Plant-Derived Natural Products as Lead Agents against Common Respiratory Diseases (original) (raw)
Abstract
Never has the world been more challenged by respiratory diseases (RDs) than it has witnessed in the last few decades. This is evident in the plethora of acute and chronic respiratory conditions, ranging from asthma and chronic obstructive pulmonary disease (COPD) to multidrug-resistant tuberculosis, pneumonia, influenza, and more recently, the novel coronavirus (COVID-19) disease. Unfortunately, the emergence of drug-resistant strains of pathogens, drug toxicity and side effects are drawbacks to effective chemotherapeutic management of RDs; hence, our focus on natural sources because of their unique chemical diversities and novel therapeutic applications. This review provides a summary on some common RDs, their management strategies, and the prospect of plant-derived natural products in the search for new drugs against common respiratory diseases.
Keywords: respiratory diseases, natural products, plant-derived compounds, lead molecules
1. Introduction
The human respiratory system, otherwise known as the ventilatory system, is a biological system made up of specific organs and structures such as oropharyngeal and nasopharyngeal cavities, larynx, and trachea (upper respiratory tract), and the lower respiratory tract, which includes bronchi, lungs, and diaphragm [1,2,3]. The lungs are an important part of the respiratory system that facilitate gas exchange from the environment into the bloodstream for healthy living [4].
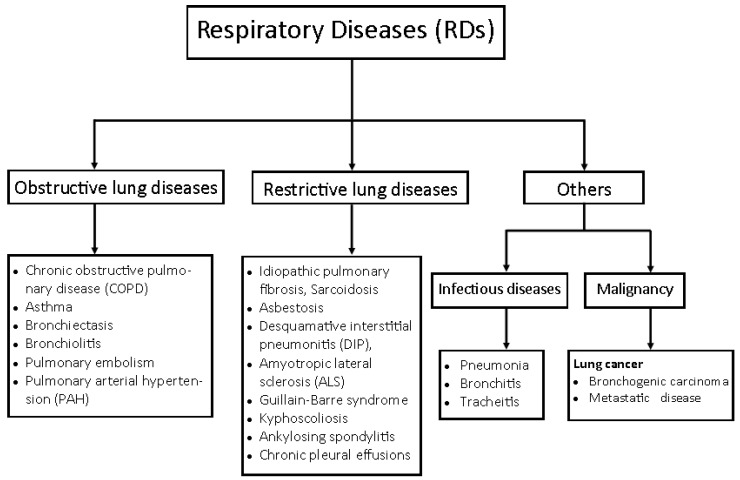
The respiratory functions can be hampered by infections and diseases of the lungs and their associated organs and structures. These diseases are categorised as obstructive and restrictive lung diseases [4]. Examples of obstructive lung diseases are asthma and chronic obstructive pulmonary disorder (chronic bronchitis), while restrictive lung diseases include idiopathic pulmonary fibrosis, pneumoconiosis, and sarcoidosis [5] (Figure 1). These respiratory diseases (RDs), otherwise referred to as “respiratory disorders”, “airways diseases”, “pulmonary diseases” or lung diseases, often arise from bacterial and viral infections in the upper and lower respiratory tracts, causing the common cold, otitis, sinusitis, pharyngitis, epiglottitis, laryngotracheitis, bronchitis, bronchiolitis, and pneumonia [6]. Some of the causative agents include Mycobacterium tuberculosis, Haemophilus influenza type b., Streptococcus pyogenes, Chlamydia sp., and Candida albicans [7] (Table 1).
Figure 1.
Group of respiratory diseases (RDs) adapted with permission from Kritek and Choi [25]. Copyright 2016, Basicmedical key.
Some viral infections of the respiratory tracts are implicated in disease pandemics such as influenza (flu), Middle east respiratory syndrome coronavirus (MERS-CoV), and more recently, the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection-causing COVID-19 disease that is currently ravaging the world [8]. SARS-CoV and MERS-CoV broke out in 2003 and 2012, respectively [9], and influenza claimed about 389,000 lives globally in the year 2017 [10]. As of 22 January 2022, about 5.59 million people had died from 346 million reported cases of COVID-19 globally [11]. These show the significant negative impacts of RDs on individual lives, national development, and human existence.
Inhalation therapy is one of the oldest approaches, yet still relevant to the management of RDs, dating back to more than 2000 years of Ayurvedic medicine in India [12]. It is centred around delivery of high pulmonary drug concentrations to the lungs, at low inhaled doses; thus, it offers substantial efficacy while simultaneously reducing the risk of side effects associated with many orally or intravenously administered drug doses [13,14]. Recent advances in the management of RDs include vaccination; use of drugs such as antibiotics, agonists, and cortisones; ventilatory support; inhalation therapy, and lung surgery [15]. Unfortunately, new RDs continue to emerge, while multi-drug resistant strains and variants of pathogens continue to render many available drugs ineffective [16,17], hence the need for more efficacious and less toxic anti-infective agents that could help to reduce the burden of RDs and forestall seasonal or regular disease pandemics in the nearest future.
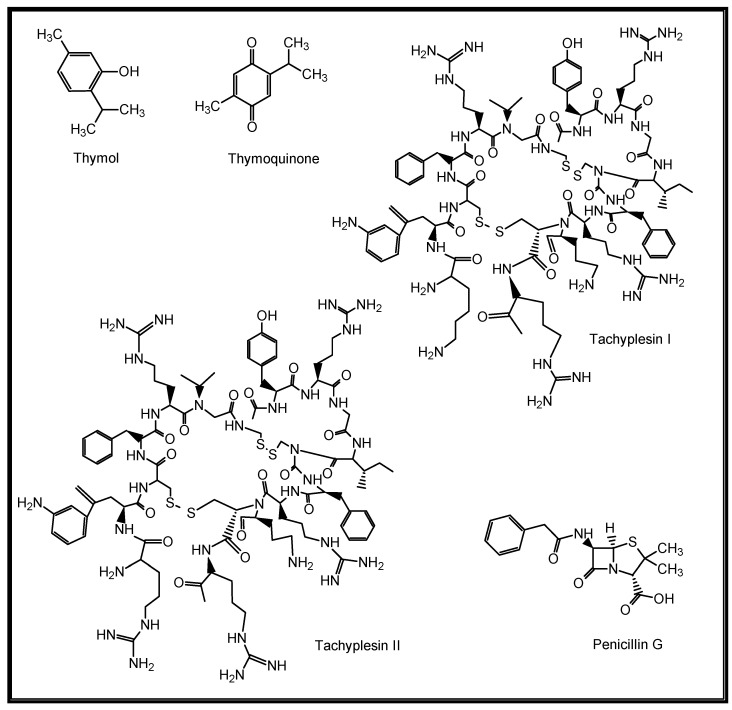
The role of natural products (NPs) in drug discovery cannot be over-emphasized. NPs are chemical substances produced by living organisms such as plants, animals, and marine organisms [18]. They are primary and secondary metabolites and may only be isolatable in small quantities from natural sources [19]. Structurally, they range from small molecules, such as thymol, thymoquinone and penicillin, to complex molecules such as tachyplesin I and II, with unique chemical and biological properties (Figure 2). They are important leads to new drugs and are thus categorised as drug candidates [20,21,22].
Figure 2.
Structures of some naturally occurring bioactive compounds.
NPs are regarded as the hallmark of modern pharmaceutical care because they continue to provide new leads with novel biological mechanisms of action against emerging diseases [23]. Currently, about 60% of drugs in the market worldwide are natural product-derived [24], which underlines the significance of NPs in the discovery of new drugs.
This review puts respiratory diseases (RDs) in perspective and summarises the prospect of plant-derived natural products in the discovery of new drugs against some common respiratory diseases, including asthma, COPD, tuberculosis, pneumonia, influenza, and COVID-19.
2. Methodology
An extensive literature survey of published articles was conducted, using scientific databases such as Google Scholar, Mendeley, PubMed, ScienceDirect and Scopus. The keywords included: “respiratory diseases”, “common respiratory diseases” and “natural products” searched singly and in pairs; “medicinal plant agents for respiratory diseases”; “natural compounds for common respiratory diseases”; and “prospects of natural products in the management of common respiratory diseases”. Publications were obtained from the literature search until March, 2022 with no language restriction. Data inclusion criteria included: reports on natural or nature-inspired compounds implicated against respiratory diseases (RDs); and reports indicating lung, airways and pulmonary disorders or diseases and their diagnostic and management strategies. Data exclusion criteria were reports on the same natural compounds with the same biological activities linked to respiratory diseases, to avoid duplication, and reports on natural compounds against diseases other than RDs as well as those biological activities (e.g., antidiabetic, antimalaria, neuroprotective and insecticidal) not directly linked to respiratory diseases. The structures of compounds were generated using the ChemDraw Ultra® 7.0 software package, CambridgeSoft Corporation (Cambridge, MA 02140, USA).
This review may be the first to highlight the major categories of respiratory diseases, their therapeutic management, and the prospect of natural products of plant origin in the discovery of new drug candidates against some common RDs such as asthma, COPD, TB, pneumonia, influenza, and COVID-19.
3. Respiratory Diseases in Focus
3.1. Risk Factors and Epidemiology
Respiratory diseases (RDs) are illnesses that affect the organs and tissues in the lungs and airways, limiting gas exchange and breathing [26]. They include acute respiratory infections and chronic respiratory diseases (CRDs) such as influenza, pneumonia, bronchitis, lung cancer, and chronic obstructive pulmonary disorder (COPD) [27]. CRDs are diseases of the airways and other structures of the lungs, such as asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, occupational lung diseases, interstitial lung disease, and pulmonary hypertension amongst others [28] (Figure 1).
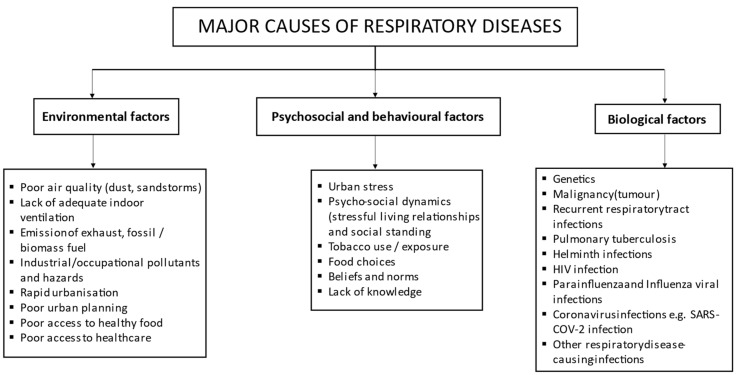
Common risk factors for RDs include tobacco smoking, high levels of air pollution, occupational hazards (dusts and chemicals), urbanization, industrialization, poor socioeconomic and health services, the HIV/AIDS epidemic, and respiratory tract infections and genetics [29,30,31] (Figure 3). Most upper respiratory tract infections are of viral aetiology except for a few caused by pathogenic bacteria, such as epiglottitis and laryngotracheitis caused by Haemophilus influenza type b, and pharyngitis often caused by Streptococcus pyogenes [32]. For example, the common cold is a viral respiratory infection caused by rhinoviruses, coronavirus, parainfluenza viruses, influenza virus, adenoviruses, and respiratory syncytial virus [32]. Some common respiratory diseases, their global morbidity ranking (disease burden), and causative agents are presented in Table 1, while Figure 3 shows the major factors responsible for RDs.
Figure 3.
Major causes of respiratory diseases, adapted with permission from Ku et al. [31].
Table 1.
Common respiratory diseases, their levels of occurrence, and causes.
| Respiratory Disease | Global MorbidityRanking[33,34,35,36] | Cause | Class | Reference |
|---|---|---|---|---|
| COPD | 1st | Haemophilus influenza and Streptococcus pneumoniae | Bacteria | [37] |
| Influenza viruses, Rhinoviruses | Virus | |||
| Asthma | 2nd | Allergens and irritants (pollen, mould, dust, feathers, animal fur, smoke, fumes, perfume)Psychosocial (mental stress, laughter)Medicines (ibuprofen, aspirin) | - | [38] |
| Haemophilus influenza and_Streptococcus pneumoniae_ | Bacteria | |||
| Pulmonary hypertension | 3rd | High blood pressure, cirrhosis, congenital and coronary heart diseases, emphysema, genetic factor | - | [39] |
| Tuberculosis | 4th | Mycobacterium tuberculosis, Mycobacterium africanum, Mycobacterium bovis, and Mycobacterium microti | Bacteria | [40] |
| Pneumonia | 5th | Adenoviruses, Parainfluenza viruses, Influenza viruses, Measles virus, Herpes simplex virus, Respiratory syncytial virus, Coronavirus | Viruses | [32,41] |
| Cryptococcus neoformans, | Bacteria | |||
| Histoplasma capsulatum, Candida albicans, Aspergillus spp. | Fungi | |||
| Influenza | 6th | Influenza A virus, Influenza B virus, Influenza C virus, Influenza D virus | Viruses | [42] |
| Lung cancer | 7th | Human Papilloma virus, Epstein-Barr virus, BK virus, JC virus, Human Cytomegalovirus, Simian virus 40, and Measles virus, Human Herpesvirus 8, Human immunodeficiency virus, | Viruses | [43] |
| Chlamydia pneumonia | Bacteria | |||
| * COVID-19 | 8th | Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) | Virus | [44] |
| Upper and lower respiratory tract infections(Pharyngitis, tonsillopharyngitisEpiglottitis and laryngotracheitis,Bronchitis and bronchiolitis) | 9th | Streptococcus pneumonia, Mycoplasma pneumonia, Haemophilus influenza type b, Corynebacterium diphtheriae | Bacteria | [32] |
| Parainfluenza virus, Epstein-Barr virus (EBV), Herpes Simplex virus, Coronavirus, Rhinovirus, Respiratory syncytial virus (RSV), Parainfluenza viruses, Adenoviruses, Herpes simplex virus | Viruses | |||
| Candida albicans | Fungi | |||
| Others:Common cold | 10th | Rhinoviruses, Parainfluenza viruses, Influenza viruses, Coronavirus, Respiratory syncytial virus | Viruses | [45,46] |
| Oral candidiasis | Candida albicans | Fungi |
Respiratory diseases (RDs) constitute a major public health problem worldwide. Ferkol and Schraufnagel highlighted five conditions that primarily contribute to the global burden of respiratory diseases, which are asthma, COPD, acute respiratory infections, tuberculosis, and lung cancer [47].
In the last one decade, an average of 65 million people suffered from moderate to severe levels of COPD, from which 3 million people die each year [48]. About 334 million people suffer from asthma, and influenza virus-related diseases are responsible for up to 400,000 deaths annually; tuberculosis caused about 1.4 million deaths in 2015, and about 1.6 million people die annually from lung cancer. More than 100 million people suffer from sleep-disordered breathing, and over 50 million people struggle with occupational lung diseases, while millions of people live with pulmonary hypertension [48]. Bronchial asthma and COPD account for a significant burden in low- and middle-income countries [28].
Furthermore, in 2017, about 540 million people in the world suffered from chronic respiratory diseases, such as asthma, COPD, pulmonary sarcoidosis, interstitial lung disease, silicosis, asbestosis, which is an increase of about 40% when compared to the 1990 figures [49,50]. Mortality due to these diseases stood at 3.9 million in 2017, which is about 18% increase since the 1990 report [34]. Tobacco smoking accounted for the most prevalent cause of disability due to RDs in men worldwide, while the leading risk factors for disability in women were household air pollution from solid fuel use in South Asia and sub-Saharan Africa, exposure to ambient particulate matter in Southeast Asia, East Asia, Oceania, and the developed regions within North Africa and Middle East, and smoking in all other developed regions [36].
In sub-Saharan Africa, about 83% of residents still use solid fuel for cooking, which, according to the WHO, is responsible for 130/100,000 deaths in the region [50]. Many countries are still battling rising epidemics of tobacco smoking among women and adolescents, while the levels of ambient particulate matter pollution, ambient ozone pollution, and several occupational exposures increased significantly between 1990 and 2017 [51,52]. A report has also shown the significant association between ambient temperature and the burden of morbidity caused by RDs within the sub-tropics, where it was found that exposure to non-optimal temperatures increased the risk of respiratory morbidity, and moderate heat contributes significantly to the morbidities of temperature related RDs [53].
Respiratory diseases are known to affect significantly the infant and young population across the globe. For instance, pneumonia has been reported to cause about 1.3 million childhood deaths every year, asthma is the commonest non-communicable disease in children, while paediatric tuberculosis (TB) constitutes up to 20% of the TB morbidity in high-incidence countries [54]. There are up to 10 million new cases of clinical TB globally and 1.5 million deaths every year, with the emergence of drug-resistant TB considered as a major public health crisis [55].
It is noteworthy that respiratory tract infections contribute significantly to morbidity and mortality of RDs. According to the WHO, lower respiratory infection is the most common infectious disease-causing deaths worldwide, accounting for the loss of about 3.46 million deaths annually, with most of them being children in developing countries [56].
Respiratory diseases impose a huge economic burden on both industrialized and developing countries [57]. RDs cost the United Kingdom about GBP 11.1 billion in 2014, which comprised GBP 9.9 billion in treatment costs and an estimated GBP 1.2 billion loss in productivity [58]. Annual expenditures for workers in the United States summed up to USD 7 billion for asthma care and USD 5 billion for COPD care between 2011 and 2015, according to the Centre for Disease Control and Prevention (CDC) report [59]. The annual cost of treatment for patients with an RD in the Asia-Pacific region was estimated at USD 4191 per patient, while the mean annual cost of treatment for patients who reported lung impairment at work was USD 7315 in 2014, thus resulting in a 36% reduction in productivity [60]. In the Central Asian countries (Eurasia) such as Kyrgyzstan, Uzbekistan, Tajikistan, Kazakhstan and Turkmenistan, the prevalence of TB is still significantly high, placing enormous costs on the government and patients [61]. In sub-Saharan Africa, deaths associated with solid fuel rose by 18% between 1990 and 2013 and cost the African economy approximately USD 232 billion by the year 2013 [62].
3.2. Management Strategies
The effective treatment of RDs will reduce the disease burden and health care costs and improve quality of life and productivity [60]. Over the last few decades, RDs have been managed by vaccination, hormone therapy such as the use of corticosteroids, targeted therapy such as the use of nebulizer, and chemotherapy such as the use of antibiotics (antibacterial and antifungal drugs) and antiviral and cytotoxic drugs [63]. However, many of these management regimens have their complications and adverse side effects. The continuous emergence of novel respiratory infections such as SAR-CoV-2, the resurgence of new strains of pathogens such as the multi-drug resistant strains of TB, and the complexities in their mode of action, are major setbacks to effective vaccination [64,65]. Hormone therapy has been reported to be associated with increased risk of asthma among pre-menopausal women [66].
