Induction of HIV-1 Replication in Latently Infected CD4+ T Cells Using a Combination of Cytokines (original) (raw)
Abstract
Although it has been demonstrated that certain cytokines, particularly proinflammatory cytokines, can enhance ongoing viral replication in peripheral blood mononuclear cells (PBMCs) of HIV-1–infected individuals, it is unclear what role these cytokines play in the induction of HIV-1 replication in latently infected, resting CD4+ T cells. This study demonstrates that the in vitro combination of the proinflammatory cytokines interleukin (IL)-6 and tumor necrosis factor (TNF)-α together with the immunoregulatory cytokine IL-2 are potent inducers of viral replication in highly purified, latently infected, resting CD4+ T cells derived from HIV-infected individuals who are antiretroviral therapy–naive as well as those who are receiving highly active antiretroviral therapy (HAART). Viral replication induced by this combination of cytokines was completely suppressed in the presence of HAART in vitro_._ Given that an array of cytokines, including IL-6, TNF-α, and IL-2, are copiously expressed in the microenvironment of the lymphoid tissues, which harbor the latent viral reservoirs, induction of HIV by this combination of cytokines may in part explain the commonly observed reappearance of detectable plasma viremia in HIV-infected individuals in whom HAART was discontinued. Moreover, since it is likely that these infected cells die upon activation of virus and that HAART prevents spread of virus to adjacent cells, the observation that this combination of cytokines can markedly induce viral replication in this reservoir may have important implications for the activation-mediated diminution of the latent reservoir of HIV in patients receiving HAART.
Keywords: HIV-1, latency, resting CD4+ T cells, cytokines, antiretroviral therapy
Cytokines are important effector molecules in the initiation and propagation of inflammatory and immune responses; in addition, certain cytokines mediate a number of important immunoregulatory functions (1). The role of cytokines in the pathogenesis of HIV disease has been extensively studied (2–5). It has been demonstrated by in vitro experiments that HIV replication in PBMCs of HIV-infected individuals is finely regulated by a variety of endogenous cytokines acting in an autocrine and paracrine manner (5, 6). Cytokine-rich supernatants derived from cultures of PBMCs from normal individuals were first shown to induce the expression of HIV-1 in chronically infected cell lines (7, 8). Subsequently, a variety of individual cytokines, particularly proinflammatory cytokines, were demonstrated to induce HIV expression either endogenously or when added to acutely or chronically infected cell cultures (3, 4, 9). Of these, IL-1, IL-6, and TNF-α have been implicated in the pathogenesis of HIV-1 as direct modulators of virus expression (3, 10–13) and higher levels of these cytokines have been detected in the sera of infected individuals; furthermore, secretion of these cytokines is increased in PBMCs of infected individuals (14–18). For these reasons, selective cytokine inhibitors such as IL-1 receptor antagonist or agents that neutralize TNF-α have been suggested as potential therapeutic strategies aimed at the control of viral replication (13, 19–23).
Recently, a small but detectable reservoir of latently infected, resting CD4+ T cells has been shown to persist in patients receiving highly active antiretroviral therapy (HAART)1 and in whom plasma viremia had fallen to below the level of detectability of commonly used assays (24– 26). The presence of this latent reservoir of HIV is of considerable concern since these cells remain as a potential source of reactivation of viral replication. In this regard, these cells reside predominantly in the microenvironment of lymphoid tissue (27), where endogenous cytokine secretion regularly occurs in response to normal antigenic stimuli (2, 28–32).
In this study, we demonstrate that the in vitro combination of cytokines IL-2, IL-6, and TNF- α has a profound effect on reactivation of HIV-1 replication in latently infected, resting CD4+ T cells both from antiretroviral naive patients and from patients who were receiving HAART and in whom plasma viremia was markedly suppressed, including some patients in whom plasma viremia was below detectable levels. In vitro HAART prevents the spread of virus in cytokine-induced cultures. These findings may explain the reappearance of plasma viremia in patients in whom HAART is discontinued due to drug toxicity or lack of compliance (33). In addition, since cytokines alone can reactivate HIV-1 replication in latently infected, resting CD4+ T cells, and since these cells probably die upon reactivation, it is conceivable that a strategy of administration of cytokines together with HAART might result in a diminution of this reservoir of latently infected cells.
Materials and Methods
Patient Population.
Six HIV-1–seropositive patients who were naive to antiretroviral therapy, and seven patients who were receiving HAART (Table 1) were subjected to apheresis in order to obtain PBMCs according to protocols approved by the National Institute of Allergy and Infectious Diseases and the University of Washington Institutional Review Boards.
Table 1.
