Microcystic adnexal carcinoma (original) (raw)
Skin nonmelanocytic tumor
Adnexal tumors
Sweat gland derived (apocrine & eccrine glands)
Microcystic adnexal carcinoma
Last author update: 12 March 2024
Last staff update: 12 March 2024
Copyright: 2002-2025, PathologyOutlines.com, Inc.
PubMed Search: Microcystic adnexal carcinoma
Page views in 2024: 17,227
Page views in 2025 to date: 797
Cite this page: Cullison C, Rohr BR. Microcystic adnexal carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticsclerosingsweatductcarcinoma.html. Accessed January 16th, 2025.
Definition / general
- Microcystic adnexal carcinoma is a rare malignant adnexal tumor with sweat duct and follicular differentiation
Essential features
- Malignant adnexal carcinoma with sweat duct and follicular differentiation
- Most commonly occurs on the face of elderly White patients
- Histopathology shows deep tumor extension with perineural invasion and may show the presence of lymphoid aggregates
- Tumors may be locally aggressive and Mohs micrographic surgery is the mainstay of treatment
Terminology
- Sclerosing sweat duct carcinoma
- Malignant syringoma
- Sweat gland carcinoma with syringomatous features
- Locally aggressive adnexal carcinoma
- Reference: Mod Pathol 2008;21:178
ICD coding
- ICD-10: C44.9 - other and unspecified malignant neoplasm of skin, unspecified
- ICD-11
Epidemiology
- Most common in White patients
- Median age: 68 years old
- Possible associations
- Prior radiation
- Immunosuppressed states
- Ultraviolet (UV) exposure
