Origins and Hallmarks of Macrophages: Development, Homeostasis, and Disease (original) (raw)
. Author manuscript; available in PMC: 2014 Apr 25.
Published in final edited form as: Nature. 2013 Apr 25;496(7446):445–455. doi: 10.1038/nature12034
Preface
Macrophages the most plastic cells of the hematopoietic system are found in all tissues and exhibit great functional diversity. They have roles in development, homeostasis, tissue repair, and immunity. While anatomically distinct, resident tissue macrophages exhibit different transcriptional profiles, and functional capabilities, they are all required for the maintenance of homeostasis. However, these reparative and homeostatic functions can be subverted by chronic insults, resulting in a causal association of macrophages with disease states. In this review, we discuss how macrophages regulate normal physiology and development and provide several examples of their pathophysiologic roles in disease. We define the “hallmarks” of macrophages performing particular functions, taking into account novel insights into the diversity of their lineages, identity, and regulation. This diversity is essential to understand because macrophages have emerged as important therapeutic targets in many important human diseases.
Introduction and Perspectives
Macrophages, originally identified by Metchnikoff by their phagocytic nature, are ancient cells in Metazoan phylogeny. In adult mammals, they are found in all tissues where they display great anatomical and functional diversity. In tissues, they are organized in defined patterns with each cell occupying its own territory, a type of tissue within a tissue. Although several attempts have been made to classify macrophages, the most successful definition is the mononuclear phagocytic system (MPS), which encompasses these highly phagocytic cells and their bone marrow (BM) progenitors. In the MPS schema, adult macrophages are defined as end cells of the mononuclear phagocytic lineage with tissue macrophages deriving from circulating monocytes that originate in the BM. However, this definition is inadequate as macrophages have several origins during ontogeny and each of these different lineages persist into adulthood where they display great diversity 1. Other classifications have included binary classifications that refer to inflammatory states. These include the activated (AM) and alternatively activated (AAM) or M1 or M2 2,3 defined by responses to the cytokines IFNγ and activation of TLRs and IL4/IL13 respectively. While this is a useful heuristic that may reflect extreme states such as in AMs in THI mediated immune responses or AAM in parasitic infections 2 it cannot represent the complex in vivo milieu for most macrophage types where numerous cytokines and growth factors interact to define the final differentiated state of macrophages. Indeed transcriptional profiling of resident macrophages by the “Immunological Genome Project” find that these populations show great transcriptional diversity with minimal overlap suggesting many unique classes1.
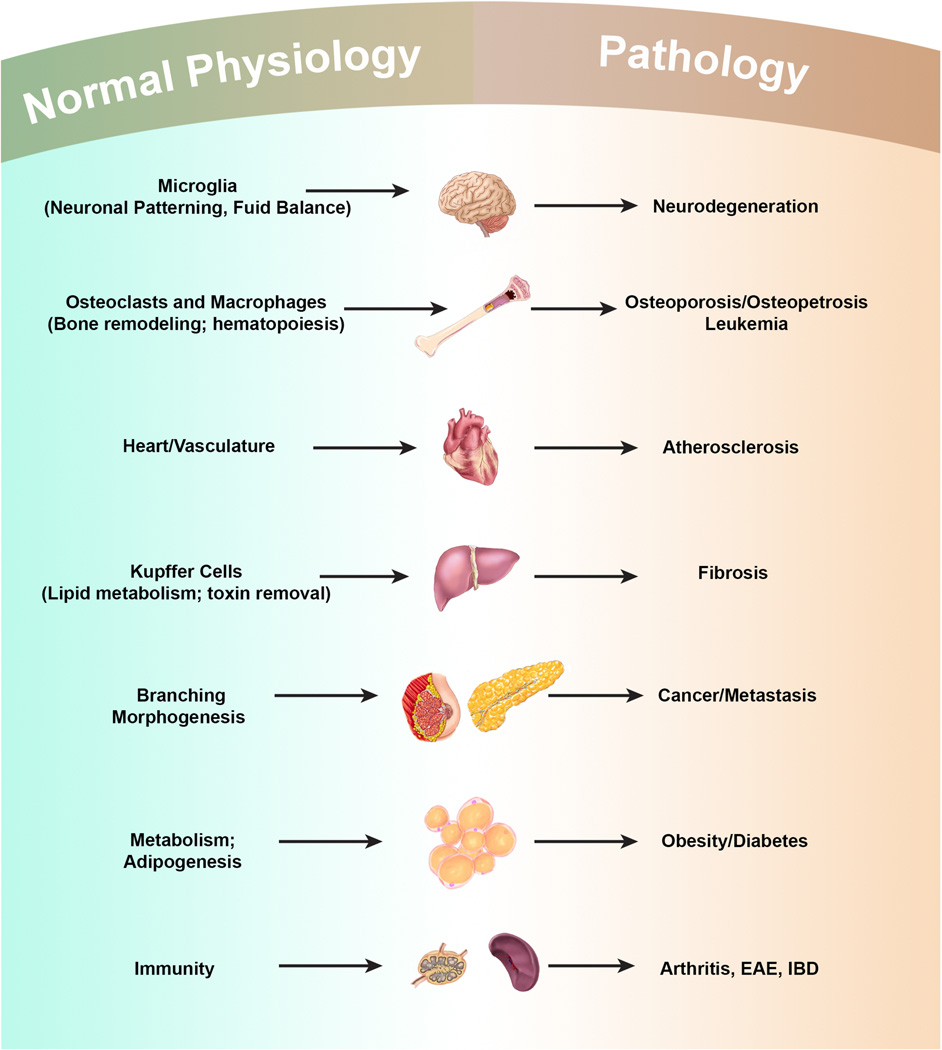
Macrophages have roles in almost every aspect of an organism’s biology ranging from development, homeostasis, to repair through to immune responses to pathogens. Resident macrophages regulate tissue homeostasis by acting as sentinels and responding to changes in physiology as well as challenges from outside. During these homeostatic adaptations, macrophages of different phenotypes can also be recruited from the monocyte reservoirs of blood, spleen and bone marrow 4, and perhaps, from resident tissue progenitors or through local proliferation 5,6. Unfortunately, in many cases, these homeostatic and reparative functions can be subverted by continuous insult, resulting in causal association of macrophages with disease states, such as fibrosis, obesity and cancer (Figure 1). Macrophages, therefore, are an incredibly diverse set of cells constantly shifting their functional state to new set points in response to changes in tissue physiology or environmental challenges. They should not even be considered as one cell type but be subdivided into different functional subsets with acknowledgement to their different origins.
Figure 1. Macrophages in Development, Homeostasis and Disease.
Macrophages play many developmental roles shaping the architecture of tissues ranging from the brain to bone to the mammary gland. Once development is over macrophages modulate homeostasis and normal physiology through regulating diverse activities including metabolism and neural connectivity and by detecting damage. These trophic and regulatory roles however, are often subverted by continuous insult and macrophages contribute to many diseases that are often associated with aging.
This review will not dwell on macrophage responses to pathogens that have been discussed extensively by others2,7,8, but will emphasize the homeostatic mechanisms by which macrophages contribute to physiological and pathophysiologic adaptations in mammals. It will define the hallmarks of “macrophage” performing particular functions, taking into account new insights into the diversity of their lineages, identity and regulation. This phenotypic diversity is essential to understand because macrophages are central to many disease states, and have emerged as important therapeutic targets in many diseases.
Macrophage Origins Rewritten
Ontologically, the MPS has been proposed to arise from a rigid temporal succession of macrophage progenitors 9. In mice, these first develop at embryonic (e) day 8 from the primitive ectoderm of the yolk sac and give rise to macrophages that do not have a monocytic progenitor. This primitive system is followed by definitive hematopoiesis in the fetal liver, which is initially seeded by hematopoietic progenitors from the yolk sac and subsequently from the hematogenic endothelium of the aorto-gonadal-mesonephros region of the embryo. Thereafter, during embryogenesis the fetal liver is the source of definitive hematopoiesis generating circulating monocytes. Coincident with the post-natal formation of bone, fetal liver hematopoiesis declines and is replaced by BM hematopoiesis. This definitive hematopoiesis is the source of circulating monocytes (resident Ly6c- and inflammatory Ly6c+ in mice) and from which it has been considered that all resident macrophages in tissues are derived 4. However, this model for the formation of the MPS has been challenged (Figure 2). First, lineage-tracing experiments have shown that Langerhans cells (LC) and microglia are primarily derived from the yolk sac progenitors while LCs have a mixed origin from YS and fetal liver 10,11. Second, even in the absence of hematopoietic stem cells, yolk sac progenitors were capable of giving rise to the major tissue resident population of macrophages (defined as F4/80 bright) in skin, spleen, pancreas, liver, brain and lung. In a few tissues, such as kidney and lung, macrophages were shown to have a chimeric origin (HSC- and yolk sac-derived), whereas other cells, such as classical dendritic cells (DC) and lesser populations of F4/80low cells, were continuously replaced by BM-derived progenitors 6. These data indicate that there are at least three lineages of macrophages in the mouse arising at different stages of development and persisting in the adult. It also calls into question the function of circulating monocytes because, at least in mice, these cells do not seed the majority of the adult tissues with macrophages. In fact, complete loss of CD16+ monocytes in humans appears to be of little consequence 12. Thus the function of monocytes needs to be defined with the possibility that patrolling monocytes (Ly6c-) act to maintain vessel integrity and to detect pathogens while inflammatory monocytes (Ly6c+) are recruited only to sites of infection or injury or to tissues that have continuous cyclical recruitment of macrophages such as the uterus.
Figure 2. Macrophage Lineages Re-Defined in Mice.
