Epidermal barrier dysfunction and cutaneous sensitization in atopic diseases (original) (raw)
Abstract
Classic atopic dermatitis is complicated by asthma, allergic rhinitis, and food allergies, cumulatively referred to as atopic diseases. Recent discoveries of mutations in the filaggrin gene as predisposing factors for atopic diseases have refocused investigators’ attention on epidermal barrier dysfunction as a causative mechanism. The skin’s barrier function has three elements: the stratum corneum (air-liquid barrier), tight junctions (liquid-liquid barrier), and the Langerhans cell network (immunological barrier). Clarification of the molecular events underpinning epidermal barrier function and dysfunction should lead to a better understanding of the pathophysiological mechanisms of atopic diseases.
Introduction
Atopic dermatitis (AD) is a chronic relapsing eczematous skin disorder that is frequently associated with elevated serum IgE levels and a family history of AD, allergic rhinitis, and/or asthma. Clinical manifestations of classic AD are dry skin and relapsing eczema, which usually start during early infancy or childhood and become complicated by food allergies, asthma, and/or allergic rhinitis during the first several years of life, in a process called “atopic march” (1). AD is highly prevalent in industrialized countries, where it affects approximately 15%–30% of children and 2%–10% of adults (2). The various observations of the disease indicate that AD has a complex etiology with genetic, immunological, and environmental aspects.
Living organisms rely critically on surface barriers to isolate themselves from the external environment and to maintain homeostasis. While unicellular organisms are enclosed by cell membranes and cell walls, epithelial barrier structures, in several forms, cover the surfaces of multicellular organisms (3). In mammals, the airway and gastrointestinal tract are lined by simple epithelia covered with mucus. In contrast, the outer surface of the body is covered by a stratified epithelial cellular sheet called the epidermis, the outermost layer of which is cornified. Recent findings have shown that disruption of epithelial barrier systems are involved in the pathogenesis of immune disorders such as inflammatory bowel disease, asthma, and AD (4–12). In this review, we describe the barrier system of the epidermis, which is far more sophisticated than previously thought (13, 14), and attempt to discuss its function with special focus on antigen penetration through these barriers and antigen capture by dendritic cells in the context of AD.
The three musketeers of the epidermal barrier
Tight junctions as a liquid-liquid interface barrier.
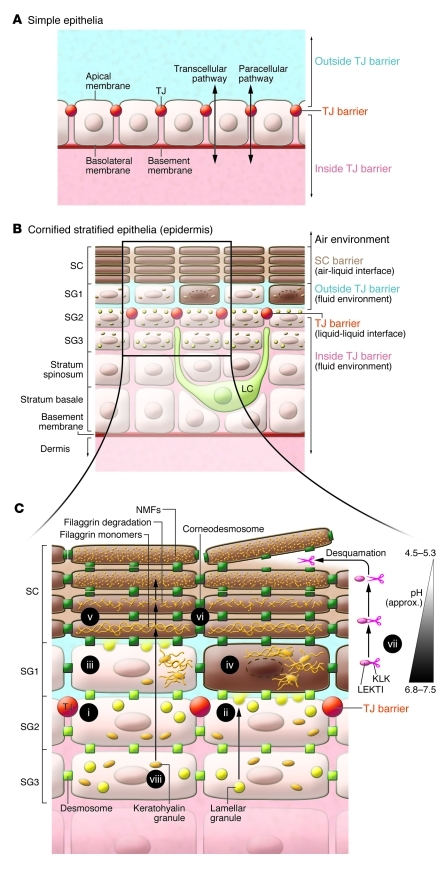
For cellular sheets to function as proper barriers, paracellular diffusion of fluid must be prevented. In simple, single-layer cellular sheets in vertebrates, tight junctions (TJs) are responsible for intercellular sealing and the compartmentalization of extracellular environments (ref. 3 and Figure 1A). TJs are not just physical barriers; they exhibit ion and size selectivity and their barrier function varies significantly in tightness, depending on cell type and physiological requirements, enabling dynamic regulation of substances that traffic between compartments. As a result, two adjacent compartments divided by TJ barriers can maintain different ionic strengths and solute concentrations (15–17).
Figure 1. Schematic representation of the barriers in simple epithelia and stratified epidermis.
(A) In simple epithelia, TJs seal the apical end of the lateral cell membrane. The extracellular fluid is compartmentalized into two parts by TJs. (B) In the mammalian epidermis, the SC serves as an air-liquid interface barrier and protects the living layers from desiccation. TJs also seal the paracellular spaces between SG2 cells. TJs act as a liquid-liquid interface barrier in both simple and cornified stratified epithelia. LCs position their dendrites upward, ready to survey antigens upon sensing perturbation. (C) Terminal differentiation in relation to TJs. When SG3 cells differentiate into SG2 cells, they form TJs (i) and begin to secrete lamellar granules from their apical membranes (ii). SG1 cells appear to lose their TJs (iii) and then undergo final cornification (iv). Mature corneocytes are encapsulated in the cornified envelope (dark brown; v), and their intercellular spaces are filled with lipid lamellae (brown). Corneodesmosomes (green squares; vi) mediate intercorneocyte adhesion. KLKs secreted into the extracellular space are strictly limited to the extra-TJ environment. As the pH becomes acidic in the upper layers of the SC, KLKs are released from LEKTI and proteolyze corneodesmosomes, initiating desquamation (vii). Profilaggrin is a component of keratohyalin granules in the SG, is degraded into filaggrin monomers, possibly in SG1 cells, and is further degraded into NMFs in the upper SC (viii).
Within the body of vertebrates, the TJ barrier acts as a liquid-liquid interface barrier to demarcate different fluid compartments. Examples of the compartmentalized fluids separated by TJ barriers are bile (in the lumen of bile ducts), urine (in the renal tubules), and cerebrospinal fluid (within the blood-brain barrier). TJs exist also in the body surface, both in the simple epithelia of body cavities such as intestine and trachea and in the stratified epithelia of skin. In the non-keratinized epidermis of fish and amphibian tadpoles, TJs separate the body from the external aquatic environment (18, 19). In terrestrial vertebrates, in which stratum corneum (SC) evolved presumably as an air-liquid interface barrier to avoid desiccation as animals adapted to living in contact with air, TJ barriers exist covertly under the SC barriers (18, 20–24). They compartmentalize the epidermal extracellular fluid environment into two parts in mammals (described below) and possibly also in reptiles and birds (Figure 1B).
Mammalian epidermis consists of a single layer of proliferating cells, the stratum basale, and several superficial layers of stratum spinosum and stratum granulosum (SG), which ultimately form the SC. As thin as it is, mouse ear epidermis has the minimal components of epidermal differentiation, with pre-SC cell flattening always occurring in three layers in the SG (25–27). The three SG layers are designated SG1, SG2, and SG3, counting from the surface inward. Our imaging studies of whole-mounted epidermal sheets have demonstrated that the intercellular spaces between SG2 cells are sealed by TJs (ref. 13 and Supplemental Video 1; supplemental material available online with this article; doi:10.1172/JCI57416DS1), as previously proposed based on careful observations via immunofluorescence and electron microscopy (22). Thus, SG1 cells that are about to cornify exist within a distinct fluid compartment outside of the TJ barrier, and cells below the SG2 layer are inside the barrier (Figure 1B).
The SC as an air-liquid interface barrier.