In recent times, many of the currently approved drugs have presented with numerous complications. For instance, bleomycin has been reported to cause inflammation of the lungs (lung fibrosis) and breathlessness, among the most common clinical presentations of which are interstitial pneumonitis/fibrosis, hypersensitivity pneumonitis, and capillary leak syndrome [67]. Beta (2)-agonists administered as therapy for asthma and COPD have recognised systemic sequelae, such as hypokalaemia and chronotropic effects that may be life-threatening in susceptible patients [68]. Intravenous RSV immunoglobulin has an unfavourable risk–benefit balance, particularly with the availability of monoclonal antibodies, while the use of corticosteroids is limited nowadays because of reported cases of adrenal suppression, especially in children [69,70]. Inhaled corticosteroids, which are commonly used in combination with long-acting β2-agonists to reduce exacerbation rate in worsening cases of COPD, have been associated with increased risk of pneumonia [71]. There has been an increasing rate of macrolide-resistant bacteria in the last few decades, making the use of drugs such as macrolides in combination with β-lactam agent ineffective for the treatment of community-acquired pneumonia [72]. Anti-TB drugs such as ethambutol, isoniazid, pyrazinamide, rifampin, and streptomycin have common side effects, which include cutaneous reactions, gastrointestinal intolerance, haematological reactions, and kidney failure [73]. Some FDA-approved anti-influenza drugs such as baloxavir marboxil, peramivir, oseltamivir phosphate and zanamivir, have proven ineffective in patients with serious influenza requiring hospitalization, and with common side effects such as bronchitis, common cold, diarrhoea, headache, and nausea [74]. Dexamethasone is a corticosteroid, anti-inflammatory and immunosuppressive drug that has been widely used in recent years for the management of COVID-19 patients who are in critical condition. However, the common side effects of this drug include acne, depression, dizziness, gastritis, headache, insomnia, restlessness, and vomiting [75]. Azithromycin is an antibiotic drug that received much attention for clinical use among patients with early-stage SARS-CoV-2 infection. However, some adverse reactions such as abdominal pain, anaphylaxis, diarrhoea, nausea, QT prolongation, Clostridium difficile infection and vomiting have been reported with azithromycin [75]. Thus, there is a need to exploit nature for its bioactive agents, which can be optimized for the chemotherapeutic treatment of the afore-mentioned RDs and many more with little or no side effect.
4. Plant-Derived Natural Products as Lead Agents against Common Respiratory Diseases
Natural products (NPs) are generally described as chemical substances produced by living organisms that are found in nature [18]. Natural product sources include plants, animals, lower and marine organisms, and minerals [76]. Plant-derived NPs are characterised by enormous chemical entities with structural complexities, which are optimized by evolution to serve specific biological functions [77]. These structurally diverse substances, also referred to as metabolites, especially secondary metabolites (terpenoids, alkaloids, flavonoids, coumarins, anthraquinones, saponins, phenolics and phenolic glycosides), produce physiological actions in man; thus, offering great therapeutic value [78].
Historically, they continue to play a key role in the therapeutic armoury of mankind against diseases. The earliest records of NPs were plant extracts such as oils from Cypress (Cupressus sempervirens) and Myrrh (Commiphora species), inscribed on clay tablets in cuneiforms from Mesopotamia (2600 B.C.), which are still used today ethnomedicinally to treat colds, coughs, and inflammation [78]. The Egyptian pharmaceutical record (Ebers Papyrus, 2900 B.C.) documented over 700 plant-based drugs in the forms of gargles, infusions, ointments and pills [79]. The Chinese Materia Medica (1100 B.C.) contained 52 prescriptions, the Shennong Herbal (~100 B.C.) enlisted 365 drugs, while the Tang Herbal (659 A.D.) contained 850 drugs, and all were documented records on the medicinal uses of NPs [79]. The Greek physician Dioscorides (100 A.D.) recorded the collection, storage and uses of medicinal herbs. Monasteries in England, Ireland, France and Germany preserved the Western knowledge of natural medicines during the Dark and Middle Ages, whilst the Arabs preserved the Greco-Roman knowledge and expanded the uses of their own resources, together with Chinese and Indian herbs [79]. Avicenna, a Persian pharmacist, physician, philosopher and poet, contributed much to the science of pharmacy and medicine in the 8th century through his work titled “Canon Medicinae” [79].
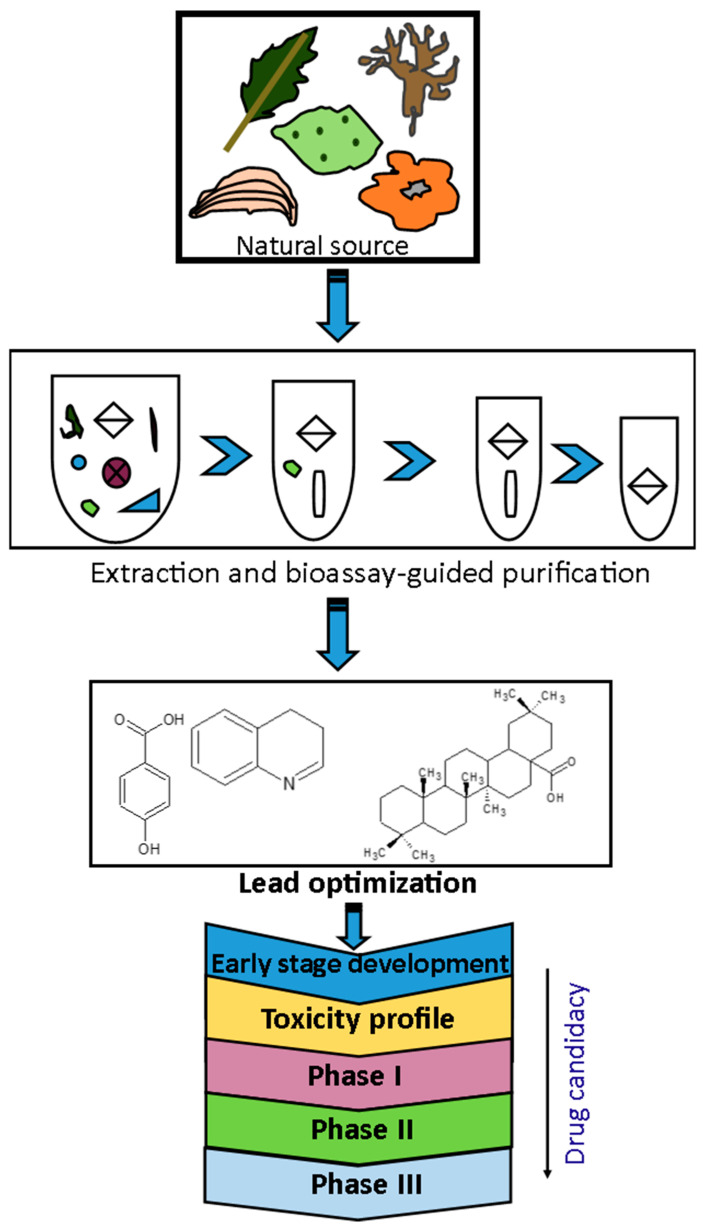
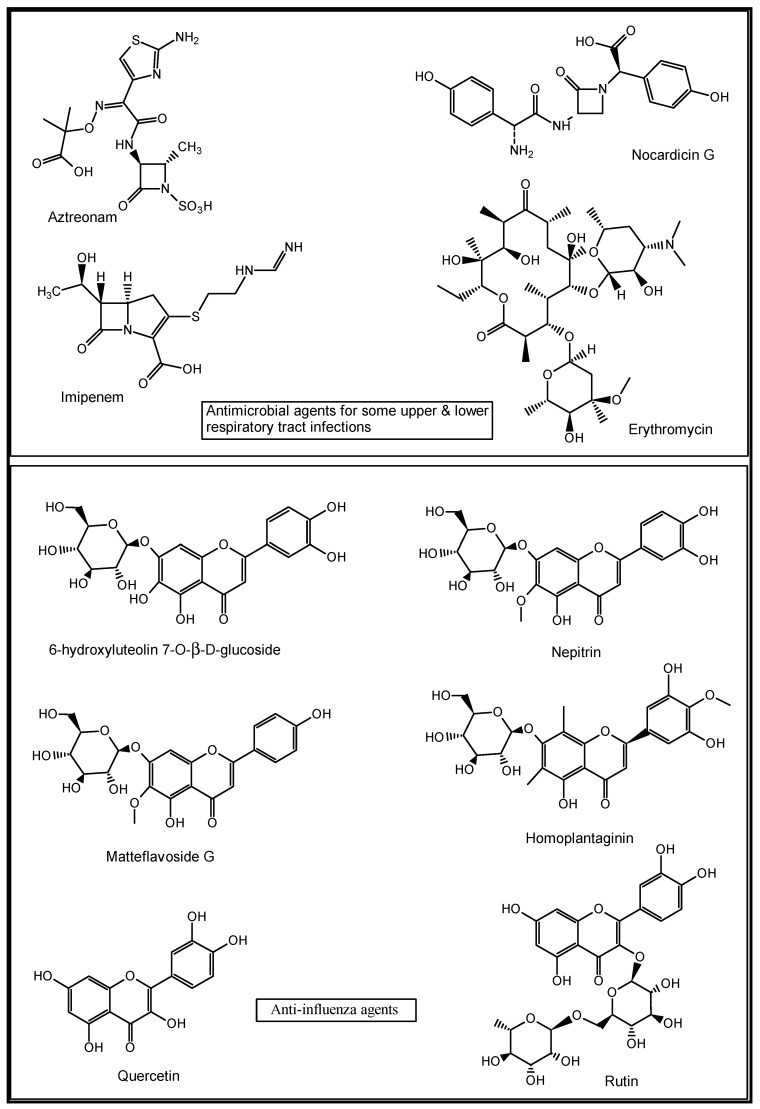
The early years of the 20th century witnessed remarkable drug discoveries from natural sources. The world’s first broadly effective antibiotic substance, penicillin, was first isolated from the fungus Penicillium notatum by Sir Alexander Fleming, a Scottish physician and microbiologist, in 1928 [80]. This discovery led to the re-isolation and in vivo and clinical studies by Fleming and co-workers in the early 1940s and commercialization of synthetic penicillins, which ultimately revolutionized drug discovery and won them the 1945 Nobel Prize in Physiology and Medicine [81]. After the first clinical report on penicillin G, there was global interest in exploiting many natural resources for new bioactive natural products. The post-Fleming era witnessed the isolation of some sulphur-containing secondary metabolites (natural antibiotics) such as aztreonam, nocardicin G and imipenem from marine organisms [78]. Erythromycin was discovered from Saccharopolyspora erythraea as an antibacterial drug with a 14-membered macrocycle composed entirely of propionate units, broadly active against Gram-positive cocci and bacilli, and is used for mild to moderate upper and lower respiratory tract infections [82]. A typical natural product drug discovery process is represented as a flow chart in Figure 4.
Figure 4.
Stages involved in the identification of new drugs from natural sources. Adapted with permission from Quan et al. [55] (Copyright 2016, Elsevier Publisher).
Plant-derived NPs continue to contribute significantly to the discovery of newer drugs. For example, the bark of Pacific yew plant, Taxus brevifolia, gave taxol, a cytotoxic compound that was latter developed as Paclitaxel for the treatment of human lung cancer and other malignant tumours [83]. Some antiviral flavonoids such as 6-hydroxyluteolin 7-_O_-β-d-glucoside, nepitrin and homoplantaginin were isolated from the methanol extract of Salvia plebeia. These compounds were found to be active against influenza virus H1N1A/PR/9/34 neuraminidase [84]. Matteflavoside G from the rhizomes of Onoclea struthiopteris showed significant inhibitory activity against the H1N1 influenza virus neuraminidase with an EC50 value of 6.8 ± 1.1 μM and an SI value of 34.4 [85]. Extracts of Humulus lupulus and five South African medicinal plants, namely Volkameria glabra, Cussonia spicata, Myrsine melanophloeos, Pittosporum viridiflorum and Tabernaemontana ventricose, are known in traditional medicine to manage inflammatory and respiratory diseases such as the influenza virus, with quercetin and rutin identified among their putative active constituents [86] (Figure 5).
Figure 5.
Structures of some natural anti-infective and anti-influenza agents [78,82,84,85,86].
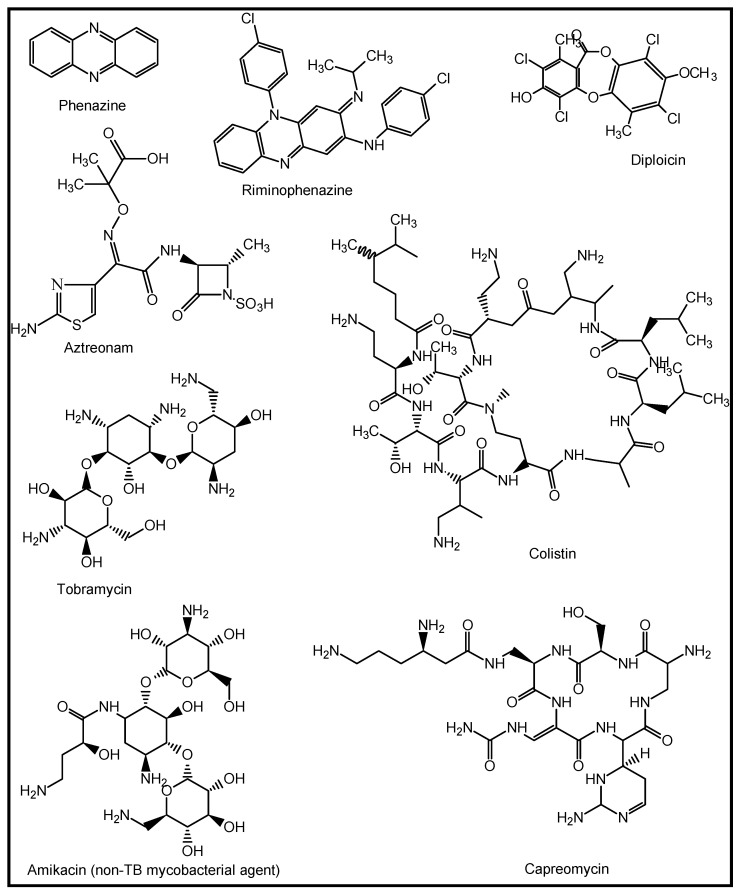
A review of high-throughput screening (HTS) by Novartis revealed that NPs were the most diverse compounds tested, with significantly higher hit rates compared to the compounds sourced from the synthetic and combinatorial libraries [87]. Some potential natural anti-TB agents include the antifungal phenazine and riminophenazine isolated from lichens. Clofazimine is a riminophenazine and TB drug originally discovered in 1954 through structural modifications of diploicin, extracted from Buellia canescens. It is currently used as a WHO group-five drug for multidrug resistant tuberculosis (MDR-TB) [88]. Natural products and NP-derived compounds, such as aztreonam, colistin, and tobramycin, have been developed for cystic fibrosis as inhalation drugs, while amikacin, arbekacin, and capreomycin are being developed for nontuberculous mycobacterial infection, bacterial pneumonia, and tuberculosis, respectively [89] (Figure 6).
Figure 6.
Structures of some nature-inspired agents against tubercular (TB) and non-TB mycobacterial infections [88,89].