- References: JAMA Dermatol 2019;155:1059, Am J Clin Oncol 2010;33:125, Dermatol Surg 2000;26:531, Mod Pathol 2020;33:1092, J Cutan Pathol 1999;26:48, Mil Med 2019;184:948
Sites
- Left side of the face in U.S. population
- Face, particularly on the lips, perioral, nasolabial, periorbital regions
- Uncommon: axilla, trunk, extremities, genitalia
- References: Arch Dermatol 2000;136:1355, JAMA Dermatol 2019;155:1059
Pathophysiology
- Mutations
- No signature mutation to date
- TP53 is the most common mutation (22%)
- JAK1 (17%)
- Other oncogenes (JAK2, MAF, MAFB, JUN, FGFR1)
- Individual cases may harbor ultraviolet pattern of mutations
- References: Mod Pathol 2020;33:1092, JAMA Dermatol 2019;155:1059
Etiology
- Largely unknown at this time
- Some cases associated with prior radiation, both ultraviolet and therapeutic
- References: Mod Pathol 2020;33:1092, JAMA Dermatol 2019;155:1059
Clinical features
- Firm, yellow or flesh colored papule, plaque or nodule
- Mean size at diagnosis: 2.8 cm
- Rarely metastasizes
- Reference: JAMA Dermatol 2019;155:1059
Diagnosis
- Skin biopsy that obtains adequate tissue depth (i.e., punch, incisional, excisional) (JAMA Dermatol 2019;155:1059)
Prognostic factors
- Proposed adverse prognostic factors (Dermatol Surg 2004;30:957, J Am Acad Dermatol 2018;79:756)
- Perineural invasion
- Regional lymph node metastasis
- Visceral metastasis
- Tumor recurrence
Case reports
- 46 year old woman with microcystic adnexal carcinoma of the left upper eyelid (Medicine (Baltimore) 2023;102:e34709)