As spinous layer cells differentiate into SG cells, they become flattened, with diameters up to 30 micrometers (27), and start to form lamellar and keratohyalin granules (Figure 1C). When SG3 cells differentiate into SG2 cells, they form TJs and acquire an apical-basal polarization of the cell membrane (13, 22). From the apical membrane of SG2 cells, which correlate with the secretory granulocytes observed by electron microscopy (28), the contents of lamellar granules (e.g., lipids, extracellular structural proteins, hydrolytic enzymes, and various antibacterial peptides such as cathelicidin and β-defensin 2; refs. 29–31) begin to be secreted into, and are kept within, the extra-TJ compartment, where they form the intercellular structures of the SC (32). After SG2 cells differentiate into SG1 cells, they appear to lose their TJs and initiate the final cornification steps of terminal differentiation, which occur outside the TJ barrier within a distinct fluid compartment that is probably required for terminal differentiation. Based on the results of electron microscopic studies and immunofluorescence studies, the observed “transient cells” (33) are likely equivalent to SG1 cells (13, 22) undergoing cornification.
During cornification, SG1 cells are enucleated, lose intracellular organelles and cell membranes, and are encapsulated in a heavily cross-linked proteinous structure called the “cornified envelope” (34). Within the extra-TJ compartment, the adhesion complexes between SG1 cells, desmosomes, are modified to corneodesmosomes through the incorporation of corneodesmosin (29, 35). Paracellular spaces outside of the TJ start to be filled with a mixture of relatively nonpolar lipids enriched in ceramides, cholesterol, free fatty acids, and cholesterol esters, which are secreted from the apical ends of SG2 cells. These lipids form intercellular lipid lamellae, or the “mortar” of the SC. SG1 cells transform into the lowermost corneocytes, which are the “bricks” surrounded by the mortar. Multiple layers of this structure form the SC, outermost bricks of which are desquamated in a well-controlled process (described below).
Langerhans cells as an immune barrier.
DCs are leukocyte subsets that specialize in antigen presentation and are distributed throughout the body to protect the body from microbial or antigenic insult. Several subsets of DCs reside in skin, and the Langerhans cells (LCs) are unique DCs of the epidermis, distinct from several subsets of dermal DCs (36, 37). Although LCs were long believed to be the initiators of immune responses in skin, several studies utilizing transgenic mice that allow selective targeting of DCs failed to demonstrate their critical contribution in hapten-induced contact hypersensitivity models (36, 37). However, more recent studies have demonstrated that LCs are indeed capable of inducing antigen-specific Th2 responses in vivo (38, 39).
Penetration of the TJ barrier by DC dendrites and subsequent uptake of extra-TJ antigens have been reported in the lamina propria of the intestine and bronchial epithelium and may also occur in nasal and adenoid epithelia (40–46). The epidermis, because of its stratification and two sets of barriers, is quite different from simple epithelia with regard to antigen penetration and the capture of antigens by DCs. Under steady-state conditions, LCs are on standby with their dendrites aimed outward, positioned close to, but never crossing, the TJ barrier (Figure 1B). SC barrier perturbation (e.g., tape-stripping or acetone treatment) has been known to stimulate cytokine production in the epidermis and/or to activate LCs (47–50). Once activated, LCs extend their dendrites through TJ barriers and take up antigens from the extra-TJ environment (Figure 2, Supplemental Video 2, and ref. 13). During this process, the tightness of the epidermal TJs is maintained by the de novo formation of TJs between keratinocytes and LCs, suggesting that LCs are able to take up foreign antigens from outside TJ barriers without penetrating these barriers (13). In contrast, dermal DCs presumably take up antigens that have penetrated both epidermal barriers. Ouchi et al. recently showed that antigen uptake through TJs by LCs leads to a protective Th2 (IgG1) humoral response in a mouse model of staphylococcal scalded skin syndrome (51). At present, it appears that LCs only induce a Th2 response in the presence of an intact TJ barrier. It would be of interest to explore the deviation of immune responses that is induced upon the disruption of TJ barriers, which might allow dermal DCs to have access to antigens, thus leading to immune responses not restricted to Th2. It will be important to assess such immune responses utilizing protein antigens that do not easily pass through TJs, instead of haptens that readily penetrate the epidermis, regardless of the barriers, to the dermis.
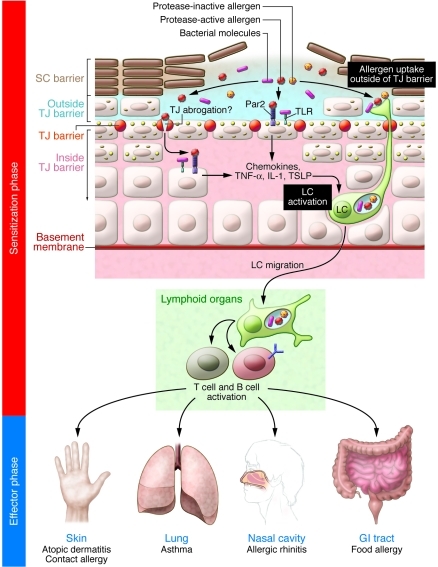
Figure 2. A model of barrier disruption and consequences of percutaneous sensitization.
SC barrier damages induce danger signals in the epidermis. After SC barrier abrogation, protease-active allergens and uncontrolled intrinsic proteases, as well as bacterial molecules such as lipoteichoic acid of gram-positive bacteria, might agonize Par2 and TLRs on keratinocytes, respectively (7, 55, 112, 123). Keratinocytes then produce TNF-α, IL-1, and thymic stromal lymphopoietin (TSLP) (47, 55), in response to which LCs become activated (54, 56, 124). Alternatively, protease-active allergens might directly obscure the TJ barrier and then penetrate the epidermis (7), where they directly or indirectly activate LCs. Upon SC perturbation, dendrites of activated LCs penetrate the TJs to take up protease-active or -inactive antigens from the extra-TJ environment (13). Such percutaneous sensitization and chronic allergen challenge via different routes, such as the lungs, nasal cavities, and intestinal tract, are speculated to manifest as the atopic march.
Dynamic cooperation and interaction of the three musketeers.
As described above, the SC, TJs, and LCs together constitute a skin surface surveillance and barrier system. The SC directly faces the external environment, protecting the inner viable layers from desiccation. The SC is not a sterile surface but controls skin flora of microorganisms via antimicrobial peptides and low pH (52). The SG1 layer exists outside of the TJ barrier and its extracellular space is rich in various proteases, antimicrobial peptides, and, under certain circumstances, bacteria and bacteria-derived metabolites/antigens. TJs in the SG2 layer compartmentalize this layer from the viable layer, preventing the potentially pro-inflammatory molecules above it from perturbing immune signals (see below). LCs, positioned covertly under the TJs, are polarized to send their dendrites outside of the TJ barrier when activated by danger signals such as TSLP, TNF-α, and IL-1β, presumably secreted from keratinocytes that somehow detect SC damages (Figure 2 and refs. 47, 53–56). The SG1 layer allows LCs to sample for foreign materials that have violated the SC barrier (13). Thus these three musketeers work all for one, and one for all, to provide a highly organized skin barrier.
Major players in SC barrier dysfunction
Filaggrin mutations as predisposing factors for atopic diseases.
