Proteinuria and risk of ocular motor cranial nerve palsy: a nationwide population-based study (original) (raw)
Introduction
Third, fourth, and sixth cranial nerve palsies (CNP) are known to affect extraocular muscles and cause symptoms of diplopia with or without abnormal head posture. They are common disease entities encountered in neuro-ophthalmology clinics. Along with paralysis of the facial nerve, paralysis of ocular motor cranial nerves (CNs) including CN3 (oculomotor nerve), CN4 (trochlear nerve), and/or CN6 (abducens nerve) is one of the most frequent mononeuropathies of the CN[1](/articles/s41598-024-62576-0#ref-CR1 "Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282. https://doi.org/10.1159/000444128
(2016)."). Many previous reports have revealed that ocular motor CNP (OCNP) has close associations with diseases that can causing vasculopathy, such as diabetes mellitus, hyperlipidemia, hypertension, and several circulatory diseases that can increase with age and lead to atherosclerotic changes[2](#ref-CR2 "Jung, J. S. & Kim, D. H. Risk factors and prognosis of isolated ischemic third, fourth, or sixth cranial nerve palsies in the Korean population. J. Neuroophthalmol. 35, 37–40.
https://doi.org/10.1097/WNO.0000000000000214
(2015)."),[3](#ref-CR3 "Greco, D., Gambina, F. & Maggio, F. Ophthalmoplegia in diabetes mellitus: A retrospective study. Acta Diabetol. 46, 23–26.
https://doi.org/10.1007/s00592-008-0053-8
(2009)."),[4](/articles/s41598-024-62576-0#ref-CR4 "Jacobson, D. M., McCanna, T. D. & Layde, P. M. Risk factors for ischemic ocular motor nerve palsies. Arch. Ophthalmol. 112, 961–966.
https://doi.org/10.1001/archopht.1994.01090190109029
(1994)."). Other conditions including aneurysm, trauma, neoplasm, brain stem infarction, infection, inflammation, sinus thrombosis, and multiple sclerosis can also cause the development of OCNP[5](#ref-CR5 "Lavin, P. J. et al. Isolated trochlear nerve palsy in patients with multiple sclerosis. Neurology 55, 321–322.
https://doi.org/10.1212/wnl.55.2.321-a
(2000)."),[6](#ref-CR6 "Munakata, A., Ohkuma, H., Nakano, T. & Shimamura, N. Abducens nerve pareses associated with aneurysmal subarachnoid hemorrhage. Incid. Clin. Featur. Cerebrovasc. Dis. 24, 516–519.
https://doi.org/10.1159/000110421
(2007)."),[7](#ref-CR7 "Rush, J. A. & Younge, B. R. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1000 cases. Arch. Ophthalmol. 99, 76–79.
https://doi.org/10.1001/archopht.1981.03930010078006
(1981)."),[8](/articles/s41598-024-62576-0#ref-CR8 "Thömke, F., Gutmann, L., Stoeter, P. & Hopf, H. C. Cerebrovascular brainstem diseases with isolated cranial nerve palsies. Cerebrovasc. Dis. 13, 147–155.
https://doi.org/10.1159/000047768
(2002)."). Although heterogeneous mechanisms might be involved in the development of OCNP[5](#ref-CR5 "Lavin, P. J. et al. Isolated trochlear nerve palsy in patients with multiple sclerosis. Neurology 55, 321–322.
https://doi.org/10.1212/wnl.55.2.321-a
(2000)."),[6](#ref-CR6 "Munakata, A., Ohkuma, H., Nakano, T. & Shimamura, N. Abducens nerve pareses associated with aneurysmal subarachnoid hemorrhage. Incid. Clin. Featur. Cerebrovasc. Dis. 24, 516–519.
https://doi.org/10.1159/000110421
(2007)."),[7](#ref-CR7 "Rush, J. A. & Younge, B. R. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1000 cases. Arch. Ophthalmol. 99, 76–79.
https://doi.org/10.1001/archopht.1981.03930010078006
(1981)."),[8](/articles/s41598-024-62576-0#ref-CR8 "Thömke, F., Gutmann, L., Stoeter, P. & Hopf, H. C. Cerebrovascular brainstem diseases with isolated cranial nerve palsies. Cerebrovasc. Dis. 13, 147–155.
https://doi.org/10.1159/000047768
(2002)."), microvascular ischemia caused by atherosclerosis is the most widely postulated mechanism for OCNP[1](/articles/s41598-024-62576-0#ref-CR1 "Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282.
https://doi.org/10.1159/000444128
(2016).").Chronic kidney disease (CKD) is a worldwide public health problem. It has been estimated that approximately 10–15% of adults in developed countries are affected by CKD[9](#ref-CR9 "Coresh, J., Astor, B. C., Greene, T., Eknoyan, G. & Levey, A. S. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 41, 1–12. https://doi.org/10.1053/ajkd.2003.50007
(2003)."),[10](#ref-CR10 "Coresh, J. et al. Prevalence of chronic kidney disease in the United States. Jama 298, 2038–2047.
https://doi.org/10.1001/jama.298.17.2038
(2007)."),[11](/articles/s41598-024-62576-0#ref-CR11 "Chadban, S. J. et al. Prevalence of kidney damage in Australian adults: The AusDiab kidney study. J. Am. Soc. Nephrol. 14, S131-138.
https://doi.org/10.1097/01.asn.0000070152.11927.4a
(2003)."). CKD is also known to cause neurological complications in peripheral and central nervous systems[12](/articles/s41598-024-62576-0#ref-CR12 "Jabbari, B. & Vaziri, N. D. The nature, consequences, and management of neurological disorders in chronic kidney disease. Hemodial. Int. 22, 150–160.
https://doi.org/10.1111/hdi.12587
(2018)."). Complications in peripheral nervous system include somatic neuropathy, myopathy, and cranial neuropathy[12](/articles/s41598-024-62576-0#ref-CR12 "Jabbari, B. & Vaziri, N. D. The nature, consequences, and management of neurological disorders in chronic kidney disease. Hemodial. Int. 22, 150–160.
https://doi.org/10.1111/hdi.12587
(2018)."). Among those with cranial neuropathies, acoustic and olfactory nerves are frequently involved[12](/articles/s41598-024-62576-0#ref-CR12 "Jabbari, B. & Vaziri, N. D. The nature, consequences, and management of neurological disorders in chronic kidney disease. Hemodial. Int. 22, 150–160.
https://doi.org/10.1111/hdi.12587
(2018)."), whereas optic neuropathy is rarely reported[13](/articles/s41598-024-62576-0#ref-CR13 "Saini, J. S., Jain, I. S., Dhar, S. & Mohan, K. Uremic optic neuropathy. J. Clin. Neuro-ophthalmol. 9, 131–133 (1989)."). Cognitive dysfunction, delirium, encephalopathy, dementia, focal stroke-related symptoms, and cortically originated abnormal movements such as cortical myoclonus, asterixis, and epileptic seizures are central nervous system disorders known to be associated with CKD[12](/articles/s41598-024-62576-0#ref-CR12 "Jabbari, B. & Vaziri, N. D. The nature, consequences, and management of neurological disorders in chronic kidney disease. Hemodial. Int. 22, 150–160.
https://doi.org/10.1111/hdi.12587
(2018).").Proteinuria is a biomarker of kidney damage that can predict early stages of CKD[14](/articles/s41598-024-62576-0#ref-CR14 "Watson, D. et al. A novel multi-biomarker assay for non-invasive quantitative monitoring of kidney injury. J. Clin. Med. 8, 499. https://doi.org/10.3390/jcm8040499
(2019)."). Its severity is correlated with a rapid decline in renal function[15](/articles/s41598-024-62576-0#ref-CR15 "Turin, T. C. et al. Proteinuria and rate of change in kidney function in a community-based population. J. Am. Soc. Nephrol. 24, 1661–1667.
https://doi.org/10.1681/ASN.2012111118
(2013)."). Proteinuria can also predict patients at increased risk of adverse clinical outcomes regardless of the estimated glomerular filtration rate (eGFR)[16](/articles/s41598-024-62576-0#ref-CR16 "Hemmelgarn, B. R. et al. Relation between kidney function, proteinuria, and adverse outcomes. Jama 303, 423–429.
https://doi.org/10.1001/jama.2010.39
(2010)."). Proteinuria is known to manifest endothelial dysfunction and systemic inflammation[17](/articles/s41598-024-62576-0#ref-CR17 "Paisley, K. E. et al. Endothelial dysfunction and inflammation in asymptomatic proteinuria. Kidney Int. 63, 624–633.