Profiles of HIV-1–infected Patients
| Patient | CD4 count | Plasma HIV RNA* | Antiretroviral treatment | Months receiving HAART‡ | Infectious viral load§ |
|---|---|---|---|---|---|
| cells/μl | copies/ml | infectious U/106 cells | |||
| 1 | 520 | 14,394 | NA | NA | 81.7 |
| 2 | 540 | 47,704 | NA | NA | 81.7 |
| 3 | 490 | 10,414 | NA | NA | 8.1 |
| 4 | 324 | 29,216 | NA | NA | 205.8 |
| 5 | 399 | 9,032 | NA | NA | 8.1 |
| 6 | 602 | 12,157 | NA | NA | 40.5 |
| 7 | 638 | 1,330 | AZT, 3TC, Ritonavir | 14.0 | 5.7 |
| 8 | 367 | 2,520 | AZT, 3TC, Indinavir | 15.0 | 40.1 |
| 9 | 1,176 | 1,034 | AZT, 3TC, Indinavir | 1.0 | 3.2 |
| 10 | 648 | <50 | AZT, 3TC, Indinavir | 2.5 | 0.5 |
| 11 | 790 | 343 | AZT, 3TC, Indinavir | 2.8 | 1.6 |
| 12 | 353 | <50 | AZT, 3TC, Indinavir | 18.0 | 0.5 |
| 13 | 689 | <50 | ddI, 3TC, Indinavir | 16.0 | 0.5 |
Isolation of Resting CD4+ T Cells.
Resting CD4+ T cells were isolated from peripheral blood of HIV-1–infected individuals using a combination of magnetic bead depletion and fluorescent activated cell sorting techniques as described previously (27).
Micro Coculture Assay.
To determine the frequency of latently infected, resting CD4+ T cells from patients carrying replication competent HIV-1, micro coculture assays were carried out as described previously (27).
Cytokines and Cell Cultures.
After isolation of resting CD4+T cells from HIV-1–infected individuals, cells (2.0–10 × 106) were incubated with complete medium consisting of RPMI supplemented with 10% FCS, penicillin–streptomycin, and l-glutamine in a tissue culture plate with the following cytokines: IL-2 (100 U/ml; Boehringer Mannheim, Indianapolis, IN), IL-1β (5 ng/ml; R&D Systems, Minneapolis, MN), IL-4 (3 ng/ml; R&D Systems), IL-6 (5 ng/ml; R&D Systems), TNF-α (2.5 ng/ml; R&D Systems), or with the combination of IL-2, IL-6, and TNF-α. Purified resting CD4+ T cells were also incubated with complete medium in the absence of any cytokines as a negative control. As a positive control, the same number of cells were incubated with anti-CD3 antibody (OKT3) in the presence of 2 × 106 irradiated PBMCs from HIV-1–seronegative individuals as feeder cells. To examine the inhibitory role of glucocorticoids in the induction of HIV-1 replication in latently infected, resting CD4+ T cells by cytokines, dexamethasone (10−8 M; Calbiochem, La Jolla, CA) was added to cultures containing the combination of three cytokines or anti-CD3 antibody. Cultures were incubated in a 37°C CO2 incubator for 9 d, and supernatants from each culture were removed on days 3, 6, and 9 for determination of HIV-1 p24 by ELISA (Coulter Corp., Miami, FL). To examine the effects of in vitro antiretroviral agents on the combination of cytokines or anti-CD3 induced viral replication, zidovudine (AZT; 4 μM;Sigma Chemical Co., St. Louis, MO), lamivudine (3TC; 5 μM; gift from Dr. Raymond Schnazi, Emory University, Atlanta, GA), and the protease inhibitor indinavir (10 μM; Merck, Rahway, NJ) were added to the media.
Flow Cytometric Analysis and Cell Proliferation Assays.
To measure cytokine-induced cellular activation in latently infected, resting CD4+ T cells, flow cytometric analysis of the expression of activation markers and thymidine incorporation assays were carried out. Resting CD4+ T cells that had been incubated with various cytokines were stained with PE-conjugated anti-CD25 (Becton Dickinson, San Jose, CA) and PE-conjugated anti–HLA-DR antibodies (Becton Dickinson) along with FITC-conjugated anti-CD4 antibody (Becton Dickinson) 6 d after incubation. On day 6, [3H]thymidine incorporation was measured in resting CD4+ T cells that had been incubated with the above cytokines or with anti-CD3 antibody.
Results
Cytokine-induced Cellular Activation in Latently Infected, Resting CD4+ T Cells.