Filaggrin is expressed in SG layers as a >400-kDa precursor protein, profilaggrin. Profilaggrin is the major component of the keratohyalin granules in SG cells. It is comprised of highly homologous tandem repeats of the filaggrin monomer (10–12 in humans and 16 in C57BL/6 mice), flanked by two imperfect repeats and N- and C-terminal domains. Profilaggrin is proteolyzed into filaggrin monomers and N- and C-terminal peptides at the boundary of the SC and SG, possibly in SG1 cells. The functions of the N- and C-terminal peptides are as yet unknown, but nuclear translocation of the former, which contains an S-100 Ca2+-binding domain, has been reported (57). Filaggrin monomers display keratin-binding activity in vitro and have been proposed to promote the compaction of corneocytes by contributing to keratin pattern formation in the lower SC (58). Filaggrin monomers are further degraded into natural moisturizing factors (NMFs) that are thought to maintain hydration of the upper SC and to reduce the pH of the skin surfaces (59–61).
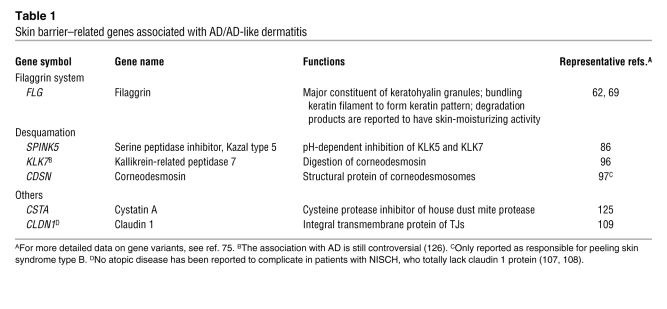
Mutations in the filaggrin (FLG) gene were identified initially as the cause of ichthyosis vulgaris and subsequently as a major predisposing factor for AD (Table 1 and refs. 62, 63). More recent studies have confirmed the association and identified additional mutations in the FLG gene that predispose to AD in European and Asian populations (64–67). FLG mutations have also been reported to be associated with atopic asthma, allergic rhinitis, nickel allergy, and food allergy (68–73), suggesting that FLG mutation–associated SC barrier defects lead to increased numbers of episodes of percutaneous allergen exposure (Figure 2). Interestingly, FLG mutations are not associated with asthma without eczema (70, 71), and most of the identified asthma-associated genes are not associated with AD (74, 75), suggesting that atopic asthma is a distinguishable sub-entity. Because filaggrin is not expressed in the upper airways (76), systemic sensitization is likely attributable to percutaneous antigen exposure through filaggrin-deficient skin. In good agreement with this hypothesis, percutaneous sensitization induces allergic responses to allergens in mice challenged via the upper airway (77, 78). Further investigation is required to clarify the impact of filaggrin deficiency on the barrier function of SC and the molecular mechanisms of percutaneous sensitization in the pathophysiology of AD and atopic diseases.
Table 1 .
Skin barrier–related genes associated with AD/AD-like dermatitis
Mouse models of filaggrin deficiency.
Flaky tail (ft) mice were created in 1958 on the background of an existing recessive hair phenotype, matted (ma), and also exhibited dry, flaky skin with annular tail and paw constrictions during the neonatal period (79). Since then, they have been maintained in a mixed strain (ft/ma) (80). The ft mutation was found to be a 1-bp deletion in filaggrin repeat 6, which leads to premature termination, analogous to common human FLG mutations (81). ft/ma mice show paracellular barrier permeability in SC (82), increased trans-epidermal water loss (TEWL), and enhanced percutaneous allergen priming (83). They also spontaneously develop dermatitis under steady-state conditions (83) and have been used as a model of filaggrin deficiency and AD. However, ma locus-eliminated homozygous ft mice (identified by the absence of matted hair) only show mild diffuse hypertrophy of the SC and sporadic superficial dermal cellular infiltrates under steady-state conditions (81). Furthermore, while ft/ma mice show elevated TEWL (83), ft mice show no statistically significant difference in baseline TEWL (81). Thus, when ft/ma mice are used in studies of AD in the context of filaggrin deficiency, the results need to be interpreted carefully. It would be of interest to identify the gene responsible for the ma phenotype, and the gene’s function, to understand the pathophysiological mechanisms behind the spontaneous development of dermatitis in ft/ma mice.
Hereditary SC barrier deficiency with complicating atopic disease.
Desquamation is a well-orchestrated process controlled by a network of proteases, which themselves are regulated by protease inhibitors and skin pH. Among these, kallikrein-related (KLK-related) peptidases and their pH-dependent inhibition by lymphoepithelial Kazal type–related inhibitor (LEKTI; encoded by serine peptidase inhibitor, Kazal type 5 [_SPINK5_] gene) are the best characterized (Figure 1B and refs. 84, 85). Under normal conditions, the neutral pH in the lower SC enables LEKTI to inactivate KLK5 and KLK7, while the acidic conditions in the uppermost part of the SC inhibit LEKTI, thereby allowing KLK5 and KLK7 to function and thus promoting skin peeling. Genetic studies have demonstrated linkage between polymorphisms in SPINK5 and AD, asthma, and elevated levels of serum IgE (86–88). Loss of function of SPINK5 causes Netherton syndrome, a severe autosomal recessive ichthyosis characterized by chronic dermatitis, asthma, and allergic rhinitis (89). Ultrastructural analyses show a marked increase in corneodesmosome cleavage and SC detachment at the border between transient cells and SG cells in the skin of patients with Netherton syndrome (90–92). Studies of _SPINK5_-knockout mice confirmed that LEKTI deficiency results in elevated KLK5 activity in the layers of the SC and subsequent breakdown of corneodesmosin, followed by SC barrier loss (93–95). Polymorphisms in SPINK5 and KLK7 associated with AD may produce a similar, but milder, SC barrier defect (Table 1 and refs. 86, 96). Genetic loss of corneodesmosin causes peeling skin syndrome type B, in which the whole SC is easily detached from the underlying living layers, leading to chronic dermatitis, asthma, allergic rhinitis, elevated levels of serum IgE, and food allergy (Table 1 and ref. 97), suggesting that SC barrier dysfunction precedes the onset of atopic diseases.
Loss of the SC barrier, as occurs in Netherton syndrome and peeling skin syndrome type B, induces dermatitis, asthma, and allergic rhinitis, suggesting that perturbation of the desquamation processes could induce SC barrier defects and predispose to AD or similar conditions. Overexpression of elastase 2 and over degradation of profilaggrin were recently reported in the skin of patients with Netherton syndrome (98), and it is necessary to evaluate whether the filaggrin system malfunction plays a direct role on the barrier dysfunction in these two diseases. Interestingly, under LEKTI-deficient conditions (as in Netherton syndrome), spontaneous protease-activated receptor 2 (Par2) activation and subsequent production of thymic stromal lymphopoietin, IL-8, and TNF-α in keratinocytes have been reported to result from uncontrolled activation of KLK5, indicating that aberrant activation of barrier-associated proteases can modulate immunity in ways that exacerbate atopic manifestations (55).
Search for additional candidate genes in atopic diseases.
As mentioned above, filaggrin mutations are, thus far, the major predisposing factor for classic atopy. However, such mutations are not found in a significant number of patients, indicating that other genetic factors that influence skin barrier function may also be important. Candidate molecules include enzymes that function in the degradation of profilaggrin (61). Retroviral-like aspartic protease (SASPase) is a skin-specific protease that directly cleaves a linker peptide in profilaggrin. Hairless mice deficient in SASPase exhibit dry skin and aberrantly processed profilaggrin accumulation in the lower SC (99). Caspase-14 is a skin-specific enzyme that may be involved in the early degradation of filaggrin monomers to NMFs, and caspase-14–knockout mice display a dry skin phenotype (100, 101). Bleomycin hydrolase has been reported to be involved in a later stage of the degradation processes (102, 103). Bleomycin hydrolase–knockout mice display generalized scaling and mild ichthyosis in their neonatal period, while adults appear normal but develop low-humidity-induced dermatitis in their tails (104). Further epidemiological studies are warranted to determine whether mutations in these proteases are predisposing factors for human AD.
