Lantus (insulin glargine): Side effects, dosage, cost, and more (original) (raw)
Lantus is a brand-name prescription medication. It’s used to improve blood sugar levels in:
- adults and children ages 6 years and older with type 1 diabetes
- adults with type 2 diabetes
For more information about type 1 and type 2 diabetes and how Lantus is used to manage these conditions, see the “Lantus uses” section below.
Note: Lantus isn’t approved to treat diabetic ketoacidosis (DKA), which is a possible complication of diabetes. For more information about DKA, see the “Common questions about Lantus” section below.
Drug details
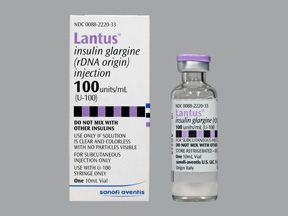
Lantus contains the drug insulin glargine, which is classified as a long-acting insulin.
Lantus is given as an injection just under your skin (a subcutaneous injection). The drug comes as a solution inside 10-milliliter (mL) vials that hold 100 units of insulin glargine per mL. The vial is used with needles, which aren’t included with the vial.
Lantus also comes as a prefilled SoloStar pen. Each pen contains 3 mL of drug solution that has 100 units of insulin per mL of solution.
Effectiveness
For information about the effectiveness of Lantus, see the “Lantus uses” section below.
The Food and Drug Administration (FDA) approves prescription drugs such as Lantus to treat certain conditions.
Lantus for type 2 diabetes
Lantus is FDA-approved to improve blood sugar levels in adults with type 2 diabetes.
Type 2 diabetes is a chronic (long-term) condition where your cells don’t respond to insulin as well as they should. Insulin is a hormone that enables sugar to pass from your blood into your cells. Because your cells don’t react to insulin the right way, they can’t get the energy they need to work properly. In addition, sugar levels build up in your blood. If not treated, this can lead to serious complications such as nerve damage.
Some people with type 2 diabetes need to take insulin because their body stops making insulin on its own.
You can learn more about this condition in our diabetes hub.
Note: Lantus isn’t approved to treat diabetic ketoacidosis (DKA), which is a possible complication of diabetes. For more information about DKA, see the “Common questions about Lantus” section below.
Lantus for type 1 diabetes
Lantus is approved by the FDA to improve blood sugar levels in adults and children with type 1 diabetes.
Type 1 diabetes is a chronic (long-term) condition where your pancreas doesn’t make insulin. Your body needs the hormone insulin to bring sugar into your cells, where sugar is used for energy. Without insulin, your cells can’t get the energy they need to work properly. It also leads to high blood sugar levels, which can cause serious problems if not treated.
People with type 1 diabetes need to take insulin to survive.
You can learn more about this condition in our diabetes hub.
Note: Lantus isn’t approved to treat DKA, which is a possible complication of diabetes. For more information about DKA, see the “Common questions about Lantus” section below.
Lantus for children
Lantus is FDA-approved to improve blood sugar levels in children ages 6 years and older with type 1 diabetes.
Most people with type 1 diabetes are diagnosed with the condition when they’re a child.
Lantus contains the active drug insulin glargine, which is a biologic medication. Biologics are made from parts of living organisms.
Lantus is currently available in a biosimilar form called Rezvoglar. Biosimilars are like a generic version of a biologic medication.
A “follow-on” insulin glargine drug called Basaglar is also available. Follow-on products are essentially the same as biosimilars, but they’re approved through an old pathway by the Food and Drug Administration (FDA). You can see the “Lantus vs. Basaglar” section below to learn how these drugs compare.
Basaglar and Rezvoglar are made with the same type of insulin as Lantus. The FDA considers biosimilars and follow-on drugs to be just as safe and effective as the original brand-name version.
Lantus can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Lantus. These lists don’t include all possible side effects.
For more information on the possible side effects of Lantus, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to notify the FDA about a side effect you’ve had with Lantus, you can do so through MedWatch.
More common side effects
The more common side effects* of Lantus can include:
- injection site reactions (redness or discoloration, itchiness, pain, or tenderness around the injection area)
- lipodystrophy (changes in skin thickness near the injection site)
- itchy skin
- rash
- edema (swelling), typically in your legs, ankles, or feet
- weight gain
- upper respiratory infections, such as the common cold
- hypoglycemia (low blood sugar levels)
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
* This is a partial list of more common side effects from Lantus. To learn about other side effects, talk with your doctor or pharmacist or check Lantus’ prescribing information.
Serious side effects
Serious side effects from Lantus aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Hypokalemia (low potassium levels). Symptoms can include:
- weakness
- fatigue (lack of energy)
- muscle cramping
- abnormal heart rhythm (a heartbeat that’s too fast, too slow, or uneven)
- paralysis (loss of movement in a body part)
- respiratory failure (meaning your lungs can’t release oxygen into your blood)
- Severe hypoglycemia (very low blood sugar levels).*
- Allergic reaction.*
* For more information on this side effect, see the “Side effect details” section below.
Side effect details
You may wonder how often certain side effects occur with this drug_._ Here’s some detail on some of the side effects this drug may cause. (In addition to the information below, you can also refer to this article about side effects of Lantus.)
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Lantus. But it’s not known how many people had an allergic reaction to Lantus during clinical studies.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
- a rash over your whole body
Call your doctor right away if you have a severe allergic reaction to Lantus. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Weight gain
Weight gain is one of the most common side effects of Lantus. In clinical studies, the average weight gain was:
- up to 1.5 pounds (lb) in adults with type 1 diabetes who took Lantus over 16 to 28 weeks
- up to 4.8 lb in children with type 1 diabetes who took Lantus and regular insulin for 28 weeks
- up to 4.4 lb in adults with type 2 diabetes who took Lantus for 1 year
Weight gain is a common side effect seen with all insulins, not just Lantus. This is a normal healthy process because insulin causes your body to store sugar for future energy needs.