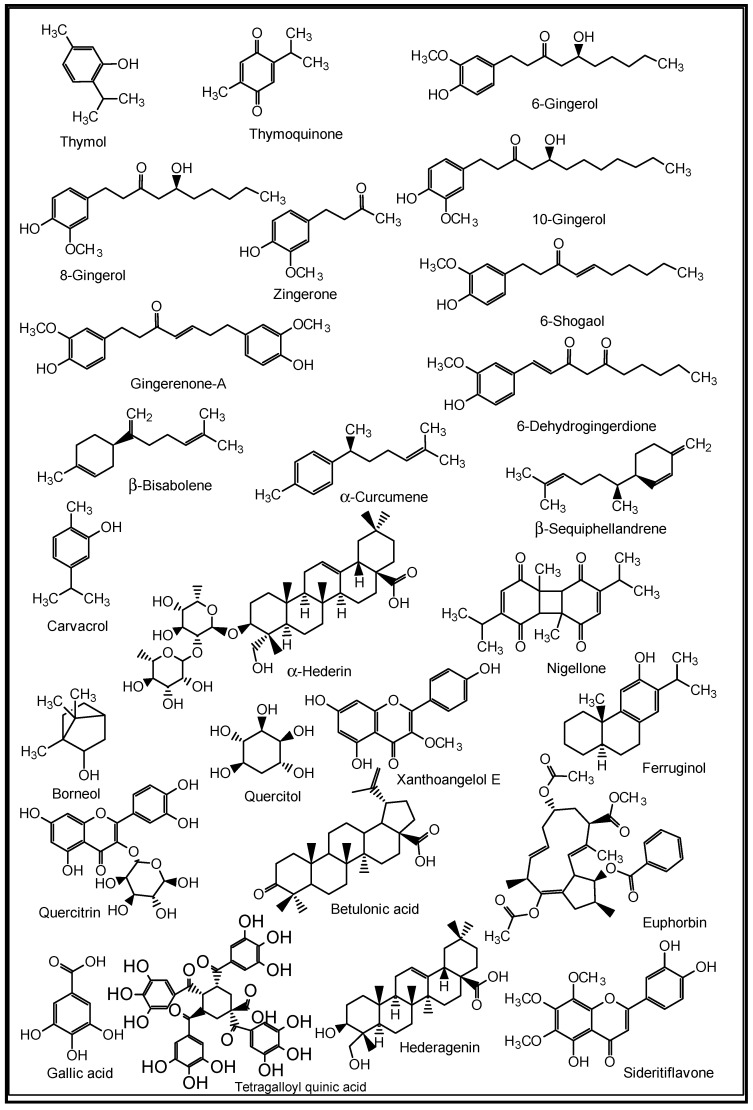
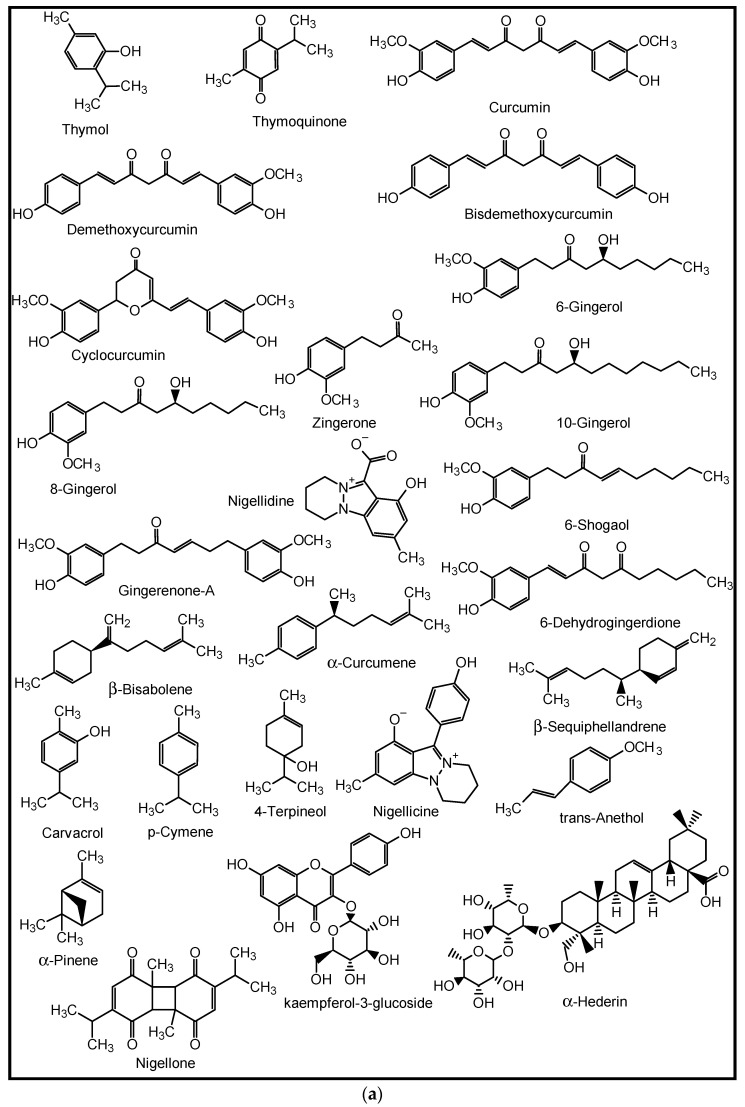
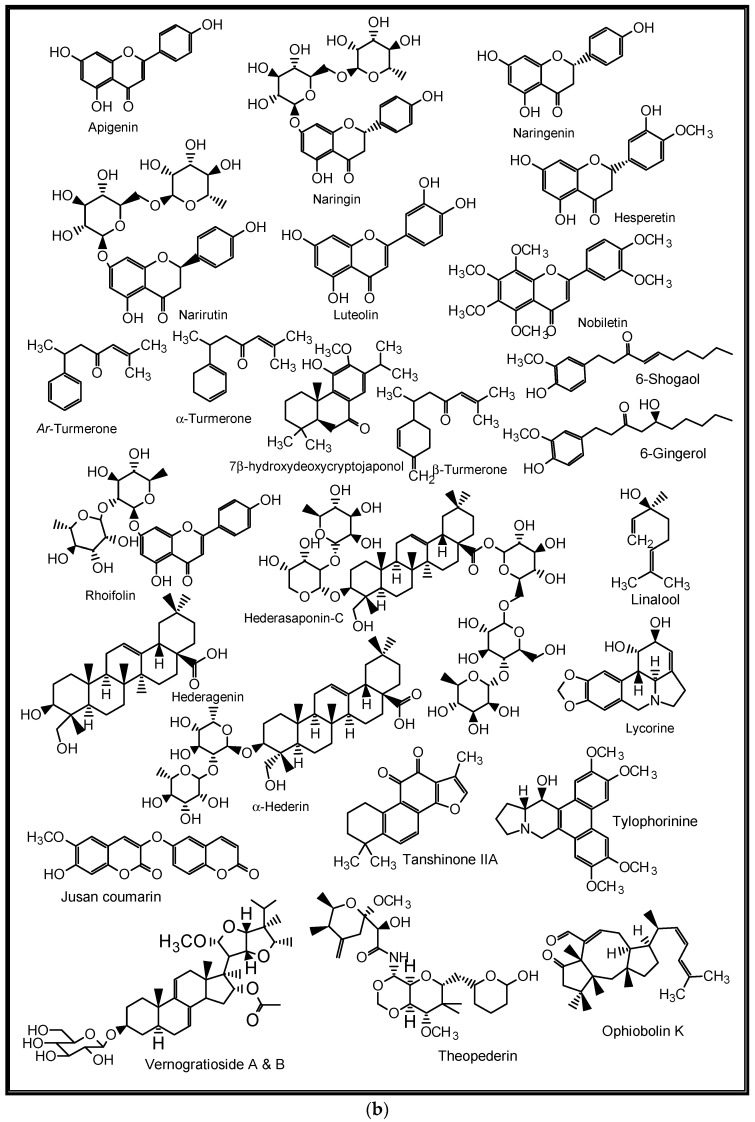
For decades, many herbs and spices have been known to be used in folkloric medicines for the management of respiratory diseases. Some of these medicinal spices and herbs are now well established in modern medicine as dietary supplements, nutraceuticals, and whole drugs because of their identified and well-defined bioactive agents [90]. The peel methanol extract of Opuntia ficus-indica, known as the prickly pear cactus, has been reported to contain some in vitro anti-pneumonia compounds such as astragalin, quercetin 5,4′-dimethyl ether, isorhamnetin-3-O-glucoside and isorhamnetin [91]. Curcumins from the turmeric rhizomes (Curcuma longa) are known anti-inflammatory, antiviral, immune modulating, anti-lung cancer and anti-SARS-CoV-2 agents, as well as inhibitors of acute and chronic respiratory disorders [92,93]. Gingerols, 6-shogaol, zingerone, gingerenone-A, 6-dehydrogingerdione, β-bisabolene, α-curcumene and β-sequiphellandrene, all from the bulbs of ginger (Zingiber officinale), are known bioactive agents against asthma, inflammation, lung cancer, acute and chronic respiratory disorders, and respiratory viruses including coronaviruses [94]. 6-Gingerol was reported to decrease the gene expression and production of MUC5AC, through affecting the ERK- and p38 MAPK signalling pathways, thus inhibiting pro-inflammatory actions of many pulmonary diseases [95]. Nigella sativa L. (black cumin seeds) contain bioactive agents such as nigelline, thymol, thymoquinone, nigellidine, nigellicine, carvacrol, p-cymene, 4-terpineol, trans-anethol, α-pinene, α-hederin, and kaempferol-3-glucoside [96]. The constituents improved antioxidant enzymes (catalase, glutathione peroxidase and glutathione-_S_-transferase), and exhibit anti-inflammatory, immune modulatory and broncho-dilatory effects against obstructive RDs [96]. The inhibitory effect of nigellone on the release of histamine from mast cells has been implicated for the management of bronchitis and asthma [97].
Additionally, some NPs such as the anti-influenza ginkgetin, 4′-_O_-methylochnaflavone, hinokiflavone from Ginkgo biloba; six cinnamic amide alkaloids from Tribulus terrestris with considerable in silico SARS-CoV PLpro activity; procyanidin B1, procyanidin A2 and cinnamtannin B1 from the dried bark (cortex) of Cinnamomum verum with in vitro anti-SARS-CoV activity; and resveratrol and pterostilbene from grapes (Vitis vinifera) interfered with the SARS-CoV-2 infection cycle and significantly inhibited COVID-19 infection in primary human bronchial epithelial cells cultured under air–liquid interface conditions [9]. Likewise, some triterpenoids such as oleanolic acid, betulinic acid, ursolic acid and saikasaponins A, C, D, B1, B2, B3, and B4, which have been isolated from some medicinal plants, are known to exhibit significant antioxidant, anti-inflammatory, cytotoxic, antibacterial, antiviral and immune modulatory activities in lung diseases such as COPD, bronchitis, lung cancer, influenza and coronaviruses [9,95,98,99,100,101]. Some medicinal plants and their active ingredients are presented in Table 2, while the structures of some of these bioactive compounds are shown in Figure 7, Figure 8, Figure 9, Figure 10 and Figure 11.
Table 2.
Some plant-derived natural products and their biological potentials against common respiratory diseases.
| Natural Source (Family) | Medicinal Use | Biological Property | Active Part/Ingredient | Reference |
|---|---|---|---|---|
| Aerva lanata (L.) A. L. Juss. ex Schultes. (Amaranthaceae) | Asthma, cough | Anti-asthmatic, antimicrobial, immunomodulatory, diuretic, anti-inflammatory | Aerial part ethanol extract | [102] |
| Ageratum conyzoides L. (Asteraceae) | Asthma | Antihistaminic,anticataleptic | Leaf hydroalcoholic extract | [103] |
| Allium sativum L. (Amaryllidaceae) | Asthma, pneumonia, influenza, COVID-19 | Antibacterial, antifungal, anti-inflammatory, immune modulating, antiviral (SARS-CoV-2), anticancer | Organosulfur compounds such as diallyl thiosulfinate (allicin) and diallyl polysulfane from the bulb | [104,105,106] |
| Amburana cearensis A.C. Smith (Fabaceae) | Asthma and other respiratory diseases | Anti-asthmatic | flavonoid-5,7,4′-trihydroxy-3-methoxyflavone (isokaempferide) from the trunk bark extract | [107] |
| Angelica keiskei (Miq.) Koidz. (Apiaceae) | COVID-19 | Antiviral, anti-SARS-CoV-2 | xanthoangelol E from the leaf extract | [108] |
| Argemone mexicana L. (Papaveraceae) | Asthma | Antiallergic, antistress | Stem aqueous extract | [109] |
| Asystasia gangetica (L.) T. Anderson (Acanthaceae) | Asthma | Anti-asthmatic, anti-inflammatory | Leaf fractions (hexane, ethyl acetate, methanol) | [110] |
| Cinnamon zeylanicum Blume (Lauraceae) | COPD, lung cancer, flu-related diseases such as influenza and coronaviruses | Antioxidant, anti-inflammatory, antimicrobial, fungitoxicant against respiratory tract mycoses (Candida sp.), antiviral, anticancer, immune modulatory | Cinnamaldehyde and trans-cinnamaldehyde, procyanidins, catechins, volatile oils from the bark | [111,112,113,114] |
| Cassia sophera (L.) Roxb. (Fabaceae) | Asthma, bronchitis (India) | Anti-asthmatic | Leaf fractions (Chloroform, ethyl acetate, methanol) | [115] |
| Chamaecyparis obtusa var. formosana Hayata (Siebold & Zucc.) Siebold & Zucc. ex Endl. (Cupressaceae) | COVID-19, SARS-CoV | Anti-SARS-CoV-2, cytotoxic | Ferruginol, betulonic acid, betulinic acid, savinin, from the heartwood extract | [108] |
| Citrus limon (L.) Burm. and Citrus peel and fruit (Rutaceae) | Bronchitis, Flu-related illnesses, COPD, lung cancer | Antioxidant, anti-inflammatory, immune modulatory, antibacterial, antiviral (rhinovirus, influenza virus, coronaviruses), anticancer | Flavonoids such as eriocitrin, hesperidin or diosmin, apigenin, naringin, naringenin, narirutin, quercetin, luteolin, hesperetin, nobiletin | [116,117,118,119,120,121] |
| Crinum glaucum A Chev. (Amaryllidaceae) | Asthma, cough, convulsion, oral thrush, COPD, lung | Antiallergic, antifungal (candidacidal), | Bulb aqueous extract | [122,123,124] |
| Cryptomeria japonica (Thunb. ex L.f.) D.Do. (Cupressaceae) | COVID-19 | Antiviral, anti-SARS-CoV-2 | 7β-hydroxydeoxy- cryptojaponol from the heartwood extract | [108] |
| Curcuma longa L. (Zingiberaceae) | Common cold, COVID-19, pneumonia, influenza, bronchial asthma, COPD, lung cancer | Antiviral, anti-SARS-CoV infections, cytotoxic, anti-influenza virus, immune modulating, anti-inflammatory | Curcumins and turmerones from the rhizomes (roots) | [92,93,125,126,127,128,129,130] |
| Euphorbia hirta Linn. (Euphorbiaceae) | Asthma, bronchitis, hay fever, oral thrush | Antihistaminic, antiallergic, anti-anaphylactic, antibacterial, antifungal, anti-inflammatory | Quercitrin, rutin, borneol, quercitol, euphorbin, gallic acid from the aerial part ethanolic extract | [131,132] |
| Ficus deltoidea Jack (Moraceae) | Flu including COVID-19 | Antiviral (coronaviruses) | Rhoifolin from the leaf extract | [108] |
| Hedera helix L. (Araliaceae) | COPD, COVID-19, bronchial asthma, bronchitis | Anti-inflammatory, expectorate, antiviral | Hederasaponin-C, hederagenin and α-hederin from the leaf extract | [133] |
| Lycoris radiata (L′Héritier) Herbert (Amaryllidaceae) | Flu such as SARS-CoV infections, COVID-19 | Antiviral, anti-SARS-CoV, anti-SARS-CoV-2 | Lycorine from the stem cortex extract | [134] |
| Mentha spicata L. (Lamiaceae) | Asthma (Japan) | Antihistaminic | Sideritiflavone from the leaf methanol extract | [135] |
| Momordica dioica Roxb. ex. Willd (Cucurbitaceae) | Asthma, bronchitis (India) | Antihistaminic | Pulp methanol and aqueous extracts | [136] |
| Myrica esculenta Buch. (Myricaceae) | Asthma, bronchitis (India) | Antiallergic, anti-inflammatory, bronchodilator, anti-anaphylactic | Aerial part and stem bark ethanol extracts | [137] |
| Nigella sativa L. (Ranunculaceae) | Bronchitis, COPD, pneumonia, flu, lung cancer | Antioxidant, immune modulatory, anti-inflammatory, preventive effect in respiratory disorders, broncho-dilatory, cytotoxic | Thymoquinone, nigellone, thymol, carvacrol, p-cymene, 4-terpineol, trans-anethole, α-pinene, α-hederin, kaempferol glucoside | [96,138] |
| Panax ginseng C. A. Meyer (Araliaceae) | Oral thrush, acute respiratory illness (pharyngitis, bronchitis, COPD, respiratory tract infections | Antifungal (candidacidal), anti-inflammatory, antibacterial, antiviral (rhinovirus, respiratory syncytial virus, coronaviruses), | Ginsenosides such as 20(S)-protopanaxatriol and 20(S)-protopanaxadiol from the root extract | [139,140,141] |
| Piper betel Linn. | Asthma, cold, cough (Asia and Africa) | Anti-asthmatic | Leaf ethanol and aqueous extracts | [142] |
| Polyherbal formulations containing some medicinal herbs and spices | Different respiratory diseases including asthma | Anti-asthmatic, mast cell stabilization, anti-inflammatory, anti-spasmodic, antiallergic, anti-anaphylactic, immunomodulatory and inhibition of mediators such as leukotrienes, histamine, cytokines | Polyherbal mixture | [143] |
| Terminalia chebula Retz. | Respiratory syncytial virus | Broad spectrum Antiviral | Chebulagic acid, punicalagin | [144] |
| Rheum palmatum L. (Polygonaceae) | COVID-19 disease | SARS-CoV-2 inhibition | Chloroform fraction from ethyl acetate and 75% ethanolic extract | [145] |
| Salvia miltiorrhiza Bge (Lamiaceae) | COPD | Antioxidant, anti-inflammatory | Tanshinone IIA from the root extract | [146] |
| Thymus vulgaris L. (Lamiaceae) | Pertussis, bronchitis, asthma, acute lung injury, influenza, COVID-19 | Antioxidant, antimicrobial, anti-inflammatory, antiviral (influenza, coronaviruses) | Thymol, p-cymene, linalool, carvacrol from the leaf infusion | [147,148,149,150] |
| Tylophora indica (Burm. f.) Merr. (Apocynaceae) | Coronavirus infections | Anti-SARS-CoV | Tylophorinine | [151] |
| Zingiber officinale Roscoe (Zingiberaceae) | Asthma, COPD, common cold, bronchitis, influenza, coronaviruses, lung cancer | Antioxidant, anti-inflammatory, antiviral (SARS-CoV), immune modulatory, cytotoxic | 6-Gingerol, 8-gingerol, 10-gingerol and 6-shogaol from the bulbs | [94,152] |
Figure 7.
Some plant-derived anti-asthmatic compounds.
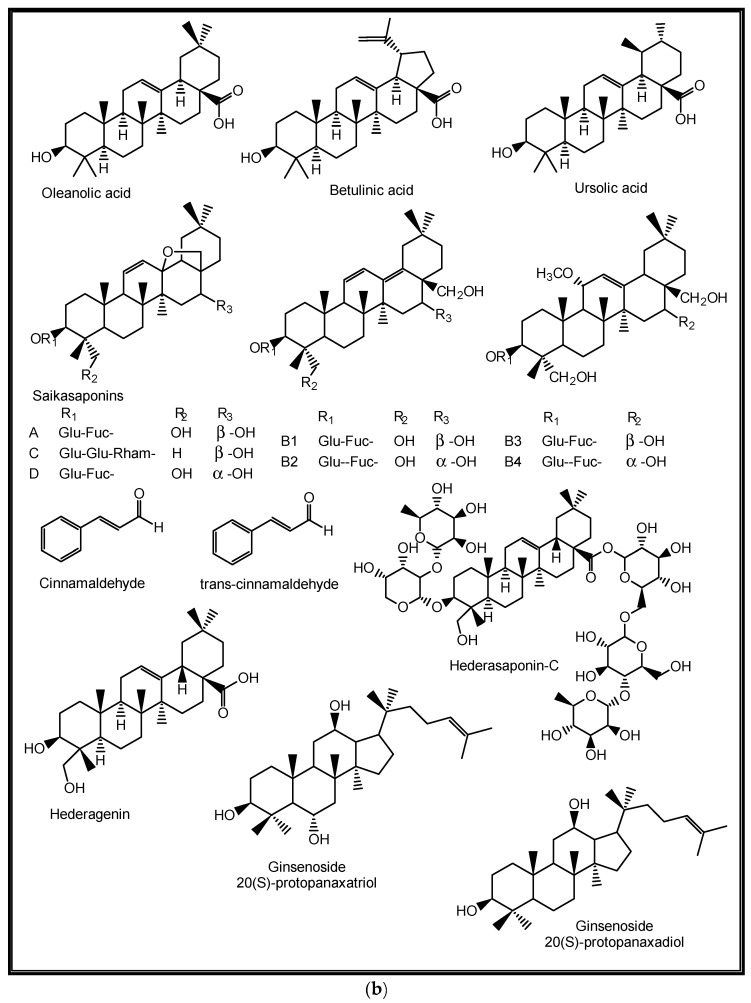
Figure 8.