TJ barriers may also be involved in proper SC formation. Claudin 1 is one of the major integral transmembrane components of epidermal TJs, and in claudin 1–knockout mice, epidermal TJs lose tightness and the SC displays compact hyperkeratosis, suggesting that loss of tightness of the TJ barrier may also affect terminal differentiation in the epidermis (22). Ectopic overexpression of periderm-specific claudin, claudin 6, in the SG induces a phenotype that is identical to claudin 1–knockout mice (105, 106), suggesting that differential expression or the balance of claudin molecules might regulate the tightness of TJ barriers. Patients with neonatal ichthyosis and sclerosing cholangitis (NISCH) have homozygous nonsense mutations in the claudin 1 gene and display ichthyosis, further suggesting the involvement of the TJ barrier in proper SC formation (107, 108). Interestingly, a polymorphism in the claudin 1 gene was recently reported as a possible candidate mutation in AD (Table 1 and ref. 109). Further large-scale epidemiological studies and careful investigation of the crosstalk between the TJ and SC barriers are necessary to assess the contribution of TJs to the pathogenesis of AD.
Percutaneous sensitization through insufficient SC barrier
LC activation induced by SC barrier perturbation.
In contrast to the above-described congenital diseases that affect the SC, the entire epidermis is lost in junctional or dystrophic epidermolysis bullosa (EB) (110). Interestingly, patients with EB do not usually develop atopic diseases, and genes responsible for EB, such as those that encode laminin 332, and the type VII and XVII collagens, were not identified in genome-wide linkage studies of AD or asthma. Thus, living layer structures of the epidermis and cellular immune components, such as LCs, may be required for the development of atopic diseases. In this context, it is important to understand how foreign antigens or allergens are taken up within the epidermis and presented to the immune system (12, 51).
To induce epicutaneous sensitization to protein antigens in mice, the tough SC barrier needs to be mechanically impaired by tape-stripping, acetone treatment, or patch dressing (78). Interestingly, tape-stripping mouse ear skin activates LCs and induces penetration of the TJ barrier by LC dendrites, suggesting that causing physical stress to the SC induces danger signals in epidermis that directly or indirectly activate LCs (Figure 2 and refs. 13, 47, 50, 53–56). Thus, perturbation of the SC barrier not only allows allergen penetration throughout this barrier, but also triggers LC activation and facilitates subsequent uptake of antigens by LCs across the epidermal TJ barrier. After antigen acquisition, LCs presumably migrate to draining lymph nodes and activate antigen-specific T cells. Although danger signals similar to those observed in simple epithelium models, such as the lungs, may also occur in skin, as shown in Figure 2 (7, 53, 111–114), it is not yet clear how LCs sense danger signals caused by SC damage, and the specific signals that are delivered across the TJ barrier remain to be investigated.
The chicken or the egg in atopic diseases.
Skin barrier defects and immune disorders present a chicken and egg dilemma in AD. Allergens that have penetrated defective skin barriers induce inflammation, while inflammation itself can alter skin barrier integrity. Th2 and Th17 cytokines have been reported to downregulate filaggrin expression or proper processing of profilaggrin (115–119). Not only genetic skin barrier defects, but also genetic immune disorders such as Wiskott-Aldrich syndrome, show atopic manifestations (120), indicating that AD emerges in the context of both epidermal barrier- and immunity-associated genetic dysfunction. Indeed, many immunity-associated genes, e.g., Th2 and Th17 cytokines, innate immune receptors, and various chemokines, have been identified through whole-genome linkage studies of susceptibility genes for atopic diseases (75), some of which have been reported to show a multiplicative effect with FLG mutations on AD (121). It seems reasonable to suggest that immunity-associated genetic factors, as well as environmental factors, may act additively (or synergistically) to produce SC barrier defects and to promote percutaneous sensitization during the onset of AD.
Conquering the epidermal barrier is a double victory
Epidermal barriers face harsh challenges in modern life. Features of current lifestyles, such as frequent bathing and regular use of soap, and living within concrete jungles with air conditioning that dehumidifies the air, may accelerate SC barrier impairment (11). Constant heating, decreased ventilation, and floors covered with carpets are likely to increase house dust mite numbers and allergen levels in living environments. These environments, which expose the skin to both mechanical and allergic cues, may induce not only SC barrier damage but also danger signals that activate LCs, and could be a part of the reason why the prevalence of atopic diseases is increasing in industrialized countries (2). FLG mutations are associated with not only AD, but also atopic asthma, allergic rhinitis, and food allergy, emphasizing the importance of percutaneous sensitization as an initial trigger of atopic cascades, which lead to the atopic march (Figure 2). A simple and straightforward approach to preventing or controlling atopic cascades is to maintain intact epidermal barriers after birth or after improvement of acute inflammation (122). Clarification of the exact molecular functions of the epidermal barrier, with the SC as an air-liquid interface barrier, TJs as a liquid-liquid interface barrier, and LCs as an immunological barrier, will lead to a more sophisticated understanding as well as practical solutions for conquering atopic diseases.
Supplementary Material
Supplemental video 1
Supplemental video 2
Acknowledgments
This work was supported by Grants-in-Aid for Scientific Research and the “Promotion of Environmental Improvement for Independence of Young Researchers” program funding from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and by Health Labour Sciences Research Grants for Research on Allergic Diseases and Immunology from the Ministry of Health, Labour, and Welfare of Japan.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2012;122(2):440–447. doi:10.1172/JCI57416
References
- 1.Spergel JM. From atopic dermatitis to asthma: the atopic march. Ann Allergy Asthma Immunol. 2010;105(2):99–106. doi: 10.1016/j.anai.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Bieber T. Atopic dermatitis. N Engl J Med. 2008;358(14):1483–1494. doi: 10.1056/NEJMra074081. [DOI] [PubMed] [Google Scholar]
- 3.Furuse M, Tsukita S. Claudins in occluding junctions of humans and flies. Trends Cell Biol. 2006;16(4):181–188. doi: 10.1016/j.tcb.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Cookson W. The immunogenetics of asthma and eczema: a new focus on the epithelium. Nat Rev Immunol. 2004;4(12):978–988. doi: 10.1038/nri1500. [DOI] [PubMed] [Google Scholar]