- 54 year old woman with a medical history of liver transplantation (JAAD Case Rep 2020;10:126)
- 55 year old man with microcystic adnexal carcinoma of the right heel (Ann Dermatol 2023;35:S215)
- 83 year old man with microcystic adnexal carcinoma colliding with squamous cell carcinoma (JAAD Case Rep 2020;6:479)
- 83 year old woman with microcystic adnexal carcinoma treated with radiation therapy (SAGE Open Med Case Rep 2020;8:2050313X20953114)
- 86 year old woman with microcystic adnexal carcinoma of the vulvar region (JAAD Case Rep 2023;38:72)
Treatment
- Mohs micrographic surgery
- Radiation therapy can be considered when surgery is not feasible
- Imaging is not routinely recommended
- References: JAMA Dermatol 2019;155:1059, Arch Dermatol 2000;136:1355, Cancer Radiother 2023;27:349
Clinical images
Images hosted on other servers:
White, irregular papule
Multiple yellow papulonodules
Pink and yellow plaque
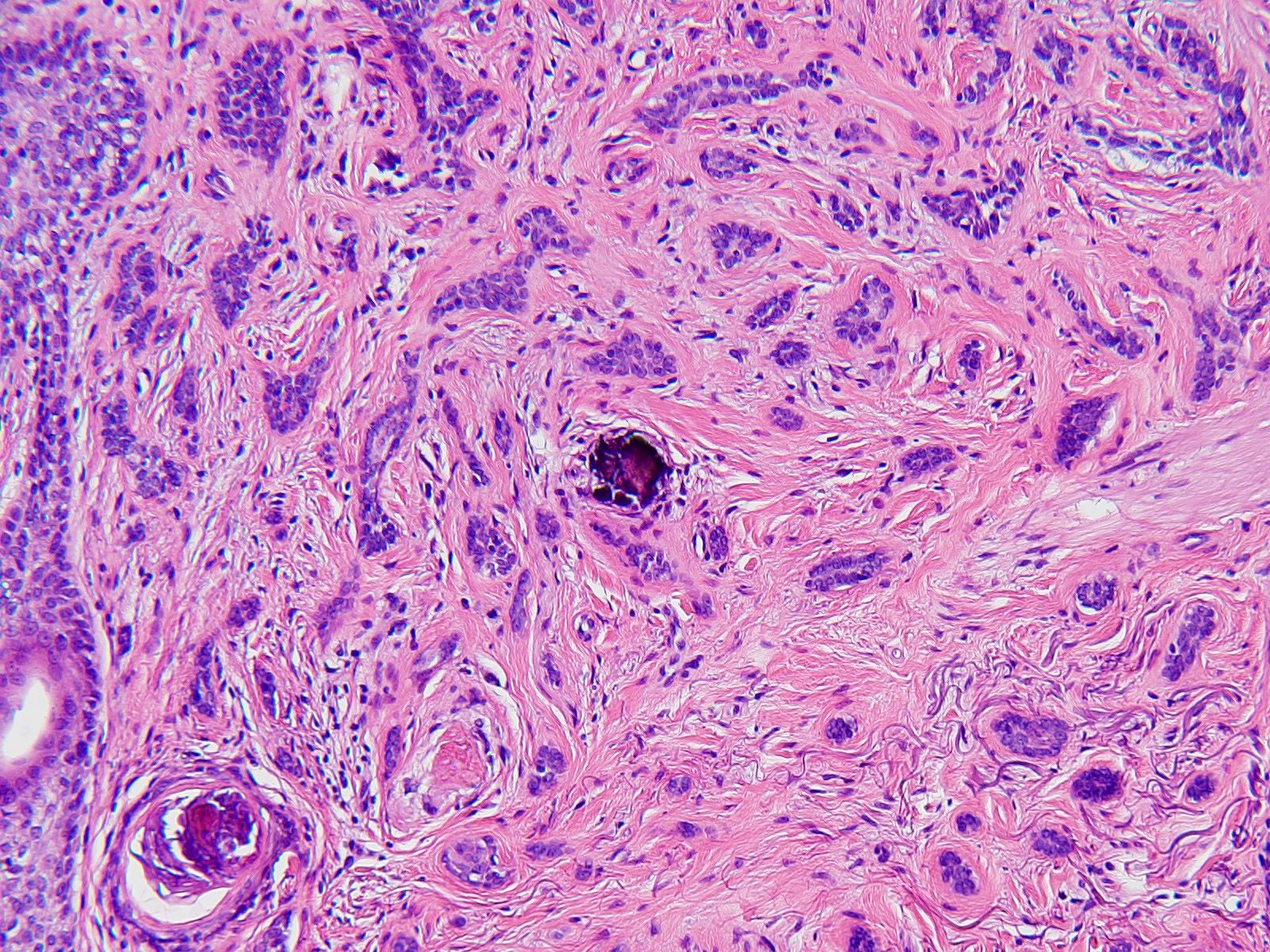
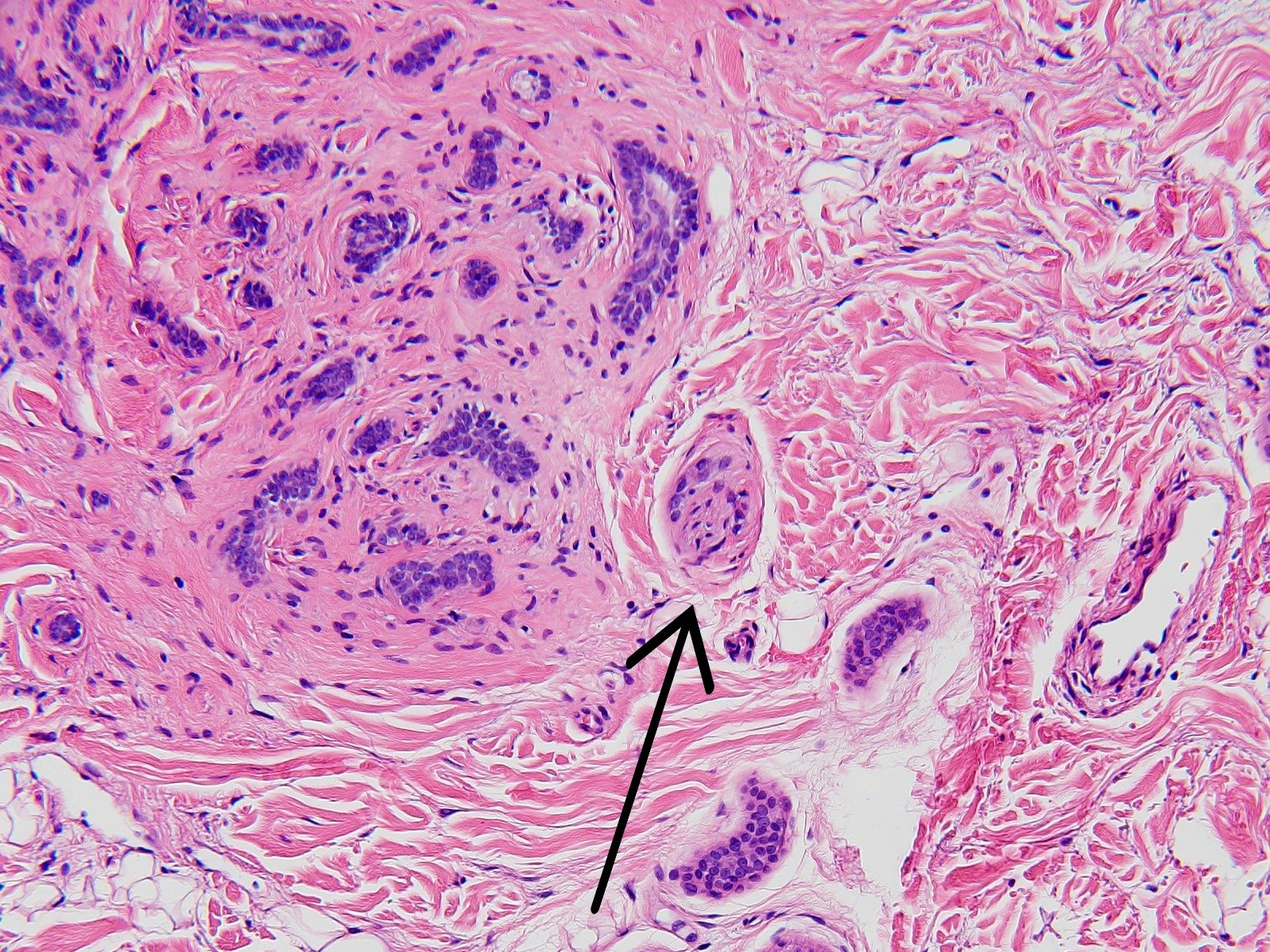
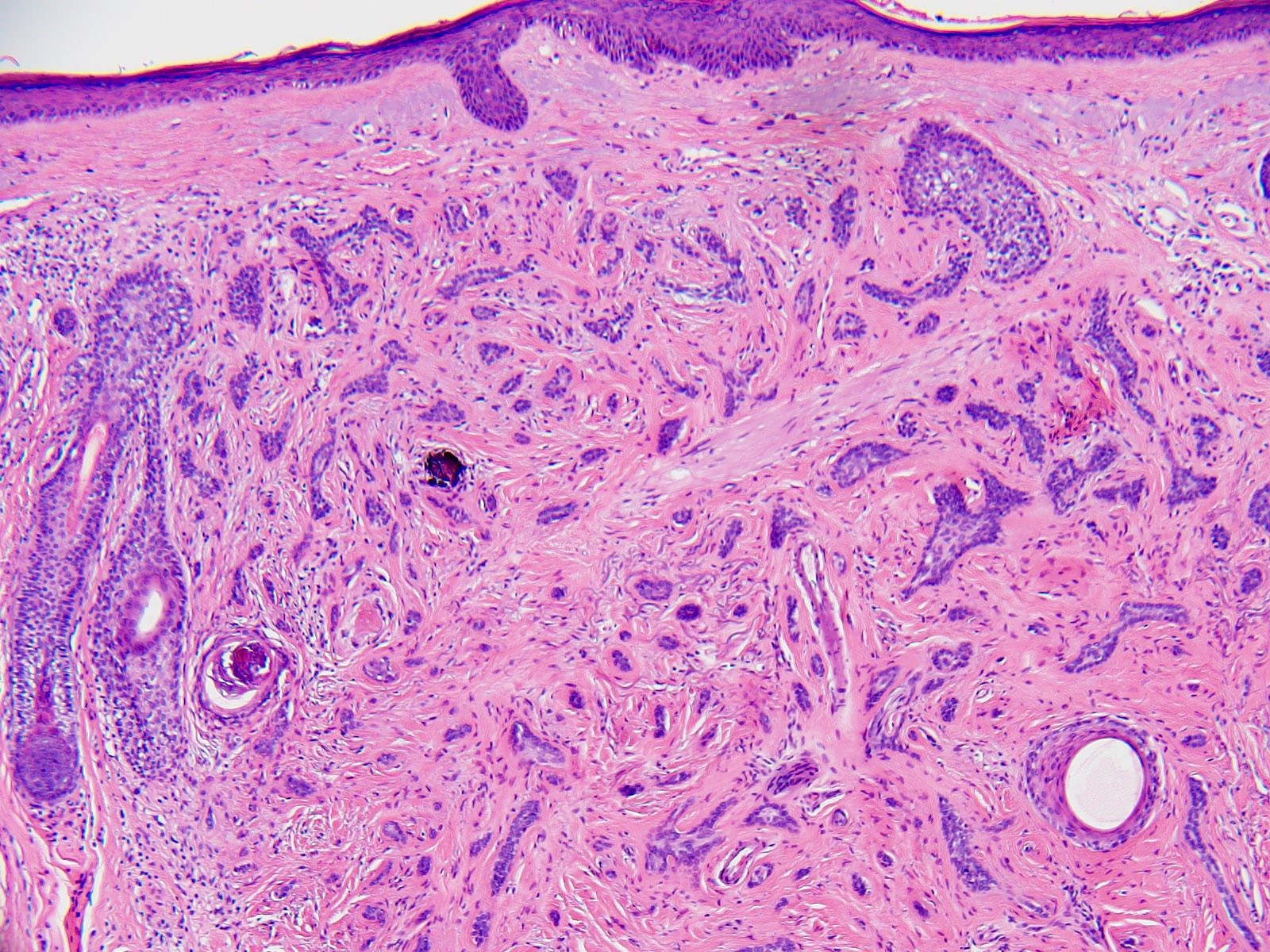
Microscopic (histologic) description
- Features of both eccrine and follicular differentiation
- Poorly circumscribed and deeply infiltrating
- Extension into the subcutaneous adipose tissue and skeletal muscle
- Superficial pseudohorn cysts containing lamellar keratin
- Small aggregates of epithelioid cells with curved and angulated shapes, sometimes referred to as having a tadpole-like morphology
- Deeper components typically have smaller tumor aggregates and can be a single cell layer thick
