Advances in the science and treatment of alcohol use disorder (original) (raw)
Pharmacological and behavioral treatments exist for alcohol use disorder, but more are needed, and several are under development.
Abstract
Alcohol is a major contributor to global disease and a leading cause of preventable death, causing approximately 88,000 deaths annually in the United States alone. Alcohol use disorder is one of the most common psychiatric disorders, with nearly one-third of U.S. adults experiencing alcohol use disorder at some point during their lives. Alcohol use disorder also has economic consequences, costing the United States at least $249 billion annually. Current pharmaceutical and behavioral treatments may assist patients in reducing alcohol use or facilitating alcohol abstinence. Although recent research has expanded understanding of alcohol use disorder, more research is needed to identify the neurobiological, genetic and epigenetic, psychological, social, and environmental factors most critical in the etiology and treatment of this disease. Implementation of this knowledge in clinical practice and training of health care providers is also needed to ensure appropriate diagnosis and treatment of individuals suffering from alcohol use disorder.
INTRODUCTION
In most regions of the world, most adults consume alcohol at least occasionally (1). Alcohol is among the leading causes of preventable death worldwide, with 3 million deaths per year attributable to alcohol. In the United States, more than 55% of those aged 26 and older consumed alcohol in a given month, and one in four adults in this age group engaged in binge drinking (defined as more than four drinks for women and five drinks for men on a single drinking occasion) (2). Excessive alcohol use costs U.S. society more than $249 billion annually and is the fifth leading risk factor for premature death and disability (3).
The morbidity and mortality associated with alcohol are largely due to the high rates of alcohol use disorder in the population. Alcohol use disorder is defined in the Diagnostic and Statistical Manual for Mental Disorders, 5th edition (DSM-5) (4) as a pattern of alcohol consumption, leading to problems associated with 2 or more of 11 potential symptoms of alcohol use disorder (see Table 1 for criteria). In the United States, approximately one-third of all adults will meet criteria for alcohol use disorder at some point during their lives (5), and approximately 15.1 million of U.S. adults meet criteria for alcohol use disorder in the previous 12 months (6). The public health impacts of alcohol use extend far beyond those individuals who drink alcohol, engage in heavy alcohol use, and/or meet criteria for an alcohol use disorder. Alcohol use is associated with increased risk of accidents, workplace productivity losses, increased medical and mental health costs, and greater rates of crime and violence (1). Analyses that take into account the overall harm due to drugs (harm to both users and others) show that alcohol is the most harmful drug (7).
Table 1. Alcohol use disorder criteria, as defined by the Diagnostic and Statistical Manual for Mental Disorders, 5th edition (DSM-5) (4), and the International Classification of Diseases, 10th edition (ICD-10) (116).
| DSM-5 criteria for alcohol use disorder | ICD-10 criteria for alcohol dependence |
|---|---|
| Tolerance | Tolerance |
| Withdrawal | Withdrawal |
| Difficulties controlling drinking(unsuccessful in cutting down orstopping drinking) | Difficulties controlling drinking(unsuccessful in cutting downor stopping drinking) |
| Neglect of activities | Neglect of activities |
| Time spent drinking or recoveringfrom effects of alcohol | Time spent drinking or recoveringfrom effects of alcohol |
| Drinking despite physical/psychological problems | Drinking despite physical/psychological problems |
| Craving | Craving |
| Alcohol consumed in largeramounts or over longer periodsthan was intended | |
| Failure to fulfill major roleobligations | |
| Recurrent alcohol use in hazardoussituations | |
| Drinking despite social/interpersonal problems | |
| (Two or more criteria met in past year) | (Three or more criteria met in past year) |
Only a small percent of individuals with alcohol use disorder contribute to the greatest societal and economic costs (8). For example, in the 2015 National Survey on Drug Use and Health survey (total n = 43,561), a household survey conducted across the United States, 11.8% met criteria for an alcohol use disorder (n = 5124) (6). Of these 5124 individuals, 67.4% (n = 3455) met criteria for a mild disorder (two or three symptoms, based on DSM-5), 18.8% (n = 964) met criteria for a moderate disorder (four or five symptoms, based on DSM-5), and only 13.8% (n = 705) met criteria for a severe disorder (six or more symptoms) (6). There is a large treatment gap for alcohol use disorder, arising from the fact that many individuals with alcohol use disorder do not seek treatment. Those with a mild or moderate alcohol use disorder may be able to reduce their drinking in the absence of treatment (9) and have a favorable course; but it is those with more severe alcohol use disorder who most often seek treatment and who may experience a chronic relapsing course (10).
HISTORY OF TREATMENT FOR ALCOHOL USE DISORDER
Near the end of the 18th century, the Pennsylvania physician Benjamin Rush described the loss of control of alcohol and its potential treatments (11). His recommendations for remedies and case examples included practicing the Christian religion, experiencing guilt and shame, pairing alcohol with aversive stimuli, developing other passions in life, following a vegetarian diet, taking an oath to not drink alcohol, and sudden and absolute abstinence from alcohol. Through the 1800s and early 1900s, the temperance movement laid the groundwork for mutual help organizations, and the notion of excessive alcohol use as a moral failing. During the same period, inebriate asylums emerged as a residential treatment option for excessive alcohol use, although the only treatment offered was forced abstinence from alcohol (12). The founding of Alcoholics Anonymous (A.A.) in the 1930s (13) and the introduction of the modern disease concept of alcohol use disorder (previously called “alcoholism”) in the 1940s (14) laid the groundwork for many of the existing treatment programs that remain widely available today. Over the past 80 years, empirical studies have provided support for both mutual support [A.A. and other support groups, such as SMART (Self-Management and Recovery Training)] and medical models of treatment for alcohol use disorder, as well as the development of new pharmacological and behavioral treatment options. In addition, there are several public health policy initiatives (e.g., taxation, restrictions on advertising, and outlet density) and brief intervention programs (e.g., social norms interventions) that can be effective in reducing prevalence of alcohol use disorder and alcohol-related harms (1).
NEUROBIOLOGY OF ALCOHOL USE DISORDER
Alcohol use disorder is characterized by loss of control over alcohol drinking that is accompanied by changes in brain regions related to the execution of motivated behaviors and to the control of stress and emotionality (e.g., the midbrain, the limbic system, the prefrontal cortex, and the amygdala). Mechanisms of positive and negative reinforcement both play important roles with individual drinking behavior being maintained by positive reinforcement (rewarding and desirable effects of alcohol) and/or negative reinforcement mechanisms (negative affective and physiological states that are relieved by alcohol consumption) (15, 16). At the neurotransmitter level, the positive reinforcing effects of alcohol are primarily mediated by dopamine, opioid peptides, serotonin, γ-aminobutyric acid (GABA), and endocannabinoids, while negative reinforcement involves increased recruitment of corticotropin-releasing factor and glutamatergic systems and down-regulation of GABA transmission (16). Long-term exposure to alcohol causes adaptive changes in several neurotransmitters, including GABA, glutamate, and norepinephrine, among many others. Discontinuation of alcohol ingestion results in the nervous system hyperactivity and dysfunction that characterizes alcohol withdrawal (15, 16). Acting on several types of brain receptors, glutamate represents one of the most common excitatory neurotransmitters. As one of the major inhibitory neurotransmitters, GABA plays a key role in the neurochemical mechanisms involved in intoxication, tolerance, and withdrawal. This brief review can offer only a very simplified overview of the complex neurobiological basis of alcohol use disorder. For deeper, more detailed analysis of this specific topic, the reader is encouraged to consult other reviews (15, 16).
CLINICAL MANAGEMENT OF ALCOHOL WITHDRAWAL SYNDROME
Alcohol withdrawal symptoms may include anxiety, tremors, nausea, insomnia, and, in severe cases, seizures and delirium tremens. Although up to 50% of individuals with alcohol use disorder present with some withdrawal symptoms after stopping drinking, only a small percentage requires medical treatment for detoxification, and some individuals may be able to reduce their drinking spontaneously. Medical treatment may take place either in an outpatient or, when clinically indicated, inpatient setting. In some cases, clinical monitoring may suffice, typically accompanied by supportive care for hydration and electrolytes and thiamine supplementation. For those patients in need of pharmacological treatment, benzodiazepines (e.g., diazepam, chlordiazepoxide, lorazepam, oxazepam, and midazolam) are the most commonly used medications to treat alcohol withdrawal syndrome. Benzodiazepines work by enhancing the effect of the GABA neurotransmitter at the GABAA receptor. Notably, benzodiazepines represent the gold standard treatment, as they are the only class of medications that not only reduces the severity of the alcohol withdrawal syndrome but also reduces the risk of withdrawal seizures and/or delirium tremens. Because of the potential for benzodiazepine abuse and the risk of overdose, if benzodiazepine treatment for alcohol withdrawal syndrome is managed in an outpatient setting, careful monitoring is required, particularly when combined with alcohol and/or opioid medications (17).
a-2 agonists (e.g., clonidine) and β-blockers (atenolol) are sometimes used as an adjunct treatment to benzodiazepines to control neuro-autonomic manifestations of alcohol withdrawal not fully controlled by benzodiazepine administration (18). However, because of the lack of efficacy of a-2 agonists and β-blockers in preventing severe alcohol withdrawal syndrome and the risk of masking withdrawal symptoms, these drugs are recommended not as monotherapy, but only as a possible adjunctive treatment.