https://doi.org/10.1046/j.1523-1755.2003.00768.x
(2003)."). It has been recently shown that proteinuria is associated with metabolic syndrome, hypertension, diabetes, fatty liver, Parkinson’s disease, and Crohn’s disease. In addition, proteinuria is associated with a worsening disease course in stroke, non-Hodgkin’s lymphoma, and endocarditis[18](#ref-CR18 "Nam, G. E. et al. Chronic renal dysfunction, proteinuria, and risk of Parkinson’s disease in the elderly. Mov. Disord. 34, 1184–1191.
https://doi.org/10.1002/mds.27704
(2019)."),[19](#ref-CR19 "Okada, R. et al. Trace proteinuria by dipstick screening is associated with metabolic syndrome, hypertension, and diabetes. Clin. Exp. Nephrol. 22, 1387–1394.
https://doi.org/10.1007/s10157-018-1601-3
(2018)."),[20](#ref-CR20 "Park, S. et al. Proteinuria is associated with the development of Crohn’s disease: A nationwide population-based study. J Clin Med
https://doi.org/10.3390/jcm10040799
(2021)."),[21](#ref-CR21 "Sun, K. et al. Fatty liver index, albuminuria and the association with chronic kidney disease: a population-based study in China. BMJ Open 8, e019097.
https://doi.org/10.1136/bmjopen-2017-019097
(2018)."),[22](/articles/s41598-024-62576-0#ref-CR22 "Wang, A. et al. Two-year changes in proteinuria and the risk of stroke in the Chinese population: A prospective cohort study. J. Am. Heart Assoc.
https://doi.org/10.1161/JAHA.117.006271
(2017)."). In recent years, the use of human urine samples to search for biomarkers has gained increasing interest due to its convenient and non-invasive collection with stable compositions[23](/articles/s41598-024-62576-0#ref-CR23 "Filip, S. et al. Urinary proteomics and molecular determinants of chronic kidney disease: Possible link to proteases. Expert Rev. Proteomics 11, 535–548.
https://doi.org/10.1586/14789450.2014.926224
(2014)."). Although urine protein-to-creatinine ratio (PCR) and urine albumin-to-creatinine ratio (ACR) are used as quantitative tests for proteinuria, their application in public health screening is prohibitively expensive. In addition, it takes a significant amount of time to confirm their results. However, a urine dipstick test is a relatively simple, fast, and inexpensive method for screening proteinuria in public healthcare systems.To the best of our knowledge, studies examining the association between proteinuria and the development of OCNP are uncommon. Thus, the purpose of this study was to determine the association of dipstick-determined proteinuria with OCNP using a large general population.
Results
Baseline clinical characteristics
A total of 4,053,012 subjects were eligible for this study. They were tracked for 33,305,711.65 person-years. According to the degree of proteinuria, they were divided into six groups: negative (n = 3,857,777, 95.18%), trace (n = 92,700, 2.29%), 1 + (68,923, 1.70%), 2 + (25,728, 0.63%), 3 + (6577, 0.16%), and 4 + (1307, 0.03%). Baseline characteristics were compared among subjects with varying degrees of proteinuria (Table 1). Age and waist measurements were positively correlated with the severity of proteinuria (both P < 0.001). Additionally, the group with severe proteinuria had higher rates of co-morbid conditions such as hypertension, diabetes, and dyslipidemia (all P < 0.001). However, individuals with higher levels of proteinuria had significantly lower rates of current smoking (P < 0.001). Other variables including gender, alcohol consumption, regular exercise, low income, and eGFR demonstrated significant differences according to proteinuria severity (all P < 0.0001).
Table 1 Baseline characteristics of patients with ocular motor cranial nerve palsy and controls.
Incidence and risk of OCNP according to proteinuria level by dipstick.
Among eligible subjects, 5,807 developed OCNP. They were assigned to the OCNP group. Remaining subjects (n = 4,047,205) were assigned to the control group. The incidence of OCNP was 0.14%. The average duration of follow-up was 8.22 ± 0.94 years.
The risk of developing OCNP was significantly higher in the proteinuria-positive group than in the proteinuria-negative group (crude hazard ratios [HRs] : 1.848, 2.939, 2.971, and 4.89 in 1 + , 2 + , 3 + and 4 + proteinuria groups, respectively, Model 1 in Table 2). A higher degree of proteinuria on the dipstick test was associated with a higher risk of developing OCNP (crude HR: 4. 89; 95% CI 2.448-9.769 in the 4+ Proteinuria group; Table 2).
Table 2 Incidence of ocular motor cranial nerve palsy according to the proteinuria.
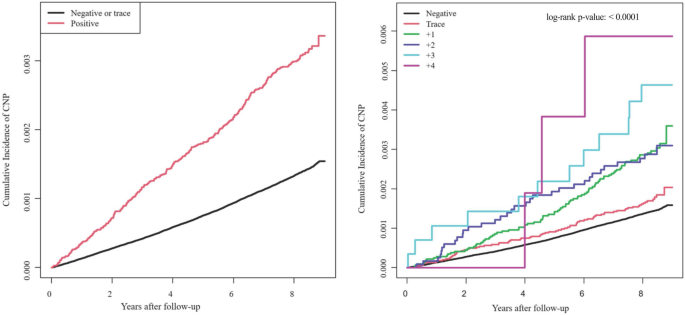
When assessing the independent relationship between proteinuria level and OCNP, we accounted for those potential confounding variables. After adjusting for age, sex, income level, smoking status, alcohol consumption status, exercise level, and comorbidities (DM, hypertension, and dyslipidemia) in model 4, the presence of proteinuria was still associated with the development of CNP. The incidence of OCNP increased with increasing urine protein levels. With the group of no proteinuria as a reference, the adjusted hazard ratio (HR) was 1.449 (95% confidence interval [CI]: 1.244–1.687) for the + 1 proteinuria group, 2.081 (95% CI 1.707–2.538) and 1.96 (95% CI 1.322-2.904) for both + 2 and + 3 proteinuria groups, and 3.011 (95% CI 1.507–6.014) for the + 4 proteinuria group (Table 2). The cumulative incidence of OCNP is displayed in Fig. 1. It increased with increasing level of proteinuria. The degree of proteinuria detected by the dipstick test was related to an increased likelihood of OCNP development (Fig. 1).
Figure 1
Kaplan–Meier curves for ocular motor cranial nerve palsy (OCNP) incidence according to the degree of dipstick proteinuria. The incidence probability of OCNP according to the presence of proteinuria (Left) and levels of proteinuria (Right) are shown.
Risk of OCNP in subgroup analysis according to age, sex, diabetes mellitus, hypertension, dyslipidemia, and metabolic syndrome
We conducted subgroup analyses to determine effects of dipstick-positive proteinuria (1 + proteinuria) on the development of OCNP stratified by age, sex, metabolism disorder, DM, hypertension, dyslipidemia, BMI, and history of cardiovascular disease (Table 3). The analysis was also adjusted for other variables such as age, sex, smoking status, drinking amount, regularity of physical activity, status of income, metabolic syndrome, and eGFR. The impact of dipstick-positive proteinuria on onset of OCNP varied significantly according to age (P = 0.0242) and DM (P = 0.04). Those with proteinuria in the age group of less than 40 years had a higher HR of 1.928 (95% CI 1.22–3.048) for the development of OCNP compared to other age groups, including the age group of 40–64-years (HR: 1.835, 95% CI 1.588–2.12) and the age group of 65 years or more (HR:1.335, 95% CI 1.077–1.655). Those with proteinuria in the DM group had a higher HR of 1.727 (95% CI 1.467–2.033) for the development of OCNP compared to the group without DM (HR:1.306, 95% CI 1.103–1.547).
Table 3 Subgroup analysis of the risk of ocular motor cranial nerve palsy among people with dipstick-positive proteinuria.
Discussion
Results of this study revealed that the incidence of OCNP among Koreans was positively associated with the presence of proteinuria. These outcomes were significant with or without adjustment for various confounders, including age, sex, smoking status, drinking amount, regularity of physical activity, the presence of metabolic syndrome, and eGFR. Especially, those with proteinuria in the age group of less than 40 years old had a higher risk of developing OCNP compared to those with proteinuria in other age groups, including the age group of 40–64 years and the age group of 65 years or more.
