Esophagogastroduodenoscopy (EGD): Background, Indications, Contraindications (original) (raw)
Background
Esophagogastroduodenoscopy (EGD) is a procedure during which a small flexible endoscope is introduced through the mouth (or, with smaller-caliber endoscopes, through the nose) and advanced through the pharynx, esophagus, stomach, and duodenum. [1] An enteroscope, a longer endoscope, can be introduced beyond the ligament of Treitz into the jejunum.
EGD is used for both diagnostic procedures and therapeutic procedures. Most modern endoscopes now use a video chip (charged coupled device) for better imaging, in contrast to the older endoscopes, which used fiberoptics for image transmission. (See the images below.)
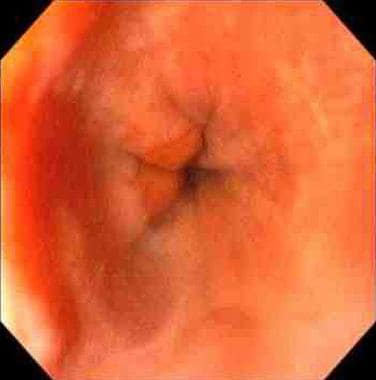
Esophagogastroduodenoscopy (EGD). Normal vocal cords as seen prior to entering the esophagus during video EGD.
Esophagogastroduodenoscopy (EGD). Normal lower esophageal sphincter seen during EGD.
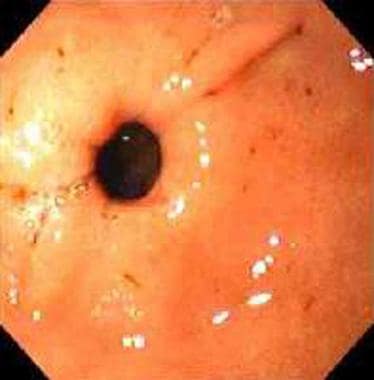
Esophagogastroduodenoscopy (EGD). Normal pylorus seen during EGD.
Esophagogastroduodenoscopy (EGD). Normal duodenum in the area of the ampulla, as seen during EGD.
In the United States, EGD is usually performed while the patient is under conscious or moderate sedation, though it can be performed with only topical anesthesia (as is common practice in Europe and Asia). General anesthesia is often used in a selected group of patients who are difficult to sedate because of chronic narcotics intake.
The procedure is usually performed in a dedicated endoscopy unit in the hospital or outpatient office setting but can also be done in the emergency department (ED), the intensive care unit (ICU), or the operating room (OR) by using portable endoscopy carts. With the aid of various types of equipment and endoscopes, endoscopic ultrasonography (EUS), endoscopic retrograde cholangiopancreatography (ERCP), and small-bowel enteroscopy can also be performed.

Indications
Indications for EGD include the following [2] :
- Diagnostic evaluation for signs or symptoms suggestive of upper gastrointestinal (GI) disease (eg, dyspepsia, dysphagia, noncardiac chest pain, or recurrent emesis), such as gastroesophageal reflux disease (GERD) [3]
- Surveillance for upper GI cancer in high-risk settings (eg, Barrett esophagus [4, 5] or polyposis syndromes)
- Biopsy for known or suggested upper GI disease (eg, malabsorption syndromes, neoplasms, or infections)
- Therapeutic intervention (eg, retrieval of foreign bodies, [6] control of hemorrhage, dilatation or stenting of stricture, ablation of neoplasms, or gastrostomy placement)

Contraindications
Contraindications for EGD include the following:
- Possible perforation
- Medically unstable patients
- Unwilling patients
- Anticoagulation, pharyngeal diverticulum, or head and neck surgery (relative contraindications)
Diagnostic EGD is considered a low-risk procedure for bleeding in patients on anticoagulants and therefore can be performed without adjustment of anticoagulation before the procedure. [7] However, if polypectomy is contemplated or conceivable, then the patient's coagulation profile should be normalized. A risk of retropharyngeal hematoma also may be present in patients with severe coagulation abnormalities.