The replication of HIV-1 is intimately associated with the state of cellular activation of susceptible cell populations (2, 28). In this regard, we first investigated the role of individual cytokines or combinations of cytokines on the activation of highly enriched, resting CD4+ T cells from HIV-1–seropositive patients by examining the expression of cell surface activation markers CD25 and HLA-DR. As shown in Table 2, in the absence of cytokines or any other activating stimuli, purified resting CD4+ T cells from infected individuals expressed no measurable CD25 or HLA-DR on their cell surfaces. After a 6-d incubation in vitro, only IL-2 and IL-4 induced slight increases in activation markers on resting CD4+ T cells. However, the combination of IL-2, IL-6, and TNF-α showed marked increases in CD25 and HLA-DR expression. The induction of cellular activation in purified resting CD4+ T cells by the combination of three cytokines was further confirmed by the cellular incorporation of DNA precursor thymidine (Fig. 1). With the exception of IL-2, which induced a slight degree of cellular proliferation, no individual cytokine resulted in active proliferation of resting CD4+ T cells. Cells stimulated with anti-CD3 antibody showed profound cellular activation as judged by both the expression of activation markers and [3H]thymidine incorporation, confirming that purified resting CD4+T cells are fully capable of undergoing cellular proliferation.
Table 2.
Cytokine-mediated Cellular Activation in Latently Infected, Resting CD4+ T Cells
| Cytokine added | % CD4+/HLA-DR+ | % CD4+/CD25+ | |
|---|---|---|---|
| Day 0 | No cytokine | 0.7 | 0.0 |
| Day 6 | No cytokine | 1.0 | 1.2 |
| IL-1β | 0.8 | 0.9 | |
| IL-2 | 5.7 | 3.3 | |
| IL-4 | 3.2 | 5.0 | |
| IL-6 | 1.5 | 1.0 | |
| TNF-α | 0.5 | 0.4 | |
| IL-2/IL-6/TNF-α | 23.7 | 8.3 | |
| anti-CD3-stimulated | 50.6 | 92.2 |
Figure 1.
Cytokine-induced cellular proliferation in latently infected, resting CD4+ T cells. Highly enriched (>99%) resting CD4+ T cells from one HIV-1–seronegative and two HIV-1–infected individuals were incubated with the indicated individual cytokines, a combination of cytokines, or anti-CD3 antibody for 6 d, and [3H]thymidine incorporation by 104 resting CD4+ T cells was measured. A representative set of results from patient no. 2 is shown.
Induction of HIV-1 Replication by the Combination of IL-2, IL-6, and TNF-α in Latently Infected, Resting CD4+ T Cells from Antiretroviral Drug–naive Patients.
Given the fact that the combination of IL-2, IL-6, and TNF-α potently activates resting CD4+ T cells as described above, we first examined the inducibility of replication-competent HIV-1 in latently infected, resting CD4+ T cells from antiretroviral therapy–naive, HIV-1–seropositive individuals using individual cytokines and combinations of cytokines in vitro. Despite the fact that highly purified, resting CD4+ T cells from all patients carried replication-competent HIV-1 with a frequency determined by micro coculture assay ranging from 8.1 to 205.8 infectious units per 106 resting CD4+T cells (Table 1), measurable p24 was not detected in cultures containing neither cytokines nor anti-CD3 antibody throughout the entire incubation period (Fig. 2). Among the individual cytokines, only IL-2 had a slight effect on the induction of HIV-1 expression in latently infected, resting CD4+ T cells (Fig. 2). However, cultures incubated with the combination of IL-2, IL-6, and TNF-α had a dramatic increase in HIV-1 replication. The level of viral production induced by this cytokine combination was equivalent to that of cells stimulated with anti-CD3 antibody. When a combination of three antiretroviral drugs was added to the cultures incubated with the three cytokine combination or with anti-CD3 antibody, viral replication was completely suppressed as shown in Fig. 2.
Figure 2.
Induction of HIV-1 replication by the combination of IL-2, IL-6, and TNF-α in latently infected, resting CD4+ T cells from antiretroviral drug–naive patients. Resting CD4+ T cells from infected patients were isolated and further incubated with no cytokine, individual cytokines as indicated, the combination of IL-2, IL-6, and TNF-α, or anti-CD3 antibody with irradiated PBMCs from HIV-1–seronegative individuals. In addition, cells were incubated with the combination of IL-2, IL-6, and TNF-α or anti-CD3 antibody in the presence of three drugs (AZT, 3TC, and Indinavir; see Materials and Methods). Supernatants from each culture were removed on days 3, 6, and 9, and HIV-1 p24 was measured by ELISA.