Proteinuria is known to be more likely to occur with aging or with comorbidities such as DM and HTN[24](/articles/s41598-024-62576-0#ref-CR24 "Boulware, L. E., Jaar, B. G., Tarver-Carr, M. E., Brancati, F. L. & Powe, N. R. Screening for proteinuria in US adults: A cost-effectiveness analysis. Jama 290, 3101–3114. https://doi.org/10.1001/jama.290.23.3101
(2003)."),[25](/articles/s41598-024-62576-0#ref-CR25 "Garg, A. X., Kiberd, B. A., Clark, W. F., Haynes, R. B. & Clase, C. M. Albuminuria and renal insufficiency prevalence guides population screening: results from the NHANES III. Kidney Int. 61, 2165–2175.
https://doi.org/10.1046/j.1523-1755.2002.00356.x
(2002)."). An epidemiological study based on the U.S. Third National Health and Nutrition Examination Survey (NHANES III) aimed to determine the association of renal insufficiency with albuminuria in whole population and in patients with DM or HTN showed similar results to ours[25](/articles/s41598-024-62576-0#ref-CR25 "Garg, A. X., Kiberd, B. A., Clark, W. F., Haynes, R. B. & Clase, C. M. Albuminuria and renal insufficiency prevalence guides population screening: results from the NHANES III. Kidney Int. 61, 2165–2175.
https://doi.org/10.1046/j.1523-1755.2002.00356.x
(2002)."). In the whole population of that study, the prevalence of albuminuria was higher in older participants: 19.1% in participants 60 years of age or older vs. < 6% in those under 40 years of age. Moreover, the prevalence of albuminuria was 34.2% in a diabetic population, 14.5% in a non-diabetic hypertensive population without DM, and 5.1% in a non-diabetic non-hypertensive population[25](/articles/s41598-024-62576-0#ref-CR25 "Garg, A. X., Kiberd, B. A., Clark, W. F., Haynes, R. B. & Clase, C. M. Albuminuria and renal insufficiency prevalence guides population screening: results from the NHANES III. Kidney Int. 61, 2165–2175.
https://doi.org/10.1046/j.1523-1755.2002.00356.x
(2002)."). However, when they observed the relationship between presence of albuminuria and renal insufficiency, 88.4% of patients with renal insufficiency showed albuminuria in those under 40 years of age, whereas only 43.6% of patients showed albuminuric renal insufficiency in those over 60–79 years of age[25](/articles/s41598-024-62576-0#ref-CR25 "Garg, A. X., Kiberd, B. A., Clark, W. F., Haynes, R. B. & Clase, C. M. Albuminuria and renal insufficiency prevalence guides population screening: results from the NHANES III. Kidney Int. 61, 2165–2175.
https://doi.org/10.1046/j.1523-1755.2002.00356.x
(2002)."). In the Heart Outcomes and Prevention Evaluation (HOPE) study, two-thirds of elderly patients with renal insufficiency showed no signs of albuminuria[26](/articles/s41598-024-62576-0#ref-CR26 "Mann, J. F., Gerstein, H. C., Pogue, J., Bosch, J. & Yusuf, S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: The HOPE randomized trial. Ann. Intern. Med. 134, 629–636.
https://doi.org/10.7326/0003-4819-134-8-200104170-00007
(2001)."). The above studies suggest that proteinuria could reflect renal function impairment better in people under 40 years of age than in elder age. In our study, proteinuria showed a greater impact on the occurrence of CNP in people under the age of 40\. Because the adjusted OR in our study was adjusted for several factors, including DM and HTN, it was hard to say that the difference in CNP occurrence was simply due to an increase of underlying disease caused by aging. We found that the occurrence of CNP was increased 1.928 (CI 1.22–3.048) times with proteinuria in young age groups (younger than 40 years). Our results suggest that caution should be exercised when proteinuria is positive in people under 40 years of age.In sub-analysis, we classified the degree of dipstick test for proteinuria from + 1 to + 4 as one group compared to negative and trace ( ±). According to the study of Iseki et al[27](/articles/s41598-024-62576-0#ref-CR27 "Iseki, K., Ikemiya, Y., Iseki, C. & Takishita, S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 63, 1468–1474. https://doi.org/10.1046/j.1523-1755.2003.00868.x
(2003).")., even a slight increase in dipstick urinalysis for proteinuria was an independent risk factor for ESRD. When the proteinuria results based on dipstick urinalysis were analyzed by dividing them to negative, trace, + 1, + 2, and ≥ + 3, the incidence of end-stage renal disease (ESRD) rose significantly and consistently as the degree of proteinuria increased. Although + 1 was not cost-effective, + 1 was found to significantly increase the risk of ESRD compared to negative (adjusted odds ratio: 1.93 (95% CI 1.53–2.41, _P_ < 0.001) in men and 2.42 (95% CI 1.91–3.06, _P_ < 0.001) in women)[27](/articles/s41598-024-62576-0#ref-CR27 "Iseki, K., Ikemiya, Y., Iseki, C. & Takishita, S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 63, 1468–1474.
https://doi.org/10.1046/j.1523-1755.2003.00868.x
(2003)."). Even a slight increase in the degree of proteinuria such as proteinuria (trace; ±) caused a change in the adjusted odds ratio (95% CI)[27](/articles/s41598-024-62576-0#ref-CR27 "Iseki, K., Ikemiya, Y., Iseki, C. & Takishita, S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 63, 1468–1474.
https://doi.org/10.1046/j.1523-1755.2003.00868.x
(2003)."). Proteinuria has been widely used as a biomarker for kidney disease in clinical practice[28](/articles/s41598-024-62576-0#ref-CR28 "Zandi-Nejad, K., Eddy, A. A., Glassock, R. J. & Brenner, B. M. Why is proteinuria an ominous biomarker of progressive kidney disease?. Kidney Int. Suppl.
https://doi.org/10.1111/j.1523-1755.2004.09220.x
(2004)."). The extent of renal dysfunction is also frequently estimated by measuring serum creatinine and calculating the eGFR[29](/articles/s41598-024-62576-0#ref-CR29 "Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080.
https://doi.org/10.1161/STROKEAHA.115.009861
(2015)."). Both eGFR and proteinuria are known to be pivotal markers for the assessment of risk such as cardiovascular risk including mortality and cardiovascular events as well as overall prognosis of CKD[30](/articles/s41598-024-62576-0#ref-CR30 "Polkinghorne, K. R. Estimated glomerular filtration rate versus albuminuria in the assessment of kidney function: What’s more important?. Clin. Biochem. Rev. 35, 67–73 (2014)."). Interpretation of results of eGFR must be done with caution because it is affected by age, sex, and lean muscle mass. In contrast, proteinuria and albuminuria are complementary indices of renal function that can assess damage to the renal filtration barrier[31](#ref-CR31 "Levey, A. S., Inker, L. A. & Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 63, 820–834.
https://doi.org/10.1053/j.ajkd.2013.12.006
(2014)."),[32](#ref-CR32 "Peralta, C. A. et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. Jama 305, 1545–1552.
https://doi.org/10.1001/jama.2011.468
(2011)."),[33](/articles/s41598-024-62576-0#ref-CR33 "Shlipak, M. G. et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl. J. Med. 369, 932–943.
https://doi.org/10.1056/NEJMoa1214234
(2013)."). Proteinuria is not simply a subsequent outcome of kidney damage. It can also pathologically produce renal tubulointerstitial damages, resulting in progressive renal function loss[34](/articles/s41598-024-62576-0#ref-CR34 "Zhuang, Y. et al. Mitochondrial dysfunction confers albumin-induced NLRP3 inflammasome activation and renal tubular injury. Am. J. Physiol. Renal Physiol. 308, F857-866.
https://doi.org/10.1152/ajprenal.00203.2014
(2015)."). Decreased eGFR or the presence of overt proteinuria is also independently related to increased all-cause mortality[35](#ref-CR35 "Iff, S. et al. Relative energy balance, CKD, and risk of cardiovascular and all-cause mortality. Am. J. Kidney Dis. 63, 437–445.
https://doi.org/10.1053/j.ajkd.2013.08.026
(2014)."),[36](#ref-CR36 "Kshirsagar, A. V. & Grubbs, V. Periodontal disease and CKD-associated morbidity: Is there now enough evidence to move from observation to intervention?. Am. J. Kidney Dis. 66, 181–183.
https://doi.org/10.1053/j.ajkd.2015.05.009
(2015)."),[37](/articles/s41598-024-62576-0#ref-CR37 "Warnock, D. G., Delanaye, P. & Glassock, R. J. Risks for all-cause mortality: Stratified by age, estimated glomerular filtration rate and albuminuria. Nephron 136, 292–297.