Certain therapeutic procedures (ie, dilations, percutaneous endoscopic gastrostomy [PEG], polypectomy, endoscopic sphincterotomy, EUS-guided fine-needle aspiration [FNA], laser ablation, and coagulation) are considered high-risk procedures for bleeding, and adjustment of anticoagulation may therefore be necessary.

Technical Considerations
Best practices
Endoscopy units are specific areas in a hospital (or physician's office) in which all endoscopic procedures are performed. For this unit to be functional and effective, according to the American Society for Gastrointestinal Endoscopy (ASGE), certain conditions must be met, [8, 9] including the following:
- Properly trained endoscopist and nursing staff
- Functioning and adequately maintained equipment
- Availability of an endoscope cleaning area
- Personnel trained to perform cardiopulmonary resuscitation
- Quality improvement program in place
Open-access endoscopy is a system designed to offset the cost of endoscopy in stable patients without significant comorbidities who have clear indications for upper GI endoscopy. [10] The responsibilities of the referring physician are to have a complete understanding of the patient's condition and to be fully aware of the accepted indications for endoscopy. If the patient is on anticoagulation or if antibiotic prophylaxis is required, these issues must be addressed via proper communication between the referring physician and the endoscopist.
According to ASGE recommendations, training in upper GI endoscopy should include an understanding of indications, limitations, contraindications, alternatives, principles of conscious sedation, and correct interpretation of endoscopic findings. [11] A minimum of 100 upper GI endoscopic procedures has been recommended for trainees to become competent in diagnostic upper GI endoscopy.
Therapeutic upper GI endoscopy requires further training and experience to gain competency. The recommendations of the ASGE for the number of procedures required to gain competency in various therapeutic upper GI endoscopic procedures are available through the society Web site (see American Society for Gastrointestinal Endoscopy).
EGD, like other endoscopic procedures, has a substantial environmental impact (eg, through greenhouse gas emission and the creation of waste, as in single-use instruments). Accordingly, the ASGE has established a Task Force on Sustainable Endoscopy to propose ways of minimizing this impact. [12]
Procedural planning
Transnasal EGD (TN-EGD) has certain limitations in bending, which can make approaching certain gastric regions difficult. Rhee et al evaluated whether the quality and quantity of two-directional TN-EGD biopsied gastric specimens were affected by this limitation. [13] Specimen quantity was assessed on the basis of diameter and depth (μm), as well as presence of tissue layers (superficial mucosa, deep mucosa, muscularis mucosa, and submucosa). Specimen quality was assessed on the basis of anatomic orientation (good, intermediate, or poor), presence of crush artifact (none to minimal, mild, or moderate), and overall diagnostic adequacy (adequate, suboptimal, or inadequate).
Of 289 TN-EGD gastric biopsy specimens, 33 (11.4%) were of poor orientation, 26 (9.0%) revealed the presence of crush, and 37 (12.8%) demonstrated overall diagnostic inadequacy. [13] In 211 (73.0%), deep mucosa was present, but only 75 specimens (26.0%) had muscularis mucosa. The posterior aspect of the cardia had the greatest limitations in specimen quantity and quality, with the shallowest depth, poorest orientation, and poorest diagnostic adequacy. The investigators recommended paying special attention to gastric lesions located on the posterior aspect of the cardia when using two-directional TN-EGD.
In a two-part study, investigators attempted to find a good washing solution to counter the known limitations of the small-caliber water-jet nozzles of TN-EGDs for cleaning lenses. [14] Komazawa et al compared oolong tea, barley tea, and distilled water as washing solutions for the endoscopic lenses. In the first part of the study, the TN-EGD lenses were soiled by lard and then washed with one of the three washing solutions. When the image quality of photographs were judged, lenses washed with oolong tea resulted in a significantly higher image quality than did lenses washed with barley tea or distilled water solutions.
In the second part of the study, 982 patients scheduled to undergo TN-EGD were randomly assigned to groups in which the endoscope lens was washed with one of the three washing solutions. [14] The investigators found that the level of lens cleansing was significantly greater and the overall time required for endoscopy was significantly shorter in the oolong tea group than in the other two groups. When the volume of washing solution used for lens cleansing was compared, significantly less was used in the oolong group compared with the distilled water group. On the basis of their findings, Komazawa et al recommended oolong tea rather than water for cleaning TN small-caliber EGD lenses.