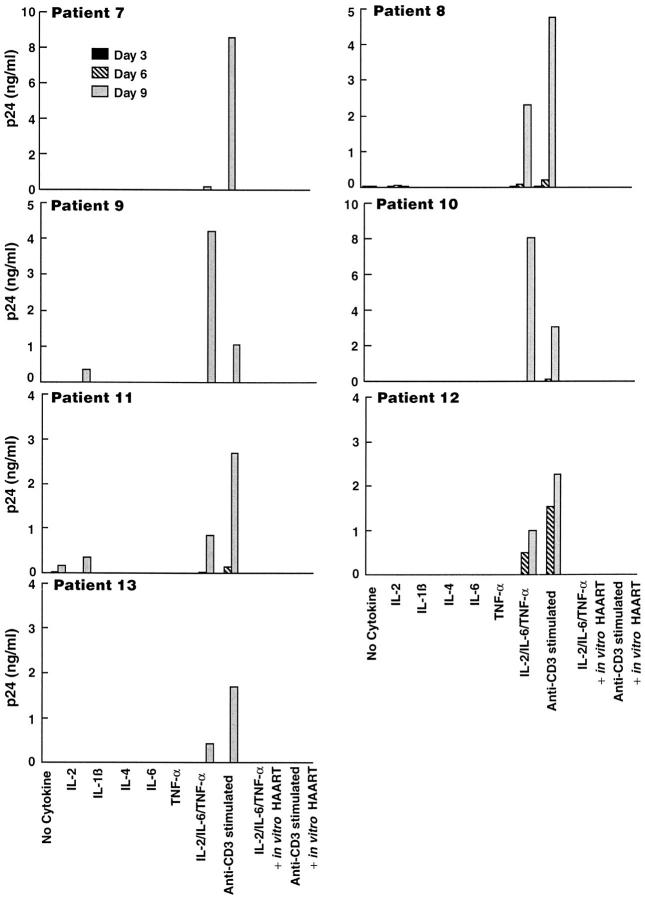
Induction of HIV-1 Replication by the Combination of IL-2, IL-6, and TNF-α in Latently Infected, Resting CD4+ T cells from Patients Receiving HAART.
We and others have recently reported that HIV-1–infected individuals receiving HAART for prolonged periods of time with no detectable plasma viremia carry a small number of latently infected, resting CD4+ T cells that produce infectious HIV-1 upon mitogenic stimulation in vitro (24–26). In this regard, we sought to determine whether activation of HIV-1 replication can be achieved by cytokines alone in the absence of a potent mitogenic stimulus in latently infected, resting CD4+ T cells from patients who had been receiving HAART for considerable periods of time and in whom plasma viremia was markedly suppressed. The frequency of latently infected, resting CD4+ T cells carrying replication-competent HIV-1 from these patients ranged from 0.5 to 40.1 infectious units per 106 resting CD4+ T cells (Table1). When purified resting CD4+ T cells from these patients were incubated with individual cytokines, including IL-2, no significant HIV-1 replication was detected in the supernatants (Fig. 3). However, the combination of IL-2, IL-6, and TNF-α effectively induced HIV-1 replication in this population of cells from seven out of seven patients receiving HAART, three of whom (patient nos. 10, 12, and 13) had no detectable plasma viremia as determined by the ultrasensitive reverse transcriptase PCR assay (Roche Labs., Nutley, NJ) with a detection limit of 50 copies of HIV-1 RNA per milliliter of plasma. As in patients receiving no antiretroviral drugs, triple combination of antiretroviral drugs in vitro completely abolished HIV-1 replication induced by either the cytokine combination or anti-CD3 stimulation.
Figure 3.
Induction of HIV-1 replication by the combination of IL-2, IL-6, and TNF- α in latently infected, resting CD4+ T cells from patients receiving HAART. Resting CD4+ T cells from infected patients were isolated and further incubated with no cytokine, individual cytokines as indicated, the combination of IL-2, IL-6, and TNF-α, or anti-CD3 antibody with irradiated PBMCs from HIV-1–seronegative individuals. In addition, cells were incubated with the combination of IL-2, IL-6, and TNF-α or anti-CD3 antibody in the presence of three drugs (AZT, 3TC, and Indinavir; see Materials and Methods). Supernatants from each culture were removed on days 3, 6, and 9, and HIV-1 p24 was measured by ELISA.
Suppression of HIV-1 Replication in Latently Infected, Resting CD4+ T Cells by Glucocorticoids.
Glucocorticoids, a class of hormones with broad antiinflammatory and immunoregulatory properties (34–36), have been shown to block HIV-1 replication in vitro and in vivo (37, 38). One of the major effects of glucocorticoids is to inhibit the secretion and effects of cytokines (39–41). In addition, it has been shown that glucocorticoids can block nuclear factor κB– mediated cellular activation in vitro (42). To examine the inhibitory role of glucocorticoids in the induction of HIV-1 replication in latently infected, resting CD4+ T cells by cytokines, dexamethasone was added to cultures containing the combination of three cytokines or anti-CD3 antibody. As shown in Fig. 4, cultures containing dexamethasone markedly inhibited replication of HIV-1 in latently infected, resting CD4+ T cells from antiretroviral drug–naive patients when cultures were stimulated with either the combination of IL-2, IL-6, and TNF-α or with anti-CD3 antibody.