(a,b) Some plant-derived anti-infective (COPD) compounds.
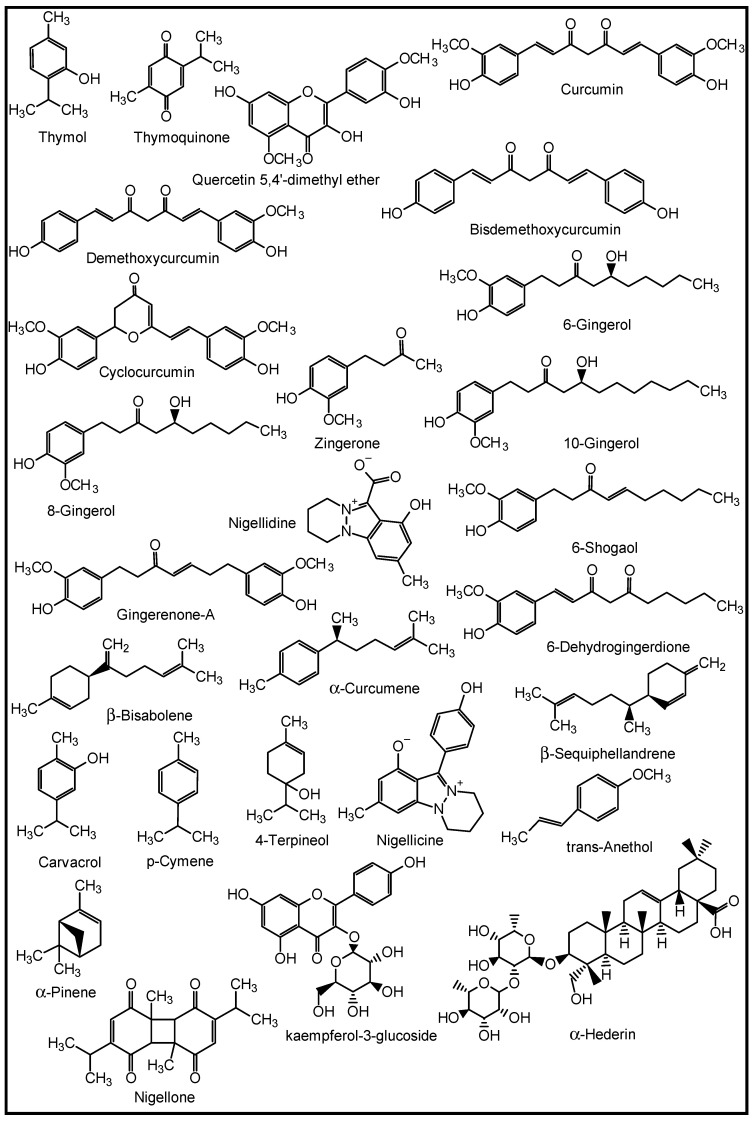
Figure 9.
Some plant-derived anti-pneumonia compounds.
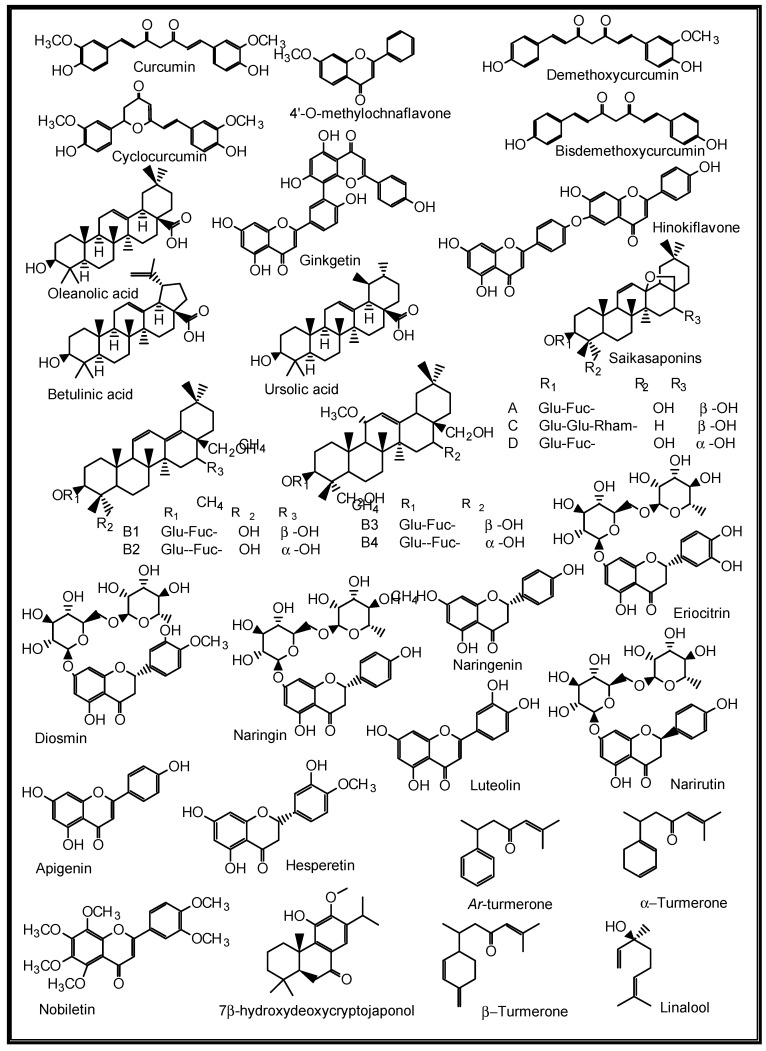
Figure 10.
Some plant-derived anti-influenza compounds.
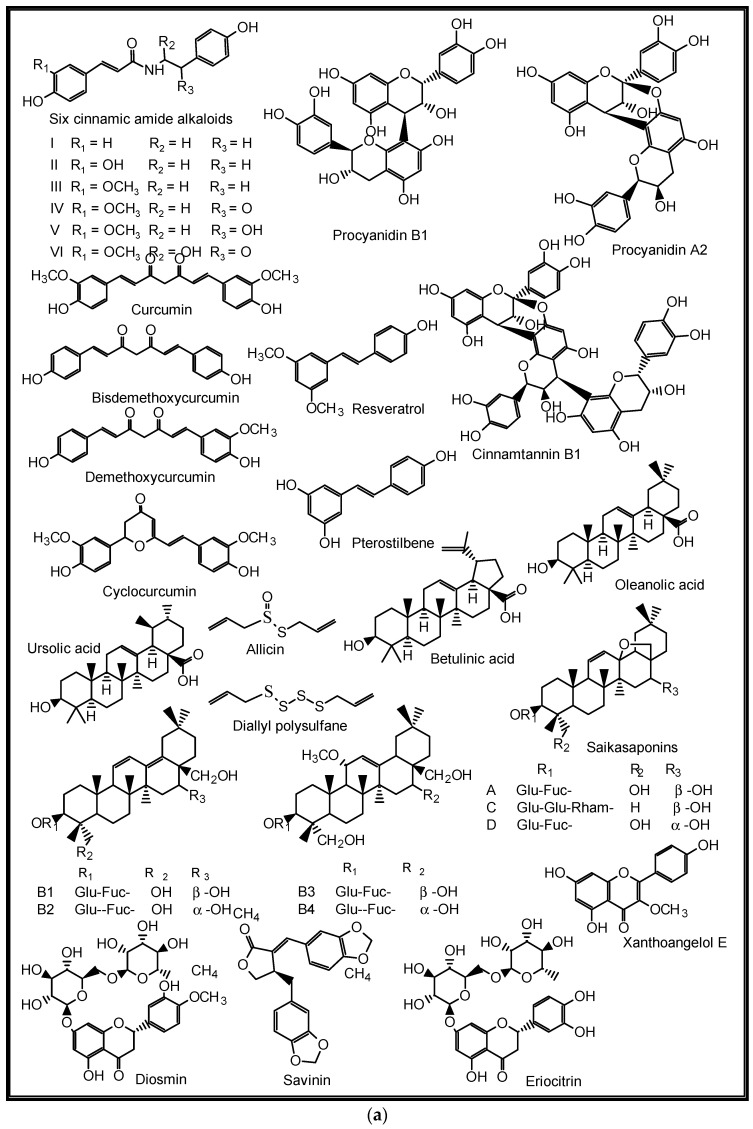
Figure 11.
(a,b) Some plant-derived anti-SARS-CoV-2 compounds.
5. Structure–Activity Relationships of Some Promising Natural Products against Common Respiratory Diseases
The study of the structure–activity relationships (SARs) is an approach designed to find the relationships between chemical structures of ligands and biological targets of studied compounds [153]. It has become increasingly essential as a tool for organizing, mining, and interpreting data, to guide further investigation for drug discovery [154]. It is also a strategy to increase the value of the activity initially detected [155]. Natural products contain steric and electronic features in their bioactive sites (pharmacophores), which are responsible for the optimal supramolecular interactions with specific biologic targets and to trigger (or block) their biologic responses. The most used features for describing pharmacophore sites are hydrogen bond acceptors and donors, acidic and basic functional groups, aliphatic and lipophilic moieties, aromatic- and hydroxyl-hydrophilic moieties amongst others [156].
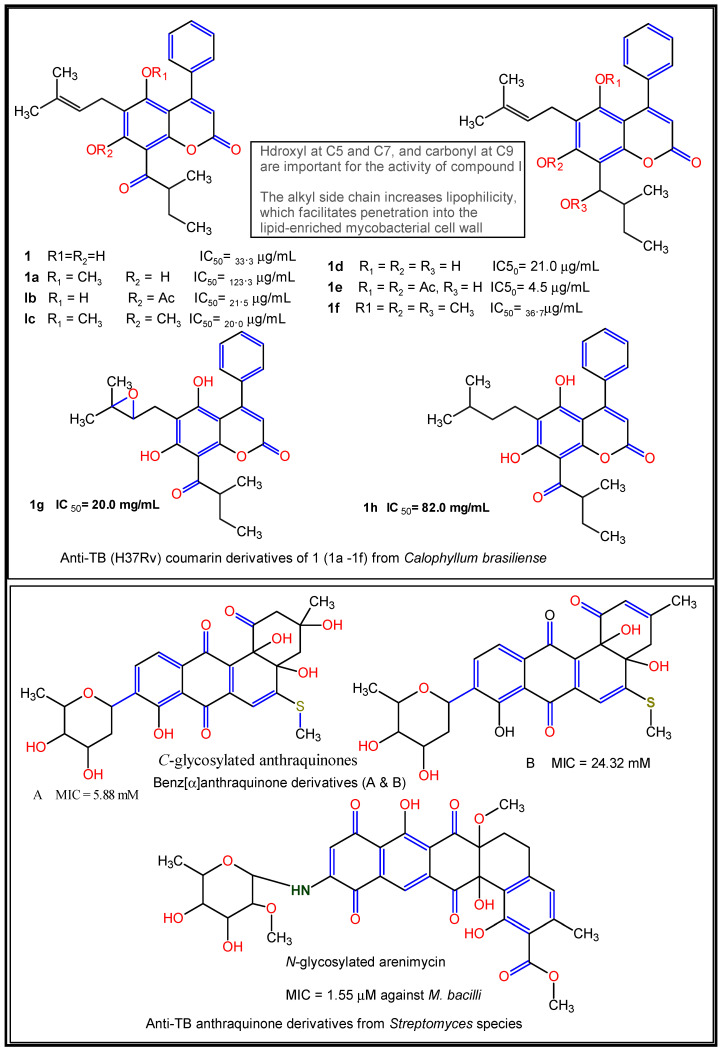
Reports have shown the SARs of some natural products implicated against some common respiratory diseases (Table 3). Pires et al. [157] reported the influence of methyl-, hydroxyl-, and carbonyl functional groups on the in vitro anti-TB activities of eight coumarin derivatives from Calophyllum brasiliense, with MIC ranging from 15.6–62.5 μg/mL and a cytotoxicity range of 4.5–82.0 μg/mL against Mycobacterium tuberculosis H37Rv and its multidrug-resistant clinical isolates. Here, the carbonyl and hydroxyl groups enhance anti-M. tuberculosis activity by the inhibition of acid-fastness formation in the mycobacterial cell wall, while the presence of lipophilic side chains such as the alkyl substituent at the C-3 position and the presence of double bonds increase the lipophilicity of the compound, thus, helping it to penetrate the lipid-enriched mycobacterial cell wall [157] (Figure 12).
Table 3.
Structure–activity relationships of some natural products against common respiratory diseases.
| Compound | Source | Bioactivity | SAR | Reference |
|---|---|---|---|---|
| 4-Deoxybostrycin | Alternaria eichhorniae 5 (isolate Ae5) | In vitro anti-mycobacterial (TB) activity (IC50 of 12.5 µM), better inhibitory effect on clinical multidrug-resistant M. tuberculosis (K2903531 and 0907961) than (Nigrosporin, the standard antitubercular drug | Hydroxyl group at C-5 enhances binding effect between the bacteria active site and the moleculemethyl at C-7 increases lipophilicity and transport across bacterial cell membrane | [159] |
| Cleistrioside-2 | Cleistopholis patens (Benth.) Engl. & DielsC. glauca Pierre ex Engl. & Diels | Cytotoxicty against the human lung cancer cell lines (NCI-H460) at CC50 = 9.1 µM.Antibacterial activity against Streptococcus pneumonia at MIC = 4 µM | C-3 glycosylation and C-4 acetate group on the terminal sugar | [161] |
| Ginsenosides | Panax ginseng C. A. Meyer | Antioxidant, immune-modulatory, and antiviral properties | Presence of an aglycon, protopanaxadiol, and a part of the sugars may contribute to the immune-modulatory properties of the herbs | [162] |
| Hydroquinone | Albizia coriaria Welw ex. Oliver | In silico anti-TB activity. Better binding affinities (−7.8 kcal/mol) for the mycobacterial ATPase and polyketide synthase-13 than isoniazid and rifampicin | Interactions of the co-crystalized ligand with amino acid residues in the binding site of ATP synthase | [163] |
| Liquiritin apioside | Glycyrrhiza glabra L.Paeonia lactiflora Pall. | Chronic obstructive pulmonary disorder (COPD) | Presence of hydroxyl group at C-5 and C-7 of ring A promotes enzymatic oxidation and consequently bonding of flavonoids with biomacromolecules | [164] |
| Jusan coumarin(Dicoumarin) | Artemisia glauca Pall. ex Willd | In silico anti-SARS-CoV-2 activity | Presence of pharmacophoric features such as two H-bond donors, one H-bond acceptor, an aromatic ring and two hydrophobic centres | [165] |
| Ophiobolin K | Emericella variecolor IFM42010 | Anti-tubercular activity. | Configuration of C-6 is key for optimal activity | [159] |
| Theopederin | Theonella species such as Theonella swinhoei Gray | In vitro antiviral activity against SARS-CoV-2) | Inhibition of SARS-CoV-2 main protease aided by terminal guanidine, cyclic hemiacetal linkage, and the length of the side chain | [166] |
| Quercetin | Many higher plants including Polygoni avicularis Herba | Anti-inflammatory effects against lung diseases such as asthma, allergy, and acute respiratory diseases, and chronic respiratory disorder (COPD) | The presence of ketonic carbonyl and double bond at C-2/C-3 of ring C induces coplanarity between rings A and C, favouring the interaction of the flavonoid with the enzymatic site receptor. Hydroxyl group at C-5/C-7 of ring A as well as at the C-3′ and C-4′ of ring B favours enzymatic and consequently bonding of flavonoids with biomacromolecules | [160,167] |
| Quercetin 5,4′-dimethyl ether | Opuntia ficus-indica (L.) Miller | Higher in vitro anti-pneumonia than Imipenem.In silico quorum sensing efficacy | π–π interaction involving flavone A- and C-rings,π–alkyl interactions involving A-, B- and C-rings | [91] |
| Vernogratioside A & B | Vernonia gratiosa Hance | In silico anti-SARS-CoV-2 main protease with comparable −7.2 and −7.6 kcal/mol binding affinity to N3 inhibitor (−7.5kcal/mol) | C-3 glycosylationand presence of alkyl substituent | [168] |
| Wollamide B | Streptomyces nov. sp. (MST-115088) | In vitro anti-tubercular activity | The presence of the basic amino acid ornithine and clusters of lipophilic amino acids impart the typical cationicity and amphiphilicity to the molecule | [158] |
Figure 12.
Structure–activity relationships of some natural product-derived anti-TB compounds. Active moieties indicated in coloured forms [157,159].
Quercetin 5,4′-dimethyl ether isolated from the fruit peel methanol extract of Opuntia ficus-indica has been reported to demonstrate double-fold in vitro anti-pneumonia activities, with MIC values of 0.49 and 0.98 µM against Klebsiella pneumonia and Moraxella catarrhalis, respectively, when compared to Imipenem, a standard anti-pneumonia drug [91]. Furthermore, an in silico molecular docking study of the compound revealed high H-bonding affinity with key amino acids such as threonine, asparagine, and tyrosine, thus suggesting it to be a natural quorum-sensing inhibitor, which is a key anti-pneumonia property [94]. Wollamide B isolated from Streptomyces nov. sp. (MST-115088) has been reported to show considerable in vitro anti-TB activity with an IC50 value of 3.1 μM against Mycobacterium bovis. The presence of the basic amino acid ornithine and clusters of lipophilic amino acids was shown to significantly contribute the typical cationicity and amphiphilicity to the molecule [158].
The presence of _C_- and _N_-glycosylation has also been reported to enhance in vitro anti-TB activity. For instance, the _C_-glycosylated benz[α]anthraquinone derivatives and an _N_-glycosylated arenimycin isolated from Streptomyces species and Salinispora arenicola, respectively, showed strong activity against Mycobacterium tuberculosis within an MIC range of 5.88–24.32 µM, while the latter molecule exhibited an MIC value of 1.5 µM [159] (Figure 12). It is also noteworthy that unsaturation in the C ring (∆2), the number and position of hydroxyl groups at the A and B rings, and the carbonyl group at C-4 of ring C for natural flavonoids are reported to contribute considerably to their anti-inflammatory properties in some common lung diseases [160].