Complication prevention
Despite the large number of endoscopic procedures performed each day, the incidence of infection transmission via endoscopes remains very low. [15, 16] Methods of reprocessing endoscopes include mechanical cleaning, high-level disinfection, rinsing, and drying. Proper and diligent care during reprocessing of endoscopes, with attention to quality control, cannot be overstated for minimizing the risk of spreading infection via endoscopic procedures. [17]

- Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. Treasure Island, FL: StatPearls; 2023. [Full Text].
- [Guideline] ASGE Standards of Practice Committee, Early DS, Ben-Menachem T, Decker GA, Evans JA, Fanelli RD, et al. Appropriate use of GI endoscopy. Gastrointest Endosc. 2012 Jun. 75 (6):1127-31. [QxMD MEDLINE Link]. [Full Text].
- Mann R, Gajendran M, Perisetti A, Goyal H, Saligram S, Umapathy C. Advanced Endoscopic Imaging and Interventions in GERD: An Update and Future Directions. Front Med (Lausanne). 2021. 8:728696. [QxMD MEDLINE Link]. [Full Text].
- Osawa H, Yamamoto H, Yamada N, Yoshizawa M, Sunada K, Kita H, et al. Diagnosis of endoscopic Barrett's esophagus by transnasal flexible spectral imaging color enhancement. J Gastroenterol. 2009. 44 (11):1125-32. [QxMD MEDLINE Link].
- [Guideline] ASGE STANDARDS OF PRACTICE COMMITTEE., Qumseya B, Sultan S, Bain P, Jamil L, Jacobson B, et al. ASGE guideline on screening and surveillance of Barrett's esophagus. Gastrointest Endosc. 2019 Sep. 90 (3):335-359.e2. [QxMD MEDLINE Link]. [Full Text].
- Marashi Nia SF, Aghaie Meybodi M, Sutton R, Bansal A, Olyaee M, Hejazi R. Outcome, complication and follow-up of patients with esophageal foreign body impaction: an academic institute's 15 years of experience. Dis Esophagus. 2020 May 15. 33 (5):[QxMD MEDLINE Link].
- [Guideline] ASGE Standards of Practice Committee., Acosta RD, Abraham NS, Chandrasekhara V, et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016 Jan. 83 (1):3-16. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Jamil LH, Naveed M, Agrawal D, Fujii-Lau LL, Al-Haddad M, Buxbaum JL, et al. ASGE guideline on minimum staffing requirements for the performance of GI endoscopy. Gastrointest Endosc. 2020 Apr. 91 (4):723-729.e17. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ASGE Ensuring Safety in the Gastrointestinal Endoscopy Unit Task Force, Calderwood AH, Chapman FJ, Cohen J, Cohen LB, Collins J, et al. Guidelines for safety in the gastrointestinal endoscopy unit. Gastrointest Endosc. 2014 Mar. 79 (3):363-72. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ASGE Standards of Practice Committee, Chandrasekhara V, Eloubeidi MA, Bruining DH, Chathadi K, Faulx AL, et al. Open-access endoscopy. Gastrointest Endosc. 2015 Jun. 81 (6):1326-9. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Ensuring competence in endoscopy. American Society for Gastrointestinal Endoscopy. Available at https://www.asge.org/docs/default-source/education/practice_guidelines/doc-competence.pdf?sfvrsn=6. Accessed: November 30, 2023.
- [Guideline] Prepared by: American Society for Gastrointestinal Endoscopy Sustainable Endoscopy Task Force, Hernandez LV, Agrawal D, Skole KS, Crockett SD, Shimpi RA, et al. Meeting the environmental challenges of endoscopy: a pathway from strategy to implementation. Gastrointest Endosc. 2023 Dec. 98 (6):881-888.e1. [QxMD MEDLINE Link]. [Full Text].