The mononuclear phagocytic system in adults derives from at least three sources. The first is the yolk sac (YS) that results in progenitors that populate all tissues and their progeny persist throughout life as F4/80 bright resident macrophages. These lineages are largely regulated by CSF1R. The second from the fetal liver is less well defined but seems to contribute to adult LCs perhaps through a progenitor derived from the YS. The third lineage derives from the bone marrow (BM) to give circulating monocytes and their progeny F4/80low macrophages and DCs. In this case the Ly6c+ monocytes give rise to classical DCs under the regulation of FLT3 and these are continuously replenished. Other macrophages that are F4/80 low also emanate from Ly6c+ monocytes and in some cases such as kidney and lung, co-exist with those derived from YS to give chimeric organs. The exact role of the patrolling Ly6cmacrophages remains unclear, as is the contribution of fetal liver to adult tissue macrophages.
Regardless of their origin, genetic and cell culture studies indicate the major lineage regulator of almost all macrophages is the colony stimulating factor 1 receptor, CSF1R. This class III transmembrane tyrosine kinase receptor is expressed on most, if not all, mononuclear phagocytic cells, and a reporter mouse expressing GFP from the Csf1r locus illustrates their relative abundance (5–20% of cells) and tissue distribution 13. Csf1r expression and its requirement for differentiation distinguish macrophages from many but not all DCs sub-types 14. Targeted ablation of the Csf1r causes severe depletion of macrophages in many tissues, such as brain, skin, bone, testis, ovary etc. Moreover, an initial comparison of the Csf1r null mice with a spontaneous mutant that lacks its cognate ligand CSF1 (Csf1op/op mice) demonstrated that all phenotypes in the receptor null were also found in the ligand null, indicating that CSF1 only has a single receptor 15. However, the phenotype of the Csf1r null mice is more severe than that of the Csf1 null mice, including the complete loss of microglia and LCs 10,16 in the Csf1r null mice, which suggested the presence of another ligand. Indeed, IL34, with a distinct but overlapping pattern of expression with Csf1, was recently identified as an additional ligand for the CSF1R 17. Targeted ablation of Il34 resulted in loss of microglia and LCs, but had little impact on BM, liver, or splenic macrophages 18.
Despite the importance of the CSF1R in macrophage specification, Csf1r null mutant mice still have some tissue macrophages, such as in the spleen, indicating the existence of other macrophage growth factors. Potential candidates include GM-CSF and IL3 that act as macrophage growth factors in tissue culture. However, mice lacking GM-CSF or IL3 do not exhibit significant defects in their tissue macrophages except alveolar ones that are regulated by GM-CSF 19. VEGF is another candidate regulator of macrophages because it can compensate for the loss of Csf1 in osteoclast development in vivo 20. In contrast to CSF-1 that is found in all tissues and serum and is a basal regulator of macrophage number through a negative feedback loop 15, GM-CSF is not a steady-state ligand and appears to be synthesized in response to challenge 21. GM-CSF and FLT3L regulate the maturation of DC populations with the notable exception of LCs, whose development is dependent on Csf1r 22. Recent genomic profiling of LCs place them closer to macrophages than DCs and this data together with their lineage dependence on Csf1r, may require changes in classification 14. DCs will not be discussed further in this review but their biology and lineages have been extensively covered recently 14.
In their basal state, resident tissue macrophages show great diversity in their morphologies, transcriptional profiles, anatomical locations, and functional capabilities 23. This functional heterogeneity likely results from the dynamic crosstalk between resident tissue macrophages and the client cells that they support. To understand this macrophage diversity there must be an understanding of transcriptional regulation. The most important of these transcription factors is PU1, Spl1, a member of the ETS family whose loss following targeted mutation results in complete depletion of Cd11b+ F4/80+ macrophages including those derived from the YS 6. However, Pu.1 action is not limited to macrophages as B cells are also severely depleted in these null mutant mice. Similarly other members of the ETS family are also involved in macrophage differentiation including Ets2 that positively regulates the Csf1r promoter. In adults, Mafb (c-Maf) is required for the local proliferation that maintains resident macrophages 4. In the differentiation of osteoclasts, Fos and Mitf are required 24, whereas Gata-2 is also required for monocyte development but not resident macrophage populations 25. However, little is known about the transcriptional control of the differentiation of the diverse tissue macrophages, such as those in the liver and brain 13. Rather most research has focused on their functional activation in response to environmental challenges 23, topics that will be discussed in following sections. Nevertheless, the recent transcriptional profiling of resident macrophages has identified many candidate transcription factors including those that may regulate core macrophage-associated genes such as MiT (Micropthalmia) family members, Tcef3, C/EBPa, Bach1, Creg-1 and those unique to sub-populations including Gata6 and Spi-c whose targeted gene ablation will undoubtedly define sub-sets of macrophages and their unique activities 1.
Macrophages in Development
Metchnikoff proposed that macrophages participate in the maintenance of tissue integrity and homoeostasis. This necessitated that macrophages be able to discriminate self from non-self, sense tissue damage, and recognize invading pathogens, an insight that led to the concept of innate immunity for which he was awarded the Nobel Prize. The properties that included sensing inside from out together with motility throughout the organism, phagocytosis and degradation were later sequestered to instruct the acquired immune system as it evolved to more efficiently deal with ever changing pathogenic challenges. This enhanced sophistication of the immune system probably resulted in the evolution of DCs as specialized mononuclear phagocytes to interface with the acquired immune system. Indeed, in mammals, DCs appear to be focused upon initiating tissue immune responses, while tissue macrophages on homeostasis and tissue integrity 9.
Emphasis on the immunological and repair aspects of macrophage function has rather overshadowed their importance in the development of many tissues. For instance, studies of Csf1 null mutant mice, which lack many macrophage populations, have revealed a cluster of developmental abnormalities 19. Most notable amongst them is the development of osteopetrosis, which is caused by the loss of bone reabsorbing macrophages known as osteoclasts. This phenotype, which is also observed in Spl1 null mice, is axiomatic for the roles of macrophages in development, in that cell fate decisions are unchanged but the tissue remodeling and expression of growth factors is lost. Specifically, while bone formation is intact in Csf1 or Spl1 null mice, the bones are not sculpted to form the cavities where hematopoiesis can ensue 19. Consequently, the functional integrity of the bones, in terms of load bearing and hematopoiesis, is compromised. Csf1 null mice survive to adulthood because of extra-medullary hematopoiesis in the spleen and liver 19, and as mice age, osteoclastogenesis is rescued by compensatory expression of VEGF 20.
Remodeling deficiencies in the absence of macrophages have also been noted in several other tissues, including the mammary gland, kidney and pancreas suggesting a general requirement for macrophages in tissue patterning and branching morphogenesis 19,26. In the mammary gland, the best studied of these tissues, macrophages are recruited to the growing ductal structure and their loss results in a slower rate of outgrowth and limited branching, phenotypes that are re-iterated during the mammary growth caused by pregnancy 19. This stems in part from the failure to remodel the extracellular matrix during the outgrowth of the ductal structures. However, recent studies have also implicated macrophages in maintaining the viability and function of mammary stem cells, which reside at the tip of the duct known as the terminal end bud and are responsible for the outgrowth of this structure 27. Similar roles for macrophages in stem cell biology has been suggested in the maintenance of intestinal integrity and its regeneration after damage 28, whereas a sub-population of macrophages in the hematopoietic niche regulates the dynamics of hematopoietic stem cell release and differentiation 29. Furthermore in regenerating livers, macrophages specify hepatic progenitor fate through the expression of WNT ligands and antagonism of Notch signaling 30. Macrophage control of stem cell function is clearly an emerging and important research area.
As professional phagocytes, macrophages perform critical functions in the remodeling of tissues, both during development and in the adult animal. For instance, during erythropoiesis, maturing erythroblasts are surrounded by macrophages, which ingest the extruded erythrocyte nuclei. Remarkably, this function of macrophages is critically important because in its absence, erythropoiesis is blocked and lethality ensues 31. Macrophages also make decisions about hematopoietic egress from the bone marrow through engulfing cells that do not express the CD47 ligand 32. They also maintain hematopoietic steady state via engulfment of neutrophils and erythrocytes in the spleen and liver and the failure of this activity results in neutropenia, splenomegaly and reduced body weight 33. Phagocytosis particularly of apoptotic cells is obviously central to macrophage function and this is emphasized by the build up in macrophage-depleted mice of such cells during development for example during the resolution of the inter-digit areas during limb formation 34. However, there is no apparent consequence to this phenomenon as non-professional phagocytes clear excess apoptotic cells. Despite this, macrophages have evolved to “eat” cells, and to suppress inflammation and auto-immunity in response to self-antigens that might arise during homeostasis 35.
Macrophages also regulate angiogenesis through a variety of mechanisms. This has been most extensively studied in the eye during its development. Early in the postnatal period during regression of the hyaloid vasculature, macrophages identify and instruct vascular endothelial cells (VEC) to undergo apoptosis if these cells do not receive a counter-balancing signal from pericytes to survive. Wnt7b synthesized by macrophages delivers this cell death signal to the VECs and either its absence or the absence of macrophages, there is vascular over-growth 36. WNT secretion is also required later in retinal vasculature development but in this case macrophage synthesized Wnt5a, a non-canonical WNT, induces expression of soluble VEGFR1 through an autocrine mechanism that titrates VEGF and thereby reduces vascular complexity so that the vascular system is appropriately patterned 37. Furthermore, at other times of ocular development macrophages regulate vascular complexity. In this circumstance macrophage synthesized VEGFC reinforces Notch signaling 38. In addition, during angiogenesis in the hindbrain macrophages enhance the anastomosis of tip and stalk cells to give functional vessels 39. These macrophage functions are not restricted to the vascular arm of the circulatory system since they also play roles in lymphangiogenesis during development 40 and in adults they play a significant role in maintaining fluid balance through their synthesis of VEGFC 41.