Figure 4.
Suppression of induction of HIV-1 replication in latently infected, resting CD4+ T cells stimulated with the combination of cytokines or anti-CD3 antibody by in vitro glucocorticoids. Resting CD4+ T cells were incubated with IL-2, IL-6, and TNF-α, or with anti-CD3 antibody with irradiated feeders in the presence or absence of dexamethasone (10−8 M). Supernatants from each culture were removed on days 3, 6, and 9, and HIV-1 p24 was measured by ELISA.
Discussion
In this study, we have examined the synergistic role of cytokines in the reactivation of HIV-1 replication in latently infected, resting CD4+ T cells from patients who were receiving no antiretroviral therapy as well as from patients who were receiving HAART and in whom plasma viremia was markedly suppressed, and in certain patients even undetectable by the ultrasensitive reverse transcriptase PCR. Despite the fact that certain proinflammatory and immunoregulatory cytokines have been shown to upregulate the expression of HIV-1 in chronically infected cell lines and in the PBMCs of infected individuals (3, 10–13), it has been unclear what effect they have on latently infected, resting CD4+ T cells. This study clearly demonstrates a synergistic role of the combination of IL-2, IL-6, and TNF-α in the induction of HIV-1 replication in latently infected, resting CD4+ T cells. The fact that individual cytokines did not induce significant replication of HIV in these cells, whereas combinations of cytokines were potent inducers, is consistent with previous observations of the synergistic effects of certain cytokines in the induction of expression of HIV from chronically infected cell lines (12). HIV-1 replication in latently infected, resting CD4+T cells induced by the three cytokine combination and anti-CD3 stimulation was effectively suppressed by dexamethasone at modest concentrations (10−8 M), which agrees with previous findings that glucocorticoids can block HIV-1 replication by inhibiting the secretion of certain cytokines, particularly proinflammatory cytokines (39–41) or by inhibiting nuclear factor κB–mediated cellular activation (42).
The findings in our study suggest that combinations of cytokines secreted in response to nonspecific stimuli or as a result of a specific antigenic stimulus could explain at least in part the reappearance of plasma viremia in patients receiving HAART in whom HIV-1 replication was successfully contained initially but in whom therapy was subsequently interrupted (33). Given the fact that the latently infected pool of resting CD4+ T cells resides predominantly in lymphoid tissue (27), and since cells situated in the microenvironment of lymphoid tissue are continually exposed to the secretion of proinflammatory and immunoregulatory cytokines (43), it is highly likely that these cytokines readily induce HIV replication in latently infected, resting CD4+ T cells in the absence of HAART or when HAART is ineffective in completely suppressing virus replication (33). The fact that latently infected, resting CD4+T cells from individuals receiving HAART and in whom plasma viremia was markedly suppressed, and in certain patients even undetectable, could be readily induced to replicate virus when cells were taken ex vivo and cultured in the presence of the combination of cytokines is highly consistent with their ability to become reactivated when in vivo HAART is discontinued. The ability of in vitro HAART to again suppress cytokine-induced virus replication underscores this observation.
Finally, given the relatively long half-life of these latently infected, resting CD4+ T cells (24–26) and the fact that they are constantly within an environment capable of providing the stimuli for reactivation, it is not unreasonable to explore strategies aimed at deliberately diminishing the size of this pool of cells. In this regard, since cytokine-mediated induction of HIV-1 replication in these cells with subsequent release of virus probably results in death of the cell (44–46), and since the presence of HAART in vitro prevents spread of released virus, it is conceivable that in vivo administration of cytokines together with HAART may have such an effect.
Acknowledgments
We thank Joseph Adelsberger, Randy Stevens, and Dr. Michael Baseler for their help with cell sorting experiments; and Shuying Liu and Julie Metcalf for providing patient laboratory data. We also thank Drs. Lawrence Corey, M. Michelle Berry, and Jo Ann M. Mican for providing PMBCs from patients.
Abbreviation used in this paper
HAART
highly active antiretroviral therapy
References
- 1.Paul WE, Seder RA. Lymphocyte responses and cytokines. Cell. 1994;76:241–251. doi: 10.1016/0092-8674(94)90332-8. [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS. Multifactorial nature of human immunodeficiency virus disease: implications for therapy. Science. 1993;262:1011–1018. doi: 10.1126/science.8235617. [DOI] [PubMed] [Google Scholar]
- 3.Poli G, Fauci AS. Cytokine modulation of HIV expression. Semin Immunol. 1993;5:165–73. doi: 10.1006/smim.1993.1020. [DOI] [PubMed] [Google Scholar]
- 4.Poli, G., and A.S. Fauci. 1995. Role of cytokines in the pathogenesis of human immunodeficiency virus infection. _In_Human Cytokines: Their Role in Disease and Therapy. B.B. Aggarwal and R.K. Puri, editors. Blackwell Science, Cambridge, MA. 421–449.