- Rhee KH, Han HS, Lee SY, Seo TH, Ko SY, Kim BK, et al. Does a small biopsied gastric specimen limit the usage of two directional transnasal esophagogastroduodenoscopy?. J Gastroenterol Hepatol. 2010 Feb. 25 (2):270-6. [QxMD MEDLINE Link].
- Komazawa Y, Amano Y, Yuki M, Fukuhara H, Mishiro T, Mishiro T, et al. Oolong tea is useful for lens cleansing in transnasal small-caliber esophagogastroduodenoscopy. Endoscopy. 2010 Feb. 42 (2):104-8. [QxMD MEDLINE Link].
- [Guideline] ASGE Quality Assurance in Endoscopy Committee., Calderwood AH, Day LW, Muthusamy VR, Collins J, Hambrick RD 3rd, et al. ASGE guideline for infection control during GI endoscopy. Gastrointest Endosc. 2018 May. 87 (5):1167-1179. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ASGE STANDARDS OF PRACTICE COMMITTEE, Coelho-Prabhu N, Forbes N, Thosani NC, Storm AC, Pawa S, et al. Adverse events associated with EGD and EGD-related techniques. Gastrointest Endosc. 2022 Sep. 96 (3):389-401.e1. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Day LW, Muthusamy VR, Collins J, Kushnir VM, Sawhney MS, Thosani NC, et al. Multisociety guideline on reprocessing flexible GI endoscopes and accessories. Gastrointest Endosc. 2021 Jan. 93 (1):11-33.e6. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ASGE Standards of Practice Committee., Storm AC, Fishman DS, Buxbaum JL, Coelho-Prabhu N, Al-Haddad MA, et al. American Society for Gastrointestinal Endoscopy guideline on informed consent for GI endoscopic procedures. Gastrointest Endosc. 2022 Feb. 95 (2):207-215.e2. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] ASGE Standards of Practice Committee, Pasha SF, Acosta R, Chandrasekhara V, Chathadi KV, Eloubeidi MA, et al. Routine laboratory testing before endoscopic procedures. Gastrointest Endosc. 2014 Jul. 80 (1):28-33. [QxMD MEDLINE Link]. [Full Text].
- Nelson DB, Block KP, Bosco JJ, Burdick JS, Curtis WD, Faigel DO, et al. Technology status evaluation report: ultrathin endoscopes esophagogastroduodenoscopy: March 2000. Gastrointest Endosc. 2000 Jun. 51 (6):786-9. [QxMD MEDLINE Link].
- de'Angelis N, Carra MC, Borrelli O, Bizzarri B, Vincenzi F, Fornaroli F, et al. Short- and long-term efficacy of endoscopic balloon dilation in Crohn's disease strictures. World J Gastroenterol. 2013 May 7. 19 (17):2660-7. [QxMD MEDLINE Link]. [Full Text].
- Cammarota G, Martino A, Di Caro S, Cianci R, Lecca PG, Vecchio FM, et al. High-resolution magnifying upper endoscopy in a patient with patchy celiac disease. Dig Dis Sci. 2005 Mar. 50 (3):601-4. [QxMD MEDLINE Link].
- Yagi K, Honda H, Yang JM, Nakagawa S. Magnifying endoscopy in gastritis of the corpus. Endoscopy. 2005 Jul. 37 (7):660-6. [QxMD MEDLINE Link].
- Zhang R, Lau LHS, Wu PIC, Yip HC, Wong SH. Endoscopic Diagnosis and Treatment of Esophageal Squamous Cell Carcinoma. Methods Mol Biol. 2020. 2129:47-62. [QxMD MEDLINE Link].
- Ozawa S, Yoshida M, Kumai K, Kitajima M. New endoscopic treatments for gastroesophageal reflux disease. Ann Thorac Cardiovasc Surg. 2005 Jun. 11 (3):146-53. [QxMD MEDLINE Link].
- Hirata M, Tanaka S, Oka S, Kaneko I, Yoshida S, Yoshihara M, et al. Magnifying endoscopy with narrow band imaging for diagnosis of colorectal tumors. Gastrointest Endosc. 2007 Jun. 65 (7):988-95. [QxMD MEDLINE Link].