Of critical importance to a successful outcome is the fact that alcohol withdrawal treatment provides an opportunity for the patient and the health care provider to engage the patient in a treatment program aimed at achieving and maintaining long-term abstinence from alcohol or reductions in drinking. Such a treatment may include pharmacological and/or psychosocial tools, as summarized in the next sections.
PHARMACOLOGICAL APPROACHES TO THE TREATMENT OF ALCOHOL USE DISORDER
U.S. Food and Drug Administration–approved pharmacological treatments
Development of novel pharmaceutical reagents is a lengthy, costly, and expensive process. Once a new compound is ready to be tested for human research use, it is typically tested for safety first via phase 0 and phase 1 clinical studies in a very limited number of individuals. Efficacy and side effects may then be further tested in larger phase 2 clinical studies, which may be followed by larger phase 3 clinical studies, typically conducted in several centers and are focused on efficacy, effectiveness, and safety. If approved for use in clinical practice, this medication is still monitored from a safety standpoint, via phase 4 postmarketing surveillance.
Only three drugs are currently approved by the U.S. Food and Drug Administration (FDA) for use in alcohol use disorder. The acetaldehyde dehydrogenase inhibitor disulfiram was the first medication approved for the treatment of alcohol use disorder by the FDA, in 1951. The most common pathway in alcohol metabolism is the oxidation of alcohol via alcohol dehydrogenase, which metabolizes alcohol to acetaldehyde, and aldehyde dehydrogenase, which converts acetaldehyde into acetate. Disulfiram leads to an irreversible inhibition of aldehyde dehydrogenase and accumulation of acetaldehyde, a highly toxic substance. Although additional mechanisms (e.g., inhibition of dopamine β-hydroxylase) may also play a role in disulfiram’s actions, the blockade of aldehyde dehydrogenase activity represents its main mechanism of action. Therefore, alcohol ingestion in the presence of disulfiram leads to the accumulation of acetaldehyde, resulting in numerous related unpleasant symptoms, including tachycardia, headache, nausea, and vomiting. In this way, disulfiram administration paired with alcohol causes the aversive reaction, initially proposed as a remedy for alcohol use disorder by Rush (11) in 1784. One challenge in conducting a double-blind, placebo-controlled alcohol trial of disulfiram is that it is easy to break the blind unless the “placebo” medication also creates an aversive reaction when consumed with alcohol, which would then provide the same mechanism of action as the medication (e.g., the placebo and disulfiram would both have the threat of an aversive reaction). Open-label studies of disulfiram do provide support for its efficacy, as compared to controls, with a medium effect size (19), as defined by Cohen’s d effect size ranges of small d = 0.2, medium d = 0.5, and large d = 0.8 (20). The efficacy of disulfiram largely depends on patient motivation to take the medication and/or supervised administration, given that the medication is primarily effective by the potential threat of an aversive reaction when paired with alcohol (21).
The next drug approved for treatment of alcohol use disorder was acamprosate; first approved as a treatment for alcohol dependence in Europe in 1989, acamprosate has subsequently been approved for use in the United States, Canada, and Japan. Although the exact mechanisms of acamprosate action are still not fully understood, there is evidence that it targets the glutamate system by modulating hyperactive glutamatergic states, possibly acting as an _N_-methyl-d-aspartate receptor agonist (22). The efficacy of acamprosate has been evaluated in numerous double-blind, randomized controlled trials and meta-analyses, with somewhat mixed conclusions (23–26). Although a meta-analysis conducted in 2013 (25) indicated small to medium effect sizes in favor of acamprosate over placebo in supporting abstinence, recent large-scale trials conducted in the United States (27) and Germany (28) failed to find effects of acamprosate distinguishable from those of a placebo. Overall, there is evidence that acamprosate may be more effective in promoting abstinence and preventing relapse in already detoxified patients than in helping individuals reduce drinking (25), therefore suggesting its use as an important pharmacological aid in treatment of abstinent patients with alcohol use disorder. The most common side effect with acamprosate is diarrhea. Other less common side effects may include nausea, vomiting, stomachache, headache, and dizziness, although the causal role of acamprosate in giving these side effects is unclear.
A third drug, the opioid receptor antagonist naltrexone, was approved for the treatment of alcohol dependence by the FDA in 1994. Later, a monthly extended-release injectable formulation of naltrexone, developed with the goal of improving patient adherence, was also approved by the FDA in 2006. Naltrexone reduces craving for alcohol and has been found to be most effective in reducing heavy drinking (25). The efficacy of naltrexone in reducing relapse to heavy drinking, in comparison to placebo, has been supported in numerous meta-analyses (23–25), although there is less evidence for its efficacy in supporting abstinence (25). Fewer studies have been conducted with the extended-release formulation, but its effects on heavy drinking, craving, and quality of life are promising (29, 30). Common side effects of naltrexone may include nausea, headache, dizziness, and sleep problems. Historically, naltrexone’s package insert has been accompanied by a risk of hepatotoxicity, a precaution primarily due to observed liver toxicity in an early clinical trial with administrating a naltrexone dosage of 300 mg per day to obese men (31). However, there is no published evidence of severe liver toxicity at the lower FDA-approved dosage of naltrexone for alcohol use disorder (50 mg per day). Nonetheless, transient, asymptomatic hepatic transaminase elevations have also been observed in some clinical trials and in the postmarketing period; therefore, naltrexone should be used with caution in patients with active liver disease and should not be used in patients with acute hepatitis or liver failure.
Additional pharmacological treatments approved for alcohol use disorder in Europe
Disulfiram, acamprosate, and naltrexone have been approved for use in Europe and in the United States. Pharmacologically similar to naltrexone, nalmefene was also approved for the treatment of alcohol dependence in Europe in 2013. Nalmefene is a m- and d-opioid receptor antagonist and a partial agonist of the k-opioid receptor (32). Side effects of nalmefene are similar to naltrexone; compared to naltrexone, nalmefene has a longer half-life. Meta-analyses have indicated that nalmefene is effective in reducing heavy drinking days (32). An indirect meta-analysis of these two drugs concluded that nalmefene may be more effective than naltrexone (33), although whether a clinically relevant difference between the two medications really exists is still an open question (34). Network meta-analysis and microsimulation studies suggest that nalmefene may have some benefits over placebo for reducing total alcohol consumption (35, 36). The approval of nalmefene in Europe was accompanied by some controversy (37); a prospective head-to-head trial of nalmefene and naltrexone could help clarify whether nalmefene has added benefits to the existing medications available for alcohol use disorder. Last, nalmefene was approved in Europe as a medication that can be taken “as needed” (i.e., on days when drinking was going to occur). Prior work has also demonstrated the efficacy of taking naltrexone only on days that drinking was potentially going to occur (38).
In addition to these drugs, a GABAB receptor agonist used to treat muscle spasms, baclofen, was approved for treatment of alcohol use disorder in France in 2018 and has been used off label for alcohol use disorder for over a decade in other countries, especially in other European countries and in Australia (39, 40). Recent human laboratory work suggests that baclofen may disrupt the effects of an initial priming dose of alcohol on subsequent craving and heavy drinking (41). Meta-analyses and systematic reviews examining the efficacy of baclofen have yielded mixed results (35, 39, 42); however, there is some evidence that baclofen might be useful in treatment of alcohol use disorder among individuals with liver disease (43, 44). Evidence of substantial heterogeneity in baclofen pharmacokinetics among different individuals with alcohol use disorder (41) could explain the variability in the efficacy of baclofen across studies. The appropriate dose of baclofen for use in treatment of alcohol use disorder remains a controversial topic, and a recent international consensus statement highlighted the importance of tailoring doses based on safety, tolerability, and efficacy (40).