- 5.Hackett T-L, Knight DA. The role of epithelial injury and repair in the origins of asthma. Curr Opin Allergy Clin Immunol. 2007;7(1):63–68. doi: 10.1097/ACI.0b013e328013d61b. [DOI] [PubMed] [Google Scholar]
- 6.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448(7152):427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 7.Hammad H, Lambrecht BN. Dendritic cells and epithelial cells: linking innate and adaptive immunity in asthma. Nat Rev Immunol. 2008;8(3):193–204. doi: 10.1038/nri2275. [DOI] [PubMed] [Google Scholar]
- 8.McGrath JA, Uitto J. The filaggrin story: novel insights into skin-barrier function and disease. Trends Mol Med. 2008;14(1):20–27. doi: 10.1016/j.molmed.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Schulzke JD, et al. Epithelial tight junctions in intestinal inflammation. Ann N Y Acad Sci. 2009;1165:294–300. doi: 10.1111/j.1749-6632.2009.04062.x. [DOI] [PubMed] [Google Scholar]
- 10.Turner JR. Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009;9(11):799–809. doi: 10.1038/nri2653. [DOI] [PubMed] [Google Scholar]
- 11.Cork MJ, et al. Epidermal barrier dysfunction in atopic dermatitis. J Invest Dermatol. 2009;129(8):1892–1908. doi: 10.1038/jid.2009.133. [DOI] [PubMed] [Google Scholar]
- 12.Beck LA, Leung DY. Allergen sensitization through the skin induces systemic allergic responses. J Allergy Clin Immunol. 2000;106(5 suppl):S258–S263. doi: 10.1067/mai.2000.110159. [DOI] [PubMed] [Google Scholar]
- 13.Kubo A, Nagao K, Yokouchi M, Sasaki H, Amagai M. External antigen uptake by Langerhans cells with reorganization of epidermal tight junction barriers. J Exp Med. 2009;206(13):2937–2946. doi: 10.1084/jem.20091527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aberg KM, et al. Co-regulation and interdependence of the mammalian epidermal permeability and antimicrobial barriers. J Invest Dermatol. 2008;128(4):917–925. doi: 10.1038/sj.jid.5701099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsukita S, Furuse M, Itoh M. Multifunctional strands in tight junctions. Nat Rev Mol Cell Biol. 2001;2(4):285–293. doi: 10.1038/35067088. [DOI] [PubMed] [Google Scholar]
- 16.Tsukita S, Yamazaki Y, Katsuno T, Tamura A. Tight junction-based epithelial microenvironment and cell proliferation. Oncogene. 2008;27(55):6930–6938. doi: 10.1038/onc.2008.344. [DOI] [PubMed] [Google Scholar]
- 17.Anderson JM, Van Itallie CM. Physiology and function of the tight junction. Cold Spring Harb Perspect Biol. 2009;1(2):a002584. doi: 10.1101/cshperspect.a002584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farquhar MG, Palade GE. Cell junctions in amphibian skin. J Cell Biol. 1965;26(1):263–291. doi: 10.1083/jcb.26.1.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mittal AK, Whitear M. Keratinization of fish skin with special reference to the catfish Bagarius bagarius. Cell Tissue Res. 1979;202(2):213–230. doi: 10.1007/BF00232236. [DOI] [PubMed] [Google Scholar]
- 20.Hashimoto K. Intercellular spaces of the human epidermis as demonstrated with lanthanum. . J Invest Dermatol. 1971;57(1):17–31. doi: 10.1111/1523-1747.ep12292052. [DOI] [PubMed] [Google Scholar]
- 21.Landmann L, Stolinski C, Martin B. The permeability barrier in the epidermis of the grass snake during the resting stage of the sloughing cycle. Cell Tissue Res. 1981;215(2):369–382. doi: 10.1007/BF00239121. [DOI] [PubMed] [Google Scholar]
- 22.Furuse M, et al. Claudin-based tight junctions are crucial for the mammalian epidermal barrier: a lesson from claudin-1-deficient mice. J Cell Biol. 2002;156(6):1099–1111. doi: 10.1083/jcb.200110122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brandner JM, et al. Organization and formation of the tight junction system in human epidermis and cultured keratinocytes. Eur J Cell Biol. 2002;81(5):253–263. doi: 10.1078/0171-9335-00244. [DOI] [PubMed] [Google Scholar]
- 24.Tsukita S, Furuse M. Claudin-based barrier in simple and stratified cellular sheets. Curr Opin Cell Biol. 2002;14(5):531–536. doi: 10.1016/S0955-0674(02)00362-9. [DOI] [PubMed] [Google Scholar]
- 25.Mackenzie IC. Relationship between mitosis and the ordered structure of the stratum corneum in mouse epidermis. Nature. 1970;226(5246):653–655. doi: 10.1038/226653a0. [DOI] [PubMed] [Google Scholar]
- 26.Christophers E. Cellular architecture of the stratum corneum. J Invest Dermatol. 1971;56(3):165–169. doi: 10.1111/1523-1747.ep12260765. [DOI] [PubMed] [Google Scholar]
- 27.Mackenzie IC. Ordered structure of the epidermis. J Invest Dermatol. 1975;65(1):45–51. doi: 10.1111/1523-1747.ep12598037. [DOI] [PubMed] [Google Scholar]
- 28.Elias PM, et al. The secretory granular cell: the outermost granular cell as a specialized secretory cell. J Invest Dermatol Symp Proc. 1998;3(2):87–100. doi: 10.1038/jidsymp.1998.20. [DOI] [PubMed] [Google Scholar]
- 29.Ishida-Yamamoto A, et al. Epidermal lamellar granules transport different cargoes as distinct aggregates. J Invest Dermatol. 2004;122(5):1137–1144. doi: 10.1111/j.0022-202X.2004.22515.x. [DOI] [PubMed] [Google Scholar]
- 30.Braff MH, Di Nardo A, Gallo RL. Keratinocytes store the antimicrobial peptide cathelicidin in lamellar bodies. J Invest Dermatol. 2005;124(2):394–400. doi: 10.1111/j.0022-202X.2004.23443.x. [DOI] [PubMed] [Google Scholar]
- 31.Oren A, Ganz T, Liu L, Meerloo T. In human epidermis, beta-defensin 2 is packaged in lamellar bodies. Exp Mol Pathol. 2003;74(2):180–182. doi: 10.1016/S0014-4800(02)00023-0. [DOI] [PubMed] [Google Scholar]
- 32.Kuroda S, et al. Perturbation of lamellar granule secretion by sodium caprate implicates epidermal tight junctions in lamellar granule function. J Dermatol Sci. 2010;59(2):107–114. doi: 10.1016/j.jdermsci.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 33.Montagna W, Parakkal P.The Structure And Function Of Skin . Orlando, Florida, USA: Academic Press; 1974. [Google Scholar]
- 34.Candi E, Schmidt R, Melino G. The cornified envelope: a model of cell death in the skin. Nat Rev Mol Cell Biol. 2005;6(4):328–340. doi: 10.1038/nrm1619. [DOI] [PubMed] [Google Scholar]
- 35.Simon M, et al. Refined characterization of corneodesmosin proteolysis during terminal differentiation of human epidermis and its relationship to desquamation. J Biol Chem. 2001;276(23):20292–20299. doi: 10.1074/jbc.M100201200. [DOI] [PubMed] [Google Scholar]
- 36.Kaplan DH. In vivo function of Langerhans cells and dermal dendritic cells. Trends Immunol. 2010;31(12):446–451. doi: 10.1016/j.it.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Merad M, Ginhoux F, Collin M. Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat Rev Immunol. 2008;8(12):935–947. doi: 10.1038/nri2455. [DOI] [PubMed] [Google Scholar]