- Kara MA, Ennahachi M, Fockens P, ten Kate FJ, Bergman JJ. Detection and classification of the mucosal and vascular patterns (mucosal morphology) in Barrett's esophagus by using narrow band imaging. Gastrointest Endosc. 2006 Aug. 64 (2):155-66. [QxMD MEDLINE Link].
- Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004 Dec. 36 (12):1080-4. [QxMD MEDLINE Link].
- Uchida D, Kato H, Matsumoto K, Ishihara Y, Matsumi A, Saragai Y, et al. Single-session esophagogastroduodenoscopy and endoscopic ultrasound using a forward-viewing radial scan ultrasonic endoscope. BMC Gastroenterol. 2019 Dec 18. 19 (1):220. [QxMD MEDLINE Link]. [Full Text].
- Jayasena H, Abeynayake D, De Silva A, Niriella M, de Silva HJ. The use of personal protective equipment in endoscopy: what should the endoscopist wear during a pandemic?. Expert Rev Gastroenterol Hepatol. 2021 Dec. 15 (12):1349-1359. [QxMD MEDLINE Link].
- [Guideline] ASGE Standards of Practice Committee., Early DS, Lightdale JR, Vargo JJ 2nd, Acosta RD, Chandrasekhara V, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018 Feb. 87 (2):327-337. [QxMD MEDLINE Link]. [Full Text].
- Poulos JE, Kalogerinis PT, Caudle JN. Propofol compared with combination propofol or midazolam/fentanyl for endoscopy in a community setting. AANA J. 2013 Feb. 81 (1):31-6. [QxMD MEDLINE Link].
- Wu H, Xin L, Lin JH, Wang QH, Li B, Jin ZD, et al. Association between sedation and small neoplasm detection during diagnostic esophagogastroduodenoscopy: a propensity score-matched retrospective study. Scand J Gastroenterol. 2022 May. 57 (5):603-609. [QxMD MEDLINE Link].
- Mariotti AL, Pattee J, Edmundowicz SA, Hardesty TD, Sharma SM, Lemley MG, et al. Operational outcomes of propofol sedation versus fentanyl, midazolam and diphenhydramine sedation for endoscopies and colonoscopies at an academic medical center. PLoS One. 2023. 18 (11):e0294418. [QxMD MEDLINE Link]. [Full Text].
- de la Morena F, Santander C, Esteban C, de Cuenca B, García JA, Sánchez J, et al. Usefulness of applying lidocaine in esophagogastroduodenoscopy performed under sedation with propofol. World J Gastrointest Endosc. 2013 May 16. 5 (5):231-9. [QxMD MEDLINE Link]. [Full Text].
- Guo Y, Zhang H, Feng X, Wang A. A retrospective study of risk factors for cardiopulmonary events during propofol-mediated gastrointestinal endoscopy in patients aged over 70 years. Middle East J Anaesthesiol. 2012 Feb. 21 (4):505-11. [QxMD MEDLINE Link].
- Oh SH. Sedation in Pediatric Esophagogastroduodenoscopy. Clin Endosc. 2018 Mar. 51 (2):120-128. [QxMD MEDLINE Link]. [Full Text].
- Wu Y, Zhang Y, Hu X, Qian C, Zhou Y, Xie J. A comparison of propofol vs. dexmedetomidine for sedation, haemodynamic control and satisfaction, during esophagogastroduodenoscopy under conscious sedation. J Clin Pharm Ther. 2015 Aug. 40 (4):419-25. [QxMD MEDLINE Link].
- [Guideline] ASGE Standards of Practice Committee, Khashab MA, Chithadi KV, Acosta RD, Bruining DH, Chandrasekhara V, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc. 2015 Jan. 81 (1):81-9. [QxMD MEDLINE Link]. [Full Text].