https://doi.org/10.1159/000455197
(2017)."). In our study, those with more than degree of + 1 in dipstick test for proteinuria showed an increase in the incidence of OCNP. As to eGFR, those with eGFR more than 90 mL/min/1.73 m2 showed an increased incidence of OCNP than those with eGFR < 60 mL/min/1.73 m2. Two issues can emerge when observing association between eGFR and risk of diseases. The first issue is that a few studies have reported that eGFR lower than 60 mL/min/1.73 m2 can be an independent predictor of mortality risk[38](/articles/s41598-024-62576-0#ref-CR38 "Cheng, T. Y. et al. Mortality risks for all causes and cardiovascular diseases and reduced GFR in a middle-aged working population in Taiwan. Am. J. Kidney Dis. 52, 1051–1060.
https://doi.org/10.1053/j.ajkd.2008.05.030
(2008)."),[39](/articles/s41598-024-62576-0#ref-CR39 "Chronic Kidney Disease Prognosis, C. et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375, 2073–2081.
https://doi.org/10.1016/S0140-6736(10)60674-5
(2010)."). However, Wu et al. have suggested that a lack of distinction below eGFR < 60 mL/min/1.73 m2 might overstate the cut-off point of eGFR to predict a result such as mortality[40](/articles/s41598-024-62576-0#ref-CR40 "Wu, J. et al. Association of estimated glomerular filtration rate and proteinuria with all-cause mortality in community-based population in China: A result from Kailuan study. Sci. Rep. 8, 2157.
https://doi.org/10.1038/s41598-018-20554-3
(2018)."). In a prospective longitudinal cohort study that included 821 consecutive patients hospitalized due to acute stroke, eGFR < 45 mL/min/1.73 m2 (vs. eGFR ≥ 60 mL/min/1.73 m2) was found to be an independent predictor of higher occurrence of death or severe sequelae after acute stoke[41](/articles/s41598-024-62576-0#ref-CR41 "Yahalom, G. et al. Chronic kidney disease and clinical outcome in patients with acute stroke. Stroke 40, 1296–1303.
https://doi.org/10.1161/STROKEAHA.108.520882
(2009)."). In addition, eGFR of < 50 mL/min/1.73 m2 (vs. eGFR ≥ 60 mL/min/1.73 m2) was significantly associated with the incidence of hypertension (HR: 1.29 (1.03–1.61)) in young to middle aged people (median age: 35 (30–40) years)[42](/articles/s41598-024-62576-0#ref-CR42 "Okumura, N. et al. Associations of proteinuria and the estimated glomerular filtration rate with incident hypertension in young to middle-aged Japanese males. Prev. Med. 60, 48–54.
https://doi.org/10.1016/j.ypmed.2013.12.009
(2014)."). Wu et al. have suggested that 45 mL/min/1.73 m2 but not 60 mL/min/1.73 m2 might be the cut-off point for eGFR as an independent predictor of all-cause mortality for a population in northern China[40](/articles/s41598-024-62576-0#ref-CR40 "Wu, J. et al. Association of estimated glomerular filtration rate and proteinuria with all-cause mortality in community-based population in China: A result from Kailuan study. Sci. Rep. 8, 2157.
https://doi.org/10.1038/s41598-018-20554-3
(2018)."). The second issue is that some results have indicated a U-shaped or J-shaped relationship between eGFR and various diseases. A multicenter population-based stroke registry-based study conducted in Japan involving 1,400,000 individuals has revealed that hazard ratios for all in-hospital death and at-discharge death/disability are higher in those with eGFR < 45 mL/min/1.73 m2 (OR: 1.54) and those with eGFR ≥ 90 mL/min/1.73 m2 (OR: 1.48) than in the reference group (eGFR = 60–89 mL/min/1.73 m2)[43](/articles/s41598-024-62576-0#ref-CR43 "Widhi Nugroho, A. et al. The association between glomerular filtration rate estimated on admission and acute stroke outcome the shiga stroke registry. J. Atheroscler. Thromb. 25, 570–579.
https://doi.org/10.5551/jat.42812
(2018)."). Another study has shown U-shaped observational associations of creatinine-based eGFR with CHD and stroke, with participants with eGFR values < 60 or > 105 mL/min/1.73 m2 having a higher risk for CHD and stroke than those with eGFR between 60 and 105 mL/min/1.73 m2[44](/articles/s41598-024-62576-0#ref-CR44 "Gaziano, L. et al. Mild-to-moderate kidney dysfunction and cardiovascular disease: Observational and mendelian randomization analyses. Circulation 146, 1507–1517.
https://doi.org/10.1161/circulationaha.122.060700
(2022)."). In our study, there was a significant difference in CNP occurrence between those with eGFR < 60 mL/min/1.73 m2 and those with eGFR > 90 mL/min/1.73 m2. CNP occurrence might have increased when eGFR levels were above 90 mL/min/1.73 m2 rather than decreased when eGFR levels were below 60 mL/min/1.73 m2. An elevated eGFR could be a potential risk factor for the development of CNP in certain populations. Further investigation into specific eGFR levels and their impact on OCNP is necessary.The most widely postulated mechanism in OCNP is microvascular ischemia to the CN due to atherosclerotic risk factors[1](/articles/s41598-024-62576-0#ref-CR1 "Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282. https://doi.org/10.1159/000444128
(2016)."), accounting for 20.7% of CN3 palsies, 18.6% of CN4 palsies, and 17.7% of CN6 palsies[7](/articles/s41598-024-62576-0#ref-CR7 "Rush, J. A. & Younge, B. R. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1000 cases. Arch. Ophthalmol. 99, 76–79.
https://doi.org/10.1001/archopht.1981.03930010078006
(1981)."),[45](/articles/s41598-024-62576-0#ref-CR45 "Rucker, C. W. The causes of paralysis of the third, fourth and sixth cranial nerves. Am. J. Ophthalmol. 61, 1293–1298.
https://doi.org/10.1016/0002-9394(66)90258-3
(1966)."). Diabetes mellitus, hyperlipidemia, and hypertension are the most prevalent microvascular ischemic conditions leading to atherosclerosis[46](/articles/s41598-024-62576-0#ref-CR46 "Richards, B. W., Jones, F. R. Jr. & Younge, B. R. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am. J. Ophthalmol. 113, 489–496.
https://doi.org/10.1016/s0002-9394(14)74718-x
(1992)."). These conditions are commonly associated with stroke[1](/articles/s41598-024-62576-0#ref-CR1 "Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282.
https://doi.org/10.1159/000444128
(2016)."). Isolated OCNP has also been reported to be a risk factor for subsequent stroke in past epidemiological studies[1](/articles/s41598-024-62576-0#ref-CR1 "Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282.
https://doi.org/10.1159/000444128
(2016)."),[47](/articles/s41598-024-62576-0#ref-CR47 "Rim, T. H., Han, J., Choi, Y. S., Lee, T. & Kim, S. S. Stroke risk among adult patients with third, fourth or sixth cranial nerve palsy: A Nationwide cohort study. Acta Ophthalmol. 95, e656–e661.
https://doi.org/10.1111/aos.13488
(2017)."),[48](/articles/s41598-024-62576-0#ref-CR48 "Park, S. J., Yang, H. K., Byun, S. J., Park, K. H. & Hwang, J. M. Ocular motor cranial nerve palsy and increased risk of stroke in the general population. PLoS One 13, e0205428.
https://doi.org/10.1371/journal.pone.0205428
(2018)."). Clinical data have revealed that patients with CN 3/4/6 palsies and those with CN3 palsies are 2.74 times and 3.69 times more likely to experience a stroke, respectively[1](/articles/s41598-024-62576-0#ref-CR1 "Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282.
https://doi.org/10.1159/000444128
(2016)."). This has been explained by a common pathophysiology shared between the underlying disease and atherosclerosis. CKD also shares conventional cardiovascular risk factors such as diabetes, hypertension, obesity, and smoking[29](/articles/s41598-024-62576-0#ref-CR29 "Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080.
https://doi.org/10.1161/STROKEAHA.115.009861
(2015)."). A cohort study has postulated that proteinuria, but not eGFR, can be a useful biomarker to predict stroke in CKD[29](/articles/s41598-024-62576-0#ref-CR29 "Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080.
https://doi.org/10.1161/STROKEAHA.115.009861
(2015)."). It proposed that CKD and cerebrovascular disease might share similar pathogenic mechanisms[29](/articles/s41598-024-62576-0#ref-CR29 "Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080.
https://doi.org/10.1161/STROKEAHA.115.009861
(2015)."). The causal mechanism between CKD and ischemic stroke is as follows. First, both the kidney and brain have microvasculature with low resistance that can be continuously perfused with a high amount of blood[29](/articles/s41598-024-62576-0#ref-CR29 "Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080.