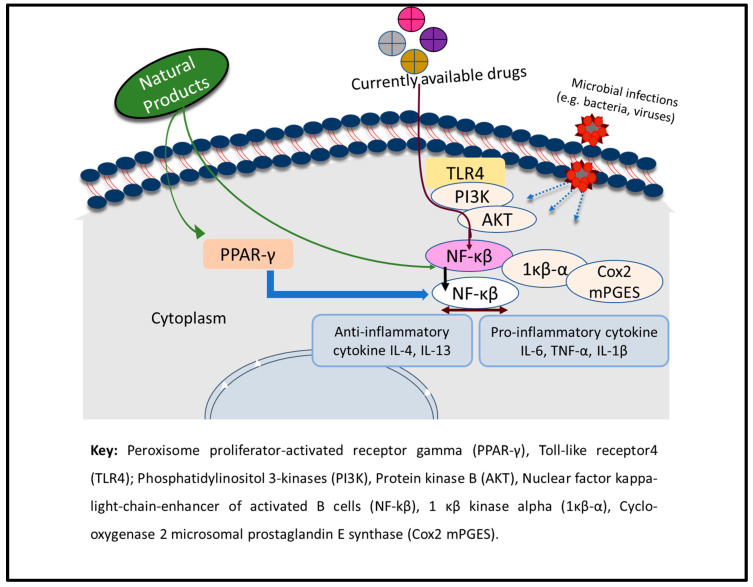
6. Mechanisms of Action of Some Plant-Derived Lead Compounds against Common Respiratory Diseases
Often, the human respiratory tracts become liable to inflammation upon microbial (especially bacterial and viral) infection and physical injury [169]. Respiratory inflammation is a hallmark of many respiratory diseases, which include asthma, COPD, and acute respiratory disorders (ARDs) [170]. During the inflammation process, inflammatory cells, which include eosinophils, lymphocytes, and macrophages, are activated to serve as the sources of different inflammatory mediators such as histamine, interleukins (IL-4, IL-1β, IL-6, and IL-5), leukotriene, prostaglandins, nitric oxide, and tumour necrosis factor (TNF-α) [171]. The release of these inflammatory mediators causes several abnormalities in the lungs and their function [170,171]. Therefore, natural products (NPs) that can target the epithelial–mesenchymal transition (EMT), oxidative stress, fibroblast activation, inflammatory injury, metabolic regulation, and extracellular matrix accumulation within the respiratory tracts are regarded as candidate anti-inflammatory agents that can be optimized as leads for new respiratory drugs [172]. The basic mechanism of action of the chemical agents involves regulating redox status, inhibiting the activities of bacteria and viruses, regulating the protease/anti-protease balance, blocking the NF-κB and MAPK signalling pathways, inhibiting the production of cytokines, suppressing the activation and migration of inflammatory cells, inhibiting the synthesis and activation of adhesion factors and growth factors, controlling the cAMP-PKA and PI3K/Akt signalling pathways, and increasing TIMP-1 expression to serve as anti-inflammatory agents in the lungs [171,173] (Figure 13).
Figure 13.
Mechanism of action of natural products during inflammation-induced respiratory illness. Adapted with permission from Timalsina et al. [171] (Copyright 2021, Hindawi).
The anti-inflammatory properties of curcumins against lung inflammation induced Klebsiella pneumonia has been demonstrated in a mouse model experiment [174]. Here, it was shown that curcumin ameliorates lung inflammation considerably by decreasing the bacterial load in the lung tissue and inducing a significant decrease in neutrophil influx into the lungs as well as in the production of MDA, NO, and MPO activity and TNF-alpha levels, whereas Augmentin, the standard antibiotic, takes care of bacterial proliferation. The study, however, highlighted the potential usefulness of curcumin as an adjunct therapy along with some antibiotics as an anti-inflammatory or an immunomodulatory agent in the case of acute lung infection [174]. Studies have also shown the significant anti-inflammatory actions of quercetin, which are believed to be mediated through the inhibition of phospholipase A2 (via arachidonic acid), lipoxygenase, cyclooxygenase, and thromboxane enzymes and through the modulation of iNOS, thereby inhibiting NO production [175,176].
Some alkylated chalcones such as xanthoangelol A-G, isolated from Angelica keiskei leaves, have been reported to show considerable in vitro and in silico anti-SARS-CoV activity. Xanthoangelol D particularly inhibited the SARS-CoV cysteine proteases with an IC50 of 1.2 µM, by both competitive and non-competitive modes, thus suggesting the molecule to be a candidate protease inhibitor in SARS-CoV-related infections [177]. Similarly, some natural phenolic compounds such as brazilin, theaflavin-3,3′-digallate and curcumin have been reported to have remarkable in vitro anti-SARS-CoV-2 activity with an IC50 ≥ 10 µM, among 56 polyphenolic compounds and plant extracts that were tested. The compounds were said to bind with the receptor-binding domain of SARS-CoV-2 spike protein, thus significantly inhibiting viral attachment to the human angiotensin-converting enzyme 2 receptor and cellular entry of pseudo-typed SARS-CoV-2 virions [178].
Tetragalloyl quinic acid isolated from Galphimia glauca has been reported as an in vivo anti-asthmatic agent at 5 mg/kg orally, by suppressing allergen- and platelet-activating factor, PAF-induced bronchial obstruction, PAF-induced bronchial hyperreactivity, and thromboxane biosynthesis in vitro. Androsin from Picrorhiza kurroa also demonstrated similar in vivo activity at 10 mg/kg orally (0.5 mg inhalative) by preventing allergen- and PAF-induced bronchial obstruction [179].
Additionally, ganoderic acid C1 in the ASHMITM herbal formula comprising Ganoderma lucidum Sophora flavescens and Glycyrrhiza uralensis has been reported to have potential for treating TNF-α mediated inflammation in asthma and other inflammatory diseases [180]. Based on clinical studies, the herbal formula significantly reduced TNF-α production by murine macrophages (RAW 264.7 cells) and peripheral blood mononuclear cells (PBMCs) from asthma patients [180,181]. The inhibition was associated with down-regulation of NF-κB expression and partial suppression of MAPK and AP-1 signalling pathways [181].
The combination of synephrine and stachydrine, both alkaloids from the dried rind of ripe Citrus reticulata Blancon fruits, has been reported to show significant spasmolytic effects on acetylcholine chloride (ACh)-induced contractions in isolated guinea pig trachea by activating β-2 adrenergic receptor signalling [182]. They also showed synergistic protection against histamine-induced experimental asthma by prolonging the latent period. Stachydrine acts as the antitussive component and is capable of significantly reducing citric acid-induced coughing; thus, the broncho-dilatory and antitussive effects of the combined alkaloids might explain their use in traditional Chinese medicine as an anti-asthmatic remedy [182]. The mechanisms of action of some plant-derived compounds implicated against some common respiratory diseases are shown in Table 4.
Table 4.
Mechanisms of action of some plant-derived lead compounds against some common respiratory diseases.
| Natural Products | Source | Mode of Action/Biological Effect | References |
|---|---|---|---|
| 1,8-Cineol | Eucalyptus globulus ssp. globulus Labill. | Inhibits nuclear translocation of NF-κB p65 and NF-κB-dependent transcriptional activity. Anti-asthmatic properties | [183,184] |
| 3-Methoxycatalposide | Platylobium rotundum I.Thomps. | Inhibits the expression of cyclooxygenase (COX)-2, nitric oxide synthase (iNOS), and proinflammatory genes (IL-6, IL-1β, and TNF-α). Anti-asthmatic properties | [184] |
| 3-O-α-L-rhamnopyranosyl-(1→2)-β-D-xylopyranosyl-(1→2)-β-D-xylopyranosyl-21-cinnamoyloxyoleanolic acid | Burkea africana Hook | Inhibition of the viral surface protein neuraminidase. In vitro anti-influenza virus activity, IC50 = 0.05 µM | [185] |
| 3-O-α-L-rhamnopyranosyl-(1→2)-β-D-xylopyranosyl-(1→2)-[α-l-rhamnopyranosyl-(1→4)]-β-D-xylopyranosyl-21-cinnamoyloxyoleanolic acid | Burkea africana Hook | inhibition of the viral surface protein neuraminidase. In vitro anti-influenza virus activity, IC50 = 0.17 µM | [185] |
| 4-(α-L-rhamnopyranosyloxy) benzyl isothiocyanate | Moringa oleifera Lam. | Inhibits inflammatory responses such as eosinophils, macrophages, dendritic cells, T-helper type 2 (Th2) cells, IgE-secreting B cells and mast cells accumulation. Anti-asthmatic activity. EC50 ≤ 50 mM in histamine and acetylcholine-exposed guinea pig ileum | [186] |
| 4-(β-D-glucopyranosyl-1→4-α-L-rhamnopyranosyloxy)-benzyl thiocarboxamide | Moringa oleifera Lam. | Inhibits inflammatory responses such as eosinophils, macrophages, dendritic cells, T-helper type 2 (Th2) cells, IgE-secreting B cells and mast cells accumulation. Anti-asthmatic activity. EC50 ≤100 mM in histamine and acetylcholine-exposed guinea pig ileum | [186] |
| Caffeic acid | Echinacea purpurea (L.) Moench | Inhibits in vitro SARS-CoV helicase activity, IC50 = 0.1 μM | [187] |
| Chlorogenic acid | Echinacea purpurea (L.) Moench | Inhibits angiotensin converting enzyme (ACE), IC50 = 0.1 μM. In vitro anti-SARS-CoV | [187] |
| Cleistanthin A | Cleistanthus collinus (Roxb.) Benth. ex Hook. f. | Inhibits the endocytic machinery, that is, by inhibiting V-type ATPase and elevating endolysosomal pH (EC of 0.1 μM). Anti-SARS-CoV | [188,189] |
| Cleistanthoside A tetraacetate | Phyllanthus taxodiifolius Beille | Neutralizes endolysosomal acidity and decreases the activity of V-type ATPase with an EC50 of 50 nM. Anti-SARS-CoV activity | [188] |
| Cryptotanshinone | Salvia miltiorrhiza Bunge | Inhibition of the in vitro SARS-CoV PLpro, IC50 = 0.8 μM | [190] |
| Curcumin | Curcuma longa L. | Inhibits SARS-CoV PLpro, IC50 = 5.7 μM, in vitroAmeliorates pneumonia-induced lung injury through a reduction of the activity and infiltration of neutrophils and the inhibition of inflammatory response in pre-clinical pneumonia models. Inhibits the production of MDA, NO, MPO activity and TNF-alpha levels. Prevents lung infections | [174,191,192] |
| (+)-Hopeaphenol | Ampelopsis brevipedunculata var. hancei (Planch.) Rehder & Li. | Inhibition of the SARS-CoV helicase activity, IC50 = 1.6 μM | [193] |
| Matteflavoside G | Matteuccia struthiopteris (L.) Tod | Inhibits H1N1 influenza virus neuraminidase with an EC50 of 6.8 μM and an SI value of 34.4 | [9] |
| Methyl galbanate | Ferula assa-foetida L. | Inhibits H1N1 influenza virus with an in vitro IC50 of 0.26 μM and significant in vitro cytotoxicity against human liver and lungs cancer cells | [194] |
| Scutellarein | Scutellaria baicalensis Georgi | Inhibition of the SARS-CoV helicase activity, IC50 of 0.86 μM | [195] |
| Silvestrol | Aglaia odorata Lour. | Inhibits the replication of MERS-CoV with an EC50 of 1.3 nM. acting as an inhibitor of RNA helicase eIF4A and protein expression via blocking replication/transcription complex formation | [196] |
| Tetra-O-galloyl-D-glucose | Rhus chinensis Mill. | Inhibition of the SARS-CoV S protein-ACE2 interaction, IC50 = 10.6 μM | [197] |
| (+)-Vitisin A | Ampelopsis brevipedunculata var. hancei (Planch.) Rehder & Li. | Inhibitory action against angiotensin converting enzyme (ACE), IC50 = 1.5 μM | [193] |
| Xanthoangelol E | Angelica keiskei (Miq.) Koidz | Inhibition of the SARS-CoV PLpro activity, IC50 = 1.2 μM | [177] |
7. Conclusions and Future Prospects
Medicinal plants and other natural sources continue to provide man with scaffolds of chemically unique and biologically active agents as drug candidates against common respiratory diseases (RDs) [193]. These lead agents include colchicine, curcumin, turmerones, gingerols, forsythiaside A, glycyrrhizin, mangiferin, zingerone and many other plant-derived NPs that have been mentioned in this review [193]. However, despite their promising biological activities, extensive clinical and toxicological reports that validate their clinical efficacy and safety are still lacking.
Therefore, future study should focus on the isolation and identification of non-/less toxic and more effective natural compounds through bioassay-guided isolation, high-throughput-screenings, metabolomics, molecular modelling, virtual screening, natural product libraries, and database mining [198], while elucidation of the mechanisms of action of bioactive compounds, lead optimization, toxicological considerations, product formulation, evaluation of pharmacokinetic parameters, dosage regimens, and targeted drug delivery will remain crucial in the discovery and development of respiratory drugs [77,199]. The development of new-age technologies such as the application of biogenetic metal-based nanoparticles in medicine (nanomedicine) is another giant stride, which so far has ensured successful drug delivery with the use of nebulizers that create a particle size capable of reaching the alveoli, for faster and more effective treatment at low therapeutic doses [200,201].
Perhaps the next generation of lead compounds that would effectively manage many of the respiratory problems of mankind lies under our very nose, demanding more intensive scientific investigations. “Respiratory disease on the rise, natural products to the rescue”.
Acknowledgments
The corresponding author is thankful to the Drug Research and Production Unit, Faculty of Pharmacy, Obafemi Awolowo University, Ile-Ife, Nigeria, for study leave permission to WSU.
Author Contributions
A.O.O. (Ayodeji Oluwabunmi Oriola): conceptualised and wrote the original manuscript draft; A.O.O. (Adebola Omowunmi Oyedeji): provided resources, supervised and reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
The authors thank the Directorate of Research Development and Innovation, Walter Sisulu University (WSU) for funding the APC.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Campbell N.A. 1993 Biology. 3rd Edition, Benjamin/Cummings, Francis Group, Redwood City-References-Scientific Research Publishing. [(accessed on 22 January 2022)]. Available online: https://www.scirp.org/(S(i43dyn45teexjx455qlt3d2q))/reference/ReferencesPapers.aspx?ReferenceID=1556565.
- 2.Hsia C.C.W., Hyde D.M., Weibel E.R. Lung Structure and the Intrinsic Challenges of Gas Exchange. Compr. Physiol. 2016;6:827. doi: 10.1002/CPHY.C150028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Kased R.F. Natural Antibacterial Remedy for Respiratory Tract Infections. Asian Pac. J. Trop. Biomed. 2016;6:270–274. doi: 10.1016/j.apjtb.2015.12.002. [DOI] [Google Scholar]
- 4.Haddad M., Sharma S. Physiology, Lung. [(accessed on 22 January 2022)]; Available online: https://www.ncbi.nlm.nih.gov/books/NBK545177/
- 5.Mannino D.M., Ford E.S., Redd S.C. Obstructive and Restrictive Lung Disease and Functional Limitation: Data from the Third National Health and Nutrition Examination. J. Intern. Med. 2003;254:540–547. doi: 10.1111/j.1365-2796.2003.01211.x. [DOI] [PubMed] [Google Scholar]
- 6.Bacterial Respiratory Tract Infection—The Lung Docs. [(accessed on 22 January 2022)]. Available online: https://www.thelungdocs.com/services/respiratory-infections/
- 7.Rosati L.A., Leslie K.O. Lung Infections. Pract. Pulm. Pathol. A Diagn. Approach. 2011:137–211. doi: 10.1016/B978-1-4160-5770-3.00006-7. [DOI] [Google Scholar]
- 8.Piret J., Boivin G. Pandemics Throughout History. Front. Microbiol. 2021;11:3594. doi: 10.3389/fmicb.2020.631736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omrani M., Keshavarz M., Nejad Ebrahimi S., Mehrabi M., McGaw L.J., Ali Abdalla M., Mehrbod P. Potential Natural Products against Respiratory Viruses: A Perspective to Develop Anti-COVID-19 Medicines. Front. Pharmacol. 2020;11:2115. doi: 10.3389/fphar.2020.586993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paget J., Spreeuwenberg P., Charu V., Taylor R.J., Iuliano A.D., Bresee J., Simonsen L., Viboud C. Global Mortality Associated with Seasonal Influenza Epidemics: New Burden Estimates and Predictors from the GLaMOR Project. J. Glob. Health. 2019;9:020421. doi: 10.7189/jogh.09.020421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. [(accessed on 22 January 2022)]. Available online: https://covid19.who.int/
- 12.Sanders M. Inhalation Therapy: An Historical Review. Prim. Care Respir. J. 2007;16:71–81. doi: 10.3132/pcrj.2007.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lavorini F., Buttini F., Usmani O.S. 100 Years of Drug Delivery to the Lungs. Handb. Exp. Pharmacol. 2019;260:143–159. doi: 10.1007/164_2019_335. [DOI] [PubMed] [Google Scholar]
- 14.Borghardt J.M., Kloft C., Sharma A. Inhaled Therapy in Respiratory Disease: The Complex Interplay of Pulmonary Kinetic Processes. Can. Respir. J. 2018;2018:2732017. doi: 10.1155/2018/2732017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geddes D. The History of Respiratory Disease Management. Medicine. 2020;48:239–243. doi: 10.1016/j.mpmed.2020.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zumla A., Memish Z.A., Maeurer M., Bates M., Mwaba P., Al-Tawfiq J.A., Denning D.W., Hayden F.G., Hui D.S. Emerging Novel and Antimicrobial-Resistant Respiratory Tract Infections: New Drug Development and Therapeutic Options. Lancet Infect. Dis. 2014;14:1136–1149. doi: 10.1016/S1473-3099(14)70828-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Behzadi M.A., Leyva-Grado V.H. Overview of Current Therapeutics and Novel Candidates against Influenza, Respiratory Syncytial Virus, and Middle East Respiratory Syndrome Coronavirus Infections. Front. Microbiol. 2019;10:1327. doi: 10.3389/fmicb.2019.01327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sorokina M., Steinbeck C. Review on Natural Products Databases: Where to Find Data in 2020. J. Cheminform. 2020;12:20. doi: 10.1186/s13321-020-00424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruce S.O., Onyegbule F.A. Biosynthesis of Natural Products. Biosynthesis. 2021 doi: 10.5772/INTECHOPEN.97660. [DOI] [Google Scholar]
- 20.Kowalczyk A., Przychodna M., Sopata S., Bodalska A., Fecka I. Thymol and Thyme Essential Oil—New Insights into Selected Therapeutic Applications. Molecules. 2020;25:4125. doi: 10.3390/molecules25184125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Badary O.A., Hamza M.S., Tikamdas R. Thymoquinone: A Promising Natural Compound with Potential Benefits for COVID-19 Prevention and Cure. Drug Des. Dev. Ther. 2021;15:1819. doi: 10.2147/DDDT.S308863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Article R. Antiviral Compounds from Marine Bivalves for Evaluation against SARS-CoV-2. J. Peersci. 2020;2:e1000015. [Google Scholar]
- 23.Cheuka P.M., Mayoka G., Mutai P., Chibale K. The Role of Natural Products in Drug Discovery and Development against Neglected Tropical Diseases. Molecules. 2017;22:58. doi: 10.3390/molecules22010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Molinari G. Natural Products in Drug Discovery: Present Status and Perspectives. Adv. Exp. Med. Biol. 2009;655:13–27. doi: 10.1007/978-1-4419-1132-2_2. [DOI] [PubMed] [Google Scholar]
- 25.Kritek P.A., Choi A.M.K. Diagnostic Procedures in Respiratory Disease|Basicmedical Key. [(accessed on 23 January 2022)]. Available online: https://basicmedicalkey.com/diagnostic-procedures-in-respiratory-disease/
- 26.Grumelli S., Corry D.B., Song L.Z., Song L., Green L., Huh J., Hacken J., Espada R., Bag R., Lewis D.E., et al. An Immune Basis for Lung Parenchymal Destruction in Chronic Obstructive Pulmonary Disease and Emphysema. PLoS Med. 2004;1:e8. doi: 10.1371/journal.pmed.0010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Respiratory Diseases Ministry of Health and Medical Services. Solomon Islands Healthy Village Facilitator’s Guide. [(accessed on 23 January 2022)]. Available online: https://www.jica.go.jp/project/solomon/002/materials/ku57pq00003um0e9-att/Respiratory_Diseases.pdf.