- 5.Fauci AS. Host factors and the pathogenesis of HIV-induced disease. Nature. 1996;384:529–534. doi: 10.1038/384529a0. [DOI] [PubMed] [Google Scholar]
- 6.Kinter AL, Poli G, Fox L, Hardy E, Fauci AS. HIV replication in IL-2–stimulated peripheral blood mononuclear cells is driven in an autocrine/paracrine manner by endogenous cytokines. J Immunol. 1995;154:2448–2459. [PubMed] [Google Scholar]
- 7.Folks T, Powell DM, Lightfoote MM, Benn S, Martin MA, Fauci AS. Induction of HTLV-III/LAV from a nonvirus-producing T-cell line: implications for latency. Science. 1986;231:600–602. doi: 10.1126/science.3003906. [DOI] [PubMed] [Google Scholar]
- 8.Folks T, Justement J, Kinter A, Dinarella C, Fauci AS. Cytokine induced expression of HIV-1 in a chronically-infected promocyte cell line. Science. 1987;238:800–801. doi: 10.1126/science.3313729. [DOI] [PubMed] [Google Scholar]
- 9.Poli, G., and A.S. Fauci. 1996. Cytokine cascades in HIV infection. In Immunology of HIV Infection. S, Gupta, editor. Plenum Press, New York. 285–301.
- 10.Osborn L, Kunkel S, Nabel GJ. Tumor necrosis factor alpha and interleukin 1 stimulate the human immunodeficiency virus enhancer by activation of the nuclear factor kappa B. Proc Natl Acad Sci USA. 1989;86:2336–2340. doi: 10.1073/pnas.86.7.2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kobayashi N, Hamamoto Y, Koyanagi Y, Chen IS, Yamamoto N. Effect of interleukin-1 on the augmentation of human immunodeficiency virus gene expression. Biochem Biophys Res Commun. 1989;165:715–721. doi: 10.1016/s0006-291x(89)80025-7. [DOI] [PubMed] [Google Scholar]
- 12.Poli G, Bressler P, Kinter A, Duh E, Timmer WC, Rabson A, Justement JS, Stanley S, Fauci AS. Interleukin 6 induces human immunodeficiency virus expression in infected monocytic cells alone and in synergy with tumor necrosis factor alpha by transcriptional and post-transcriptional mechanisms. J Exp Med. 1990;172:151–158. doi: 10.1084/jem.172.1.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poli G, Kinter AL, Fauci AS. Interleukin 1 induces expression of the human immunodeficiency virus alone and in synergy with interleukin 6 in chronically infected U1 cells: inhibition of inductive effects by the interleukin 1 receptor antagonist. Proc Natl Acad Sci USA. 1994;91:108–112. doi: 10.1073/pnas.91.1.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belec L, Meillet D, Hernvann A, Gresenguet G, Gherardi R. Differential elevation of circulating interleukin-1 beta, tumor necrosis factor alpha, and interleukin-6 in AIDS-associated cachectic states. Clin Diagn Lab Immunol. 1994;1:117–120. doi: 10.1128/cdli.1.1.117-120.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roux-Lombard P, Modoux C, Cruchaud A, Dayer JM. Purified blood monocytes from HIV 1–infected patients produce high levels of TNF alpha and IL-1. Clin Immunol Immunopathol. 1989;50:374–384. doi: 10.1016/0090-1229(89)90144-x. [DOI] [PubMed] [Google Scholar]
- 16.Hober D, Haque A, Wattre P, Beaucaire G, Mouton Y, Capron A. Production of tumour necrosis factor-alpha (TNF-alpha) and interleukin-1 (IL-1) in patients with AIDS. Enhanced level of TNF-alpha is related to a higher cytotoxic activity. Clin Exp Immunol. 1989;78:329–333. [PMC free article] [PubMed] [Google Scholar]
- 17.Navikas V, Link J, Persson C, Olsson T, Hojeberg B, Ljungdahl A, Link H, Wahren B. Increased mRNA expression of IL-6, IL-10, TNF-alpha, and perforin in blood mononuclear cells in human HIV infection. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;9:484–489. [PubMed] [Google Scholar]
- 18.Trentin L, Garbisa S, Zambello R, Agostini C, Caenazzo C, Di Francesco C, Cipriani A, Francavilla E, Semenzato G. Spontaneous production of interleukin-6 by alveolar macrophages from human immunodeficiency virus type 1–infected patients. J Infect Dis. 1992;166:731–737. doi: 10.1093/infdis/166.4.731. [DOI] [PubMed] [Google Scholar]