https://doi.org/10.1161/STROKEAHA.115.009861
(2015)."). Second, endothelial damage is recognized as a common mediator of small vessel cerebrovascular disease and renal dysfunction of the brain[29](/articles/s41598-024-62576-0#ref-CR29 "Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080.
https://doi.org/10.1161/STROKEAHA.115.009861
(2015)."),[49](/articles/s41598-024-62576-0#ref-CR49 "Kang, D. H. et al. Role of the microvascular endothelium in progressive renal disease. J. Am. Soc. Nephrol. 13, 806–816.
https://doi.org/10.1681/asn.V133806
(2002)."). Endothelial damage can induce basement membrane thickening and cellular proliferation, resulting in narrowing of the vascular lumen[5](/articles/s41598-024-62576-0#ref-CR5 "Lavin, P. J. et al. Isolated trochlear nerve palsy in patients with multiple sclerosis. Neurology 55, 321–322.
https://doi.org/10.1212/wnl.55.2.321-a
(2000)."),[50](/articles/s41598-024-62576-0#ref-CR50 "Doostkam, A., Mirkhani, H., Iravani, K., Karbalay-Doust, S. & Zarei, K. Effect of rutin on diabetic auditory neuropathy in an experimental rat model. Clin. Exp. Otorhinolaryngol. 14, 259–267.
https://doi.org/10.21053/ceo.2019.02068
(2021)."). Albuminuria has been postulated to indicate systemic endothelial dysfunction[51](/articles/s41598-024-62576-0#ref-CR51 "Pedrinelli, R. et al. Microalbuminuria and endothelial dysfunction in essential hypertension. Lancet (London, England) 344, 14–18.
https://doi.org/10.1016/s0140-6736(94)91047-2
(1994)."),[52](/articles/s41598-024-62576-0#ref-CR52 "Jensen, J. S., Borch-Johnsen, K., Jensen, G. & Feldt-Rasmussen, B. Microalbuminuria reflects a generalized transvascular albumin leakiness in clinically healthy subjects. Clin. Sci. 88, 629–633.
https://doi.org/10.1042/cs0880629
(1995)."), which affects inflammatory and thrombotic cascades[53](/articles/s41598-024-62576-0#ref-CR53 "Kario, K. et al. Factor VII hyperactivity and endothelial cell damage are found in elderly hypertensives only when concomitant with microalbuminuria. Arterioscler. Thromb. Vasc. Biol. 16, 455–461.
https://doi.org/10.1161/01.atv.16.3.455
(1996)."),[54](/articles/s41598-024-62576-0#ref-CR54 "Shen, L. et al. Von Willebrand factor, ADAMTS13 activity, TNF-α and their relationships in patients with chronic kidney disease. Exp. Therap. Med. 3, 530–534.
https://doi.org/10.3892/etm.2011.432
(2012).") and contributes to atherothrombotic events such as stroke. Third, disruption of the integrity of the blood–brain barrier by uremia might have implications for small vessel disease and lacunar stroke risk[55](/articles/s41598-024-62576-0#ref-CR55 "Wardlaw, J. M., Sandercock, P. A., Dennis, M. S. & Starr, J. Is breakdown of the blood-brain barrier responsible for lacunar stroke, leukoaraiosis, and dementia?. Stroke 34, 806–812.
https://doi.org/10.1161/01.STR.0000058480.77236.B3
(2003)."). Serum component leakage into and through walls of small cerebral vessels cam lead to neuronal and glial damage, which might be an essential common mechanism for these disparate conditions[55](/articles/s41598-024-62576-0#ref-CR55 "Wardlaw, J. M., Sandercock, P. A., Dennis, M. S. & Starr, J. Is breakdown of the blood-brain barrier responsible for lacunar stroke, leukoaraiosis, and dementia?. Stroke 34, 806–812.
https://doi.org/10.1161/01.STR.0000058480.77236.B3
(2003)."). The widespread development of OCNPs in proteinuria in this study was presumed to result from a similar micro-ischemic process.This study has several limitations. Since the dipstick test can respond to proteins other than albumin, low-grade proteinuria does not always indicate albuminuria. Despite the inaccuracy of albuminuria measurement, urine dipstick test is useful for risk stratification due to its low cost and simplicity. Second, because this was a cross-sectional study, there was no evidence of a cause-and-effect relationship between OCNP and proteinuria. Third, the high cut-off value prevented the observation of the impact of a decrease in eGFR on the occurrence of CNP. Further research is required to distinguish eGFR into more specific units to uncover the U-shaped relationship between eGFR and CNP occurrence that might have been concealed. Last, there were numerous confounders between OCNP and proteinuria. Although our study showed significant results after adjusting for these confounders, additional research is required to identify biomarkers that can directly explain this mechanism more directly.
In conclusion, we found that subjects with dipstick-determined proteinuria showed an increased risk of having OCNP in a large general population. Especially, patients with proteinuria in the age group of 40 years or younger have a risk of OCNP development. If the pathophysiological mechanism linking the two diseases is investigated, a method of early OCNP prevention can be proposed.
Materials and methods
In this cohort study, medical data from Korea’s National Health Insurance Service (NHIS), a national insurer covering approximately 97% of the Korean population under the supervision of the Ministry of Health and Welfare, were analyzed. The NHIS database contains demographic data, disease codes, procedural codes, details on inpatient and outpatient care, and information on prescribed medications. The government recommends regular health checkups at least biannually for enrollees of the NHIS that all Koreans are mandatory to subscribe to[56](/articles/s41598-024-62576-0#ref-CR56 "Seong, S. C. et al. Cohort profile: The National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 7, e016640. https://doi.org/10.1136/bmjopen-2017-016640
(2017)."),[57](/articles/s41598-024-62576-0#ref-CR57 "Song, S. O. et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diab. Metab. J. 38, 395–403.
https://doi.org/10.4093/dmj.2014.38.5.395
(2014)."). In the above database, the NHIS National Sample Cohort (NSC) database of Korea were utilized to investigate the association between chronic kidney disease and OCNP in Korean adults.Data of 4,233,273 individuals aged 20 years or more who underwent regular health checkups in 2009 were collected. This study assessed a total of 4,053,012 eligible persons after removing those who had previously been diagnosed with OCNP (n = 2872), those with missing data (n = 166,467), and those who were newly diagnosed with OCNP or who died within one year of being tested (n = 10,922). Participants ultimately included in the study population were tracked until December 31, 2018. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes were used to identify patients who had recently developed ocular motor CNP. A one-year time lag was established to prevent a situation in which the causal link was inverted.
This study adhered to principles outlined in the Declaration of Helsinki. It was authorized by the Institutional Review Board (IRB) of Samsung Medical Center (IRB no. SMC 2020-09-050). Patients' informed consent was waived because data used in this study were publicly accessible and anonymized in accordance with confidentiality guidelines.