Promising pharmacological treatments
Numerous other medications have been used off label in the treatment of alcohol use disorder, and many of these have been shown to be modestly effective in meta-analyses and systematic reviews (23, 24, 26, 35). Systematic studies of these medications suggest promising findings for topiramate, ondansetron, gabapentin, and varenicline. The anticonvulsant drug topiramate represents one of the most promising medications in terms of efficacy, based on its medium effect size from several clinical trials [for a review, see (45)], including a multisite clinical study (46). One strength of topiramate is the possibility of starting treatment while people are still drinking alcohol, therefore serving as a potentially effective treatment to initiate abstinence (or to reduce harm) rather than to prevent relapse in already detoxified patients (45). Although not approved by the FDA, it is worth noticing that topiramate is a recommended treatment for alcohol use disorder in the U.S. Department of Veterans Affairs (47). A concern with topiramate is the potential for significant side effects, especially those affecting cognition and memory, warranting a slow titration of its dose and monitoring for side effects. Furthermore, recent attention has been paid on zonisamide, another anticonvulsant medication, whose pharmacological mechanisms of actions are similar to topiramate but with a better tolerability and safety profile (48). Recently published and ongoing research focuses on a potential pharmacogenetic approach to treatment in the use of topiramate to treat alcohol use disorder, based on the possibility that both efficacy and tolerability and safety of topiramate may be moderated by a functional single-nucleotide polymorphism (rs2832407) in GRIK1, encoding the kainate GluK1 receptor subunit (49). Human laboratory studies (50) and treatment clinical trials (51) have also used a primarily pharmacogenetic approach to testing the efficacy of the antinausea drug ondansetron, a 5HT3 antagonist, in alcohol use disorder. Overall, these studies suggest a potential role for ondansetron in alcohol use disorder, but only in those individuals with certain variants of the genes encoding the serotonin transporter 5-HTT and the 5-HT3 receptor. The anticonvulsant gabapentin has shown promising results in human laboratory studies and clinical trials (52–54), although a more recent multisite trial with an extended-release formulation of the medication did not have an effect of gabapentin superior to that of a placebo (55). Although the latter findings might be related to potential pharmacokinetic issues secondary to the specific formulation used, it is nonetheless possible that gabapentin may be more effective in patients with more clinically relevant alcohol withdrawal symptoms (52). Several human laboratory studies support a role for varenicline, a nicotinic acetylcholine receptor partial agonist approved for smoking cessation, in alcohol use disorder [for a review, see (56)], and two of three clinical trials also support its efficacy on alcohol outcomes (57–59), especially in heavy drinkers who are males (59) and in male and female alcohol-dependent individuals who are also smokers (60). Additional details on the FDA-approved medications and other medications tested in clinical research settings for the treatment of alcohol use disorder are summarized in Table 2.
Table 2. FDA-approved medications and other medications tested in clinical research settings (phase 2 or 3 medication trials) for the treatment of alcohol use disorder.
FDA, U.S. Food and Drug Administration; AMPA, α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid; NMDA, _N_-methyl-d-aspartate; PO, per os (oral); IM, intramuscular; HT, serotonin.
| FDA-approved medications for alcohol use disorder | ||
|---|---|---|
| Daily total dose | Pharmacological mechanism(s) and additional information | |
| Acamprosate (PO) | 1998 mg per day | Unclear—it has been suggested that acamprosate isa modulator of hyperactive glutamatergic states,possibly as an NMDA receptor agonist |
| Disulfiram (PO) | 250–500 mg per day | Inhibition of acetaldehyde dehydrogenase |
| Naltrexone (PO) | 50 mg per day | m-opioid receptor antagonist |
| Naltrexone (IM) | 380 mg once a month | m-opioid receptor antagonist |
| Not FDA-approved medications tested for alcohol use disorder | ||
| Baclofen (PO) | 30–80 mg per day | GABAB receptor agonist |
| Approved in France by the National Agency for theSafety of Medicines and Healthcare Products | ||
| Gabapentin (PO) | 900–1800 mg per day | Unclear—the most likely mechanism is blockade ofvoltage-dependent Ca2+ channels. Although it is aGABA analog, gabapentin does not seem to act onthe GABA receptors |
| Nalmefene (PO) | 18 mg per day | m- and d-opioid receptor antagonist and k-opioidreceptor partial agonist |
| Approved in Europe by the European MedicinesAgency | ||
| Ondansetron (PO) | 0.5 mg per day (fixed dose) or up to36 mcg/kg per day | 5HT3 antagonist |
| Prazosin/doxazosin (PO) | Up to 16 mg per day | a-1 receptor antagonists |
| Topiramate (PO) | Up to 300 mg per day | Topiramate is an anticonvulsant with multipletargets. It increases GABAA-facilitated neuronalactivity and simultaneously antagonizes AMPAand kainate glutamate receptors. It also inhibitsl-type calcium channels, limits the activity ofvoltage-dependent sodium channels andfacilitates potassium conductance. Furthermore, itis a weak inhibition of the carbonic anhydraseisoenzymes, CA-II and CA-IV |
| Varenicline (PO) | 2 mg per day | Nicotinic acetylcholine receptor partial agonist |
The medications and targets described above have shown promising results in phase 2 or phase 3 medication trials. However, owing to the development of novel neuroscience techniques, a growing and exciting body of data is expanding the armamentarium of targets currently under investigation in animal models and/or in early-phase clinical studies. Pharmacological approaches with particular promise for future drug development include, but are not limited to the following [for recent reviews, see, e.g., (56, 61–68)]: the antipsychotic drug aripiprazole, which has multiple pharmacological actions (mainly on dopamine and serotonin receptors), the antihypertensive alpha-1 blocker drugs prazosin and doxazosin, neurokinin-1 antagonism, the glucocorticoid receptor blocker mifepristone, vasopressin receptor 1b antagonism, oxytocin, ghrelin receptor antagonism, glucagon-like peptide-1 agonism, and pharmacological manipulations of the nociception receptor (We are intentionally using a general pharmacological terminology for the nociceptin receptor, given that it is unclear whether agonism, antagonism, or both may represent the best approach.). New medications development is particularly important for the treatment of comorbid disorders that commonly co-occur among individuals with alcohol use disorder, particularly affective disorders, anxiety disorders, suicidality, and other substance use disorders. This aspect of alcohol use disorder is relevant to the fact that addictive disorders often present with significantly more severe symptoms when they coexist with other mental health disorders (69). Likewise, there is evidence that pharmacotherapy is most effective when implemented in conjunction with behavioral interventions (70), and all phase 2 and phase 3 medication trials, mentioned above, have included a brief psychosocial behavioral treatment in combination with medication.
BEHAVIORAL/PSYCHOLOGICAL TREATMENTS FOR ALCOHOL USE DISORDER
Evidence-based treatments
A wide range of behavioral and psychological treatments are available for alcohol use disorder, and many treatments are equally effective in supporting abstinence or drinking reduction goals (71–74). Treatments with the greatest evidence of efficacy range from brief interventions, including motivational interviewing approaches, to operant conditioning approaches, including contingency management and the community reinforcement approach, to cognitive behavioral treatments, including coping skills training and relapse prevention, and to acceptance- and mindfulness-based approaches. Twelve-step facilitation, which was designed specifically to connect individuals with mutual support groups, has also been shown to be effective (75). In addition, harm reduction treatments, including guided self-control training and controlled drinking interventions, have been successful in supporting drinking reduction goals (70).
Meta-analyses and systematic reviews have found that brief interventions, especially those based on the principles of motivational interviewing, are effective in the treatment of alcohol use disorder. These interventions can include self-monitoring of alcohol use, increasing awareness of high-risk situations, and training in cognitive and behavioral techniques to help clients cope with potential drinking situations, as well as life skills training, communication training, and coping skills training. Cognitive behavioral treatments can be delivered in individual or group settings and can also be extended to the treatment of families and couples (72, 73).
Acceptance- and mindfulness-based interventions are increasingly being used to target alcohol use disorder and show evidence of efficacy in a variety of settings and formats, including brief intervention formats (76). Active ingredients include raising present moment awareness, developing a nonjudgmental approach to self and others, and increasing acceptance of present moment experiences. Acceptance- and mindfulness-based interventions are commonly delivered in group settings and can also be delivered in individual therapy contexts.
Computerized, web-based, and mobile interventions have also been developed, incorporating the principles of brief interventions, behavioral and cognitive behavioral approaches, as well as mindfulness and mutual support group engagement; many of these approaches have demonstrated efficacy in initial trials (77–79). For example, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) has developed the Take Control computerized intervention that includes aspects of motivational interviewing and coping skills training and was designed to provide psychosocial support (particularly among those assigned to the placebo medication) and also to increase adherence and retention among individuals enrolled in pharmacotherapy trials (80).
Mutual support group (e.g., A.A. and SMART) attendance and engagement have been shown to be associated with recovery from alcohol use disorder, even in the absence of formal treatment (81). However, selection biases (e.g., people selecting to attend these groups) raise difficulties in assessing whether other factors that are associated with treatment effectiveness may be the active ingredients for improving outcomes among those who attend mutual support groups. For example, individuals who are highly motivated to change might be more likely to attend mutual support groups. Likewise, mutual support groups often provide individuals with increased social network support for abstinence (82). Motivation to change and having a social network that supports abstinence (or reductions in drinking) are both factors that are associated with greater treatment effectiveness (83).
As noted above, most behavioral and psychological treatments are equally effective with small effect size differences [Cohen’s _d_ = 2.0 to 0.3 (20)] between active treatments (84–88). Behavioral interventions have also been shown to be as effective as pharmacotherapy options, with a 16-week cognitive behavioral intervention shown to be statistically equivalent to naltrexone in reducing heavy drinking days in a large randomized trial (27). One of the challenges of examining behavioral interventions in randomized trials is that intervention blinding and placebo controls cannot be implemented in most contexts, other than in computerized interventions. Furthermore, the general therapeutic factors common to most behavioral interventions (e.g., therapist empathy and supportive therapeutic relationship) in treatment of alcohol use disorder are as powerful as the specific therapeutic targets of specific behavioral interventions (e.g., teaching skills in a cognitive behavioral treatment) in facilitating behavioral change (89).