If you’re concerned about weight gain while taking Lantus, talk with your healthcare team. They can suggest helpful diet and exercise tips.
Hypoglycemia
Hypoglycemia (low blood sugar levels) is one of the most common side effects of Lantus and other insulins.
It’s important to be aware of the symptoms of low blood sugar so you can fix it before it becomes severe. Symptoms of mild low blood sugar include:
- shakiness
- headache
- hunger
- dizziness
- fast heartbeat
- irritability
- nervousness
If your blood sugar levels get and stay too low, your symptoms can become a medical emergency. Symptoms of severe hypoglycemia (very low blood sugar levels) can include:
- drowsiness
- headache
- anxiety
- confusion
- hunger
- irritable mood (being easily upset)
- sweating
- fast heartbeat
- seizures
- coma
Also, it’s important to note that making any changes to your insulin treatment plan could increase your risk for both hypoglycemia and hyperglycemia (high blood sugar levels). These changes include using a new insulin product, taking a new dosage of insulin, or administering the drug differently than you usually do.
If you’re making any changes to your insulin treatment plan, talk with your doctor about your risk for hypoglycemia and hyperglycemia.
How common hypoglycemia is with Lantus
Clinical studies looked at adults who took Lantus for type 1 diabetes. A 16-week study found that 6.5% of the adults experienced at least one episode of severe hypoglycemia. And a 28-week study found that 10.6% of adults experienced severe hypoglycemia at least once.
Another study looked at children who took Lantus for type 1 diabetes. In this group, 23% of the children had an episode of severe hypoglycemia over a 6-month period.
In a 5-year clinical study in adults with type 2 diabetes, 7.8% of them had a severe hypoglycemic episode while taking Lantus with regular insulin.
What you can do for hypoglycemia
If your blood sugar is low, try to fix it right away. Eat or drink carbohydrates that are easy to digest so they can raise your blood sugar quickly. Some examples of these foods and drinks include:
- honey
- saltine crackers
- hard candy
- sugar
- glucose tablets
- regular (not diet) soda
If you’re at risk for frequent episodes of low blood sugar, talk with your doctor. They may give you a prescription for glucagon (a hormone) to quickly raise your blood sugar levels in an emergency.
Side effects in children
Side effects of Lantus in children are similar to those seen in adults.
However, in clinical studies of people with type 1 diabetes who took Lantus, children had more episodes of hypoglycemia (low blood sugar level) than did adults. In the 26-week study, 23% of children had at least one episode of severe low blood sugar. This was compared to 10.6% of adults in a 28-week study.
If you’re a parent or caregiver of a child who takes Lantus, know the symptoms of hypoglycemia. (See the section just above for details.) This will help you notice when your child needs to consume foods or drinks to quickly raise their blood sugar. By aiding your child right away, you can help prevent a medical emergency.
Other drugs are available that can treat your condition. Some may be better suited for you than others. If you’re interested in finding an alternative to Lantus, talk with your doctor. They can tell you about other medications that may work well for you.
There are several different types of drugs that can be used to improve blood sugar levels for people with diabetes. Your doctor will prescribe the best medication for you based on several factors, including:
- the type of diabetes you have (type 1 or type 2)
- your history of blood sugar control
- your other health conditions
- your other medications
People with type 1 diabetes need insulin treatment because their bodies don’t make insulin on their own. People with type 2 diabetes may need insulin treatment if other diabetes drugs aren’t working or if their bodies stop making insulin.
There are also several non-insulin treatment options that may help improve blood sugar levels in people with type 1 or type 2 diabetes.
Note: Some of the drugs listed here are used off-label to treat these specific conditions.
Alternatives for improving blood sugar levels in type 1 or type 2 diabetes
Examples of other insulins that may be used to improve blood sugar levels in people with type 1 or type 2 diabetes include:
- long-acting insulins, which help improve blood sugar levels for about 24 hours:
- insulin glargine (Basaglar, Toujeo)
- insulin degludec (Tresiba)
- insulin detemir (Levemir)
- intermediate-acting insulins, which lower blood sugar levels for about 12 to 18 hours:
- insulin NPH (Humulin N, Novolin N)
- short-acting insulins, which lower blood sugar levels for about 3 to 6 hours:
- insulin regular (human) (Humulin R, Novolin R)
- rapid-acting insulins, which lower blood sugar levels for about 2 to 4 hours:
Several premixed insulin products are also available. They contain long-acting insulins and shorter-acting insulins. These combination medications help control baseline blood sugar levels and any blood sugar spikes that can occur around mealtime.
Examples of non-insulin diabetes medications that can be used to improve blood sugar levels in people with type 1 or type 2 diabetes include:
- pramlintide (Symlin)
- liraglutide (Saxenda, Victoza)
- exenatide (Bydureon, Byetta)
- canagliflozin (Invokana)
- dapagliflozin (Farxiga)
Alternatives for improving blood sugar levels in type 2 diabetes
There are also combination medications that contain insulin. They can be used to improve blood sugar levels in people with type 2 diabetes, including:
- insulin glargine and lixisenatide (Soliqua)
- insulin degludec and liraglutide (Xultophy 100/3.6)
You may wonder how Lantus compares with Toujeo. These medications contain the same active drug, insulin glargine. However, Toujeo is more concentrated than Lantus. You can see this article for a detailed comparison of Lantus and Toujeo.
You may wonder how Lantus compares to other medications that are prescribed for similar uses. Here we look at how Lantus and Levemir are alike and different.
Uses
The Food and Drug Administration (FDA) has approved both Lantus and Levemir to improve blood sugar levels in children and adults with type 1 diabetes. Lantus is approved for children ages 6 years and older with type 1 diabetes. Levemir is approved for children ages 2 years and older with type 1 diabetes.