Definition of OCNP and confounders
This study’s primary outcome was a newly developed OCNP. For identifying OCNP, ICD-10 codes H49.0 (3rd CNP), H49.1 (4th CNP), and H49.2 (6th CNP) were utilized. In this study, those with diagnosis codes of H06.2 (dysthyroid exophthalmos), E05 (thyrotoxicosis), or G70.0 (myasthenia gravis) were excluded[58](/articles/s41598-024-62576-0#ref-CR58 "Kim, J., Han, K., Yoo, J., Park, K. A. & Oh, S. Y. Liver enzymes and risk of ocular motor cranial nerve palsy: a nationwide population-based study. Neurol Sci 43, 3395–3405. https://doi.org/10.1007/s10072-021-05735-9
(2022)."). Age, gender, income status, smoking status, regular physical activity, and drinking amount were considered as confounding variables in the relationship between OCNP and proteinuria.Baseline data including age, findings at physical examination, and laboratory data were collected at the time of diagnosis of proteinuria. Physical examinations including height, weight, body mass index (BMI), blood pressure, and basic laboratory tests were used as covariates. Body mass index (BMI) was calculated by dividing weight (kg) by an individual's height (in meters) squared. Using self-reported questionnaires, information on past medical history and social history (including alcohol consumption and smoking status, and physical activity) were gathered. Information was gathered from the questionnaire completed at the time of proteinuria diagnosis. Lifestyle habits were recorded as either current or past depending on the time of diagnosis. Participants in the study were classified as either nonsmokers, formerly smoking individuals, or currently smoking individuals about their smoking status. Regarding the use of alcohol, participants were considered heavy drinkers if they consumed more than 30 g of alcohol per day[59](/articles/s41598-024-62576-0#ref-CR59 "Agarwal, D. P. Cardioprotective effects of light-moderate consumption of alcohol: a review of putative mechanisms. Alcohol Alcohol. (Oxford, Oxfordshire) 37, 409–415. https://doi.org/10.1093/alcalc/37.5.409
(2002)."). We considered individuals to be engaging in a regular physical activity if they performed at least 20 min of high-intensity exercise three times per week or 30 min of moderate-intensity exercise five times per week. Income levels were separated into the bottom 20% and the rest.Participants' baseline comorbidities were determined using their medical histories in conjunction with clinical and pharmacy codes of the ICD-10-CM. Comorbidities such as hypertension, diabetes, and dyslipidemia were adjusted according to the following criteria as described previously[58](/articles/s41598-024-62576-0#ref-CR58 "Kim, J., Han, K., Yoo, J., Park, K. A. & Oh, S. Y. Liver enzymes and risk of ocular motor cranial nerve palsy: a nationwide population-based study. Neurol Sci 43, 3395–3405. https://doi.org/10.1007/s10072-021-05735-9
(2022)."). Hypertension was defined as getting antihypertensive drugs at least once a year under ICD-10-CM codes I10-I13, I15, or having a blood pressure of 140/90 mmHg or higher. Diabetes mellitus (DM) was defined as having a fasting glucose level of more than 126 mg/dL or getting a prescription for hypoglycemic drugs at least once a year under ICD-10-CM code E11-E14\. Dyslipidemia was defined as having a total cholesterol level of 240 mg/dL or higher or as at least one claim per year for prescription of a lipid-lowering drug under ICD-10-CM code E78.To define metabolic syndrome, we used the same criteria as described in a previous study[58](/articles/s41598-024-62576-0#ref-CR58 "Kim, J., Han, K., Yoo, J., Park, K. A. & Oh, S. Y. Liver enzymes and risk of ocular motor cranial nerve palsy: a nationwide population-based study. Neurol Sci 43, 3395–3405. https://doi.org/10.1007/s10072-021-05735-9
(2022)."). Both modified criteria of the National Cholesterol Education Program Adult Treatment Panel III and modified waist circumference (WC) cutoff for Asians were used to define metabolic syndrome[60](/articles/s41598-024-62576-0#ref-CR60 "Kim, M. K. et al. Clinical practice guidelines for overweight and obesity in Korea. Endocrinol. Metab. (Seoul) 29, 405–409.
https://doi.org/10.3803/EnM.2014.29.4.405
(2014)."),[61](/articles/s41598-024-62576-0#ref-CR61 "Alberti, K. G. et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645.
https://doi.org/10.1161/CIRCULATIONAHA.109.192644
(2009)."). Individuals were considered to have metabolic syndrome if they possessed at least three of the following characteristics: (i) abdominal obesity, WC ≥ 90 cm for men or ≥ 85 cm for women; (ii) hypertriglyceridemia, serum triglycerides ≥ 1.70 mmol/L or treatment with lipid-lowering medication; (iii) low high-density lipoprotein (HDL), serum HDL-cholesterol < 1.04 mmol/L for men or < 1.30 mmol/L for women or treatment with lipid-lowering medication; (iv) hypertension, systolic blood pressure (BP) ≥ 130 mmHg, diastolic BP ≥ 85 mmHg, or treatment with antihypertensive medication; and (v) glucose intolerance, fasting plasma glucose ≥ 5.55 mmol/L or use of hypoglycemic agents.Definition of proteinuria
Proteinuria was determined using a urine dipstick test. With high sensitivity and specificity of more than 90%, the urine dipstick test can find proteinuria when the reference standard is ACR 300 mg/g.[62](/articles/s41598-024-62576-0#ref-CR62 "White, S. L. et al. Diagnostic accuracy of urine dipsticks for detection of albuminuria in the general community. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 58, 19–28. https://doi.org/10.1053/j.ajkd.2010.12.026
(2011)."),[63](/articles/s41598-024-62576-0#ref-CR63 "Lim, D. et al. Diagnostic accuracy of urine dipstick for proteinuria in older outpatients. Kidney Res. Clin. Pract. 33, 199–203.
https://doi.org/10.1016/j.krcp.2014.10.003
(2014).") In the urine dipstick test, the degree of proteinuria was measured as negative, trace, 1 + , 2 + , 3 + , or 4 + according to proteinuria concentration-dependent color difference. The color of the dipstick, which ranged from negative to + 4, corresponded to the following urine protein concentrations: undetectable, 10 mg/dL, 30mg/dL, 100 mg/dL, 300mg/dL, and 1000 mg/dL, respectively.The study population was classified into six groups according to the degree of proteinuria (negative, trace, 1 + , 2 + , 3 + , and 4 +). The eGFR was calculated using the following formula from the Modification of Diet in Renal Disease study: eGFR = 175 serum creatinine-1.154 age-0.203 0.70 (for women)[18](/articles/s41598-024-62576-0#ref-CR18 "Nam, G. E. et al. Chronic renal dysfunction, proteinuria, and risk of Parkinson’s disease in the elderly. Mov. Disord. 34, 1184–1191. https://doi.org/10.1002/mds.27704
(2019)."),[31](/articles/s41598-024-62576-0#ref-CR31 "Levey, A. S., Inker, L. A. & Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 63, 820–834.
https://doi.org/10.1053/j.ajkd.2013.12.006
(2014).").Statistical analysis
For continuous variables, data are presented as mean and standard deviation. For categorical variables, data are presented as numbers and percentages. Baseline characteristics were compared according to levels of proteinuria using either analysis of variance (ANOVA) for continuous variables or chi-squared test for categorical variables. Baseline characteristics are primarily presented as mean ± standard deviation (SD). The incidence of OCNP was expressed as the incidence rate per 100,000 person-years by dividing the number of cases of OCNP by the total number of person-years. Using the Kaplan–Meier method and the log-rank test, the cumulative incidence of ONCP was compared by proteinuria level.
To examine the relationship between proteinuria and the risk of OCNP, we used the Cox proportional hazards model and reported results as HRs with 95% confidence intervals (CIs). To adjust for other potential confounding factors, we independently set up and compared four models. Model 1 was analyzed without adjustment. Model 2 was adjusted for gender and age. Model 3 was adjusted for gender, age, smoking status, alcohol consumption, regularity of physical activity, and income status. Model 4 was adjusted for gender, age, smoking status, alcohol consumption, regularity of physical activity, income status, metabolic syndrome, and eGFR. HR and CI were also determined to evaluate the risk of incidence of OCNP in relation to the level of proteinuria detected by a dipstick test. Statistical significance was considered if _p_-value was less than 0.05. All statistical analyses were conducted using SAS software version 9.3 (SAS Institute, Cary, NC, USA).
Data availability
The data used in the current study were obtained under a license from the National Health Insurance Sharing Service of Korea and are not publicly available. Data can be accessed by the corresponding author, Kyung-Ah Park, upon a reasonable request and with the permission of the National Health Insurance Sharing Service of Korea.
References
- Hoi, C. P., Chen, Y. T., Fuh, J. L., Yang, C. P. & Wang, S. J. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: A nationwide cohort study. Cerebrovasc. Dis. 41, 273–282. https://doi.org/10.1159/000444128 (2016).
Article PubMed Google Scholar - Jung, J. S. & Kim, D. H. Risk factors and prognosis of isolated ischemic third, fourth, or sixth cranial nerve palsies in the Korean population. J. Neuroophthalmol. 35, 37–40. https://doi.org/10.1097/WNO.0000000000000214 (2015).
Article PubMed Google Scholar - Greco, D., Gambina, F. & Maggio, F. Ophthalmoplegia in diabetes mellitus: A retrospective study. Acta Diabetol. 46, 23–26. https://doi.org/10.1007/s00592-008-0053-8 (2009).
Article PubMed Google Scholar - Jacobson, D. M., McCanna, T. D. & Layde, P. M. Risk factors for ischemic ocular motor nerve palsies. Arch. Ophthalmol. 112, 961–966. https://doi.org/10.1001/archopht.1994.01090190109029 (1994).
Article CAS PubMed Google Scholar - Lavin, P. J. et al. Isolated trochlear nerve palsy in patients with multiple sclerosis. Neurology 55, 321–322. https://doi.org/10.1212/wnl.55.2.321-a (2000).
Article CAS PubMed Google Scholar - Munakata, A., Ohkuma, H., Nakano, T. & Shimamura, N. Abducens nerve pareses associated with aneurysmal subarachnoid hemorrhage. Incid. Clin. Featur. Cerebrovasc. Dis. 24, 516–519. https://doi.org/10.1159/000110421 (2007).