Brain development is also influenced by macrophages. These macrophages called microglia depend on CSF1R signaling for their presence 10,16. In the absence of this signaling there are no microglia and the brains of these mice have significant structural defects as they mature 16. Both CSF1 and IL34 are expressed by neurons in a mutually restricted pattern of expression with IL34 being the major factor for microglial differentiation and viability 10,42. The disruption of architecture in the Csf1r null mouse brain together with well-documented deficiencies in neuronal processing regulating olfaction and the reproductive axis in the hypothalamus in Csf1 null mice strongly suggest that microglia are involved in the development of neuronal circuitry and maintenance of brain structure 16,19. Indeed microglia have been shown to promote neuron viability 19, modulate neuronal activity 43, to prune synapse during development 44 as well as express a range of neuronal growth and survival factors including NGF 19. This conjecture is reinforced because a hypomorphic mutation in the CSF1R in humans is responsible for hereditary diffuse leukoencephalopathy with spheroids that results from loss of myelin sheaves and axonal destruction 45. These trophic activities of microglia are also consistent with macrophage roles in neuroprotection following injury in a variety of contexts. These effects include the promotion of survival and proliferation of retinal progenitor cells and the regeneration of adult sensory neurons 46–48. However, caution needs to be exercised in attributing all the phenotypes observed in the brains of Csf1r mutant mice or humans to the loss of microglia as Csf1r expression has been reported on neuronal stem cells and their development in vivo is regulated by CSF1R 42. Nevertheless, it seems likely that microglia play important roles in the development of neuronal circuitry though their effects on the proliferation, survival and connectivity of neurons 43 or through effects on myelination or by modulating angiogenesis and fluid balance in the brain 16.
The examples cited above indicate a few of the roles for macrophages in normal development and these are likely to expand with further study. Phenotypically in mice, macrophages are all Cd11b+, CD68+ CSF1R+ F4/80+ and phagocytic and their activities are through the temporal and spatial delivery of developmentally important molecules such VEGFs and WNTs as well as proteases. These developmental roles of macrophages are re-capitulated in repair as described below but are also intimately involved in chronic conditions that lead to pathologies as well as the development and progression of malignancies.
Macrophages in Metabolic Homeostasis
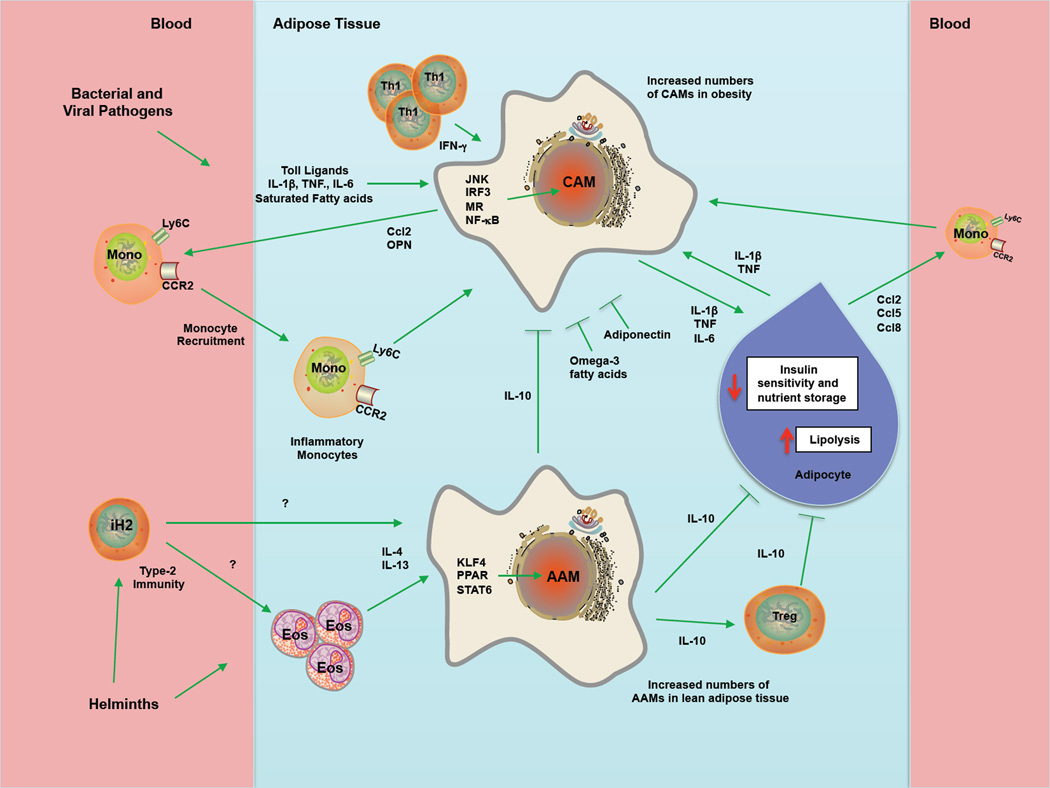
Mammalian metabolic organs like liver, pancreas, and adipose tissue are composed of parenchymal and stromal cells, including macrophages, which function together to maintain metabolic homeostasis 49. By regulating this interaction, mammals are able make dramatic adaptations to changes in their environment and nutrient intake. For instance, during bacterial infection, innate activation of macrophages results in secretion of pro-inflammatory cytokines, such as TNFα, IL6 and IL1β, which collectively promote peripheral insulin resistance to decrease nutrient storage50,51. This metabolic adaptation is absolutely necessary for mounting an effective defense against bacterial and viral pathogens because nearly all activated immune cells preferentially utilize glycolysis to fuel their functions in host defense. However, this adaptive strategy of nutrient reallocation becomes maladaptive in the setting of diet-induced obesity, a state characterized by chronic low-grade macrophage-mediated inflammation51,52. In the sections below, we provide a general framework for understanding the pleiotropic functions performed by macrophages to maintain metabolic homeostasis (Figure 3). Although our current knowledge in this area is primarily derived from studies in obese insulin resistant mice, it is likely that tissue resident macrophages also participate in facilitating metabolic adaptations in healthy animals.
Figure 3. Activated and alternatively activated macrophages differentially regulate insulin sensitivity in obesity.
In lean healthy animals, adipose tissue macrophages comprise 10–15% of stromal cells and express markers that link them with alternatively-activated macrophages, which are critical for maintaining insulin sensitivity in adipocytes, in part via the production of IL-10. Type-2 cytokines such as IL4 and IL13 derived from a variety of cellular sources, including eosinophils, appear to be important for maintaining the AAM phenotype in lean tissues. In contrast, during obesity Ly6Chi monocytes are recruited, which increases macrophage content to 45–60%. These macrophages, in contrast to normal resident macrophages, express an inflammatory phenotype, characterized by the production of TNFα, IL6 and IL1β These inflammatory macrophages decrease insulin sensitivity while facilitating the storage of excess nutrients. The enlarging white adipose tissues in turn release chemokines, such as CCL2, CcCL5, and CCL8, to recruit additional Ly6Chi inflammatory monocytes that further exacerbate the process. This mechanism is also enhanced during bacterial and viral infections so essential nutrients are diverted to lymphocytes, which must utilize glycolysis to enhance their activation at times of stress.
White adipose tissue
White adipose tissue (WAT) is not only the principal site for long-term storage of nutrients but also regulates systemic metabolism via release of hormones termed “adipokines”53. These metabolic functions of WAT are primarily performed by adipocytes with trophic support provided by stromal cells, including macrophages. In this scenario, macrophage representation in WAT, both in terms of numbers and their activation state, reflects the metabolic health of adipocytes51. For instance, in lean healthy animals, adipose tissue macrophages comprise 10–15% of stromal cells and express the canonical markers (Arg1+, CD206+, CD301+) of AAMs 54. In contrast, macrophage content increases to 45–60% during obesity 55,56, resulting from increased recruitment of Ly6Chi monocytes that differentiate into inflammatory macrophages, as judged by their expression of Nos2, Tnfa, and Itgax 54,55. Although these macrophages contribute to development of insulin resistance in adipocytes, recent studies suggest that these cells also participate in remodeling of the enlarging WAT, functions that facilitate the storage of excess nutrients in adipocytes 57. This suggests that two macrophage subsets coordinate homeostatic adaptations in adipocytes of lean and obese animals.
In healthy animals, AAMs are critical for maintaining insulin sensitivity in adipocytes51. This trophic effect of AAMs is, in part, mediated by secretion of IL-10, which potentiates insulin action in adipocytes 54. These observations led various groups to focus on cell-intrinsic and extrinsic mechanisms that control alternative activation of adipose tissue macrophages. For cell-intrinsic factors, transcription factors downstream of IL-4/IL-13 signaling, such as PPARγ, PPARδ, and KLF4, were found to be required for the maintenance of AAMs in WAT and metabolic homeostasis 58–61. The dominant cell extrinsic factors regulating maturation of AAMs in lean WAT are the type 2 cytokines, IL-4 and IL-13 60. Absence of eosinophils, which constitute the major cell type capable of IL-4 secretion in WAT 62, impairs alternative activation of adipose tissue macrophages and makes mice susceptible to obesity-induced insulin resistance. Together, these reports have established that homeostatic functions performed by AAMs in WAT are required for metabolic adaptations to excessive nutrient intake.
While adipocytes in lean animals can easily accommodate acute changes in energy intake, chronic increase in energy intake places adipocytes under considerable metabolic stress. Consequently, the enlarging WAT releases chemokines, such as CCL2, CCL5, and CCL8, to recruit Ly6Chi inflammatory monocytes into the WAT 63, where these cells differentiate into CD11c+ macrophages and form “crown-like structures” around dead adipocytes 54,64. As these CD11c+ macrophages phagocytize dead adipocytes and become lipid engorged, they initiate expression of inflammatory cytokines, such as TNF-α and IL-6, which promote insulin resistance in the surrounding adipocytes 54. Presumably, this initial decrease in adipocyte insulin sensitivity is an adaptation to limit nutrient storage. However, in the setting of unabated increase in caloric intake, this adaptive response becomes maladaptive, contributing to pathogenesis of obesity-induced systemic insulin resistance.