Lantus is approved to treat adults with type 2 diabetes. Levemir is approved to treat both children and adults with type 2 diabetes.
Lantus and Levemir are both long-acting insulins. This means that they work the same way in the body. They both help control blood sugar levels for up to 24 hours or longer.
Lantus contains the drug insulin glargine. Levemir contains the drug insulin detemir.
Drug forms and administration
Lantus and Levemir both come as liquid solutions.
The two drugs come in two different forms:
- as a 10-milliliter (mL) vial that contains 100 units of insulin per mL (needles aren’t included with the vials and must be bought separately)
- as a disposable, prefilled pen
The Lantus pen is called Lantus SoloStar. It contains 3 mL of solution with 100 units of insulin per mL.
The Levemir pen is called Levemir FlexTouch. It also contains 3 mL of solution with 100 units of insulin per mL.
Lantus and Levemir are both given as an injection just under your skin (a subcutaneous injection).
Lantus is typically given once a day. Levemir is given once or twice a day.
Side effects and risks
Lantus and Levemir both contain long-acting insulins. Therefore, both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
This list contains examples of more common side effects that can occur with both Lantus and Levemir (when taken individually):
- hypoglycemia (low blood sugar levels)
- injection site reactions (redness or discoloration, itchiness, pain, tenderness around the injection area)
- upper respiratory infections, such as the common cold
- lipodystrophy (changes in skin thickness near the injection site)
- rash
- itchy skin
- edema (swelling), typically in your legs, ankles, or feet
- weight gain
Serious side effects
This list contains examples of serious side effects that can occur with both Lantus and Levemir (when taken individually):
- severe hypoglycemia (very low blood sugar levels)
- hypokalemia (low potassium levels)
- allergic reaction
Effectiveness
Lantus and Levemir have different FDA-approved uses. But they’re both used to treat adults and children with type 1 diabetes and adults with type 2 diabetes.
A review of studies found that Lantus and Levemir were equally effective at improving blood sugar levels in adults with type 1 diabetes. There was also no difference in the risk of low blood sugar episodes between the two drugs.
The review of studies also looked at people with type 2 diabetes. The analysis found no difference between Lantus and Levemir in improving blood sugar levels or in the rates of low blood sugar episodes.
Costs
Lantus and Levemir are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
The price you’ll pay for either drug will depend on your dose, your insurance plan, your location, and the pharmacy you use.
Note: In addition to the information above, you can also refer to this article for a detailed comparison of Levemir and Lantus.
You may wonder how Lantus compares to other medications that are prescribed for similar uses. Here we look at how Lantus and Basaglar are alike and different.
Uses
The Food and Drug Administration (FDA) has approved both Lantus and Basaglar to improve blood sugar levels in children (ages 6 and older) and adults with type 1 diabetes.
Both drugs are also approved to improve blood sugar levels in adults with type 2 diabetes.
Lantus and Basaglar both contain insulin glargine.
Basaglar is called an insulin follow-on drug to Lantus. This means that Basaglar is a biologic product (made from parts of living organisms) that is highly similar to Lantus. The FDA considers follow-on drugs to be just as effective and safe as the original brand-name version of the drug.
Drug forms and administration
Lantus and Basaglar both come as a liquid solution in a disposable, prefilled pen.
The Lantus pen is called Lantus SoloStar. The Basaglar pen is called Basaglar KwikPen.
The Lantus SoloStar and Basaglar KwikPen pens each contain 3 milliliters (mL) of solution with 100 units of insulin per mL.
Lantus solution also comes in a 10-mL vial that contains 100 units of insulin per mL.
Lantus and Basaglar are both given as an injection just under your skin (a subcutaneous injection). The drugs are typically given once a day.
Side effects and risks
Lantus and Basaglar both contain insulin glargine. Therefore, both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
This list contains examples of more common side effects that can occur with both Lantus and Basaglar (when taken individually):
- hypoglycemia (low blood sugar levels)
- injection site reactions (redness or discoloration, itchiness, pain, or tenderness around the area of injection)
- lipodystrophy (changes in skin thickness near the area of injection)
- itchy skin
- rash
- edema (swelling), typically in your legs, ankles, or feet
- weight gain
- upper respiratory infections, such as the common cold
- infections other than the common cold, such as urinary tract infections
Serious side effects
This list contains examples of serious side effects that can occur with both Lantus and Basaglar (when taken individually):
- allergic reaction
- hypokalemia (low potassium levels)
- severe hypoglycemia (very low blood sugar levels)
Effectiveness
Lantus and Basaglar are both FDA-approved to lower blood sugar levels in adults and children with type 1 diabetes. They are also both approved to lower blood sugar levels in adults with type 2 diabetes.
The use of Lantus and Basaglar for type 1 diabetes and type 2 diabetes has been directly compared. In a 1-year study, Lantus and Basaglar were found to be equally effective at improving blood sugar levels in people with type 1 diabetes. The people had similar rates of hypoglycemia (low blood sugar), allergic reactions, and changes in weight. In this study, both drugs were used in combination with mealtime insulin.
In another clinical study, Lantus and Basaglar helped control blood sugar levels about equally well in people with type 2 diabetes. The drugs were used in combination with oral (taken by mouth) medications for six months.
Costs
Lantus and Basaglar are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
The price you’ll pay for either drug will depend on your dose, your insurance plan, your location, and the pharmacy you use.
Note: In addition to the information above, you can also refer to this article for a detailed comparison of Basaglar and Lantus.
You may wonder how Lantus compares to other medications that are prescribed for similar uses. Here we look at how Lantus and Tresiba are alike and different.
Uses
The Food and Drug Administration (FDA) has approved both Lantus and Tresiba to improve blood sugar levels in people with diabetes.