Article Google Scholar - Rush, J. A. & Younge, B. R. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1000 cases. Arch. Ophthalmol. 99, 76–79. https://doi.org/10.1001/archopht.1981.03930010078006 (1981).
Article CAS PubMed Google Scholar - Thömke, F., Gutmann, L., Stoeter, P. & Hopf, H. C. Cerebrovascular brainstem diseases with isolated cranial nerve palsies. Cerebrovasc. Dis. 13, 147–155. https://doi.org/10.1159/000047768 (2002).
Article PubMed Google Scholar - Coresh, J., Astor, B. C., Greene, T., Eknoyan, G. & Levey, A. S. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 41, 1–12. https://doi.org/10.1053/ajkd.2003.50007 (2003).
Article Google Scholar - Coresh, J. et al. Prevalence of chronic kidney disease in the United States. Jama 298, 2038–2047. https://doi.org/10.1001/jama.298.17.2038 (2007).
Article CAS PubMed Google Scholar - Chadban, S. J. et al. Prevalence of kidney damage in Australian adults: The AusDiab kidney study. J. Am. Soc. Nephrol. 14, S131-138. https://doi.org/10.1097/01.asn.0000070152.11927.4a (2003).
Article PubMed Google Scholar - Jabbari, B. & Vaziri, N. D. The nature, consequences, and management of neurological disorders in chronic kidney disease. Hemodial. Int. 22, 150–160. https://doi.org/10.1111/hdi.12587 (2018).
Article PubMed Google Scholar - Saini, J. S., Jain, I. S., Dhar, S. & Mohan, K. Uremic optic neuropathy. J. Clin. Neuro-ophthalmol. 9, 131–133 (1989).
CAS Google Scholar - Watson, D. et al. A novel multi-biomarker assay for non-invasive quantitative monitoring of kidney injury. J. Clin. Med. 8, 499. https://doi.org/10.3390/jcm8040499 (2019).
Article CAS PubMed PubMed Central Google Scholar - Turin, T. C. et al. Proteinuria and rate of change in kidney function in a community-based population. J. Am. Soc. Nephrol. 24, 1661–1667. https://doi.org/10.1681/ASN.2012111118 (2013).
Article PubMed PubMed Central Google Scholar - Hemmelgarn, B. R. et al. Relation between kidney function, proteinuria, and adverse outcomes. Jama 303, 423–429. https://doi.org/10.1001/jama.2010.39 (2010).
Article CAS PubMed Google Scholar - Paisley, K. E. et al. Endothelial dysfunction and inflammation in asymptomatic proteinuria. Kidney Int. 63, 624–633. https://doi.org/10.1046/j.1523-1755.2003.00768.x (2003).
Article PubMed Google Scholar - Nam, G. E. et al. Chronic renal dysfunction, proteinuria, and risk of Parkinson’s disease in the elderly. Mov. Disord. 34, 1184–1191. https://doi.org/10.1002/mds.27704 (2019).
Article PubMed Google Scholar - Okada, R. et al. Trace proteinuria by dipstick screening is associated with metabolic syndrome, hypertension, and diabetes. Clin. Exp. Nephrol. 22, 1387–1394. https://doi.org/10.1007/s10157-018-1601-3 (2018).
Article CAS PubMed Google Scholar - Park, S. et al. Proteinuria is associated with the development of Crohn’s disease: A nationwide population-based study. J Clin Med https://doi.org/10.3390/jcm10040799 (2021).
Article PubMed PubMed Central Google Scholar - Sun, K. et al. Fatty liver index, albuminuria and the association with chronic kidney disease: a population-based study in China. BMJ Open 8, e019097. https://doi.org/10.1136/bmjopen-2017-019097 (2018).
Article PubMed PubMed Central Google Scholar - Wang, A. et al. Two-year changes in proteinuria and the risk of stroke in the Chinese population: A prospective cohort study. J. Am. Heart Assoc. https://doi.org/10.1161/JAHA.117.006271 (2017).
Article ADS PubMed PubMed Central Google Scholar - Filip, S. et al. Urinary proteomics and molecular determinants of chronic kidney disease: Possible link to proteases. Expert Rev. Proteomics 11, 535–548. https://doi.org/10.1586/14789450.2014.926224 (2014).
Article CAS PubMed Google Scholar - Boulware, L. E., Jaar, B. G., Tarver-Carr, M. E., Brancati, F. L. & Powe, N. R. Screening for proteinuria in US adults: A cost-effectiveness analysis. Jama 290, 3101–3114. https://doi.org/10.1001/jama.290.23.3101 (2003).
Article CAS PubMed Google Scholar - Garg, A. X., Kiberd, B. A., Clark, W. F., Haynes, R. B. & Clase, C. M. Albuminuria and renal insufficiency prevalence guides population screening: results from the NHANES III. Kidney Int. 61, 2165–2175. https://doi.org/10.1046/j.1523-1755.2002.00356.x (2002).
Article PubMed Google Scholar - Mann, J. F., Gerstein, H. C., Pogue, J., Bosch, J. & Yusuf, S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: The HOPE randomized trial. Ann. Intern. Med. 134, 629–636. https://doi.org/10.7326/0003-4819-134-8-200104170-00007 (2001).
Article CAS PubMed Google Scholar - Iseki, K., Ikemiya, Y., Iseki, C. & Takishita, S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 63, 1468–1474. https://doi.org/10.1046/j.1523-1755.2003.00868.x (2003).
Article PubMed Google Scholar - Zandi-Nejad, K., Eddy, A. A., Glassock, R. J. & Brenner, B. M. Why is proteinuria an ominous biomarker of progressive kidney disease?. Kidney Int. Suppl. https://doi.org/10.1111/j.1523-1755.2004.09220.x (2004).
Article PubMed Google Scholar - Sandsmark, D. K. et al. Proteinuria, but Not eGFR, predicts stroke risk in chronic kidney disease: chronic renal insufficiency cohort study. Stroke 46, 2075–2080. https://doi.org/10.1161/STROKEAHA.115.009861 (2015).
Article CAS PubMed PubMed Central Google Scholar - Polkinghorne, K. R. Estimated glomerular filtration rate versus albuminuria in the assessment of kidney function: What’s more important?. Clin. Biochem. Rev. 35, 67–73 (2014).
PubMed PubMed Central Google Scholar - Levey, A. S., Inker, L. A. & Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 63, 820–834. https://doi.org/10.1053/j.ajkd.2013.12.006 (2014).
Article Google Scholar - Peralta, C. A. et al. Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. Jama 305, 1545–1552. https://doi.org/10.1001/jama.2011.468 (2011).
Article CAS PubMed PubMed Central Google Scholar - Shlipak, M. G. et al. Cystatin C versus creatinine in determining risk based on kidney function. N Engl. J. Med. 369, 932–943. https://doi.org/10.1056/NEJMoa1214234 (2013).
Article CAS PubMed PubMed Central Google Scholar - Zhuang, Y. et al. Mitochondrial dysfunction confers albumin-induced NLRP3 inflammasome activation and renal tubular injury. Am. J. Physiol. Renal Physiol. 308, F857-866. https://doi.org/10.1152/ajprenal.00203.2014 (2015).
Article CAS PubMed Google Scholar - Iff, S. et al. Relative energy balance, CKD, and risk of cardiovascular and all-cause mortality. Am. J. Kidney Dis. 63, 437–445. https://doi.org/10.1053/j.ajkd.2013.08.026 (2014).
Article PubMed Google Scholar - Kshirsagar, A. V. & Grubbs, V. Periodontal disease and CKD-associated morbidity: Is there now enough evidence to move from observation to intervention?. Am. J. Kidney Dis. 66, 181–183. https://doi.org/10.1053/j.ajkd.2015.05.009 (2015).
Article PubMed Google Scholar - Warnock, D. G., Delanaye, P. & Glassock, R. J. Risks for all-cause mortality: Stratified by age, estimated glomerular filtration rate and albuminuria. Nephron 136, 292–297. https://doi.org/10.1159/000455197 (2017).
Article PubMed Google Scholar - Cheng, T. Y. et al. Mortality risks for all causes and cardiovascular diseases and reduced GFR in a middle-aged working population in Taiwan. Am. J. Kidney Dis. 52, 1051–1060. https://doi.org/10.1053/j.ajkd.2008.05.030 (2008).
Article CAS PubMed Google Scholar - Chronic Kidney Disease Prognosis, C. et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375, 2073–2081. https://doi.org/10.1016/S0140-6736(10)60674-5 (2010).