Promising future behavioral treatments and neuromodulation treatments
With respect to behavioral treatments, there are numerous opportunities for the development of novel mobile interventions that could provide treatment and recovery support in near real time. This mobile technology may also extend the reach of treatments to individuals with alcohol use disorder, particularly in rural areas. On the basis of a contextual self-regulation model of alcohol use (90), it is critical to address the immediate situational context alongside the broader social, environmental, and familial context in which an individual experiences the world and engages in momentary decision-making. Ambulatory assessment, particularly tools that require only passive monitoring (e.g., GPS, heart rate, and skin conductance) and real-time support via mobile health, could provide immediate environmental supports and could extend the reach of medications and behavioral treatments for alcohol use disorder. For example, a mobile device could potentially signal a high-risk situation by indicating the geographic location (near a favorite drinking establishment) and the heart rate (increased heart rate when approaching the establishment). The device could provide a warning either to the individual under treatment and/or to a person supporting that individual’s recovery. In addition, developments in alcohol sensing technology (e.g., transdermal alcohol sensors) could greatly increase rigor of research on alcohol use disorder and also provide real-time feedback on alcohol consumption levels to individuals who are attempting to moderate and/or reduce their alcohol use.
Recent advances in neuromodulation techniques may also hold promise for the development of novel treatments for alcohol use disorder. Deep brain stimulation, transcranial magnetic stimulation, transcranial electrical stimulation (including transcranial direct current stimulation and transcranial alternating current stimulation), and real-time neurofeedback have recently been tested as potential treatments for addiction, although evidence in favor of these treatments is currently uncertain and focused mostly on intermediate targets (e.g., alcohol craving) (91). These techniques attempt to directly target specific brain regions and addiction-related cognitive processes via surgically implanted electrodes (deep brain stimulation), electrical currents or magnetic fields applied to the scalp (transcranial electrical and magnetic stimulation, respectively), or individual self-generated modulation via feedback (neurofeedback). Although robust large scale trials with double-blind, sham controls, and long-term follow-ups of alcohol behavior change and relapse have not been conducted (91), the heterogeneity of alcohol use disorder suggests that targeting one specific neural region may be insufficient to treat such a complex disorder, with its multiple etiologies and diverse clinical courses (92).
Factors contributing to the effectiveness of treatments
Numerous models have examined factors that predict treatment readiness, treatment engagement, and treatment outcomes for alcohol use disorder. The transtheoretical model of change proposes that an individual’s own readiness to change his or her drinking behavior may have an impact on treatment engagement and effectiveness (93). The dynamic model of relapse proposes the involvement of multiple interacting biological, psychological, cognitive, emotional, social, and situational risk factors that are static and dynamic in their association with treatment outcomes (83). Neurobiological models of addiction focus on the brain reward and stress system dysfunction that contributes to the development and maintenance of alcohol use disorder, that is, the “addiction cycle” (15, 16). The alcohol and addiction research domain criteria (AARDoC) (92), which have been operationalized in the addictions neuroclinical assessment (94), focus on the following three domains that correspond to particular phases in the addiction cycle: incentive salience in the binge/intoxication phase, negative emotionality in the withdrawal/negative affect phase, and executive function in the preoccupation/anticipation phase. Within each domain of the AARDoC, the addictions neuroclinical assessment proposes constructs that can be measured at multiple levels of analysis, such as craving in the incentive salience domain, negative affect and emotion dysregulation in the negative emotionality domain, and cognitive impairment and impulsivity in the executive function domain. The AARDoC acknowledge that environmental and contextual factors play a role in alcohol use disorder and treatment outcomes. Moreover, because of the heterogeneity of alcohol use disorder, the significance of these domains in causing alcohol use disorder and alcohol-related problems will vary among individuals.
Each of the abovementioned theoretical models proposes factors that may affect treatment effectiveness; however, many of the constructs proposed in each of these models are overlapping and likely contribute to the effectiveness of alcohol use disorder treatment across a range of populations and settings. A heuristic model combining components from each of these models is shown in Fig. 1. Specifically, this model highlights the precipitants of alcohol use that are influenced by the neurobiological adaptations proposed in the addiction cycle (indicated by bold font) and additional contextual factors (regular font) that decrease or increase the likelihood of drinking in context, depending on whether an individual uses effective coping regulation in the moment. The domains supporting alcohol use/coping regulation (negative emotionality, executive function, incentive salience, and social environment) may interact to predict alcohol use or coping regulation in the moment. For example, network support for abstinence could improve decision-making and decrease likelihood of drinking. Conversely, experiences of physical pain are associated with increases in negative affect and poorer executive function, which could both increase likelihood of drinking. Both of these examples require environmental access to alcohol and a desire to drink alcohol. Treatment effectiveness will depend on the extent to which a particular treatment targets those risk factors that are most likely to increase or decrease the likelihood of drinking for each individual, as well as the personal resources that each individual brings to treatment and/or that could be enhanced in treatment. A functional analysis of contextual risk and protective factors can be critically important in guiding treatment.
Fig. 1. Conceptual model of factors that affect treatment effectiveness.
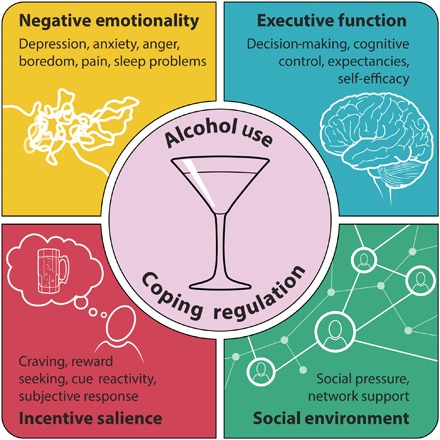
Risk factors proposed in the AARDoC, including incentive salience, negative emotionality, executive function, and social environmental factors, are shown in black bold font encircling alcohol use. Contextual risk factors, including decision-making, self-efficacy, pain, craving, etc., are shown in black font in colored boxes. Risk and protective factors overlap with alcohol use and interact in predicting coping regulation and alcohol use among individual patients.
For example, there is considerable heterogeneity in treatment response to naltrexone, which may vary in efficacy in some individuals. Recent studies conducted to determine whether certain patients may benefit more from naltrexone have yielded mixed findings (95). Promising evidence suggests that individuals with the OPRM1 A118G G (Asp40) allele may have a better response to naltrexone (96–98); however, a prospective study of medication response among individuals stratified by presence of the Asp40 allele did not provide support for the genotype by treatment interaction (99), and recent human laboratory studies have not confirmed the hypothesized mechanisms underlying the pharmacogenomic effect (100). Initial evidence suggests that naltrexone may be more effective in reducing heavy drinking among smokers (101) and among those with a larger number of heavy drinkers in their social networks (102). With respect to reinforcement typologies, recent work has found that naltrexone may be more effective among those who tend to drink alcohol for rewarding effects (103), and acamprosate may also be more effective for individuals who drink to relieve negative affect (104).
GAPS IN SCIENTIFIC KNOWLEDGE AND NEW RESEARCH DIRECTIONS
Heterogeneity of individuals with alcohol use disorder
This review has briefly summarized the treatments currently available for alcohol use disorder that are relatively effective, at least in some patients. Many new treatments are also being developed, and some of them seem promising. Nevertheless, numerous gaps in scientific knowledge remain. Notably, most people who drink alcohol do not develop an alcohol use disorder, most people with alcohol use disorder do not seek treatment, and most of those who do not seek treatment “recover” from alcohol use disorder without treatment (2). Very little is known about factors, particularly neurobiological, genetic, and epigenetic factors, that predict the transition from alcohol use to alcohol use disorder, although basic science models suggest that a cycle of neuroadaptations could be at play (15, 16). We also lack a basic understanding of how individuals recover from alcohol use disorder in the absence of treatment and what neurobiological, psychological, social, and environmental factors are most important for supporting recovery from alcohol use disorder. Gaining a better understanding of recovery in the absence of treatment, particularly modifiable psychological, neurobiological, and epigenetic factors, could provide novel insights for medications and behavioral treatment development. Among many other factors, special attention is needed in future studies to shed light on the role of sex and gender in the development and maintenance of alcohol use disorder and on the response to pharmacological, behavioral, and other treatments.