Lantus is approved for people ages 6 years and older with type 1 diabetes and for adults with type 2 diabetes.
Tresiba is approved for people ages 1 year and older with type 1 or type 2 diabetes.
Drug forms and administration
Lantus and Tresiba both come as a liquid solution.
Lantus contains the drug insulin glargine. It comes in two forms:
- a 10-milliliter (mL) vial that contains 100 units of insulin per mL
- a 3-mL prefilled SoloStar pen that contains 100 units of insulin per mL
Tresiba contains the drug insulin degludec. It comes in:
- a 10-mL vial that contains 100 units of insulin per mL
- a 3-mL prefilled FlexTouch pen that contains 100 units of insulin per mL
- a 3-mL prefilled FlexTouch pen that contains 200 units of insulin per mL
Both Lantus and Tresiba are given as an injection just under your skin (a subcutaneous injection). They’re typically given once a day.
Side effects and risks
Lantus and Tresiba both contain long-acting insulins. Therefore, both medications can cause very similar side effects. Below are examples of these side effects.
More common side effects
This list contains examples of more common side effects that can occur with both Lantus and Tresiba (when taken individually):
- injection site reactions (redness or discoloration, itchiness, pain, tenderness around area of injection)
- upper respiratory infections, such as the common cold
- lipodystrophy (change in skin thickness near injection site)
- itchy skin
- rash
- edema (swelling), typically in your legs, ankles, or feet
- weight gain
- hypoglycemia (low blood sugar levels)
Serious side effects
This list contains examples of serious side effects that can occur with both Lantus and Tresiba (when taken individually):
- allergic reaction
- severe hypoglycemia (very low blood sugar levels)
- hypokalemia (low potassium levels)
Effectiveness
Lantus and Tresiba are both FDA-approved to improve blood sugar levels in people with type 1 and type 2 diabetes.
The use of Lantus and Tresiba in treating type 1 diabetes has been directly compared in several clinical studies. In a pooled analysis of these studies, Lantus and Tresiba were found to be equally effective at improving blood sugar levels in adults with type 1 diabetes. However, the analysis found that people who took Tresiba were 32% less likely to have low blood sugar levels at night.
Another clinical study found no difference in blood sugar level improvements between Lantus and Tresiba in children with type 1 diabetes.
The use of Lantus and Tresiba in treating type 2 diabetes has also been directly compared. A pooled analysis of nine studies found that Lantus and Tresiba improved blood sugar levels to a similar degree in adults with type 2 diabetes. However, there was a lower risk of severe low blood sugar and low blood sugar at night with Tresiba.
Costs
Lantus and Tresiba are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
The price you’ll pay for either drug will depend on your dose, your insurance plan, your location, and the pharmacy you use.
The Lantus dosage your doctor prescribes will depend on several factors. These include:
- the severity of the condition you’re using Lantus to treat
- your weight
- your history of blood sugar control
- your blood sugar level goals
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs. (In addition to the information below, you can also refer to this detailed article about the dosage of Lantus.)
Note: Making any changes to your insulin treatment plan could increase your risk for both hypoglycemia (low blood sugar levels) and hyperglycemia (high blood sugar levels). These changes include using a new insulin product, taking a new dosage of insulin, or administering the drug differently than you usually do.
If you’re making any changes to your insulin treatment plan, talk with your doctor about your risk for hypoglycemia and hyperglycemia.
Drug forms and strengths
Lantus comes as a liquid solution inside vials and disposable, prefilled pens.
Each vial of Lantus contains 10 milliliters (mL) of solution. Each mL contains 100 units of insulin glargine. So, there’s a total of 1,000 units of insulin glargine in each vial. This strength is also called Lantus U-100.
The disposable, prefilled pen of Lantus is called SoloStar. Each pen contains 3 mL of solution. There are 100 units of insulin glargine in each mL. That adds up to a total of 300 units of insulin per Lantus SoloStar pen.
Lantus SoloStar pens come in a package of five.
Needles aren’t included in the packages of either form of Lantus. (And keep in mind that each form of Lantus takes a different needle type.)
The Lantus vial and Lantus SoloStar pen are both meant to be used more than once. (This is known as being multi-dose.) The number of times will be different for each person, depending on your dosage. You can use the vials and pens for up to 28 days after you open them. After that time, you should dispose of the vial or pen, even if it still contains some of the drug.
But you should use each needle only once.
Dosage for type 1 diabetes
If you have type 1 diabetes, the starting dose of Lantus is generally about one-third of your total daily insulin dose.
Your total daily insulin dose is based on your weight. It typically ranges from 0.4 to 1.0 units per kilogram (kg) a day. (There are about 2.2 pounds [lb] per kg.)
For example, a 150-lb man weighs about 68 kg. If his doctor prescribes 0.5 units/kg a day, his total daily insulin dose would be 34 units a day. His starting dose of Lantus would be about one-third of 34 units, which is about 11 units of Lantus.
Lantus is typically taken once a day, not twice a day.
The drug is given as an injection just under your skin (a subcutaneous injection). You can inject Lantus in the skin of your upper arms, belly (at least 2 inches away from your belly button), or thighs.
Dosage for type 2 diabetes
The usual starting dose of Lantus for people with type 2 diabetes is 0.2 units/kg. (There are about 2.2 lb/kg.)
The maximum starting dose of Lantus is 10 units a day.
Lantus is typically taken once a day, not twice a day.
The drug is given as an injection just under your skin (a subcutaneous injection). You can inject Lantus in the skin of your upper arms, belly (at least 2 inches away from your belly button), or thighs.
Pediatric dosage
The usual starting dose of Lantus for children with type 1 diabetes is calculated in the same way as for adults.
The dosage of Lantus for these children is about one-third of their total daily insulin dose. The total daily dose is based on the child’s weight. It ranges from 0.4 to 1.0 units/kg a day. (There are about 2.2 lb/kg.)