- 38.Nagao K, et al. Murine epidermal Langerhans cells and langerin-expressing dermal dendritic cells are unrelated and exhibit distinct functions. Proc Natl Acad Sci U S A. 2009;106(9):3312–3317. doi: 10.1073/pnas.0807126106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elentner A, et al. Langerhans cells are critical in the development of atopic dermatitis-like inflammation and symptoms in mice. J Cell Mol Med. 2009;13(8B):2658–2672. doi: 10.1111/j.1582-4934.2009.00797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rescigno M, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2(4):361–367. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- 41.Ichiyasu H, McCormack JM, McCarthy KM, Dombkowski D, Preffer FI, Schneeberger EE. Matrix metalloproteinase-9-deficient dendritic cells have impaired migration through tracheal epithelial tight junctions. Am J Respir Cell Mol Biol. 2004;30(6):761–770. doi: 10.1165/rcmb.2003-0370OC. [DOI] [PubMed] [Google Scholar]
- 42.Niess JH, et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005;307(5707):254–258. doi: 10.1126/science.1102901. [DOI] [PubMed] [Google Scholar]
- 43.Takano K, et al. HLA-DR- and CD11c-positive dendritic cells penetrate beyond well-developed epithelial tight junctions in human nasal mucosa of allergic rhinitis. J Histochem Cytochem. 2005;53(5):611–619. doi: 10.1369/jhc.4A6539.2005. [DOI] [PubMed] [Google Scholar]
- 44.Chieppa M, Rescigno M, Huang AYC, Germain RN. Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J Exp Med. 2006;203(13):2841–2852. doi: 10.1084/jem.20061884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Blank F, Rothen-Rutishauser B, Gehr P. Dendritic cells and macrophages form a transepithelial network against foreign particulate antigens. Am J Respir Cell Mol Biol. 2007;36(6):669–677. doi: 10.1165/rcmb.2006-0234OC. [DOI] [PubMed] [Google Scholar]
- 46.Ogasawara N, et al. Epithelial barrier and antigen uptake in lymphoepithelium of human adenoids. Acta Otolaryngol. 2011;131(2):116–123. doi: 10.3109/00016489.2010.520022. [DOI] [PubMed] [Google Scholar]
- 47.Wood LC, Jackson SM, Elias PM, Grunfeld C, Feingold KR. Cutaneous barrier perturbation stimulates cytokine production in the epidermis of mice. J Clin Invest. 1992;90(2):482–487. doi: 10.1172/JCI115884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Streilein JW, Lonsberry LW, Bergstresser PR. Depletion of epidermal langerhans cells and Ia immunogenicity from tape-stripped mouse skin. . J Exp Med. 1982;155(3):863–871. doi: 10.1084/jem.155.3.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lessard RJ, Wolff K, Winkelmann RK. The disappearance and regeneration of Langerhans cells following epidermal injury. J Invest Dermatol. 1968;50(2):171–179. doi: 10.1038/jid.1968.20. [DOI] [PubMed] [Google Scholar]
- 50.Nishijima T, Tokura Y, Imokawa G, Seo N, Furukawa F, Takigawa M. Altered permeability and disordered cutaneous immunoregulatory function in mice with acute barrier disruption. J Invest Dermatol. 1997;109(2):175–182. doi: 10.1111/1523-1747.ep12319282. [DOI] [PubMed] [Google Scholar]
- 51.Ouchi T, et al. Langerhans cell antigen capture through tight junctions confers preemptive immunity in experimental staphylococcal scalded skin syndrome. J Exp Med. 2011;208(13):2607–2613. doi: 10.1084/jem.20111718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schröder JM, Harder J. Antimicrobial skin peptides and proteins. Cell Mol Life Sci. 2006;63(4):469–486. doi: 10.1007/s00018-005-5364-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dai X, et al. Mite allergen is a danger signal for the skin via activation of inflammasome in keratinocytes. J Allergy Clin Immunol. 2011;127(3):806–814. doi: 10.1016/j.jaci.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 54.Nishibu A, Ward BR, Boes M, Takashima A. Roles for IL-1 and TNFalpha in dynamic behavioral responses of Langerhans cells to topical hapten application. J Dermatol Sci. 2007;45(1):23–30. doi: 10.1016/j.jdermsci.2006.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Briot A, et al. Kallikrein 5 induces atopic dermatitis-like lesions through PAR2-mediated thymic stromal lymphopoietin expression in Netherton syndrome. J Exp Med. 2009;206(5):1135–1147. doi: 10.1084/jem.20082242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ebner S, et al. Thymic stromal lymphopoietin converts human epidermal Langerhans cells into antigen-presenting cells that induce proallergic T cells. J Allergy Clin Immunol. 2007;119(4):982–990. doi: 10.1016/j.jaci.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 57.Pearton DJ, Dale BA, Presland RB. Functional analysis of the profilaggrin N-terminal peptide: identification of domains that regulate nuclear and cytoplasmic distribution. J Invest Dermatol. 2002;119(3):661–669. doi: 10.1046/j.1523-1747.2002.01831.x. [DOI] [PubMed] [Google Scholar]
- 58.Dale BA, Holbrook KA, Steinert PM. Assembly of stratum corneum basic protein and keratin filaments in macrofibrils. Nature. 1978;276(5689):729–731. doi: 10.1038/276729a0. [DOI] [PubMed] [Google Scholar]
- 59.Scott IR, Harding CR. Filaggrin breakdown to water binding compounds during development of the rat stratum corneum is controlled by the water activity of the environment. Dev Biol. 1986;115(1):84–92. doi: 10.1016/0012-1606(86)90230-7. [DOI] [PubMed] [Google Scholar]
- 60.Rawlings AV, Matts PJ. Stratum corneum moisturization at the molecular level: an update in relation to the dry skin cycle. J Invest Dermatol. 2005;124(6):1099–1110. doi: 10.1111/j.1523-1747.2005.23726.x. [DOI] [PubMed] [Google Scholar]
- 61.J Cell Sci. 2009;122(9):1285–1294. doi: 10.1242/jcs.033969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Smith FJD, et al. Loss-of-function mutations in the gene encoding filaggrin cause ichthyosis vulgaris. Nat Genet. 2006;38(3):337–342. doi: 10.1038/ng1743. [DOI] [PubMed] [Google Scholar]
- 63.Palmer CN, et al. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006;38(4):441–446. doi: 10.1038/ng1767. [DOI] [PubMed] [Google Scholar]
- 64.Sandilands A, et al. Comprehensive analysis of the gene encoding filaggrin uncovers prevalent and rare mutations in ichthyosis vulgaris and atopic eczema. Nat Genet. 2007;39(5):650–654. doi: 10.1038/ng2020. [DOI] [PubMed] [Google Scholar]
- 65.O’Regan GM, Sandilands A, McLean WHI, Irvine AD. Filaggrin in atopic dermatitis. J Allergy Clin Immunol. 2008;122(4):689–693. doi: 10.1016/j.jaci.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 66.Akiyama M. FLG mutations in ichthyosis vulgaris and atopic eczema: spectrum of mutations and population genetics. Br J Dermatol. 2010;162(3):472–477. doi: 10.1111/j.1365-2133.2009.09582.x. [DOI] [PubMed] [Google Scholar]
- 67.Poninska J, et al. Filaggrin gene defects are independent risk factors for atopic asthma in a Polish population: a study in ECAP cohort. PLoS ONE. 2011;6(2):e16933. doi: 10.1371/journal.pone.0016933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Basu K, et al. Filaggrin null mutations are associated with increased asthma exacerbations in children and young adults. Allergy. 2008;63(9):1211–1217. doi: 10.1111/j.1398-9995.2008.01660.x. [DOI] [PubMed] [Google Scholar]
