, MD, ME, PhD, FACC, MA is a member of the following medical societies: American College of Cardiology, International Society for Magnetic Resonance in Medicine, American College of Physicians, American Federation for Medical Research, Radiological Society of North America
Disclosure: Nothing to disclose.