For example, a 60-lb child weighs about 27 kg. If her doctor prescribes 0.5 units/kg a day, her total daily insulin dose would be about 14 units a day. The child’s starting dose of Lantus would be about one-third of 14 units, which is about 5 units.
Lantus is typically taken once a day, not twice a day.
The drug is given as an injection just under your skin (a subcutaneous injection). You can inject Lantus in the skin of your upper arms, belly (at least 2 inches away from your belly button), or thighs.
What if I miss a dose?
If you miss a dose, take it as soon as you remember. If it’s almost time for your next dose, skip the missed dose and go back to your normal schedule.
Don’t take more than one dose in 24 hours unless your doctor tells you to. This could increase your risk for serious side effects, such as hypoglycemia (low blood sugar levels).
Medication reminders can help make sure that you don’t miss a dose.
Will I need to use this drug long term?
You might. Lantus is typically used for long-term treatment of diabetes. If your doctor decides that Lantus is effective and safe for you, you’ll probably use it long term.
As with all medications, the cost of Lantus can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Financial and insurance assistance
If you need financial support to pay for Lantus, help is available.
Sanofi-Aventis US LLC, the manufacturer of Lantus, offers a copay savings card and a program called Valyou Savings Program. For more information on these options, and to find out if you’re eligible for one of them, visit the manufacturer’s website.
If you have Medicare Part D, you can check to see if your insurance plan covers Lantus at the manufacturer’s website.
Lantus can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Lantus and other medications
Below are lists of medications that can interact with Lantus. These lists don’t contain all the drugs that may interact with Lantus.
Before taking Lantus, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Lantus and diabetes medications
Lantus can interact in different ways with different diabetes medications.
Lantus and certain diabetes medications
Taking Lantus with other diabetes medications can increase your risk for hypoglycemia (low blood sugar level). If you take Lantus with other diabetes drugs, your doctor may need to adjust your dosage of one or all of them to reduce your risk for low blood sugar. They may also want you to monitor your blood sugar levels more often.
Examples of other diabetes medications that can increase your risk for low blood sugar if taken with Lantus include:
- mealtime insulins, such as insulin aspart (NovoLog, Fiasp) and insulin lispro (Admelog, Humalog)
- metformin (Glumetza, Glucophage)
- pramlintide (Symlin)
Lantus and diabetes drugs called thiazolidinediones
Taking Lantus with thiazolidinediones can cause heart failure, or worsen heart failure if you already have it. If you take a thiazolidinedione, be sure to discuss it with your doctor before you start treatment with Lantus. If you take one of these drugs with Lantus, your doctor will likely monitor you for signs of heart failure.
Examples of thiazolidinediones include:
Lantus and certain blood pressure medications
Taking Lantus with certain blood pressure medications can increase your risk for hypoglycemia (low blood sugar level). If you take Lantus with one of these drugs, your doctor may need to adjust the dosage of either Lantus or the blood pressure medication. They may also want you to monitor your blood sugar levels more often.
Examples of blood pressure medications that can increase your risk for low blood sugar if taken with Lantus include:
- lisinopril (Prinivil, Zestril)
- benazepril (Lotensin)
- captopril
- enalapril (Vasotec)
- candesartan (Atacand)
- losartan (Cozaar)
- valsartan (Diovan)
Taking Lantus with other types of blood pressure medications can hide the symptoms of low blood sugar when they occur. This can put you at risk for severe hypoglycemia (very low blood sugar level) with little warning. If you take Lantus with any of these drugs, your doctor may want you to check your blood sugar levels more often.
Examples of these medications include:
- atenolol (Tenormin)
- metoprolol (Lopressor, Toprol XL)
- nadolol (Corgard)
- propranolol (Inderal, Innopran XL)
- clonidine (Catapres, Kapvay)
- reserpine
Lantus and certain antipsychotic medications
Taking Lantus with certain antipsychotics can decrease how well Lantus works. This can lead to high blood sugar levels and an increased risk of complications from diabetes. If you’re taking Lantus with one of these medications, your doctor may increase your dose of Lantus. They may also recommend that you check your blood sugar levels more often.
Examples of antipsychotics that can decrease how well Lantus works include:
- olanzapine (Zyprexa)
- clozapine (Clozaril)
- quetiapine (Seroquel)
- risperidone (Risperdal)
Lantus and corticosteroids
Taking Lantus with corticosteroids can decrease how well Lantus works. This could increase your blood sugar levels, leading to a higher risk of serious complications, such as heart disease. If you’re taking Lantus with a corticosteroid, your doctor may increase your dose of Lantus. They will also advise you to check your blood sugar levels more often.
Examples of corticosteroids that can decrease how well Lantus works include:
- hydrocortisone (Cortef, many others)
- prednisone (Rayos)
- prednisolone (Orapred, Prelone)
- methylprednisolone (Medrol)
Lantus and alcohol
There’s no known interaction between Lantus and alcohol. However, drinking too much alcohol while taking Lantus can increase your risk for hypoglycemia (low blood sugar levels). This is because both alcohol and Lantus can lower blood sugar levels on their own.
If you drink alcohol, ask your doctor about how much is safe for you to drink.
Lantus is classified as a long-acting insulin. It lowers blood sugar levels in people with type 1 or type 2 diabetes. Lantus is made to work like natural insulin in your body. Insulin is a hormone that does the following:
- helps bring sugar from your blood into your cells, and the cells then use the sugar for energy
- helps your muscles use sugar for energy
- stops your liver from making more sugar
- helps your body create proteins and store sugar as fat
This is how your body keeps your blood sugar at a safe level.
In type 1 diabetes, your pancreas doesn’t make insulin. So you take medication, such as Lantus, to replace the insulin.