- 28.WHO Package of Essential NCD Interventions (PEN) Management of Chronic Respiratory Diseases . Training Manual WHO Package of Essential NCD Interventions (PEN) Management of Chronic Respiratory Diseases 1. Asthma 2. Chronic Obstructive Pulmonary Diseases (COPD) WHO; Geneva, Switzerland: 2020. 77p. [Google Scholar]
- 29.Chronic Respiratory Diseases. [(accessed on 23 January 2022)]. Available online: https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_1.
- 30.Estimating the Burden of Respiratory Diseases. [(accessed on 23 January 2022)]; Available online: https://www.ncbi.nlm.nih.gov/books/NBK310631/
- 31.Ku G.M.V., Da Silveira V.C., Develtere P., Nemery B., Marchal B., Dossou J.P., Bossyns P., Gyselinck K., Kegels G. Strategic Responses to CRD in Africa Chronic Respiratory Diseases (CRD) in Africa Identifying Social Determinants and Formulating Appropriate, Strategic Responses. [(accessed on 23 January 2022)]. Available online: https://www.researchgate.net/publication/351618613.
- 32.Dasaraju P.V., Liu C. Concise Handbook of Infectious Diseases. Jaypee Brothers Medical Publisher Inc.; New Delhi, India: 1996. Infections of the Respiratory System; p. 65. [DOI] [Google Scholar]
- 33.Wisnivesky J., De-Torres J.P. The Global Burden of Pulmonary Diseases: Most Prevalent Problems and Opportunities for Improvement. Ann. Glob. Health. 2019;85:1. doi: 10.5334/aogh.2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Labaki W.W., Han M.L.K. Chronic Respiratory Diseases: A Global View. Lancet Respir. Med. 2020;8:531–533. doi: 10.1016/S2213-2600(20)30157-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burney P., Jarvis D., Perez-Padilla R. The Global Burden of Chronic Respiratory Disease in Adults. Int. J. Tuberc. Lung Dis. 2015;19:10–20. doi: 10.5588/ijtld.14.0446. [DOI] [PubMed] [Google Scholar]
- 36.Soriano J.B., Kendrick P.J., Paulson K.R., Gupta V., Abrams E.M., Adedoyin R.A., Adhikari T.B., Advani S.M., Agrawal A., Ahmadian E., et al. Prevalence and Attributable Health Burden of Chronic Respiratory Diseases, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2020;8:585–596. doi: 10.1016/S2213-2600(20)30105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shimizu K., Yoshii Y., Morozumi M., Chiba N., Ubukata K., Uruga H., Hanada S., Saito N., Kadota T., Ito S., et al. Pathogens in COPD Exacerbations Identified by Comprehensive Real-Time PCR plus Older Methods. Int. J. Chronic Obstr. Pulm. Dis. 2015;10:2009. doi: 10.2147/COPD.S82752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gautier C., Charpin D. Environmental Triggers and Avoidance in the Management of Asthma. J. Asthma Allergy. 2017;10:47. doi: 10.2147/JAA.S121276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pulmonary Hypertension|Cdc.Gov. [(accessed on 23 January 2022)]; Available online: https://www.cdc.gov/heartdisease/pulmonary_hypertension.htm.
- 40.Adigun R., Singh R. Tuberculosis. [(accessed on 23 January 2022)]; Available online: https://www.ncbi.nlm.nih.gov/books/NBK441916/
- 41.Lim W.S. Pneumonia—Overview. Ref. Modul. Biomed. Sci. 2020:185–197. doi: 10.1016/B978-0-12-801238-3.11636-8. [DOI] [Google Scholar]
- 42.Krammer F., Smith G.J.D., Fouchier R.A.M., Peiris M., Kedzierska K., Doherty P.C., Palese P., Shaw M.L., Treanor J., Webster R.G., et al. Influenza. Nat. Rev. Dis. Primers. 2018;4:3. doi: 10.1038/s41572-018-0002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.dela Cruz C.S., Tanoue L.T., Matthay R.A. Lung Cancer: Epidemiology, Etiology, and Prevention. Clin. Chest. Med. 2011;32:605–644. doi: 10.1016/j.ccm.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19) [(accessed on 31 January 2022)]; Available online: https://pubmed.ncbi.nlm.nih.gov/32150360/ [PubMed]
- 45.Pappas D.E. Principles and Practice of Pediatric Infectious Diseases. Elsevier Public Health Emergency Collection; Amsterdam, The Netherlands: 2018. The Common Cold; p. 199. [DOI] [Google Scholar]
- 46.Taylor M., Raja A. StatPearls. StatPearls Publishing; Mountain View, CA, USA: 2022. Oral Candidiasis. [PubMed] [Google Scholar]
- 47.Ferkol T., Schraufnagel D. The Global Burden of Respiratory Disease. Ann. Am. Thorac. Soc. 2014;11:404–406. doi: 10.1513/AnnalsATS.201311-405PS. [DOI] [PubMed] [Google Scholar]
- 48.Forum of International Respiratory Societies The Global Impact of Respiratory Disease. 2012. [(accessed on 23 January 2022)]. Available online: https://www.thoracic.org/about/newsroom/press-releases/journal/2017/forum-of-international-respiratory-societies-releases--the-global-impact-of-respiratory-diseases.php.
- 49.Boehm A., Pizzini A., Sonnweber T., Loeffler-Ragg J., Lamina C., Weiss G., Tancevski I. Assessing Global COPD Awareness with Google Trends. Eur. Respir. J. 2019;53:1900351. doi: 10.1183/13993003.00351-2019. [DOI] [PubMed] [Google Scholar]
- 50.Air Pollution. [(accessed on 11 February 2022)]. Available online: https://www.who.int/data/gho/data/themes/theme-details/GHO/air-pollution.
- 51.Wang M., Luo X., Xu S., Liu W., Ding F., Zhang X., Wang L., Liu J., Hu J., Wang W. Trends in Smoking Prevalence and Implication for Chronic Diseases in China: Serial National Cross-Sectional Surveys from 2003 to 2013. Lancet Respir. Med. 2019;7:35–45. doi: 10.1016/S2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 52.Stanaway J.D., Afshin A., Gakidou E., Lim S.S., Abate D., Abate K.H., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., et al. Global, Regional, and National Comparative Risk Assessment of 84 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–1994. doi: 10.1016/S0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhao Y., Huang Z., Wang S., Hu J., Xiao J., Li X., Liu T., Zeng W., Guo L., Du Q., et al. Morbidity Burden of Respiratory Diseases Attributable to Ambient Temperature: A Case Study in a Subtropical City in China. Environ. Health. 2019;18:89. doi: 10.1186/s12940-019-0529-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zar H.J., Ferkol T.W. The Global Burden of Respiratory Disease-Impact on Child Health. Pediatr. Pulmonol. 2014;49:430–434. doi: 10.1002/ppul.23030. [DOI] [PubMed] [Google Scholar]
- 55.Quan D., Nagalingam G., Payne R., Triccas J.A. New Tuberculosis Drug Leads from Naturally Occurring Compounds. Int. J. Infect. Dis. 2017;56:212–220. doi: 10.1016/j.ijid.2016.12.024. [DOI] [PubMed] [Google Scholar]
- 56.Straif-Bourgeois S., Ratard R., Kretzschmar M. Handbook of Epidemiology. Elsevier; Amsterdam, The Netherlands: 2014. Infectious Disease Epidemiology; pp. 2041–2119. [DOI] [Google Scholar]
- 57.Aït-Khaled N., Enarson D., Bousquet J. Chronic Respiratory Diseases in Developing Countries: The Burden and Strategies for Prevention and Management. Bull. World Health Organ. 2001;79:971–979. [PMC free article] [PubMed] [Google Scholar]
- 58.Burki T.K. The Economic Cost of Respiratory Disease in the UK. Lancet Respir. Med. 2017;5:381. doi: 10.1016/S2213-2600(17)30108-X. [DOI] [PubMed] [Google Scholar]
- 59.Kuehn B.M. Lung Diseases Affecting US Workers Cost Billions Annually. JAMA. 2020;324:734. doi: 10.1001/jama.2020.14764. [DOI] [PubMed] [Google Scholar]
- 60.Wang D.Y., Ghoshal A.G., bin Abdul Muttalif A.R., Lin H.C., Thanaviratananich S., Bagga S., Faruqi R., Sajjan S., Brnabic A.J.M., Dehle F.C., et al. Quality of Life and Economic Burden of Respiratory Disease in Asia-Pacific-Asia-Pacific Burden of Respiratory Diseases Study. Value Health Reg Issues. 2016;9:72–77. doi: 10.1016/j.vhri.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 61.Tabyshova A., Emilov B., Postma M.J., Chavannes N.H., Sooronbaev T., van Boven J.F.M. Prevalence and Economic Burden of Respiratory Diseases in Central Asia and Russia: A Systematic Review. Int. J. Environ. Res. Public Health. 2020;17:7483. doi: 10.3390/ijerph17207483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Erhabor G.E., Erhabor G.E. Respiratory Health in Africa: Strides and Challenges. J. Pan Afr. Thorac. Soc. 2021;2:11–17. doi: 10.25259/JPATS_30_2020. [DOI] [Google Scholar]
- 63.Khamees A., Bani-Issa J., Zoubi M.S., Qasem T., AbuAlArjah M.I., Alawadin S.A., Al-Shami K., Hussein F.E., Hussein E., Bashayreh I.H., et al. SARS-CoV-2 and Coronavirus Disease Mitigation: Treatment Options, Vaccinations and Variants. Pathogens. 2022;11:275. doi: 10.3390/pathogens11020275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matić Z., Šantak M. Current View on Novel Vaccine Technologies to Combat Human Infectious Diseases. Appl. Microbiol. Biotechnol. 2022;106:25–56. doi: 10.1007/s00253-021-11713-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hossain M.K., Hassanzadeganroudsari M., Apostolopoulos V. The Emergence of New Strains of SARS-CoV-2. What Does It Mean for COVID-19 Vaccines? Expert. Rev. Vaccines. 2021;20:635–638. doi: 10.1080/14760584.2021.1915140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Barr R.G., Camargo C.A. Hormone Replacement Therapy and Obstructive Airway Diseases. Treat. Respir. Med. 2004;3:1–7. doi: 10.2165/00151829-200403010-00001. [DOI] [PubMed] [Google Scholar]
- 67.Patil N., Paulose R.M., Udupa K.S., Ramakrishna N., Ahmed T. Pulmonary Toxicity of Bleomycin—A Case Series from a Tertiary Care Center in Southern India. J. Clin. Diagn. Res. 2016;10:FR01. doi: 10.7860/JCDR/2016/18773.7626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Newnham D.M. Asthma Medications and Their Potential Adverse Effects in the Elderly: Recommendations for Prescribing. Drug Saf. 2001;24:1065–1080. doi: 10.2165/00002018-200124140-00005. [DOI] [PubMed] [Google Scholar]
- 69.de Benedictis F.M., Bush A. Corticosteroids in Respiratory Diseases in Children. Am. J. Respir. Crit Care Med. 2012;185:12–23. doi: 10.1164/rccm.201107-1174CI. [DOI] [PubMed] [Google Scholar]
- 70.Lenney W., Boner A.L., Bont L., Bush A., Carlsen K.H., Eber E., Fauroux B., Götz M., Greenough A., Grigg J., et al. Medicines Used in Respiratory Diseases Only Seen in Children. Eur. Respir. J. 2009;34:531–551. doi: 10.1183/09031936.00166508. [DOI] [PubMed] [Google Scholar]
- 71.Kew K.M., Seniukovich A. Inhaled Steroids and Risk of Pneumonia for Chronic Obstructive Pulmonary Disease. Cochrane. Database Syst. Rev. 2014;2014 doi: 10.1002/14651858.CD010115.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Restrepo M.I., Sole-Violan J., Martin-Loeches I. Macrolide Therapy of Pneumonia: Is It Necessary, and How Does It Help? Curr. Opin. Infect. Dis. 2016;29:212–217. doi: 10.1097/QCO.0000000000000250. [DOI] [PubMed] [Google Scholar]
- 73.Forget E.J., Menzies D. Adverse Reactions to First-Line Antituberculosis Drugs. Expert. Opin. Drug Saf. 2006;5:231–249. doi: 10.1517/14740338.5.2.231. [DOI] [PubMed] [Google Scholar]
- 74.Influenza (Flu) Antiviral Drugs and Related Information|FDA. [(accessed on 12 February 2022)]; Available online: https://www.fda.gov/drugs/information-drug-class/influenza-flu-antiviral-drugs-and-related-information.
- 75.Zadeh N.M., Asl N.S.M., Forouharnejad K., Ghadimi K., Parsa S., Mohammadi S., Omidi A. Mechanism and Adverse Effects of COVID-19 Drugs: A Basic Review. Int. J. Physiol. Pathophysiol. Pharmacol. 2021;13:102. [PMC free article] [PubMed] [Google Scholar]
- 76.Leisegang K. Herbal Medicine in Andrology. Elsevier Inc.; Amsterdam, The Netherlands: 2021. Herbal Pharmacognosy: An Introduction; pp. 17–26. [DOI] [Google Scholar]
- 77.Atanasov A.G., Zotchev S.B., Dirsch V.M., Orhan I.E., Banach M., Rollinger J.M., Barreca D., Weckwerth W., Bauer R., Bayer E.A., et al. Natural Products in Drug Discovery: Advances and Opportunities. Nat. Rev. Drug Discov. 2021;20:200–216. doi: 10.1038/s41573-020-00114-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dias D.A., Urban S., Roessner U. A Historical Overview of Natural Products in Drug Discovery. Metabolites. 2012;2:303–336. doi: 10.3390/metabo2020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Haefner B. Drugs from the Deep: Marine Natural Products as Drug Candidates. Drug Discov. Today. 2003;8:536–544. doi: 10.1016/S1359-6446(03)02713-2. [DOI] [PubMed] [Google Scholar]
- 80.Tan S.Y., Tatsumura Y. Alexander Fleming (1881–1955): Discoverer of Penicillin. Singap. Med. J. 2015;56:366. doi: 10.11622/smedj.2015105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wainwright M. Miracle Cure: The Story of Penicillin and the Golden Age of Antibiotics. [(accessed on 26 February 2022)]. Available online: https://www.wiley.com/en-gb/Miracle+Cure%3A+The+Story+of+Penicillin+and+the+Golden+Age+of+Antibiotics-p-9780631164920.
- 82.Maplestone R.A., Stone M.J., Williams D.H. The Evolutionary Role of Secondary Metabolites—A Review. Gene. 1992;115:151–157. doi: 10.1016/0378-1119(92)90553-2. [DOI] [PubMed] [Google Scholar]
- 83.Success Story: Taxol. [(accessed on 26 February 2022)]; Available online: https://dtp.cancer.gov/timeline/flash/success_stories/s2_taxol.htm.