Brown Adipose Tissue
In mammals, brown adipose tissue (BAT) is the primary thermogenic organ that is activated by exposure to environmental cold 65. For decades, it had been thought that hypothalamic sensing of cold triggers an increase in sympathetic nerve activity to stimulate the BAT program of adaptive thermogenesis 65. However, recent work has demonstrated a requirement for resident macrophages in facilitating the metabolic adaptations of brown and white adipose tissues to cold. Specifically, exposure to cold temperatures results in alternative activation of BAT and WAT macrophages, which are required for induction of thermogenic genes in BAT and lipolysis of stored triglycerides in WAT 66. Accordingly, mice lacking AAMs are unable to mobilize fatty acids from WAT to maximally support BAT thermogenesis, which is necessary for the maintenance of core body temperature in cold environments. These supportive functions of macrophages are mediated by their secretion of norepinephrine, which surprisingly accounts for ~50% of the catecholamine content of BAT and WAT in the cold. Thus, cold-induced alternative activation of BAT and WAT macrophages provides an example of how resident macrophages provide trophic support to facilitate the function of tissue parenchymal cells, in this case the white and brown adipocytes.
Liver and Pancreas
Liver integrates nutrient, hormonal, and environmental signals to maintain glucose and lipid homeostasis in mammals. Over the last few years, evidence has emerged that Kupffer cells, the resident macrophages of liver, facilitate the metabolic adaptations of hepatocytes during increased caloric intake. During obesity, an imbalance between the uptake, synthesis, and oxidation of fatty acids results in increased lipid storage in hepatocytes, a key factor in the development of hepatic insulin resistance 67. Interestingly, Kupffer cells directly participate in this process by regulating the oxidation of fatty acids in hepatocytes. An early insight into this process came from studies that identified PPARδ as an important regulator of IL-4 and IL-13 driven program of alternative macrophage activation 58,61. These studies revealed that loss of PPARδ in myeloid cells specifically impaired alternative activation of Kupffer cells, resulting in hepatic steatosis and insulin resistance. A similar phenotype was observed when Kupffer cells were depleted in rodents using gadolinium chloride or clodronate-containing liposomes 68 Although the precise factors elaborated by Kupffer cells are still not known, co-culture studies suggest that Kupffer cell-derived factors work in trans to maintain hepatic lipid homeostasis 58,61.
Pancreas functions as an endocrine and exocrine gland in mammals. Recent findings suggest that, analogous to obesity-induced WAT inflammation, high fat feeding induces the infiltration of macrophages into the insulin-producing islets. In this case, the increased intake of dietary lipids results in β-cell dysfunction, which induces the expression of chemokines, such as CCL2 and CCCL1, to recruit inflammatory monocytes/macrophages into the islets 69,70. Consequently, the secretion of IL1β and TNFα by the infiltrating macrophages augments β-cell dysfunction, resulting in impaired insulin secretion and hyperglycemia in obese mice. Although these reports have elucidated the pathogenic role of macrophages in β-cell dysfunction, in the future it will be important to determine whether macrophages also participate in the physiologic regulation of β-cell biology as they do during development and pregnancy 19.
Macrophages in disease
When tissues are damaged following infection or injury, inflammatory monocytes (Ly6c+ in mice) are recruited from the circulation and differentiate into macrophages as they migrate into the affected tissues 4. These recruited macrophages often exhibit a pro-inflammatory phenotype in the early stages of a wound healing response. They secrete a variety of inflammatory mediators including, TNFα, IL1, and nitric oxide (NO), which activate anti-microbial defense mechanisms, including oxidative processes that contribute to the killing of invading organisms 7. They also produce IL12 and IL23, which direct the differentiation and expansion of anti-microbial TH1 and TH17 cells that help drive inflammatory responses forward 3. Although these inflammatory macrophages are initially beneficial because they facilitate the clearance of invading organisms, they also trigger substantial collateral tissue damage because of the toxic activity of reactive oxygen and nitrogen species and of TH1 and TH17 cells 71. Indeed, if the inflammatory macrophage response is not quickly controlled, it can become pathogenic and contribute to disease progression, as is seen in many chronic inflammatory and autoimmune diseases 72,73. To counteract the tissue damaging potential of the inflammatory macrophage response, macrophages undergo apoptosis or switch into an anti-inflammatory or suppressive phenotype that dampens the pro-inflammatory response, while facilitating wound healing 7. These regulatory macrophages often produce ligands associated with development such as WNT ligands, that are essential for tissue repair 74. It is becoming increasingly clear that the mechanisms that regulate the transformation of inflammatory macrophages into an anti-inflammatory cell or suppressive macrophages back into a proinflammatory phenotype has a major impact on the progression and resolution of many chronic diseases, as discussed in the following sections (Figure 4).
Figure 4. Macrophages exhibiting unique activation profiles regulate disease progression and resolution.
Macrophages are highly plastic cells that adopt a variety of activation states in response to stimuli found in the local milieu. During pathogen invasion or following tissue injury, local tissue macrophages often adopt an activated or “inflammatory phenotype”. These cells are commonly called “classically activated” macrophages (CAM), because they were the first activated macrophage population to receive a formal definition. These macrophages are activated by IFN-γ and/or following Tolllike receptor engagement, leading to the activation of the NF-kβ and Stat1 signaling pathways, which in turn increases production of reactive oxygen and nitrogen species and pro-inflammatory cytokines like TNF-α, IL-1, and IL-6 that enhance antimicrobial and anti-tumor immunity, but may also contribute to the development of insulin resistance and diet-induced obesity. Epithelial derived alarmins and the type-2 cytokines IL4 and IL13, in contrast, result in an “alternative” state of macrophage activation that has been associated with wound healing, fibrosis, insulin sensitivity, and immunoregulatory functions. These wound healing, pro-angiogenic, and pro-fibrotic macrophages (PfMø) express TGF-β1, PDGF, VEGF, WNT ligands, and various matrix metalloproteinases that regulate myofibroblast activation and deposition of extracellular matrix components. Alternatively activated macrophages (AAMs) also express a variety of immunoregulatory proteins like arginase-1 (Arg1), Relm-alpha (Retnla), Pdl2, and Il10 that regulate the magnitude and duration of immune responses. Therefore, in contrast to CAMs that activate immune defenses, AAMs are typically involved in the suppression of immunity and re-establishment of homeostasis. Although type-2 cytokines are important inducers of suppressive or immunoregulatory macrophages, it is now clear that several additional mechanisms can also contribute to the activation of macrophages with immunoregulatory activity. Indeed, IL10-producing Tregs, Fc gamma receptor engagement, engulfment of apoptotic cells, and prostaglandins have also been shown to preferentially increase the numbers of regulatory macrophages (Mregs) that suppress inflammation and inhibit anti-microbial and anti-tumor defenses. The tumor microenvironment itself also promotes the recruitment and activation of immune inhibitory cells, including those of the mononuclear phagocytic series such as myeloid-derived suppressor cells (MDSCs), tumor-infiltrating macrophages (TIMs), tumor-associated macrophages (TAMs) and metastasis-associated macrophages (MAMs) that promote angiogenesis and tumor growth, while suppressing anti-tumor immunity.
Macrophages in Cancer
Tumors are abundantly populated by macrophages 3. Originally thought to be part of an anti-tumor response, clinical and experimental data indicate that in the large majority of cases macrophages promote tumor initiation, progression and metastasis 75. Macrophages in response to persistent infections or chronic irritation, synthesize inflammatory cytokines, IFNγ, TNFα, IL6, that engage other immune cells to sustain the chronic inflammation that appears to be causal in tumor initiation and promotion 76. The tumor-inducing activities are multi-factorial for example, through the production of inflammatory cytokines such as IFNγ in UV-induced skin cancer 77, TNFα in carcinogen induced cancer, as well as by generating a mutagenic environment 76,78 or through alterations of the microbiome 79. However, once tumors become established they educate the tumor associated macrophages (TAMs) away from an immunologically active state to adopt a trophic immunosuppressive phenotype that promotes tumor progression to malignancy 75.
In established tumors TAMs stimulate tumor cell migration, invasion, intravasation as well as the angiogenic response required for tumor growth 75,80,81. These events are required for tumor cells to become metastatic by facilitating their escape into the circulatory or lymphatic system. Evidence from autochthonous models of breast cancer suggests that the macrophages take on these activities in response to CSF1 and IL4/IL13 encountered in the tumor microenvironment. For example, IL4 mediated differentiation 80 results in a reciprocal paracrine dialog between CSF-1 synthesized by tumor cells and EGF by TAMs that promotes tumor cell invasion and intravasation in mammary cancer 82. In mammary cancers this loop is initiated by CXCL12 in the Polyoma Middle T-induced (PyMT) model or Heregulin in the Her2/Neu model. In human xenograft models, CCL18 is also required for tumor cell invasion and metastasis through triggering integrin clustering 83. TAMs also remodel the tumor microenvironment through the expression of proteases such as matrix metalloproteinases (MMPs), cathepsins and uPA and matrix remodeling enzymes including lysyl oxidase and SPARC 81,84. The proteases, such as Cathepsin B, MMP2, 7 and 9 cleave ECM providing conduits for the tumor cells as well as release of growth factors such as HB-EGF and EGF mimics that foster tumor cell invasion and metastasis 84,85.
Macrophages play an important role in tumor angiogenesis regulating the dramatic increase in vascular density known as the angiogenic switch required for the transition to the malignant state 86. These angiogenic TAMs are characterized by the expression of the angiopoietin receptor, TIE2, similar to that found in macrophages during development 87,88. Ablation of this specific population inhibits tumor angiogenesis and thus tumor growth and metastasis in a variety of models 87,88. TAMs secrete many angiogenic molecules including VEGF family members, TNFα, IL1β, IL8, PDGF and FGF 75,88,89. Of these myeloid derived VEGF is required for the angiogenic switch 89 but other aspects of angiogenesis can be independent of VEGF and involve the secreted protein Bv8 90. Angiogenic macrophages can be recruited to the tumors by hypoxia 88,91 but also by growth factors such as CSF1 and VEGF 92.