In type 2 diabetes, your body’s cells don’t respond to insulin the way they should. Your pancreas may also stop making insulin, which would need to be replaced with medication. You may also need insulin if other drugs can’t control your blood sugar levels.
Lantus replaces naturally occurring insulin for people with type 1 or type 2 diabetes.
How long does it take to work?
Lantus starts lowering blood sugar levels within a few hours. It’s a long-acting insulin that’s meant to help control blood sugar levels over 24 hours or longer. Long-acting insulins take longer than short-acting insulins to start working. But they last longer in your body.
After you inject Lantus, the drug forms clusters beneath your skin. As these clusters break down, insulin is slowly released into your bloodstream throughout the 24-hour period. But each person’s body will respond differently to Lantus.
Lantus doesn’t work right away like rapid-acting mealtime insulins do. So, Lantus should not be used in emergency situations.
You should take Lantus according to your doctor or healthcare professional’s instructions.
Lantus comes as a liquid solution inside:
- vials
- prefilled SoloStar pens
The solution in the vial is injected using a syringe and needle. Needles aren’t included in the package.
The SoloStar pen also uses special needles, which aren’t included in the package. The manufacturer of Lantus recommends using BD Ultra-Fine needles.
Your doctor will discuss whether the vial or SoloStar pen is right for you. Whether you use a syringe or the SoloStar pen, never reuse a needle or share a needle with another person. This helps prevent the spread of germs.
Below is information on how to use the vial and syringe, and SoloStar pen. You can also visit the manufacturer’s site for helpful images, a video, and more.
Lantus injection sites
Lantus is given as an injection just under your skin (a subcutaneous injection), once a day. When you first get your Lantus prescription, your healthcare professional will explain how to inject the medication yourself.
How to inject Lantus using a syringe and vial
If you’re going to inject Lantus using a syringe and vial, follow these steps.
Gathering supplies and preparing the vial
Before you inject Lantus, first collect your supplies and get the vial ready.
- Gather what you’ll need for your injection: alcohol swabs, Lantus vial, insulin syringe, sharps container.
- Wash your hands with soap and water. Then dry them.
- Check your insulin vial to make sure the solution is clear and colorless. If it’s cloudy or if there are particles in it, don’t use it. Throw the vial away.
- Remove the protective cap from the vial. This is if you’re using a new vial.
- Wipe the top of the vial with an alcohol swab to sterilize (clean) it.
Preparing your dose
Once you have your supplies and cleaned the vial, you’re ready to fill the syringe.
- Pick up the syringe and take off its protective cap.
- Pull the syringe’s plunger to draw air into the syringe. Keep pulling until you reach the measuring line that’s equal to your dose.
- Push the needle of the syringe through the rubber top on the vial.
- Press the syringe’s plunger completely down to push all of the air into the vial.
- Keeping the syringe in the vial, turn the vial and syringe upside down. The vial will be above the syringe.
- Hold the syringe and vial in one hand. Make sure the tip of the needle is in the insulin solution.
- With your other hand, pull down on the plunger until it reaches the measuring line that’s equal to your dose.
- With the needle still in the vial, check to make sure there are no air bubbles in the syringe.
- If there are bubbles in the syringe, hold the syringe straight up and gently tap on the side of the syringe. This should make the bubbles float up to the top.
- When the bubbles are at the top of the syringe, press the plunger to push the bubbles out of the syringe.
- Pull back on the syringe plunger again to draw your correct dose.
- Once your correct dose is inside the syringe with no bubbles, remove the needle from the vial. Don’t let the needle touch anything.
Choosing your injection spot
Now you’re ready to prepare the part of your body where you’ll give yourself the injection.
- Choose the area where you’re going to inject Lantus. Your injection can be in the skin of your upper arms, belly (at least 2 inches away from your belly button), or thighs.
- Look for a healthy spot of skin. Don’t choose an area that’s red or bruised, or where you have a cut or wound.
- Choose a different injection site each time. This helps prevent the site from getting red, sore, or swollen.
- Clean the injection site with a new alcohol swab. Let the alcohol dry before you inject.
Injecting Lantus using a syringe
It’s time to give yourself the Lantus injection.
- Pinch a 1- to 2-inch fold of skin and fat between your first finger and thumb of one hand.
- With your other hand, slowly push the needle into your skin at a 90-degree angle. Make sure the needle is completely in your skin.
- Once the needle is fully inserted, let go of the pinch of skin.
- Push the plunger into the syringe with your thumb at a steady pace.
- Leave the needle in your skin for 10 seconds. This helps make sure all the insulin has been injected.
- Pull the needle straight out of your skin.
- Press on the injection site gently for a few seconds.
- Put the needle in your sharps container.
How to inject Lantus using a SoloStar pen
If your doctor wants you to use a Lantus SoloStar pen, follow these steps.
Preparing the pen
Here’s how to get your Lantus SoloStar pen ready for use.
- If the pen hasn’t been opened yet, it should be in the refrigerator. Take it out and let it come to room temperature naturally. This may take 1 to 2 hours. Don’t try to warm the pen up in the microwave or by running it under hot water. This can make Lantus less safe, and it may not work as well. (Once you use a pen, don’t put it back in the refrigerator. Instead, store it at room temperature.)
- Gather what you’ll need for your injection: SoloStar pen, new needle, alcohol swabs, sharps container.
- Wash your hands with soap and water. Then dry them.
- Remove the cap from the SoloStar pen.
- Check the solution through the viewing window on the pen. Make sure the solution is clear. If the solution looks cloudy, is colored, or has particles in it, throw the pen away.
- Take an alcohol swab and wipe the rubber seal on the pen tip.
Attaching a needle to the pen
Once the pen is at room temperature and you’ve prepared it, you’re ready to attach the needle.
- Remove the protective seal from a new needle.