- Yun HW, Shim KN, Na SK, Ryu JI, Lee MJ, Song EM, et al. Comparison between the Effectiveness of Oral Phloroglucin and Cimetropium Bromide as Premedication for Diagnostic Esophagogastroduodenoscopy: An Open-Label, Randomized, Comparative Study. Clin Endosc. 2015 Jan. 48 (1):48-51. [QxMD MEDLINE Link].
- Wang P, Xu T, Ngamruengphong S, Makary MA, Kalloo A, Hutfless S. Rates of infection after colonoscopy and osophagogastroduodenoscopy in ambulatory surgery centres in the USA. Gut. 2018 Sep. 67 (9):1626-1636. [QxMD MEDLINE Link].
- Majeski J, Lynch W, Durst G. Esophageal perforation during esophagogastroduodenoscopy. Am J Surg. 2009 Nov. 198 (5):e56-7. [QxMD MEDLINE Link].
- Chan MF. Complications of upper gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 1996 Apr. 6 (2):287-303. [QxMD MEDLINE Link].
Author
Tony E Yusuf, MD Assistant Professor, Department of Internal Medicine, Division of Gastroenterology, Hepatology and Nutrition, The University of Texas Houston Medical School
Tony E Yusuf, MD is a member of the following medical societies: American College of Gastroenterology, American College of Physicians, American Medical Association, Louisiana State Medical Society, Medical Society of the State of New York, Minnesota Medical Association, American Gastroenterological Association, American Society for Gastrointestinal Endoscopy
Disclosure: Nothing to disclose.
Coauthor(s)
Manoop S Bhutani, MD Professor, Co-Director, Center for Endoscopic Research, Training and Innovation (CERTAIN), Director, Center for Endoscopic Ultrasound, Department of Medicine, Division of Gastroenterology, University of Texas Medical Branch; Director, Endoscopic Research and Development, The University of Texas MD Anderson Cancer Center
Manoop S Bhutani, MD is a member of the following medical societies: American Association for the Advancement of Science, American College of Gastroenterology, American College of Physicians, American Gastroenterological Association, American Institute of Ultrasound in Medicine, American Society for Gastrointestinal Endoscopy
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Douglas M Heuman, MD, FACP, FACG, AGAF Chief of Hepatology, Hunter Holmes McGuire Department of Veterans Affairs Medical Center; Professor, Department of Internal Medicine, Division of Gastroenterology, Virginia Commonwealth University School of Medicine
Douglas M Heuman, MD, FACP, FACG, AGAF is a member of the following medical societies: American Association for the Study of Liver Diseases, American College of Physicians, American Gastroenterological Association
Disclosure: Received grant/research funds from Novartis for other; Received grant/research funds from Bayer for other; Received grant/research funds from Otsuka for none; Received grant/research funds from Bristol Myers Squibb for other; Received none from Scynexis for none; Received grant/research funds from Salix for other; Received grant/research funds from MannKind for other.
Chief Editor
Additional Contributors
Maurice A Cerulli, MD, FACP, FACG, FASGE, AGAF Associate Professor of Clinical Medicine, Albert Einstein College of Medicine of Yeshiva University; Associate Professor of Clinical Medicine, Hofstra Medical School
Maurice A Cerulli, MD, FACP, FACG, FASGE, AGAF is a member of the following medical societies: American Association for the Study of Liver Diseases, American College of Gastroenterology, American College of Physicians, New York Society for Gastrointestinal Endoscopy, American Gastroenterological Association, American Medical Association, American Society for Gastrointestinal Endoscopy
Disclosure: Nothing to disclose.
Acknowledgements
Acknowledgments
Medscape Reference thanks George Y Wu, MD, PhD, Professor, Department of Medicine, Director, Hepatology Section, Herman Lopata Chair in Hepatitis Research, University of Connecticut School of Medicine, for assistance with the video contribution to this article.
Medscape Reference also thanks Dawn Sears, MD, Associate Professor of Internal Medicine, Division of Gastroenterology and Hepatology, Scott and White Memorial Hospital; and Dan C Cohen, MD, Fellow in Gastroenterology, Scott and White Hospital, Texas A&M Health Science Center College of Medicine, for assistance with the video contribution to this article.