- 69.Novak N, et al. Loss-of-function mutations in the filaggrin gene and allergic contact sensitization to nickel. J Invest Dermatol. 2008;128(6):1430–1435. doi: 10.1038/sj.jid.5701190. [DOI] [PubMed] [Google Scholar]
- 70.Rodríguez E, et al. Meta-analysis of filaggrin polymorphisms in eczema and asthma: robust risk factors in atopic disease. J Allergy Clin Immunol. 2009;123(6):1361–1370. doi: 10.1016/j.jaci.2009.03.036. [DOI] [PubMed] [Google Scholar]
- 71.Schuttelaar MLA, et al. Filaggrin mutations in the onset of eczema, sensitization, asthma, hay fever and the interaction with cat exposure. Allergy. 2009;64(12):1758–1765. doi: 10.1111/j.1398-9995.2009.02080.x. [DOI] [PubMed] [Google Scholar]
- 72.Thyssen JP, et al. The association between null mutations in the filaggrin gene and contact sensitization to nickel and other chemicals in the general population. Br J Dermatol. 2010;162(6):1278–1285. doi: 10.1111/j.1365-2133.2010.09708.x. [DOI] [PubMed] [Google Scholar]
- 73.Brown SJ, et al. Loss-of-function variants in the filaggrin gene are a significant risk factor for peanut allergy. J Allergy Clin Immunol. 2011;127(3):661–667. doi: 10.1016/j.jaci.2011.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vercelli D. Discovering susceptibility genes for asthma and allergy. Nat Rev Immunol. 2008;8(3):169–182. doi: 10.1038/nri2257. [DOI] [PubMed] [Google Scholar]
- 75.Barnes KC. An update on the genetics of atopic dermatitis: scratching the surface in 2009. J Allergy Clin Immunol. 2010;125(1):16–29. doi: 10.1016/j.jaci.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.De Benedetto A, Qualia CM, Baroody FM, Beck LA. Filaggrin expression in oral, nasal, and esophageal mucosa. J Invest Dermatol. 2008;128(6):1594–1597. doi: 10.1038/sj.jid.5701208. [DOI] [PubMed] [Google Scholar]
- 77.Kodama M, et al. Strain-specific phenotypes of airway inflammation and bronchial hyperresponsiveness induced by epicutaneous allergen sensitization in BALB/c and C57BL/6 mice. Int Arch Allergy Immunol. 2010;152 suppl 1:67–74. doi: 10.1159/000312128. [DOI] [PubMed] [Google Scholar]
- 78.Spergel JM, Mizoguchi E, Brewer JP, Martin TR, Bhan AK, Geha RS. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest. 1998;101(8):1614–1622. doi: 10.1172/JCI1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Presland RB, Boggess D, Lewis SP, Hull C, Fleckman P, Sundberg JP. Loss of normal profilaggrin and filaggrin in flaky tail (ft/ft) mice: an animal model for the filaggrin-deficient skin disease ichthyosis vulgaris. J Invest Dermatol. 2000;115(6):1072–1081. doi: 10.1046/j.1523-1747.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 80.Sundberg JP. The flaky tail (ft) mutation. In: Sundberg JP, ed.Handbook of Mouse Mutations with Skin and Hair Abnormalities. Animal Models and Biochemical Tools . Vol. 2. Ann Arbor, Michigan, USA: CRC Press; 1984:269–273. [Google Scholar]
- 81.Fallon PG, et al. A homozygous frameshift mutation in the mouse Flg gene facilitates enhanced percutaneous allergen priming. Nat Genet. 2009;41(5):602–608. doi: 10.1038/ng.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Scharschmidt TC, et al. Filaggrin deficiency confers a paracellular barrier abnormality that reduces inflammatory thresholds to irritants and haptens. J Allergy Clin Immunol. 2009;124(3):496–506. doi: 10.1016/j.jaci.2009.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Moniaga CS, et al. Flaky tail mouse denotes human atopic dermatitis in the steady state and by topical application with Dermatophagoides pteronyssinus extract. Am J Pathol. 2010;176(5):2385–2393. doi: 10.2353/ajpath.2010.090957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Deraison C, et al. LEKTI fragments specifically inhibit KLK5, KLK7, and KLK14 and control desquamation through a pH-dependent interaction. Mol Biol Cell. 2007;18(9):3607–3619. doi: 10.1091/mbc.E07-02-0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ovaere P, Lippens S, Vandenabeele P, Declercq W. The emerging roles of serine protease cascades in the epidermis. Trends Biochem Sci. 2009;34(9):453–463. doi: 10.1016/j.tibs.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 86.Walley AJ, et al. Gene polymorphism in Netherton and common atopic disease. Nat Genet. 2001;29(2):175–178. doi: 10.1038/ng728. [DOI] [PubMed] [Google Scholar]
- 87.Kato A, Fukai K, Oiso N, Hosomi N, Murakami T, Ishii M. Association of SPINK5 gene polymorphisms with atopic dermatitis in the Japanese population. Br J Dermatol. 2003;148(4):665–669. doi: 10.1046/j.1365-2133.2003.05243.x. [DOI] [PubMed] [Google Scholar]
- 88.Nishio Y, et al. Association between polymorphisms in the SPINK5 gene and atopic dermatitis in the Japanese. Genes Immun. 2003;4(7):515–517. doi: 10.1038/sj.gene.6363889. [DOI] [PubMed] [Google Scholar]
- 89.Chavanas S, et al. Mutations in SPINK5, encoding a serine protease inhibitor, cause Netherton syndrome. Nat Genet. 2000;25(2):141–142. doi: 10.1038/75977. [DOI] [PubMed] [Google Scholar]
- 90.Frenk E, Mevorah B. Ichthyosis linearis circumflexa Comèl with Trichorrhexis invaginata (Netherton’s Syndrom): an ultrastructural study of the skin changes. Arch Dermatol Forsch. 1972;245(1):42–49. doi: 10.1007/BF00596151. [DOI] [PubMed] [Google Scholar]
- 91.Fartasch M, Williams ML, Elias PM. Altered lamellar body secretion and stratum corneum membrane structure in Netherton syndrome: differentiation from other infantile erythrodermas and pathogenic implications. Arch Dermatol. 1999;135(7):823–832. doi: 10.1001/archderm.135.7.823. [DOI] [PubMed] [Google Scholar]
- 92.Müller FB, et al. Genetic analysis of a severe case of Netherton syndrome and application for prenatal testing. Br J Dermatol. 2002;146(3):495–499. doi: 10.1046/j.1365-2133.2002.04625.x. [DOI] [PubMed] [Google Scholar]
- 93.Yang T, Liang D, Koch PJ, Hohl D, Kheradmand F, Overbeek PA. Epidermal detachment, desmosomal dissociation, and destabilization of corneodesmosin in Spink5–/– mice. . Genes Dev. 2004;18(19):2354–2358. doi: 10.1101/gad.1232104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Descargues P, et al. Spink5-deficient mice mimic Netherton syndrome through degradation of desmoglein 1 by epidermal protease hyperactivity. Nat Genet. 2005;37(1):56–65. doi: 10.1038/ng1493. [DOI] [PubMed] [Google Scholar]
- 95.Descargues P, et al. Corneodesmosomal cadherins are preferential targets of stratum corneum trypsin- and chymotrypsin-like hyperactivity in Netherton syndrome. J Invest Dermatol. 2006;126(7):1622–1632. doi: 10.1038/sj.jid.5700284. [DOI] [PubMed] [Google Scholar]
- 96.Vasilopoulos Y, et al. Genetic association between an AACC insertion in the 3’UTR of the stratum corneum chymotryptic enzyme gene and atopic dermatitis. J Invest Dermatol. 2004;123(1):62–66. doi: 10.1111/j.0022-202X.2004.22708.x. [DOI] [PubMed] [Google Scholar]