- Wu, J. et al. Association of estimated glomerular filtration rate and proteinuria with all-cause mortality in community-based population in China: A result from Kailuan study. Sci. Rep. 8, 2157. https://doi.org/10.1038/s41598-018-20554-3 (2018).
Article ADS CAS PubMed PubMed Central Google Scholar - Yahalom, G. et al. Chronic kidney disease and clinical outcome in patients with acute stroke. Stroke 40, 1296–1303. https://doi.org/10.1161/STROKEAHA.108.520882 (2009).
Article PubMed Google Scholar - Okumura, N. et al. Associations of proteinuria and the estimated glomerular filtration rate with incident hypertension in young to middle-aged Japanese males. Prev. Med. 60, 48–54. https://doi.org/10.1016/j.ypmed.2013.12.009 (2014).
Article PubMed Google Scholar - Widhi Nugroho, A. et al. The association between glomerular filtration rate estimated on admission and acute stroke outcome the shiga stroke registry. J. Atheroscler. Thromb. 25, 570–579. https://doi.org/10.5551/jat.42812 (2018).
Article PubMed Google Scholar - Gaziano, L. et al. Mild-to-moderate kidney dysfunction and cardiovascular disease: Observational and mendelian randomization analyses. Circulation 146, 1507–1517. https://doi.org/10.1161/circulationaha.122.060700 (2022).
Article CAS PubMed PubMed Central Google Scholar - Rucker, C. W. The causes of paralysis of the third, fourth and sixth cranial nerves. Am. J. Ophthalmol. 61, 1293–1298. https://doi.org/10.1016/0002-9394(66)90258-3 (1966).
Article CAS PubMed Google Scholar - Richards, B. W., Jones, F. R. Jr. & Younge, B. R. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am. J. Ophthalmol. 113, 489–496. https://doi.org/10.1016/s0002-9394(14)74718-x (1992).
Article CAS PubMed Google Scholar - Rim, T. H., Han, J., Choi, Y. S., Lee, T. & Kim, S. S. Stroke risk among adult patients with third, fourth or sixth cranial nerve palsy: A Nationwide cohort study. Acta Ophthalmol. 95, e656–e661. https://doi.org/10.1111/aos.13488 (2017).
Article PubMed Google Scholar - Park, S. J., Yang, H. K., Byun, S. J., Park, K. H. & Hwang, J. M. Ocular motor cranial nerve palsy and increased risk of stroke in the general population. PLoS One 13, e0205428. https://doi.org/10.1371/journal.pone.0205428 (2018).
Article CAS PubMed PubMed Central Google Scholar - Kang, D. H. et al. Role of the microvascular endothelium in progressive renal disease. J. Am. Soc. Nephrol. 13, 806–816. https://doi.org/10.1681/asn.V133806 (2002).
Article PubMed Google Scholar - Doostkam, A., Mirkhani, H., Iravani, K., Karbalay-Doust, S. & Zarei, K. Effect of rutin on diabetic auditory neuropathy in an experimental rat model. Clin. Exp. Otorhinolaryngol. 14, 259–267. https://doi.org/10.21053/ceo.2019.02068 (2021).
Article CAS PubMed Google Scholar - Pedrinelli, R. et al. Microalbuminuria and endothelial dysfunction in essential hypertension. Lancet (London, England) 344, 14–18. https://doi.org/10.1016/s0140-6736(94)91047-2 (1994).
Article CAS PubMed Google Scholar - Jensen, J. S., Borch-Johnsen, K., Jensen, G. & Feldt-Rasmussen, B. Microalbuminuria reflects a generalized transvascular albumin leakiness in clinically healthy subjects. Clin. Sci. 88, 629–633. https://doi.org/10.1042/cs0880629 (1995).
Article CAS Google Scholar - Kario, K. et al. Factor VII hyperactivity and endothelial cell damage are found in elderly hypertensives only when concomitant with microalbuminuria. Arterioscler. Thromb. Vasc. Biol. 16, 455–461. https://doi.org/10.1161/01.atv.16.3.455 (1996).
Article CAS PubMed Google Scholar - Shen, L. et al. Von Willebrand factor, ADAMTS13 activity, TNF-α and their relationships in patients with chronic kidney disease. Exp. Therap. Med. 3, 530–534. https://doi.org/10.3892/etm.2011.432 (2012).
Article CAS Google Scholar - Wardlaw, J. M., Sandercock, P. A., Dennis, M. S. & Starr, J. Is breakdown of the blood-brain barrier responsible for lacunar stroke, leukoaraiosis, and dementia?. Stroke 34, 806–812. https://doi.org/10.1161/01.STR.0000058480.77236.B3 (2003).
Article CAS PubMed Google Scholar - Seong, S. C. et al. Cohort profile: The National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 7, e016640. https://doi.org/10.1136/bmjopen-2017-016640 (2017).
Article PubMed PubMed Central Google Scholar - Song, S. O. et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diab. Metab. J. 38, 395–403. https://doi.org/10.4093/dmj.2014.38.5.395 (2014).
Article Google Scholar - Kim, J., Han, K., Yoo, J., Park, K. A. & Oh, S. Y. Liver enzymes and risk of ocular motor cranial nerve palsy: a nationwide population-based study. Neurol Sci 43, 3395–3405. https://doi.org/10.1007/s10072-021-05735-9 (2022).
Article PubMed Google Scholar - Agarwal, D. P. Cardioprotective effects of light-moderate consumption of alcohol: a review of putative mechanisms. Alcohol Alcohol. (Oxford, Oxfordshire) 37, 409–415. https://doi.org/10.1093/alcalc/37.5.409 (2002).
Article CAS Google Scholar - Kim, M. K. et al. Clinical practice guidelines for overweight and obesity in Korea. Endocrinol. Metab. (Seoul) 29, 405–409. https://doi.org/10.3803/EnM.2014.29.4.405 (2014).
Article PubMed Google Scholar - Alberti, K. G. et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644 (2009).
Article CAS PubMed Google Scholar - White, S. L. et al. Diagnostic accuracy of urine dipsticks for detection of albuminuria in the general community. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 58, 19–28. https://doi.org/10.1053/j.ajkd.2010.12.026 (2011).
Article Google Scholar - Lim, D. et al. Diagnostic accuracy of urine dipstick for proteinuria in older outpatients. Kidney Res. Clin. Pract. 33, 199–203. https://doi.org/10.1016/j.krcp.2014.10.003 (2014).
Article PubMed PubMed Central Google Scholar
Funding
This research was supported by a grant (No. NRF-2021R1A2C1007718 to Kyung-Ah Park) of the National Research Foundation (NRF) funded by the Korean government (MSIT) and a grant (NTX 121267 to Sei Yeul Oh) of the Basic Science Research Program through the NRF funded by the Ministry of Science and ICT, Republic of Korea.
Author information
Author notes
- These authors contributed equally: Juha Lee and Kyungdo Han.
Authors and Affiliations
- Department of Ophthalmology, Kangwon National University Hospital, Chuncheon, Republic of Korea
Juha Lee - Department of Statistics and Actuarial Science, Soongsil University, Seoul, Republic of Korea
Kyungdo Han - Department of Biomedicine and Health Science, The Catholic University of Korea, Seoul, Republic of Korea
Juhwan Yoo - Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul, 06351, Republic of Korea
Kyung-Ah Park & Sei Yeul Oh
Authors
- Juha Lee
You can also search for this author inPubMed Google Scholar - Kyungdo Han
You can also search for this author inPubMed Google Scholar - Juhwan Yoo
You can also search for this author inPubMed Google Scholar - Kyung-Ah Park
You can also search for this author inPubMed Google Scholar - Sei Yeul Oh
You can also search for this author inPubMed Google Scholar
Contributions
Kyung-Ah Park and Kyungdo Han contributed to the study concept and study design. Juhwan Yoo and Kyungdo Han contributed to data collection. Juhwan Yoo, and Kyungdo Han contributed to data analysis and data interpretation. Juha Lee and Kyung-Ah Park drafted the manuscript. Kyung-Ah Park and Sei Yeul Oh performed critical revision of the manuscript for intellectual contents.
Corresponding authors
Correspondence toKyung-Ah Park or Sei Yeul Oh.
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, J., Han, K., Yoo, J. et al. Proteinuria and risk of ocular motor cranial nerve palsy: a nationwide population-based study.Sci Rep 14, 12012 (2024). https://doi.org/10.1038/s41598-024-62576-0
- Received: 25 September 2023
- Accepted: 20 May 2024
- Published: 26 May 2024
- DOI: https://doi.org/10.1038/s41598-024-62576-0