Tumors have a proclivity to metastasize to particular sites and this phenotype is partially defined by macrophages. Data suggest that the tumor produced fragments of ECM molecules or exosomes prepare these sites, known as pre-metastatic niches, to be receptive to the circulating tumor cells through recruitment of myeloid cells characterized by CD11b and VEGFR1 positivity 93,94. These niches are tumor type dependent and the fate of the tumor cells can be reprogrammed to a different tissue by transfer of tumor-conditioned serum to a naïve mouse strain 93. These niches are also dependent on coagulation as this is necessary for recruitment of the myeloid cells that have recently been more precisely defined as F4/80+ macrophages 95. At lung metastatic sites mini-clots form that allow the arrest of tumor cells 95 that then produce CCL2 to recruit CCR2+ Ly6c+ inflammatory monocytes that rapidly develop into Ly6c- metastasis-associated macrophages (MAMs) 96. These monocytes and MAMs promote tumor cell extravasation in part through their expression of VEGF that induces local vascular permeability. MAMs that are in intimate association with the tumor cells, also promote their viability via clustering of tumor cell expressed VECAM1 that interlocks with the MAM expressed counter receptor integrin a4 83. MAMs also promote subsequent growth of the metastatic cells and importantly ablation of these cells after the metastases are established inhibits metastatic growth 75.
In mice these individual pro-tumoral functions are performed by different sub-populations albeit expressing canonical markers such as CD11b, F4/80 and CSF1R 75. This view is consistent with recent profiling of immune cells both in various tumor types in mice and human that indicates both differences in the extent of macrophage infiltrate as well as in phenotype 97. For example detailed profiling in human hepatocellular carcinoma shows various macrophage sub-types defined by specific location that have both pro- and anti-tumoral properties through their engagement of the acquired immune system although overall the balance is tilted towards pro-tumoral functions 98. Transcriptional profiling of TAM sub-populations in mice suggest they more closely resemble embryonic macrophages than inflammatory ones, being enriched in expression of developmentally relevant molecules such as those of the WNT pathway 75. This strongly suggests that the trophic roles of macrophages found during development, in metabolism and in the maintenance of homeostasis are subverted by tumors to enhance their growth, invasion and complexity. However, transcriptional control of these different phenotypes is only just being revealed especially in vivo 3. Many studies have analyzed macrophage response to LPS signaling via NFkB but this results in “activated” macrophages that largely are involved in anti-bacterial responses and likely to be anti-tumoral 23. In contrast, TAMs in their trophic and immunosuppressive functions are shaped by IL-10 and IL4/13 that signal to STAT3 and STAT6 respectively 3,99. PARPs and KLF4 also cooperate to induce a range of gene expression associated with their phenotype 3. CSF1R in macrophages also signals to a wide range of transcriptional factors including classic ones such and MYC and FOS 15. MYC signaling has been shown to be important for pro-tumoral phenotypes 100. In turn, CSF1R expression is regulated by ETS2 transcription factors and genetic ablation of this factor in macrophages in PyMT tumors recapitulates the loss of CSF1 in tumors by inhibiting angiogenesis and decreased tumor growth 101. The interaction of these factors together with other regulatory molecules such as miRNAs and epigenetic controls 3 will require sophisticated genomic analysis that will help differentiate the regulation of the multiple sub-sets 23. These functions and other regulatory systems have been thoroughly reviewed recently 3.
Macrophages in inflammatory disease
Macrophages play major roles in many chronic diseases including atherosclerosis, asthma, inflammatory bowel disease, rheumatoid arthritis, and fibrosis7,102–104. In these conditions their contribution varies greatly in different situations and is controlled by many factors. For example, allergic asthma is a complex chronic inflammatory disease of the lung defined by airway inflammation, airway obstruction, airway hyper-responsiveness and pathological lung remodeling. The inflammatory response is characterized by the recruitment of TH2 lymphocytes, mast cells, eosinophils, and macrophages to the lung and by elevated expression of allergen-specific IgE in the serum. It has been suggested that the chronicity of type-2 cytokine-mediated airway inflammation that is characteristic of allergic asthma is explained by the presence of a macrophage-like APC population that persists in the airway lumen 105. Pulmonary macrophages produce a variety of factors that directly stimulate airway smooth muscle contractility and degradation of the ECM that contributes to pathological airway remodeling. Airway macrophages from some asthmatics are bathed in type-2-associated cytokines, including IL-4, IL-13, and IL-33, causing their differentiation that have been implicated in the pathogenesis of asthma 2. These macrophages in turn promote the production of type-2 cytokines by pulmonary CD4 T lymphocytes and produce a variety of cytokines and chemokines that regulate the recruitment of eosinophils, Th2 cells, and basophils to the lung suggesting a viscous cycle that worsens disease7. Adoptive transfer studies have shown that the severity of allergen-induced disease is exacerbated by IL-4R+ macrophages 106, while protection from allergic airway disease is associated with a reduction in IL-4R+ macrophages in some studies 107. Increased numbers of IL-4R+ macrophages have also been reported in the lungs of asthmatic patients that have reduced lung function 108. Nevertheless, studies conducted with LysM(cre)_IL4R_α−/lox mice in which Cre-mediated recombination results in deletion of the IL-4Rα chain in the myeloid cell lineage surprisingly identified no substantial role for IL-4Rα activated macrophages in ovalbumin- and house dust mite-induced allergic airway disease 109.
Macrophages have also been implicated in the pathogenesis of a variety of autoimmune diseases including rheumatoid arthritis, multiple sclerosis, and inflammatory bowel disease. In these diseases, macrophages are an important source of many of the key inflammatory cytokines that have been identified as important drivers of autoimmune inflammation, including IL12, IL18, IL23, and TNFα110. Macrophage-derived IL23 promotes end-stage joint autoimmune inflammation in mice. TNFα also functions as an important driver of chronic polyarthritis, while IFN-γ- and TNFα-dependent arthritis in mice has been attributed to macrophages and DCs producing IL-18 and IL-12. The pathogenesis of chronic demyelinating diseases of the central nervous system (CNS) has also been attributed to macrophages displaying a pro-inflammatory phenotype. These inflammatory macrophages contribute to axon demyelination in autoimmune encephalomyelitis (EAE) in mice, a frequently used model of multiple sclerosis. Consequently, novel therapeutic strategies that target specific myeloid cell populations could help ameliorate pathogenic inflammation in the CNS 111. The pathogenesis of inflammatory bowel disease is also tightly regulated by inflammatory macrophages. A subset of TLR2+ CCR2+ CX3CR1int Ly6Chi Gr-1+ macrophages has been shown to promote colonic inflammation by producing TNFα 112. A recent study showed that inflammatory mediators produced in the colon convert homeostatic anti-inflammatory macrophages into proinflammatory DC-like cells that are capable of producing large quantities of IL12, IL23, iNOS, and TNF 113. CD14+ macrophages producing IL23 and TNF have also been identified in Crohn’s disease patients 103. Thus, macrophages and DCs are key producers of many of the cytokines that have been implicated in the pathogenesis of IBD.
While there is substantial evidence supporting roles for inflammatory macrophages in autoimmune inflammation, numerous studies have also reported suppressive roles for macrophages. For example, macrophages producing reactive oxygen species can protect mice from arthritis by inhibiting T cell activation 114. Pro-inflammatory cytokines produced by activated macrophages have also been shown to protect mice from Crohn’s disease by facilitating the clearance of pathogenic commensal bacteria from the mucosal lining of the bowel 115. Recruited monocytes and resident tissue macrophages are also thought to maintain homeostasis in the intestine by clearing apoptotic cells and debris, promoting epithelial repair, antagonizing pro-inflammatory macrophages, and by producing the suppressive cytokine IL-10, which is critical for the maintenance of FoxP3 expression in colonic Treg cells 113,115,116. Macrophages also protect rodents from demyelinating diseases of the CNS by promoting T cell apoptosis and by expressing the anti-inflammatory cytokines TGFβ1 and IL-10. The inhibitory receptor CD200 (also known as OX2), which is also expressed on antiinflammatory macrophages, has been shown to prevent the onset of EAE in mice 117. A unique population of monocyte-derived macrophages also reduces inflammation resulting from spinal cord injury, providing further evidence of a protective role for macrophages in the CNS 118. Together, these observations illustrate how changes in macrophage differentiation in the local milieu can play a decisive role in the pathogenesis of a wide variety of autoimmune and inflammatory diseases.