The heterogeneity of alcohol use disorder presents a major challenge to scientific understanding and to the development of effective treatments for prevention and intervention (92). For example, a DSM-5 diagnosis of alcohol use disorder requires 2 or more symptoms, out of 11, over the past year. That requirement equates to exactly 2048 potential symptom combinations that would meet the criteria of alcohol use disorder. An individual who only meets criteria for tolerance and withdrawal (i.e., physiological dependence) likely requires a very different course of treatment from an individual who only meets the criteria for failure to fulfill role obligations and use of alcohol in hazardous situations. Gaining a better understanding of the etiology and course of alcohol use disorder, as well as identifying whether different subtypes of drinkers may respond better to certain treatments (103, 104), is critical for advancing the science of alcohol use disorder prevention and treatment. Alternative conceptualizations of alcohol use disorder may also aid in improving our understanding of the disorder and reducing heterogeneity. For example, the pending International Classification of Diseases, 11th edition, will simplify the diagnosis of alcohol dependence to requiring only two of three criteria in the past 12 months: (i) impaired control over alcohol use; (ii) alcohol use that dominates over other life activities; and (iii) persistence of alcohol use despite consequences. The diagnosis will be made with or without physiological dependence, as characterized by tolerance, withdrawal, or repeated use to prevent or alleviate withdrawal (105). It remains to be seen whether simplification of the criteria set will narrow our conceptualization or potentially increase heterogeneity of this disorder among those diagnosed with alcohol dependence.
Placebo effect
An additional challenge to development of pharmacological treatments for alcohol use disorder is the high placebo response rates seen in drug trials (106). The tendency for individuals to have a good treatment response when assigned to placebo medication reflects both the high probability of recovery without treatment and the heterogeneity in the disorder itself. Many people who enter treatment are already motivated to change behavior, and receiving a placebo medication can help these individuals continue the process of change. Gaining a better understanding of which kinds of individuals respond to placebo and of the overall physiological and behavioral complexities in the placebo response is critical to identifying those individuals who will benefit the most from active medication. More generally, very little is understood about how motivation to change drinking behavior may influence the efficacy of active medications, particularly via adherence mechanisms. Additional research on targeted (i.e., as needed) dosing of medications, such as nalmefene and naltrexone (32, 38), would be promising from the perspective of increasing adherence to medications and also raising awareness of potentially heavy drinking occasions.
Recent developments in pharmacological and behavioral approaches
In addition to gaining a better understanding of the disorder and who benefits from existing treatments, the examination of molecular targets for alcohol use disorder could open up multiple innovative directions for future translational research on the treatment of alcohol use disorder. Recent research has identified many targets that might be important for future medication trials (67). For example, most of the medication development efforts in past decades have focused on pathways and targets typically related to reward processing and positive reinforcement. While important, this approach ignores the important role of stress-related pathways (e.g., corticotropin release factor and other related pathways) in negative reinforcement and in the later stages of alcohol use disorder, which is often characterized by physical dependence, anxiety, and relief drinking [for reviews, see (15, 16)]. Furthermore, it is also becoming more and more apparent that other promising targets may be identified by looking at the brain not as an isolated system but rather as an organ with bidirectional interactions with peripheral systems. Examples of the latter approach include the growing evidence suggesting a potential role of inflammation and neuroinflammation and of the gut-liver-brain axis in the neurobiological mechanisms that regulate the development and/or maintenance of alcohol use disorder (107–109). Moving medications development from phase 1 to phase 2 and 3 trials has also been a difficulty in the field. Future directions that might improve translation of basic science into clinical practice include the broader use of human laboratory models and pilot clinical trials (110), as well as expanding the outcomes that might be targeted in phase 2 and phase 3 trials to include drinking reduction outcomes (111, 112).
New directions for behavioral treatment development include a greater focus on identifying effective elements of behavioral treatments and on the components of treatment that are most critical for successful behavior change (89, 113). Studies investigating the effects of specific treatment components are critical for refining treatment protocols to more efficiently target the symptoms of alcohol use disorder. Continued development of mobile health interventions will also help with disseminating treatment to a wider range of individuals struggling with alcohol use disorder.
Translation of addiction science to clinical practice
Last, but not the least, there is also a critical need for more research on dissemination and implementation, given the fact that many treatment programs still do not incorporate evidence-based practices, such as cognitive behavioral skills training, mindfulness-based interventions, and medications. Both pharmacological and behavioral treatments for alcohol use disorder are markedly underused; the recent Surgeon General’s report Facing Addiction in America (114) highlights the fact that only about 1 in 10 people with a substance use disorder receives any type of specialty treatment. Therefore, basic science and human research efforts will need to be accompanied by translational approaches, where effective novel medications and precision medicine strategies are effectively translated from research settings to clinical practice. Greater integration of alcohol screening and medication in primary care and other clinical settings, as well as research on best methods for implementation, has great potential for expanding access to effective treatment options (115). Because the heterogeneity of alcohol use disorder makes it highly unlikely that one single treatment will work for all individuals, it is important to provide a menu of options for pharmacological and behavioral therapies to both clinicians and patients. Reducing the stigma of alcohol use disorder and moving toward a public health approach to addressing this problem may further increase the range of acceptable treatment options.
Acknowledgment
Funding: This research was supported by a grant from NIAAA (R01 AA022328) awarded to K.W. (principal investigator). R.Z.L. is funded by NIAAA. L.L. is jointly funded by NIAAA and the National Institute on Drug Abuse (NIDA) (ZIA-AA000218). The content of this review does not necessarily represent the official views of the funders. Author contributions: K.W. wrote the first draft of the manuscript. K.W., R.Z.L., and L.L. provided additional text and edits. All authors approved the final draft. Competing interests: The authors declare that they have no competing interests. Data and materials availability: All data needed to evaluate the conclusions in the paper are present in the paper and/or in the materials cited herein. Additional data related to this paper may be requested from the authors.
REFERENCES AND NOTES
- 1.World Health Organization, Global Status Report on Alcohol and Health 2018 (2018); www.who.int/substance_abuse/publications/global_alcohol_report/en/.
- 2.Substance Abuse and Mental Health Services Administration, Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53) (2018); www.samhsa.gov/data/.
- 3.Sacks J. J., Gonzales K. R., Bouchery E. E., Tomedi L. E., Brewer R. D., 2010 national and state costs of excessive alcohol consumption. Am. J. Prev. Med. 49, e73–e79 (2015). [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association, Diagnostic and Statistical Manual for Mental Disorders (American Psychiatric Publishing, ed. 5, 2013). [Google Scholar]
- 5.Grant B. F., Goldstein R. B., Saha T. D., Chou S. P., Jung J., Zhang H., Pickering R. P., Ruan W. J., Smith S. M., Huang B., Hasin D. S., Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiat. 72, 757–766 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51) (2016); www.samhsa.gov/data/.