- Screw the new needle onto the pen tip. Don’t screw the needle on too tightly. If your needle is a “push-on” needle, push it onto the pen in a straight line.
- Once the needle is attached, take the outer cap off the needle. Set it aside because you’ll need it later.
- Take the inner needle cap off and throw it in the trash.
Testing the pen
Before you use the SoloStar pen, test it to make sure it’s working properly. Don’t worry about wasting the drug. It’s important to test the pen to help ensure that it delivers the right amount of medication for your dose.
- Turn the dose counter on the pen to 2 units.
- Hold the pen straight with the needle pointing up.
- Tap the insulin viewing window to make all air bubbles rise to the top of the pen.
- Once all the bubbles are at the top, press the pen’s injection button all the way in.
- Watch to see if insulin comes out of the needle. The counter should go back to 0 (zero) after you release the injection button.
- If no insulin came out during the test, repeat the test two more times.
- If there still isn’t any insulin coming out of the pen, change the needle and repeat the test. Don’t use the pen if no insulin comes out after trying the test with the second needle.
Setting the dose
Now that you know your pen is working correctly, set the dose your doctor recommended.
- Once you’ve tested your pen and seen that it’s working, make sure the dose window shows 0 (zero). If you don’t start at zero, you may inject too much insulin.
- Select your dose by turning the dial at the end of the pen. If you go too far, you can turn the dial up and down to get to the correct dose.
Choosing your injection area
Now you’re ready to prepare the part of your body where you’ll give yourself the injection.
- Choose the area where you’re going to inject Lantus. Your injection can be in the skin of your upper arms, thighs, or belly (at least 2 inches away from your belly button).
- Don’t choose an area that is red, bruised, or where you have a cut or wound.
- Choose a different injection site each time. This helps prevent the site from getting red, sore, or swollen.
- Clean the injection site with a new alcohol swab. Let the alcohol dry before you inject.
Injecting Lantus using the Lantus SoloStar pen
It’s time to give yourself an injection with the Lantus SoloStar pen.
- Push the pen straight into the injection site.
- Use your thumb to press the injection button all the way in.
- Watch the dose counter to make sure it returns to 0 (zero) as you inject.
- Count to 10 slowly while holding down the injection button.
- Release the button and pull the needle out of your skin.
Removing the needle
Now that you’ve given yourself the injection, you need to remove the needle from the pen.
- Place the outer needle cap back onto the pen. It should cover the needle.
- Pull or unscrew the needle from the pen.
- Put the needle in your sharps container.
- Place the SoloStar pen cap back on the pen.
- Store the open pen at room temperature for up to 28 days.
When to take
You can take Lantus at any time, but it should be at the same time each day. Ask your doctor what time is best for you. They’ll base the timing on how your blood sugar levels change throughout the day and night. Many people take their Lantus dose at bedtime.
Talk with your doctor, and they’ll help you determine the best time of day to take Lantus.
Medication reminders can help make sure that you don’t miss a dose.
Taking Lantus with food
You don’t need to eat food when you inject Lantus.
Taking too much Lantus can increase your risk for serious side effects.
Overdose symptoms
Symptoms of an overdose can include:
- severe hypoglycemia (very low blood sugar levels), which can cause:
- shakiness
- anxiety
- confusion
- seizures
- coma
- in severe cases, death
- hypokalemia (low potassium levels), which can cause:
- muscle cramps
- weakness
- constipation
- heart palpitations (feeling of skipped or extra heartbeats)
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use its online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
There aren’t enough studies of Lantus use during human pregnancy to know exactly how safe it is.
However, according to the American Diabetes Association, insulin therapy (such as Lantus) is the first-choice option for diabetes treatment during pregnancy. It’s recommended for people who had diabetes before they were pregnant. Insulin therapy is also recommended for people who develop diabetes while pregnant (called gestational diabetes).
If you need treatment to help control your blood sugar levels during pregnancy, talk with your doctor. They’ll recommend the right type of insulin for you.
If you’re already taking insulin, such as Lantus, when you become pregnant, your doctor may recommend dosage changes. This can help keep your blood sugar levels in a safe range for you and your baby.
Lantus is generally considered safe to take while you’re breastfeeding.
However, you may need a different dose of Lantus for a time after you give birth. This is due to changes in your body and changes in your sleep and mealtime schedules.
If you’re considering breastfeeding while taking Lantus, talk with your doctor about the best dosage for you.
Here are answers to some frequently asked questions about Lantus.
Will I still use my mealtime insulin or other insulins with Lantus?
You might. Lantus is a long-acting insulin that’s meant to work over the course of an entire day. Long-acting insulin is typically called basal or “background” insulin because it helps control blood sugar levels between meals and overnight while you sleep.
However, Lantus isn’t typically used to control blood sugar spikes after meals. You may need a rapid-acting insulin, short-acting insulin, or intermediate-acting insulin to fine-tune your blood sugar level control. Many people who use a long-acting insulin such as Lantus will also need rapid-acting or short-acting insulin to control blood sugar levels after meals.
If you do take more than one type of insulin, don’t mix Lantus in the same syringe with any other insulins. This could change how well the insulins work.
If you have any questions about when or how to take each type of insulin, talk with your doctor or pharmacist.
Is it better to take Lantus in the morning or at night?
The best time to take Lantus depends on how your blood sugar levels change throughout the day.
In clinical studies, blood sugar levels were reduced to a similar degree whether people took Lantus in the morning or evening.
Your doctor will monitor how your blood sugar levels change throughout the day. Then they’ll recommend the best time for you to take Lantus.
Will Lantus cause hypoglycemia?
It can. Hypoglycemia (low blood sugar levels) is one of the most common side effects of insulin products, including Lantus.