Macrophages in Fibrosis
Although macrophages phagocytose and clear apoptotic cells as a part of their normal homeostatic function in tissues, when they encounter invading organisms or necrotic debris following injury, they become activated by endogenous dangers signals and PAMPs. These activated macrophages produce anti-microbial mediators like reactive oxygen and nitrogen species and proteinases that help kill invading pathogens, which helps restore tissue homeostasis. However, they also produce a variety of inflammatory cytokines and chemokines like TNFα, IL1, IL6, and CCL2 that help drive inflammatory and anti-microbial responses forward 8,72, which exacerbate tissue injury and in some cases lead to aberrant wound healing and ultimately fibrosis (scarring) if the response is not adequately controlled, as has been demonstrated by the selective depletion of macrophages at various stages of the wound healing response 119. Therefore, in recent years research has focused on elucidating the mechanisms that suppress inflammation and prevent the development of fibrosis. Although most wound healing responses are self-limiting once the tissue-damaging irritant is removed, in many chronic fibrotic diseases the irritant is either unknown or cannot be easily eliminated 120. In this situation, it is imperative that the macrophage response converts from a pro-inflammatory phenotype to one exhibiting antiinflammatory, suppressive, or regulatory characteristics so that collateral tissue damage is kept at a minimum (Figure 4). A variety of mediators and mechanisms have been shown to regulate this conversion including the cytokines IL4 and IL13, Fcγ receptor and Toll like receptor signaling, the purine nucleoside adenosine and A2A receptor signaling, prostaglandins, Tregs, and B1 B cells120,121, to name just a few. Each of these mediators has been shown to activate distinct populations of macrophages with suppressive or regulatory characteristics. These “regulatory” macrophages express a variety of soluble mediators, signaling intermediates, and cell surface receptors including IL-10, Arginase-1, IKK alpha, MMP13, maresins, CD200 (Ox-2), Relm-alpha, and PD-L2, which have each been shown to decrease the magnitude and/or duration of inflammatory responses, and in some cases contribute to the resolution of fibrosis 7. They also produce a variety of soluble mediators including CSF-1, insulin-like growth factor 1, and VEGF that promote wound healing 122. Consequently, in addition to promoting fibrosis, macrophages are also intimately involved in the recovery phase of fibrosis by inducing ECM degradation, phagocytosing apoptotic myofibroblasts, and by dampening the immune response that contributes to tissue injury 120. Therefore, current fibrosis research is focused on characterizing these regulatory macrophage populations and devising therapeutics strategies that can exploit their anti-inflammatory, anti-fibrotic, and wound healing properties.
Perspectives
The understanding of macrophage biology is rapidly expanding with an appreciation of their diverse origins, transcriptional complexity, lability and phenotypic switching according to homeostatic demands and in response to insult. Macrophages are involved in almost every disease and thus represent extremely attractive therapeutic targets that either augment or inhibit their responses. However for these therapies to be effective it is necessary to understand macrophage diversity and define the cells according to anatomical location and function as well as the regulation of the particular set-points that defines the particular recognizable macrophages such as microglia, osteoclasts and Kuppffer cells. In fact the recognition of multiple origins (YS, FL, BM) may result in the conclusion that there is no such thing as a “macrophage” but rather clades of cells that have similar characteristics but with different origins. In fact, their different origins may allow unique opportunities to selectively target the recruited ones in the context of the chronic diseases discussed above thereby inhibiting the pathology without disturbance of resident macrophages and thereby normal homeostasis. To define these similarities and differences it will be necessary to determine proteomes and transcriptomes of particular subtypes as was recently performed for resident macrophages 1. Clearly the rapidly advancing field of genomic analysis will provide unique insights and novel ways of defining macrophage types. Furthermore macrophage biology in humans is poorly developed because of the obvious technical limitations of getting fresh material for FACS and the over-reliance in functional and genomic studies on cell lines such as the myelomonocytic leukemic cell line THP1 123 or the in vitro differentiation of circulating monocytes by CSF-1. Significant differences also exist between human and mouse macrophages for example the inability of human macrophages to increase arginase-1 expression that is an important marker of IL4-regulated macrophages in mice 3. These differences render even binary classifications such as M1 and M2 wanting let alone more complex ones. Definition of human macrophage diversity is just beginning 124 with several ongoing sequencing efforts and these efforts will enhance the essential need to translate mouse biology into the human context.
Considerable advances in defining macrophage biology have recently been made using mouse genetic approaches. For example the use of fluorescently labeled macrophages by expressing GFP from the Csf1r promoter to define and in some case live image them using intravital microscopy 125. Furthermore, the development of macrophage restricted cre recombinases for example expressed from the LysM or Csf1r promoters and the ability to ablate macrophages through the expression of the Diptheria toxin receptor that sensitized mouse cells to the toxic effect of Diptheria toxin 119 or using miRNAs to direct expression of HSV TK in macrophages has been key to defining functions. While these systems have given major insights into macrophage function caution needs to be exercised as none of the promoters are uniquely expressed in macrophages and they are also expressed in most macrophage types thereby making it difficult to discriminate the functions of sub-classes of macrophages. As we move forward specific promoters will be developed to ablate genes in particular sub-sets and more sophisticated lineage tracing to follow fates and sub-type switching will be possible through photoactivatable flours such as Dendra2 that allow single or a few cells to be tracked 125.
Therapeutic targeting of macrophages is now well underway 21,23. Most of the therapies are targeted at pan-macrophage markers such as the CSF1R. Reagents either inhibiting the ligand, ligand binding or the tyrosine kinase activity are various stages of clinical trials in cancer, including small molecules and mAbs directed against CSF1R 21. Other strategies in fibrosis and cancer have been to target recruitment of macrophages particularly through inhibition of inflammatory monocyte trafficking with anti-CCL2 or CCR2 antibodies. In other circumstances, the protective effects of recombinant human serum amyloid P (SAP; also known as pentraxin 2) in IPF and post-surgical scarring in patients treated for glaucoma is thought to be through the reduction of inflammation and fibrosis by inducing the production of IL-10 in regulatory macrophages 107. Neutralization of GM-CSF using antibodies is being tested in phase II trials for multiple sclerosis and Rheumatoid arthritis 21. In the future it seems it will be possible to exploit the inherent plasticity of macrophages to adjust their set points to control obesity by down-modulating inflammatory cytokines, to resolve fibrosis by inducing the differentiation of resolving macrophages and to treat cancer by converting macrophages from their trophic to an immunologically activated anti-tumoral state.
Acknowledgements
Macrophage biology is an enormous field with many thousands of references published each year. Thus unfortunately we are unable to cite even a small portion of these papers and for this we apologize to our many colleagues. TAW is supported by the intramural research program of the National Institutes of Allergy and Infectious Diseases/National Institutes of Health, Bethesda, MD. JWP is supported by the National Cancer Institute of the National Institutes of Health under award numbers R01CA131270 and PO1CA100324 while A.C under the award numbers HL076746, DK094641, DK094641 as well as the Diabetes Family Fund (UCSF), AHA Innovative Award (12PILT11840038) and an NIH Director’s Pioneer Award (DP1AR064158).
References
- 1.Gautier EL, et al. Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat Immunol. 2012;13:1118–1128. doi: 10.1038/ni.2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 3.Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. The Journal of clinical investigation. 2012;122:787–795. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geissmann F, et al. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327:656–661. doi: 10.1126/science.1178331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jenkins SJ, et al. Local Macrophage Proliferation, Rather than Recruitment from te Blood, Is a Sinature of Th2 Inflammation. Science. 2011 doi: 10.1126/science.1204351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulz C, et al. A lineage of myeloid cells independent of Myb and hematopoietic stem cells. Science. 2012;336:86–90. doi: 10.1126/science.1219179. [DOI] [PubMed] [Google Scholar]
- 7.Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nature reviews. Immunology. 2011;11:723–737. doi: 10.1038/nri3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wynn TA, Barron L. Macrophages: master regulators of inflammation and fibrosis. Semin Liver Dis. 2010;30:245–257. doi: 10.1055/s-0030-1255354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 10.Ginhoux F, et al. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science. 2010;330:841–845. doi: 10.1126/science.1194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoeffel G, et al. Adult Langerhans cells derive predominantly from embryonic fetal liver monocytes with a minor contribution of yolk sac-derived macrophages. J Exp Med. 2012;209:1167–1181. doi: 10.1084/jem.20120340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frankenberger M, et al. A defect of CD16-positive monocytes can occur without disease. Immunobiology. 2012 doi: 10.1016/j.imbio.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 13.Hume DA. Macrophages as APC and the dendritic cell myth. J Immunol. 2008;181:5829–5835. doi: 10.4049/jimmunol.181.9.5829. [DOI] [PubMed] [Google Scholar]