- 84.Bang S., Li W., Ha T.K.Q., Lee C., Oh W.K., Shim S.H. Anti-Influenza Effect of the Major Flavonoids from Salvia Plebeia R.Br. via Inhibition of Influenza H1N1 Virus Neuraminidase. Nat. Prod. Res. 2018;32:1224–1228. doi: 10.1080/14786419.2017.1326042. [DOI] [PubMed] [Google Scholar]
- 85.Li B., Ni Y., Zhu L.J., Wu F.B., Yan F., Zhang X., Yao X.S. Flavonoids from Matteuccia Struthiopteris and Their Anti-Influenza Virus (H1N1) Activity. J. Nat. Prod. 2015;78:987–995. doi: 10.1021/np500879t. [DOI] [PubMed] [Google Scholar]
- 86.Mehrbod P., Abdalla M.A., Fotouhi F., Heidarzadeh M., Aro A.O., Eloff J.N., McGaw L.J., Fasina F.O. Immunomodulatory Properties of Quercetin-3-O-α-L-Rhamnopyranoside from Rapanea Melanophloeos against Influenza a Virus. BMC Complement. Altern. Med. 2018;18:184. doi: 10.1186/s12906-018-2246-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sukuru S.C.K., Jenkins J.L., Beckwith R.E.J., Scheiber J., Bender A., Mikhailov D., Davies J.W., Glick M. Plate-Based Diversity Selection Based on Empirical HTS Data to Enhance the Number of Hits and Their Chemical Diversity. J. Biomol. Screen. 2009;14:690–699. doi: 10.1177/1087057109335678. [DOI] [PubMed] [Google Scholar]
- 88.Caminero J.A., Sotgiu G., Zumla A., Migliori G.B. Best Drug Treatment for Multidrug-Resistant and Extensively Drug-Resistant Tuberculosis. Lancet Infect. Dis. 2010;10:621–629. doi: 10.1016/S1473-3099(10)70139-0. [DOI] [PubMed] [Google Scholar]
- 89.Igarashi M., Ishizaki Y., Takahashi Y. New Antituberculous Drugs Derived from Natural Products: Current Perspectives and Issues in Antituberculous Drug Development. J. Antibiot. 2017;71:15–25. doi: 10.1038/ja.2017.126. [DOI] [PubMed] [Google Scholar]
- 90.Mahomoodally M.F. Traditional Medicines in Africa: An Appraisal of Ten Potent African Medicinal Plants. Evid.-Based Complement. Altern. Med. 2013;2013:617459. doi: 10.1155/2013/617459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Elkady W.M., Bishr M.M., Abdel-Aziz M.M., Salama O.M. Identification and Isolation of Anti-Pneumonia Bioactive Compounds from Opuntia ficus-indica Fruit Waste Peels. Food Funct. 2020;11:5275–5283. doi: 10.1039/D0FO00817F. [DOI] [PubMed] [Google Scholar]
- 92.Alexandrow M.G., Song L.J., Altiok S., Gray J., Haura E.B., Kumar N.B. Curcumin: A Novel Stat3 Pathway Inhibitor for Chemoprevention of Lung Cancer. Eur. J. Cancer Prev. 2012;21:407–412. doi: 10.1097/CEJ.0b013e32834ef194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rattis B.A.C., Ramos S.G., Celes M.R.N. Curcumin as a Potential Treatment for COVID-19. Front. Pharmacol. 2021;12:1068. doi: 10.3389/fphar.2021.675287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mao Q.Q., Xu X.Y., Cao S.Y., Gan R.Y., Corke H., Beta T., Li H. bin Bioactive Compounds and Bioactivities of Ginger (Zingiber officinale Roscoe) Foods. 2019;8:185. doi: 10.3390/foods8060185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Li X., Jin F., Lee H.J., Lee C.J. Recent Advances in the Development of Novel Drug Candidates for Regulating the Secretion of Pulmonary Mucus. Biomol. Ther. 2020;28:293–301. doi: 10.4062/biomolther.2020.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gholamnezhad Z., Keyhanmanesh R., Boskabady M.H. Anti-Inflammatory, Antioxidant, and Immunomodulatory Aspects of Nigella Sativa for Its Preventive and Bronchodilatory Effects on Obstructive Respiratory Diseases: A Review of Basic and Clinical Evidence. J. Funct. Foods. 2015;17:910–927. doi: 10.1016/j.jff.2015.06.032. [DOI] [Google Scholar]
- 97.Gholamnezhad Z., Shakeri F., Saadat S., Ghorani V., Boskabady M.H. Clinical and Experimental Effects of Nigella Sativa and Its Constituents on Respiratory and Allergic Disorders. Avicenna J. Phytomed. 2019;9:195. [PMC free article] [PubMed] [Google Scholar]
- 98.Shu G., Xu D., Ran C., Yin L., Lin J., Fu H., Zhang W., Bai S., Peng X., Zhao X., et al. Protective Effect of Dietary Supplementation of Bupleurum Falcatum L Saikosaponins on Ammonia Exposure–Induced Ileum Injury in Broilers. Poult. Sci. 2021;100:100803. doi: 10.1016/j.psj.2020.10.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Li X.Q., Song Y.N., Wang S.J., Rahman K., Zhu J.Y., Zhang H. Saikosaponins: A Review of Pharmacological Effects. J. Asian Nat. Prod. Res. 2018;20:399–411. doi: 10.1080/10286020.2018.1465937. [DOI] [PubMed] [Google Scholar]
- 100.Cheng P.W., Ng L.T., Chiang L.C., Lin C.C. Antiviral Effects of saikosaponins on human coronavirus 229E in vitro. Clin. Exp. Pharmacol. Physiol. 2006;33:612. doi: 10.1111/j.1440-1681.2006.04415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Li C., Chen J., Yuan W., Zhang W., Chen H., Tan H. Preventive Effect of Ursolic Acid Derivative on Particulate Matter 2.5-Induced Chronic Obstructive Pulmonary Disease Involves Suppression of Lung Inflammation. IUBMB Life. 2020;72:632–640. doi: 10.1002/iub.2201. [DOI] [PubMed] [Google Scholar]
- 102.Kumar D., Prasad D.N., Kumar D. Antiasthmatic Activity of Ethanolic Extract of Aerva Lanata Linn. Pharmacologyonline. 2009;2:1075–1081. [Google Scholar]
- 103.Effect of Ageratum conyzoides Linn on Clonidine and Haloperidol Induced Catalepsy in Mice. [(accessed on 27 February 2022)]. Available online: https://www.researchgate.net/publication/285674932_Effect_of_Ageratum_conyzoides_Linn_on_clonidine_and_haloperidol_induced_catalepsy_in_mice.
- 104.Arreola R., Quintero-Fabián S., Lopez-Roa R.I., Flores-Gutierrez E.O., Reyes-Grajeda J.P., Carrera-Quintanar L., Ortuno-Sahagun D. Immunomodulation and Anti-Inflammatory Effects of Garlic Compounds. J. Immunol. Res. 2015;2015:401630. doi: 10.1155/2015/401630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Borlinghaus J., Albrecht F., Gruhlke M.C.H., Nwachukwu I.D., Slusarenko A.J. Allicin: Chemistry and Biological Properties. Molecules. 2014;19:12591–12618. doi: 10.3390/molecules190812591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mösbauer K., Fritsch V.N., Adrian L., Bernhardt J., Gruhlke M.C.H., Slusarenko A.J., Niemeyer D., Antelmann H. The Effect of Allicin on the Proteome of SARS-CoV-2 Infected Calu-3 Cells. Front. Microbiol. 2021;12:3238. doi: 10.3389/fmicb.2021.746795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Leal L.K.A.M., Costa M.F., Pitombeira M., Barroso V.M., Silveira E.R., Canuto K.M., Viana G.S.B. Mechanisms Underlying the Relaxation Induced by Isokaempferide from Amburana cearensis in the Guinea-Pig Isolated Trachea. Life Sci. 2006;79:98–104. doi: 10.1016/j.lfs.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 108.Verma S., Twilley D., Esmear T., Oosthuizen C.B., Reid A.M., Nel M., Lall N. Anti-SARS-CoV Natural Products with the Potential to Inhibit SARS-CoV-2 (COVID-19) Front. Pharmacol. 2020;11:1514. doi: 10.3389/fphar.2020.561334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Anti-Stress and Antiallergic Effect of Argemone Mexicana Stems in Asthma|Request PDF. [(accessed on 27 February 2022)]. Available online: https://www.researchgate.net/publication/285320843_Anti-Stress_and_Antiallergic_Effect_of_Argemone_Mexicana_Stems_in_Asthma.
- 110.Akah P.A., Ezike A.C., Nwafor S.V., Okoli C.O., Enwerem N.M. Evaluation of the Anti-Asthmatic Property of Asystasia gangetica Leaf Extracts. J. Ethnopharmacol. 2003;89:25–36. doi: 10.1016/S0378-8741(03)00227-7. [DOI] [PubMed] [Google Scholar]
- 111.Rao P.V., Gan S.H. Cinnamon: A Multifaceted Medicinal Plant. Evid.-Based Complementary Altern. Med. 2014:642942. doi: 10.1155/2014/642942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Singh H.B., Srivastava M., Singh A.B., Srivastava A.K. Cinnamon Bark Oil, a Potent Fungitoxicant against Fungi Causing Respiratory Tract Mycoses. Allergy. 1995;50:995–999. doi: 10.1111/j.1398-9995.1995.tb02515.x. [DOI] [PubMed] [Google Scholar]
- 113.Lucas K., Fröhlich-Nowoisky J., Oppitz N., Ackermann M. Cinnamon and Hop Extracts as Potential Immunomodulators for Severe COVID-19 Cases. Front. Plant Sci. 2021;12:263. doi: 10.3389/fpls.2021.589783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ranasinghe P., Jayawardena R., Pigera S., Wathurapatha W.S., Weeratunga H.D., Premakumara G.A.S., Katulanda P., Constantine G.R., Galappaththy P. Evaluation of Pharmacodynamic Properties and Safety of Cinnamomum Zeylanicum (Ceylon Cinnamon) in Healthy Adults: A Phase I Clinical Trial. BMC Complementary Altern. Med. 2017;17:550. doi: 10.1186/s12906-017-2067-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Evaluation of Antiasthmatic Activity of Cassia sophera Linn|Semantic Scholar. [(accessed on 27 February 2022)]. Available online: https://www.semanticscholar.org/paper/Evaluation-of-antiasthmatic-activity-of-Cassia-linn-Nagore-Ghosh/d36e402528ff9ab4e7c8f98d4ac5a932ab4ab7a8.
- 116.Zeng W., Jin L., Zhang F., Zhang C., Liang W. Naringenin as a Potential Immunomodulator in Therapeutics. Pharmacol. Res. 2018;135:122–126. doi: 10.1016/j.phrs.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 117.Elango R., Athinarayanan J., Subbarayan V.P., Lei D.K.Y., Alshatwi A.A. Hesperetin Induces an Apoptosis-Triggered Extrinsic Pathway and a P53- Independent Pathway in Human Lung Cancer H522 Cells. J. Asian Nat. Prod. Res. 2018;20:559–569. doi: 10.1080/10286020.2017.1327949. [DOI] [PubMed] [Google Scholar]
- 118.Chen X.M., Tait A.R., Kitts D.D. Flavonoid Composition of Orange Peel and Its Association with Antioxidant and Anti-Inflammatory Activities. Food Chem. 2017;218:15–21. doi: 10.1016/j.foodchem.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 119.Wei X., Shao X. Nobiletin Alleviates Endometriosis via Down-Regulating NF-ΚB Activity in Endometriosis Mouse Model. Biosci. Rep. 2018;38:BSR20180470. doi: 10.1042/BSR20180470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Muhammad T., Ikram M., Ullah R., Rehman S.U., Kim M.O. Hesperetin, a Citrus Flavonoid, Attenuates LPS-Induced Neuroinflammation, Apoptosis and Memory Impairments by Modulating TLR4/NF-ΚB Signaling. Nutrients. 2019;11:648. doi: 10.3390/nu11030648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhou L., Gu W., Kui F., Gao F., Niu Y., Li W., Zhang Y., Guo L., Wang J., Guo Z., et al. The Mechanism and Candidate Compounds of Aged Citrus Peel (Chenpi) Preventing Chronic Obstructive Pulmonary Disease and Its Progression to Lung Cancer. Food Nutr. Res. 2021;65 doi: 10.29219/fnr.v65.7526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Okpo S.O., Adeyemi O.O. The Anti-Allergic Effects of Crinum Glaucum Aqueous Extract. Phytomedicine. 2002;9:438–441. doi: 10.1078/09447110260571698. [DOI] [PubMed] [Google Scholar]
- 123.Lawal I.O., Olufade I.I., Rafiu B.O., Aremu A.O. Ethnobotanical Survey of Plants Used for Treating Cough Associated with Respiratory Conditions in Ede South Local Government Area of Osun State, Nigeria. Plants. 2020;9:647. doi: 10.3390/plants9050647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ajayi G., Adegunloye B., Oroye O. Effects of crinum glaucum on cardiorespiratory function in anaesthetised CAT. Niger. J. Nat. Prod. Med. 1997;1:15–16. doi: 10.4314/njnpm.v1i1.11791. [DOI] [Google Scholar]
- 125.Bormann M., Alt M., Schipper L., van de Sand L., Le-Trilling V.T.K., Rink L., Heinen N., Madel R.J., Otte M., Wuensch K., et al. Turmeric Root and Its Bioactive Ingredient Curcumin Effectively Neutralize SARS-CoV-2 In Vitro. Viruses. 2021;13:1914. doi: 10.3390/v13101914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Abdollahi E., Momtazi A.A., Johnston T.P., Sahebkar A. Therapeutic Effects of Curcumin in Inflammatory and Immune-Mediated Diseases: A Nature-Made Jack-of-All-Trades? J. Cell. Physiol. 2018;233:830–848. doi: 10.1002/jcp.25778. [DOI] [PubMed] [Google Scholar]
- 127.Praditya D., Kirchhoff L., Brüning J., Rachmawati H., Steinmann J., Steinmann E. Anti-Infective Properties of the Golden Spice Curcumin. Front. Microbiol. 2019;10:912. doi: 10.3389/fmicb.2019.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Abidi A., Gupta S., Agarwal M., Bhalla H.L., Saluja M. Evaluation of Efficacy of Curcumin as an Add-on Therapy in Patients of Bronchial Asthma. J. Clin. Diagn. Res. 2014;8:HC19. doi: 10.7860/JCDR/2014/9273.4705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tang L., Liu J., Zhu L., Chen Q., Meng Z., Sun L., Hu J., Ni Z., Wang X. Curcumin Inhibits Growth of Human NCI-H292 Lung Squamous Cell Carcinoma Cells by Increasing FOXA2 Expression. Front. Pharmacol. 2018;9:60. doi: 10.3389/fphar.2018.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Dai J., Gu L., Su Y., Wang Q., Zhao Y., Chen X., Deng H., Li W., Wang G., Li K. Inhibition of Curcumin on Influenza a Virus Infection and Influenzal Pneumonia via Oxidative Stress, TLR2/4, P38/JNK MAPK and NF-ΚB Pathways. Int. Immunopharmacol. 2018;54:177–187. doi: 10.1016/j.intimp.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 131.Youssouf M.S., Kaiser P., Tahir M., Singh G.D., Singh S., Sharma V.K., Satti N.K., Haque S.E., Johri R.K. Anti-Anaphylactic Effect of Euphorbia Hirta. Fitoterapia. 2007;78:535–539. doi: 10.1016/j.fitote.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 132.Kumar S., Malhotra R., Kumar D. Euphorbia Hirta: Its Chemistry, Traditional and Medicinal Uses, and Pharmacological Activities. Pharmacogn. Rev. 2010;4:58. doi: 10.4103/0973-7847.65327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Barnes L.A., Leach M., Anheyer D., Brown D., Carè J., Lauche R., Medina D.N., Pinder T.A., Bugarcic A., Steel A. The Effects of Hedera Helix on Viral Respiratory Infections in Humans: A Rapid Review. Adv. Integr. Med. 2020;7:222. doi: 10.1016/j.aimed.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ponz F., Noguchi H., Matveeva T., Khafizova G., Sokornova S. In Search of Herbal Anti-SARS-CoV2 Compounds. Front. Plant Sci. 2020;11:1807. doi: 10.3389/fpls.2020.589998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yamamura S., Ozawa K., Ohtani K., Kasai R., Yamasaki K. Antihistaminic Flavones and Aliphatic Glycosides from Mentha Spicata. Phytochemistry. 1998;48:131–136. doi: 10.1016/S0031-9422(97)01112-6. [DOI] [Google Scholar]
- 136.Effect of Various Extracts of Momordica Dioica Pulp O# CLO#IDI#E A#D Haloperidoli#Duced Catalepsy I# Mice|Semantic Scholar. [(accessed on 27 February 2022)]. Available online: https://www.semanticscholar.org/paper/EFFECT-OF-VARIOUS-EXTRACTS-OF-MOMORDICA-DIOICA-PULP-Rakh-Raut/13b2dd45eaa81ed6499b7e1ceeaef6af4663b606.
- 137.Taur D.J., Patil R.Y. Some Medicinal Plants with Antiasthmatic Potential: A Current Status. Asian Pac. J. Trop. Biomed. 2011;1:413. doi: 10.1016/S2221-1691(11)60091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Abdulhafidh A., Kadhim H.S. Effects of Black Seed on Lung Cancer: In Vitro Study Role of Viruses in Patients with Renal Transplant. View Project. Med. J. Babylon. 2015;12:363–377. [Google Scholar]
- 139.Iqbal H., Rhee D. kwon Ginseng Alleviates Microbial Infections of the Respiratory Tract: A Review. J. Ginseng Res. 2020;44:194. doi: 10.1016/j.jgr.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sung W.S., Lee D.G. In Vitro Candidacidal Action of Korean Red Ginseng Saponins against Candida albicans. Biol. Pharm. Bull. 2008;31:139–142. doi: 10.1248/bpb.31.139. [DOI] [PubMed] [Google Scholar]
- 141.Alsayari A., Muhsinah A.B., Almaghaslah D., Annadurai S., Wahab S. Pharmacological Efficacy of Ginseng against Respiratory Tract Infections. Molecules. 2021;26:4095. doi: 10.3390/molecules26134095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hajare R., Darvhekar V.M., Shewale A., Patil V. Evaluation of Antihistaminic Activity of Piper betel Leaf in Guinea Pig. Afr. J. Pharm. Pharmacol. 2011;5:113–117. doi: 10.5897/AJPP09.376. [DOI] [Google Scholar]
- 143.Evaluation of Anti Asthmatic Activity of Urtica Dioica (Linn.) Leaves and Its Phytochemical Studies Master of Pharmacy in Branch IV: Pharmacology Submitted by. [(accessed on 7 March 2022)]. Available online: http://repository-tnmgrmu.ac.in/10654/1/260403218vijaykumar.pdf.