- 97.Oji V, et al. Loss of corneodesmosin leads to severe skin barrier defect, pruritus, and atopy: unraveling the peeling skin disease. Am J Hum Genet. 2010;87(2):274–281. doi: 10.1016/j.ajhg.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bonnart C, et al. Elastase 2 is expressed in human and mouse epidermis and impairs skin barrier function in Netherton syndrome through filaggrin and lipid misprocessing. J Clin Invest. 2010;120(3):871–882. doi: 10.1172/JCI41440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Matsui T, et al. Skin-specific aspartic protease SASPase regulate stratum corneum hydration through profilaggrin processing. EMBO Mol Med. 2011;3(6):320–333. doi: 10.1002/emmm.201100140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Denecker G, et al. Caspase-14 protects against epidermal UVB photodamage and water loss. Nat Cell Biol. 2007;9(6):666–674. doi: 10.1038/ncb1597. [DOI] [PubMed] [Google Scholar]
- 101.Hoste E, et al. Caspase–14 is required for filaggrin degradation to natural moisturizing factors in the skin [published online ahead of print June 9, 2011].J Invest Dermatol . doi:10.1038/jid.2011.153. [DOI] [PubMed] [Google Scholar]
- 102.Kamata Y, et al. Neutral cysteine protease bleomycin hydrolase is essential for the breakdown of deiminated filaggrin into amino acids. J Biol Chem. 2009;284(19):12829–12836. doi: 10.1074/jbc.M807908200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kamata Y, et al. Bleomycin hydrolase is regulated biphasically in a differentiation- and cytokine-dependent manner: relevance to atopic dermatitis. J Biol Chem. 2011;286(10):8204–8212. doi: 10.1074/jbc.M110.169292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schwartz DR, Homanics GE, Hoyt DG, Klein E, Abernethy J, Lazo JS. The neutral cysteine protease bleomycin hydrolase is essential for epidermal integrity and bleomycin resistance. Proc Natl Acad Sci U S A. 1999;96(8):4680–4685. doi: 10.1073/pnas.96.8.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Morita K, et al. Molecular architecture of tight junctions of periderm differs from that of the maculae occludentes of epidermis. J Invest Dermatol. 2002;118(6):1073–1079. doi: 10.1046/j.1523-1747.2002.01774.x. [DOI] [PubMed] [Google Scholar]
- 106.Development. 2002;129(7):1775–1784. doi: 10.1242/dev.129.7.1775. [DOI] [PubMed] [Google Scholar]
- 107.Hadj-Rabia S, et al. Claudin-1 gene mutations in neonatal sclerosing cholangitis associated with ichthyosis: a tight junction disease. Gastroenterology. 2004;127(5):1386–1390. doi: 10.1053/j.gastro.2004.07.022. [DOI] [PubMed] [Google Scholar]
- 108.Feldmeyer L, Huber M, Fellmann F, Beckmann JS, Frenk E, Hohl D. Confirmation of the origin of NISCH syndrome. Hum Mutat. 2006;27(5):408–410. doi: 10.1002/humu.20333. [DOI] [PubMed] [Google Scholar]
- 109.De Benedetto A, et al. Tight junction defects in patients with atopic dermatitis. J Allergy Clin Immunol. 2011;127(3):773–786. doi: 10.1016/j.jaci.2010.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Uitto J, McGrath JA, Rodeck U, Bruckner-Tuderman L, Robinson EC. Progress in epidermolysis bullosa research: toward treatment and cure. . J Invest Dermatol. 2010;130(7):1778–1784. doi: 10.1038/jid.2010.90. [DOI] [PubMed] [Google Scholar]
- 111.Wan H, et al. Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions. J Clin Invest. 1999;104(1):123–133. doi: 10.1172/JCI5844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hammad H, Chieppa M, Perros F, Willart MA, Germain RN, Lambrecht BN. House dust mite allergen induces asthma via Toll-like receptor 4 triggering of airway structural cells. Nat Med. 2009;15(4):410–416. doi: 10.1038/nm.1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kato T, et al. Mite serine protease activates protease-activated receptor-2 and induces cytokine release in human keratinocytes. Allergy. 2009;64(9):1366–1374. doi: 10.1111/j.1398-9995.2009.02023.x. [DOI] [PubMed] [Google Scholar]
- 114.Vu AT, et al. Staphylococcus aureus membrane and diacylated lipopeptide induce thymic stromal lymphopoietin in keratinocytes through the Toll-like receptor 2-Toll-like receptor 6 pathway. J Allergy Clin Immunol. 2010;126(5):985–993. doi: 10.1016/j.jaci.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 115.Kim BE, et al. TNF-alpha downregulates filaggrin and loricrin through c-Jun N-terminal kinase: role for TNF-alpha antagonists to improve skin barrier. . J Invest Dermatol. 2011;131(6):1272–1279. doi: 10.1038/jid.2011.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Howell MD, et al. Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol. 2007;120(1):150–155. doi: 10.1016/j.jaci.2007.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gutowska-Owsiak D, Schaupp AL, Salimi M, Taylor S, Ogg GS. Interleukin-22 downregulates filaggrin expression and affects expression of profilaggrin processing enzymes. Br J Dermatol. 2011;165(3):492–498. doi: 10.1111/j.1365-2133.2011.10400.x. [DOI] [PubMed] [Google Scholar]
- 118.Hvid M, Vestergaard C, Kemp K, Christensen GB, Deleuran B, Deleuran M. IL-25 in atopic dermatitis: a possible link between inflammation and skin barrier dysfunction? J Invest Dermatol. 2011;131(1):150–157. doi: 10.1038/jid.2010.277. [DOI] [PubMed] [Google Scholar]
- 119.Hvid M, Johansen C, Deleuran B, Kemp K, Deleuran M, Vestergaard C. Regulation of caspase 14 expression in keratinocytes by inflammatory cytokines - a possible link between reduced skin barrier function and inflammation? Exp Dermatol. 2011;20(8):633–636. doi: 10.1111/j.1600-0625.2011.01280.x. [DOI] [PubMed] [Google Scholar]
- 120.Ozcan E, Notarangelo LD, Geha RS. Primary immune deficiencies with aberrant IgE production. J Allergy Clin Immunol. 2008;122(6):1054–1062. doi: 10.1016/j.jaci.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 121.Lesiak A, et al. Combined occurrence of filaggrin mutations and IL-10 or IL-13 polymorphisms predisposes to atopic dermatitis. Exp Dermatol. 2011;20(6):491–495. doi: 10.1111/j.1600-0625.2010.01243.x. [DOI] [PubMed] [Google Scholar]
- 122.Simpson EL, Berry TM, Brown PA, Hanifin JM. A pilot study of emollient therapy for the primary prevention of atopic dermatitis. J Am Acad Dermatol. 2010;63(4):587–593. doi: 10.1016/j.jaad.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Stefansson K, et al. Activation of proteinase-activated receptor-2 by human kallikrein-related peptidases. J Invest Dermatol. 2008;128(1):18–25. doi: 10.1038/sj.jid.5700965. [DOI] [PubMed] [Google Scholar]
- 124.Enk AH, Angeloni VL, Udey MC, Katz SI. An essential role for Langerhans cell-derived IL-1 beta in the initiation of primary immune responses in skin. . J Immunol. 1993;150(9):3698–3704. [PubMed] [Google Scholar]
- 125.Vasilopoulos Y, et al. A nonsynonymous substitution of cystatin A, a cysteine protease inhibitor of house dust mite protease, leads to decreased mRNA stability and shows a significant association with atopic dermatitis. Allergy. 2007;62(5):514–519. doi: 10.1111/j.1398-9995.2007.01350.x. [DOI] [PubMed] [Google Scholar]
- 126.Hubiche T, et al. Analysis of SPINK 5, KLK 7 and FLG genotypes in a French atopic dermatitis cohort. Acta Dermato-Venereologica. 2007;87(6):499–505. doi: 10.2340/00015555-0329. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental video 1
Supplemental video 2