- Some islands of tumor cells will show ductal differentiation with luminal centers lined by a pink cuticle
- Dense fibrous stroma consisting of thick collagen bundles that surround the tumor aggregates
- Mild cytologic atypia with often bland appearing cells characterized by monomorphic nuclei and scant cytoplasm
- Lymphoid aggregates adjacent to or in association with tumor
- Incidental calcifications can be present
- Mitotic figures are often absent
- Perineural invasion is a common feature
- References: Mod Pathol 2008;21:178, Mod Pathol 2006;19:S93
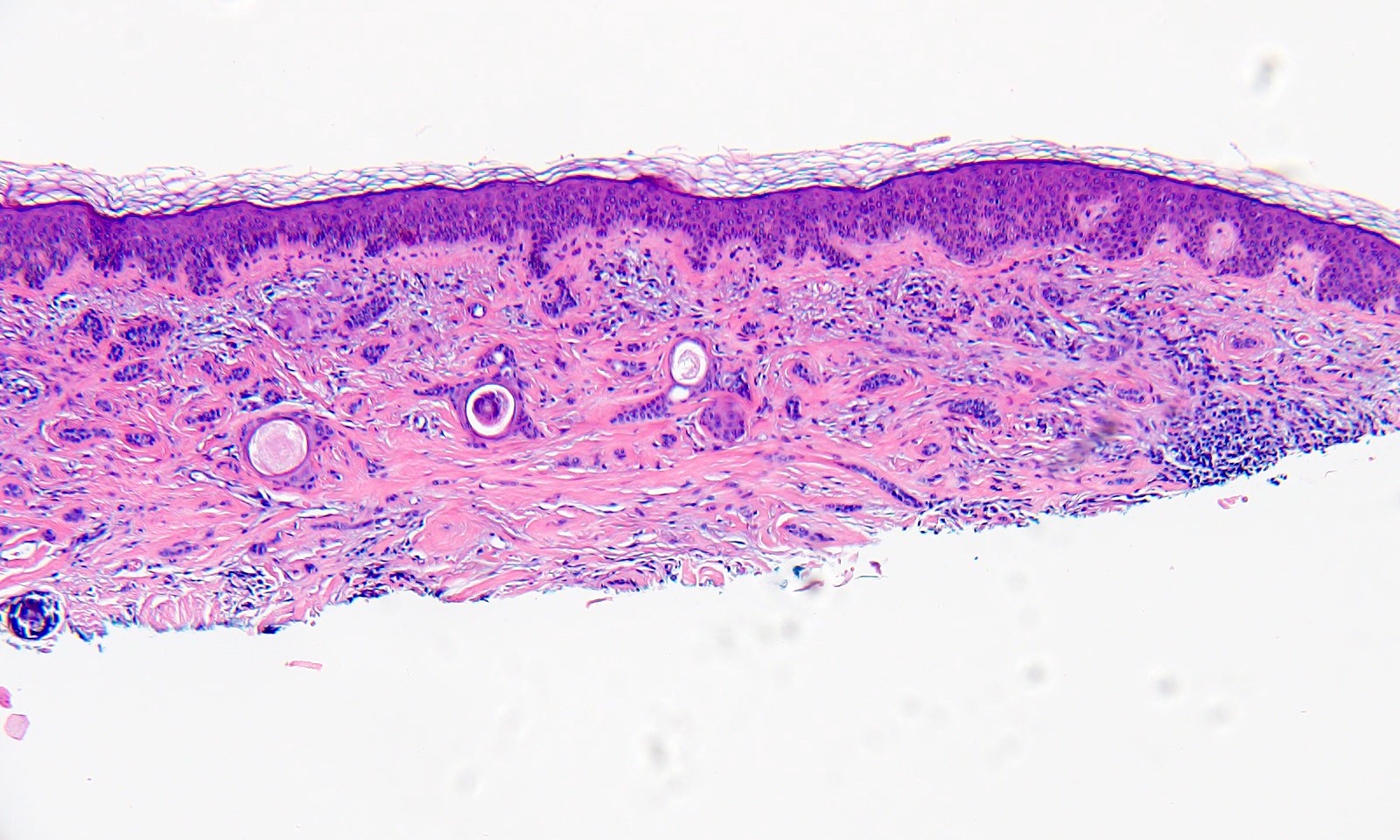
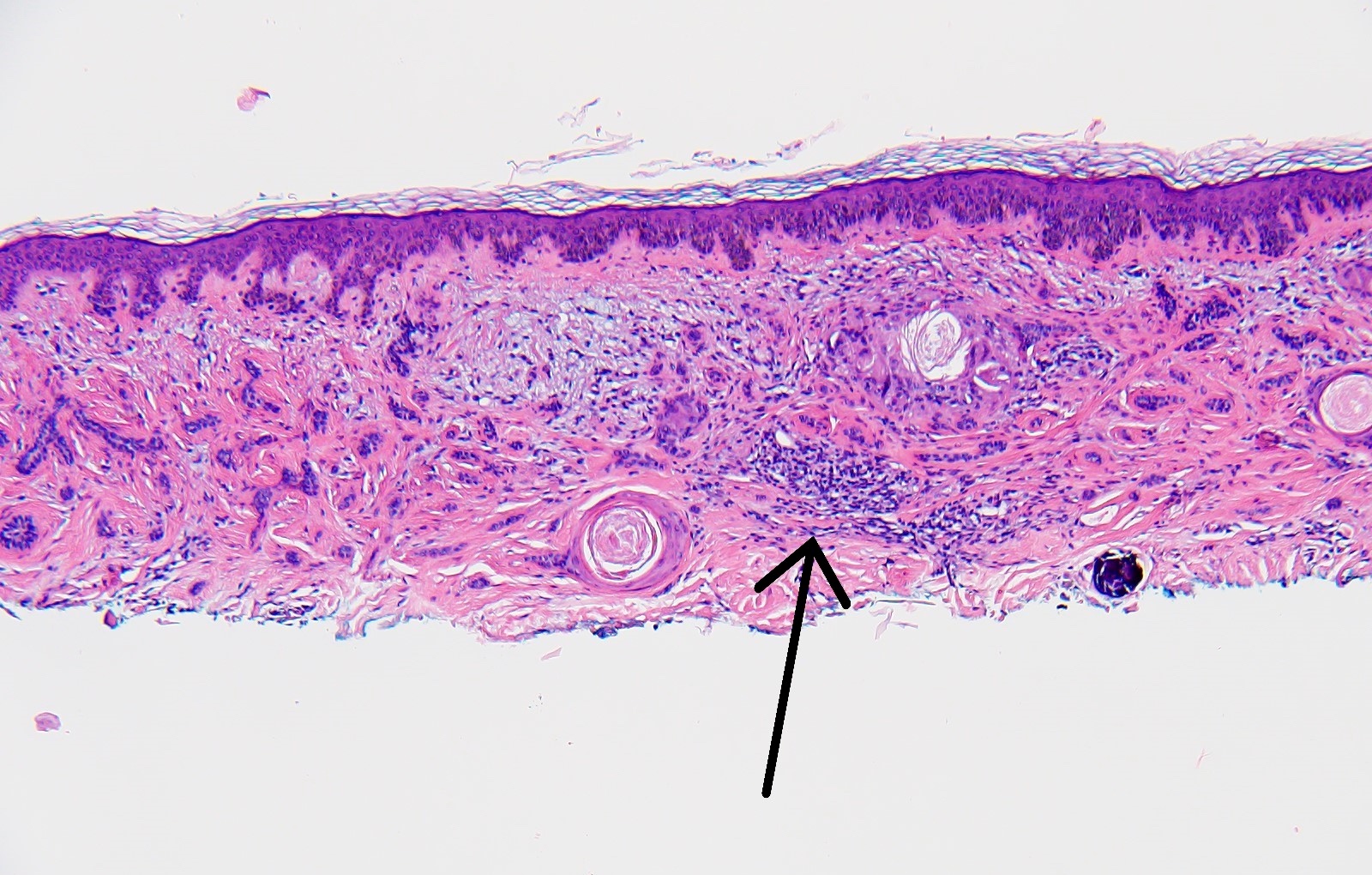
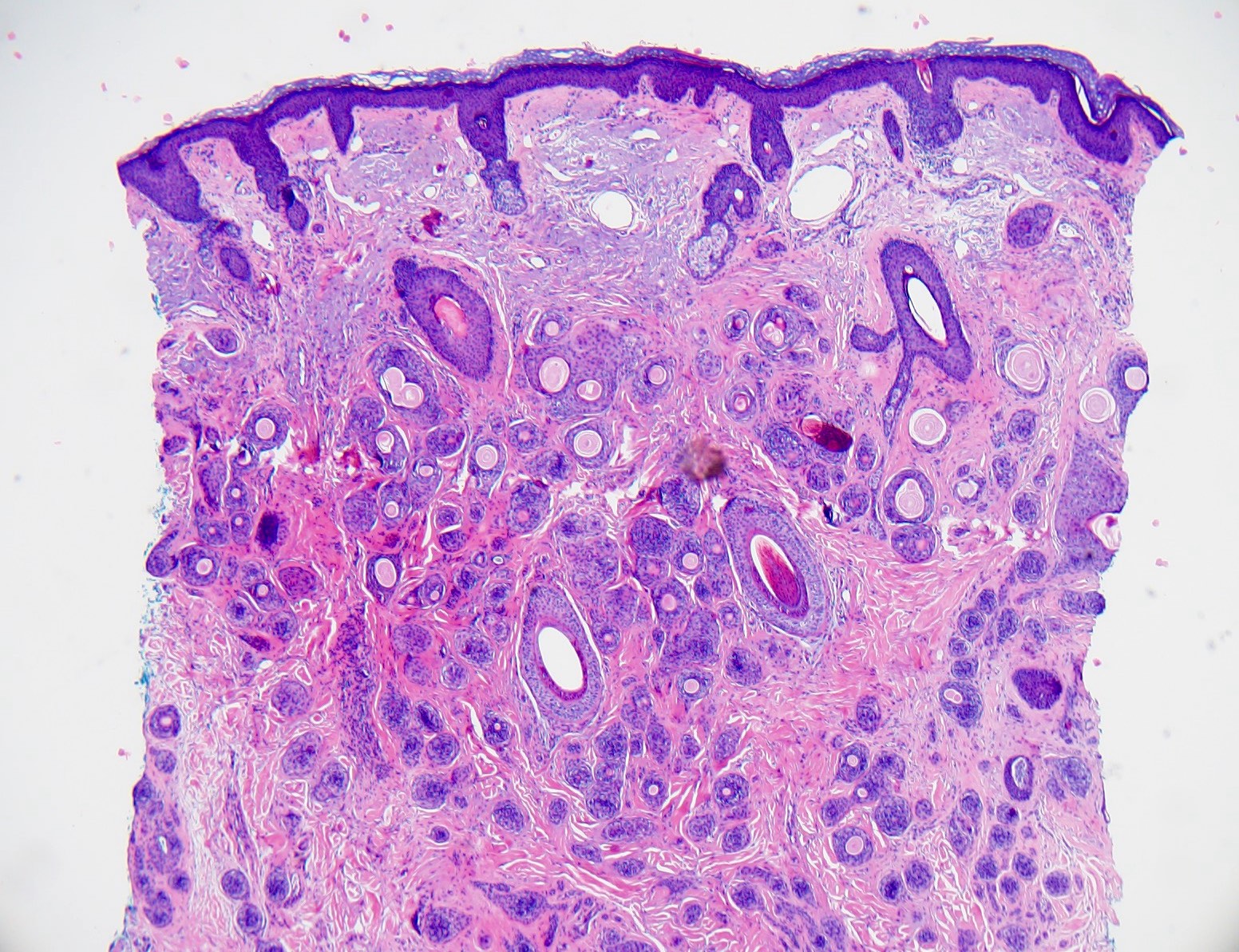
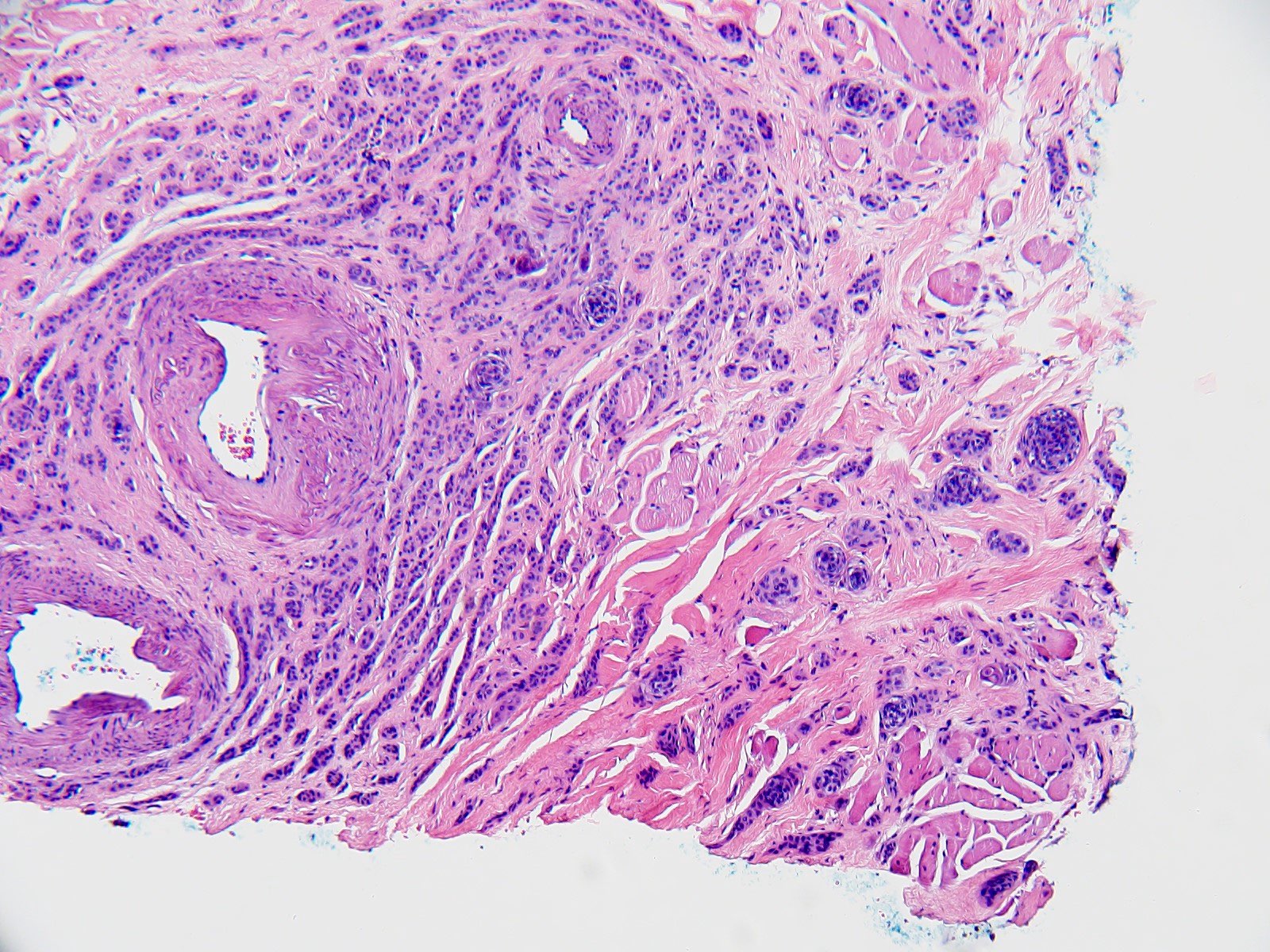
Microscopic (histologic) images
Contributed by Christopher Cullison, M.D. and Bethany R. Rohr, M.D.