- 14.Satpathy AT, Wu X, Albring JC, Murphy KM. Re(de)fining the dendritic cell lineage. Nat Immunol. 2012;13:1145–1154. doi: 10.1038/ni.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chitu V, Stanley ER. Colony-stimulating factor-1 in immunity and inflammation. Current opinion in immunology. 2006;18:39–48. doi: 10.1016/j.coi.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Erblich B, Zhu L, Etgen AM, Dobrenis K, Pollard JW. Absence of colony stimulation factor-1 receptor results in loss of microglia, disrupted brain development and olfactory deficits. PLoS One. 2011;6:e26317. doi: 10.1371/journal.pone.0026317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wei S, et al. Functional overlap but differential expression of CSF-1 and IL-34 in their CSF-1 receptor-mediated regulation of myeloid cells. Journal of Leukocyte Biology. 2010;88:495–505. doi: 10.1189/jlb.1209822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, et al. IL-34 is a tissue-restricted ligand of CSF1R required for the development of Langerhans cells and microglia. Nat Immunol. 2012 doi: 10.1038/ni.2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pollard JW. Trophic macrophages in development and disease. Nat Rev Immunol. 2009;9:259–270. doi: 10.1038/nri2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niida S, et al. Vascular endothelial growth factor can substitute for macrophage colony-stimulating Factor in the Support of Osteoclastic Bone Resorption. Journal of Experimental Medicine. 1999;190:293–298. doi: 10.1084/jem.190.2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton JA, Achuthan A. Colony stimulating factors and myeloid cell biology in health and disease. Trends in immunology. 2012 doi: 10.1016/j.it.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Miller JC, et al. Deciphering the transcriptional network of the dendritic cell lineage. Nature immunology. 2012;13:888–899. doi: 10.1038/ni.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hume DA. The complexity of constitutive and inducible gene expression in mononuclear phagocytes. Journal of Leukocyte Biology. 2012 doi: 10.1189/jlb.0312166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Edwards JR, Mundy GR. Advances in osteoclast biology: old findings and new insights from mouse models. Nature reviews. Rheumatology. 2011;7:235–243. doi: 10.1038/nrrheum.2011.23. [DOI] [PubMed] [Google Scholar]
- 25.Bigley V, et al. The human syndrome of dendritic cell, monocyte, B and NK lymphoid deficiency. Journal of Experimental Medicine. 2011;208:227–234. doi: 10.1084/jem.20101459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stefater JA, 3rd, Ren S, Lang RA, Duffield JS. Metchnikoff’s policemen: macrophages in development, homeostasis and regeneration. Trends in molecular medicine. 2011 doi: 10.1016/j.molmed.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gyorki DE, Asselin-Labat ML, van Rooijen N, Lindeman GJ, Visvader JE. Resident macrophages influence stem cell activity in the mammary gland. Breast Cancer Res. 2009;11:R62. doi: 10.1186/bcr2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pull SL, Doherty JM, Mills JC, Gordon JI, Stappenbeck TS. Activated macrophages are an adaptive element of the colonic epithelial progenitor niche necessary for regenerative responses to injury. Proc Natl Acad Sci U S A. 2005;102:99–104. doi: 10.1073/pnas.0405979102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chow A, et al. Bone marrow CD169+ macrophages promote the retention of hematopoietic stem and progenitor cells in the mesenchymal stem cell niche. Journal of Experimental Medicine. 2011;208:261–271. doi: 10.1084/jem.20101688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boulter L, et al. Macrophage-derived Wnt opposes Notch signaling to specify hepatic progenitor cell fate in chronic liver disease. Nat Med. 2012;18:572–579. doi: 10.1038/nm.2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawane K, et al. Requirement of DNase II for definitive erythropoiesis in the mouse fetal liver. Science. 2001;292:1546–1549. doi: 10.1126/science.292.5521.1546. [DOI] [PubMed] [Google Scholar]
- 32.Jaiswal S, et al. CD47 is upregulated on circulating hematopoietic stem cells and leukemia cells to avoid phagocytosis. Cell. 2009;138:271–285. doi: 10.1016/j.cell.2009.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordy C, Pua H, Sempowski GD, He YW. Regulation of steady-state neutrophil homeostasis by macrophages. Blood. 2011;117:618–629. doi: 10.1182/blood-2010-01-265959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dai X, et al. Targeted disruption of the mouse CSF-1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primititive progenitor cell frequencies and reproductive defects. Blood. 2002;99:111–120. doi: 10.1182/blood.v99.1.111. [DOI] [PubMed] [Google Scholar]
- 35.Savill J, Dransfield I, Gregory C, Haslett C. A blast from the past: clearance of apoptotic cells regulates immune responses. Nat Rev Immunol. 2002;2:965–975. doi: 10.1038/nri957. [DOI] [PubMed] [Google Scholar]
- 36.Rao S, et al. Development. Vol. 134. Cambridge, England: 2007. Obligatory participation of macrophages in an angiopoietin 2– mediated cell death switch; pp. 4449–4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stefater JA, 3rd, et al. Regulation of angiogenesis by a non-canonical Wnt-Flt1 pathway in myeloid cells. Nature. 2011;474:511–515. doi: 10.1038/nature10085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tammela T, et al. VEGFR-3 controls tip to stalk conversion at vessel fusion sites by reinforcing Notch signalling. Nature cell biology. 2011;13:1202–1213. doi: 10.1038/ncb2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fantin A, et al. Tissue macrophages act as cellular chaperones for vascular anastomosis downstream of VEGF-mediated endothelial tip cell induction. Blood. 2010;116:829–840. doi: 10.1182/blood-2009-12-257832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gordon EJ, et al. Development. Vol. 137. Cambridge, England: 2010. Macrophages define dermal lymphatic vessel calibre during development by regulating lymphatic endothelial cell proliferation; pp. 3899–3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Machnik A, et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nature Medicine. 2009;15:545–552. doi: 10.1038/nm.1960. [DOI] [PubMed] [Google Scholar]
- 42.Nandi S, et al. The CSF-1 receptor ligands IL-34 and CSF-1 exhibit distinct developmental brain expression patterns and regulate neural progenitor cell maintenance and maturation. Developmental biology. 2012;367:100–113. doi: 10.1016/j.ydbio.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li Y, Du XF, Liu CS, Wen ZL, Du JL. Reciprocal Regulation between Resting Microglial Dynamics and Neuronal Activity In Vivo. Developmental cell. 2012;23:1189–1202. doi: 10.1016/j.devcel.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 44.Paolicelli RC, et al. Synaptic pruning by microglia is necessary for normal brain development. Science. 2011;333:1456–1458. doi: 10.1126/science.1202529. [DOI] [PubMed] [Google Scholar]
- 45.Rademakers R, et al. Mutations in the colony stimulating factor 1 receptor (CSF1R) gene cause hereditary diffuse leukoencephalopathy with spheroids. Nature genetics. 2012;44:200–205. doi: 10.1038/ng.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.London A, et al. Neuroprotection and progenitor cell renewal in the injured adult murine retina requires healing monocyte-derived macrophages. J Exp Med. 2011;208:23–39. doi: 10.1084/jem.20101202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kigerl KA, et al. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29:13435–13444. doi: 10.1523/JNEUROSCI.3257-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Salegio EA, Pollard AN, Smith M, Zhou XF. Macrophage presence is essential for the regeneration of ascending afferent fibres following a conditioning sciatic nerve lesion in adult rats. BMC neuroscience. 2011;12:11. doi: 10.1186/1471-2202-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 50.Chawla A, Nguyen KD, Goh YP. Macrophage-mediated inflammation in metabolic disease. Nat Rev Immunol. 2011;11:738–749. doi: 10.1038/nri3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Odegaard JI, Chawla A. Pleiotropic actions of insulin resistance and inflammation in metabolic homeostasis. Science. 2013;229:172–177. doi: 10.1126/science.1230721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Olefsky J, Glass C. Macrophages, Inflammation, and Insulin Resistance. Annu Rev Physiol. 2010;72:1–28. doi: 10.1146/annurev-physiol-021909-135846. [DOI] [PubMed] [Google Scholar]
- 53.Rosen ED, Spiegelman BM. Adipocytes as regulators of energy balance and glucose homeostasis. Nature. 2006;444:847–853. doi: 10.1038/nature05483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117:175–184. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weisberg SP, et al. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–1808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu H, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–1830. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sun K, Kusminski CM, Scherer PE. Adipose tissue remodeling and obesity. J Clin Invest. 2011;121:2094–2101. doi: 10.1172/JCI45887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kang K, et al. Adipocyte-derived Th2 cytokines and myeloid PPARdelta regulate macrophage polarization and insulin sensitivity. Cell Metab. 2008;7:485–495. doi: 10.1016/j.cmet.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liao X, et al. Kruppel-like factor 4 regulates macrophage polarization. J Clin Invest. 2011;121:2736–2749. doi: 10.1172/JCI45444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Odegaard JI, et al. Macrophage-specific PPARgamma controls alternative activation and improves insulin resistance. Nature. 2007;447:1116–1120. doi: 10.1038/nature05894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Odegaard JI, et al. Alternative M2 activation of Kupffer cells by PPARdelta ameliorates obesity-induced insulin resistance. Cell Metab. 2008;7:496–507. doi: 10.1016/j.cmet.2008.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu D, et al. Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science. 2011;332:243–247. doi: 10.1126/science.1201475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Weisberg SP, et al. CCR2 modulates inflammatory and metabolic effects of high-fat feeding. J Clin Invest. 2006;116:115–124. doi: 10.1172/JCI24335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cinti S, et al. Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J Lipid Res. 2005;46:2347–2355. doi: 10.1194/jlr.M500294-JLR200. [DOI] [PubMed] [Google Scholar]
- 65.Lowell BB, Spiegelman BM. Towards a molecular understanding of adaptive thermogenesis. Nature. 2000;404:652–660. doi: 10.1038/35007527. [DOI] [PubMed] [Google Scholar]
- 66.Nguyen KD, et al. Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nature. 2011;480:104–108. doi: 10.1038/nature10653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Samuel VT, Shulman GI. Mechanisms for insulin resistance: common threads and missing links. Cell. 2012;148:852–871. doi: 10.1016/j.cell.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Huang W, et al. Depletion of liver Kupffer cells prevents the development of diet-induced hepatic steatosis and insulin resistance. Diabetes. 2010;59:347–357. doi: 10.2337/db09-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Eguchi K, et al. Saturated fatty acid and TLR signaling link beta cell dysfunction and islet inflammation. Cell Metab. 2012;15:518–533. doi: 10.1016/j.cmet.2012.01.023. [DOI] [PubMed] [Google Scholar]
- 70.Ehses JA, et al. Increased number of islet-associated macrophages in type 2 diabetes. Diabetes. 2007;56:2356–2370. doi: 10.2337/db06-1650. [DOI] [PubMed] [Google Scholar]