- 144.Lin L.T., Chen T.Y., Lin S.C., Chung C.Y., Lin T.C., Wang G.H., Anderson R., Lin C.C., Richardson C.D. Broad-Spectrum Antiviral Activity of Chebulagic Acid and Punicalagin against Viruses That Use Glycosaminoglycans for Entry. BMC Microbiol. 2013;13:187. doi: 10.1186/1471-2180-13-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Anti-SARS Coronavirus 3C-Like Protease Effects of Rheum palmatum L. Extracts—PubMed. [(accessed on 7 March 2022)]; Available online: https://pubmed.ncbi.nlm.nih.gov/20103835/ [PubMed]
- 146.Wang X., Yang Y., Liu X., Gao X. Pharmacological Properties of Tanshinones, the Natural Products from Salvia miltiorrhiza. Adv. Pharmacol. 2020;87:43–70. doi: 10.1016/BS.APHA.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 147.Wan L., Meng D., Wang H., Wan S., Jiang S., Huang S., Wei L., Yu P. Preventive and Therapeutic Effects of Thymol in a Lipopolysaccharide-Induced Acute Lung Injury Mice Model. Inflammation. 2018;41:183–192. doi: 10.1007/s10753-017-0676-4. [DOI] [PubMed] [Google Scholar]
- 148.Nabissi M., Marinelli O., Morelli M.B., Nicotra G., Iannarelli R., Amantini C., Santoni G., Maggi F. Thyme Extract Increases Mucociliary-Beating Frequency in Primary Cell Lines from Chronic Obstructive Pulmonary Disease Patients. Biomed. Pharmacother. 2018;105:1248–1253. doi: 10.1016/j.biopha.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 149.Farahani M. Antiviral Effect Assay of Thymus Kotschyanus on HSV-1 Multiplication. Alborz Univ. Med. J. 2017;6:269–275. doi: 10.29252/aums.6.4.269. [DOI] [Google Scholar]
- 150.Sardari S., Mobaien A., Ghassemifard L., Kamali K., Khavasi N. Therapeutic Effect of Thyme (Thymus vulgaris) Essential Oil on Patients with COVID19: A Randomized Clinical Trial. J. Adv. Med. Biomed. Res. 2021;29:83–91. doi: 10.30699/jambs.29.133.83. [DOI] [Google Scholar]
- 151.Yang C.W., Lee Y.Z., Kang I.J., Barnard D.L., Jan J.T., Lin D., Huang C.W., Yeh T.K., Chao Y.S., Lee S.J. Identification of Phenanthroindolizines and Phenanthroquinolizidines as Novel Potent Anti-Coronaviral Agents for Porcine Enteropathogenic Coronavirus Transmissible Gastroenteritis Virus and Human Severe Acute Respiratory Syndrome Coronavirus. Antivir. Res. 2010;88:160–168. doi: 10.1016/j.antiviral.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Townsend E.A., Siviski M.E., Zhang Y., Xu C., Hoonjan B., Emala C.W. Effects of Ginger and Its Constituents on Airway Smooth Muscle Relaxation and Calcium Regulation. Am. J. Respir. Cell Mol. Biol. 2013;48:157. doi: 10.1165/rcmb.2012-0231OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Introduction to (Quantitative) Structure Activity Relationships—OECD. [(accessed on 7 March 2022)]. Available online: https://www.oecd.org/chemicalsafety/risk-assessment/introductiontoquantitativestructureactivityrelationships.htm.
- 154.Tong W., Welsh W.J., Shi L., Fang H., Perkins R. Structure-Activity Relationship Approaches and Applications. Environ. Toxicol. Chem. 2003;22:1680–1695. doi: 10.1897/01-198. [DOI] [PubMed] [Google Scholar]
- 155.Duque C., Castellanos L., Tello E. Corals in a Changing World. IntechOpen Ltd.; London, UK: 2018. Structure-Activity Relationship (SAR) Studies to Maximize the Activity of Compounds Isolated from Octocorals. [DOI] [Google Scholar]
- 156.Vanommeslaeghe K., Hatcher E., Acharya C., Kundu S., Zhong S., Shim J., Darian E., Guvench O., Lopes P., Vorobyov I., et al. CHARMM General Force Field: A Force Field for Drug-like Molecules Compatible with the CHARMM All-Atom Additive Biological Force Fields. J. Comput. Chem. 2010;31:671–690. doi: 10.1002/jcc.21367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Pires C.T.A., Scodro R.B.L., Cortez D.A.G., Brenzan M.A., Siqueira V.L.D., Caleffi-Ferracioli K.R., Vieira L.C.C., Monteiro J.L., Corrêa A.G., Cardoso R.F. Structure-Activity Relationship of Natural and Synthetic Coumarin Derivatives against Mycobacterium tuberculosis. Future Med. Chem. 2020;12:1533–1546. doi: 10.4155/fmc-2018-0281. [DOI] [PubMed] [Google Scholar]
- 158.Asfaw H., Laqua K., Walkowska A.M., Cunningham F., Martinez-Martinez M.S., Cuevas-Zurita J.C., Ballell-Pages L., Imming P. Design, Synthesis and Structure-Activity Relationship Study of Wollamide B; a New Potential Anti TB Agent. PLoS ONE. 2017;12:e0176088. doi: 10.1371/journal.pone.0176088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hou X.M., Wang C.Y., Gerwick W.H., Shao C.L. Marine Natural Products as Potential Anti-Tubercular Agents. Eur. J. Med. Chem. 2019;165:273–292. doi: 10.1016/j.ejmech.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 160.Lago J.H.G., Toledo-Arruda A.C., Mernak M., Barrosa K.H., Martins M.A., Tibério I.F.L.C., Prado C.M. Structure-Activity Association of Flavonoids in Lung Diseases. Molecules. 2014;19:3570–3595. doi: 10.3390/molecules19033570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Shi P., Silva M.C., Wang H.Y.L., Wu B., Akhmedov N.G., Li M., Beuning P.J., O’Doherty G.A. Structure–Activity Study of the Cleistriosides and Cleistetrosides for Antibacterial/Anticancer Activity. ACS Med. Chem. Lett. 2012;3:1086. doi: 10.1021/ml300303g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Tanaka H., Morinaga O., Uto T., Fuji S., Aboagye F.A., Tung N.H., Li X.W., Putalun W., Shoyama Y. Application of Monoclonal Antibodies against Bioactive Natural Products: Eastern Blotting and Preparation of Knockout Extract. Int. J. Anal. Chem. 2012;2012:1–10. doi: 10.1155/2012/260425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Obakiro S.B., Kiprop A., K’Owino I., Andima M., Owor R.O., Chacha R., Kigondu E. Phytochemical, Cytotoxicity, and Antimycobacterial Activity Evaluation of Extracts and Compounds from the Stem Bark of Albizia coriaria Welw Ex. Oliver. Evid.-Based Complementary Altern. Med. 2022;2022:7148511. doi: 10.1155/2022/7148511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Guan Y., Li F.F., Hong L., Yan X.F., Tan G.L., He J.S., Dong X.W., Bao M.J., Xie Q.M. Protective Effects of Liquiritin Apioside on Cigarette Smoke-Induced Lung Epithelial Cell Injury. Fundam. Clin. Pharmacol. 2012;26:473–483. doi: 10.1111/j.1472-8206.2011.00956.x. [DOI] [PubMed] [Google Scholar]
- 165.Suleimen Y.M., Jose R.A., Suleimen R.N., Ishmuratova M.Y., Toppet S., Dehaen W., Alsfouk A.A., Elkaeed E.B., Eissa I.H., Metwaly A.M. Isolation and In Silico SARS-CoV-2 Main Protease Inhibition Potential of Jusan Coumarin, a New Dicoumarin from Artemisia glauca. Molecules. 2022;27:2281. doi: 10.3390/molecules27072281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.El-Demerdash A., Al-Karmalawy A.A., Abdel-Aziz T.M., Elhady S.S., Darwish K.M., Hassan A.H.E. Investigating the Structure–Activity Relationship of Marine Natural Polyketides as Promising SARS-CoV-2 Main Protease Inhibitors. RSC Adv. 2021;11:31339–31363. doi: 10.1039/D1RA05817G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Coutinho M.A.S., Muzitano M.F., Costa S.S. Flavonoids: Potential Therapeutic Agents for the Inflammatory Process. Rev. Virtual Química. 2009;1:241–256. doi: 10.5935/1984-6835.20090024. [DOI] [Google Scholar]
- 168.van Cong P., Anh H.L.T., Trung N.Q., Quang Minh B., Viet Duc N., van Dan N., Trang N.M., Phong N.V., Vinh L.B., Anh L.T., et al. Isolation, Structural Elucidation and Molecular Docking Studies against SARS-CoV-2 Main Protease of New Stigmastane-Type Steroidal Glucosides Isolated from the Whole Plants of Vernonia gratiosa. Nat. Prod. Res. 2022:1–9. doi: 10.1080/14786419.2022.2042534. [DOI] [PubMed] [Google Scholar]
- 169.Delclaux C., Azoulay E. Inflammatory Response to Infectious Pulmonary Injury. Eur. Respir. J. 2003;22:10s–14s. doi: 10.1183/09031936.03.00420203. [DOI] [PubMed] [Google Scholar]
- 170.Santana F.P.R., Pinheiro N.M., Mernak M.I.B., Righetti R.F., Martins M.A., Lago J.H.G., Lopes F.D.T.Q.D.S., Tibério I.F.L.C., Prado C.M. Evidences of Herbal Medicine-Derived Natural Products Effects in Inflammatory Lung Diseases. Mediat. Inflamm. 2016;2016:2348968. doi: 10.1155/2016/2348968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Timalsina D., Pokhrel K.P., Bhusal D. Pharmacologic Activities of Plant-Derived Natural Products on Respiratory Diseases and Inflammations. BioMed Res. Int. 2021;2021:1636816. doi: 10.1155/2021/1636816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Gong J.H., Cho I.H., Shin D., Han S.Y., Park S.H., Kang Y.H. Inhibition of Airway Epithelial-to-Mesenchymal Transition and Fibrosis by Kaempferol in Endotoxin-Induced Epithelial Cells and Ovalbumin-Sensitized Mice. Lab. Investig. 2013;94:297–308. doi: 10.1038/labinvest.2013.137. [DOI] [PubMed] [Google Scholar]
- 173.Wang C., Zhou J., Wang J., Li S., Fukunaga A., Yodoi J., Tian H. Progress in the Mechanism and Targeted Drug Therapy for COPD. Signal Transduct. Target. Ther. 2020;5:248. doi: 10.1038/s41392-020-00345-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Bansal S., Chhibber S. Curcumin Alone and in Combination with Augmentin Protects against Pulmonary Inflammation and Acute Lung Injury Generated during Klebsiella pneumoniae B5055-Induced Lung Infection in BALB/c Mice. J. Med. Microbiol. 2010;59:429–437. doi: 10.1099/jmm.0.016873-0. [DOI] [PubMed] [Google Scholar]
- 175.Yoon J.H., Baek S.J. Molecular Targets of Dietary Polyphenols with Anti-Inflammatory Properties. Yonsei Med. J. 2005;46:585–596. doi: 10.3349/ymj.2005.46.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Santangelo C., Scazzocchio B., Filesi C. Polyphenols, Intracellular Signalling and Inflammation. Ann.-Ist. Super. Di Sanita. 2007;43:394–405. [PubMed] [Google Scholar]
- 177.Park J.Y., Ko J.A., Kim D.W., Kim Y.M., Kwon H.J., Jeong H.J., Kim C.Y., Park K.H., Lee W.S., Ryu Y.B. Chalcones Isolated from Angelica Keiskei Inhibit Cysteine Proteases of SARS-CoV. J. Enzym. Inhib. Med. Chem. 2016;31:23–30. doi: 10.3109/14756366.2014.1003215. [DOI] [PubMed] [Google Scholar]
- 178.Goc A., Sumera W., Rath M., Niedzwiecki A. Phenolic Compounds Disrupt Spike-Mediated Receptor-Binding and Entry of SARS-CoV-2 Pseudo-Virions. PLoS ONE. 2021;16:e0253489. doi: 10.1371/journal.pone.0253489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Dorsch W., Wagner H. New Antiasthmatic Drugs from Traditional Medicine? Int. Arch. Allergy Appl. Immunol. 1991;94:262–265. doi: 10.1159/000235378. [DOI] [PubMed] [Google Scholar]
- 180.Liu C., Yang N., Song Y., Wang L., Zi J., Zhang S., Dunkin D., Busse P., Weir D., Tversky J., et al. Ganoderic Acid C1 Isolated from the Anti-Asthma Formula, ASHMITM Suppresses TNF-α Production by Mouse Macrophages and Peripheral Blood Mononuclear Cells from Asthma Patients. Int. Immunopharmacol. 2015;27:224–231. doi: 10.1016/j.intimp.2015.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Liu C., Dunkin D., Lai J., Song Y., Ceballos C., Benkov K., Li X.M. Anti-Inflammatory Effects of Ganoderma lucidum Triterpenoid in Human Crohn’s Disease Associated with Downregulation of NF-ΚB Signaling. Inflamm. Bowel Dis. 2015;21:1918–1925. doi: 10.1097/MIB.0000000000000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Shi Q., Liu Z., Yang Y., Geng P., Zhu Y.Y., Zhang Q., Bai F., Bai G. Identification of Anti-Asthmatic Compounds in Pericarpium citri reticulatae and Evaluation of Their Synergistic Effects. Acta Pharmacol. Sin. 2009;30:567–575. doi: 10.1038/aps.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Greiner J.F.W., Müller J., Zeuner M.T., Hauser S., Seidel T., Klenke C., Grunwald L.M., Schomann T., Widera D., Sudhoff H., et al. 1,8-Cineol Inhibits Nuclear Translocation of NF-ΚB P65 and NF-ΚB-Dependent Transcriptional Activity. Biochim. Et Biophys. Acta (BBA)-Mol. Cell Res. 2013;1833:2866–2878. doi: 10.1016/j.bbamcr.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 184.Ryu H.W., Lee S.U., Lee S., Song H.H., Son T.H., Kim Y.U., Yuk H.J., Ro H., Lee C.K., Hong S.T., et al. 3-Methoxy-Catalposide Inhibits Inflammatory Effects in Lipopolysaccharide-Stimulated RAW264.7 Macrophages. Cytokine. 2017;91:57–64. doi: 10.1016/j.cyto.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 185.Mair C.E., Grienke U., Wilhelm A., Urban E., Zehl M., Schmidtke M., Rollinger J.M. Anti-Influenza Triterpene Saponins from the Bark of Burkea africana. J. Nat. Prod. 2018;81:515–523. doi: 10.1021/acs.jnatprod.7b00774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Alagar Yadav S. A Review on Phytoconstituents against Asthma. Int. J. Pharm. Sci. Rev. Res. 2015;30:7–16. [Google Scholar]
- 187.Chiou S.Y., Sung J.M., Huang P.W., Lin S.D. Antioxidant, Antidiabetic, and Antihypertensive Properties of Echinacea Purpurea Flower Extract and Caffeic Acid Derivatives Using In Vitro Models. J. Med. Food. 2017;20:171–179. doi: 10.1089/jmf.2016.3790. [DOI] [PubMed] [Google Scholar]
- 188.Zhang Z., Ma J., Zhu L., Zhao Y. Synthesis and Identification of Cytotoxic Diphyllin Glycosides as Vacuolar H+-ATPase Inhibitors. Eur. J. Med. Chem. 2014;82:466–471. doi: 10.1016/j.ejmech.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 189.Pan S., Cai H., Gu L., Cao S. Cleistanthin A Inhibits the Invasion and Metastasis of Human Melanoma Cells by Inhibiting the Expression of Matrix Metallopeptidase-2 and-9. Oncol. Lett. 2017;14:6217–6223. doi: 10.3892/ol.2017.6917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Park J.Y., Kim J.H., Kim Y.M., Jeong H.J., Kim D.W., Park K.H., Kwon H.J., Park S.J., Lee W.S., Ryu Y.B. Tanshinones as Selective and Slow-Binding Inhibitors for SARS-CoV Cysteine Proteases. Bioorg. Med. Chem. 2012;20:5928–5935. doi: 10.1016/j.bmc.2012.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Magro M., Campos R., Baratella D., Ferreira M.I., Bonaiuto E., Corraducci V., Uliana M.R., Lima G.P.P., Santagata S., Sambo P., et al. Magnetic Purification of Curcumin from Curcuma Longa Rhizome by Novel Naked Maghemite Nanoparticles. J. Agric. Food Chem. 2015;63:912–920. doi: 10.1021/jf504624u. [DOI] [PubMed] [Google Scholar]
- 192.Alikiaii B., Bagherniya M., Askari G., Sathyapalan T., Sahebkar A. Evaluation of the Effect of Curcumin on Pneumonia: A Systematic Review of Preclinical Studies. Phytother. Res. 2021;35:1939–1952. doi: 10.1002/ptr.6939. [DOI] [PubMed] [Google Scholar]
- 193.Su P.S., Doerksen R.J., Chen S.H., Sung W.C., Juan C.C., Rawendra R.D.S., Chen C.R., Li J.W., Aisha, Huang T.C., et al. Screening and Profiling Stilbene-Type Natural Products with Angiotensin-Converting Enzyme Inhibitory Activity from Ampelopsis Brevipedunculata Var. Hancei (Planch.) Rehder. J. Pharm. Biomed. Anal. 2015;108:70–77. doi: 10.1016/j.jpba.2015.01.053. [DOI] [PubMed] [Google Scholar]
- 194.Lee C.L., Chiang L.C., Cheng L.H., Liaw C.C., Abd El-Razek M.H., Chang F.R., Wu Y.C. Influenza A (H(1)N(1)) Antiviral and Cytotoxic Agents from Ferula assa-foetida. J. Nat. Prod. 2009;72:1568–1572. doi: 10.1021/np900158f. [DOI] [PubMed] [Google Scholar]
- 195.Yu M.S., Lee J., Lee J.M., Kim Y., Chin Y.W., Jee J.G., Keum Y.S., Jeong Y.J. Identification of Myricetin and Scutellarein as Novel Chemical Inhibitors of the SARS Coronavirus Helicase, NsP13. Bioorg. Med. Chem. Lett. 2012;22:4049–4054. doi: 10.1016/j.bmcl.2012.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Miean K.H., Mohamed S. Flavonoid (Myricetin, Quercetin, Kaempferol, Luteolin, and Apigenin) Content of Edible Tropical Plants. J. Agric. Food Chem. 2001;49:3106–3112. doi: 10.1021/jf000892m. [DOI] [PubMed] [Google Scholar]
- 197.Yi L., Li Z., Yuan K., Qu X., Chen J., Wang G., Zhang H., Luo H., Zhu L., Jiang P., et al. Small Molecules Blocking the Entry of Severe Acute Respiratory Syndrome Coronavirus into Host Cells. J. Virol. 2004;78:11334–11339. doi: 10.1128/JVI.78.20.11334-11339.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Najmi A., Javed S.A., al Bratty M., Alhazmi H.A. Modern Approaches in the Discovery and Development of Plant-Based Natural Products and Their Analogues as Potential Therapeutic Agents. Molecules. 2022;27:349. doi: 10.3390/molecules27020349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Tyson R.J., Park C.C., Powell J.R., Patterson J.H., Weiner D., Watkins P.B., Gonzalez D. Precision Dosing Priority Criteria: Drug, Disease, and Patient Population Variables. Front. Pharmacol. 2020;11:420. doi: 10.3389/fphar.2020.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Chaccour C., Abizanda G., Irigoyen-Barrio Á., Casellas A., Aldaz A., Martínez-Galán F., Hammann F., Gil A.G. Nebulized Ivermectin for COVID-19 and Other Respiratory Diseases, a Proof of Concept, Dose-Ranging Study in Rats. Sci. Rep. 2020;10:17073. doi: 10.1038/s41598-020-74084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., Rodriguez-Torres M.D.P., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S., et al. Nano Based Drug Delivery Systems: Recent Developments and Future Prospects. J. Nanobiotechnol. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]