- 19.Ito M, Baba M, Mori S, Hirabayashi K, Sato A, Shigeta S, De Clercq E. Tumor necrosis factor antagonizes inhibitory effect of azidothymidine on human immunodeficiency virus (HIV) replication in vitro. Biochem Biophys Res Commun. 1990;166:1095–1101. doi: 10.1016/0006-291x(90)90979-w. [DOI] [PubMed] [Google Scholar]
- 20.Le Naour R, Raoul H, Mabondzo A, Henin Y, Bousseau A, Dormont D. Treatment of human monocyte-derived macrophages with a TNF alpha synthesis inhibitor prior to HIV1 infection: consequences on cytokine production and viral replication. Res Virol. 1994;145:199–207. doi: 10.1016/s0923-2516(07)80023-9. [DOI] [PubMed] [Google Scholar]
- 21.Granowitz EV, Saget BM, Wang MZ, Dinarello CA, Skolnik PR. Interleukin 1 induces HIV-1 expression in chronically infected U1 cells: blockade by interleukin 1 receptor antagonist and tumor necrosis factor binding protein type 1. Mol Med. 1995;1:667–677. [PMC free article] [PubMed] [Google Scholar]
- 22.Goletti D, Kinter AL, Hardy EC, Poli G, Fauci AS. Modulation of endogenous IL-1 beta and IL-1 receptor antagonist results in opposing effects on HIV expression in chronically infected monocytic cells. J Immunol. 1996;156:3501–3508. [PubMed] [Google Scholar]
- 23.Herbein G, Montaner LJ, Gordon S. Tumor necrosis factor alpha inhibits entry of human immunodeficiency virus type 1 into primary human macrophages: a selective role for the 75-kilodalton receptor. J Virol. 1996;70:7388–7397. doi: 10.1128/jvi.70.11.7388-7397.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chun TW, Stuyver L, Mizell SB, Ehler LA, Mican JA, Baseler M, Lloyd AL, Nowak MA, Fauci AS. Presence of an inducible HIV-1 latent reservoir during highly active antiretroviral therapy. Proc Natl Acad Sci USA. 1997;94:13193–13197. doi: 10.1073/pnas.94.24.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finzi D, Hermankova M, Pierson T, Carruth LM, Buck C, Chaisson RE, Quinn TC, Chadwick K, Margolick J, Brookmeyer R, et al. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science. 1997;278:1295–300. doi: 10.1126/science.278.5341.1295. [DOI] [PubMed] [Google Scholar]
- 26.Wong JK, Hezareh M, Gunthard HF, Havlir DV, Ignacio CC, Spina CA, Richman DD. Recovery of replication-competent HIV despite prolonged suppression of plasma viremia. Science. 1997;278:1291–1295. doi: 10.1126/science.278.5341.1291. [DOI] [PubMed] [Google Scholar]
- 27.Chun TW, Carruth L, Finzi D, Shen X, DiGiuseppe JA, Taylor H, Hermankova M, Chadwick K, Margolick J, Quinn TC, et al. Quantification of latent tissue reservoirs and total body viral load in HIV-1 infection. Nature. 1997;387:183–188. doi: 10.1038/387183a0. [DOI] [PubMed] [Google Scholar]
- 28.Pantaleo G, Fauci AS. New concepts in the immunopathogenesis of HIV infection. Annu Rev Immunol. 1995;13:487–512. doi: 10.1146/annurev.iy.13.040195.002415. [DOI] [PubMed] [Google Scholar]
- 29.Stanley S, Ostrowski MA, Justement JS, Gantt K, Hedayati S, Mannix M, Roche K, Schwartzentruber DJ, Fox CH, Fauci AS. Effect of immunization with a common recall antigen on viral expression in patients infected with human immunodeficiency virus type 1. N Engl J Med. 1996;334:1222–1230. doi: 10.1056/NEJM199605093341903. [DOI] [PubMed] [Google Scholar]
- 30.Staprans SI, Hamilton BL, Follansbee SE, Elbeik T, Barbosa P, Grant RM, Feinberg MB. Activation of virus replication after vaccination of HIV-1–infected individuals. J Exp Med. 1995;182:1727–1737. doi: 10.1084/jem.182.6.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O'Brien WA, Grovit-Ferbas K, Namazi A, Ovcak-Derzic S, Wang HJ, Park J, Yeramian C, Mao SH, Zack JA. Human immunodeficiency virus type 1 replication can be increased in peripheral blood of seropositive patients after influenza vaccination. Blood. 1995;86:1082–1089. [PubMed] [Google Scholar]