- 71.Nathan C, Ding A. Nonresolving inflammation. Cell. 2010;140:871–882. doi: 10.1016/j.cell.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 72.Sindrilaru A, et al. An unrestrained proinflammatory M1 macrophage population induced by iron impairs wound healing in humans and mice. J Clin Invest. 2011;121:985–997. doi: 10.1172/JCI44490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krausgruber T, et al. IRF5 promotes inflammatory macrophage polarization and TH1-TH17 responses. Nature immunology. 2011;12:231–238. doi: 10.1038/ni.1990. [DOI] [PubMed] [Google Scholar]
- 74.Ahn GO, et al. Inhibition of Mac-1 (CD11b/CD18) enhances tumor response to radiation by reducing myeloid cell recruitment. Proc Natl Acad Sci U S A. 2010;107:8363–8368. doi: 10.1073/pnas.0911378107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Balkwill FR, Mantovani A. Cancer-related inflammation: common themes and therapeutic opportunities. Seminars in cancer biology. 2012;22:33–40. doi: 10.1016/j.semcancer.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 77.Zaidi MR, et al. Interferon-gamma links ultraviolet radiation to melanomagenesis in mice. Nature. 2011;469:548–553. doi: 10.1038/nature09666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Deng L, et al. A novel mouse model of inflammatory bowel disease links mammalian target of rapamycin-dependent hyperproliferation of colonic epithelium to inflammation-associated tumorigenesis. American Journal of Pathology. 2010;176:952–967. doi: 10.2353/ajpath.2010.090622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Arthur JC, et al. Intestinal Inflammation Targets Cancer-Inducing Activity of the Microbiota. Science. 2012 doi: 10.1126/science.1224820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.DeNardo DG, Andreu P, Coussens LM. Interactions between lymphocytes and myeloid cells regulate pro- versus anti-tumor immunity. Cancer metastasis reviews. 2010;29:309–316. doi: 10.1007/s10555-010-9223-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hanahan D, Coussens LM. Accessories to the crime: functions of cells recruited to the tumor microenvironment. Cancer Cell. 2012;21:309–322. doi: 10.1016/j.ccr.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 82.Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006;124:263–266. doi: 10.1016/j.cell.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 83.Chen J, et al. CCL18 from tumor-associated macrophages promotes breast cancer metastasis via PITPNM3. Cancer Cell. 2011;19:541–555. doi: 10.1016/j.ccr.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mason SD, Joyce JA. Proteolytic networks in cancer. Trends Cell Biol. 2011;21:228–237. doi: 10.1016/j.tcb.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lin EY, et al. Macrophages regulate the angiogenic switch in a mouse model of breast cancer. Cancer research. 2006;66:11238–11246. doi: 10.1158/0008-5472.CAN-06-1278. [DOI] [PubMed] [Google Scholar]
- 87.Mazzieri R, et al. Targeting the ANG2/TIE2 axis inhibits tumor growth and metastasis by impairing angiogenesis and disabling rebounds of proangiogenic myeloid cells. Cancer Cell. 2011;19:512–526. doi: 10.1016/j.ccr.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 88.Murdoch C, Muthana M, Coffelt SB, Lewis CE. The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer. 2008;8:618–631. doi: 10.1038/nrc2444. [DOI] [PubMed] [Google Scholar]
- 89.Stockmann C, et al. Deletion of vascular endothelial growth factor in myeloid cells accelerates tumorigenesis. Nature. 2008;456:814–818. doi: 10.1038/nature07445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shojaei F, et al. Tumor refractoriness to anti-VEGF treatment is mediated by CD11b+Gr1+ myeloid cells. Nature biotechnology. 2007;25:911–920. doi: 10.1038/nbt1323. [DOI] [PubMed] [Google Scholar]
- 91.Du R, et al. HIF1alpha induces the recruitment of bone marrow-derived vascular modulatory cells to regulate tumor angiogenesis and invasion. Cancer Cell. 2008;13:206–220. doi: 10.1016/j.ccr.2008.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lin EY, et al. Vascular endothelial growth factor restores delayed tumor progression in tumors depleted of macrophages. Molecular Oncology. 2007;1:288–302. doi: 10.1016/j.molonc.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Psaila B, Lyden D. The metastatic niche: adapting the foreign soil. Nat Rev Cancer. 2009;9:285–293. doi: 10.1038/nrc2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Peinado H, et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med. 2012;18:883–891. doi: 10.1038/nm.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gil-Bernabe AM, et al. Recruitment of monocytes/macrophages by tissue factor-mediated coagulation is essential for metastatic cell survival and premetastatic niche establishment in mice. Blood. 2012;119:3164–3175. doi: 10.1182/blood-2011-08-376426. [DOI] [PubMed] [Google Scholar]
- 96.Qian BZ, et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011 doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Coussens LM, Pollard JW. Leukocytes in mammary development and cancer. Cold Spring Harb Perspect Biol. 2011;3 doi: 10.1101/cshperspect.a003285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wu Y, Zheng L. Dynamic education of macrophages in different areas of human tumors. Cancer microenvironment : official journal of the International Cancer Microenvironment Society. 2012;5:195–201. doi: 10.1007/s12307-012-0113-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hagemann T, et al. “Re-educating” tumor-associated macrophages by targeting NF-kappaB. J Exp Med. 2008;205:1261–1268. doi: 10.1084/jem.20080108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pello OM, et al. Role of c-MYC in alternative activation of human macrophages and tumor-associated macrophage biology. Blood. 2012;119:411–421. doi: 10.1182/blood-2011-02-339911. [DOI] [PubMed] [Google Scholar]
- 101.Zabuawala T, et al. An ets2-driven transcriptional program in tumor-associated macrophages promotes tumor metastasis. Cancer Res. 2010;70:1323–1333. doi: 10.1158/0008-5472.CAN-09-1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12:204–212. doi: 10.1038/ni.2001. [DOI] [PubMed] [Google Scholar]
- 103.Kamada N, et al. Unique CD14 intestinal macrophages contribute to the pathogenesis of Crohn disease via IL-23/IFN-gamma axis. J Clin Invest. 2008;118:2269–2280. doi: 10.1172/JCI34610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 105.Julia V, et al. A restricted subset of dendritic cells captures airborne antigens and remains able to activate specific T cells long after antigen exposure. Immunity. 2002;16:271–283. doi: 10.1016/s1074-7613(02)00276-5. [DOI] [PubMed] [Google Scholar]
- 106.Ford AQ, et al. Adoptive transfer of IL-4Ralpha(+) macrophages is sufficient to enhance eosinophilic inflammation in a mouse model of allergic lung inflammation. BMC Immunol. 2012;13:6. doi: 10.1186/1471-2172-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Moreira AP, et al. Serum amyloid P attenuates M2 macrophage activation and protects against fungal spore-induced allergic airway disease. The Journal of allergy and clinical immunology. 2010;126:712–721. doi: 10.1016/j.jaci.2010.06.010. e717. [DOI] [PubMed] [Google Scholar]
- 108.Melgert BN, et al. More alternative activation of macrophages in lungs of asthmatic patients. The Journal of allergy and clinical immunology. 2011;127:831–833. doi: 10.1016/j.jaci.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 109.Nieuwenhuizen NE, et al. Allergic airway disease is unaffected by the absence of IL-4Ralpha-dependent alternatively activated macrophages. The Journal of allergy and clinical immunology. 2012 doi: 10.1016/j.jaci.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 110.Murray PJ, Wynn TA. Obstacles and opportunities for understanding macrophage polarization. J Leukoc Biol. 2011;89:557–563. doi: 10.1189/jlb.0710409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ponomarev ED, Veremeyko T, Barteneva N, Krichevsky AM, Weiner HL. MicroRNA-124 promotes microglia quiescence and suppresses EAE by deactivating macrophages via the C/EBP-alpha-PU.1 pathway. Nat Med. 2011;17:64–70. doi: 10.1038/nm.2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Platt AM, Bain CC, Bordon Y, Sester DP, Mowat AM. An independent subset of TLR expressing CCR2-dependent macrophages promotes colonic inflammation. J Immunol. 2010;184:6843–6854. doi: 10.4049/jimmunol.0903987. [DOI] [PubMed] [Google Scholar]
- 113.Rivollier A, He J, Kole A, Valatas V, Kelsall BL. Inflammation switches the differentiation program of Ly6Chi monocytes from antiinflammatory macrophages to inflammatory dendritic cells in the colon. The Journal of experimental medicine. 2012;209:139–155. doi: 10.1084/jem.20101387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gelderman KA, et al. Macrophages suppress T cell responses and arthritis development in mice by producing reactive oxygen species. J Clin Invest. 2007;117:3020–3028. doi: 10.1172/JCI31935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Smith AM, et al. Disordered macrophage cytokine secretion underlies impaired acute inflammation and bacterial clearance in Crohn’s disease. J Exp Med. 2009;206:1883–1897. doi: 10.1084/jem.20091233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Murai M, et al. Interleukin 10 acts on regulatory T cells to maintain expression of the transcription factor Foxp3 and suppressive function in mice with colitis. Nat Immunol. 2009;10:1178–1184. doi: 10.1038/ni.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hoek RM, et al. Down-regulation of the macrophage lineage through interaction with OX2 (CD200) Science. 2000;290:1768–1771. doi: 10.1126/science.290.5497.1768. [DOI] [PubMed] [Google Scholar]
- 118.Shechter R, et al. Infiltrating blood-derived macrophages are vital cells playing an anti-inflammatory role in recovery from spinal cord injury in mice. PLoS Med. 2009;6:e1000113. doi: 10.1371/journal.pmed.1000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Duffield JS, et al. Selective depletion of macrophages reveals distinct, opposing roles during liver injury and repair. J Clin Invest. 2005;115:56–65. doi: 10.1172/JCI22675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wynn TA, Ramalingam TR. Mechanisms of fibrosis: therapeutic translation for fibrotic disease. Nature medicine. 2012;18:1028–1040. doi: 10.1038/nm.2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8:958–969. doi: 10.1038/nri2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Thomas JA, et al. Macrophage therapy for murine liver fibrosis recruits host effector cells improving fibrosis, regeneration, and function. Hepatology. 2011;53:2003–2015. doi: 10.1002/hep.24315. [DOI] [PubMed] [Google Scholar]
- 123.Ravasi T, et al. An Atlas of Combinatorial Transcriptional Regulation in Mouse and Man. Cell. 2010;140:744–752. doi: 10.1016/j.cell.2010.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Frankenberger M, et al. Transcript profiling of CD16-positive monocytes reveals a unique molecular fingerprint. European journal of immunology. 2012;42:957–974. doi: 10.1002/eji.201141907. [DOI] [PubMed] [Google Scholar]
- 125.Entenberg D, et al. Setup and use of a two-laser multiphoton microscope for multichannel intravital fluorescence imaging. Nature protocols. 2011;6:1500–1520. doi: 10.1038/nprot.2011.376. [DOI] [PMC free article] [PubMed] [Google Scholar]