Some factors that can increase your risk for hypoglycemia are:
- changes in diet, such as not eating enough food
- changes in the timing of meals or skipping meals
- sickness or stress
- sudden increases in exercise or physical activity
- new or different doses of insulin or other medications you take
- accidentally taking more Lantus than you’re prescribed
Also, making any changes to your insulin treatment plan could increase your risk for both hypoglycemia and hyperglycemia (high blood sugar levels). These changes include using a new insulin product, taking a new dosage of insulin, or administering the drug differently than you usually do.
It’s important to know the symptoms of low blood sugar, so you can treat it before it becomes serious. Severe hypoglycemia (very low blood sugar level) can be life-threatening if not treated right away.
Some symptoms of low blood sugar include:
- anxiety
- sweating
- confusion
- headache
- hunger
- dizziness
- nausea
Talk with your doctor or pharmacist about creating a plan to prevent and manage low blood sugar levels.
Does Lantus treat diabetic ketoacidosis?
No. Lantus isn’t used to treat diabetic ketoacidosis (DKA).
DKA is a serious complication of diabetes. It occurs when your blood sugar levels are very high but your insulin levels are low. Because insulin isn’t available to move sugar into your cells, they can’t use the sugar as fuel. Instead, your body starts breaking down fat into ketones (a certain type of protein) for energy. High levels of ketones make your blood more acidic, which can harm many organs in your body.
DKA treatment takes place in a hospital setting. Treatment involves using insulin to bring sugar into your cells. However, Lantus isn’t the best type of insulin for this process because it takes too long to start working. Faster-acting insulins such as insulin aspart (Fiasp, NovoLog), insulin glulisine (Apidra), or insulin lispro (Admelog, Humalog) are typically used as part of DKA treatment.
Before taking Lantus, talk with your doctor about your health history. Lantus may not be right for you if you have certain medical conditions. These include:
- Allergic reaction to Lantus. If you’ve had an allergic reaction to Lantus or any of the inactive ingredients in Lantus, you should not use the drug. If you’re unsure about whether you’ve had an allergic reaction to Lantus or any of its ingredients in the past, talk with your doctor before you take Lantus.
- Current episode of hypoglycemia. Do not take Lantus if you’re currently experiencing an episode of hypoglycemia (low blood sugar levels). Wait until you have managed the episode and your blood sugar levels have returned to normal before you take your dose of Lantus.
- Hypokalemia (low potassium levels). Lantus may lower potassium levels. So, if you already have low potassium, taking Lantus may lower your levels even more. If you have low potassium, or if you’re at risk for it, your doctor may monitor your levels during your Lantus treatment.
Note: For more information about the potential negative effects of Lantus, see the “Lantus side effects” section above.
When you get Lantus from the pharmacy, the pharmacist will add an expiration date to the label on the bottle. This date is typically one year from the date they dispensed the medication.
The expiration date helps guarantee the effectiveness of the medication during this time. The current stance of the Food and Drug Administration (FDA) is to avoid using expired medications. If you have unused medication that has gone past the expiration date, talk to your pharmacist about whether you might still be able to use it.
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Storing unopened vials
You should store unopened Lantus vials in your refrigerator until the expiration date listed on the package. You can also store them at room temperature for 28 days, but you’ll need to throw them away after 28 days.
Storing opened vials
Once you open a Lantus vial, you can store it at room temperature or in the refrigerator for 28 days.
Storing unopened pens
You should store unopened Lantus SoloStar pens in the refrigerator until the expiration date listed on the package. You can also store them for 28 days at room temperature, but you’ll need to throw them away after 28 days.
Storing opened pens
Once you open a Lantus SoloStar pen, you can store it for 28 days at room temperature. You should not store opened Lantus SoloStar pens in the refrigerator.
You should never freeze Lantus vials and SoloStar pens. Also, keep them out of direct heat and light.
Disposal
Once you’ve used a syringe or pen to inject Lantus, safely discard the needle right away in a sharps disposal container. You can get an FDA-approved sharps container at your pharmacy, through medical supply companies, or online. Find a local program that will take your sharps disposal container when it’s full.
If you no longer need to take Lantus and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
The FDA website provides several useful tips on medication disposal. You can also ask your pharmacist for information on how to dispose of your medication.
The following information is provided for clinicians and other healthcare professionals.
Indications
Lantus (insulin glargine) is indicated to improve blood glucose control in adults and children with type 1 diabetes and in adults with type 2 diabetes.
Note: Lantus isn’t approved to treat diabetic ketoacidosis.
Mechanism of action
Lantus is a long-acting analog of human insulin engineered to be less soluble at physiological pH, causing crystallization at the injection site, a delay in absorption, and prolongation of action.
Lantus exerts its hypoglycemic effects by increasing peripheral glucose uptake and inhibiting hepatic gluconeogenesis. It also prevents fat and protein degradation while stimulating protein synthesis.
Pharmacokinetics and metabolism
Following subcutaneous injection, absorption of Lantus is relatively constant over a 24-hour period. Due to the consistency of insulin glargine, it does not have a defined half-life or peak.
There is no peak concentration, as the release in the body remains constant. It has been shown to release its effect in the body for 24 hours in 50% of people who received Lantus in clinical trials.
Lantus is partly metabolized in the subcutaneous depot to two active metabolites, which have similar activity to human insulin. Median time to end of pharmacological effect is 24 hours.
Contraindications
Lantus is contraindicated for use during hypoglycemic episodes. It’s also contraindicated for people with a history of hypersensitivity to Lantus or any of the product’s excipients.
Storage
Unopened Lantus vials and SoloStar pens should be stored at room temperature (< 86°F or < 30°C) for 28 days or in the refrigerator until the expiration date.
Opened vials can be stored at room temperature or in the refrigerator for 28 days.
Opened pens should be stored at room temperature for 28 days. Opened pens should not be refrigerated.
Do not freeze vials or pens at any time. Protect them from direct heat and light.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.