- 32.Ostrowski MA, Stanley SK, Justement JS, Gantt K, Goletti D, Fauci AS. Increased in vitro tetanus-induced production of HIV type 1 following in vivo immunization of HIV type 1–infected individuals with tetanus toxoid. AIDS Res Hum Retroviruses. 1997;13:473–480. doi: 10.1089/aid.1997.13.473. [DOI] [PubMed] [Google Scholar]
- 33.de Jong MD, de Boer RJ, de Wolf F, Foudraine NA, Boucher CA, Goudsmit J, Lange JM. Overshoot of HIV-1 viraemia after early discontinuation of antiretroviral treatment. AIDS (London) 1997;11:F79–84. doi: 10.1097/00002030-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Parrillo JE, Fauci AS. Mechanisms of glucocorticoid action on immune processes. Annu Rev Pharmacol Toxicol. 1979;19:179–201. doi: 10.1146/annurev.pa.19.040179.001143. [DOI] [PubMed] [Google Scholar]
- 35.Zimmerman GA, Prescott SM, McIntyre TM. Endothelial cell interactions with granulocytes: tethering and signaling molecules. Immunol Today. 1992;13:93–100. doi: 10.1016/0167-5699(92)90149-2. [DOI] [PubMed] [Google Scholar]
- 36.Sternberg EM, Chrousos GP, Wilder RL, Gold PW. The stress response and the regulation of inflammatory disease. Ann Intern Med. 1992;117:854–866. doi: 10.7326/0003-4819-117-10-854. [DOI] [PubMed] [Google Scholar]
- 37.Bressler P, Poli G, Justement JS, Biswas P, Fauci AS. Glucocorticoids synergize with tumor necrosis factor alpha in the induction of HIV expression from a chronically infected promonocytic cell line. AIDS Res Hum Retroviruses. 1993;9:547–551. doi: 10.1089/aid.1993.9.547. [DOI] [PubMed] [Google Scholar]
- 38.Biswas P, Poli G, Orenstein JM, Fauci AS. Cytokine-mediated induction of human immunodeficiency virus (HIV) expression and cell death in chronically infected U1 cells: do tumor necrosis factor alpha and gamma interferon selectively kill HIV-infected cells? . J Virol. 1994;68:2598–2604. doi: 10.1128/jvi.68.4.2598-2604.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schleimer, R.P. 1993. An overview of glucocorticoid anti-inflammatory actions. Eur. J. Clin. Pharmacol. 45(Suppl. 1):S3–7. [DOI] [PubMed]
- 40.Almawi WY, Beyhum HN, Rahme AA, Rieder MJ. Regulation of cytokine and cytokine receptor expression by glucocorticoids. J Leukocyte Biol. 1996;60:563–572. doi: 10.1002/jlb.60.5.563. [DOI] [PubMed] [Google Scholar]
- 41.Schwiebert LM, Beck LA, Stellato C, Bickel CA, Bochner BS, Schleimer RP, Schwiebert LA. Glucocorticosteroid inhibition of cytokine production: relevance to antiallergic actions. J Allergy Clin Immunol. 1996;97:143–152. doi: 10.1016/s0091-6749(96)80214-4. [DOI] [PubMed] [Google Scholar]
- 42.Scheinman RI, Cogswell PC, Lofquist AK, Baldwin AS., Jr Role of transcriptional activation of I kappa B alpha in mediation of immunosuppression by glucocorticoids. Science. 1995;270:283–286. doi: 10.1126/science.270.5234.283. [DOI] [PubMed] [Google Scholar]
- 43.Graziosi C, Pantaleo G, Gantt KR, Fortin JP, Demarest JF, Cohen OJ, Sekaly RP, Fauci AS. Lack of evidence for the dichotomy of TH1 and TH2 predominance in HIV-infected individuals. Science. 1994;265:248–252. doi: 10.1126/science.8023143. [DOI] [PubMed] [Google Scholar]
- 44.Ho DD, Neumann AU, Perelson AS, Chen W, Leonard JM, Markowitz M. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature. 1995;373:123–126. doi: 10.1038/373123a0. [DOI] [PubMed] [Google Scholar]
- 45.Wei X, Ghosh SK, Taylor ME, Johnson VA, Emini EA, Deutsch P, Lifson JD, Bonhoeffer S, Nowak MA, Hahn BH, et al. Viral dynamics in human immunodeficiency virus type 1 infection. Nature. 1995;373:117–122. doi: 10.1038/373117a0. [DOI] [PubMed] [Google Scholar]
- 46.Perelson AS, Neumann AU, Markowitz M, Leonard JM, Ho DD. HIV-1 dynamics in vivo: virion clearance rate, infected cell life-span, and viral generation time. Science. 1996;271:1582–1586. doi: 10.1126/science.271.5255.1582. [DOI] [PubMed] [Google Scholar]
- 47.Myers LE, McQuay LJ, Hollinger FB. Dilution assay statistics. J Clin Microbiol. 1994;32:732–739. doi: 10.1128/jcm.32.3.732-739.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]