- 7.Nutt D. J., King L. A., Phillips L. D.; Independent Scientific Committee on Drugs , Drug harms in the UK: A multicriteria decision analysis. Lancet 376, 1558–1565 (2010). [DOI] [PubMed] [Google Scholar]
- 8.Bouchery E. E., Harwood H. J., Sacks J. J., Simon C. J., Brewer R. D., Economic costs of excessive alcohol consumption in the U.S., 2006. Am. J. Prev. Med. 41, 516–524 (2011). [DOI] [PubMed] [Google Scholar]
- 9.Witkiewitz K., Dearing R. L., Maisto S. A., Alcohol use trajectories among non-treatment-seeking heavy drinkers. J. Stud. Alcohol Drugs 75, 415–422 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tuithof M., Ten Have M., van den Brink W., Vollebergh W., de Graaf R., Treatment seeking for alcohol use disorders: Treatment gap or adequate self-selection? Eur. Addict. Res. 22, 277–285 (2016). [DOI] [PubMed] [Google Scholar]
- 11.B. Rush, An Inquiry into the Effects of Ardent Spirits upon the Human Body and Mind: With an Account of the Means of Preventing, and of the Remedies for Curing Them (E. Merriam & Co., ed. 8 revised, 1784). [Google Scholar]
- 12.Baumohl J., Inebriate institutions in North America, 1840-1920. Br. J. Addict. 85, 1187–1204 (1990). [DOI] [PubMed] [Google Scholar]
- 13.White W. L., Kurtz E., Twelve defining moments in the history of alcoholics anonymous. Recent Dev. Alcohol. 18, 37–57 (2008). [DOI] [PubMed] [Google Scholar]
- 14.E. M. Jellinek, Alcohol Addiction and Chronic Alcoholism (Yale Univ. Press, 1942). [Google Scholar]
- 15.Koob G. F., Alcoholism: Allostasis and beyond. Alcohol. Clin. Exp. Res. 27, 232–243 (2003). [DOI] [PubMed] [Google Scholar]
- 16.Koob G. F., Volkow N. D., Neurobiology of addiction: A neurocircuitry analysis. Lancet Psychiatry 3, 760–773 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Votaw V. R., Witkiewitz K., Valeri L., Bogunovic O., McHugh R. K., Nonmedical prescription sedative/tranquilizer use in alcohol and opioid use disorders. Addict. Behav. 88, 48–55 (2019). [DOI] [PubMed] [Google Scholar]
- 18.Mirijello A., D’Angelo C., Ferrulli A., Vassallo G., Antonelli M., Caputo F., Leggio L., Gasbarrini A., Addolorato G., Identification and management of alcohol withdrawal syndrome. Drugs 75, 353–365 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skinner M. D., Lahmek P., Pham H., Aubin H. J., Disulfiram efficacy in the treatment of alcohol dependence: A meta-analysis. PlOS ONE 9, e87366 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.J. Cohen, Statistical Power Analysis For the Behavioral Sciences (Lawrence Erlbaum Associates, 1988). [Google Scholar]
- 21.Allen J. P., Litten R. Z., Techniques to enhance compliance with disulfiram. Alcohol. Clin. Exp. Res. 16, 1035–1041 (1992). [DOI] [PubMed] [Google Scholar]
- 22.Rösner S., Hackl-Herrwerth A., Leucht S., Lehert P., Vecchi S., Soyka M., Acamprosate for alcohol dependence. Cochrane Database Syst. Rev. 2010, Cd004332 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jonas D. E., Amick H. R., Feltner C., Bobashev G., Thomas K., Wines R., Kim M. M., Shanahan E., Gass C. E., Rowe C. J., Garbutt J. C., Pharmacotherapy for adults with alcohol use disorders in outpatient settings: A systematic review and meta-analysis. JAMA 311, 1889–1900 (2014). [DOI] [PubMed] [Google Scholar]
- 24.Kranzler H. R., Soyka M., Diagnosis and pharmacotherapy of alcohol use disorder: A review. JAMA 320, 815–824 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maisel N. C., Blodgett J. C., Wilbourne P. L., Humphreys K., Finney J. W., Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: When are these medications most helpful? Addiction 108, 275–293 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soyka M., Kranzler H. R., Hesselbrock V., Kasper S., Mutschler J., Möller H. J.; WFSBP Task Force on Treatment Guidelines for Substance Use Disorders , Guidelines for biological treatment of substance use and related disorders, part 1: Alcoholism, first revision. World J. Biol. Psychiatry 18, 86–119 (2017). [DOI] [PubMed] [Google Scholar]
- 27.Anton R. F., O’Malley S. S., Ciraulo D. A., Cisler R. A., Couper D., Donovan D. M., Gastfriend D. R., Hosking J. D., Johnson B. A., LoCastro J. S., Longabaugh R., Mason B. J., Mattson M. E., Miller W. R., Pettinati H. M., Randall C. L., Swift R., Weiss R. D., Williams L. D., Zweben A.; COMBINE Study Research Group , Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE study: A randomized controlled trial. JAMA 295, 2003–2017 (2006). [DOI] [PubMed] [Google Scholar]
- 28.Mann K., Lemenager T., Hoffmann S., Reinhard I., Hermann D., Batra A., Berner M., Wodarz N., Heinz A., Smolka M. N., Zimmermann U. S., Wellek S., Kiefer F., Anton R. F.; PREDICT Study Team , Results of a double-blind, placebo-controlled pharmacotherapy trial in alcoholism conducted in Germany and comparison with the US COMBINE study. Addict. Biol. 18, 937–946 (2013). [DOI] [PubMed] [Google Scholar]
- 29.Pettinati H. M., Gastfriend D. R., Dong Q., Kranzler H. R., O’Malley S. S., Effect of extended-release naltrexone (XR-NTX) on quality of life in alcohol-dependent patients. Alcohol. Clin. Exp. Res. 33, 350–356 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kranzler H. R., Wesson D. R., Billot L.; DrugAbuse Sciences Naltrexone Depot Study Group , Naltrexone depot for treatment of alcohol dependence: A multicenter, randomized, placebo-controlled clinical trial. Alcohol. Clin. Exp. Res. 28, 1051–1059 (2004). [DOI] [PubMed] [Google Scholar]
- 31.Mitchell J. E., Morley J. E., Levine A. S., Hatsukami D., Gannon M., Pfohl D., High-dose naltrexone therapy and dietary counseling for obesity. Biol. Psychiatry 22, 35–42 (1987). [DOI] [PubMed] [Google Scholar]
- 32.Mann K., Torup L., Sørensen P., Gual A., Swift R., Walker B., van den Brink W., Nalmefene for the management of alcohol dependence: Review on its pharmacology, mechanism of action and meta-analysis on its clinical efficacy. Eur. Nueropsychopharmacol. 26, 1941–1949 (2016). [DOI] [PubMed] [Google Scholar]
- 33.Soyka M., Friede M., Schnitker J., Comparing nalmefene and naltrexone in alcohol dependence: Are there any differences? Results from an indirect meta-analysis. Pharmacopsychiatry 49, 66–75 (2016). [DOI] [PubMed] [Google Scholar]
- 34.Swift R. M., Naltrexone and nalmefene: Any meaningful difference? Biol. Psychiatry 73, 700–701 (2013). [DOI] [PubMed] [Google Scholar]
- 35.Palpacuer C., Duprez R., Huneau A., Locher C., Boussageon R., Laviolle B., Naudet F., Pharmacologically controlled drinking in the treatment of alcohol dependence or alcohol use disorders: A systematic review with direct and network meta-analyses on nalmefene, naltrexone, acamprosate, baclofen and topiramate. Addiction 113, 220–237 (2018). [DOI] [PubMed] [Google Scholar]
- 36.Millier A., Laramée P., Rahhali N., Aballéa S., Daeppen J. B., Rehm J., Toumi M., Cost-effectiveness of nalmefene added to psychosocial support for the reduction of alcohol consumption in alcohol-dependent patients with high/very high drinking risk levels: A microsimulation model. J. Stud. Alcohol Drugs 78, 867–876 (2017). [DOI] [PubMed] [Google Scholar]
- 37.Palpacuer C., Laviolle B., Boussageon R., Reymann J. M., Bellissant E., Naudet F., Risks and benefits of nalmefene in the treatment of adult alcohol dependence: A systematic literature review and meta-analysis of published and unpublished double-blind randomized controlled trials. PLOS Med. 12, e1001924 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kranzler H. R., Tennen H., Armeli S., Chan G., Covault J., Arias A., Oncken C., Targeted naltrexone for problem drinkers. J. Clin. Psychopharmacol. 29, 350–357 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leggio L., Garbutt J. C., Addolorato G., Effectiveness and safety of baclofen in the treatment of alcohol dependent patients. CNS Neurol. Disord. Drug Targets 9, 33–44 (2010). [DOI] [PubMed] [Google Scholar]
- 40.Agabio R., Sinclair J. M. A., Addolorato G., Aubin H. J., Beraha E. M., Caputo F., Chick J. D., de la Selle P., Franchitto N., Garbutt J. C., Haber P. S., Heydtmann M., Jaury P., Lingford-Hughes A. R., Morley K. C., Müller C. A., Owens L., Pastor A., Paterson L. M., Pélissier F., Rolland B., Stafford A., Thompson A., van den Brink W., de Beaurepaire R., Leggio L., Baclofen for the treatment of alcohol use disorder: The Cagliari Statement. Lancet Psychiatry 5, 957–960 (2018). [DOI] [PubMed] [Google Scholar]
- 41.Farokhnia M., Deschaine S. L., Sadighi A., Farinelli L. A., Lee M. R., Akhlaghi F., Leggio L., A deeper insight into how GABA-B receptor agonism via baclofen may affect alcohol seeking and consumption: Lessons learned from a human laboratory investigation. Mol. Psychiatry 10.1038/s41380-018-0287-y (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minozzi S., Saulle R., Rösner S., Baclofen for alcohol use disorder. Cochrane Database Syst. Rev. 11, Cd012557 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Addolorato G., Leggio L., Ferrulli A., Cardone S., Vonghia L., Mirijello A., Abenavoli L., D’Angelo C., Caputo F., Zambon A., Haber P. S., Gasbarrini G., Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: Randomised, double-blind controlled study. Lancet 370, 1915–1922 (2007). [DOI] [PubMed] [Google Scholar]
- 44.Morley K. C., Baillie A., Fraser I., Furneaux-Bate A., Dore G., Roberts M., Abdalla A., Phung N., Haber P. S., Baclofen in the treatment of alcohol dependence with or without liver disease: Multisite, randomised, double-blind, placebo-controlled trial. Br. J. Psychiatry 212, 362–369 (2018). [DOI] [PubMed] [Google Scholar]
- 45.Kenna G. A., Lomastro T. L., Schiesl A., Leggio L., Swift R. M., Review of topiramate: An antiepileptic for the treatment of alcohol dependence. Curr. Drug Abuse Rev. 2, 135–142 (2009). [DOI] [PubMed] [Google Scholar]
- 46.Johnson B. A., Rosenthal N., Capece J. A., Wiegand F., Mao L., Beyers K., McKay A., Ait-Daoud N., Anton R. F., Ciraulo D. A., Kranzler H. R., Mann K., O’Malley S. S., Swift R. M., Topiramate for treating alcohol dependence: A randomized controlled trial. JAMA 298, 1641–1651 (2007). [DOI] [PubMed] [Google Scholar]
- 47.Department of Defense, VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders (2015); www.healthquality.va.gov/guidelines/MH/sud/VADoDSUDCPGProviderSummaryRevised22216.pdf.