Jagged tumor islands
Lymphoid aggregate
Follicular and ductal differentiation
Skeletal muscle invasion
Incidental calcification
Perineural invasion
Virtual slides
Images hosted on other servers:
Deeply invasive tumor islands
Videos
Microcystic adnexal carcinoma by Dr. Jerad Gardner
Differential diagnosis
- Skin, left cheek, punch biopsy:
- Microcystic adnexal carcinoma (see comment)
- Comment: The sections reveal a deeply infiltrating carcinoma with ductal and follicular differentiation. There are surrounding lymphoid aggregates and focal perineural invasion.
Differential diagnosis
- Desmoplastic trichoepithelioma:
- Not deeply invasive
- Central dell
- Rare reports of perineural invasion (J Cutan Pathol 2012;39:317)
- CK20 positive Merkel cells retained (J Cutan Pathol 2008;35:174)
- Median age: 52 years (J Am Acad Dermatol 2010;62:102)
- CK19 negative (22 - 57%)
- Morpheaform basal cell carcinoma (J Clin Pathol 2007;60:145):
- Syringoma (J Clin Pathol 2007;60:145):
- Lacks horn cysts
- Clear cell variant
- Not deeply invasive
- No perineural invasion
- Typically located on eyelids (unless eruptive)
Board review style question #1
Which immunohistochemical stain is likely to be positive in the tumor shown above?
- AR
- CK19
- CK20
- S100
Board review style answer #1
B. CK19. CK19 has a cytoplasmic staining pattern for eccrine glands and stains positive in 70 - 100% of microcystic adnexal carcinomas. Answer A is incorrect because androgen receptor does not stain positive in microcystic adnexal carcinoma; rather, it typically stains sebaceous glands and apocrine glands. Answer C is incorrect because CK20 is a stain for Merkel cells that is typically lost in microcystic adnexal carcinoma. Answer D is incorrect because S100 is not expressed in microcystic adnexal carcinomas.
Reference: Microcystic adnexal carcinoma
Board review style question #2
Microcystic adnexal carcinoma is most likely to have which of the following findings at diagnosis?
- Angiolymphatic invasion
- Distant organ metastasis
- Lymph node metastasis
- Perineural invasion
Board review style answer #2
D. Perineural invasion. Perineural involvement is a common feature in microcystic adnexal carcinomas. Answers A - C are incorrect because metastasis of microcystic adnexal carcinoma is exceedingly uncommon and is not reported to have angioinvasion on pathology.
Reference: Microcystic adnexal carcinoma
Board review style question #3
Which of the following features can differentiate microcystic adnexal carcinoma from syringoma and desmoplastic trichoepithelioma?
- Depth of invasion
- Presence of ductal differentiation
- Presence of follicular differentiation
- Sclerotic stroma
Board review style answer #3
A. Depth of invasion. Microcystic adnexal carcinoma typically has a depth of invasion to at least the deep reticular dermis and may invade into subcutaneous structures, including adipose tissue, skeletal muscle or bone. Answer B is incorrect because syringoma will also have presence of ductal differentiation. Answer C is incorrect because desmoplastic trichoepithelioma will also have presence of follicular differentiation. Answer D is incorrect because both syringoma and desmoplastic trichoepithelioma can have a sclerotic stroma.
Reference: Microcystic adnexal carcinoma