- 48.Arias A. J., Feinn R., Oncken C., Covault J., Kranzler H. R., Placebo-controlled trial of zonisamide for the treatment of alcohol dependence. J. Clin. Psychopharmacol. 30, 318–322 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kranzler H. R., Covault J., Feinn R., Armeli S., Tennen H., Arias A. J., Gelernter J., Pond T., Oncken C., Kampman K. M., Topiramate treatment for heavy drinkers: Moderation by a GRIK1 polymorphism. Am. J. Psychiatry 171, 445–452 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kenna G. A., Zywiak W. H., Swift R. M., McGeary J. E., Clifford J. S., Shoaff J. R., Vuittonet C., Fricchione S., Brickley M., Beaucage K., Haass-Koffler C. L., Leggio L., Ondansetron reduces naturalistic drinking in nontreatment-seeking alcohol-dependent individuals with the LL 5′-HTTLPR genotype: A laboratory study. Alcohol. Clin. Exp. Res. 38, 1567–1574 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson B. A., Ait-Daoud N., Seneviratne C., Roache J. D., Javors M. A., Wang X. Q., Liu L., Penberthy J. K., DiClemente C. C., Li M. D., Pharmacogenetic approach at the serotonin transporter gene as a method of reducing the severity of alcohol drinking. Am. J. Psychiatry 168, 265–275 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anton R. F., Myrick H., Baros A. M., Latham P. K., Randall P. K., Wright T. M., Stewart S. H., Waid R., Malcolm R., Efficacy of a combination of flumazenil and gabapentin in the treatment of alcohol dependence: Relationship to alcohol withdrawal symptoms. J. Clin. Psychopharmacol. 29, 334–342 (2009). [DOI] [PubMed] [Google Scholar]
- 53.Mason B. J., Light J. M., Williams L. D., Drobes D. J., Proof-of-concept human laboratory study for protracted abstinence in alcohol dependence: Effects of gabapentin. Addict. Biol. 14, 73–83 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mason B. J., Quello S., Goodell V., Shadan F., Kyle M., Begovic A., Gabapentin treatment for alcohol dependence: A randomized controlled trial. JAMA Intern. Med. 174, 70–77 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Falk D. E., Ryan M. L., Fertig J. B., Devine E. G., Cruz R., Brown E. S., Burns H., Salloum I. M., Newport D. J., Mendelson J., Galloway G., Kampman K., Brooks C., Green A. I., Brunette M. F., Rosenthal R. N., Dunn K. E., Strain E. C., Ray L., Shoptaw S., Tiouririne N. A.-D., Gunderson E. W., Ransom J., Scott C., Leggio L., Caras S., Mason B. J., Litten R. Z.; National Institute on Alochol Abuse and Alcoholism Clinical Investigations Group (NCIG) Study Group , Gabapentin enacarbil extended-release for alcohol use disorder: A randomized, double-blind, placebo-controlled, multisite trial assessing efficacy and safety. Alcohol. Clin. Exp. Res. 43, 158–169 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Litten R. Z., Falk D. E., Ryan M. L., Fertig J., Leggio L., Advances in pharmacotherapy development: Human clinical studies. Handb. Exp. Pharmacol. 248, 579–613 (2018). [DOI] [PubMed] [Google Scholar]
- 57.Litten R. Z., A double-blind, placebo-controlled trial assessing the efficacy of varenicline tartrate for alcohol dependence. J. Addict. Med. 7, 277–286 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.de Bejczy A., Löf E., Walther L., Guterstam J., Hammarberg A., Asanovska G., Franck J., Isaksson A., Söderpalm B., Varenicline for treatment of alcohol dependence: A randomized, placebo-controlled trial. Alcohol. Clin. Exp. Res. 39, 2189–2199 (2015). [DOI] [PubMed] [Google Scholar]
- 59.O’Malley S. S., Zweben A., Fucito L. M., Wu R., Piepmeier M. E., Ockert D. M., Bold K. W., Petrakis I., Muvvala S., Jatlow P., Gueorguieva R., Effect of varenicline combined with medical management on alcohol use disorder with comorbid cigarette smoking. JAMA Psychiat. 75, 129–138 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Falk D. E., Castle I. J., Ryan M., Fertig J., Litten R. Z., Moderators of varenicline treatment effects in a double-blind, placebo-controlled trial for alcohol dependence: An exploratory analysis. J. Addict. Med. 2015, 296–303 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tunstall B. J., Carmack S. A., Koob G. F., Vendruscolo L. F., Dysregulation of brain stress systems mediates compulsive alcohol drinking. Curr. Opin. Behav. Sci. 13, 85–90 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schank J. R., Ryabinin A. E., Giardino W. J., Ciccocioppo R., Heilig M., Stress-related neuropeptides and addictive behaviors: Beyond the usual suspects. Neuron 76, 192–208 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Witkin J. M., Statnick M. A., Rorick-Kehn L. M., Pintar J. E., Ansonoff M., Chen Y., Tucker R. C., Ciccocioppo R., The biology of Nociceptin/Orphanin FQ (N/OFQ) related to obesity, stress, anxiety, mood, and drug dependence. Pharmacol. Ther. 141, 283–299 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farokhnia M., Faulkner M. L., Piacentino D., Lee M. R., Leggio L., Ghrelin: From a gut hormone to a potential therapeutic target for alcohol use disorder. Physiol. Behav. 204, 49–57 (2019). [DOI] [PubMed] [Google Scholar]
- 65.Lee M. R., Rohn M. C. H., Tanda G., Leggio L., Targeting the oxytocin system to treat addictive disorders: Rationale and progress to date. CNS Drugs 30, 109–123 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Haass-Koffler C. L., Swift R. M., Leggio L., Noradrenergic targets for the treatment of alcohol use disorder. Psychopharmacology 235, 1625–1634 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yardley M. M., Ray L. A., Medications development for the treatment of alcohol use disorder: Insights into the predictive value of animal and human laboratory models. Addict. Biol. 22, 581–615 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jerlhag E., GLP-1 signaling and alcohol-mediated behaviors; preclinical and clinical evidence. Neuropharmacology 136, 343–349 (2018). [DOI] [PubMed] [Google Scholar]
- 69.Tolliver B. K., Anton R. F., Assessment and treatment of mood disorders in the context of substance abuse. Dialogues Clin. Neurosci. 17, 181–190 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marlatt G. A., Witkiewitz K., Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment. Addict. Behav. 27, 867–886 (2002). [DOI] [PubMed] [Google Scholar]
- 71.Miller W. R., Wilbourne P. L., Mesa Grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction 97, 265–277 (2002). [DOI] [PubMed] [Google Scholar]
- 72.McCrady B. S., Owens M. D., Borders A. Z., Brovko J. M., Psychosocial approaches to alcohol use disorders since 1940: A review. J. Stud. Alcohol Drugs Suppl. 75 ( Suppl 17), 68–78 (2014). [DOI] [PubMed] [Google Scholar]
- 73.Witkiewitz K., Marlatt A., Behavioral therapy across the spectrum. Alcohol Res. Health 33, 313–319 (2011). [PMC free article] [PubMed] [Google Scholar]
- 74.Imel Z. E., Wampold B. E., Miller S. D., Fleming R. R., Distinctions without a difference: Direct comparisons of psychotherapies for alcohol use disorders. Psychol. Addict. Behav. 22, 533–543 (2008). [DOI] [PubMed] [Google Scholar]
- 75.Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J. Stud. Alcohol 58, 7–29 (1997). [PubMed] [Google Scholar]
- 76.Wilson A. D., Roos C. R., Robinson C. S., Stein E. R., Manuel J. A., Enkema M. C., Bowen S., Witkiewitz K., Mindfulness-based interventions for addictive behaviors: Implementation issues on the road ahead. Psychol. Addict. Behav. 31, 888–896 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kazemi D. M., Borsari B., Levine M. J., Li S., Lamberson K. A., Matta L. A., A systematic review of the mHealth interventions to prevent alcohol and substance abuse. J. Health Commun. 22, 413–432 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gustafson D. H., McTavish F. M., Chih M. Y., Atwood A. K., Johnson R. A., Boyle M. G., Levy M. S., Driscoll H., Chisholm S. M., Dillenburg L., Isham A., Shah D., A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiat. 71, 566–572 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kiluk B. D., Devore K. A., Buck M. B., Nich C., Frankforter T. L., LaPaglia D. M., Yates B. T., Gordon M. A., Carroll K. M., Randomized trial of computerized cognitive behavioral therapy for alcohol use disorders: Efficacy as a virtual stand-alone and treatment add-on compared with standard outpatient treatment. Alcohol. Clin. Exp. Res. 40, 1991–2000 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Devine E. G., Ryan M. L., Falk D. E., Fertig J. B., Litten R. Z., An exploratory evaluation of Take Control: A novel computer-delivered behavioral platform for placebo-controlled pharmacotherapy trials for alcohol use disorder. Contemp. Clin. Trials 50, 178–185 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kelly J. F., Bergman B., Hoeppner B. B., Vilsaint C., White W. L., Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug Alcohol Depend. 181, 162–169 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wu J., Witkiewitz K., Network support for drinking: An application of multiple groups growth mixture modeling to examine client-treatment matching. J. Stud. Alcohol Drugs 69, 21–29 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Witkiewitz K., Marlatt G. A., Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. Am. Psychol. 59, 224–235 (2004). [DOI] [PubMed] [Google Scholar]
- 84.Hennessy E. A., Tanner-Smith E. E., Mavridis D., Grant S. P., Comparative effectiveness of brief alcohol interventions for college students: Results from a network meta-analysis. Prev. Sci. 2019, 715–740 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jonas D. E., Garbutt J. C., Amick H. R., Brown J. M., Brownley K. A., C. L. Council, Viera A. J., Wilkins T. M., Schwartz C. J., Richmond E. M., Yeatts J., Swinson Evans T., Wood S. D., Harris R. P., Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann. Internal Med. 157, 645–654 (2012). [DOI] [PubMed] [Google Scholar]
- 86.Magill M., Ray L. A., Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. J. Stud. Alcohol Drugs 70, 516–527 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schmidt C. S., Schulte B., Seo H. N., Kuhn S., O’Donnell A., Kriston L., Verthein U., Reimer J., Meta-analysis on the effectiveness of alcohol screening with brief interventions for patients in emergency care settings. Addiction 111, 783–794 (2016). [DOI] [PubMed] [Google Scholar]
- 88.Tanner-Smith E. E., Risser M. D., A meta-analysis of brief alcohol interventions for adolescents and young adults: Variability in effects across alcohol measures. Am. J. Drug Alcohol Abuse 42, 140–151 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Magill M., Kiluk B. D., McCrady B. S., Tonigan J. S., Longabaugh R., Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: Progress 10 years later. Alcohol. Clin. Exp. Res. 39, 1852–1862 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Roos C. R., Witkiewitz K., A contextual model of self-regulation change mechanisms among individuals with addictive disorders. Clin. Psychol. Rev. 57, 117–128 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Luigjes J., Segrave R., de Joode N., Figee M., Denys D., Efficacy of invasive and non-invasive brain modulation interventions for addiction. Neuropsychol. Rev. 29, 116–138 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Litten R. Z., Ryan M. L., Falk D. E., Reilly M., Fertig J. B., Koob G. F., Heterogeneity of alcohol use disorder: Understanding mechanisms to advance personalized treatment. Alcohol. Clin. Exp. Res. 39, 579–584 (2015). [DOI] [PubMed] [Google Scholar]
- 93.Carbonari J. P., DiClemente C. C., Using transtheoretical model profiles to differentiate levels of alcohol abstinence success. J. Consult. Clin. Psychol. 68, 810–817 (2000). [PubMed] [Google Scholar]
- 94.Kwako L. E., Momenan R., Litten R. Z., Koob G. F., Goldman D., Addictions neuroclinical assessment: A neuroscience-based framework for addictive disorders. Biol. Psychiatry 80, 179–189 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Garbutt J. C., Greenblatt A. M., West S. L., Morgan L. C., Kampov-Polevoy A., Jordan H. S., Bobashev G. V., Clinical and biological moderators of response to naltrexone in alcohol dependence: A systematic review of the evidence. Addiction 109, 1274–1284 (2014). [DOI] [PubMed] [Google Scholar]
- 96.Anton R. F., Oroszi G., O’Malley S., Couper D., Swift R., Pettinati H., Goldman D., An evaluation of μ-Opioid receptor (OPRM1) as a predictor of naltrexone response in the treatment of alcohol Dependence. Arch. Gen. Psychiatry 65, 135–144 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chamorro A. J., Marcos M., Mirón-Canelo J. A., Pastor I., González-Sarmiento R., Laso F. J., Association of μ-opioid receptor (OPRM1) gene polymorphism with response to naltrexone in alcohol dependence: A systematic review and meta-analysis. Addict. Biol. 17, 505–512 (2012). [DOI] [PubMed] [Google Scholar]
- 98.Jonas D. E., Amick H. R., Feltner C., Wines R., Shanahan E., Rowe C. J., Garbutt J. C., Genetic polymorphisms and response to medications for alcohol use disorders: A systematic review and meta-analysis. Pharmacogenomics 15, 1687–1700 (2014). [DOI] [PubMed] [Google Scholar]
- 99.Oslin D. W., Leong S. H., Lynch K. G., Berrettini W., O’Brien C. P., Gordon A. J., Rukstalis M., Naltrexone vs placebo for the treatment of alcohol dependence. JAMA Psychiat. 72, 430–437 (2015). [DOI] [PubMed] [Google Scholar]
- 100.Sloan M. E., Klepp T. D., Gowin J. L., Swan J. E., Sun H., Stangl B. L., Ramchandani V. A., The OPRM1 A118G polymorphism: Converging evidence against associations with alcohol sensitivity and consumption. Neuropsychopharmacology 43, 1530–1538 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Anton R. F., Latham P. K., Voronin K. E., Randall P. K., Book S. W., Hoffman M., Schacht J. P., Nicotine-use/smoking is associated with the efficacy of naltrexone in the treatment of alcohol dependence. Alcohol. Clin. Exp. Res. 42, 751–760 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Worley M. J., Witkiewitz K., Brown S. A., Kivlahan D. R., Longabaugh R., Social network moderators of naltrexone and behavioral treatment effects on heavy drinking in the COMBINE study. Alcohol. Clin. Exp. Res. 39, 93–100 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mann K., Roos C. R., Hoffmann S., Nakovics H., Leménager T., Heinz A., Witkiewitz K., Precision medicine in alcohol dependence: A controlled trial testing pharmacotherapy response among reward and relief drinking phenotypes. Neuropsychopharmacology 43, 891–899 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Roos C. R., Mann K., Witkiewitz K., Reward and relief dimensions of temptation to drink: Construct validity and role in predicting differential benefit from acamprosate and naltrexone. Addict. Biol. 22, 1528–1539 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Poznyak V., Reed G. M., Medina-Mora M. E., Aligning the ICD-11 classification of disorders due to substance use with global service needs. Epidemiol. Psychiatr. Sci. 27, 212–218 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Litten R. Z., Castle I. J. P., Falk D., Ryan M., Fertig J., Chen C. M., Yi H. Y., The placebo effect in clinical trials for alcohol dependence: An exploratory analysis of 51 naltrexone and acamprosate studies. Alcohol. Clin. Exp. Res. 37, 2128–2137 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ch’Ng S. S., Lawrence A. J., Investigational drugs for alcohol use disorders: A review of preclinical data. Expert Opin. Investig. Drugs 27, 459–474 (2018). [DOI] [PubMed] [Google Scholar]
- 108.Temko J. E., Bouhlal S., Farokhnia M., Lee M. R., Cryan J. F., Leggio L., The microbiota, the gut and the brain in eating and alcohol use disorders: A “Menage a Trois”? Alcohol Alcohol 52, 403–413 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kenna G. A., Swift R. M., Hillemacher T., Leggio L., The relationship of appetitive, reproductive and posterior pituitary hormones to alcoholism and craving in humans. Neuropsychol. Rev. 22, 211–228 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ray L. A., Bujarski S., Roche D. J. O., Magill M., Overcoming the “Valley of Death” in medications development for alcohol use disorder. Alcohol. Clin. Exp. Res. 42, 1612–1622 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Falk D. E., O’Malley S. S., Witkiewitz K., Anton R. F., Litten R. Z., Slater M., Kranzler H. R., Mann K. F., Hasin D. S., Johnson B., Meulien D., Ryan M., Fertig J.; Alcohol Clinical Trials Initiative (ACTIVE) Workgroup , Evaluation of drinking risk levels as outcomes in alcohol pharmacotherapy trials: A secondary analysis of 3 randomized clinical trials. JAMA Psychiatry 76, 374–381 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Witkiewitz K., Hallgren K. A., Kranzler H. R., Mann K. F., Hasin D. S., Falk D. E., Litten R. Z., O'Malley S. S., Anton R. F., Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the world health organization risk drinking levels. Alcohol. Clin. Exp. Res. 41, 179–186 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Magill M., Bernstein M. H., Hoadley A., Borsari B., Apodaca T. R., Gaume J., Tonigan J. S., Do what you say and say what you are going to do: A preliminary meta-analysis of client change and sustain talk subtypes in motivational interviewing. Psychother. Res. 2018, 1–10 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Department of Health and Human Services (HHS), Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health (HHS, 2016). [PubMed] [Google Scholar]
- 115.Rehm J., Anderson P., Manthey J., Shield K. D., Struzzo P., Wojnar M., Gual A., Alcohol use disorders in primary health care: What do we know and where do we go? Alcohol Alcohol 51, 422–427 (2016). [DOI] [PubMed] [Google Scholar]
- 116.World Health Organization, ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th revision (World Health Organization, 2004). [Google Scholar]